Abstract
Introduction: The role of laser in conservative management of oral disease is well established. Laser procedures are common in the fields of oral surgery, implant dentistry, endodontic, and periodontic therapy.
Case: This case series describes the use of diode laser for the excision of oral exophytic lesions. All the patients attended the oral medicine department of Shahid Beheshti University of Medical Sciences, Tehran, Iran. Criteria in patient selection were accessibility to lesions, patient fear from blade surgery, aesthetics, and probability of bleeding. An informed consent was filled by every patient. All of the lesions were completely excised under local anaesthesia by diode laser with 300 μm-fibre tip, 808 nm continuous wavelength and 3-3.5 W power for 3×60 seconds (Dr Smile, Italia). During surgery, the fibre tip was in contact with lesions. No analgesics were prescribed to the patients. The patients were followed for the first, second, and forth week after treatment.
Conclusion: The lesions could be excised using the diode laser. This procedure was a quick clinical technique without bleeding.
Keywords: Oral, Benign exophytic lesions, Diode laser
Introduction
Laser systems in oral surgery are improving at full speed today.1,2 Laser plays a role in oral cavity surgery; and this role is established well.1 Laser surgery can be implement for ablation of lesions, different types of biopsies, gingivoplasties, gingivectomies, soft tissue tuberosity reductions, and certain crown lengthening procedure.3-9 According to a study, the use of diode laser systems for treatment of oral diseases has found application in removal of premalignant lesions of the oral cavity.1 The advantages of oral-laser surgery include an great visibility in field, precision, enhanced infection control and elimination of bacteraemia, quite bloodless surgical and postsurgical period, minimum swelling and scarring, reduced postsurgical pain, minimal administration of anaesthetics shots and that means less time spent in the dental chair.1-3,10 Laser applications also enable patients to enjoy a more relaxed dental experience, reducing their fears.3 Diode laser was introduced in dentistry from 1999,3 and it is considered an important tool for a number of applications.1 Diode laser with wavelengths ranging from 810 nm to 980 nm in continuous or pulsed mode was used as a possible modality for soft tissue surgery in the oral cavity.2,3 Based on the photo thermal effect of diode laser, lesions of the oral mucosa are removed with an excision technique, or by ablation/vaporization procedures.2 Heat production causes an excellent haemostasis in blood vessels at this wavelength.3,10 This study reports the use of diode laser for excision of various oral lesions.
Case 1
A 38 year-old female was referred with complaint of soft tissue swelling in her anterior maxilla. According to the history, this lesion occurred 6 months before referral when she recognized the expansion of a lesion at the anterior of the maxilla. Clinical examination showed that there was a pedunculated pink-coloured nodule with popular surface at the anterior of the hard palate in the rogue region with approximately 7 mm × 7 mm in size (Figure 1A). There was nothing abnormal in her past medical history. The lesion was excised completely from its connection to the hard palate through local anaesthesia by diode laser with 300 µm-fibre tip, 808 nm continuous wavelength and 3-3.5 W power for 3×60 seconds (Dr Smile, Italia). During surgery, the fibre tip was in contact with lesions.
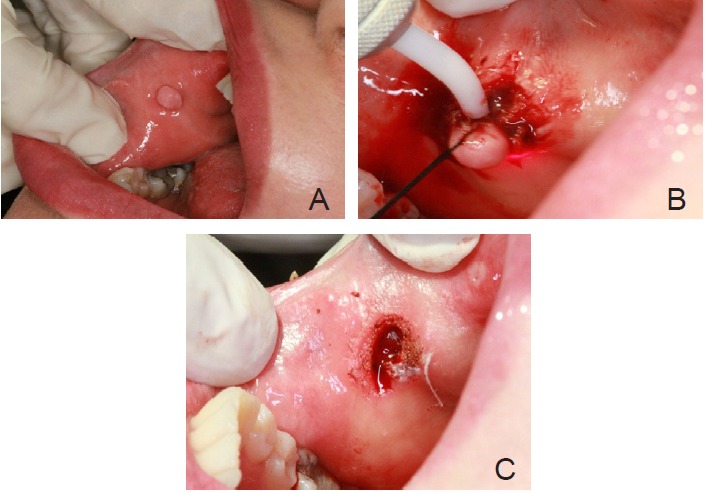
Figure 1 .
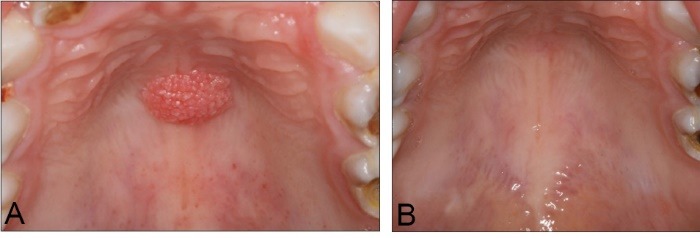
(A) A pedunculated pink-coloured nodule with popular surface at the anterior of the hard palate. (B) A month later, clinical follow-up showed complete tissue healing.
Sections showed characteristic findings of a squamous papilloma, consisting multiple squamous lined papillary fronds including fibrovascular cores. A month later, clinical follow-up showed complete tissue healing (Figure 1B).
Case 2
A 75-year-old married female referred with a chief complaint of painless mass on the palate for many years. There was no history of pain. The present lesion was exophytic and pedunculated in nature, pink-to-red in colour with pebbled surface, firm in consistency, 7 mm × 8 mm in size, and situated on posterior left palate (Figure 2A and B). No similar papule was seen on skin. Past medical, dental and personal history was not significant. No evidence of lymphadenopathy was observed. In this case the lesion was asymptomatic. Lesion was excised completely from its attachment to the palate with diode laser with 300 µm-fibre tip, 808 nm continuous wavelength and 3-3.5 W power for 3×60 seconds (Dr Smile, Italia). During surgery, the fibre tip was in contact with lesions.
Figure 2 .
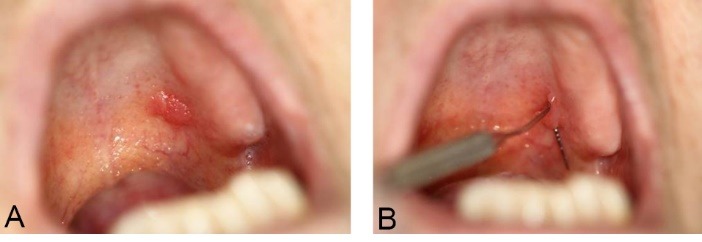
(A) An exophytic and pedunculated lesion, pink-to-red in colour with pebbled surface and situated on posterior left palate. (B) An exophytic and pedunculated lesion, pink-to-red in colour with pebbled surface and situated on posterior left palate
Sections showed an epithelial lesion composed of proliferative para keratinized stratified squamous epithelium with finger like projection and fibrovascular connective tissue cores. Koilocytes and exocytosis was seen in the epithelium. In the underlying loose connective tissue, inflammatory cells infiltration was evident. Final pathologic report was squamous papilloma. Two weeks later, clinical follow-up showed complete tissue healing.
Case 3
A 50-year-old male reported with a small growth on the lingual gingiva of the right mandibular canine. The lesion measured approximately 5×3 mm, papillary surface, normal colour and pedunculated (Figure 3A). It was not tender and firm in consistency with no history of trauma. The patient had noticed the growth over the gingiva four years prior to referral. Lesion had a pedunculated base that was connected to marginal and the attached gingiva. The patient was a smoker and nonalcoholic. For biopsy the lesion was excised under local anaesthesia, by diode laser with 808 nm wavelength and 3.5 W power with 300 µm-fibre tip, for 3×60 seconds (Dr Smile, Italia). During surgery, the fibre tip was in contact with lesions.
Figure 3 .
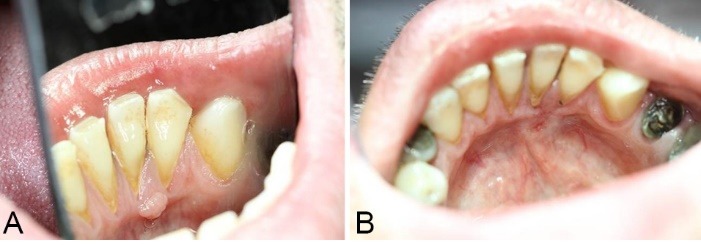
(A) The lesion measured approximately 5 mm × 3 mm, papillary surface, normal colour and pedunculated. (B) A week later, clinical follow-up showed complete tissue healing.
Sections showed a mucosal mass covered by para keratinized stratified squamous epithelium with narrow and enlarged rete ridges. The underlying fibrovascular connective tissue revealed numerous large, stellate fibroblasts and scattered perivascular chronic inflammatory cells infiltration. A week later, the clinical follow-up showed complete tissue healing (Figure 3B). Pathologic features were compatible with giant cell fibroma (GCF).
GCF is an unusual fibrous mucosal mass with several unique features separating it from other oral fibrous hyperplasia.11,12 It was reported by Weathers and Callihan in 1974 first time,13 GCF is found predominantly in the first three decades of life with slight female predilection. The aetiology for GCF remains unknown and it seems that not be associated with chronic irritation.11,12 It typically manifests as an asymptomatic sessile or pedunculated mass in the anterior region of the jaw.11-14 It is a nodule with the size of less than 1 cm, more frequently seen in the mandibular gingiva and the lesion might remain for several years.15
Case 4
A 48-year-old female referred with a chief complaint of 2 masses in right and left cheek regions for last 2 years. The lesions started as small painless mucosal nodules and gradually increased in size with no history of bleeding, paresthesia and pain. Intraoral examination revealed 2-exophytic growth along the right and left buccal mucosa, measuring approximately 20×15 mm in right and 9×10 mm in left side. The overlying mucosa was normal in colour, with no evidence of ulceration (Figure 4A and B). The masses were soft in consistency, sessile, nontender with no bruit or pulse. The lesion was completely excised under local anaesthesia by diode laser with 300 µm-fibre tip, 808 nm continuous wavelength and 3-3.5 W power for 3×60 seconds (Dr Smile, Italia). During surgery, the fibre tip was in contact with lesions.
Figure 4 .
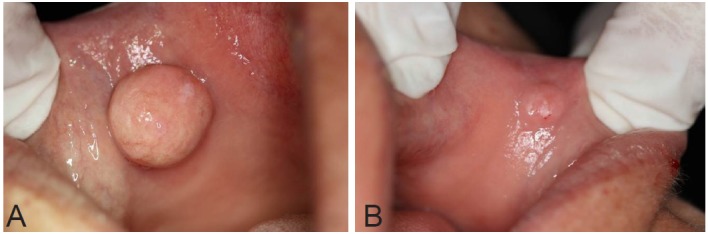
(A) An exophytic growth along the right buccal mucosa, measuring approximately 20 mm × 15 mm. The overlying mucosa was normal in colour, with no evidence of ulceration. (B) An exophytic growth along the left buccal mucosa, measuring approximately 9 mm × 10 mm in left side. The overlying mucosa was normal in colour, with no evidence of ulceration.
Sections showed a nodular mass composed of dense collagen bundles arranged in circular, radiating and haphazard fashion and many fibroblasts. The lesion was covered by hyperkeratotic and parakeratinized stratified squamous epithelium that was compatible with traumatic fibroma.
The patient reported no pain or discomfort during the days after surgery. The healing of the soft tissue was satisfying and scarring could not be seen in the surgery region. The excision of the fibroma with the diode laser was a safe, quick procedure, with minimum complications.
Traumatic fibroma, also known as irritation fibroma, is a frequent exophytic oral lesion that is benign and develops secondary to tissue Injury.
Traumatic fibroma is commonly seen on the tongue, buccal mucosa, and lower labial mucosa.3,7 The potential of growth in fibroma does not exceed 10-20 mm in diameter.3,8
Case 5
A 37 years old woman was referred with a complaint of soft tissue mass in the right buccal surface of her mouth. According to the history, this lesion occurred 2 years prior to referral and it has been larger during this period.
Systemic review showed gastrointestinal disease diagnosed as colitis with no other systemic diseases. Intraoral examination showed an exophytic lesion with smooth surface and sessile base on the right buccal surface of the mouth. The colour of the lesion was pale pink and its consistency was firm with 3 mm × 4 mm in size ( Figure 5A). In her history she noted that she bites this area. For biopsy lesion was excised under local anaesthesia, by diode laser with 808 nm wavelength and 3 W power with 300 µm-fibre tip, continuous wavelength for 3×60 seconds (Dr Smile, Italia). During surgery, fibre tip was in contact with lesions ( Figure 5B and C).
Figure 5 .
(A) An exophytic lesion with smooth surface and sessile base on the right buccal surface of the mouth. (B) The lesion was excised by diode laser with 808nm wavelength and 3W power. (C) The excision of lesions using the diode laser was a quick clinical procedure without bleeding.
Pathology revealed characteristic findings of nodular mass of fibrous tissue and collagen bundles in connective tissue. Final pathologic report was fibroepithelial hyperplasia.
Case 6
A 43-year-old female patient was referred with a complaint of soft tissue mass in the buccal vestibule of the anterior part of the mandible. According to the history, this lesion occurred 5 to 6 months prior to the visit.
Systemic review showed cardiovascular disease and high blood pressure controlled with medication.
Intraoral examination showed an exophytic lesion with smooth surface with sessile base on the right buccal surface of the mouth, approximately 3 mm × 4 mm. Its consistency was firm and the colour of the lesion was pale pink. In her history she noted that she bites this area. The lesion was completely excised under local anaesthesia by diode laser with 300 µm-fibre tip, 808 nm continuous wavelength and 3-3.5 W power for 3×60 seconds (Dr Smile, Italia). During surgery, the fibre tip was in contact with lesions. Procedure was performed more conservatively, with fewer traumas and without bleeding for patient.
Pathology revealed characteristic findings of nodular mass of fibrous tissue and collagen bundles in connective tissue. Final pathologic report was fibroepithelial hyperplasia.
Case 7
A 64-year-old woman was referred with a complaint of soft tissue mass in the dorsal surface of her tongue. According to the history, this lesion occurred 6 years prior to referral.
Systemic review showed prosthetic cardiac valve replacement due to infective endocarditis 41 years ago and a single platelet transfusion. A history of goitre and thyroid surgery and recently, erosive oral lichen planus (6 months duration). The patient was on the following drugs: Warfarin, triamterene H, Ca, Mg, and dexamethasone (mouth wash).
Intraoral examination showed a nodular exophytic lesion with smooth surface on the anterior part of dorsal surface of tongue. Dimensions were approximately 3 mm × 4 mm. Its consistency was firm and the colour of lesion was pale pink (Figure 6A). Dental examination showed incisal edges of mandibular incisors were ruffle and irregular, also degrees of periodontitis was evident.
Figure 6 .
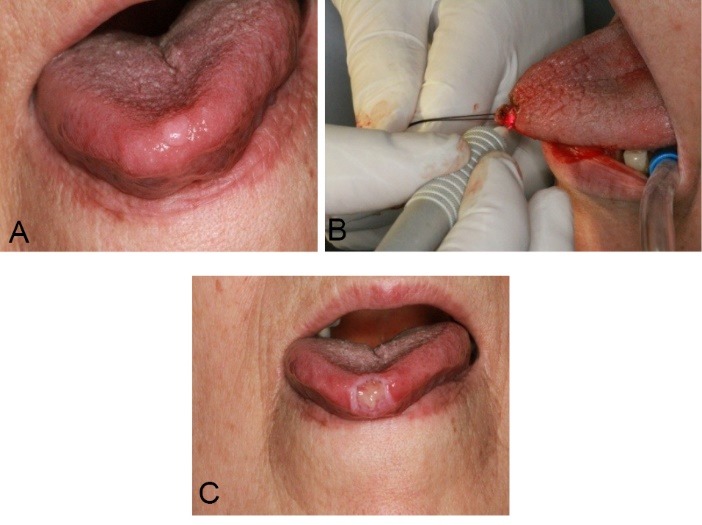
(A) A nodular exophytic lesion with smooth surface on anterior part of dorsal surface of tongue. (B) Lesion was excised with diode laser. (C) Seven days after procedure we saw an ulcer with fibrino-leucocytaire-pseudomembrane on surface.
PT/INR was evaluated, then the lesion was excised for biopsy under local anaesthesia by diode laser with 300 µm-fibre tip, 808 nm continuous wavelength and 3-3.5 W power for 3×60 seconds (Dr Smile, Italia). During surgery, the fibre tip was in contact with lesions (Figure 6B).
7 days after procedure we saw an ulcer with fibrino-leucocytaire membrane on that surface (Figure 6C).
15 days after procedure, healing of the lesion was approximately occurring.
Pathology revealed characteristic findings of nodular mass of fibrous tissue and collagen bundles in connective tissue. Final pathologic report was fibroepithelial hyperplasia.
Case 8
A 19 years old male referred because of swelling in the right of lower lip. The history of the present illness revealed swelling in the lower lip in the inner aspect of lower lip. It had increased for 6 days. The lesion was painless and history of fever or malaise was not reported. It was firm, fluctuant and palpable and the temperature was normal. The size of lesion was 10 mm (Figure 7). The lesion was excised under local anaesthesia, by diode laser with 808 nm wavelength and 3.5 W power (with 300 µm-fibre tip, continuous wavelength for 3×60 seconds [Dr Smile, Italia]. During surgery, the fibre tip was in contact with lesions). 7 days after procedure, we saw an ulcer with fibrino-leucocytaire pseudo-membrane on that surface. 15 days after procedure, healing of the lesion was approximately occurring.
Figure 7 .

Swelling in the Right of Lower Lip.
Pathology revealed characteristic findings of spilled mucin areas containing many mucinophages surrounded by granulation tissue. The lesion was covered by parakeratotic stratified squamous epithelium at surface. Minor salivary gland structures with dilated ducts, patchy chronic inflammatory cell infiltration and haemorrhage were seen.
Mucoceles present as small, translucent, soft, painless swelling of the mucosa with the colour of pink to blue. They are hardly observed on the upper lip, retromolar pad or palate. They might appear at any age, but are seen most commonly in the second and a third decade of life.16 There has no sex predilection reported for this lesion.16
Case 9
A 21-year-old healthy man was referred with complaint of labial mucosal swelling. According to the history, the lesion appeared 1 month prior to referral, after accidental biting of labial mucosa with teeth. The lesion interfered with chewing.
Intra oral examination showed an exophytic lesion, with smooth surface and nodular base on the mucosal surface of right lower lip. The lesion was soft with dimensions of 15 mm × 8 mm. The colour of the lesion and its periphery was red- purple (Figure 8A and 8B). Differential diagnoses for this lesion are mucocele, oral lymphangioma or hemangioma, lipoma, and soft tissue abscess. The lesion was completely excised under local anaesthesia by diode laser with 300µm-fibre tip, 808 nm continuous wavelength and 3-3.5 W power for 3×60 seconds (Dr Smile, Italia). During surgery, the fibre tip was in contact with lesions (Figure 8C). Two weeks after laser surgery, healing was good with minimal scar (Figure 8D).
Figure 8 .
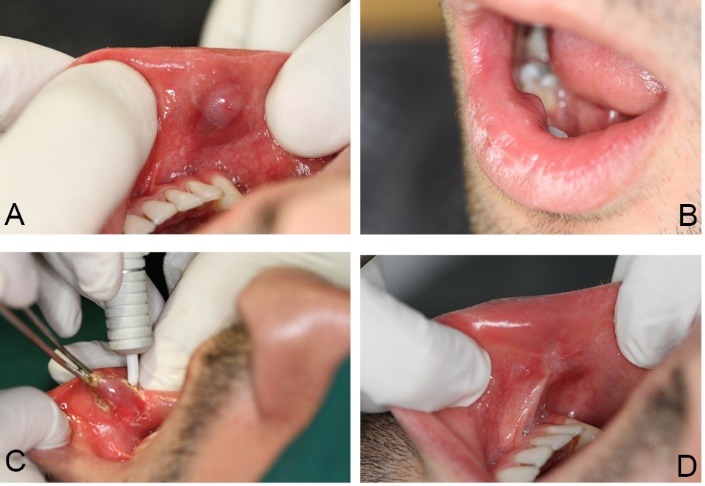
(A) An exophytic lesion, with smooth surface and nodular base on the mucosal surface of lower lip. (B) An exophytic lesion on lower lip. (C) The lesion was excised with diode laser. (D) Two weeks after laser surgery, healing was good with minimal scar.
Pathology revealed characteristic findings of spilled mucin areas containing many mucinophages surrounded by granulation tissue. The lesion was covered by parakeratotic stratified squamous epithelium at surface. Minor salivary gland structures with dilated ducts, patchy chronic inflammatory cell infiltration and haemorrhage were seen.
Case 10
56 years old female referred with chief complain of swelling in cheek. The history of the present illness showed swelling in the right buccal mucosa that was painless. History of fever or malaise was not present. It was a fluctuant, sessile mass with normal colour and smooth surface (Figure 9A). The lesion was excised under local anaesthesia, by diode laser with 808 nm wavelength and 3.5 W power with 300 µm-fibre tip, continuous wavelength for 3×60 seconds (Dr Smile, Italia). During surgery, the fibre tip was in contact with lesions.
Figure 9 .
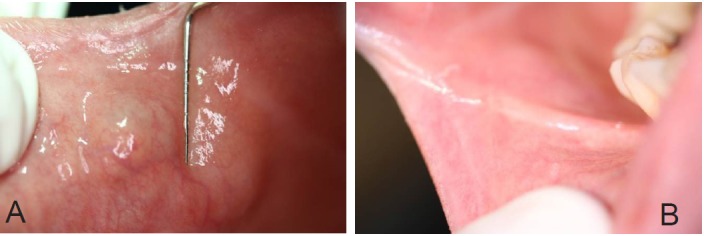
(A) A fluctuant, sessile mass with normal colour and smooth surface. (B) A week later, the clinical follow-up showed complete tissue healing.
Pathology revealed characteristic findings of spilled mucin areas containing many mucinophages surrounded by granulation tissue. The lesion was covered by parakeratotic stratified squamous epithelium at surface. Minor salivary gland structures with dilated ducts, chronic inflammatory cell infiltration were seen. A week later, the clinical follow-up showed complete tissue healing (Figure 9B).
Case 11
A 62 year-old man referred to the clinic with the chief complaint of mass of labial mucosa. The history of the present illness consisted of a mass in left labial mucosa from 12 years before referral, which grew up in the course of time. Lesion was exophytic with smooth and lobulated surface, bluish colour with approximately 15 mm ×18 mm in size (Figure 10A and B). Consistency was firm and without bleeding or pulsating. Diascopy test was positive (Figure 10 C). The lesion was excised under local anaesthesia, by diode laser with 808 nm wavelength and 3 W power (with 300 µm-fibre tip, continuous wavelength for 3×60 seconds [Dr Smile, Italia]. During surgery, the fibre tip was in contact with lesions) (Figure 10 D, E, F). Two weeks after procedure, healing of lesion was approximately occurring.
Figure 10 .
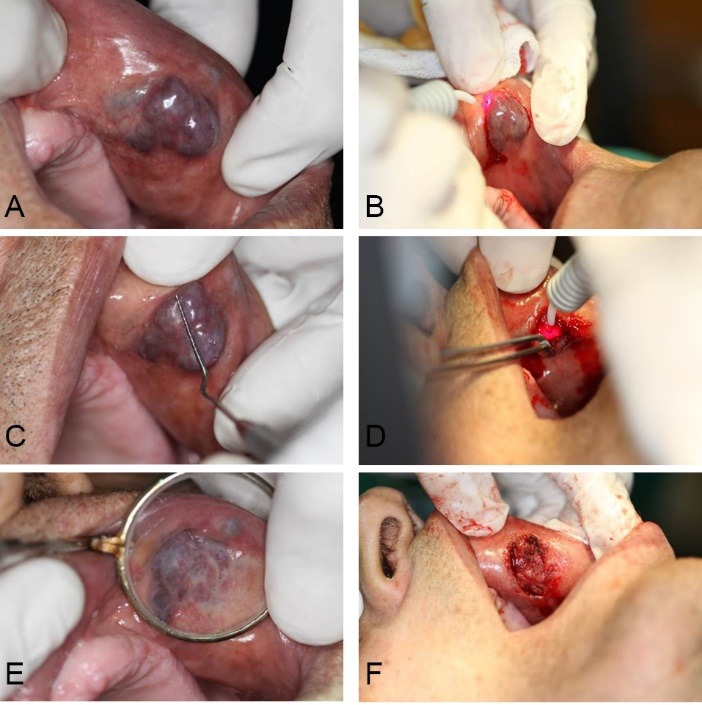
(A) An exophytic mass with smooth and lobulated surface and bluish colour. (B) Lesions were approximately 15×18 mm in diameter. (C) Diascopy test was positive. (D) The lesion was excised with diode laser by 808nm wavelength and 3 watt power was set. (E) The lesion was excised with diode laser. (F) The excision of lesions using the diode laser was quick clinical procedure without bleeding.
Section showed a nodular mass covered by acanthotic stratified squamous epithelium. In the underlying connective tissue, dilated blood vessels with variable size and thickened media layer were seen. Sections of striated muscle, nerve bundle, minor salivary gland structures and haemorrhage were also evident. One year of follow-up was done and no evidence of recurrence of the lesion was noted. The final pathology report was varicosity.
Discussion
We removed 11 oral exophytic lesions by diode laser which had various etiologies, including: vascular, epithelial, salivary gland, and connective tissue. The result was good with rapid tissue healing.
Many investigators use laser to improve dental care. Currently, the primary clinical use of lasers in dentistry is for soft tissue surgery. Several case reports explained that diode laser surgery was highly effective. With laser irradiation, there is less damage to adjacent tissues and better visibility.
The mechanisms of laser, which result in ablation, or decomposition of biological materials are thermal, photochemical, or plasma mediated. The diode laser has been approved by the food and drug administration for virtually all the soft tissue procedures.3 Since the appearance of lasers in dentistry, lasers like carbon dioxide laser (CO2), neodymium-doped yttrium aluminium garnet (Nd:YAG), and erbium-doped YAG (Er:YAG) was used for treatment of a number of intraoral soft tissues lesions such as haemangioma, papilloma and pyogenic granuloma.
The safety and efficacy of laser systems and especially the diode laser have already been evaluated for treatment of facial pigmented, orofacial pain, and intraoral surgery for frenulectomy, and gingivae hyperplasia.1,3,17 The plus point of laser include a approximately bloodless surgical and postsurgical course, the ability to seal nerve endings and lymphatics, minimal swelling and scarring, maintenance of the elastic tissue properties, coagulation and minimal cutting or no suturing in most surgical procedures, reduction in surgical time, reduction in the need for postoperative analgesics/narcotics, and reduced bacterial count.1,3
Moreover no sutures are required and the risk of infection after operation is limited. The clinician has to decide which technique is medically superior for his patients. In the cases explained previously, the use of diode laser was preferred. Also compared to conventional methods, laser surgery is less time consuming. The whole procedure was performed without pain and no sutures were necessary. Haemostasis was optimum immediately after the removal of the lesions. The patients were content with the laser surgery due to the painless procedure either intraoperatively or postoperatively.1
Diode laser contributes significantly to the field of oral soft tissue surgery issues. Diode laser provides advantages to patients and professionals in the field of dentistry. It seems that use of diode laser to be promising in patients who need to be treated with a technique where the blood loss and discomfort should be reduced.1,
Conclusion
This article shows that complete removal of benign exophytic soft tissue lesions with diode laser (with 300 µm-fibre tip, 808 nm continuous wavelength) has been associated with appropriate healing time and minimal bleeding. Also it is useful for lesions inaccessible with blade, lesions in aesthetic zone, lesions with probability of bleeding such as vascular lesions, and for patients with fear from blade surgery. We hope aggressive surgical modalities will be replaced by laser surgery in future.
Conflict of Interest
The authors have no conflict of interest to declare.
Please cite this article as follows: Mazarei Sotoode S, Azimi S, Taheri SA, et al. Diode laser in minor oral surgery: a case series of laser removal of different benign exophytic lesions. J Lasers Med Sci. 2015;6(3):133-138. doi:10.15171/jlms.2015.08.
References
- 1.Eliades A, Stavrianos C, Kokkas A, Kafas P, Nazaroglou I. 808 nm diode laser in oral surgery: a case report of laser removal of fibroma. Res J Med Sci. 2010;4(3):175–8. doi: 10.3923/rjmsci.2010.175.178. [DOI] [Google Scholar]
- 2.Azma E, Safavi N. Diode laser application in soft tissue oral surgery. J Lasers Med Sci. 2013;4(4):206–211. [PMC free article] [PubMed] [Google Scholar]
- 3.Pai JB, Padma R, Divya Malagi S, Kamath V, Shridhar A, Mathews A. Excision of fibroma with diode laser: a case series. J Dent Lasers. 2014;8(1):34–38. doi: 10.4103/0976-2868.134124. [DOI] [Google Scholar]
- 4.Bouquot JE, Gundlach KK. Oral exophytic lesions in 23,616 white Americans over 35 years of age. Oral Surg Oral Med Oral Pathol. 1986;62:284–291. doi: 10.1016/0030-4220(86)90010-1. [DOI] [PubMed] [Google Scholar]
- 5.Kalyanyama BM, Matee MI, Vuhahula E. Oral tumours in Tanzanian children based on biopsy materials examined over 15-year period from 1982 to 1997. Int Dent J. 2002;52:10–14. doi: 10.1111/j.1875-595x.2002.tb00590.x. [DOI] [PubMed] [Google Scholar]
- 6.Esmeili T, Lozada-Nur F, Epstein J. Common benign oral tissue masses. Dent Clin North Am. 2005;49:223–240. doi: 10.1016/j.cden.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 7.Filhoa WN, Morosollib AR, Bianchib M. CO2 laser surgery of obstructive fibroma in the oropharyngeal cavity. J Oral Laser Appl. 2005;5:103–105. [Google Scholar]
- 8. Regezi JA, Sciubba JJ, Jordan RC, Abrahams PH. Oral Pathology: Clinical Pathologic Correlations. 5th ed. St Louis: WB Saunders; 2003:165-166.
- 9.Wigdor AH, Walsh JT Jr, Featherstone JD, Visuri SR, Freid D, Waldvogel JL. Lasers in dentistry. Lasers Surg Med. 1995;16:103–133. doi: 10.1016/0030-4220(86)90010-1. [DOI] [PubMed] [Google Scholar]
- 10. Kalantar Motamedi MH. A Textbook of Advanced Oral and Maxillofacial Surgery. InTech; 2013:341-382.
- 11.Sonalika WG, Sahu A, Deogade SC. et al. Giant cell fibroma of tongue: understanding the nature of an unusual histopathological entity. Case Rep Dent. 2014;2014:864512. doi: 10.1155/2014/864512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gnepp DR. Diagnostic Surgical Pathology of the Head and Neck. 2nd edition. Philadelphia: Saunder; 2009.
- 13.Weathers DR, Callihan MD. Giant cell fibroma. Oral Surg Oral Med Oral Pathol. 1974;37(3):374–384. doi: 10.1016/0030-4220(74)90110-8. [DOI] [PubMed] [Google Scholar]
- 14.Jimson S, Jimson S. Giant cell fibroma: a case report with immunohistochemical markers. J Clin Diagn Res. 2013;7(12):3079–3080. doi: 10.7860/jcdr/2013/6476.3859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Antony VV, Khan R. Giant Cell Fibroma–A Case Report. J Dent Med Sci. 2013;6(6):117–119. [Google Scholar]
- 16.Gupta B, Anegundi R. Mucocele: two case reports. Int J Dent Sci. 2007;6(1):12. [Google Scholar]
- 17.Khalighi HR, Anbari F, Taheri JB, Bakhtiari S, Namazi Z, Pouralibaba F. Effect of low-power laser on treatment of orofacial pain. J Dent Res Dent Clin Prospect. 2010;4(3):75–78. doi: 10.5681/joddd.2010.019. [DOI] [PMC free article] [PubMed] [Google Scholar]


