Abstract
Background
Although there is a close relationship between dietary sodium and hypertension, the concept that persons with relatively high dietary sodium are at increased risk of developing hypertension compared with those with relatively low dietary sodium has not been studied intensively in a cohort.
Methods and Results
We conducted an observational study to investigate whether dietary sodium intake predicts future blood pressure and the onset of hypertension in the general population. Individual sodium intake was estimated by calculating 24-hour urinary sodium excretion from spot urine in 4523 normotensive participants who visited our hospital for a health checkup. After a baseline examination, they were followed for a median of 1143 days, with the end point being development of hypertension. During the follow-up period, hypertension developed in 1027 participants (22.7%). The risk of developing hypertension was higher in those with higher rather than lower sodium intake (hazard ratio 1.25, 95% CI 1.04 to 1.50). In multivariate Cox proportional hazards regression analysis, baseline sodium intake and the yearly change in sodium intake during the follow-up period (as continuous variables) correlated with the incidence of hypertension. Furthermore, both the yearly increase in sodium intake and baseline sodium intake showed significant correlations with the yearly increase in systolic blood pressure in multivariate regression analysis after adjustment for possible risk factors.
Conclusions
Both relatively high levels of dietary sodium intake and gradual increases in dietary sodium are associated with future increases in blood pressure and the incidence of hypertension in the Japanese general population.
Keywords: blood pressure, diet, hypertension, lifestyle, prediction, salt
Hypertension is a leading cause of the mortality and morbidity of cardiovascular disease worldwide,1–4 and reducing elevated blood pressure reduces the risk of developing cardiovascular diseases.5–7 Numerous factors, including genetic, environmental, and lifestyle factors, accelerate or contribute to the development of hypertension.4 Among them, a high level of dietary salt intake is quite important as a modifiable factor.8,9 Epidemiological studies revealed that the incidence of hypertension was greater in populations with higher rather than lower dietary sodium consumption.10 The INTERSALT11 and PURE studies12 demonstrated a positive relationship between 24-hour urinary sodium excretion and blood pressure in a cross-sectional analysis. A close association between dietary sodium consumption and blood pressure levels in individuals has also been proven by interventional studies reducing or increasing daily sodium intake in persons with or without hypertension.13–19
On this basis, guidelines for the treatment of hypertension recommend dietary salt restriction,4,20–22 and many governments in the world recommend a reduction in salt intake for their citizens. The Japanese government (Ministry of Health, Labor, and Welfare [MHLW]) recommends salt intake of <9.0 g/day for the male general population and <7.5 g/day for the female general population.23 Population-based surveys, however, have failed to confirm that public health campaigns aimed at reducing salt intake have been very successful, although effectiveness differs among countries and regions. Individual dietary salt consumption in Japan is still higher than the targets recommended by the MHLW despite gradual yearly reduction. To promote effective salt restriction in the population at large, it is necessary to provide evidence from longitudinal studies that persons with relatively high dietary sodium intake are at higher risk of hypertension compared with those with relatively low dietary sodium consumption. This issue has not been studied intensively in an observational study, although previous cross-sectional and interventional studies strongly suggest that a difference in dietary sodium among individuals in a cohort results in a difference in future blood pressure levels. The present observational study was designed to investigate whether individual levels of dietary sodium critically affect future increases in blood pressure in the general population.
Methods
Study Design
This study was an observational and follow-up study to assess the impact of sodium intake on the incidence of hypertension. We undertook the study in accordance with the principles of the Declaration of Helsinki. The study protocol was approved by the ethics committee of Enshu Hospital. All participants gave written informed consent to participate prior to the start of the study and at each study visit.
Study Participants and Procedures
The present study included men and women aged ≥20 years without hypertension. Participants who visited our hospital for a yearly physical checkup (n =7512) between July 2008 and June 2010 were screened for their eligibility for the present study. Participants undergoing medical treatment for hypertension (n =1409) were excluded. Among the remaining participants (n =6103), the checkup program (including an interview regarding health status, routine physical examination, chest x-ray, electrocardiography, and laboratory assessment of cardiovascular risk factors) revealed that 5237 persons were without hypertension, and they were enrolled in the present study. The follow-up period lasted until June 2013 with the end point being the onset of hypertension. During the follow-up period, blood pressure was measured once a year at the annual health checkup. At each physical checkup, participants were instructed to collect overnight urine in a paper cup and to bring a sample of the urine in a plastic tube. Sodium intake was assessed by estimating 24-hour urinary sodium excretion, which was calculated using the Kamata formula.24 The formula estimates 24-hour sodium excretion using overnight urine and lean body mass in the Japanese population, and the correlation coefficient between measured and estimated sodium excretion is 0.78.24 Linear regression analysis was performed for each participant using a change in blood pressure or sodium intake as a dependent variable and follow-up period (in years) as an independent variable; the slope of the regression line was considered as the yearly change in blood pressure or sodium intake, respectively. For participants who started antihypertensive medication during the study period, changes in blood pressure and sodium intake were calculated using data from before the prescription of antihypertensive drugs. The impact of baseline sodium-intake levels on the yearly change in blood pressure or the onset of hypertension was investigated. The relationship between changes in dietary sodium intake during the follow-up period and blood pressure progression was also analyzed. Because 713 participants attended the health checkup program <3 times after enrollment, data from the remaining 4523 participants (follow-up rate 86.4%; male, n =2903 [64.2%]; mean age 54.1 years; age range 22 to 85 years) were included in the final analysis. Blood pressure was measured by trained technicians using a standard mercury sphygmomanometer in the morning after overnight fasting, with the participant in the sitting position. Three consecutive blood pressure measurements were taken at 2-minute intervals, and the mean of the second and third measurements was recorded as the blood pressure. Hypertension was defined as systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg, or the use of antihypertensive medications.4 Diabetes mellitus was defined as fasting plasma glucose ≥126 mg/dL or the use of antidiabetic medications, and dyslipidemia was defined as low-density lipoprotein cholesterol ≥140 mg/dL, high-density lipoprotein cholesterol <40 mg/dL, triglyceride ≥150 mg/dL, or the use of antidyslipidemic medications.25 The estimated glomerular filtration rate was calculated using the modified Modification of Diet in Renal Disease study formula for the Japanese population.26
Statistical Analysis
All analyses were performed using the software package IBM SPSS Statistics 18 (IBM Corp). Data in the text and tables are expressed as the mean±SD except for the follow-up period, which is expressed as the median value and interquartile range. Differences between 2 means from normally distributed variables were compared using unpaired Student t tests. The significance of any difference in medians was assessed by the Mann–Whitney U test. Yates’ corrected chi-square test was used for comparisons between categorical data. Cumulative incidence rates of new-onset hypertension were calculated using the Kaplan–Meier procedure, and the impact of the estimated 24-hour sodium excretion on the incident hypertension was evaluated by the log-rank and weighed log-rank (Gehan-Wilcoxon) tests. Multivariate Cox proportional hazards regression model was used to obtain hazard ratios and 95% CIs for the time to first diagnosis of hypertension. The proportional hazards assumption was examined and confirmed by using log-log plots. Multivariate Cox proportional hazards regression models were also applied to examine the relationship between baseline sodium intake or a yearly increase in sodium intake, as continuous variables, and the new onset of hypertension. Furthermore, multivariate linear regression analysis was performed to assess the relationship between baseline or a yearly increase in sodium intake and the yearly increase in blood pressure. P<0.05 was considered significant.
Results
Table 1 lists the baseline characteristics of all participants. Sodium intake was significantly higher in men than in women (4.7±1.2 versus 3.3±0.8 g/day, respectively; P<0.001). The actual follow-up period of the present study was 14 072 person-years, and the median follow-up period was 1143 days (interquartile range 741 to 1457 days).
Table 1.
Baseline Characteristics of the Study Participants (n =4523)
| Age, y | 54.1±10.9 |
| Male | 2903 (64.2) |
| Body height, cm | 163.1±8.7 |
| Body weight, kg | 59.4±10.6 |
| Body mass index, kg/m2 | 22.2±2.9 |
| Systolic blood pressure, mm Hg | 118.9±12.4 |
| Diastolic blood pressure, mm Hg | 73.6±8.2 |
| Heart rate, beats/min | 61.8±8.9 |
| Serum creatinine, mg/dL | 0.75±0.15 |
| eGFR, mL/min/1.73 m2 | 78.8±13.8 |
| Uric acid, mg/dL | 5.3±1.4 |
| Fasting plasma glucose, mg/dL | 95.3±15.8 |
| LDL-C, mg/dL | 120.4±27.7 |
| HDL-C, mg/dL | 59.8±14.1 |
| Triglyceride, mg/dL | 107.1±72.9 |
| Hemoglobin, g/dL | 13.9±1.4 |
| Obesity (BMI ≥25) | 690 (15.3) |
| Diabetes mellitus | 261 (5.8) |
| Dyslipidemia | 1781 (39.4) |
| Chronic kidney disease (eGFR <60) | 299 (6.6) |
| Current smoking | 1177 (26.0) |
| Sodium intake, g/day | 4.2±1.3 |
Values are mean±SD or the number (percentage) of participants. BMI indicates body mass index; eGFR, estimated glomerular filtration rate; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol.
Incidence of Hypertension
During the follow-up period, hypertension developed in 1027 participants (22.7%; 73.0 per 1000 person-years), with a higher incidence in men (26.2%; 84.8 per 1000 person-years) than in women (16.5%; 52.3 per 1000 person-years). Table 2 describes the results of the retrospective analyses, showing the characteristics of the participants who did and did not develop hypertension. Baseline sodium intake and the yearly increase in sodium intake were significantly higher in participants with, rather than without, future hypertension (Table 2).
Table 2.
Retrospective Analysis of the Characteristics of the Study Participants
| Without HT (n =3496) | With Future HT (n =1027) | |
|---|---|---|
| Baseline data | ||
| Age, y | 52.9±10.8 | 58.4±10.2* |
| Body height, cm | 163.1±8.8 | 163.3±8.5 |
| Body weight, kg | 58.8±10.5 | 61.5±10.7* |
| BMI, kg/m2 | 22.0±2.8 | 23.0±2.9* |
| SBP, mm Hg | 116.7±12.1 | 126.3±10.2* |
| DBP, mm Hg | 72.4±8.0 | 77.9±7.5* |
| Heart rate, beats/min | 61.7±8.9 | 62.3±8.7‡ |
| Serum creatinine, mg/dL | 0.75±0.15 | 0.77±0.17* |
| eGFR, mL/min/1.73 m2 | 79.3±13.4 | 77.3±14.6* |
| Uric acid, mg/dL | 5.3±1.3 | 5.6±1.3* |
| Fasting plasma glucose, mg/dL | 94.1±13.9 | 99.3±20.4* |
| LDL-C, mg/dL | 119.8±27.4 | 122.5±28.6† |
| HDL-C, mg/dL | 60.2±14.1 | 58.1±14.1* |
| Triglyceride, mg/dL | 103.1±63.1 | 120.6±98.2* |
| Hemoglobin, g/dL | 13.8±1.4 | 14.1±1.4* |
| Current smoking | 912 (26.1) | 265 (25.8) |
| Sodium intake, g/day | 4.1±1.3 | 4.5±1.3 |
| Follow-up data | ||
| Follow-up period, days,median (IQR) | 1428 (1088 to 1460) | 726 (366 to 1088) * |
| Yearly increase in sodium intake, g/day per year§ | 0.02±0.36 | 0.11±0.85* |
| Yearly increase in SBP, mm Hg/year§ | –0.2±3.5 | 6.2±9.8* |
| Yearly increase in DBP, mm Hg/year§ | –0.1±2.5 | 3.2±7.1* |
Values are mean±SD or the number (percentage) of participants, except as noted. BMI indicates body mass index; DBP, diastolic blood pressure; eGFR, estimated glomerular filtration rate; HDL-C, high-density lipoprotein cholesterol; HT, hypertension; IQR, interquartile range; LDL-C, low-density lipoprotein cholesterol; SBP, systolic blood pressure.
P<0.001,
P<0.01,
P<0.05 vs without HT (unpaired Student t test, chi-square test [current smoking], or Mann–Whitney U test [follow-up period]).
In participants who started antihypertensive medication during the study period, yearly changes in sodium intake, SBP, and DBP were calculated using data before the prescription of antihypertensive drugs.
To evaluate the impact of sodium intake at baseline on the incidence of hypertension, participants were divided into 2 groups using the dietary salt (sodium) targets recommended by the Japanese MHLW (men <9.0 g/day; women <7.5 g/day [<3.5 and <3.0 g/day, respectively]). Analysis of the plot of cumulative incidence rates of hypertension revealed that unadjusted risk for hypertension was higher in participants with higher, rather than lower, sodium intake (Figure). Adjustment for age, sex, body mass index, systolic blood pressure, heart rate, serum creatinine, uric acid, fasting plasma glucose, low-density lipoprotein cholesterol, current smoking habit, and family history at baseline showed that the risk of developing hypertension was higher in participants with higher sodium intake (82.1 per 1000 person-years) compared with lower sodium intake (44.0 per 1000 person-years; hazard ratio 1.25, 95% CI 1.04 to 1.50).
Figure 1.
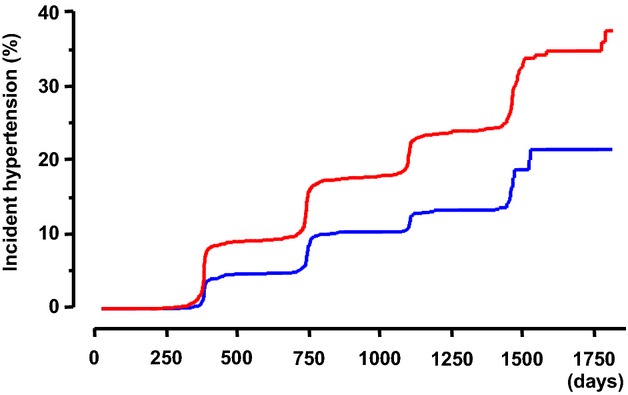
Plots of incidence rate for the new onset of hypertension. Participants were divided into 2 groups using the salt (sodium) intake targets recommended by the Japanese Ministry of Health, Labor, and Welfare (men <9.0 g/day; women <7.5 g/day [<3.5 and <3.0 g/day, respectively]). The red line indicates participants who were above the recommended dietary salt intake target, and the blue line indicates participants who were below the target at baseline (P<0.001, log-rank; P<0.0001, Gehan-Wilcoxon).
We then investigated the impact of baseline sodium intake and the yearly change in sodium intake during the follow-up period (as continuous variables) on the incidence of hypertension (Table 3). In both univariate and multivariate Cox proportional hazards regression analyses (adjusted for age, sex, body mass index, systolic blood pressure, heart rate, serum creatinine, uric acid, fasting plasma glucose, low-density lipoprotein cholesterol, current smoking habit, and family history at baseline), these 2 indices, which represent sodium dependency in individuals, correlated with the incidence of hypertension. To confirm the finding that baseline sodium intake predicts new-onset hypertension, the relationship between the average estimated sodium intake over available annual checkups and the incidence of hypertension during the follow-up period was studied (cross-sectional analysis). The results indicated that the average estimated sodium intake was significantly correlated with the incidence of hypertension during the study period in univariate (r =11.69, P<0.001) and multivariate logistic regression analyses after adjustment for age, sex, body mass index, systolic blood pressure, heart rate, serum creatinine, uric acid, fasting plasma glucose, low-density lipoprotein cholesterol, current smoking habit, and family history (r =2.26, P<0.05).
Table 3.
Univariate and Multivariate Cox Proportional Hazards Regression Analyses Demonstrating the Relationship Between Baseline Sodium Intake or the Yearly Increase in Sodium Intake During the Follow-up Period and the Incidence of Hypertension
| Univariate Analysis | Multivariate Analysis* | |||
|---|---|---|---|---|
| HR (95% CI) | P Value | HR (95% CI) | P Value | |
| Age | 1.04 (1.04 to 1.05) | <0.001 | 1.03 (1.03 to 1.04) | <0.001 |
| Sex, male | 1.63 (1.42 to 1.88) | <0.001 | 1.23 (0.97 to 1.57) | 0.09 |
| Body mass index | 1.10 (1.08 to 1.12) | <0.001 | 1.04 (1.02 to 1.07) | 0.002 |
| Systolic blood pressure | 1.07 (1.06 to 1.08) | <0.001 | 1.07 (1.06 to 1.08) | <0.001 |
| Heart rate | 1.01 (1.00 to 1.02) | 0.004 | 1.00 (1.00 to 1.01) | 0.27 |
| Serum creatinine | 2.71 (1.84 to 3.99) | <0.001 | 0.73 (0.41 to 1.29) | 0.28 |
| Uric acid | 1.17 (1.12 to 1.22) | <0.001 | 1.09 (1.03 to 1.16) | 0.006 |
| Fasting plasma glucose | 1.01 (1.01 to 1.01) | <0.001 | 1.01 (1.00 to 1.01) | 0.003 |
| LDL-C | 1.00 (1.00 to 1.01) | 0.02 | 0.99 (1.00 to 1.00) | 0.28 |
| Current smoking | 0.97 (0.85 to 1.12) | 0.71 | 1.20 (1.02 to 1.42) | 0.03 |
| Family history of HT | 1.54 (1.35 to 1.77) | <0.001 | 1.52 (1.32 to 1.77) | <0.001 |
| Baseline sodium intake | 1.20 (1.15 to 1.26) | <0.001 | 1.09 (1.02 to 1.17) | 0.01 |
| Yearly increase in sodium intake | 1.67 (1.43 to 1.96) | <0.001 | 1.54 (1.32 to 1.81) | <0.001 |
HR indicates hazard ratio; HT, hypertension; LDL-C, low-density lipoprotein cholesterol.
Multivariate model includes age, sex, body mass index, systolic blood pressure, heart rate, serum creatinine, uric acid, fasting plasma glucose, LDL-C, current smoking habit, and family history at baseline as well as baseline sodium intake and yearly increase in sodium intake as confounding factors.
Changes in Blood Pressure
Table 4 shows factors contributing to an increase in systolic blood pressure during the follow-up period. In a univariate regression analysis, the yearly increase in systolic blood pressure was positively correlated with the yearly increase in sodium intake but not with baseline sodium intake; however, baseline sodium intake and yearly increase in sodium intake showed significant correlations with the yearly change in systolic blood pressure in multivariate regression analysis after adjustment for age, sex, body mass index, systolic blood pressure, heart rate, serum creatinine, uric acid, fasting plasma glucose, low-density lipoprotein cholesterol, current smoking habit, and family history at baseline.
Table 4.
Univariate and Multivariate Regression Analyses Demonstrating Factors Having a Possible Relationship With the Yearly Increase in Systolic Blood Pressure
| Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|
| Standardized Coefficient | P Value | Standardized Coefficient | P Value | |
| Age | 0.14 | <0.001 | 0.16 | <0.001 |
| Sex, male | 0.07 | <0.001 | 0.04 | 0.09 |
| Body mass index | 0.02 | 0.25 | 0.06 | <0.001 |
| SBP | –0.18 | <0.001 | –0.24 | <0.001 |
| Heart rate | –0.03 | 0.05 | 0.02 | 0.21 |
| Serum creatinine | 0.02 | 0.14 | –0.06 | 0.006 |
| Uric acid | 0.06 | <0.001 | 0.06 | <0.001 |
| Fasting plasma glucose | 0.08 | <0.001 | 0.06 | <0.001 |
| LDL-C | –0.01 | 0.67 | –0.02 | 0.11 |
| Current smoking | 0.06 | <0.001 | 0.03 | 0.11 |
| Family history of HT | 0.05 | 0.002 | 0.08 | <0.001 |
| Baseline sodium intake | 0.03 | 0.08 | 0.04 | 0.03 |
| Yearly increase in sodium intake | 0.13 | <0.001 | 0.14 | <0.001 |
All variables included in the multivariate analysis are listed in the table. HT indicates hypertension; LDL-C, low-density lipoprotein cholesterol; SBP, systolic blood pressure.
Changes in Sodium Intake
For participants who developed hypertension during the follow-up period, average sodium intake before and after new onset of hypertension was calculated because lifestyle modification including sodium restriction may be recommended by medical professionals after the diagnosis of hypertension; however, the average sodium intake was significantly greater after the onset of hypertension (4.6±1.2 g/day) than before onset (4.5±1.2 g/day; P<0.001). Furthermore, the yearly increase in sodium intake was not reduced after the onset of hypertension (0.11±0.85 versus 0.02±0.76 g/day per year before versus after hypertension, respectively; P =0.070).
Discussion
The present observational study suggests that dietary sodium intake plays an important role in the development of hypertension in the population at large. A small difference in dietary sodium intake among those without hypertension may result in critical differences in individual blood pressure after several years.
The relationship between dietary sodium and hypertension has been discussed intensively for a long time.27 Epidemiological evidence of the relationship between sodium intake and blood pressure has been based on cross-sectional studies,10–12 and clinical interventional studies investigated the effects of changes in sodium intake.13–19 This evidence strongly suggests that persons with relatively high dietary sodium intake are more likely to develop hypertension than those with relatively low dietary sodium consumption. The present study actually observed and confirmed this important concept: The risk of developing hypertension is greater in those with relatively high dietary sodium consumption compared with those with relatively low sodium intake. The present study was not designed to study the mechanisms underlying the hypertensive effects of excessive sodium consumption; therefore, a causal relationship between dietary sodium and the incidence of hypertension cannot be discussed. Nonetheless, taking into consideration previous experimental and clinical studies that showed dietary sodium to be one of the most important keys to the development of hypertension, the present results showed that mild reduction in dietary sodium intake may be useful for preventing new onset of hypertension and reducing age-dependent increase in blood pressure.
Plots of cumulative incidence rates demonstrated that participants with excessive dietary sodium intake were at high risk of developing hypertension. The relationship between dietary sodium and future incidence of hypertension was further confirmed by analyzing sodium intake as a continuous variable. Importantly, sodium intake was also a significant predictor of the yearly increase in blood pressure. This observation reinforces the tight association between dietary sodium and blood pressure. Furthermore, this type of information (risk of accelerated increase in blood pressure) and the finding that sodium is a risk factor for hypertension must be important for the evaluation of cardiovascular risk because the definition of hypertension is arbitrary, and a close and continuous relationship exists between blood pressure and cardiovascular morbidity and mortality.
In the present study, a spot urine specimen was used for estimation of 24-hour urinary sodium excretion, although the gold standard is 24-hour urinary measurement. Furthermore, there is large within-individual and day-to-day variability in dietary sodium. Nonetheless, the results of the cross-sectional analysis in which a significant correlation between the average estimated 24-hour sodium intake during the follow-up period and incident hypertension was observed enhances the present results obtained using a spot urine specimen.
It is noteworthy that we have proposed a new index, the change in dietary sodium, as a predictor of developing hypertension and increasing blood pressure. The observation that the yearly increase in sodium intake correlated with the onset of hypertension or future increases in blood pressure, independent of baseline sodium intake, suggests that the increase in dietary sodium itself plays some role in the development of hypertension. This findings may, at least in part, be attributable to age-dependent increase in salt sensitivity of blood pressure.28 Alternatively, an increase in dietary sodium simply means excessive individual sodium consumption. Although excessive sodium intake causes an increase in blood pressure,16,17 blood pressure does not respond to an increase in sodium intake in sodium-insensitive persons. This may be an excuse for many people not to reduce their sodium intake, although sodium sensitivity increases with increasing age.28 Sodium restriction in the general population and in hypertensive patients is not very successful in Japan.4 An effort not to increase dietary sodium may be effective in preventing the development of hypertension in those with normal blood pressure, although a reduction in sodium consumption is a better strategy for the primary prevention of hypertension.
The present study demonstrates that estimated salt intake is relatively high compared with recommendations in Japan, the United States, and elsewhere. This reinforces the importance of population education for strict dietary salt restriction. In most guidelines for the management of hypertension, lifestyle modification, including salt restriction, is recommended.4,20–22 Unfortunately, dietary sodium intake was not reduced after the development of hypertension in the present observational study, indicating that sodium restriction is not appropriately encouraged at many medical facilities or that people do not or cannot reduce dietary sodium even after development of hypertension. This finding strongly suggests that appropriate methods of effective education need to be developed to reduce dietary sodium intake in hypertensive patients and in the general population.
The present study has some limitations when considering the relationship between sodium intake and blood pressure. Sodium intake was estimated using a spot urine specimen. The gold standard for estimating sodium excretion is 24-hour urinary measurement,29 but this approach is not practical for large-scale studies. In a previous report, the difference between estimated and measured sodium excretion was increased with increasing sodium excretion, and the formula used in the present study tended to underestimate sodium excretion in participants with relatively high sodium excretion.24 Moreover, there is large within-individual and day-to-day variability in dietary sodium.29 Lack of information about alcohol intake, physical activity, and urinary potassium is also a weakness of the present study because close relationships between these factors and the incidence of hypertension have been demonstrated. Another point is that the measurements of urinary sodium and blood pressure were taken only once a year, and the diagnosis of hypertension was based on blood pressure measured on only 1 occasion. Finally, numerous differences were observed at baseline between participants who did and did not develop hypertension. These differences might have affected future blood pressure, although multivariate analyses adjusted for these variables. These points should be considered when interpreting the present data.
In conclusion, the present study demonstrated that both a relatively high level of dietary sodium intake and a gradual increase in dietary sodium, estimated by urinary sodium excretion, are associated with a future increase in blood pressure and incidence of hypertension in the general population. The fact that a mild increase in sodium intake within the range observed in usual daily life but not a drastic sodium load, as observed in interventional studies,16,17 increases the chance of developing hypertension may become a driving force for the reduction of dietary sodium consumption in the general population. Furthermore, an effort not to increase dietary sodium as well as an effort to reduce dietary sodium intake may be effective for the primary prevention of hypertension or reduction of blood pressure in the population at large.
Disclosures
None.
References
- Kannel WB. Hypertension as a risk factor for cardiac events: epidemiologic results of long-term studies. J Cardiovasc Pharmacol. 1993;21:S27–S37. doi: 10.1097/00005344-199321002-00006. [DOI] [PubMed] [Google Scholar]
- Havas S, Roccella EJ, Lenfant C. Reducing the public health burden from elevated blood pressure levels in the United States by lowering intake of dietary sodium. Am J Public Health. 2004;94:19–22. doi: 10.2105/ajph.94.1.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikeda A, Iso H, Yamagishi K, Inoue M, Tsugane S. Blood pressure and the risk of stroke, cardiovascular disease, and all-cause mortality among Japanese: the JPHC Study. Am J Hypertens. 2009;22:273–280. doi: 10.1038/ajh.2008.356. [DOI] [PubMed] [Google Scholar]
- Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, Imai Y, Imaizumi T, Ishimitsu T, Ito M, Ito S, Itoh H, Iwao H, Kai H, Kario K, Kashihara N, Kawano Y, Kim-Mitsuyama S, Kimura G, Kohara K, Komuro I, Kumagai H, Matsuura H, Miura K, Morishita R, Naruse M, Node K, Ohya Y, Rakugi H, Saito I, Saitoh S, Shimada K, Shimosawa T, Suzuki H, Tamura K, Tanahashi N, Tsuchihashi T, Uchiyama M, Ueda S, Umemura S Japanese Society of Hypertension Committee for Guidelines for the Management of Hypertension. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014) Hypertens Res. 2014;37:253–387. doi: 10.1038/hr.2014.20. [DOI] [PubMed] [Google Scholar]
- Psaty BM, Smith NL, Siscovick DS, Koepsell TD, Weiss NS, Heckbert SR, Lemaitre RN, Wagner EH, Furberg CD. Health outcomes associated with antihypertensive therapies used as first line agents. A systematic review and meta analysis. JAMA. 1997;277:739–745. [PubMed] [Google Scholar]
- Blood Pressure Lowering Treatment Trialists’ Collaboration. Turnbull F, Neal B, Pfeffer M, Kostis J, Algert C, Woodward M, Chalmers J, Zanchetti A, MacMahon S. Blood pressure dependent and independent effects of agents that inhibit the renin angiotensin system. J Hypertens. 2007;25:951–958. doi: 10.1097/HJH.0b013e3280bad9b4. [DOI] [PubMed] [Google Scholar]
- Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665. doi: 10.1136/bmj.b1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chien KL, Hsu HC, Chen PC, Su TC, Chang WT, Chen MF, Lee YT. Urinary sodium and potassium excretion and risk of hypertension in Chinese: report from a community-based cohort study in Taiwan. J Hypertens. 2008;26:1750–1756. doi: 10.1097/HJH.0b013e328306a0a7. [DOI] [PubMed] [Google Scholar]
- Weinberger MH. Sodium, potassium, and blood pressure. Am J Hypertens. 1997;10:46S–48S. [PubMed] [Google Scholar]
- Meneely GR, Dahl LK. Electrolytes in hypertension: the effects of sodium chloride. The evidence from animal and human studies. Med Clin North Am. 1961;45:271–283. doi: 10.1016/s0025-7125(16)33891-3. [DOI] [PubMed] [Google Scholar]
- Intersalt Cooperative Research Group. Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. BMJ. 1988;297:319–328. doi: 10.1136/bmj.297.6644.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mente A, O’Donnell MJ, Rangarajan S, McQueen MJ, Poirier P, Wielgosz A, Morrison H, Li W, Wang X, Di C, Mony P, Devanath A, Rosengren A, Oguz A, Zatonska K, Yusufali AH, Lopez-Jaramillo P, Avezum A, Ismail N, Lanas F, Puoane T, Diaz R, Kelishadi R, Iqbal R, Yusuf R, Chifamba J, Khatib R, Teo K, Yusuf S PURE Investigators. Association of urinary sodium and potassium excretion with blood pressure. N Engl J Med. 2014;371:601–611. doi: 10.1056/NEJMoa1311989. [DOI] [PubMed] [Google Scholar]
- The effects of nonpharmacologic interventions on blood pressure of persons with high normal levels. Results of the Trials of Hypertension Prevention, Phase I. JAMA. 1992;267:1213–1220. doi: 10.1001/jama.1992.03480090061028. [DOI] [PubMed] [Google Scholar]
- Whelton PK, Appel LJ, Espeland MA, Applegate WB, Ettinger WH, Jr, Kostis JB, Kumanyika S, Lacy CR, Johnson KC, Folmar S, Cutler JA. Sodium reduction and weight loss in the treatment of hypertension in older persons: a randomized controlled trial of nonpharmacologic interventions in the elderly (TONE). TONE Collaborative Research Group. JAMA. 1998;279:839–846. doi: 10.1001/jama.279.11.839. [DOI] [PubMed] [Google Scholar]
- Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER, III, Simons-Morton DG, Karanja N, Lin PH DASH-Sodium Collaborative Research Group. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344:3–10. doi: 10.1056/NEJM200101043440101. . Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. [DOI] [PubMed] [Google Scholar]
- Luft FC, Rankin LI, Bloch R, Weyman AE, Willis LR, Murray RH, Grim CE, Weinberger MH. Cardiovascular and humoral responses to extremes of sodium intake in normal black and white men. Circulation. 1979;60:697–706. doi: 10.1161/01.cir.60.3.697. [DOI] [PubMed] [Google Scholar]
- Murray RH, Luft FC, Bloch R, Weyman AE. Blood pressure responses to extremes of sodium intake in normal man. Proc Soc Exp Biol Med. 1978;159:432–436. doi: 10.3181/00379727-159-40364. [DOI] [PubMed] [Google Scholar]
- He FJ, MacGregor GA. Effect of modest salt reduction on blood pressure: a meta-analysis of randomized trials. Implications for public health. J Hum Hypertens. 2002;16:761–770. doi: 10.1038/sj.jhh.1001459. [DOI] [PubMed] [Google Scholar]
- Dickinson HO, Mason JM, Nicolson DJ, Campbell F, Beyer FR, Cook JV, Williams B, Ford GA. Lifestyle interventions to reduce raised blood pressure: a systematic review of randomized controlled trials. J Hypertens. 2006;24:215–233. doi: 10.1097/01.hjh.0000199800.72563.26. [DOI] [PubMed] [Google Scholar]
- Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F, Redon J, Dominiczak A, Narkiewicz K, Nilsson PM, Burnier M, Viigimaa M, Ambrosioni E, Caufield M, Coca A, Olsen MH, Schmieder RE, Tsioufis C, van de Borne P, Zamorano JL, Achenbach S, Baumgartner H, Bax JJ, Bueno H, Dean V, Deaton C, Erol C, Fagard R, Ferrari R, Hasdai D, Hoes AW, Kirchhof P, Knuuti J, Kolh P, Lancellotti P, Linhart A, Nihoyannopoulos P, Piepoli MF, Ponikowski P, Sirnes PA, Tamargo JL, Tendera M, Torbicki A, Wijns W, Windecker S, Clement DL, Coca A, Gillebert TC, Tendera M, Rosei EA, Ambrosioni E, Anker SD, Bauersachs J, Hitij JB, Caulfield M, De Buyzere M, De Geest S, Derumeaux GA, Erdine S, Farsang C, Funck-Brentano C, Gerc V, Germano G, Gielen S, Haller H, Hoes AW, Jordan J, Kahan T, Komajda M, Lovic D, Mahrholdt H, Olsen MH, Ostergren J, Parati G, Perk J, Polonia J, Popescu BA, Reiner Z, Rydén L, Sirenko Y, Stanton A, Struijker-Boudier H, Tsioufis C, van de Borne P, Vlachopoulos C, Volpe M, Wood DA. 2013 ESH/ESC guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) Eur Heart J. 2013;34:2159–2219. doi: 10.1093/eurheartj/eht151. [DOI] [PubMed] [Google Scholar]
- James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC, Jr, Svetkey LP, Taler SJ, Townsend RR, Wright JT, Jr, Narva AS, Ortiz E. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) JAMA. 2014;311:507–520. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Guideline: Sodium intake for adults and children. Geneva: World Health Organization (WHO); 2012. . Available at: http://apps.who.int/iris/bitstream/10665/77985/1/9789241504836_eng.pdf?ua=1&ua=1. Accessed June 11, 2015. [PubMed] [Google Scholar]
- National Institute of Health and Nutrition. 2010. Dietary Reference Intakes for Japanese ). The summary report from the Scientific Committee of “Dietary Reference intakes for Japanese”. Available at: http://www0.nih.go.jp/eiken/info/pdf/dris2010en.pdf. Accssed June 11, 2015.
- Kamata K, Tochikubo O. Estimation of 24-h urinary sodium excretion using lean body mass and overnight urine collected by a pipe-sampling method. J Hypertens. 2002;20:2191–2197. doi: 10.1097/00004872-200211000-00018. [DOI] [PubMed] [Google Scholar]
- Teramoto T, Sasaki J, Ueshima H, Egusa G, Kinoshita M, Shimamoto K, Daida H, Biro S, Hirobe K, Funahashi T, Yokote K, Yokode M Japan Atherosclerosis Society (JAS) Committee for Epidemiology and Clinical Management of Atherosclerosis. Diagnostic criteria for dyslipidemia. Executive summary of Japan Atherosclerosis Society (JAS) guideline for diagnosis and prevention of atherosclerotic cardiovascular diseases for Japanese. J Atheroscler Thromb. 2007;14:155–158. doi: 10.5551/jat.e537. [DOI] [PubMed] [Google Scholar]
- Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, Yamagata K, Tomino Y, Yokoyama H, Hishida A Collaborators developing the Japanese equation for estimated GFR. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–992. doi: 10.1053/j.ajkd.2008.12.034. [DOI] [PubMed] [Google Scholar]
- Whelton PK. Sodium, potassium, blood pressure, and cardiovascular disease in humans. Curr Hypertens Rep. 2014;16:465. doi: 10.1007/s11906-014-0465-5. [DOI] [PubMed] [Google Scholar]
- Weinberger MH, Fineberg NS. Sodium and volume sensitivity of blood pressure. Age and pressure change over time. Hypertension. 1991;18:67–71. doi: 10.1161/01.hyp.18.1.67. [DOI] [PubMed] [Google Scholar]
- Whelton PK, Appel LJ, Sacco RL, Anderson CA, Antman EM, Campbell N, Dunbar SB, Frohlich ED, Hall JE, Jessup M, Labarthe DR, MacGregor GA, Sacks FM, Stamler J, Vafiadis DK, Van Horn LV. Sodium, blood pressure, and cardiovascular disease: further evidence supporting the American Heart Association sodium reduction recommendations. Circulation. 2012;126:2880–2889. doi: 10.1161/CIR.0b013e318279acbf. [DOI] [PubMed] [Google Scholar]


