Abstract
Background
More than 30% of patients hospitalized for heart failure are rehospitalized or die within 90 days of discharge. Lower health literacy is associated with mortality among outpatients with chronic heart failure; little is known about this relationship after hospitalization for acute heart failure.
Methods and Results
Patients hospitalized for acute heart failure and discharged home between November 2010 and June 2013 were followed through December 31, 2013. Nurses administered the Brief Health Literacy Screen at admission; low health literacy was defined as Brief Health Literacy Screen ≤9. The primary outcome was all-cause mortality. Secondary outcomes were time to first rehospitalization and, separately, time to first emergency department visit within 90 days of discharge. Cox proportional hazards models determined their relationships with health literacy, adjusting for age, gender, race, insurance, education, comorbidity, and hospital length of stay. For the 1379 patients, average age was 63.1 years, 566 (41.0%) were female, and 324 (23.5%) had low health literacy. Median follow-up was 20.7 months (interquartile range 12.8 to 29.6 months), and 403 (29.2%) patients died. Adjusted hazard ratio for death among patients with low health literacy was 1.34 (95% CI 1.04, 1.73, P=0.02) compared to Brief Health Literacy Screen >9. Within 90 days of discharge, there were 415 (30.1%) rehospitalizations and 201 (14.6%) emergency department visits, with no evident association with health literacy.
Conclusions
Lower health literacy was associated with increased risk of death after hospitalization for acute heart failure. There was no evident relationship between health literacy and 90-day rehospitalization or emergency department visits.
Keywords: health literacy, health services research, heart failure, mortality
Heart failure affects nearly 6 million Americans, and total direct medical costs exceed $21 billion. By 2030, an estimated 8 million people are expected to have heart failure, with costs exceeding $53 billion.1–3 Patients with heart failure are among those most frequently admitted to the hospital,4–6 and patients hospitalized for acute heart failure (AHF) are at 3 times greater risk for all-cause mortality compared to patients managed as outpatients.7,8 Readmission after hospitalization for AHF is common9; reimbursement and quality measures have been tied to rehospitalization within 30 days, in part to provide incentive to reduce rehospitalizations and emphasize outpatient care for patients with heart failure.
Self-care is a vital component of chronic heart failure management, particularly following hospitalization.10 Health literacy is closely tied to skills necessary for effective self-care of chronic heart failure, including monitoring weight, salt, and fluid intake as well as titration of diuretics.11 Self-management programs targeting low health literacy patients have demonstrated reduced hospitalization or death;12,13 however, other work among outpatients with heart failure found no association between health literacy and self-care.14,15 Healthcare providers frequently overestimate the health literacy skills of their patients16,17; the Institute of Medicine has highlighted the importance of health literacy and the need for methods for identifying patients at risk for low health literacy as part of routine clinical care.18
Among patients with stable chronic heart failure, low health literacy is associated with all-cause mortality but not with hospitalization.19,20 Our aims were to test the hypotheses that among patients hospitalized for acute heart failure with low health literacy there is a greater risk for death, 90-day rehospitalization, and 90-day emergency department (ED) visits.
Methods
Study Design, Setting, and Data Sources
As part of the Health Literacy Screening study,21 we assembled a retrospective cohort of patients who were discharged from an AHF hospitalization at a quaternary care hospital between November 1, 2010 and June 30, 2013. This hospital has 648 beds and receives >44 000 hospitalizations per year. All health literacy and patient outcome data were extracted from the medical center’s enterprise data warehouse and research derivative databases, where data from the electronic health record (EHR) are stored. The medical center’s Institutional Review Board approved this study with a waiver of informed consent.
Population
Hospitalization for AHF was defined as a primary discharge diagnosis of heart failure, indicated by ICD-9 billing codes 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, 404.93, or 428.*. This algorithm was developed for use in all-payer claims datasets22 and has been utilized in multiple prior publications to identify AHF hospitalizations.23–25 Patients were included if they were age 18 years or older; race and gender were available in the EHR; the 3 Brief Health Literacy Screen (BHLS) items were recorded during the index hospitalization; and the patient was discharged from the hospital to home. Patients transferred to other facilities such as rehabilitation or postacute care facilities were excluded because these patients would not typically manage their own medications and diet. Patients who were discharged with home hospice were excluded because they often had end-stage heart failure. The first hospitalization for AHF during the study period was used as the index hospitalization.
Patient-Reported Health Literacy
Health literacy was measured by the BHLS,26,27 which consists of 3 items, each on a 5-point scale (“How often do you have problems learning about your medical condition because of difficulty understanding written information?”; “How confident are you filling out medical forms by yourself?”; and “How often do you have someone (like a family member, friend, hospital/clinic worker, or caregiver) help you read hospital materials?”). Since 2010, these items have been routinely administered by nursing staff as part of hospital admission intake.21 Language preference and use of an interpreter were recorded in the nursing intake assessment. Implementation and widespread use of the BHLS as part of nursing intake was accomplished prior to this study using a quality-improvement framework, with a focus on acceptability, adoption, appropriateness, feasibility, fidelity, and sustainability. The BHLS was implemented across all adult hospital units, the ED, and 3 primary care practices between November 2010 and April 2012. Completion rate was 91.8% for the hospital among 55 611 adult inpatient admissions between November 2010 and September 2011.21 Nurses orally administered the items and recorded patient responses as well as highest level of education, generally within the first 24 hours of hospitalization. Continued compliance with documentation of these items has been high (85% to 90%), though nurses could opt out of asking the BHLS questions if the patient was unable to answer due to medical reasons such as intubation or altered mental status. The nurse-administered BHLS has been shown to be a valid measure of health literacy in our health system when compared to the BHLS and short Test of Functional Health Literacy in Adults administered by research personnel.21,28
The BHLS item addressing confidence with forms was reverse scored, and the 3 responses were summed to generate a score between 3 and 15, where higher scores indicated higher health literacy. Low health literacy was defined as a BHLS score ≤9. This threshold is based on our prior work and was chosen to maximize sensitivity and specificity for correctly classifying patients with low health literacy compared to the short Test of Functional Health Literacy in Adults.29
Outcomes: Death, 90-Day Rehospitalization, ED Visit
The primary outcome was the time from hospital discharge to death, which was censored on December 31, 2013. Date of death was obtained from the Social Security Death Index (SSDI) and by extraction from the institution’s EHR, which also contains clinical documentation of deaths. Of 403 identified deaths, 286 (71.0%) were identified in both Social Security Death Index and EHR; 64 (15.9%) were identified by Social Security Death Index, and 53 (13.2%) were identified in the EHR (and confirmed by chart review). Planned secondary outcomes included time to the first rehospitalization and time to the first ED visit within 90 days of index hospital discharge. Date of rehospitalization and ED visits were identified by extraction from the EHR. Only rehospitalizations and ED visits at the index medical center were identified. ED visits that resulted in rehospitalization were categorized as rehospitalizations.
Covariates
Covariates were chosen based on expected relationships with health literacy, death, or healthcare utilization. The following covariates were recorded during the index hospitalization and extracted from the EHR: age, sex, race (white, black, other; by self-report),30 insurance (private, state/federal, uninsured), and highest level of education. Hospital length of stay was computed by administrative time stamps, and comorbid conditions31 were measured by the Elixhauser comorbidity index. The Elixhauser index includes 30 comorbid conditions and is associated with hospital length of stay, hospital charges, and mortality.32
Statistical Analysis
The primary analysis tested the a priori hypothesis that patients with low health literacy had a shorter time/greater risk of the outcome of death after hospitalization for AHF. Cumulative incidence plots were constructed to visualize the relationship between health literacy level (BHLS ≤9 versus BHLS >9) and outcomes, and the log rank test was used to compare the survival distributions. Adjusted analyses used a Cox proportional hazards model to examine the relationships between health literacy and the primary outcome of time-to-death, adjusting for covariates age, sex, race, insurance status, education, index hospital length of stay, and the Elixhauser comorbidity index. The proportional hazards assumption was evaluated by log-log plots and tested using Schoenfeld residuals.33 The same modeling approach was applied to the planned secondary outcomes of time-to-first rehospitalization and time-to-first ED visit within 90 days, in separate models. Adjusted hazard ratios (aHR) and 95% CI were calculated.
Sensitivity and Subgroup Analyses
Planned sensitivity analyses assessed whether our definitions affected study findings. First, we examined the relationship between health literacy and death across the range of health literacy thresholds. Adjusted Cox regression was repeated for BHLS dichotomized at a score of 14 (BHLS=15, BHLS <15) and for continuous BHLS with restricted cubic splines with 4 knots (at 13, 10, 7, and 4). Second, we conducted stratified analyses by age (<65, ≥65), race (white, nonwhite), education (high school, less than high school), and length of stay for the index hospitalization (≤5 days, >5 days). Third, patients could have multiple hospitalizations over the course of the study duration; therefore, we evaluated rehospitalizations and ED visits using robust standard errors. No adjustment was made for multiple analyses.34 Analyses were conducted using Stata 12.0 (StataCorp, College Station, TX).
Results
Between November 1, 2010 and June 30, 2013, there were 2132 patients hospitalized for AHF; of these, 162 died in the hospital or had unknown hospital disposition and 251 were transferred to a care facility or hospice. Of the remaining 1719 patients, 245 had incomplete BHLS and 95 were missing covariates, leaving 1379 who were discharged home and had complete BHLS and demographic information (Figure 1). Of these, 1055 (76.5%) had a BHLS >9, and 324 (23.5%) had low health literacy (BHLS ≤9). Use of an interpreter was recorded for 33 patients (2.3%). Patient characteristics by health literacy status are found in Table 1; analysis results are found in Table 2 and Table 3. Patients with low health literacy were older and more likely to be male, insured by federal or state health insurance, and to have not completed high school. Elixhauser index and hospital length of stay were similar between the 2 groups. Characteristics of patients excluded from the analyses for missing BHLS or covariates are shown in TableTable 4.
Figure 1.
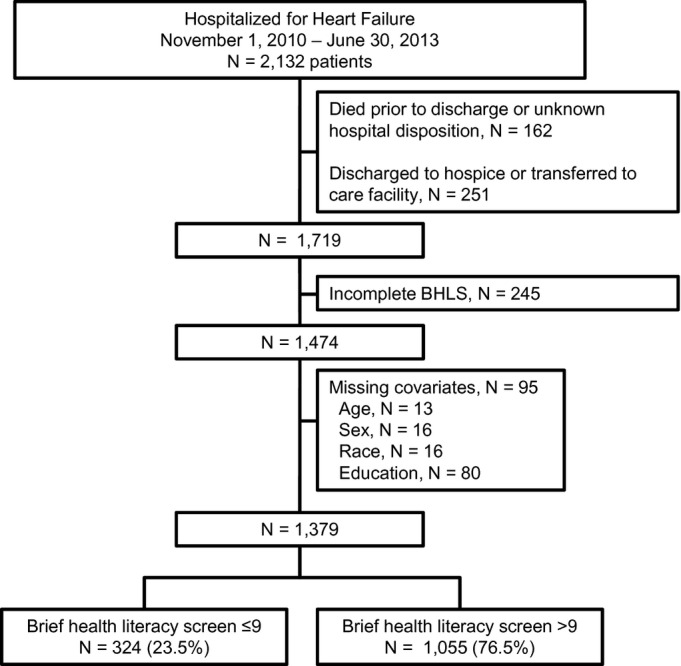
Patient selection. BHLS indicates Brief Health Literacy Screen.
Table 1.
Characteristics of Patients by BHLS Score
| Overall N=1379 | BHLS >9 N=1055 | BHLS ≤9 N=324 | |
|---|---|---|---|
| Age, mean (SD) | 63.1 (14.8) | 61.8 (14.3) | 67.4 (15.7) |
| Female, n (%) | 566 (41.0) | 452 (42.8) | 114 (35.2) |
| Race, n (%) | |||
| White | 1053 (76.4) | 811 (76.9) | 242 (74.7) |
| Black | 294 (21.3) | 225 (21.3) | 69 (21.3) |
| Other | 32 (2.3) | 19 (1.8) | 13 (4.0) |
| Insurance, n (%) | |||
| Private | 328 (23.8) | 284 (26.9) | 44 (13.6) |
| Federal or state | 977 (70.9) | 715 (67.8) | 262 (80.9) |
| Uninsured | 74 (5.4) | 56 (5.3) | 18 (5.6) |
| Completed high school, n (%) | 1285 (93.2) | 1009 (95.6) | 276 (85.2) |
| Hospital LOS, mean (SD) | 4.7 (5.4) | 4.6 (5.0) | 4.9 (6.4) |
| Elixhauser comorbidity index, mean (SD) | 14.9 (6.8) | 14.7 (6.7) | 15.6 (7.1) |
| BHLS, median (IQR) | 13 (10, 15) | 14 (12, 15) | 7 (6, 9) |
| Follow-up time (person-days) | 1 187 089 | 930 494 | 256 595 |
BHLS indicates Brief Health Literacy Screen; IQR, interquartile range; LOS, length of stay.
Table 2.
Adjusted Cox Regression Analyses for Outcomes: Death, 90-Day Rehospitalization, and 90-Day ED Visit by BHLS
| BHLS >9 | BHLS ≤9 | |
|---|---|---|
| N=1055 | N=324 | |
| Deaths* | 279 | 124 |
| Person-time (person-days) | 930 494 | 256 595 |
| Event rate/10 000 person-days (95% CI) | 3.0 (2.6, 3.3) | 4.8 (4.1, 5.8) |
| Adjusted HR (95% CI)†‡ | Reference | 1.32 (1.05, 1.66)§ |
| 90-day rehospitalization | 315 | 100 |
| Person-time (person-days) | 78 644 | 23 699 |
| Event rate/10 000 person-days (95% CI) | 40.1 (35.9, 44.7) | 42.2 (34.7, 51.3) |
| Adjusted HR (95% CI)‡ | Reference | 1.07 (0.83, 1.36) |
| 90-day ED visit | 155 | 46 |
| Person-time (person-days) | 86 897 | 27 119 |
| Event rate/10 000 person-days (95% CI) | 17.8 (15.2, 20.9) | 17.0 (12.7, 22.6) |
| Adjusted HR (95% CI)‡ | Reference | 0.88 (0.61, 1.25) |
| BHLS=15 vs BHLS <15 | BHLS=15 | BHLS <15 |
|---|---|---|
| N=495 | N=884 | |
| Deaths* | 113 | 290 |
| Person-time (person-days) | 450 411 | 736 678 |
| Event rate/10 000 person-days (95% CI) | 2.5 (2.1, 3.0) | 3.9 (3.5, 4.4) |
| Adjusted HR (95% CI)‡ | Reference | 1.35 (1.08, 1.69) § |
BHLS indicates Brief Health Literacy Screen; ED, emergency department; HR, hazard ratio.
N patients included in each analysis.
Cox regression adjusted for age, gender, race, insurance, education, index hospitalization length of stay, and disease severity.
Cox model demonstrates the hazard for the risk of the outcome among those with a BHLS score ≤9 compared to those with a BHLS score >9.
P<0.05.
Table 3.
Stratified Analyses for Mortality by Subgroups
| BHLS >9 | BHLS ≤9 | ||
|---|---|---|---|
| N=1055 | N=324 | P Value for Interaction | |
| Age <65 | |||
| Deaths | 133 | 38 | |
| Person-time (person-days) | 535 143 | 114 147 | |
| Adjusted HR (95% CI)*† | Reference | 1.10 (0.74, 1.63) | |
| Age ≥65 | |||
| Deaths | 146 | 86 | |
| Person-time (person-days) | 395 351 | 142 448 | |
| Adjusted HR (95% CI)*† | Reference | 1.53 (1.15, 2.03)‡ | 0.27 |
| White | |||
| Deaths | 225 | 93 | |
| Person-time (person-days) | 705 104 | 192 585 | |
| Adjusted HR (95% CI)*† | Reference | 1.22 (0.94, 1.58) | |
| Nonwhite | |||
| Deaths | 54 | 31 | |
| Person-time (person-days) | 225 390 | 64 010 | |
| Adjusted HR (95% CI)*† | Reference | 1.76 (1.09, 2.84)‡ | 0.26 |
| Completed high school | |||
| Deaths | 15 | 23 | |
| Person-time (person-days) | 38 293 | 35 519 | |
| Adjusted HR (95% CI)*† | Reference | 1.56 (0.76, 3.16) | |
| Did not complete high school | |||
| Deaths | 264 | 101 | |
| Person-time (person-days) | 892 201 | 221 076 | |
| Adjusted HR (95% CI)*† | Reference | 1.30 (1.03, 1.64)‡ | 0.63 |
| Index hospital LOS ≤5 days | |||
| Deaths | 186 | 92 | |
| Person-time (person-days) | 739 854 | 196 040 | |
| Adjusted HR (95% CI)*† | Reference | 1.52 (1.16, 1.99)‡ | |
| Index hospital LOS >5 days | |||
| Deaths | 93 | 32 | |
| Person-time (person-days) | 190 640 | 60 555 | |
| Adjusted HR (95% CI)*† | Reference | 0.90 (0.57, 1.40) | 0.46 |
BHLS indicates Brief Health Literacy Screen; HR, hazard ratio; LOS, length of stay.
Cox regression adjusted for age, gender, race, insurance, education, index hospitalization length of stay, and disease severity.
Cox model demonstrates the hazard for the risk of the outcome among those with a BHLS score ≤9 compared to those with a BHLS score >9.
P<0.05.
Table 4.
Patient Characteristics Among Those With Incomplete BHLS, BHLS ≤9, and BHLS >9
| Incomplete BHLS | BHLS >9 | BHLS ≤9 | ||
|---|---|---|---|---|
| N=245 | N=1055 | N=324 | P Value* | |
| Age, mean (SD) | 62.0 (18.0) | 61.8 (14.3) | 67.4 (15.7) | 0.01 |
| Female, n (%) | 156 (63.7) | 452 (24.8) | 114 (35.2) | 0.02 |
| Race, n (%) | ||||
| White | 194 (79.2) | 811 (76.9) | 242 (74.7) | 0.40 |
| Black | 45 (18.4) | 225 (21.3) | 69 (21.3) | |
| Other | 6 (2.5) | 19 (1.8) | 13 (4.0) | |
| Insurance, n (%) | <0.001 | |||
| Private | 71 (29.0) | 284 (26.9) | 44 (13.6) | |
| Federal or state | 169 (69.0) | 715 (67.8) | 262 (80.9) | |
| Uninsured | 5 (2.0) | 56 (5.3) | 18 (5.6) | |
| Completed high school, n (%) | 0 (0) | 1009 (95.6) | 276 (85.2) | <0.001 |
| Missing | 220 (89.8) | — | — | |
| Hospital LOS, mean (SD) | 2.8 (5.0) | 4.6 (5.0) | 4.9 (6.4) | <0.001 |
| Elixhauser comorbidity index, mean (SD) | 11.9 (5.8) | 14.7 (6.7) | 15.6 (7.1) | <0.001 |
| Deaths† | 44 | 279 | 124 | |
| Person-time (person-days) | 23 408 | 930 494 | 256 595 | |
| Adjusted HR (95% CI) | 0.74 (0.30, 1.79) | Reference | 1.36 (1.09, 1.71) | |
| Reference | 0.73 (0.30, 1.76)‡ | |||
BHLS indicates Brief Health Literacy Screen; HR, hazard ratio; LOS, length of stay.
Kruskal–Wallis or nonparametric test for trend, as appropriate.
Cox regression for death by BHLS >9, BHLS ≤9, incomplete BHLS; adjusted for age, gender, race, insurance, education, index hospitalization length of stay, and disease severity.
Comparison of subjects with missing BHLS to those with complete BHLS.
Primary Outcome: Hazard of Mortality by Health Literacy
There were 403 (29.2%) deaths during study follow-up (Table2). Median follow-up was 20.7 months (interquartile range 12.8, 29.6 months). Of the 324 patients with BHLS ≤9, 124 (38.3%) died, compared to 279 (26.5%) deaths among the 1055 patients with BHLS >9. The cumulative incidence plots for death are shown in Figure 2. The median time to death was shorter for patients with BHLS ≤9 than for patients with BHLS >9 (log rank P<0.001). After adjusting for age, gender, race, insurance, highest level of education, hospital length of stay, and comorbid conditions, the risk of death for patients with BHLS ≤9 was 32% higher than for patients with BHLS >9 (aHR 1.32; 95% CI 1.05, 1.66, P=0.02).
Figure 2.
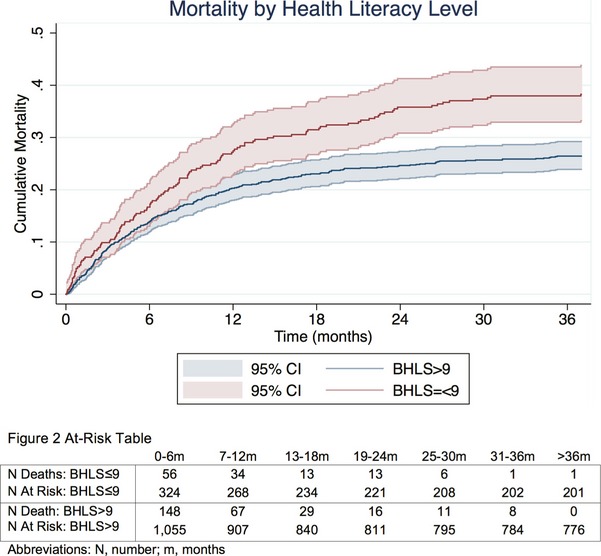
Cumulative hazard of death, by health literacy. BHLS indicates Brief Health Literacy Screen.
Secondary Outcomes: Rehospitalization, ED Visits Within 90 Days
During the 90-day follow-up after each hospitalization for AHF, 415 (30.1%) patients were rehospitalized and 201 (14.6%) had an ED visit and were discharged home. The average number of ED visits within 90 days per patient was 1.84 (median 1, interquartile range 0, 2). There was no evident association of health literacy with time to first rehospitalization or ED visit (Table2).
Sensitivity and Subgroup Analysis
There were 495 (35.9%) patients with the maximum BHLS score of 15. When we varied the threshold for low health literacy to a BHLS score of <15, results were consistent with the main findings (aHR=1.35, 95% CI 1.08, 1.69). When BHLS was modeled using restricted cubic splines, the hazard of death increased as BHLS decreased (Figure 3). Thus, the risk of death for each decreasing level of health literacy was as follows: aHR 1.23 (95% CI 1.03, 1.47), 1.43 (95% CI 1.11, 1.85), 1.48 (95% CI 1.14, 1.91), and 1.50 (95% CI 1.05, 2.13) for BHLS scores of 13, 10, 7, and 4, respectively.
Figure 3.
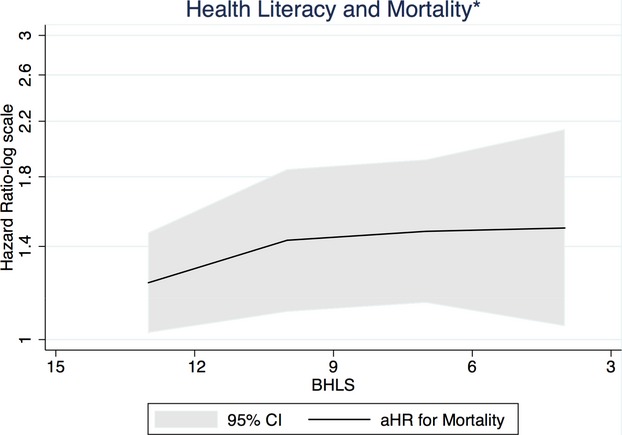
Health literacy and association with mortality—restricted cubic splines. aHR indicates adjusted hazard ratio; BHLS, Brief Health Literacy Screen. *Adjusted for age, sex, race, insurance, education, index hospitalization length of stay, and disease severity.
There was no evidence for effect modification by age, race, education, and hospital length-of-stay, with interaction term P-values all larger than 0.05, although relationships between literacy and mortality were statistically significant only among subgroups for subjects with age ≥65 years, nonwhite race, less than high school education, and index hospital length-of-stay ≤5 days (Table3). Allowing multiple hospitalizations did not change the results of analyses for rehospitalizations or ED visits.
Incomplete BHLS
There were 245 subjects excluded for incomplete BHLS. Compared to patients who completed all 3 BHLS survey items, those with incomplete BHLS were younger, more likely to be female, white, have private insurance, and have had a shorter hospital length of stay. Education level was missing for 220 (89.8%) of these patients; of the 25 patients with education available, none had completed high school (Table4). After adjustment for disease severity and comorbid conditions, there was no difference in mortality risk between those with incomplete and complete BHLS (aHR of death 0.73, 95% CI 0.30, 1.76, Table4).
Discussion
In this study of 1379 patients hospitalized for AHF, low health literacy was associated with increased risk of death (aHR 1.32, 95% CI 1.05, 1.66, P=0.02) after adjustment for education, age, sex, race, health insurance status, hospital length of stay, and comorbidities. This finding was robust across several BHLS cutoffs. Low health literacy, defined as BHLS <15, BHLS <13, or BHLS ≤9 was associated with increased risk of mortality. Taken together, these results suggest that patients with anything less than optimal health literacy who are hospitalized for AHF may warrant additional health resources, assistance, discharge planning, or coordination of care to facilitate the transition from hospital to outpatient care in order to optimize long-term self-care of heart failure. In this study, the relationship between health literacy and mortality was not modified by age, race, or education.
Our findings lend additional weight to the importance of health literacy and provide guidance for healthcare providers as they risk stratify patients hospitalized for AHF. In our healthcare system, results of the health literacy measure are available to all healthcare providers through the EHR, overcoming previous difficulties identifying patients with low health literacy16,17; in the future, this easy access to a reliable measure of health literacy may facilitate more accurate identification of and intervention for patients with heart failure to reduce the risk of death. In general, low health literacy has been associated with multiple health outcomes, including death and healthcare utilization.19,35 Self-care is recognized as a vital component of chronic heart failure management,10 which includes monitoring weight, salt intake, and fluid intake, and titrating diuretics; these in turn may be related to health literacy and mortality. However, the direct relationships among health literacy, self-care, and outcomes including mortality and healthcare utilization are not well understood.14,15 Investigation regarding effective interventions to improve heart failure chronic self-care and patient-centered outcomes is ongoing.36 Patient education alone has generally not been enough to improve outcomes.37
Health literacy can influence chronic disease management. Healthcare providers often overestimate the health literacy skills of their patients.16,17 As a result, patients with unrecognized low health literacy may receive healthcare instructions and prescription regimens that are complex, difficult to understand and implement, limiting their ability to successfully achieve outpatient disease control. These patients may also have difficulty communicating with healthcare providers, navigating the health care system, recognizing signs of health decline, and knowing when and who to contact when they do become ill. Low health literacy may influence mortality via disease self-management as well as unrecognized impact on outpatient disease management by healthcare providers.
In analyses of 90-day rehospitalization and ED visits, we did not find evidence for a relationship with health literacy. These findings are consistent with work by Peterson et al,19 which was conducted among outpatients with heart failure in which the BHLS was administered via mail; in their study, low health literacy (defined as BHLS <6) was found to predict all-cause mortality but not hospitalization. We expand on these findings by showing that this association with mortality is also found among patients hospitalized for AHF and that the risk of death is borne by patients with BHLS <15, not only those with BHLS ≤9 or even BHLS <6. Although we did not find evidence for a relationship between low health literacy and ED visits or with rehospitalizations within 90 days, the proportion of patients who were rehospitalized or had an ED visit is similar to those reported elsewhere.38 ED visits and rehospitalizations after AHF are multifactorial39,40; the relationship between health literacy and mortality among patients with heart failure may be independent of markers of healthcare utilization such as ED visits and rehospitalization. In addition, a weak relationship with ED visits or rehospitalization may not have been detectable in the 90-day follow-up period, compared to the multiyear follow-up for mortality. Finally, we cannot conclusively exclude a relationship between health literacy and rehospitalizations or ED visits because we were unable to include all rehospitalizations and ED visits to other hospitals.
Health literacy was measured by the BHLS, a 3-item survey administered by nursing staff at the time of hospitalization. We have shown this method of administration to be a valid measure of health literacy compared to the short Test of Functional Health Literacy in Adults.41 While patient self-report may increase the risk of social desirability bias, nondifferential misclassification of health literacy would underestimate the true risk of death.42 In a highly health-literate population, the BHLS may be subject to a ceiling effect. However, even in our population, in which 23.5% had low health literacy, we found that low health literacy was associated with increased risk of death.
Limitations to our study should be noted. Analyses included adjustment for age, sex, race, health insurance, highest level of education, hospital length of stay, and comorbidities. Despite this, it is possible that type of heart disease or other difficult-to-measure factors such as depression and patient frailty may have a residual influence on the relationship between health literacy and mortality. We did not include medication changes and management decisions made after discharge from the hospital, as these may be part of the path between patient’s health literacy and outcomes. Hospitalized patients with incomplete education or BHLS may differ in their characteristics from those who with complete BHLS information.43 We did not perform multiple imputation of the BHLS for the 245 subjects with 1 or more BHLS items missing due to the possibility that missingness may not have been random. However, after adjusting for patient characteristics, we did not find a difference in the risk of death between patients with complete and those with incomplete BHLS (Table4). Within the available data, we are unable to account for potential prior hospitalizations, cardiac events, or other indicators of disease severity such as ejection fraction, which have been shown to be associated with death8,44 and may be related to health literacy. Medication adherence was also not available. Finally, we selected this population from patients hospitalized at a quaternary medical center for AHF. While this population may not be reflective of all patients hospitalized with AHF, the methods for identifying patients hospitalized for AHF are standardized and widely used for quality metric reporting. As a result, our findings are likely to be generalizable to many patients hospitalized for AHF who have low health literacy.
Conclusions
In this retrospective study of patients discharged home after hospitalization for AHF, death, rehospitalization, and ED visits were common. Patients with a lower level of health literacy as measured by the BHLS had an increased risk of all-cause death; this risk rose with decreasing health literacy. This suggests that additional measures to overcome barriers to effective long-term heart failure self-care may be needed among patients with any degree of low health literacy.
Acknowledgments
We thank Dr Jesse Ehrenfeld for his assistance with the Elixhauser comorbidity index.
Sources of Funding
This research was supported by funding from the National Heart, Lung, and Blood Institute (R21HL096581, K12HL109109, and UL1TR000445).
Disclosures
Dr Storrow is a current consultant for Roche Diagnostics; Novartis Pharmaceuticals Corp, USA; Alere Diagnostics; Trevena; and Beckman Coulter.
References
- O’Connell JB, Bristow MR. Economic impact of heart failure in the United States: time for a different approach. J Heart Lung Transplant. 1994;13:S107–S112. [PubMed] [Google Scholar]
- Heidenreich PA, Albert NM, Allen LA, Bluemke DA, Butler J, Fonarow GC, Ikonomidis JS, Khavjou O, Konstam MA, Maddox TM, Nichol G, Pham M, Pina IL, Trogdon JG American Heart Association Advocacy Coordinating C, Council on Arteriosclerosis T, Vascular B, Council on Cardiovascular R, Intervention, Council on Clinical C, Council on E, Prevention, Stroke C. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6:606–619. doi: 10.1161/HHF.0b013e318291329a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Soliman EZ, Sorlie PD, Sotoodehnia N, Turan TN, Virani SS, Wong ND, Woo D, Turner MB. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation. 2012;125:e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor CM, Stough WG, Gallup DS, Hasselblad V, Gheorghiade M. Demographics, clinical characteristics, and outcomes of patients hospitalized for decompensated heart failure: observations from the IMPACT-HF registry. J Card Fail. 2005;11:200–205. doi: 10.1016/j.cardfail.2004.08.160. [DOI] [PubMed] [Google Scholar]
- Shah RU, Tsai V, Klein L, Heidenreich PA. Characteristics and outcomes of very elderly patients after first hospitalization for heart failure. Circ Heart Fail. 2011;4:301–307. doi: 10.1161/CIRCHEARTFAILURE.110.959114. [DOI] [PubMed] [Google Scholar]
- Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- Solomon SD, Dobson J, Pocock S, Skali H, McMurray JJ, Granger CB, Yusuf S, Swedberg K, Young JB, Michelson EL, Pfeffer MA. Influence of nonfatal hospitalization for heart failure on subsequent mortality in patients with chronic heart failure. Circulation. 2007;116:1482–1487. doi: 10.1161/CIRCULATIONAHA.107.696906. [DOI] [PubMed] [Google Scholar]
- Setoguchi S, Stevenson LW, Schneeweiss S. Repeated hospitalizations predict mortality in the community population with heart failure. Am Heart J. 2007;154:260–266. doi: 10.1016/j.ahj.2007.01.041. [DOI] [PubMed] [Google Scholar]
- Bueno H, Ross JS, Wang Y, Chen J, Vidan MT, Normand SL, Curtis JP, Drye EE, Lichtman JH, Keenan PS, Kosiborod M, Krumholz HM. Trends in length of stay and short-term outcomes among Medicare patients hospitalized for heart failure, 1993–2006. JAMA. 2010;303:2141–2147. doi: 10.1001/jama.2010.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riegel B, Moser DK, Anker SD, Appel LJ, Dunbar SB, Grady KL, Gurvitz MZ, Havranek EP, Lee CS, Lindenfeld J, Peterson PN, Pressler SJ, Schocken DD, Whellan DJ. State of the science: promoting self-care in persons with heart failure: a scientific statement from the American Heart Association. Circulation. 2009;120:1141–1163. doi: 10.1161/CIRCULATIONAHA.109.192628. [DOI] [PubMed] [Google Scholar]
- Macabasco-O’Connell A, DeWalt DA, Broucksou KA, Hawk V, Baker DW, Schillinger D, Ruo B, Bibbins-Domingo K, Holmes GM, Erman B, Weinberger M, Pignone M. Relationship between literacy, knowledge, self-care behaviors, and heart failure-related quality of life among patients with heart failure. J Gen Intern Med. 2011;26:979–986. doi: 10.1007/s11606-011-1668-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeWalt DA, Malone RM, Bryant ME, Kosnar MC, Corr KE, Rothman RL, Sueta CA, Pignone MP. A heart failure self-management program for patients of all literacy levels: a randomized, controlled trial [ISRCTN11535170] BMC Health Serv Res. 2006;6:30. doi: 10.1186/1472-6963-6-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feltner C, Jones CD, Cene CW, Zheng ZJ, Sueta CA, Coker-Schwimmer EJ, Arvanitis M, Lohr KN, Middleton JC, Jonas DE. Transitional care interventions to prevent readmissions for persons with heart failure: a systematic review and meta-analysis. Ann Intern Med. 2014;160:774–784. doi: 10.7326/M14-0083. [DOI] [PubMed] [Google Scholar]
- Chen AM, Yehle KS, Albert NM, Ferraro KF, Mason HL, Murawski MM, Plake KS. Health literacy influences heart failure knowledge attainment but not self-efficacy for self-care or adherence to self-care over time. Nurs Res Pract. 2013;2013:353290. doi: 10.1155/2013/353290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen AM, Yehle KS, Albert NM, Ferraro KF, Mason HL, Murawski MM, Plake KS. Relationships between health literacy and heart failure knowledge, self-efficacy, and self-care adherence. Res Social Adm Pharm. 2014;10:378–386. doi: 10.1016/j.sapharm.2013.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly PA, Haidet P. Physician overestimation of patient literacy: a potential source of health care disparities. Patient Educ Couns. 2007;66:119–122. doi: 10.1016/j.pec.2006.10.007. [DOI] [PubMed] [Google Scholar]
- Powell CK, Kripalani S. Brief report: resident recognition of low literacy as a risk factor in hospital readmission. J Gen Intern Med. 2005;20:1042–1044. doi: 10.1111/j.1525-1497.2005.0220.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. Health Literacy: A Prescription to End Confusion. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- Peterson PN, Shetterly SM, Clarke CL, Bekelman DB, Chan PS, Allen LA, Matlock DD, Magid DJ, Masoudi FA. Health literacy and outcomes among patients with heart failure. JAMA. 2011;305:1695–1701. doi: 10.1001/jama.2011.512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu JR, Holmes GM, DeWalt DA, Macabasco-O’Connell A, Bibbins-Domingo K, Ruo B, Baker DW, Schillinger D, Weinberger M, Broucksou KA, Erman B, Jones CD, Cene CW, Pignone M. Low literacy is associated with increased risk of hospitalization and death among individuals with heart failure. J Gen Intern Med. 2013;28:1174–1180. doi: 10.1007/s11606-013-2394-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cawthon C, Mion LC, Willens DE, Roumie CL, Kripalani S. Implementing routine health literacy assessment in hospital and primary care patients. Jt Comm J Qual Patient Saf. 2014;40:68–76. doi: 10.1016/s1553-7250(14)40008-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Medicare & Medicaid Services. Heart failure/pneumonia payment measures. Hospital-level, risk-standardized payment associated with a 30-day episode of care for heart failure.Available at: http://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier4&cid=1228774267884. Accessed March 9, 2015.
- Hasegawa K, Tsugawa Y, Camargo CA, Jr, Brown DF. Frequent utilization of the emergency department for acute heart failure syndrome: a population-based study. Circ Cardiovasc Qual Outcomes. 2014;7:735–742. doi: 10.1161/CIRCOUTCOMES.114.000949. [DOI] [PubMed] [Google Scholar]
- Suter LG, Li SX, Grady JN, Lin Z, Wang Y, Bhat KR, Turkmani D, Spivack SB, Lindenauer PK, Merrill AR, Drye EE, Krumholz HM, Bernheim SM. National patterns of risk-standardized mortality and readmission after hospitalization for acute myocardial infarction, heart failure, and pneumonia: update on publicly reported outcomes measures based on the 2013 release. J Gen Intern Med. 2014;29:1333–1340. doi: 10.1007/s11606-014-2862-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krumholz HM, Lin Z, Keenan PS, Chen J, Ross JS, Drye EE, Bernheim SM, Wang Y, Bradley EH, Han LF, Normand SL. Relationship between hospital readmission and mortality rates for patients hospitalized with acute myocardial infarction, heart failure, or pneumonia. JAMA. 2013;309:587–593. doi: 10.1001/jama.2013.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36:588–594. [PubMed] [Google Scholar]
- Chew LD, Griffin JM, Partin MR, Noorbaloochi S, Grill JP, Snyder A, Bradley KA, Nugent SM, Baines AD, Vanryn M. Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med. 2008;23:561–566. doi: 10.1007/s11606-008-0520-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallston KA, Cawthon C, McNaughton CD, Rothman RL, Osborn CY, Kripalani S. Psychometric properties of the brief health literacy screen in clinical practice. J Gen Intern Med. 2014;29:119–126. doi: 10.1007/s11606-013-2568-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willens DE, Kripalani S, Schildcrout JS, Cawthon C, Wallston K, Mion LC, Davis C, Danciu I, Rothman RL, Roumie CL. Association of brief health literacy screening and blood pressure in primary care. J Health Commun. 2013;18(suppl 1):129–142. doi: 10.1080/10810730.2013.825663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Echols MR, Felker GM, Thomas KL, Pieper KS, Garg J, Cuffe MS, Gheorghiade M, Califf RM, O’Connor CM. Racial differences in the characteristics of patients admitted for acute decompensated heart failure and their relation to outcomes: results from the OPTIME-CHF trial. J Card Fail. 2006;12:684–688. doi: 10.1016/j.cardfail.2006.08.003. [DOI] [PubMed] [Google Scholar]
- Pocock SJ, Wang D, Pfeffer MA, Yusuf S, McMurray JJ, Swedberg KB, Ostergren J, Michelson EL, Pieper KS, Granger CB. Predictors of mortality and morbidity in patients with chronic heart failure. Eur Heart J. 2006;27:65–75. doi: 10.1093/eurheartj/ehi555. [DOI] [PubMed] [Google Scholar]
- Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- Schoenfeld D. Chi-squared goodness-of-fit tests for the proportional hazards regression model. Biometrika. 1980;67:145–153. [Google Scholar]
- Savitz DA, Olshan AF. Describing data requires no adjustment for multiple comparisons: a reply from Savitz and Olshan. Am J Epidemiol. 1998;147:813–814. doi: 10.1093/oxfordjournals.aje.a009532. ; discussion 815. [DOI] [PubMed] [Google Scholar]
- Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155:97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- Yehle KS, Plake KS. Self-efficacy and educational interventions in heart failure: a review of the literature. J Cardiovasc Nurs. 2010;25:175–188. doi: 10.1097/JCN.0b013e3181c71e8e. [DOI] [PubMed] [Google Scholar]
- Smith B, Forkner E, Krasuski RA, Galbreath AD, Freeman GL. Educational attainment has a limited impact on disease management outcomes in heart failure. Dis Manag. 2006;9:157–166. doi: 10.1089/dis.2006.9.157. [DOI] [PubMed] [Google Scholar]
- Chun S, Tu JV, Wijeysundera HC, Austin PC, Wang X, Levy D, Lee DS. Lifetime analysis of hospitalizations and survival of patients newly admitted with heart failure. Circ Heart Fail. 2012;5:414–421. doi: 10.1161/CIRCHEARTFAILURE.111.964791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunlay SM, Redfield MM, Weston SA, Therneau TM, Hall Long K, Shah ND, Roger VL. Hospitalizations after heart failure diagnosis a community perspective. J Am Coll Cardiol. 2009;54:1695–1702. doi: 10.1016/j.jacc.2009.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNaughton CD, Collins SP, Kripalani S, Rothman R, Self WH, Jenkins C, Miller K, Arbogast P, Naftilan A, Dittus RS, Storrow AB. Low numeracy is associated with increased odds of 30-day emergency department or hospital recidivism for patients with acute heart failure. Circ Heart Fail. 2013;6:40–46. doi: 10.1161/CIRCHEARTFAILURE.112.969477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallston KA, Cawthon C, McNaughton CD, Rothman RL, Osborn CY, Kripalani S. Psychometric properties of the brief health literacy screen in clinical practice. J Gen Intern Med. 2013;1:119–126. doi: 10.1007/s11606-013-2568-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips CV, LaPole LM. Quantifying errors without random sampling. BMC Med Res Methodol. 2003;3:9. doi: 10.1186/1471-2288-3-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNaughton CD, Kripalani S, Cawthon C, Mion LC, Wallston KA, Roumie CL. Association of health literacy with elevated blood pressure: a cohort study of hospitalized patients. Med Care. 2014;52:346–353. doi: 10.1097/MLR.0000000000000101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee DS, Austin PC, Stukel TA, Alter DA, Chong A, Parker JD, Tu JV. “Dose-dependent” impact of recurrent cardiac events on mortality in patients with heart failure. Am J Med. 2009;122:162–169.e161. doi: 10.1016/j.amjmed.2008.08.026. [DOI] [PubMed] [Google Scholar]


