Abstract
Background
Differences in activation of emergency medical services (EMS) may contribute to racial/ethnic and sex disparities in stroke outcomes. The purpose of this study was to determine whether EMS use varied by race/ethnicity and sex among a current, diverse national sample of hospitalized acute stroke patients.
Methods and Results
We analyzed data from 398 798 stroke patients admitted to 1613 Get With The Guidelines–Stroke participating hospitals between October 2011 and March 2014. Multivariable logistic regression was used to evaluate the associations between combinations of racial/ethnic and sex groups with EMS use, adjusting for potential confounders including demographics, medical history, and stroke symptoms. Patients were 50% female, 69% white, 19% black, 8% Hispanic, 3% Asian, and 1% other, and 86% had ischemic stroke. Overall, 59% of stroke patients were transported to the hospital by EMS. White women were most likely to use EMS (62%); Hispanic men were least likely to use EMS (52%). After adjustment for patient characteristics, Hispanic and Asian men and women had 20% to 29% lower adjusted odds of using EMS versus their white counterparts; black women were less likely than white women to use EMS (odds ratio 0.75, 95% CI 0.72 to 0.77). Patients with weakness or paresis, altered level of consciousness, and/or aphasia were significantly more likely to use EMS than patients without each symptom; the observed racial/ethnic and sex differences in EMS use remained significant after adjustment for stroke symptoms.
Conclusions
EMS use differed by race/ethnicity and sex. These contemporary data document suboptimal use of EMS transport among US stroke patients, especially by racial/ethnic minorities and those with less recognized stroke symptoms.
Keywords: disparities, emergency medical services, race/ethnicity, sex, stroke
Stroke is the fourth leading cause of death and the leading cause of serious long-term disability in the United States.1 Racial/ethnic and sex disparities in stroke-related mortality and disability are well documented. Black men and women, for example, have substantially higher stroke mortality rates than white and other persons.1 Functional status after stroke is lower among survivors from racial/ethnic minority backgrounds compared with non-Hispanic white survivors2–5 and is lower among women than men, even after accounting for age and comorbidity.6–8
A significant predictor of stroke-related mortality and disability is the time interval between symptom onset and medical treatment.9–12 Calling emergency services (eg, 911) is recommended as the first action when experiencing stroke symptoms13; the use of emergency medical service (EMS) transport is associated with shorter hospital arrival times,14 more rapid door-to–brain imaging times, and more frequent use of tissue plasminogen activator for acute ischemic stroke with shorter door-to-needle times.15,16
Differences in EMS activation rates could contribute to racial/ethnic and sex disparities in stroke outcomes. Racial/ethnic and sex differences in frequency of stroke symptoms may contribute to disparities in EMS use. The purpose of this study was to determine the association between racial/ethnic group and EMS transport among hospitalized male and female stroke patients, adjusting for confounders. A secondary aim was to determine the independent association between stroke signs or symptoms and EMS use and whether the association was modified by patient race/ethnicity or sex. We hypothesized that EMS use would be lower among racial/ethnic minority men and women compared with their white counterparts and that differences in EMS use by race/ethnicity or sex may be explained in part by differences in stroke symptoms.
Methods
Data Source
The data source for this research was the American Heart Association and American Stroke Association Get With the Guidelines–Stroke (GWTG-Stroke) registry. Details of the design and conduct of the GWTG-Stroke program have been published previously.17,18 Briefly, GWTG-Stroke is an initiative to improve the quality of care delivered to patients with acute stroke and was made available to US hospitals in 2003.17 GWTG-Stroke collects patient-level data on characteristics, diagnostic testing, treatments, adherence to quality measures, and in-hospital outcomes in patients hospitalized with stroke or transient ischemic attack.19
Currently, >1600 hospitals participate in GWTG-Stroke. A central audit has shown good reliability for abstracted variables in the database.20 The company Quintiles serves as the data collection vendor (through its patient management tool) and registry coordination center for GWTG-Stroke and has an agreement to analyze the aggregated deidentified data for research purposes. All participating institutions are required to comply with local regulatory and privacy guidelines and, if required, to secure institutional review board approval. Because data are deidentified, are abstracted from the medical record without registry-specific patient contact, and are used primarily at the local site for quality improvement, many sites were granted a waiver of informed consent under the common rule.
Study Population
The study population comprised patients identified in the GWTG-Stroke registry who were admitted to a GWTG hospital site with an acute stroke diagnosis, who were not transferred from another hospital, and in whom symptom onset did not occur in a health care setting, over the 2.5-year period between October 1, 2011, and March 31, 2014. Of the 569 336 acute strokes, patients were excluded if they were missing data for (1) the location in which stroke symptoms occurred (n=8066; 1%), (2) the mode of transportation to the hospital (n=76 224; 13%), (3) the initial exam (including documentation of stroke symptoms; n=74 417; 13%), or (4) race/ethnicity or sex (n=11 831; 2%). With these exclusions, the primary analysis included 398 798 stroke patients from 1613 participating hospitals (Figure 1).
Figure 1.
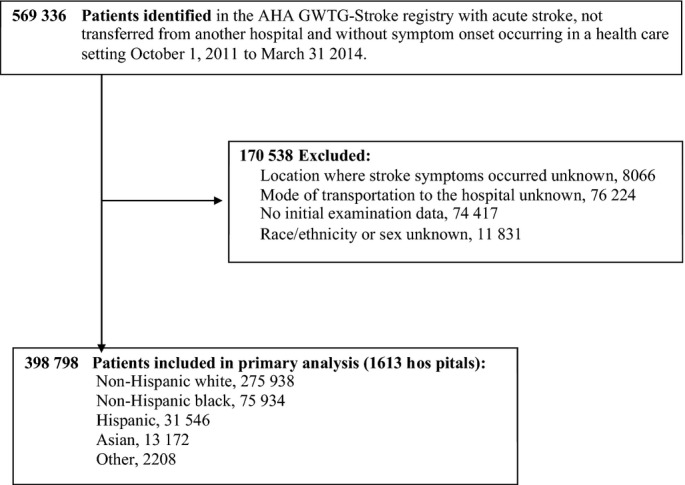
Selection of the study population. AHA indicates American Heart Association; GWTG, Get With The Guidelines.
Study Variables
Race and ethnicity were self-reported by each patient and recorded separately by trained hospital personnel. Race/ethnicity was categorized in this study as (1) non-Hispanic white, (2) non-Hispanic black, (3) Hispanic, (4) Asian, or (5) other (native Hawaiian, Pacific Islander, American Indian, and Alaska Native). Sex and other patient-level data including age, health insurance, medical history (atrial fibrillation or flutter, prior stroke or transient ischemic attack, coronary artery disease or prior myocardial infarction, carotid stenosis, diabetes, peripheral vascular disease, hypertension, dyslipidemia), and admission characteristics (stroke type, National Institutes of Health Stroke Scale [NIHSS], prestroke ambulatory status, and hospital arrival time) were also collected by trained hospital personnel. EMS transport to the hospital (yes versus no) was documented by data collectors at hospital facilities. The presence or absence of specific stroke symptoms or signs was abstracted from each patient’s initial and neurological examinations: (1) weakness or paresis, (2) altered level of consciousness, (3) aphasia, (4) “other neurological symptoms,” and (5) no neurological signs or symptoms. Hospital-level characteristics (region, number of beds, teaching hospital, location [rural versus urban]) were obtained from the American Hospital Association Hospital Statistics.21
Statistical Analyses
Frequency statistics (categorical variables) and quartiles (continuous variables) were completed to describe the distribution of patient characteristics. For categorical variables, Pearson chi-square tests were used to evaluate differences in proportion across racial/ethnic groups. For continuous or ordinal variables, Kruskal–Wallis tests were used to evaluate differences by race or ethnic group.
The association between race or ethnic group and EMS use by men and women was examined using multivariable logistic regression with generalized estimating equations to account for correlation within sites. Adjusted models included the following prespecified covariates: age, health insurance, medical history (atrial fibrillation or flutter, prior stroke or transient ischemic attack, coronary artery disease or prior myocardial infarction, carotid stenosis, diabetes, peripheral vascular disease, hypertension, dyslipidemia), on-hours arrival (Monday to Friday, 7 am to 6 pm), ability to ambulate at admission, initial examination findings for stroke symptoms (weakness or paresis, altered level of consciousness, aphasia, other neurological symptoms, no neurological symptoms), stroke type, and site characteristics (geographic region, rural versus urban, teaching hospital, number of beds). The interaction between race/ethnicity and sex was assessed, and, if significant, relevant pairwise comparisons of race/ethnicity and sex combinations were made using odds ratios.
Potential mediation of the association between race or ethnic group and EMS use by the presence or absence of stroke symptoms was similarly evaluated using multivariable logistic regression to evaluate the associations (1) between race or ethnic group and EMS use, controlling for stroke symptoms; (2) between race or ethnicity and stroke symptoms; and (3) between stroke symptoms and EMS use. In each case, as described for the main effect model, multivariable models with generalized estimating equations to account for correlation within sites were adjusted for prespecified covariates, and race/ethnicity–sex interaction was evaluated.
Missing values of covariates were imputed using the most common value for categorical variables and the median for continuous variables. Data were most commonly missing for ambulatory status at admission (25.0%) and insurance (5.2%); other variables were missing <2.5%. Analyses were repeated to include only patients with documented NIHSS (72% of study population) and were adjusted for NIHSS; this analysis yielded results similar to the primary analyses, thus results for the entire sample were reported without adjustment for NIHSS. We performed a sensitivity analysis in which we used multiple imputation and reran the primary model, which examined the association of race/ethnicity and sex with EMS use. Results from this analysis were not substantially different from the original results and thus are not reported.
Quintiles served as the registry coordinating center. The Duke Clinical Research Institute served as the data analysis center, and institutional review board approval was granted to analyze aggregated deidentified data for research purposes. All P values were 2-sided, and statistical significance was set at P<0.05. Analyses were completed using SAS software version 9.3 or higher (SAS Institute).
Results
Baseline Characteristics
Table 1 describes the demographic, clinical, and hospital characteristics of study participants. Among 398 798 hospitalized stroke patients, 69% were non-Hispanic white, 19% were non-Hispanic black, 8% were Hispanic, 3% were Asian, and 1% other. The majority of admissions (86%) were for ischemic stroke. Patient demographics, admission, and medical conditions varied significantly among racial/ethnic groups.
Table 1.
Participant Demographic, Health Insurance, Admission, Medical, and Hospital Characteristics by Racial/Ethnic Group
| Variables | Overall (N=398 798) | Non-Hispanic White (n=275 938) | Non-Hispanic Black (n=75 934) | Hispanic (n=31 546) | Asian (n=13 172) | Other* (n=2208) |
|---|---|---|---|---|---|---|
| Demographics | ||||||
| Age, y (median)† | 71 | 74 | 63 | 66 | 70 | 65 |
| Male, % | 49.6 | 49.6 | 47.9 | 52.8 | 52.0 | 50.1 |
| Health insurance status, % | ||||||
| Private/VA/Champus/Other | 44.2 | 48.0 | 35.7 | 33.0 | 40.0 | 43.1 |
| Medicaid | 10.5 | 6.4 | 19.6 | 21.4 | 19.5 | 19.5 |
| Medicare | 37.0 | 40.2 | 30.3 | 28.8 | 28.8 | 26.8 |
| Self-pay/no insurance | 7.6 | 5.0 | 13.5 | 16.2 | 10.5 | 9.3 |
| Medical history, % | ||||||
| Atrial fibrillation/flutter | 16.8 | 20.0 | 8.2 | 10.7 | 14.2 | 13.7 |
| Prior stroke/TIA | 29.3 | 28.6 | 33.3 | 27.5 | 24.7 | 29.7 |
| CAD/prior MI | 23.4 | 26.1 | 17.4 | 18.4 | 14.9 | 19.7 |
| Carotid stenosis | 3.2 | 4.0 | 1.3 | 1.8 | 1.6 | 2.4 |
| Diabetes mellitus | 32.1 | 28.3 | 40.5 | 43.1 | 35.4 | 44.5 |
| Hypertension | 75.7 | 73.7 | 83.3 | 75.4 | 76.2 | 76.0 |
| Dyslipidemia | 42.9 | 45.2 | 36.3 | 39.6 | 41.6 | 40.9 |
| Peripheral vascular disease | 4.3 | 4.8 | 3.4 | 2.8 | 1.5 | 2.9 |
| Admission characteristics | ||||||
| Stroke type, % | ||||||
| Ischemic stroke | 85.6 | 86.9 | 85.7 | 81.4 | 76.7 | 82.4 |
| Subarachnoid hemorrhage | 2.5 | 2.4 | 2.2 | 4.0 | 3.9 | 3.8 |
| Intracerebral hemorrhage | 10.6 | 9.8 | 10.9 | 13.5 | 18.6 | 12.6 |
| Stroke NOS | 1.1 | 1.0 | 1.2 | 1.1 | 0.8 | 1.2 |
| NIH stroke scale (median)† | 4.0 | 3.0 | 4.0 | 4.0 | 4.0 | 5.0 |
| Unable to ambulate, % | 32.9 | 32.4 | 32.7 | 34.7 | 38.9 | 37.7 |
| On-hour arrival (Monday to Friday, 7 am to 6 pm), % | 54.8 | 55.6 | 52.9 | 53.5 | 51.2 | 52.1 |
| Hospital characteristics | ||||||
| Region, % | ||||||
| West | 18.6 | 18.2 | 7.4 | 31.6 | 54.0 | 55.8 |
| South | 36.7 | 34.0 | 50.2 | 38.7 | 14.2 | 20.0 |
| Midwest | 17.7 | 19.5 | 18.1 | 6.0 | 8.7 | 11.6 |
| Northeast | 27.0 | 28.4 | 24.3 | 23.8 | 23.0 | 12.6 |
| Number of beds (median)† | 363.0 | 348.0 | 424.0 | 377.0 | 359.0 | 361.0 |
| Teaching hospital, % | 57.4 | 54.1 | 68.8 | 56.9 | 61.5 | 64.5 |
| Site location, % | ||||||
| Rural | 4.7 | 5.9 | 2.5 | 0.9 | 2.0 | 6.5 |
| Urban | 95.3 | 94.1 | 97.5 | 99.1 | 98.0 | 93.5 |
P values are based on Pearson chi-square tests for all categorical row variables; for continuous/ordinal row variables, P values are based on Kruskal–Wallis tests. All tests treat the column variable as nominal (overall column excluded). All comparisons among racial/ethnic groups are statistically significant at P<0.0001. CAD indicates coronary artery disease; MI, myocardial infarction; NIH, National Institutes of Health; NOS, not otherwise specified; TIA, transient ischemic attack; US Department of Veterans Affairs.
Other races include Native Hawaiian, Pacific Islander, American Indian, or Alaskan Native.
P values are based on Kruskal–Wallis tests.
EMS Use by Race/Ethnicity and Sex
Overall, 58.6% of stroke patients used EMS for transport to the hospital. Frequency of EMS use differed by race/ethnicity and by sex (interaction P<0.001) (Figure 2). White women were most likely to use EMS (62.0%); Hispanic men were least likely to use EMS (52.2%). In multivariable models adjusted for prespecified covariates including stroke symptoms, Hispanic and Asian men and women were less likely than their white counterparts to use EMS; black women were less likely than white women to use EMS, but black and white men had similar rates (Table 2).
Figure 2.

Frequency of emergency medical services use by race/ethnicity and sex.
Table 2.
EMS Use by Race/Ethnicity Among Male and Female Stroke Patients
| Subgroup | N | EMS Use, % | Unadjusted OR OR (95% CI) | Adjusted OR* OR (95% CI) |
|---|---|---|---|---|
| Race/ethnicity and sex | ||||
| Men | ||||
| Male/black | 36 403 | 57.9 | 0.91 (0.87 to 0.94) | 1.00 (0.96 to 1.03) |
| Male/Hispanic | 16 646 | 52.2 | 0.72 (0.69 to 0.76) | 0.77 (0.73 to 0.80) |
| Male/Asian | 6854 | 55.4 | 0.84 (0.79 to 0.89) | 0.80 (0.75 to 0.85) |
| Male/other | 1105 | 58.9 | 1.04 (0.92 to 1.19) | 1.09 (0.94 to 1.26) |
| Male/white | 136 773 | 57.0 | (Reference) | (Reference) |
| Women | ||||
| Female/black | 39 531 | 58.0 | 0.75 (0.72 to 0.77) | 0.87 (0.84 to 0.91) |
| Female/Hispanic | 14 900 | 55.5 | 0.66 (0.63 to 0.69) | 0.71 (0.67 to 0.74) |
| Female/Asian | 6318 | 57.2 | 0.74 (0.70 to 0.79) | 0.71 (0.67 to 0.76) |
| Female/other | 1103 | 56.7 | 0.79 (0.69 to 0.91) | 0.89 (0.76 to 1.04) |
| Female/white | 139 165 | 62.0 | (Reference) | (Reference) |
EMS indicates emergency medical services; OR, odds ratio.
Adjusted model contains the following covariates: age, insurance, medical history, on-hours arrival, ability to ambulate at admission, initial examination findings, stroke type, and site characteristics. The race/ethnicity–sex interaction term was statistically significant (likelihood ratio chi-square 119.1, 4 degrees of freedom, P<0.001).
Stroke Symptoms and EMS Use by Race/Ethnicity and Sex
Frequency of stroke symptoms by race/ethnicity and sex is presented in Table 3. Weakness or paresis was the most common stroke symptom (67.3%) and was more frequent among men versus women and among racial/ethnic minorities versus white patients. Aphasia (41.3%) and altered level of consciousness (22.3%) were less frequent, and the frequency varied by both sex and racial/ethnic group (interaction P=0.0007 and P<0.0001, respectively).
Table 3.
Race/Ethnicity and Sex as Predictors of Stroke Symptoms
| Stroke Symptom | Race/Sex Category | With Stroke Symptom (%) | Adjusted OR (95% CI) |
|---|---|---|---|
| Weakness/paresis | Men | 68 | 1.10 (1.06 to 1.15) |
| Women | 67 | Reference | |
| Black | 70 | 1.16 (1.14 to 1.19) | |
| Hispanic | 69 | 1.09 (1.06 to 1.12) | |
| Asian | 69 | 1.23 (1.17 to 1.29) | |
| Other | 69 | 1.16 (1.02 to 1.33) | |
| White | 66 | Reference | |
| Altered level of consciousness | Male/black | 21 | 1.17 (1.13 to 1.20) |
| Male/Hispanic | 22 | 1.11 (1.06 to 1.16) | |
| Male/Asian | 24 | 1.07 (1.00 to 1.13) | |
| Male/other | 25 | 1.17 (1.00 to 1.37) | |
| Male/white | 20 | Reference | |
| Female/black | 22 | 1.02 (0.99 to 1.05) | |
| Female/Hispanic | 26 | 0.99 (0.95 to 1.04) | |
| Female/Asian | 29 | 1.04 (0.97 to 1.11) | |
| Female/other | 29 | 1.18 (1.03 to 1.35) | |
| Female/white | 25 | Reference | |
| Aphasia | Male/black | 41 | 1.07 (1.04 to 1.10) |
| Male/Hispanic | 39 | 0.95 (0.92 to 0.99) | |
| Male/Asian | 39 | 0.97 (0.92 to 1.03) | |
| Male/other | 43 | 1.07 (0.94 to 1.21) | |
| Male/white | 41 | Reference | |
| Female/black | 41 | 1.00 (0.97 to 1.03) | |
| Female/Hispanic | 40 | 0.90 (0.87 to 0.94) | |
| Female/Asian | 39 | 0.91 (0.85 to 0.96) | |
| Female/other | 40 | 0.93 (0.82 to 1.06) | |
| Female/white | 43 | Reference | |
| Other neurological symptoms | Men | 33 | 0.95 (0.91 to 0.99) |
| Women | 32 | Reference | |
| Black | 34 | 0.95 (0.93 to 0.97) | |
| Hispanic | 34 | 1.08 (1.05 to 1.11) | |
| Asian | 35 | 1.05 (1.01 to 1.09) | |
| Other | 35 | 1.00 (0.91 to 1.09) | |
| White | 32 | Reference |
OR indicates odds ratio.
Multivariable models were adjusted for: age, insurance, medical history (atrial fibrillation/flutter, prior stroke or transient ischemic attack, coronary artery disease or prior myocardial infarction, carotid stenosis, diabetes, peripheral vascular disease, hypertension, dyslipidemia), on-hours arrival, ability to ambulate at admission, stroke diagnosis, and site characteristics (geographic region, rural vs urban, teaching hospital, number of beds).
Race and sex were significant predictors of each symptom type; race–sex interactions were not significant for weakness/paresis or other neurological symptoms (P>0.05), thus only main effects are shown for those symptom types.
Approximately one-third of patients (32.4%) had other neurological symptoms on initial examination. The adjusted odds of presenting with other neurological symptoms were higher among women than men and among Asian and Hispanic patients compared with white patients; however, the odds were lower among black patients compared with white patients.
Patients with weakness or paresis, altered level of consciousness, or aphasia on initial examination were more likely to use EMS compared with patients without each symptom (Table 4). The magnitude of the association between the presence versus absence of these stroke symptoms and EMS use was higher among men than among women. The adjusted odds of EMS use among patients with versus without weakness/paresis or aphasia varied by racial/ethnic group and were highest among white patients.
Table 4.
Stroke Symptoms as Predictors of EMS Use
| Stroke Symptom | Race/Sex Category | With Symptom That Used EMS (%) | Without Symptom That Used EMS (%) | Adjusted OR* (95% CI) |
|---|---|---|---|---|
| Weakness/paresis, | Male | 61 | 49 | 1.41 (1.34 to 1.48) |
| Female | 64 | 53 | 1.37 (1.30 to 1.44) | |
| White | 64 | 51 | 1.54 (1.49 to 1.58) | |
| Black | 60 | 52 | 1.34 (1.28 to 1.40) | |
| Hispanic | 56 | 48 | 1.30 (1.22 to 1.38) | |
| Asian | 58 | 52 | 1.22 (1.11 to 1.35) | |
| Other race | 61 | 51 | 1.46 (1.22 to 1.75) | |
| Altered level of consciousness | Male | 78 | 51 | 2.18 (2.10 to 2.25) |
| Female | 80 | 54 | 2.06 (1.99 to 2.13) | |
| Aphasia, | Male | 65 | 51 | 1.33 (1.26 to 1.39) |
| Female | 68 | 55 | 1.28 (1.22 to 1.35) | |
| White | 68 | 54 | 1.45 (1.41 to 1.49) | |
| Black | 65 | 54 | 1.29 (1.24 to 1.34) | |
| Hispanic | 62 | 48 | 1.35 (1.26 to 1.43) | |
| Asian | 64 | 52 | 1.33 (1.22 to 1.45) | |
| Other race | 62 | 55 | 1.04 (0.85 to 1.27) | |
| Other neurological symptoms | All patients | 54 | 61 | 0.93 (0.91 to 0.96) |
EMS indicate emergency medical services.
Multivariable models adjusted for age, health insurance, medical history, on-hours arrival, ability to ambulate at admission, stroke type, and site characteristics and interaction terms if applicable. Tests for 3-way interactions among sex, race/ethnicity, and each stroke symptom were not statistically significant. Interaction-adjusted results are presented if the interaction between sex and symptom or between race/ethnicity and symptom was significant.
Interaction between sex and symptom was significant.
Interaction between race/ethnicity and symptom was significant.
Patients presenting with other neurological symptoms on initial examination were significantly less likely to use EMS transport than those without other neurological symptoms. This association did not vary by race/ethnicity or by sex.
Discussion
In this large, current, national sample of stroke patients, we documented that <60% of acute stroke patients used EMS transport and that racial/ethnic and sex disparities in EMS transport were present. The presence of weakness or paresis, altered level of consciousness, or aphasia was each associated with increased odds of EMS use, whereas other neurological symptoms were associated with lower EMS use. The frequency of each stroke symptom and the magnitude of the association between stroke symptom and EMS use varied by sex and across racial/ethnic groups. The observed associations between race/ethnicity and sex with EMS use persisted after adjustment for stroke symptoms and other prespecified covariates, showing that the racial/ethnic and sex differences in EMS use were not driven solely by differences in stroke symptoms.
Prior research has documented a similarly moderate overall rate of EMS transport among stroke patients, suggesting no substantial increase over recent decades.16,22,23 Lower EMS transport among Hispanic and black versus white stroke patients has also been shown in less contemporary patient populations.16,23 We identified that the racial/ethnic disparity exists among both male and female Hispanic patients, supporting patterns observed in prior research in smaller samples.24 To our knowledge, lower EMS use specifically among female black versus white stroke patients has not been documented previously.
Our study may be among the first to evaluate frequency of EMS use among US Asian stroke patients, overall and by sex. Historical data from the Minnesota Stroke Survey (1991–1993) are consistent with our finding that EMS use is lower among Asian versus white stroke patients, but the relatively low sample size of Asian patients in that study limited the conclusions that could be drawn from those data.25
EMS use was more common among patients with “classic” major stroke symptoms: weakness, aphasia, or altered level of consciousness. These symptoms may be recognized more consistently as signs of stroke than other symptoms. Higher EMS use in patients with these symptoms may also reflect that symptoms are more severe and more likely to interfere with daily function, prompting a call to emergency services, even if not recognized as potentially stroke-related. This finding is consistent with prior research that has documented different frequencies of 911 calls26,27 or seeking hospital care28–30 according to stroke symptom. Public education campaigns have tended to emphasize motor and speech symptoms as signs of stroke and may have influenced EMS activation patterns. The American Heart Association FAST campaign (Face, Arm, Speech, Time to call 911), launched in 2013, is based on recognition of weakness and aphasia or dysarthria.31 The magnitude of the associations between stroke symptoms and EMS activation was greatest among men and white patients, suggesting that women and racial/ethnic minorities may be less influenced by symptom type when deciding to use EMS compared with men and white persons.
The presence of other neurological symptoms on initial examination was associated with lower EMS use, suggesting that, as observed in prior research, patients presenting without motor or speech symptoms have a hospital transport experience different from those with better recognized stroke symptoms.26,32 Almost 1 in 3 patients in this study had other neurological symptoms documented on examination, indicating a potential opportunity to educate about less well-recognized stroke symptoms and calling emergency services. Consistent with prior research, women in this study were more likely than men to present with other neurological symptoms.30,33–35 Hispanic and Asian patients were more likely than white patients to present with other neurological symptoms, a factor that contributed to but did not fully explain the lower EMS use among them.
Strengths of this study include the large diverse national sample, which allowed us to evaluate EMS use overall and by sex and race/ethnicity and to test for interaction between race/ethnicity and sex on EMS use. We were able to illustrate significant relative differences in EMS use and to document absolute differences in EMS use by sex–race/ethnicity strata; absolute differences of almost 10 percentage points were documented when comparing female white and male Hispanic patients. The research was further strengthened by rich covariate data available to adjust for confounding.
This research has limitations. Other factors that may be associated with EMS use among stroke patients, such as the presence of someone else at the time of stroke,7,27,29,36 differential knowledge of stroke symptoms,37,38 English-language proficiency,39 or distance between the stroke location and the hospital, were not measured. Although health insurance type was used as a proxy for socioeconomic status, additional markers of socioeconomic status were not available in the GWTG-Stroke database. The registry did not differentiate between east and south Asian patients, so we cannot comment on any potential impact of our observations regarding Asian participants. GWTG-Stroke and non–GWTG-Stroke participating hospitals differ based on location and size; however, acute stroke patients entered in the GWTG-Stroke program have been shown to be similar to their counterparts admitted to nonparticipating hospitals, supporting the generalizability of results.40 These results do not take into account the potentially most serious stroke patients, who died out of the hospital. Stroke symptom data were collected as part of the initial examination, so we cannot be certain that these same stroke symptoms were present prior to hospital arrival at the time of the decision to call or not call EMS.
Conclusion
In this large sample of patients hospitalized with acute stroke, EMS transport was higher among patients with weakness, aphasia, or altered level of consciousness and lower among those with other neurological symptoms. Hispanic and Asian men and women and black women were less likely to use EMS compared with their white counterparts, independent of stroke symptoms. These contemporary data document suboptimal use of EMS transport among US stroke patients, especially by racial/ethnic minorities and those with less well-recognized stroke symptoms.
Sources of Funding
The Get With The Guidelines–Stroke (GWTG-Stroke) program is provided by the American Heart Association/American Stroke Association. GWTG-Stroke has been funded in the past through support from Boeringher-Ingelheim, Merck, Bristol-Myers Squib/Sanofi Pharmaceutical Partnership, Janssen Pharmaceutical Companies of Johnson & Johnson and the American Heart Association Pharmaceutical Roundtable.
Disclosures
Mochari-Greenberger: None; Xian: None; Hellkamp: None; Schulte: None; Bhatt: Advisory Board: Cardax, Elsevier Practice Update Cardiology, Medscape Cardiology, Regado Biosciences; Board of Directors: Boston VA Research Institute, Society of Cardiovascular Patient Care; Chair: American Heart Association Get With The Guidelines Steering Committee; Data Monitoring Committees: Duke Clinical Research Institute, Harvard Clinical Research Institute, Mayo Clinic, Population Health Research Institute; Honoraria: American College of Cardiology (Senior Associate Editor, Clinical Trials and News, ACC.org), Belvoir Publications (Editor in Chief, Harvard Heart Letter), Duke Clinical Research Institute (clinical trial steering committees), Harvard Clinical Research Institute (clinical trial steering committee), HMP Communications (Editor in Chief, Journal of Invasive Cardiology), Journal of the American College of Cardiology (Associate Editor; Section Editor, Pharmacology), Population Health Research Institute (clinical trial steering committee), Slack Publications (Chief Medical Editor, Cardiology Today’s Intervention), WebMD (CME steering committees); Other: Clinical Cardiology (Deputy Editor); Research Funding: Amarin, AstraZeneca, Bristol-Myers Squibb, Eisai, Ethicon, Forest Laboratories, Ischemix, Medtronic, Pfizer, Roche, Sanofi Aventis, The Medicines Company; Unfunded Research: FlowCo, PLx Pharma, Takeda; Fonarow: Member of the GWTG steering committee, research support from PCORI (significant), and employee of the University of California, which holds a patent on retriever devices for stroke; Saver: Dr Saver is an employee of the University of California. The University of California, Regents receive funding for Dr Saver’s services as a scientific consultant regarding trial design and conduct to Covidien, Stryker, BrainsGate, Pfizer, and St. Jude Medical. Dr Saver has served as an unpaid site investigator in multicenter trials run by Lundbeck for which the UC Regents received payments on the basis of clinical trial contracts for the number of subjects enrolled. Dr Saver serves as an unpaid consultant to Genentech advising on the design and conduct of the PRISMS trial; neither the University of California nor Dr Saver received any payments for this voluntary service. The University of California has patent rights in retrieval devices for stroke; Reeves: None; Schwamm: Chair American Heart Association Get With The Guidelines–Stroke clinical work group (unpaid); Smith: Membership on the Get With The Guidelines Steering Committee (unpaid).
References
- Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Judd SE, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Mackey RH, Magid DJ, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, III, Moy CS, Mussolino ME, Neumar RW, Nichol G, Pandey DK, Paynter NP, Reeves MJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Wong ND, Woo D, Turner MB On Behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation. 2014;129:e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ottenbacher KJ, Campbell J, Kuo YF, Deutsch A, Ostir GC, Granger CV. Racial and ethnic differences in postacute rehabilitation outcomes after stroke in the United States. Stroke. 2008;39:1514–1519. doi: 10.1161/STROKEAHA.107.501254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stansbury JP, Huanguang J, Williams LS, Vogel VB, Duncan PW. Ethnic disparities in stroke: epidemiology, acute care, and postacute outcomes. Stroke. 2005;36:374–386. doi: 10.1161/01.STR.0000153065.39325.fd. [DOI] [PubMed] [Google Scholar]
- Cruz-Flores S, Rabinstein A, Biller J, Elkind MSV, Griffith P, Gorelick PB, Howard G, Leira EC, Morgenstern LB, Ovbiagele B, Peterson E, Rosamond W, Trimble B, Valderrama AL. Racial-ethnic disparities in stroke care: the American experience: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42:2091–2116. doi: 10.1161/STR.0b013e3182213e24. [DOI] [PubMed] [Google Scholar]
- Differences in disability among black and white stroke survivors—United States, 2000–2001. MMWR Morb Mortal Wkly Rep. 2005;54:3–6. [PubMed] [Google Scholar]
- Gargano JW, Reeves MJ. Sex difference in stroke recovery and stroke-specific quality of life: results from a statewide stroke registry. Stroke. 2007;38:2541–2548. doi: 10.1161/STROKEAHA.107.485482. [DOI] [PubMed] [Google Scholar]
- Reeves MJ, Bushnell CD, Howard G, Gargano JW, Duncan PW, Lynch G, Khatiwoda A, Lisabeth L. Sex differences in stroke: epidemiology, clinical presentation, medical care, and outcomes. Lancet Neurol. 2008;7:915–926. doi: 10.1016/S1474-4422(08)70193-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitson HE, Landerman LR, Newman AB, Fried LP, Pieper CF, Cohen HJ. Chronic medical conditions and the sex-based disparity in disability: the Cardiovascular Health Study. J Gerontol A Biol Sci Med Sci. 2010;65:1325–1331. doi: 10.1093/gerona/glq139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saver JL, Fonarow GC, Smith EE, Reeves MJ, Grau-Sepulveda MV, Pan W, Olson DM, Hernandez AF, Peterson ED, Schwamm LH. Time to treatment with intravenous tissue plasminogen activator and outcome from acute ischemic stroke. JAMA. 2013;309:2480–2488. doi: 10.1001/jama.2013.6959. [DOI] [PubMed] [Google Scholar]
- Moser DK, Kimble LP, Alberts MJ, Alonzo A, Croft JB, Dracup K, Evenson KR, Go AS, Hand MM, Kothari RU, Mensah GA, Morris DL, Pancioli AM, Riegel B, Zerwic JJ. Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke. A scientific statement from the American Heart Association Council on Cardiovascular Nursing and Stroke Council. Circulation. 2006;114:168–182. doi: 10.1161/CIRCULATIONAHA.106.176040. [DOI] [PubMed] [Google Scholar]
- Emberson J, Lees KR, Lyden P, Blackwell L, Albers G, Bluhmki E, Brott T, Cohen G, Davis S, Donnan G, Grotta J, Howard G, Kaste M, Koga M, von Kummer R, Lansberg M, Lindley RI, Murray G, Olivot JM, Parsons M, Tilley B, Toni D, Toyoda K, Wahlgren N, Wardlaw J, Whiteley W, Del Zoppo GJ, Baigent C, Sandercock P, Hacke W for the Stroke Thrombolysis Trialists’ Collaborative Group. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet. 2014;384:1929–1935. doi: 10.1016/S0140-6736(14)60584-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fassbender K, Balucani C, Walter S, Levine SR, Haass A, Grotta J. Streamlining of prehospital stroke management: the golden hour. Lancet Neurol. 2013;12:585–596. doi: 10.1016/S1474-4422(13)70100-5. [DOI] [PubMed] [Google Scholar]
- Jauch EC, Saver JL, Adams HP, Jr, Bruno A, Connors JJ, Demaerschalk BM, Khatri P, McMullan PW, Jr, Qureshi AI, Rosenfield K, Scott PA, Summers DR, Wang DZ, Wintermark M, Yonas H American Heart Association Stroke Council; Council on Cardiovascular Nursing; Council on Peripheral Vascular Disease; Council on Clinical Cardiology. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:870–947. doi: 10.1161/STR.0b013e318284056a. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Prehospital and hospital delays after stroke onset—United States, 2005–2006. MMWR Morb Mortal Wkly Rep. 2007;56:474–478. [PubMed] [Google Scholar]
- Lin CB, Peterson ED, Smith EE, Saver JL, Liang L, Xian Y, Olson DM, Shah BR, Hernandez AF, Schwamm LH, Fonarow GC. Emergency medical service hospital prenotification is associated with improved evaluation and treatment of acute ischemic stroke. Circ Cardiovasc Qual Outcomes. 2012;5:514–522. doi: 10.1161/CIRCOUTCOMES.112.965210. [DOI] [PubMed] [Google Scholar]
- Ekundayo OJ, Saver JL, Fonnarow GC, Schwamm LH, Xian Y, Zhao X, Hernanzez AF, Peterson ED, Cheng EM. Patterns of emergency medical services use and its association with timely stroke treatment. Findings from Get With The Guidelines-Stroke. Circ Cardiovasc Qual Outcomes. 2013;6:262–269. doi: 10.1161/CIRCOUTCOMES.113.000089. [DOI] [PubMed] [Google Scholar]
- Schwamm LH, Fonarow GC, Reeves MJ, Pan W, Frankel MR, Smith EE, Ellrodt G, Cannon CP, Liang L, Peterson E, Labresh KA. Get With The Guidelines-Stroke is associated with sustained improvement in care for patients hospitalized with acute stroke or transient ischemic attack. Circulation. 2009;119:107–115. doi: 10.1161/CIRCULATIONAHA.108.783688. [DOI] [PubMed] [Google Scholar]
- Fonarow GC, Reeves MJ, Smith EE, Saver JL, Zhao X, Olson DW, Hernandez AF, Peterson ED, Schwamm LH. Characteristics, performance measures, and in-hospital outcomes of the first one million stroke and transient ischemic attack admissions in Get With The Guidelines-Stroke. Circ Cardiovasc Qual Outcomes. 2010;3:291–302. doi: 10.1161/CIRCOUTCOMES.109.921858. [DOI] [PubMed] [Google Scholar]
- American Heart Association/American Stroke Association. Get With The Guidelines-Stroke Registry. Fact Sheet. Available at: http://www.heart.org/idc/groups/heart-public/@wcm/@gwtg/documents/downloadable/ucm_310976.pdf. Accessed July 1, 2015.
- Xian Y, Fonarow GC, Reeves MJ, Webb LE, Blevins J, Demyanenko VS, Zhao X, Olson DM, Hernandez AF, Peterson ED, Schwamm LH, Smith EE. Data quality in the American Heart Association Get With the Guidelines Stroke program: results from a national data validation audit. Am Heart J. 2012;163:392–398. doi: 10.1016/j.ahj.2011.12.012. [DOI] [PubMed] [Google Scholar]
- American Hospital Association. American Hospital Association Hospital Statistics 2009. Chicago, IL: American Hospital Association; 2009. [Google Scholar]
- Kamel H, Navi BB, Fahimi J. National trends in ambulance use by patients with stroke, 1997–2008. JAMA. 2012;307:1026–1028. doi: 10.1001/jama.2012.285. [DOI] [PubMed] [Google Scholar]
- Govindarajan P, Gonzales R, Maselli JH, Johnston SC, Fahimi J, Poisson S, Stein JC. Regional differences in emergency medical services use for patients with acute stroke (findings from the National Hospital Ambulatory Medical Care Survey Emergency Department Data File) J Stroke Cerebrovasc Dis. 2013;22:e257–e263. doi: 10.1016/j.jstrokecerebrovasdis.2012.02.014. [DOI] [PubMed] [Google Scholar]
- Smith MA, Lisabeth LD, Bonikowski F, Morgenstern LB. The role of ethnicity, sex and language on delay in hospital arrival for acute ischemic stroke. Stroke. 2010;41:905–909. doi: 10.1161/STROKEAHA.110.578112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith MA, Doliszny KM, Shahar E, McGovern PG, Arnett DK, Leupker RV. Delayed hospital arrival for acute stroke: the Minnesota Stroke Survey. Ann Intern Med. 1998;129:190–196. doi: 10.7326/0003-4819-129-3-199808010-00005. [DOI] [PubMed] [Google Scholar]
- Kleindorfer D, Lindsell CJ, Moomaw CJ, Alwell K, Woo D, Flaherty ML, Adeoye O, Zakaria T, Broderick JP, Kissela BM. Which stroke symptoms prompt a 911 call? A population-based study. Am J Emerg Med. 2010;28:607–612. doi: 10.1016/j.ajem.2009.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosley I, Nicol M, Donnan G, Patrick I, Dewey H. Stroke symptoms and the decision to call for an ambulance. Stroke. 2007;38:361–366. doi: 10.1161/01.STR.0000254528.17405.cc. [DOI] [PubMed] [Google Scholar]
- Maze LM, Bakas T. Factors associated with hospital arrival time for stroke patients. J Neurosci Nurs. 2004;36:136–141. 155. [PubMed] [Google Scholar]
- Mandelzweig L, Goldbourt U, Boyko V, Tanne D. Perceptual, social, and behavioral factors associated with delays in seeking medical care in patients with symptoms of acute stroke. Stroke. 2006;37:1248–1253. doi: 10.1161/01.STR.0000217200.61167.39. [DOI] [PubMed] [Google Scholar]
- Gargano JW, Wehner S, Reeves MJ. Do presenting symptoms explain sex differences in emergency department delays among patients with acute stroke. Stroke. 2009;40:1114–1120. doi: 10.1161/STROKEAHA.108.543116. [DOI] [PubMed] [Google Scholar]
- American Heart Association/American Stroke Association Spot a Stroke FAST. Stroke Warning Signs and Symptoms. Available at: http://strokeassociation.org/STROKEORG/WarningSigns/Stroke-Warning-Signs-and-Symptoms_UCM_308528_SubHomePage.jsp. Accessed July 1, 2015.
- Zerwic J, Hwang SY, Tucco L. Interpretation of symptoms and delay in seeking treatment by patients who have had a stroke: exploratory study. Heart Lung. 2007;36:25–34. doi: 10.1016/j.hrtlng.2005.12.007. [DOI] [PubMed] [Google Scholar]
- Stuart-Shor EM, Wellenius GA, delloIacono DM, Mittleman MA. Gender differences in presenting and prodromal stroke symptoms. Stroke. 2009;40:1121–1126. doi: 10.1161/STROKEAHA.108.543371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lisabeth LD, Brown DL, Hughes R, Majersik JJ, Morgenstern LB. Acute stroke symptoms. Comparing women and men. Stroke. 2009;40:2031–2036. doi: 10.1161/STROKEAHA.109.546812. [DOI] [PubMed] [Google Scholar]
- Beal CC. Gender and stroke symptoms: a review of the current literature. J Neurosci Nurs. 2010;42:80–87. [PubMed] [Google Scholar]
- Schroeder EB, Rosamond WD, Morris DL, Evanson KR, Hinn AR. Determinants of use of emergency medical services in a population with stroke symptoms. The Second Delay in Accessing Stroke Healthcare (DASH II) Study. Stroke. 2000;31:2591–2596. doi: 10.1161/01.str.31.11.2591. [DOI] [PubMed] [Google Scholar]
- Ferris A, Robertson R, Fabunmi R, Mosca L. American Heart Association and American Stroke Association national survey of stroke risk awareness among women. Circulation. 2005;111:1321–1326. doi: 10.1161/01.CIR.0000157745.46344.A1. [DOI] [PubMed] [Google Scholar]
- Mochari-Greenberger H, Towfighi A, Mosca L. National women’s knowledge of stroke warning signs, overall and by race/ethnic group. Stroke. 2014;45:1180–1182. doi: 10.1161/STROKEAHA.113.004242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DuBard CA, Garrett J, Gizlice Z. Effect of language on heart attack and stroke awareness among U.S. Hispanics. Am J Prev Med. 2006;30:189–196. doi: 10.1016/j.amepre.2005.10.024. [DOI] [PubMed] [Google Scholar]
- Reeves MJ, Fonarow GC, Smith EE, Pan W, Olson D, Hernandez AF, Peterson ED, Schwamm LH. Representativeness of the Get With The Guidelines-Stroke Registry. Stroke. 2012;43:44–49. doi: 10.1161/STROKEAHA.111.626978. [DOI] [PubMed] [Google Scholar]


