Abstract
HIV disclosure to sexual partners facilitates joint decision-making and risk reduction strategies for safer sex behaviors, but disclosure may be impacted by depression symptoms. Disclosure is also associated with disclosure self-efficacy, which in turn may also be influenced by depressive symptoms. This study examined the relationship between depression and HIV disclosure to partners following diagnosis among men who have sex with men (MSM), mediated by disclosure self-efficacy. Newly HIV-diagnosed MSM (n = 92) who reported sexual activity after diagnosis completed an assessment soon after diagnosis which measured depressive symptoms, and another assessment within 3 months of diagnosis that measured disclosure self-efficacy and disclosure. Over one-third of the sample reported elevated depressive symptoms soon after diagnosis and equal proportions (one-third each) disclosed to none, some, or all partners in the 3 months after diagnosis. Depressive symptoms were negatively associated with disclosure self-efficacy and disclosure to partners, while disclosure self-efficacy was positively associated with disclosure. Disclosure self-efficacy partially mediated the relationship between depression and disclosure, accounting for 33% of the total effect. These findings highlight the importance of addressing depression that follows diagnosis to enhance subsequent disclosure to sexual partners.
Introduction
HIV disclosure is an important protective behavior for people living with HIV (PLHIV). Disclosure to individuals within one's social network can lead to improved behavior and health outcomes, such as adherence,1,2 and may lead to improvements in mental well-being.3 Disclosure to sexual partners facilitates communication and informed decision making about sexual behaviors and risks. Although findings have been mixed regarding the impact of disclosure on decreasing unprotected sex,4 disclosure has been associated with intermediate factors related to greater chance of protected sex, such as increased discussions about condom use and safer sex.5
Disclosure can promote other strategies that PLHIV, and men who have sex with men (MSM) living with HIV in particular, use to engage in safer sex behaviors, such as facilitating pre-exposure prophylaxis6 and serosorting.7 Because of the potential for HIV disclosure to improve sexual communication and health, it is important to understand what factors, such as depression, affect disclosure early in the course of living with HIV.
Making decisions about disclosure can act as a potent stressor, as those who are newly diagnosed deal with the fears and consequences of whether to disclose.8 Men living with HIV have difficulty disclosing their HIV status to their sexual partners,9 and MSM are less likely to disclose to all of their sexual partners compared to women and heterosexual men.10 In deciding to disclose, PLHIV weigh the benefits and risks of sharing one's serostatus.11
For MSM living with HIV, they may benefit from disclosure by gaining control, sharing responsibility for sexual risk with partners, and eliciting social support.12 The social support that can result from disclosure may foster coping and psychological adjustment to diagnosis.13 MSM may decide to avoid the risks of disclosure when fearing a negative reaction, rejection, or stigma.12 Nondisclosure may be socially isolating, but serves as an option for some PLHIV to help them assert control over coping with their serostatus by avoiding potentially stressful and stigmatizing disclosure encounters.8
Disclosure to sexual partners after diagnosis may be influenced by depressive symptoms. Rates of depression among both PLHIV14 and MSM15 are higher than the general population. Depression is often exacerbated by stressful life events, and although HIV is becoming increasingly manageable, an HIV diagnosis can raise emotional distress that increases depressive symptoms.16 Depressive symptoms that occur after diagnosis may limit one's ability to cope with the stress of diagnosis and disclosure, therefore affecting decision making17 and potentially leading to fewer disclosures.
PLHIV may also turn to substance use (e.g., alcohol and drugs) as a maladaptive coping mechanism to deal with diagnosis, which may exacerbate depressive symptoms and negatively impact disclosure. While depression may co-vary with or result from negative disclosure experiences,18–20 for disclosures to family and friends,21,22 less is known about how depression following diagnosis (whether it precedes or results from diagnosis) impacts subsequent disclosure to sexual partners. Depression may reduce the motivation to disclose in the context of sexual relationships9 and may affect how MSM living with HIV weigh the benefits and risks in deciding to disclose to their sexual partners, (i.e., engaging in disclosure to garner emotional and social support and reduce risk behaviors with partners, or refraining from disclosure to regain control and avoid stigma and rejection).8
Disclosure may be impacted by depression following diagnosis through the intermediate effects of disclosure self-efficacy. Self-efficacy is people's belief in their ability to perform a certain behavior under specified conditions,23 and thus self-efficacy for disclosure is believing that one can disclose an HIV status under a certain set of circumstances and with certain partner types.24 Disclosure self-efficacy is a strong predictor of disclosure,9 such that those with lower disclosure self-efficacy are more likely to avoid disclosure or inconsistently disclose to sexual partners.25 The negative impact of depression on self-efficacy for safer sex has been demonstrated for MSM,26,27 but it is not known how depression influences self-efficacy for disclosure.
The purpose of this study is to examine the relationship between depression and disclosure to sexual partners in the initial stages of coping with an HIV diagnosis. Studies examining how disclosure patterns develop over the course of living with HIV, including immediately after diagnosis, are limited.28 Understanding how depression and self-efficacy affect disclosure behaviors immediately after diagnosis can help inform interventions to improve disclosure. To explore how depression affects disclosure, disclosure self-efficacy was tested as a mediator of the relationship between depression and disclosure to sexual partners. Identifying the mechanisms that influence the disclosure process to sexual partners after diagnosis may provide insights into the development of long-term health behavior patterns that reduce the risk of onward HIV transmission.
Methods
Participants and procedures
Study participants were recruited between June 2009 and May 2011 for enrollment into a randomized control trial testing a brief risk reduction intervention delivered to newly HIV-diagnosed patients.29 The research was conducted in a Federally Qualified Community Health Center in New York City which serves lesbian, gay, bisexual, and transgender communities. Recruitment at the Health Center occurred during the HIV post-test counseling or the initial HIV care visit with a health care provider, and interested patients were referred to study staff who administered the assessment to screen for study eligibility.
Eligible participants were required to have received an HIV diagnosis in the previous 3 months, were 18 years or older, reported having unprotected anal intercourse with a male in the 3 months prior to diagnosis, identified as male sex at birth (regardless of current gender identity), and were fluent in English.
In total, 152 individuals completed the screening assessment, and of those, 119 met the eligibility criteria. Of those eligible, 102 participants then completed a second assessment (baseline for intervention trial, approximately 3 months after HIV diagnosis) prior to enrolling in the full trial. Hereafter, the screening and baseline assessments are referred to as the Time 1 and Time 2 assessments, respectively. The Time 1 (screening) assessment occurred 41 days, on average, after HIV diagnosis, and the Time 2 (baseline) assessment occurred 45 days, on average, after the Time 1 assessment.
The assessments were administered by study staff in a private setting using a combination of Computer Assisted Self Interview (CASI) and a time-line follow back (TLFB) calendar. The TLFB aided the recall of detailed sexual activity and substance use behaviors over the 3-month period after diagnosis that was measured at the Time 2 assessment.30 Study procedures were approved by the ethical review boards at all participating institutions, and participants provided written consent after learning about the study procedures.
Measures
Demographic characteristics
Demographic information was measured at the Time 1 assessment and included age, ethnicity, education, income, and employment.
Depressive symptoms
The Beck Depression Inventory (BDI) was administered during the Time 1 assessment to measure self-reported depressive symptoms.31 The 21-item measure reflects affective, behavioral, cognitive, and somatic symptoms of depression in the previous week. Each question has a response range of 0–3, with a higher value indicating more depression and total scores range between 0–63 (α = 0.89). A score of 16 or higher on the BDI met the clinical cut-point for elevated depressive symptoms and was used for descriptive analysis.
Substance use
Using the TLFB administered at the Time 2 assessment, participants reported if they had any alcohol or drug use (yes/no) in the 3 months after diagnosis. For alcohol use, participants identified the days during which they drank and the total number of drinks consumed in this period. This information was used to calculate the mean number of drinking days per month, mean number of drinks per month, and mean number of drinks per drinking occasion.
Sexual behavior
Participants reported on the TLFB if they had a primary sexual partner and the total number of sexual partners in the 3 months after diagnosis (on the Time 2 assessment). Participants also indicated all the occasions when they had sexual intercourse, whether the sex was protected, and the serostatus of their partner. This information was used to create two binary indicators (yes/no) for the 3 months after diagnosis: (1) having had unprotected sex with an HIV negative or unknown serostatus partner; and (2) having had protected sex only.
Disclosure
At the Time 2 assessment, participants reported the total number of sexual partners in the 3 months since diagnosis to whom they disclosed their HIV status. This form of the disclosure variable as a continuous count was used in the mediation analysis. Further, from the reported total number of sexual partners to whom to disclose, an additional variable was created for categories of disclosure—categorized as ‘none,’ ‘some,’ and ‘all’ for what proportion of their sexual partners to whom the participants disclosed. This categorized form of the disclosure outcome was used in describing the sample. Participants who reported no sexual partners in the 3 months after diagnosis did not complete the question regarding disclosure to sexual partners.
Disclosure self-efficacy
During the Time 2 assessment, participants responded to three brief vignettes describing situations in which they meet a hypothetical sex partner.24 After reading each vignette, the participants were asked “How confident are you that you could make an effective decision of whether to tell this person you are HIV positive in this situation?” to which they responded on a 10-point scale, with a higher response indicating greater disclosure self-efficacy. The three items factored onto one dimension and the total scores ranged between 0–30 (α = 0.88).
Analysis
Of the 102 participants who completed both the Time 1 and Time 2 assessments, the sample used for analysis only included participants who reported sexual activity in the 3 months after diagnosis (n = 94 or 92.2% of the sample), and therefore completed the Time 2 assessment question about disclosing to sexual partners. Additionally, two participants were excluded who reported sexual partners but were missing data on disclosure, for a final sample size of 92. The 10 participants excluded from the analysis were not significantly different on age, disclosure self-efficacy, and elevated depressive symptoms (BDI ≥16). However, all 10 participants excluded from the analysis reported at least some college.
To describe the relationships between the key study variables and risk behaviors, bivariate analyses were conducted for three tasks. First, the associations of the elevated depressive symptoms cutpoint (BDI ≥16 vs. <16) with demographic characteristics, substance use, and sexual risk behaviors were explored by calculating frequencies and conducting chi-square tests with dichotomous covariates, and by calculating means and conducting t-tests with continuous covariates. Second, the Pearson correlation coefficients were calculated among the key study variables of interest. Third, the Pearson chi-square test was used to compare sexual behaviors among the three categories for disclosure based on the proportion of partners to whom the participant has disclosed (none, some, all).
To test the hypothesis that disclosure self-efficacy mediates the relationship between depression and disclosure to sexual partners, a series of three regression equations were conducted using the continuous count disclosure variable:
 |
 |
 |
where f is a log-link function for the Poisson distribution for the count outcome, Y is the count of disclosure to sex partners, X is the depression score, and M is the disclosure self-efficacy score. Equation 1 calculated the relationship between depressive symptoms and disclosure (c effect). Equation 2 tested the association between depressive symptoms and disclosure self-efficacy (a effect). Equation 3 computed the effect of depressive symptoms (c' effect) on disclosure while adjusting for disclosure self-efficacy (b effect) (Fig. 1).
FIG. 1.
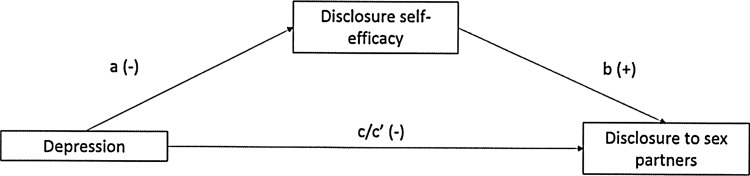
Model of the mediation analysis with the hypothesized direction of the relationship between variables.
Using the PROC GENMOD procedure in SAS 9.2 (SAS Institute, Cary, NC), Poisson regression was conducted for the disclosure count outcome in Equations 1 and 3, and linear regression analysis for the disclosure self-efficacy continuous outcome in Equation 2. Each regression equation was adjusted for three covariates that were possible confounders: race, any alcohol use, and having a main sexual partner in the 3 months after diagnosis. In addition, each model controlled for the total number of sexual partners in the 3 months after diagnosis to adjust for participants with a greater total number of sexual partners to whom they could disclose.
A significant Poisson regression coefficient (β) indicates the difference in the rate of disclosure to sexual partners based on a one unit increase in the independent variable. Exponentiating this coefficient (i.e., exp(β)) represents the ratio of the mean number of disclosures that occur between any one-unit increment along the independent variable.
To determine the mediated effect, the products of coefficients approach was used because this calculation has high statistical power while maintaining accurate Type I errors.32 This approach determined the coefficient relating depressive symptoms to disclosure self-efficacy (a) and the coefficient relating disclosure self-efficacy to disclosure (b) while controlling for depressive symptoms, and computed the products of these coefficients (a*b). The standard error for the asymmetric distribution of the products of the coefficients was calculated for the confidence interval for the mediated effect using RMediation.33 Finally, the percent of the total effect of depressive symptoms on disclosure that was mediated by disclosure self-efficacy was computed using the ab/(c' + ab) as this calculation does not require standardization of the coefficients across regression equations.34
Results
Characteristics of the sample
The sample consisted of 92 newly HIV diagnosed MSM (Table 1). Participants had a mean age of 32 (SD = 8.4) and were ethnically diverse (15.2% black, 31.5% Hispanic/Latino, 37.0% white, and 16.3% other). Approximately three-quarters (72.8%) reported that they earned less than $30,000 annually, and three-quarters (76.1%) had at least some college education. Over two-thirds (69.6%) were employed or a student. Over two-thirds (65.2%) used any alcohol, and under half (40.2%) reported using any drugs in the 3 months after diagnosis. All participants reported having sex with male partners only.
Table 1.
Characteristics of the Sexually Active Sample (n = 92) by Elevated Depression Cutpoint
| Total sample(n = 92) | Elevated depression (BDI ≥16)(n = 37) | Non-elevated depression (BDI <16)(n = 55) | |||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | p Value | |
| Age (Mean, SD) | 31.8 | 8.4 | 31.5 | 7.0 | 32.0 | 9.3 | 0.80 |
| Ethnicity | 0.89 | ||||||
| African American/black | 14 | 15.2 | 5 | 13.5 | 9 | 16.4 | |
| Hispanic/Latino | 29 | 31.5 | 10 | 27.0 | 19 | 34.6 | |
| Other (Asian, Pacific Islander, Native American) | 15 | 16.3 | 7 | 19.0 | 8 | 14.4 | |
| White | 34 | 37.0 | 15 | 40.5 | 19 | 34.6 | |
| Education | 0.28 | ||||||
| High school or less | 22 | 23.9 | 11 | 29.7 | 11 | 20.0 | |
| At least some college | 70 | 76.1 | 26 | 70.3 | 44 | 80.0 | |
| Income | 0.65 | ||||||
| ≤$30,000 | 67 | 72.8 | 26 | 70.3 | 41 | 74.6 | |
| Over $30,000 | 25 | 27.2 | 11 | 29.7 | 14 | 25.4 | |
| Employment | 0.56 | ||||||
| Employed/student | 64 | 69.6 | 27 | 73.0 | 37 | 67.3 | |
| Unemployed/disabled | 28 | 30.4 | 10 | 27.0 | 18 | 32.7 | |
| Substance use @ Time 2 | |||||||
| Drank alcohol (any) | 60 | 65.2 | 18 | 47.7 | 42 | 76.4 | <0.01 |
| Mean number of drinking days per month (Mean, SD) (n = 60) | 10.7 | 9.2 | 10.8 | 9.4 | 10.6 | 9.2 | 0.94 |
| Mean number of drinks per month (Mean, SD) (n = 60) | 38.1 | 43.3 | 49.2 | 59.2 | 33.3 | 34.1 | 0.30 |
| Mean drinks per drinking occasion (Mean, SD) (n = 60) | 3.1 | 1.7 | 3.6 | 2.4 | 2.9 | 1.3 | 0.21 |
| Drug use (any) | 37 | 40.2 | 15 | 40.5 | 22 | 40.0 | 0.96 |
| Sexual behavior @ Time 2 | |||||||
| Had a primary partner | 40 | 43.5 | 17 | 46.0 | 23 | 41.8 | 0.70 |
| Number of partners (Mean, SD) | 5.6 | 8.0 | 6.4 | 10.1 | 5.0 | 6.3 | 0.45 |
| Had unprotected sex with HIV- or HIV unknown serostatus partner | 27 | 29.4 | 10 | 27.0 | 17 | 30.9 | 0.69 |
| Had protected sex only | 32 | 34.8 | 13 | 35.1 | 19 | 34.6 | 0.95 |
| Key study variables | |||||||
| Depression (Mean, SD) | 15.3 | 9.6 | 25.1 | 23.2 | 8.7 | 7.4 | <0.001 |
| Disclosure self-efficacy (Mean, SD) | 16.3 | 9.3 | 13.7 | 10.7 | 18.1 | 15.6 | 0.03 |
| Number of disclosures to partners (Mean, SD) | 2.3 | 3.6 | 2.3 | 3.5 | 2.2 | 3.7 | 0.92 |
For comparing differences between participants with and without elevated depression symptoms, the t statistic was calculated when comparing continuous variables and the X2 statistic for comparing categorical variables.
In the 3 months after diagnosis, almost a third (29.4%) reported at least one occasion of unprotected anal intercourse that occurred with a seronegative or a serostatus-unknown partner at risk for HIV transmission, and just over a third (34.8%) reported only having protected intercourse. Less than half (43.5%) had a primary sexual partner. Participants reported a mean of 5.6 partners (median = 2, SD = 8.0) during the 3 months following diagnosis. No significant associations were found between elevated depression and demographic characteristics and sexual risk behaviors. However, participants who reported any drinking were less likely to report elevated depressive symptoms (BDI ≥16).
Description of depression, disclosure self-efficacy, and disclosure to sexual partners
At the Time 1 assessment, participants reported a mean depressive symptoms score of 15.3 (SD = 9.6, range 0–37) (Table 1). Over a third (n = 37, 39.2%) reached the threshold (BDI ≥16) for mild elevated depression. In the 3 months after diagnosis at the Time 2 assessment, participants had a mean disclosure self-efficacy score of 16.8 (SD = 9.0, range 0–27) and disclosed their HIV status to a mean number of 2.3 sexual partners (SD = 3.6, range 0–24).
Depressive symptoms were negatively correlated with disclosure self-efficacy (r = −0.28, p = 0.007) and disclosure self-efficacy was positively correlated with number of disclosures (r = 0.25, p = 0.02). Number of sexual partners was highly correlated with number of disclosures (r = 0.65, p < 0.001). Although depression was not significantly associated with number of disclosures, this finding is expected given that the bivariate association does not adjust for the potential for greater disclosures among those who report more total sexual partners.
Disclosure to sexual partners
On average, participants shared their status with nearly half of their partners (mean disclosure rate = 0.47, SD = 0.48). Nearly a third (n = 29, 31.5%) reported disclosing their status to all of their sexual partners in the 3 months after diagnosis, and an approximately equal proportion reported disclosing to none (n = 30, 32.6%) and some (n = 33, 35.9%) of their sexual partners (Table 2).
Table 2.
Relationship Between Sexual Behaviors at Time 2 Assessment and Disclosure to Sexual Partners
| Disclosed to no partners(n = 30) n, % | Disclosed to some partners(n = 33) n, % | Disclosed to all partners(n = 29) n, % | χ2 | |
|---|---|---|---|---|
| Had a primary partner | ||||
| Yes | 13 (43.3) | 12 (36.4) | 15 (51.7) | 1.48 |
| No | 17 (56.7) | 21 (63.6) | 14 (48.3) | |
| Number of sex partners | ||||
| One to two | 22 (73.3) | 5 (15.1) | 20 (69.0) | 28.81*** |
| Three to six | 5 (16.7) | 12 (36.4) | 6 (20.7) | |
| Seven or more | 3 (10.0) | 16 (48.5) | 3 (10.3) | |
| Had unprotected sex with HIV- or HIV unknown serostatus partner | ||||
| Yes | 4 (13.3) | 15 (45.5) | 8 (27.6) | 7.88* |
| No | 26 (86.7) | 18 (54.6) | 21 (72.4) | |
| Had protected sex only | ||||
| Yes | 16 (53.3) | 10 (30.3) | 6 (20.7) | 7.38* |
| No | 14 (46.7) | 23 (69.7) | 23 (79.3) | |
Because the disclosure question was not linked to specific sexual partners, participants could report more disclosures than sexual partners. Three participants disclosed to a greater number of partners than they had reported in the3 months after diagnosis. These three participants disclosed to either one or two additional partners and were placed in the “disclosed to all” category. *p < 0.05; ***p < 0.001.
Having a primary partner was not significantly associated with the degree of disclosure (χ2 = 1.48, p = 0.48). Participants who disclosed to some of their partners were significantly more likely to have had seven or more sex partners (48.5% for disclosure to some partners vs. 10.0% for disclosure to no partners, and 10.3% for disclosure to all partners, χ2 = 28.81, p < 0.001). Participants who disclosed to none or to all of their sexual partners were less likely to report having had unprotected sex with an HIV negative or unknown partner compared to those who disclosed to some of their partners (13.3% for none and 27.6% for all vs. 45.5% for some disclosure, χ2 = 7.88, p = 0.02). Participants who disclosed to none of their partners were more likely to have had protected sex only compared to those who disclosed to all partners (53.3% for none vs. 20.7% for all, χ2 = 7.38, p = 0.02).
Mediation analysis
In the mediation analysis (Table 3), the total effect of depressive symptoms at the Time 1 assessment was associated with fewer disclosures to sexual partners following diagnosis (βc = −0.026, SD = 0.009, χ2 = 11.33, p < 0.001). For every one unit increase in the depressive symptoms, the rate ratio indicates that participants disclosed to 2.9% fewer partners. As depressive symptoms increased, disclosure self-efficacy decreased (βa = −0.272, SE = 0.099, t = 7.59, p < 0.01).
Table 3.
Regression Models to Test Relationship Between Depression and Disclosure to Sex Partners Mediated by Disclosure Self-Efficacy (n = 92)
| Multiple regression modela | |||||||
|---|---|---|---|---|---|---|---|
| Outcome | Predictor | Path | β (SE) | Statistic | 95% CI | p | Rate ratio (eβ) |
| Disclosure to sex partner | Depression | c | −0.029 (0.009) | 11.33 | −0.046, −0.012 | <0.001 | 0.971 |
| Disclosure self-efficacy | Depression | a | −0.272 (0.099) | 7.59 | −0.465, −0.078 | <0.01 | – |
| Disclosure to sex partner | Disclosure self-efficacy | b | 0.037 (0.010) | 14.02 | 0.018, 0.056 | <0.001 | 1.038 |
| Depression | c' | −0.020 (0.009) | 4.77 | −0.038, −0.002 | 0.02 | 0.980 | |
| a*b product | −0.01 (0.005) | −0.022, −0.002 | – | ||||
All models adjusted for race, number of sex partners in the 3 months after diagnosis, any drinking in the 3 months after diagnosis, and having a main sex partner in the 3 months after diagnosis.
Disclosure self-efficacy was positively associated with the number of partners to whom one disclosed (βb = 0.037, SE = 0.010, χ2 = 14.02, p < 0.001) when adjusting for depressive symptoms. A one unit increase in the disclosure self-efficacy score was associated with disclosure to 3.8% more partners. Depressive symptoms were attenuated, but still significantly associated with disclosure (βc' = −0.020, SE = 0.009, χ2 = 4.77, p = 0.02) once disclosure self-efficacy was included in the model.
The relationship between depressive symptoms and disclosure was partially mediated by disclosure self-efficacy. The statistically significant effect of depression on disclosure (c path) was attenuated when disclosure self-efficacy was included in the model (c' path). The products of the coefficients was significant as determined by the 95% asymmetric confidence interval (a*b = −0.01, SE = 0.005, 95% CI = −0.022, −0.002). The indirect effect of disclosure self-efficacy accounted for 33% of the total effect of depressive symptoms on disclosure (ab/(c'+ab) = −0.01/(−0.02 + −0.01) = 0.33).
Discussion
Among a sample of newly diagnosed MSM, participants reported high levels of depressive symptoms and those with more depressive symptoms disclosed to fewer sexual partners in the first 3 months after diagnosis. Previous research showed that depression is highly co-morbid with HIV35 and that moderate levels of depression among PLHIV are associated with sexual risk behaviors36 and reduced adherence to antiretroviral therapy,37 impacting the transmission of HIV. The study findings suggest that depression also may negatively impact disclosure, another behavior potentially linked to the transmission of HIV.
This relationship between depressive symptoms and disclosure was partially mediated by disclosure self-efficacy, such that having more depressive symptoms was associated with less disclosure self-efficacy, which in turn was associated with fewer disclosures to sexual partners. These findings highlight the need to address mental health symptoms among MSM who are newly diagnosed, as a direct means to improve disclosure to sexual partners, as well as an indirect way by addressing disclosure self-efficacy as an important intermediate target for disclosure.
The influence of depression on disclosure is brought to bear by how high the levels of depression are among the sample of newly HIV-diagnosed MSM, which were slightly above the 20–30% prevalence of depression among patients engaged in HIV care.35 The elevated depressive symptoms may have resulted from adjustment disorder that emerges from heightened emotional distress following diagnosis with a potentially life threatening illnesses, such as HIV.38
In addition to adjustment disorder, the presence of elevated depressive symptoms soon after diagnosis may also indicate that the participants had depression disorder present prior to diagnosis, which is prevalent among MSM.39 While the BDI has previously measured high rates of depression among PLHIV, this finding was driven by the close association between somatic symptoms of depression and HIV-related symptoms in a time before highly active antiretroviral therapy (HAART) was available.40 With the advent and benefits of HIV treatment, the association between high rates of depression and somatic symptoms as measured with the BDI may be less pronounced.
This study cannot distinguish between depressive symptoms that resulted from adjustment disorder, from the potential correlation between somatic symptoms and depression and HIV-related symptoms, or from an underlying depressive disorder, because participants were enrolled only after their HIV diagnosis, self-reported their depressive symptoms, and did not report their HIV-related symptoms concurrently with the BDI. Future research exploring the impact of diagnosis on depression should consider assessing depression and HIV symptomatology at the time of HIV testing in order to get a baseline measure with which to compare post-diagnosis depression.
Similar proportions of participants disclosed to all, some, or none of their sexual partners. These categories may be mapped onto how newly diagnosed MSM utilize different strategies that guide their decisions to disclose. Qualitatively these categories may suggest different approaches for coping with HIV; disclosing to: (1) no one to maintain privacy, and avoid stigma and reprisal; (2) some people to choose selectively those who were anticipated as providing the most support; and (3) nearly everyone to avoid keeping secrets and garner maximum social support.8
PLHIV have also been shown to disclose to sexual partners selectively based on the partner type (e.g., primary or casual) and serostatus.10 For disclosures to sexual partners, the distribution in the amount of disclosure categories was associated with the number of sexual partners. MSM with fewer partners were more likely to disclose to none or all their partners, which suggests that MSM with the most partners have to make the most choices around selecting and enacting a disclosure approach, which may change over time. While disclosure to sexual partners is not consistently related to increased safer sex behaviors,19 disclosure is a necessary precursor to jointly managing risk reduction strategies between partners. Disclosure studies that use longitudinal designs with longer follow-up periods are needed to characterize how these patterns of disclosure following diagnosis are related to the characteristics and expectations for the relationships that MSM have with their sexual partners (e.g., casual or committed).
The findings support the hypothesis that depression is associated with fewer disclosures to sexual partners. In addition, the study provides evidence for a mediation mechanism by which depression affects disclosure behavior. The mediation pathway for disclosure self-efficacy accounts for just under half of the total effect of depression on disclosure to sexual partners. Fostering self-efficacy has been shown to be an important predecessor for enhancing behaviors tied to health outcomes.41,42 While the findings establish an association between depression and disclosure to sexual partners, how depression continues to impact patterns of disclosure over time via a pathway through disclosure self-efficacy needs to be examined.
The disclosure patterns that develop in the period immediately after diagnosis may set the course for disclosure to sexual partners long after diagnosis. Similar patterns have been found for other sexual risk behaviors, in which an initial risk behavior has great influence on how that risk behavior persist over time.43 If depression at diagnosis does have a long-term effect on disclosure patterns, then it will be necessary to intervene on depression early in the course of living with HIV, starting at the time of diagnosis.
The results of this study should be considered with regards to the following limitations. First, participants were recruited into the study, on average, over a month after diagnosis. Because depression was not measured before diagnosis, it was impossible to distinguish whether participants already had depressive symptoms and/or developed depressive symptoms as a result of adjustment disorder following diagnosis. However, both sources of depression potentially impact disclosure.
Second, the data for disclosure to sexual partners was measured broadly as the total number of disclosures, rather than disclosures linked to specific sexual partners. Participants who were not sexually active following diagnosis may have had sexual partners before diagnosis to whom they disclosed, but those participants did not report on disclosure to sexual partners and were excluded from the analysis. Participants who were sexually active may have also reported disclosing to past sexual partners with whom they were not sexually active after diagnosis. Due to the inability to link disclosure to specific sexual partners, this study was not able to explore partnership characteristics that have previously been shown to impact disclosure (e.g., partner serostatus and relationship type).
In using the measure of total number of disclosures as count outcome, participants who reported a greater number of partners had more partners (i.e., a higher count) to whom they could disclose. To account for the differential number of disclosures based on the number of sexual partners, the mediation analysis was adjusted for the total number of sex partners. Future research should measure disclosures to specific partners in order to link partner characteristics to the likelihood of disclosure and to create an accurate measure of disclosure rates.
Fourth, the findings cannot fully establish the temporality and causality of the relationships presented. The independent variable (depression) was measured on average a month after diagnosis, after which several weeks passed, prior to measuring the mediator (disclosure self-efficacy) and the outcome (disclosure to the number of sexual partners in the three months following diagnosis). The relationship between disclosure self-efficacy and disclosure is likely bi-directional (i.e., disclosure experiences also impact disclosure self-efficacy).24
Because disclosure and disclosure self-efficacy were measured at the same time point, it is likely that disclosure self-efficacy had been affected by disclosure experiences and vice versa. Exploring how the bi-directional relationship between disclosure and disclosure self-efficacy is influenced by depression should be studied with longitudinal designs and qualitative methods.
Finally, this was a small sample of MSM who were recruited from a health center in New York City. Thus, the findings may not be generalizable to the broader population of MSM in New York City and elsewhere who do not seek care.
Given the potential for high levels of emotional distress resulting from an HIV diagnosis, the study underscores the importance of diagnosing and addressing depression in the period following HIV diagnosis. This would not only benefit the health and well-being of newly diagnosed MSM but may also reduce the risk of onward transmission to their sexual partners through increased HIV disclosure. HIV patients are not typically screened for depression by their HIV care providers.44 Depression screening should be offered universally to newly diagnosed MSM and depression treatment should be provided, when applicable. Integrating treatment for depression into HIV care, including cognitive behavioral therapy (CBT) and pharmacological approaches, has been successful among patients living with HIV45 and, in turn, can increase HIV treatment adherence.46
So that both partners in a sexual relationship can make informed decisions about risk reduction,47 efforts to increase disclosure should specifically address disclosure self-efficacy for the different types of partners and situations in which one may need to disclose. Disclosure skills building can readily be integrated into the initial stages of HIV care.48 Health care providers who address issues related to disclosure with their patients living with HIV may lead to higher rates of disclosure.9 Improvements to disclosure resulting from provider discussions may result from increasing patients' disclosure self-efficacy, as patient–provider discussions have been shown to increase adherence via adherence self-efficacy.49
This study highlights the high levels of depressive symptoms in newly diagnosed MSM and the impact that depression has on disclosure to sexual partners during the initial period after diagnosis. It is critical for health care providers to screen for and address depressive symptoms among MSM after diagnosis. Depressive symptoms act as a barrier to sharing ones' serostatus with sexual partners and disclosure self-efficacy mediates the depression–disclosure relationship. The mediation pathway suggests that disclosure self-efficacy could serve as an important intermediate target of interventions aiming to increase disclosure to sexual partners. Future research on this topic is needed to understand how depressive symptoms after diagnosis impact long-term disclosure patterns.
Acknowledgements
This research was funded by the NIH Grant R01-MH078731 and facilitated by the Duke Center for AIDS Research (P30-AI064518). We are grateful for our longstanding collaboration with Callen Lorde Community Health Center and the individuals who offered their participation in the study.
Author Disclosure Statement
All authors declare that they have no conflict of financial interest.
References
- 1.Anglemyer A, Rutherford GW, Horvath T, Baggaley RC, Egger M, Siegfried N. Antiretroviral therapy for prevention of HIV transmission in HIV-discordant couples. Cochrane Database Syst Rev 2013. April 30;4:CD009153. doi: 10.1002/14651858.CD009153.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dodds S, Blakley T, Lizzotte J, et al. Retention, adherence, and compliance: Special needs of HIV-infected adolescent girls and young women. J Adolesc Health 2003;33:39–47 [DOI] [PubMed] [Google Scholar]
- 3.Lam PK, Naar-King S, Wright K. Social support and disclosure as predictors of mental health in HIV-positive youth. AIDS Patient Care STDs 2007;21:20–29 [DOI] [PubMed] [Google Scholar]
- 4.Simoni JM, Pantalone DW. Secrets and safety in the age of AIDS: Does HIV disclosure lead to safer sex? Top HIV Med 2004;12:109–118 [PubMed] [Google Scholar]
- 5.Crepaz N, Marks G. Serostatus disclosure, sexual communication and safer sex in HIV-positive men. AIDS Care 2003;15:379–387 [DOI] [PubMed] [Google Scholar]
- 6.Brooks RA, Landovitz RJ, Kaplan RL, Lieber E, Lee SJ, Barkley TW. Sexual risk behaviors and acceptability of HIV pre-exposure prophylaxis among HIV-negative gay and bisexual men in serodiscordant relationships: A mixed methods study. AIDS Patient Care STDs 2012;26:87–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Relf M, Bishop T, Lachat M, et al. A qualitative analysis of partner selection, HIV serostatus disclosure, and sexual behaviors among HIV-positive urban men. AIDS Educ Prev 2009;21:280–297 [DOI] [PubMed] [Google Scholar]
- 8.Hult JR, Wrubel J, Branstrom R, Acree M, Moskowitz JT. Disclosure and nondisclosure among people newly diagnosed with HIV: An analysis from a stress and coping perspective. AIDS Patient Care STDs 2012;26:181–190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sullivan KM. Male self-disclosure of HIV-positive serostatus to sex partners: A review of the literature. JANAC 2005;16:33–47 [DOI] [PubMed] [Google Scholar]
- 10.Przybyla SM, Golin CE, Widman L, Grodensky CA, Earp JA, Suchindran C. Serostatus disclosure to sexual partners among people living with HIV: Examining the roles of partner characteristics and stigma. AIDS Care 2013;15:566–572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Serovich JM, McDowell TL, Grafsky EL. Women's report of regret of HIV disclosure to family, friends and sex partners. AIDS Behav 2008;12:227–231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bird JD, Voisin DR. A conceptual model of HIV disclosure in casual sexual encounters among men who have sex with men. J Health Psychol 2011;16:365–373 [DOI] [PubMed] [Google Scholar]
- 13.Bairan A, Taylor GA, Blake BJ, Akers T, Sowell R, Mendiola R., Jr. A model of HIV disclosure: Disclosure and types of social relationships. J Am Acad Nurse Pract 2007;19:242–250 [DOI] [PubMed] [Google Scholar]
- 14.Valente SM. Depression and HIV disease. JANAC 2003;14:41–51 [DOI] [PubMed] [Google Scholar]
- 15.Mills TC, Paul J, Stall R, et al. Distress and depression in men who have sex with men: The Urban Men's Health Study. Am J Psychiatry 2004;161:278–285 [DOI] [PubMed] [Google Scholar]
- 16.Moskowitz JT, Wrubel J, Hult JR, Maurer S, Acree M. Illness appraisals and depression in the first year after HIV diagnosis. PloS One 2013;8:e78904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Murphy FC, Rubinsztein JS, Michael A, et al. Decision-making cognition in mania and depression. Psychol Med 2001;31:679–693 [DOI] [PubMed] [Google Scholar]
- 18.Comer LK, Henker B, Kemeny M, Wyatt G. Illness disclosure and mental health among women with HIV/AIDS. J Community Appl Soc 2000;10:449–464 [Google Scholar]
- 19.Simoni JM, Demas P, Mason HR, Drossman JA, Davis ML. HIV disclosure among women of African descent: Associations with coping, social support, and psychological adaptation. AIDS Behav 2000;4:147–158 [Google Scholar]
- 20.Zea MC, Reisen CA, Poppen PJ, Echeverry JJ. Disclosure of HIV status and psychological well-being among Latino gay and bisexual men. AIDS Behav 2005;9:15–26 [DOI] [PubMed] [Google Scholar]
- 21.Fekete EM, Antoni MH, Durán R, Stoelb BL, Kumar M, Schneiderman N. Disclosing HIV serostatus to family members: Effects on psychological and physiological health in minority women living with HIV. Int J Behav Med 2009;16:367–376 [DOI] [PubMed] [Google Scholar]
- 22.Kalichman SC, DiMarco M, Austin J, Luke W, DiFonzo K. Stress, social support, and HIV-status disclosure to family and friends among HIV-positive men and women. J Behav Med 2003;26:315–332 [DOI] [PubMed] [Google Scholar]
- 23.Bandura A. Self-efficacy: The Exercise of Control. New York: Freeman, 1997 [Google Scholar]
- 24.Kalichman SC, Nachimson D. Self-efficacy and disclosure of HIV-positive serostatus to sex partners. Health Psychol 1999;18:281–287 [DOI] [PubMed] [Google Scholar]
- 25.Mutchler MG, Bogart LM, Elliott MN, McKay T, Suttorp MJ, Schuster MA. Psychosocial correlates of unprotected sex without disclosure of HIV-positivity among African-American, Latino, and White men who have sex with men and women. Arch Sex Behav 2008;37:736–747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Alvy LM, McKirnan DJ, Mansergh G, et al. Depression is associated with sexual risk among men who have sex with men, but is mediated by cognitive escape and self-efficacy. AIDS Behav 2011;15:1171–1179 [DOI] [PubMed] [Google Scholar]
- 27.Tucker A, Liht J, de Swardt G, et al. An exploration into the role of depression and self-efficacy on township men who have sex with men's ability to engage in safer sexual practices. AIDS Care 2013;25:1227–1235 [DOI] [PubMed] [Google Scholar]
- 28.Chaudoir SR, Fisher JD, Simoni JM. Understanding HIV disclosure: A review and application of the Disclosure Processes Model. Soc Sci Med 2011;72:1618–1629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sikkema KJ, Abler L, Hansen NB, et al. Positive choices: Outcomes of a brief risk reduction intervention for newly HIV-diagnosed men who have sex with men. AIDS Behav 2014;18:1808–1819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Weinhardt LS, Carey MP, Maisto SA, Carey KB, Cohen MM, Wickramasinghe SM. Reliability of the timeline follow-back sexual behavior interview. Ann Behav Med 1998;20:25–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Beck AT, Steer RA. Beck Depression Inventory Manual. San Antonio: The Psychological Corporation, 1993 [Google Scholar]
- 32.MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods 2002;7:83–104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tofighi D, MacKinnon DP. RMediation: An R package for mediation analysis confidence intervals. Behav Res Methods 2011;43:692–700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.MacKinnon D. Introduction to Statistical Mediation Analysis: CRC Press, 2007 [Google Scholar]
- 35.Bing EG, Burnam MA, Longshore D, et al. Psychiatric disorders and drug use among human immunodeficiency virus-infected adults in the United States. Arch Gen Psychiatry 2001;58:721–728 [DOI] [PubMed] [Google Scholar]
- 36.O'Cleirigh C, Newcomb ME, Mayer KH, Skeer M, Traeger L, Safren SA. Moderate levels of depression predict sexual transmission risk in HIV-infected MSM: A longitudinal analysis of data from six sites involved in a “Prevention for Positives” study. AIDS Behav 2013;17:1754–1769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sin NL, DiMatteo MR. Depression treatment enhances adherence to antiretroviral therapy: A meta-analysis. Ann Behav Med 2013;1–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Angelino AF. Depression and adjustment disorder in patients with HIV disease. Top HIV Med 2002;10:31–35 [PubMed] [Google Scholar]
- 39.Herek GM, Garnets LD. Sexual orientation and mental health. Ann Rev Clin Psychol 2007;3:353–375 [DOI] [PubMed] [Google Scholar]
- 40.Kalichman SC, Sikkema KJ, Somlai A. Assessing persons with human immunodeficiency virus (HIV) infection using the Beck Depression Inventory: Disease processes and other potential confounds. J Pers Assess 1995;64:86–100 [DOI] [PubMed] [Google Scholar]
- 41.Dilorio C, Dudley WN, Soet J, Watkins J, Maibach E. A social cognitive-based model for condom use among college students. Nurs Res 2000;49:208–214 [DOI] [PubMed] [Google Scholar]
- 42.Wolf MS, Davis TC, Osborn CY, Skripkauskas S, Bennett CL, Makoul G. Literacy, self-efficacy, and HIV medication adherence. Patient Educ Couns 2007;65:253–260 [DOI] [PubMed] [Google Scholar]
- 43.Butera NM, Lanza ST, Coffman DL. A framework for estimating causal effects in latent class analysis: Is there a causal link between early sex and subsequent profiles of delinquency? Prev Sci 2014;15:397–407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bess KD, Adams J, Watt MH, et al. Providers' attitudes towards treating depression and self-reported depression treatment practices in HIV outpatient care. AIDS Patient Care STDs 2013;27:171–180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Simoni JM, Safren SA, Manhart LE, et al. Challenges in addressing depression in HIV research: Assessment, cultural context, and methods. AIDS Behav 2011;15:376–388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Safren SA, O'Cleirigh CM, Bullis JR, Otto MW, Stein MD, Pollack MH. Cognitive behavioral therapy for adherence and depression (CBT-AD) in HIV-infected injection drug users: A randomized controlled trial. J Consult Clin Psychol 2012;80:404–415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gorbach P, Galea J, Amani B, et al. Don't ask, don't tell: Patterns of HIV disclosure among HIV positive men who have sex with men with recent STI practising high risk behaviour in Los Angeles and Seattle. Sex Transm Infect 2004;80:512–517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sikkema KJ, Hansen NB, Kochman A, et al. The development and feasibility of a brief risk reduction intervention for newly HIV-diagnosed men who have sex with men. J Community Psychol 2011;39:717–732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Johnson MO, Chesney MA, Goldstein RB, et al. Positive provider interactions, adherence self-efficacy, and adherence to antiretroviral medications among HIV-infected adults: A mediation model. AIDS Patient Care STDs 2006;20:258–268 [DOI] [PMC free article] [PubMed] [Google Scholar]


