Abstract
Background: Currently, over 30% of US youth are overweight and 1 in 6 have metabolic syndrome, making youth obesity one of the major global health challenges of the 21st century. Few enduring treatment strategies have been identified in youth populations, and the majority of standard weight loss programs fail to adequately address the impact of psychological factors on eating behavior and the beneficial contribution of parental involvement in youth behavior change.
Methods: A critical need exists to expand treatment development efforts beyond traditional education and cognitive-behavioral programs and explore alternative treatment models for youth obesity. Meditation-based mindful eating programs represent a unique and novel scientific approach to the current youth obesity epidemic given that they address key psychological variables affecting weight.
Results: The recent expansion of mindfulness programs to include family relationships shows the immense potential for broadening the customarily individual focus of this intervention to include contextual factors thought to influence youth health outcomes.
Conclusions: This article provides an overview of how both mindful eating and family systems theory fits within a conceptual framework in order to guide development of a comprehensive family-based mindful eating program for overweight youth.
Introduction
The prevalence of obesity (BMI ≥ 95th percentile) among youths in the United States ages 12–19 years increased 83% from 1999 to 2012 (from 11.2% to 20.5%).1,2 According to the latest National Health and Nutrition Examination Survey (2011–2012), the percentage of overweight (BMI ≥85th percentile) adolescents is even higher at 34.5%.1 Though some data suggest that increases in obesity rates have leveled off in 2011–2012, young adults still experience some of the highest levels of obesity in the nation.3 Further, recent investigations have shown that obese teens may not be spared from early health complications.4 At present, diabetes is the third-most prevalent chronic disease of childhood in the United States, and the proportion of those with diabetes or “prediabetes” increased from 9% in 1999 to 23% in 2008.5 Obesity during adolescence is the single best predictor of adult obesity and ensuing health complications, including Type 2 diabetes mellitus, heart disease, and premature death.6–8 Thus, adolescence is a critical period for obesity treatment and prevention.9
Efficacy of Traditional Weight Loss Interventions
Until recently, the obesity treatment literature has focused significantly more attention on children and adults then on adolescents as fewer randomized, controlled trials of weight loss interventions have been conducted with youth ages 13–18.4 Reviews have summarized the results of different aspects of youth obesity treatment, including nutrition education, exercise, dietary interventions, behavioral therapy, and medication trials,10–12 though the majority of interventions produce only modest effects.13,14 Currently, there is limited evidence for clinically effective, long-term weight management interventions that are sustainable in community settings,4,13 and the examination of mind-body therapies in youth weight loss research is practically nonexistent.15,16 Thus, a critical need exists to expand treatment development efforts beyond traditional education and behavioral programs and explore alternative treatment models for youth obesity.
The Influence of Psychosocial Factors on Eating Behaviors
One area of research that has received little attention in treatment development efforts is the influence of psychological factors. Psychosocial factors are found to play a prominent role in obesity and eating behavior and in the development and maintenance of metabolic syndrome.15,17,18 Indeed, the widespread prevalence of psychological distress in obesity populations is thought to be a key factor in the inability to maintain behavior change over time.19 Three primary psychosocial factors stand out as being highly correlated with eating behaviors in youth, including psychological distress, body dissatisfaction, and physiological distress.9,17,20–22 For example, overweight youth report engaging in significantly more emotional binge eating behaviors and experiencing lower self-esteem, and higher levels of emotional distress, than their non-overweight peers.23–26 In regard to depression, the considerable literature on this topic connects symptoms of depression and being overweight27–29 in a bidirectional manner. Specifically, not only can the experience of being overweight increase depressive symptoms,29 but studies also show a predictive relationship between depressive symptoms and later development of obesity.30,31
Research suggests that social stigmatization regarding weight may mediate the relationship between obesity and psychosocial functioning through its association with increased depression and body dissatisfaction.32–36 Body dissatisfaction has been implicated as another key psychosocial outcome given that it puts youth at high risk for engaging in disordered eating behaviors, including use of unhealthy weight control practices,37–40 dietary restraint,9,41 and binge eating.42–44 In addition, and of particular relevance to obesity prevention efforts, is that recent findings from the seminal study, Project EAT, suggests that body dissatisfaction actually predicts increased weight gain over time.45,46 Thus, researchers have contended that not only does body dissatisfaction make it difficult to engage in self-care behaviors, but also that its effect on disordered eating behaviors contributes to the maintenance of obesity long term.9
Chronic psychosocial stressors, including household (e.g., family relationship strain), environmental (e.g., neighborhood safety), and peer and school (e.g., bullying) have also been linked to obesity risk.20 Though the stress and obesity connection in youth is complex,47 two primary pathways of influence have been hypothesized. The first is through chronically elevated glucocorticoid levels resulting from hypothalamic-pituitary-adrenal axis activation.17,48 Elevated glucocorticoids stimulate appetite while conserving energy expenditure, thereby leading to weight gain. Glucocorticoids also enhance the preference for calorically dense “comfort foods.”48 Also hypothesized is that psychosocial stressors can influence obesity risk through use of maladaptive coping behaviors, such as lack of exercise and overeating.20,49 Thus, the need for obesity treatment programs that teach youth how to build resources to cope effectively with stressors is being increasingly acknowledged.17,18
Expanding Treatment Models for Youth Obesity
Overall, there appears to be a consistent association between reduced psychosocial functioning, disordered eating behaviors, and maladaptive coping strategies in overweight youth.9,22,46 However, traditional weight loss interventions may not adequately address these important risk factors.16,37,50 Traditional behavioral weight loss interventions focus primarily on increasing physical activity, reducing caloric intake, and teaching cognitive and behavioral control strategies, such as, but not limited to, cognitive restructuring for negative thoughts, and behavioral monitoring.51,52 Though they have shown promise in decreasing the incidence of obesity and its comorbidities,53,54 benefits have been extremely limited in youth, as observed by modest effect sizes, high rates of attrition, and low levels of compliance, with most participants quickly regaining weight.4,55,56 It has been theorized that the long-term lack of success may be owing, in part, to an incomplete understanding of the critical psychosocial factors that lead to disordered eating behaviors among youth.37,57 In addition, research findings are beginning to support the notion that dieting is not a sustainable strategy for weight loss or for promoting a healthy lifestyle.58,59 Indeed, dieting is now coming into question owing to long-term ineffectiveness and unfavorable physio- and psychological effects.60,61 Instead, an emphasis on reducing overeating tendencies is increasingly being recommended as an alternative to dieting.62 Given that the literature continues to show a link between obesity and disordered eating,63,64 the relevance of multiple psychosocial factors continues to grow. Austin (2011) states that it is indeed the field's inability to recognize and target the multidimensional psychological factors involved in eating behavior that is the current “blind spot” of pediatric obesity treatment efforts.65
The Role of Mindful Eating for Weight Loss
Mindfulness is a state of consciousness, defined in the literature as “the awareness that emerges through paying attention on purpose, in the present moment, and non-judgmentally to the unfolding of experience moment to moment.”66 It is thought that through continuous nonjudgmental attention to, and acceptance of, the moment-to-moment experience,67 a heightened sense of self emerges, which can allow an individual to disengage from habitual reactions and patterns related to thoughts, emotions, and behaviors.68,69
Mindfulness-based programs are now being modified successfully for populations attempting to make dietary health changes,16,72,73 and recent reviews conclude that these programs warrant further clinical and empirical attention16,72 owing to their positive effects on psychological distress,74 disordered eating,75 and weight loss.76,77 The focal point of these programs is the use of mindfulness, or increased awareness of mental and physical states, and the physical, cognitive, and emotional triggers to eat.78 Of particular relevance to overweight youth, three key therapeutic factors are targeted and include: (1) experiential acceptance as a positive coping skill for controlling responses to psychological distress; (2) self-regulation through developed awareness of the emotional and physical cues to eat; and (3) compassion as a way to cultivate self-acceptance and body satisfaction.
An underlying tenet of mindfulness-based models is that many forms of disordered behavior (including maladaptive eating patterns) are related to attempts to avoid or escape aversive internal experiences.75,79 Indeed, consistent findings across studies suggest a pattern of experiential avoidance in overweight individuals.19 Characteristics that have been ascribed include psychological inflexibility and the use of maladaptive coping responses during stress.19,80 With chronic exposure to stressors, they tend to use passive coping strategies, such as avoidance distraction or emotional-oriented styles of coping, and often binge eat in response to stress.72,81 Increasing awareness of the connections between emotional states and impulsive eating patterns is an essential component of mindful eating75,82 and is predicated on the assumption that healthy eating choices depend on one's ability to tolerate and accept aversive internal experiences (i.e., to develop experiential acceptance).83 Remaining in mental contact with uncomfortable experiences, without judging or reacting upon them, can foster emotional balance and assist in interrupting patterns of automatic reactivity as it relates to maladaptive eating choices.83–85
Further, overweight individuals often underestimate how much food they are eating and tend to eat in a dissociative manner.86 Thus, mindful eating promotes intuitive eating, an eating style that relies on physiological hunger and satiety cues to guide eating, rather than externally driven emotional factors or dieting behaviors.82,87 The emphasis on calorie reduction taught in traditional weight loss programs depends, to a large degree, on ignoring body signals related to hunger and satiety. Thus, a commonality between emotional eating and dieting is their association with ignored or suppressed responses to internal and external cues.88,89 In contrast, mindful eating promotes a healthier approach by attempting to restore body/mind balance by reconnecting individuals with natural internal cues of hunger and satiety.58 By strengthening the awareness of both the physical and emotional triggers to eat, individuals can develop a trust in their body's ability to know when and how much to eat while utilizing other self-care strategies to manage psychological distress.90
Finally, increased self-compassion is an additional mechanism by which mindfulness may have clinical benefit through its ability to foster present moment acceptance for body shape and size and promoting lower self-criticism.91,92
Whereas mindfulness-based interventions have typically been used in adult populations, the literature on their use in youth populations is gathering considerable momentum. Over the past few years, it is becoming more commonplace to see mindful programs implemented among youth in school-, community-, and clinic-based settings.94 Along with their adult counterparts, the use of mindfulness with youth has proven successful with various conditions, such as anxiety,95 attention deficit hyperactivity disorder,96,97 blood pressure and heart rate,98,99 chronic pain,100 inflammatory bowel disease,101 post-traumatic stress,102 sleep quality,103 and heterogeneous mental health disorders.104
Family Systems Theory in Youth Weight Loss
Over the past decade, there has been a shift in the mode of treatment services for youth obesity that prioritizes the development of interventions that target multiple factors. One of the driving forces in this shift is the recognition that the development of overweight and obesity involves interactions among multiple domains, including interpersonal, environmental/social, and physiological. Researchers increasingly recognize that improving obesity treatment outcomes necessitates moving beyond the lens of individual intrapersonal factors to incorporate the social, contextual, and environmental influences associated with health behaviors.18 For example, youth eating behaviors are not developed in a vacuum, but are vastly influenced by family and culture. Thus, incorporating the family system into obesity interventions has been identified as an important strategy for sustained behavioral change.105,106 Several home environment characteristics have been identified as correlates of obesity that have potential for significant family influence. Eating practices in the home, eating-related parenting styles, and family relationships hold the potential to either help or hinder obesity outcomes.106–107 For example, not only is a youth's BMI most strongly predicted by parental BMI,108 family environmental factors, such as levels of conflict and cohesion in family relationships, contribute an additional layer of risk factors for youth overweight/obesity.109
According to Kitzman-Ulrich and colleagues, Family Systems Theory (FST) provides a conceptual framework for how family factors influence youth health behaviors.110 Specifically, key variables to consider when developing health behavior change programs include components to improve family functioning, such as promoting authoritative style parenting (providing a nurturing environment), enhancing parenting skills (monitoring, reinforcement, and role modeling), and teaching child management strategies to encourage positive behaviors in weight loss programs.110 Among the links studied, evidence over the last few years indicates that positive family relationships can serve as a protective influence against youth psychosocial difficulties that have been associated with overweight during adolescence.18,106 In general, the family's social-emotional environment, including family connectedness, prioritizing of family meals, and a positive family mealtime environment, are positively associated with higher self-esteem and body satisfaction and inversely associated with unhealthy weight control behaviors among at-risk-for-overweight and overweight youth.111 These findings provide further support for the consideration of additional contextual factors, such as improvement in family relationships, for inclusion into the next generation of treatment programs.23
Conceptual Model for a Family-Systems Based Mindful Eating Program
The recent expansion of mindfulness programs to include family relationships shows the immense potential for broadening the customarily individual focus of mindfulness interventions to include other factors thought to influence youth health outcomes. New models for family-based prevention programs that integrate mindfulness into existing evidence-based behavioral programs (e.g., youth substance abuse prevention) have begun to show promising results given that they seek to extend the concepts and practices of mindfulness to parenting relationships.112,113 With this newly emerging evidence, we contend that a family systems framework provides the most comprehensive perspective from which to teach mindful eating skills for adolescents.
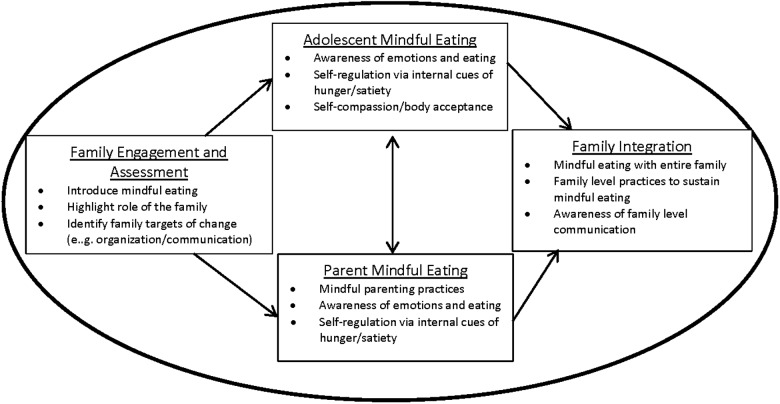
The following is a description of how both mindfulness and family systems theory could fit within a conceptual framework for an integrated family-based mindful eating program for overweight youths.
Figure 1 provides a schematic conceptual model for how a family-systems based mindful eating program might be run. The inner rectangles reflect the goals and specific family participants at various phases of the program. The outer circle highlights the ongoing influence of the family throughout the program, regardless of which family members attend treatment.
Figure 1.
Conceptual model of a family systems-based mindful eating intervention. Oval represents the family system as environment. Bullet point represent examples of intervention content within each phase.
Phase 1: Family Engagement and Assessment
The first phase of the program would ideally include all family members. This initial phase serves multiple purposes that include introducing the family to the concept of mindful eating, providing an engaging first experience of a mindful practice, identifying areas of potential resistance, enhancing motivation if necessary, highlighting the role of the family in both helpful and unhelpful eating behaviors, and encouraging active support from the entire family. The purpose of the assessment is to identify potential targets of change in family eating-related practices and behaviors, and to identify relationally oriented issues that may contribute to poorly regulated and mindless eating that could be addressed directly through the mindful eating intervention. Examples include family organization and planning for meals, food acquisition habits, mealtime practices, family, or dyadic food-related communication and affective tone.
Phase 2: Parent and Adolescent Mindful Eating Groups
The middle rectangles in the model reflect a mindful-eating intervention run as two separate, but concurrent, groups with overlapping content and some combined group practice. The groups would have separate instructors and the material would be taught with experiential exercises related to mindful and mindless eating in addition to formal meditation practices that enhance body awareness, such as the body scan. Separating the groups allows for discussions that are developmentally appropriate for teens and parents. The adolescent group might emphasize more informal practices and games to teach mindful awareness and mindful eating principles than the parent group. The parent group could include additional discussions of mindful parenting practices to further support healthy eating-related behaviors in the family.
Phase 3: Family Integration
The final phase of the intervention would involve integration of the mindful eating principles within the entire family. This may involve, for example, formal practices of mindful eating with the entire family, problem solving family-related barriers to mindful eating, or identifying family-level practices that can help sustain mindful eating. Attention to positive changes in family-level communication around eating is another potential component. The overall goal would be to identify what is needed within the family system to sustain change in mindful eating habits over time.
Conclusions
The robust research findings linking psychosocial distress with disordered eating behaviors in overweight youth illustrate the need to expand treatment efforts beyond providing core diet and exercise education and begin to identify protective factors that can assist in developing healthy psychological functioning while promoting positive and adaptive eating styles.114,115 Mindful eating programs represent a promising approach to youth obesity given that they have been shown to address key psychosocial variables associated with treatment outcomes and seek to provide a balanced, integrated approach to the prevention of weight-related problems in youth. The lack of long-term effectiveness regarding traditional weight loss interventions, coupled with the prioritization of multicomponent treatment programs, and the successful integration of mindfulness techniques with families point toward the potential of this novel, alternative model that could help augment and advance youth obesity treatment efforts. We believe that integration of these components will provide a richer picture of relevancy, broadening the content of what can be addressed within weight loss interventions. The growth of the literature on the use of mindfulness-based eating programs has gathered considerable momentum over the past decade and conveys the potential of this treatment in both prevention and intervention efforts. It is time to capitalize on this advancement and move this treatment modality outside the realm of the individual to a focus on systems. Investigators are beginning to work toward this end by integrating mindfulness within family-based programs.113,116 We have introduced a conceptual model of a family systems-based mindful eating program in order to provide an initial framework to begin to generate discussion within the scientific and clinical community. However, much more research is needed in this area to help inform and propel further advances in the treatment of obesity and shed light on how mindfulness can be successfully integrated with broader social factors influencing youth health outcomes.
Acknowledgments
This article was supported by funding from the National Center for Complementary and Integrative Health of the NIH (1R34AT007843).
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Ogden CL, Carroll MD, Kit BK, et al. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014;311:806–814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ogden CL, Flegal KM, Carroll MD, et al. Prevalence and trends in overweight among US children and adolescents, 1999–2000. JAMA 2002;288:1728–1732 [DOI] [PubMed] [Google Scholar]
- 3.Mokdad AH, Serdula MK, Dietz WH, et al. The spread of the obesity epidemic in the United States, 1991–1998. JAMA 1999;282:1519–1522 [DOI] [PubMed] [Google Scholar]
- 4.Butryn ML, Wadden TA, Rukstalis MR, et al. Maintenance of weight loss in adolescents: Current status and future directions. J Obes 2010;2010:789280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.May AL, Kuklina EV, Yoon PW. Prevalence of cardiovascular disease risk factors among US adolescents, 1999–2008. Pediatrics 2012;129:1035–1041 [DOI] [PubMed] [Google Scholar]
- 6.Freedman DS, Khan LK, Dietz WH, et al. Relationship of childhood obesity to coronary heart disease risk factors in adulthood: The Bogalusa Heart Study. Pediatrics 2001;108:712–718 [DOI] [PubMed] [Google Scholar]
- 7.Must A, Jacques PF, Dallal GE, et al. Long-term morbidity and mortality of overweight adolescents. A follow-up of the Harvard Growth Study of 1922 to 1935. N Engl J Med 1992;327:1350–1355 [DOI] [PubMed] [Google Scholar]
- 8.NIH. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. NIH: Bethesda, MD, 1998 [PubMed] [Google Scholar]
- 9.Goldfield GS, Moore C, Henderson K, et al. Body dissatisfaction, dietary restraint, depression, and weight status in adolescents. J Sch Health 2010;80:186–192 [DOI] [PubMed] [Google Scholar]
- 10.Oude Luttikhuis H, Baur L, Jansen H, et al. Interventions for treating obesity in children. Cochrane Database Syst Rev 2009;(1):CD001872. [DOI] [PubMed] [Google Scholar]
- 11.Ho M, Garnett SP, Baur L, et al. Effectiveness of lifestyle interventions in child obesity: Systematic review with meta-analysis. Pediatrics 2012;130:e1647–e1671 [DOI] [PubMed] [Google Scholar]
- 12.Lavelle HV, Mackay DF, Pell JP. Systematic review and meta-analysis of school-based interventions to reduce body mass index. J Public Health (Oxf) 2012;34:360–369 [DOI] [PubMed] [Google Scholar]
- 13.Nguyen B, Shrewsbury VA, O'Connor J, et al. Twelve-month outcomes of the loozit randomized controlled trial: A community-based healthy lifestyle program for overweight and obese adolescents. Arch Pediatr Adolesc Med 2012;166:170–177 [DOI] [PubMed] [Google Scholar]
- 14.Vasques C, Magalhaes P, Cortinhas A, et al. Effects of intervention programs on child and adolescent BMI: A meta-analysis study. J Phys Act Health 2014;11:426–444 [DOI] [PubMed] [Google Scholar]
- 15.Anderson JG, Taylor AG. The metabolic syndrome and mind-body therapies: A systematic review. J Nutr Metab 2011;2011:276419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.O'Reilly GA, Cook L, Spruijt-Metz D, et al. Mindfulness-based interventions for obesity-related eating behaviours: A literature review. Obes Rev 2014;15:453–461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gundersen C, Mahatmya D, Garasky S, et al. Linking psychosocial stressors and childhood obesity. Obes Rev 2011;12:e54–e63 [DOI] [PubMed] [Google Scholar]
- 18.Lawman HG, Wilson DK. A review of family and environmental correlates of health behaviors in high-risk youth. Obesity (Silver Spring) 2012;20:1142–1157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lillis J, Hayes SC, Bunting K, et al. Teaching acceptance and mindfulness to improve the lives of the obese: A preliminary test of a theoretical model. Ann Behav Med 2009;37:58–69 [DOI] [PubMed] [Google Scholar]
- 20.Wilson SM, Sato AF. Stress and paediatric obesity: What we know and where to go. Stress Health 2014;30:91–102 [DOI] [PubMed] [Google Scholar]
- 21.Morgan CM, Yanovski SZ, Nguyen TT, et al. Loss of control over eating, adiposity, and psychopathology in overweight children. Int J Eat Disord 2002;31:430–441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nemiary D, Shim R, Mattox G, et al. The relationship between obesity and depression among adolescents. Psychiatr Ann 2012;42:305–308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mellin AE, Neumark-Sztainer D, Story M, et al. Unhealthy behaviors and psychosocial difficulties among overweight adolescents: The potential impact of familial factors. J Adolesc Health 2002;31:145–153 [DOI] [PubMed] [Google Scholar]
- 24.Neumark-Sztainer D, Story M, French SA, et al. Psychosocial concerns and health-compromising behaviors among overweight and nonoverweight adolescents. Obes Res 1997;5:237–249 [DOI] [PubMed] [Google Scholar]
- 25.French SA, Perry CL, Leon GR, et al. Self-esteem and change in body mass index over 3 years in a cohort of adolescents. Obes Res 1996;4:27–33 [DOI] [PubMed] [Google Scholar]
- 26.French SA, Jeffery RW. Consequences of dieting to lose weight: Effects on physical and mental health. Health Psychol 1994;13:195–212 [DOI] [PubMed] [Google Scholar]
- 27.Blaine B. Does depression cause obesity?: A meta-analysis of longitudinal studies of depression and weight control. J Health Psychol 2008;13:1190–1197 [DOI] [PubMed] [Google Scholar]
- 28.de Wit L, Luppino F, van Straten A, et al. Depression and obesity: A meta-analysis of community-based studies. Psychiatry Res 2010;178:230–235 [DOI] [PubMed] [Google Scholar]
- 29.Luppino FS, de Wit LM, Bouvy PF, et al. Overweight, obesity, and depression: A systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry 2010;67:220–229 [DOI] [PubMed] [Google Scholar]
- 30.Goodman E, Whitaker RC. A prospective study of the role of depression in the development and persistence of adolescent obesity. Pediatrics 2002;110:497–504 [DOI] [PubMed] [Google Scholar]
- 31.Liem ET, Sauer PJ, Oldehinkel AJ, et al. Association between depressive symptoms in childhood and adolescence and overweight in later life: Review of the recent literature. Arch Pediatr Adolesc Med 2008;162:981–988 [DOI] [PubMed] [Google Scholar]
- 32.Storch EA, Milsom VA, Debraganza N, et al. Peer victimization, psychosocial adjustment, and physical activity in overweight and at-risk-for-overweight youth. J Pediatr Psychol 2007;32:80–89 [DOI] [PubMed] [Google Scholar]
- 33.Puhl RM, Latner JD. Stigma, obesity, and the health of the nation's children. Psychol Bull 2007;133:557–580 [DOI] [PubMed] [Google Scholar]
- 34.Tang-Peronard JL, Heitmann BL. Stigmatization of obese children and adolescents, the importance of gender. Obes Rev 2008;9:522–534 [DOI] [PubMed] [Google Scholar]
- 35.Eisenberg ME, Neumark-Sztainer D, Haines J, et al. Weight-teasing and emotional well-being in adolescents: Longitudinal findings from Project EAT. J Adolesc Health 2006;38:675–683 [DOI] [PubMed] [Google Scholar]
- 36.Goldfield G, Moore C, Henderson K, et al. The relation between weight-based teasing and psychological adjustment in adolescents. Paediatr Child Health 2010;15:283–288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Neumark-Sztainer D. Integrating messages from the eating disorders field into obesity prevention. Adolesc Med State Art Rev 2012;23:529–543 [PubMed] [Google Scholar]
- 38.Shaw H, Ramirez L, Trost A, et al. Body image and eating disturbances across ethnic groups: more similarities than differences. Psychol Addict Behav 2004;18:12–18 [DOI] [PubMed] [Google Scholar]
- 39.Pesa JA, Syre TR, Jones E. Psychosocial differences associated with body weight among female adolescents: The importance of body image. J Adolesc Health 2000;26:330–337 [DOI] [PubMed] [Google Scholar]
- 40.Latzer Y, Stein D. A review of the psychological and familial perspectives of childhood obesity. J Eat Disord 2013;1:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hawks S, Madanat H, Christley H. Psychosocial associations of dietary restraint: Implications for healthy weight promotion. Ecol Food Nutr 2008;47:450–483 [Google Scholar]
- 42.Puhl RM, Moss-Racusin CA, Schwartz MB. Internalization of weight bias: Implications for binge eating and emotional well-being. Obesity (Silver Spring) 2007;15:19–23 [DOI] [PubMed] [Google Scholar]
- 43.Danielsen YS, Stormark KM, Nordhus IH, et al. Factors associated with low self-esteem in children with overweight. Obes Facts 2012;5:722–733 [DOI] [PubMed] [Google Scholar]
- 44.Herbozo S, Schaefer LM, Thompson JK. A comparison of eating disorder psychopathology, appearance satisfaction, and self-esteem in overweight and obese women with and without binge eating. Eat Behav 2015;17:86–89 [DOI] [PubMed] [Google Scholar]
- 45.Eisenberg ME, Neumark-Sztainer D, Paxton SJ. Five-year change in body satisfaction among adolescents. J Psychosom Res 2006;61:521–527 [DOI] [PubMed] [Google Scholar]
- 46.Neumark-Sztainer D, Wall M, Larson NI, et al. Dieting and disordered eating behaviors from adolescence to young adulthood: Findings from a 10-year longitudinal study. J Am Diet Assoc 2011;111:1004–1011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.van Jaarsveld CH, Fidler JA, Steptoe A, et al. Perceived stress and weight gain in adolescence: A longitudinal analysis. Obesity (Silver Spring) 2009;17:2155–2161 [DOI] [PubMed] [Google Scholar]
- 48.Sominsky L, Spencer SJ. Eating behavior and stress: A pathway to obesity. Front Psychol 2014;5:434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Siervo M, Wells JC, Cizza G. The contribution of psychosocial stress to the obesity epidemic: An evolutionary approach. Horm Metab Res 2009;41:261–270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lillis J, Kendra KE. Acceptance and commitment therapy for weight control: Model, evidence, and future directions. J Contextual Behav Sci 2014;3:1–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Butryn ML, Webb V, Wadden TA. Behavioral treatment of obesity. Psychiatr Clin North Am 2011;34:841–859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kong AS, Dalen J, Negrete S, et al. Interventions for treating overweight and obesity in adolescents. Adolesc Med State Art Rev 2012;23:544–570 [PubMed] [Google Scholar]
- 53.Faith M, Saelens B, Wilfley D. Behavioral treatment of childhood and adolescent obesity: Current status, challenges, and future directions. In: Thompson JK, Smolak L. (eds), Body Image, Eating Disorders, and Obesity in Youth: Assessment, Prevention, and Treatment. American Psychological Association: Washington, DC, 2001, pp. 313–319 [Google Scholar]
- 54.Saelens BE, Sallis JF, Wilfley DE, et al. Behavioral weight control for overweight adolescents initiated in primary care. Obes Res 2002;10:22–32 [DOI] [PubMed] [Google Scholar]
- 55.Jeffrey RW, Drewnowski A, Epstein LH, et al. Long-term maintenance of weight loss: Current status. Health Psychol 2000;19:5–16 [DOI] [PubMed] [Google Scholar]
- 56.Bacon L, Stern JS, Van Loan MD, et al. Size acceptance and intuitive eating improve health for obese, female chronic dieters. J Am Diet Assoc 2005;105:929–936 [DOI] [PubMed] [Google Scholar]
- 57.Bennett J, Greene G, Schwartz-Barcott D. Perceptions of emotional eating behavior. A qualitative study of college students. Appetite 2013;60:187–192 [DOI] [PubMed] [Google Scholar]
- 58.Denny KN, Loth K, Eisenberg ME, et al. Intuitive eating in young adults. Who is doing it, and how is it related to disordered eating behaviors? Appetite 2013;60:13–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Katan MB. Weight-loss diets for the prevention and treatment of obesity. N Engl J Med 2009;360:923–925 [DOI] [PubMed] [Google Scholar]
- 60.Mann T, Tomiyama AJ, Westling E, et al. Medicare's search for effective obesity treatments: Diets are not the answer. Am Psychol 2007;62:220–233 [DOI] [PubMed] [Google Scholar]
- 61.Bacon L, Aphramor L. Weight science: Evaluating the evidence for a paradigm shift. Nutr J 2011;10:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Herman CP, van Strien T, Polivy J. Undereating or eliminating overeating? Am Psychol 2008;63:202–203 [DOI] [PubMed] [Google Scholar]
- 63.Haines J, Neumark-Sztainer D. Prevention of obesity and eating disorders: A consideration of shared risk factors. Health Educ Res 2006;21:770–782 [DOI] [PubMed] [Google Scholar]
- 64.Neumark-Sztainer DR, Wall MM, Haines JI, et al. Shared risk and protective factors for overweight and disordered eating in adolescents. Am J Prev Med 2007;33:359–369 [DOI] [PubMed] [Google Scholar]
- 65.Austin SB. The blind spot in the drive for childhood obesity prevention: Bringing eating disorders prevention into focus as a public health priority. Am J Public Health 2011;101:e1–e4 [DOI] [PubMed] [Google Scholar]
- 66.Kabat-Zinn J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. Delacourt: New York, 1990 [Google Scholar]
- 67.Bishop S, Lau M, Shapiro S, et al. Mindfulness: A proposed operational definition. Clin Psychol Sci Prac 2004;V11:230–241 [Google Scholar]
- 68.Shapiro SL, Carlson LE, Astin JA, et al. Mechanisms of mindfulness. J Clin Psychol 2006;62:373–386 [DOI] [PubMed] [Google Scholar]
- 69.Dobkin PL. Mindfulness-based stress reduction: What processes are at work? Complement Ther Clin Pract 2008;14:8–16 [DOI] [PubMed] [Google Scholar]
- 70.Ludwig DS, Kabat-Zinn J. Mindfulness in medicine. JAMA 2008;300:1350–1352 [DOI] [PubMed] [Google Scholar]
- 71.Baer RA. Mindfulness training as a clinical intervention: A conceptual and empirical review. Clin Psychol Sci Prac 2003;10:125–143 [Google Scholar]
- 72.Katterman SN, Kleinman BM, Hood MM, et al. Mindfulness meditation as an intervention for binge eating, emotional eating, and weight loss: A systematic review. Eat Behav 2014;15:197–204 [DOI] [PubMed] [Google Scholar]
- 73.Kristeller JL, Baer RA, Quillian-Wolever R. Mindfulness-based approaches to eating disorders. In: Baer RA. (ed), Midfullness-Based Treatment Approaches. Academic: Oxford, UK, 2006, pp. 75–91 [Google Scholar]
- 74.Goyal M, Singh S, Sibinga EM, et al. Meditation programs for psychological stress and well-being: A systematic review and meta-analysis. JAMA Int Med 2014;174:357–368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Baer RA, Fischer S, Huss DB. Mindfulness and acceptance in the treatment of disordered eating. J Ration Emot Cogn Behav Ther 2006;23:281–300 [Google Scholar]
- 76.Dalen J, Smith BW, Shelley BM, et al. Pilot study: Mindful Eating and Living (MEAL): Weight, eating behavior, and psychological outcomes associated with a mindfulness-based intervention for people with obesity. Complement Ther Med 2010;18:260–264 [DOI] [PubMed] [Google Scholar]
- 77.Tapper K, Shaw C, Ilsley J, et al. Exploratory randomised controlled trial of a mindfulness-based weight loss intervention for women. Appetite 2009;52:396–404 [DOI] [PubMed] [Google Scholar]
- 78.Kristeller JL, Hallett B. An exploratory study of a meditation-based intervention for binge eating disorder. J Health Psychol 1999;4:357–363 [DOI] [PubMed] [Google Scholar]
- 79.Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol 2003;84:822–848 [DOI] [PubMed] [Google Scholar]
- 80.Freeman LM, Gil KM. Daily stress, coping, and dietary restraint in binge eating. Int J Eat Disord 2004;36:204–212 [DOI] [PubMed] [Google Scholar]
- 81.Spoor ST, Bekker MH, Van Strien T, et al. Relations between negative affect, coping, and emotional eating. Appetite 2007;48:368–376 [DOI] [PubMed] [Google Scholar]
- 82.Kristeller JL, Wolever RQ. Mindfulness-based eating awareness training for treating binge eating disorder: The conceptual foundation. Eat Disord 2011;19:49–61 [DOI] [PubMed] [Google Scholar]
- 83.Forman EM, Butryn ML. A new look at the science of weight control: How acceptance and commitment strategies can address the challenge of self-regulation. Appetite 2015;84:171–180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Alberts HJ, Schneider F, Martijn C. Dealing efficiently with emotions: Acceptance-based coping with negative emotions requires fewer resources than suppression. Cogn Emot 2012;26:863–870 [DOI] [PubMed] [Google Scholar]
- 85.Forman EM, Butryn ML. A new look at the science of weight control: How acceptance and commitment strategies can address the challenge of self-regulation. Appetite 2014;84c:171–180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kristeller JL, Hallett B. Effects of a meditation-based intervention in the treatment of binge eating. J Health Psychol 1999;4:357–363 [DOI] [PubMed] [Google Scholar]
- 87.Daubenmier J, Kristeller J, Hecht FM, et al. Mindfulness intervention for stress eating to reduce cortisol and abdominal fat among overweight and obese women: An exploratory randomized controlled study. J Obes 2011;2011:651936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Heatherton TF, Baumeister RF. Binge eating as escape from self-awareness. Psychol Bull 1991;110:86–108 [DOI] [PubMed] [Google Scholar]
- 89.Whiteside U, Chen E, Neighbors C, et al. Difficulties regulating emotions: Do binge eaters have fewer strategies to modulate and tolerate negative affect? Eat Behav 2007;8:162–169 [DOI] [PubMed] [Google Scholar]
- 90.Kristeller JL. Mindfulness, wisdom and eating: Applying a multi-domain model of meditation effects. J Construct Hum Sci 2003;8:107–118 [Google Scholar]
- 91.Chiesa A, Anselmi R, Serretti A. Psychological mechanisms of mindfulness-based interventions: What do we know? Holistic Nurs Prac 2014;28:124–148 [DOI] [PubMed] [Google Scholar]
- 92.Neff KD, Germer CK. A pilot study and randomized controlled trial of the mindful self-compassion program. J Clin Psychol 2013;69:28–44 [DOI] [PubMed] [Google Scholar]
- 93.Miller CK, Kristeller JL, Headings A, et al. Comparison of a mindful eating intervention to a diabetes self-management intervention among adults with type 2 diabetes: A randomized controlled trial. Health Educ Behav 2014;41:145–154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Black DS, Milam J, Sussman S. Sitting-meditation interventions among youth: A review of treatment efficacy. Pediatrics 2009;124:e532–e541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Sibinga EM, Perry-Parrish C, Chung SE, et al. School-based mindfulness instruction for urban male youth: A small randomized controlled trial. Prev Med 2013;57:799–801 [DOI] [PubMed] [Google Scholar]
- 96.van de Weijer-Bergsma E, Formsma AR, de Bruin EI, et al. The effectiveness of mindfulness training on behavioral problems and attentional functioning in adolescents with ADHD. J Child Fam Stud 2012;21:775–787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.van der Oord S, Bogels SM, Peijnenburg D. The effectiveness of mindfulness training for children with ADHD and mindful parenting for their parents. J Child Fam Stud 2012;21:139–147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Barnes VA, Davis HC, Murzynowski JB, et al. Impact of meditation on resting and ambulatory blood pressure and heart rate in youth. Psychosom Med 2004;66:909–914 [DOI] [PubMed] [Google Scholar]
- 99.Gregoski MJ, Barnes VA, Tingen MS, et al. Breathing awareness meditation and LifeSkills Training programs influence upon ambulatory blood pressure and sodium excretion among African American adolescents. J Adolesc Health 2011;48:59–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Jastrowski Mano KE, Salamon KS, Hainsworth KR, et al. A randomized, controlled pilot study of mindfulness-based stress reduction for pediatric chronic pain. Altern Ther Health Med 2013;19:8–14 [PubMed] [Google Scholar]
- 101.Cotton S, Humenay Roberts Y, Tsevat J, et al. Mind-body complementary alternative medicine use and quality of life in adolescents with inflammatory bowel disease. Inflamm Bowel Dis 2010;16:501–506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Gordon JS, Staples JK, Blyta A, et al. Treatment of posttraumatic stress disorder in postwar Kosovar adolescents using mind-body skills groups: A randomized controlled trial. J Clin Psychiatry 2008;69:1469–1476 [DOI] [PubMed] [Google Scholar]
- 103.Bei B, Byrne ML, Ivens C, et al. Pilot study of a mindfulness-based, multi-component, in-school group sleep intervention in adolescent girls. Early Interv Psychiatry 2013;7:213–220 [DOI] [PubMed] [Google Scholar]
- 104.Tan L, Martin G. Taming the adolescent mind: Preliminary report of a mindfulness-based psychological intervention for adolescents with clinical heterogeneous mental health diagnoses. Clin Child Psychol Psychiatry 2013;18:300–312 [DOI] [PubMed] [Google Scholar]
- 105.Golan M, Kaufman V, Shahar DR. Childhood obesity treatment: Targeting parents exclusively v. parents and children. Br J Nutr 2006;95:1008–1015 [DOI] [PubMed] [Google Scholar]
- 106.Bauer KW, Berge JM, Neumark-Sztainer D. The importance of families to adolescents' physical activity and dietary intake. Adolesc Med State Art Rev 2011;22:601–613, xiii. [PubMed] [Google Scholar]
- 107.Davis M, Gance-Cleveland B, Hassink S, et al. Recommendations for prevention of childhood obesity. Pediatrics 2007;120:S229–S253 [DOI] [PubMed] [Google Scholar]
- 108.Dowda M, Ainsworth BE, Addy CL, et al. Environmental influences, physical activity, and weight status in 8- to 16-year-olds. Arch Pediatr Adolesc Med 2001;155:711–717 [DOI] [PubMed] [Google Scholar]
- 109.Dalton WT, 3rd, Kitzmann KM. Broadening parental involvement in family-based interventions for pediatric overweight: Implications from family systems and child health. Fam Community Health 2008;31:259–268 [DOI] [PubMed] [Google Scholar]
- 110.Kitzman-Ulrich H, Wilson DK, St George SM, et al. The integration of a family systems approach for understanding youth obesity, physical activity, and dietary programs. Clin Child Fam Psychol Rev 2010;13:231–253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Fulkerson JA, Strauss J, Neumark-Sztainer D, et al. Correlates of psychosocial well-being among overweight adolescents: The role of the family. J Consult Clin Psychol 2007;75:181–186 [DOI] [PubMed] [Google Scholar]
- 112.Duncan LG, Coatsworth JD, Greenberg MT. Pilot study to gauge acceptability of a mindfulness-based, family-focused preventive intervention. J Prim Prev 2009;30:605–618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Duncan LG, Coatsworth JD, Greenberg MT. A model of mindful parenting: implications for parent-child relationships and prevention research. Clin Child Fam Psychol Rev 2009;12:255–270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Glasofer DR, Tanofsky-Kraff M, Eddy KT, et al. Binge eating in overweight treatment-seeking adolescents. J Pediatr Psychol 2007;32:95–105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Smith T, Hawks S. Intuitive eating, diet composition, and the meaning of food in healthy weight promotion. Am J Health Educ 2006;37:130–136 [Google Scholar]
- 116.Perez-Blasco J, Viguer P, Rodrigo MF. Effects of a mindfulness-based intervention on psychological distress, well-being, and maternal self-efficacy in breast-feeding mothers: Results of a pilot study. Arch Womens Ment Health 2013;16:227–236 [DOI] [PubMed] [Google Scholar]