Abstract
Background
Short-term risk assessment tools for prediction of cardiovascular disease events are widely recommended in clinical practice and are used largely for single time-point estimations; however, persons with low predicted short-term risk may have higher risks across longer time horizons.
Methods and Results
We estimated short-term and lifetime cardiovascular disease risk in a pooled population from 2 studies of Peruvian populations. Short-term risk was estimated using the atherosclerotic cardiovascular disease Pooled Cohort Risk Equations. Lifetime risk was evaluated using the algorithm derived from the Framingham Heart Study cohort. Using previously published thresholds, participants were classified into 3 categories: low short-term and low lifetime risk, low short-term and high lifetime risk, and high short-term predicted risk. We also compared the distribution of these risk profiles across educational level, wealth index, and place of residence. We included 2844 participants (50% men, mean age 55.9 years [SD 10.2 years]) in the analysis. Approximately 1 of every 3 participants (34% [95% CI 33 to 36]) had a high short-term estimated cardiovascular disease risk. Among those with a low short-term predicted risk, more than half (54% [95% CI 52 to 56]) had a high lifetime predicted risk. Short-term and lifetime predicted risks were higher for participants with lower versus higher wealth indexes and educational levels and for those living in urban versus rural areas (P<0.01). These results were consistent by sex.
Conclusions
These findings highlight potential shortcomings of using short-term risk tools for primary prevention strategies because a substantial proportion of Peruvian adults were classified as low short-term risk but high lifetime risk. Vulnerable adults, such as those from low socioeconomic status and those living in urban areas, may need greater attention regarding cardiovascular preventive strategies.
Keywords: cardiovascular risk, lifetime cardiovascular risk, Pooled Cohort Risk Equations, risk estimation tools, short-term cardiovascular risk
Although the incidence of cardiovascular disease (CVD) has decreased in many high-income countries, the burden of CVD in low- and middle-income countries remains high.1,2 Intensive primary and secondary prevention efforts are important to reduce the burden of CVD in low- and middle-income countries because CVD has large economic and public health effects.3 In this context, the identification and treatment of persons with high risk of a cardiovascular event in the future are key components of CVD prevention.4 Many risk assessment tools have been developed to stratify asymptomatic persons, especially for short-term risk (eg, 10 years).5–8 Nonetheless, a large proportion of those who are considered to be at low risk for CVD in the short term may have clinical characteristics that place them at risk for a CVD event long term9 and thus may represent an important concern for public health planning.
Current guidelines recommend stratifying asymptomatic persons based on their short-term and lifetime predicted CVD risk.10,11 This approach to CVD risk stratification has been evaluated in China12 and India9 and in US South Asian participants13 but has been limited in Central and South America.14–16 Previous studies in populations from low- and middle-income countries used the ATP III risk assessment tool,9,17 which includes only coronary heart disease as an outcome.18 The clinical guidelines developed by the American Heart Association (AHA) and the American College of Cardiology (ACC) recommend the use of the atherosclerotic CVD Pooled Cohort Risk Equations, which predict risk for fatal and nonfatal ischemic heart disease and stroke events.19
The objective of this study is to estimate short-term and lifetime predicted CVD risk using baseline participant information from 2 population-based longitudinal studies in Peru and to compare short-term and lifetime CVD risk across socioeconomic status (SES), assessed by education, wealth index, and place of residence.
Methods
Study Participants
We identified eligible participants in 2 Peruvian longitudinal population-based studies: the CRONICAS cohort study (n=3619, baseline conducted in 2010–2011) and the PERU MIGRANT study (n=989, baseline conducted in 2007–2008). The CRONICAS cohort study aimed to assess the prevalence and incidence of cardiometabolic and pulmonary diseases among populations living in distinct urban or rural patterns in 3 Peruvian settings: Lima, Tumbes, and Puno. All participants were aged ≥35 years and were full-time residents of the area. The PERU MIGRANT study was designed to investigate the differences in CVD risk factors between rural-to-urban migrant and nonmigrant groups. This study was performed in participants aged ≥30 years from the rural site of Ayacucho or the urban site of Lima and rural-to-urban migrants from Ayacucho residing in Lima. In both studies, participants were sex and age stratified, single-stage random sampling was used, and only 1 participant per household was enrolled. Study design, fieldwork, and laboratory details of both studies have been described previously.20,21
We excluded participants with past history of ischemic heart disease, defined as self-reported diagnosis of myocardial infarction, unstable angina, or stable angina by the Rose angina questionnaire,22 and those with past history of stroke.
Risk Factor Definitions
Hypertension was defined as systolic blood pressure ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg, diagnosis by a physician, or use of antihypertensive medications. Dyslipidemia was defined as total cholesterol level ≥200 mg/dL or as low high-density lipoprotein cholesterol <50 mg/dL in women and <40 mg/dL in men.18 Diabetes was defined as fasting glucose ≥126 mg/dL or use of diabetes medication.23 Current tobacco use was self-reported and defined as having smoked at least 1 cigarette in the previous 30 days.
Short-Term and Lifetime Predicted Risk Stratification
Short-term predicted risk was defined as the 10-year calculated risk of having a first atherosclerotic CVD event, which consisted of a nonfatal myocardial infarction, a fatal or nonfatal stroke, or a coronary heart disease–related death. This was estimated for all participants using coefficients of the Pooled Cohort Risk Equations, defined in the 2013 ACC/AHA Guideline on the Assessment of Cardiovascular Risk, which included age, total cholesterol level, high-density lipoprotein cholesterol, systolic blood pressure, use of antihypertensive medication, current smoking status, and presence of diabetes mellitus for each sex.19 High short-term risk was defined as a 10-year predicted risk for an atherosclerotic CVD event of ≥7.5%, as recommended by 2013 ACC/AHA guidelines. Participants with low short-term predicted risk (<7.5%) were assigned to categories of lifetime risk based on risk-factor profiles using the existing algorithm developed from the Framingham Heart Study cohort.24 Low predicted lifetime risk was defined as having all optimal risk factors or ≥1 nonoptimal risk factor, whereas high lifetime predicted risk was defined as having ≥1 elevated or ≥1 major risk factor (Table 1). This definition is based on clinical relevance because those with at least 1 elevated risk factor have a calculated lifetime risk for CVD ≥39%.25 Participants were then classified, using these 2 risk assessment tools, into 3 groups: low short-term and low lifetime risk, low short-term and high lifetime risk, and high short-term predicted risk.18
Table 1.
Risk Factors Stratification and Predicted Lifetime Risks24
| CVD Risk Factors | Optimal | Nonoptimal | Elevated | Major |
|---|---|---|---|---|
| Blood pressure, mm Hg | <120/80 | 120 to 139/80 to 89 | 140 to 159/90 to 99 | ≥160/≥100 (or treated) |
| Total cholesterol, mg/dL | <180 | 180 to 199 | 200 to 239 | ≥240 (or treated) |
| Diabetes mellitus | No | No | No | Yes |
| Smoking | No | No | No | Yes |
CVD indicates cardiovascular disease.
Excluded Patients
Due to the specifications of Pooled Cohort Risk Equations, we included only participants in the age range of 40 to 79 years without past history of ischemic heart disease or stroke. Participants with missing values for age, systolic blood pressure, total cholesterol, high-density lipoprotein cholesterol, history of antihypertensive treatment, or current tobacco use were also excluded from the analysis.
Statistical Analysis
We used summary statistics to describe each predicted risk group by their demographic characteristics. The proportions of participants in each predicted risk group and the corresponding 95% CIs were estimated independently for men and women. The differences in proportion of participants within each predicted risk group were compared across age range, level of education (highest level reached), possessions weighted asset index (in tertiles), and place of residence (urban or rural).
Multiple parameters could be used to assess SES, including educational status and wealth index based on asset possessions.26 All sites included in the CRONICAS and PERU MIGRANT studies were located in low-SES areas; however, levels of poverty varied across and within sites, allowing for individual participants to be properly grouped in context by wealth index and educational attainment.
To compare the distribution of CVD risk strata across level of education and wealth index, as measures of SES, and by place of residence, we used logistic regression—separately for each CVD risk stratum—adjusted by each variable (highest educational level, wealth index tertiles, or location, respectively) and by age. Binary outcomes were presence or absence of each CVD risk stratum. We used Stata version 12 (StataCorp LP) for all analyses.
This study was approved by the institutional review committee at Universidad Peruana Cayetano Heredia. All study participants gave informed consent.
Results
Overall, 4608 individuals were enrolled in both baseline surveys of the CRONICAS cohort study and the PERU MIGRANT study. Of the total 4608 participants in the 2 cohorts, 788 were excluded due to age, 526 due to past history of ischemic heart disease or stroke, and 389 due to missing data. Data from 61 subjects who were participants in both studies were included in this pooled cohort only once to avoid duplicate information. A total of 2844 participants were included in the analysis. Participants had a mean age of 55.9 years (SD 10.2 years), and 50% were men (Table 2).
Table 2.
Characteristics of the Pooled Population From the CRONICAS cohort study and PERU MIGRANT study (n=2844)
| Variables | Low Short-Term/Low Lifetime Risk (n*=858, 353, 505) | Low Short-Term/High Lifetime Risk (n*=1007, 356, 651) | High Short-Term Risk (n*=979, 713, 266) |
|---|---|---|---|
| Age, y, mean (SD) | 50.9 (7.7) | 51.0 (6.9) | 65.3 (8.4) |
| Men | 49.6 (6.3) | 47.2 (5.0) | 63.4 (8.5) |
| Women | 51.8 (8.4) | 53.0 (6.9) | 70.3 (5.6) |
| SBP, mm Hg, mean (SD) | 109.7 (11.7) | 116.8 (16.6) | 130.1 (20.6) |
| Men | 114.4 (10.0) | 120.9 (15.1) | 128.8 (19.5) |
| Women | 106.5 (11.7) | 114.5 (16.9) | 133.6 (22.9) |
| DBP, mm Hg, mean (SD) | 69.6 (8.0) | 73.9 (10.8) | 77.2 (12.0) |
| Men | 71.7 (7.7) | 76.7 (10.2) | 77.8 (11.7) |
| Women | 68.1 (8.0) | 72.4 (10.8) | 75.7 (12.4) |
| BMI, kg/m2, mean (SD) | 26.4 (4.4) | 28.9 (4.9) | 27.2 (4.4) |
| Men | 25.5 (3.5) | 27.3 (3.8) | 27.1 (4.1) |
| Women | 27.1 (4.8) | 29.7 (5.3) | 27.6 (4.9) |
| Waist circumference, cm, mean (SD) | 87.2 (11.2) | 93.1 (10.9) | 93.0 (11.1) |
| Men | 88.6 (9.7) | 93.1 (9.4) | 94.0 (10.5) |
| Women | 86.3 (12.0) | 93.1 (11.6) | 90.5 (12.2) |
| Total cholesterol, mg/dL, mean (SD) | 169.1 (22.5) | 220.9 (35.6) | 202.9 (41.0) |
| Men | 166.3 (23.0) | 210.6 (34.7) | 201.2 (40.6) |
| Women | 171.0 (21.9) | 226.4 (34.8) | 207.5 (41.7) |
| HDL-C, mg/dL, mean (SD) | 41.5 (11.2) | 43.5 (11.6) | 40.5 (11.2) |
| Men | 40.3 (11.1) | 42.5 (11.9) | 39.5 (10.5) |
| Women | 42.4 (11.2) | 44.1 (11.5) | 43.2 (12.4) |
| Triglycerides, mg/dL, mean (SD) | 131.5 (71.2) | 178.9 (104.1) | 173.3 (111.1) |
| Men | 134.7 (84.1) | 175.9 (110.6) | 171.8 (107.5) |
| Women | 129.3 (60.7) | 180.6 (100.4) | 177.5 (120.4) |
| Total cholesterol/HDL, mean (SD) | 4.1 (1.1) | 5.0 (1.4) | 5.0 (1.6) |
| Men | 4.0 (1.1) | 4.7 (1.5) | 5.1 (1.5) |
| Women | 4.1 (1.1) | 5.1 (1.4) | 4.7 (2.2) |
| Current tobacco use, n (%) | 0 (0.0) | 123 (12.2) | 163 (16.7) |
| Men | 0 (0.0) | 88 (24.7) | 151 (21.2) |
| Women | 0 (0.0) | 35 (5.4) | 12 (4.5) |
| Diabetes, n (%) | 0 (0.0) | 84 (8.3) | 136 (13.9) |
| Men | 0 (0.0) | 13 (3.7) | 88 (12.3) |
| Women | 0 (0.0) | 71 (10.9) | 48 (18.1) |
| Hypertension, n (%) | 0 (0.0) | 233 (19.9) | 309 (37.9) |
| Men | 0 (0.0) | 96 (18.9) | 179 (31.9) |
| Women | 0 (0.0) | 137 (20.7) | 130 (51.2) |
| Dyslipidemia, n (%) | 576 (67.1) | 924 (91.8) | 814 (83.2) |
| Men | 185 (52.4) | 297 (83.4) | 574 (80.5) |
| Women | 391 (77.4) | 627 (96.3) | 240 (90.2) |
| Antihypertensive therapy, n (%) | 0 (0.0) | 77 (7.7) | 164 (16.8) |
| Men | 0 (0.0) | 7 (2.0) | 72 (10.1) |
| Women | 0 (0.0) | 70 (10.8) | 92 (34.6) |
| Pooled Cohort Risk Equations, % (mean, SD) | 2.4 (1.9) | 3.4 (1.9) | 17.0 (9.7) |
| Men | 3.3 (2.0) | 4.3 (1.8) | 17.6 (10.1) |
| Women | 1.8 (1.6) | 2.9 (1.8) | 15.5 (8.1) |
Dyslipidemia: TC ≥200 mg/dL or HDL-C <50 mg/dL (women), HDL-C <40 mg/dL (men). Hypertension: SBP ≥140 mm Hg, or DBP ≥90 mm Hg, or diagnosed by physician or taking antihypertensive medications. Diabetes: fasting glucose ≥126 mg/dL or taking diabetes medication. BMI indicates body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; HDL-C, high-density lipoprotein cholesterol.
n for total, men, and women.
In the aggregate population, the prevalence of participants classified as high short-term risk was 34.4% (95% CI 32.7 to 36.2), with a prevalence of 50.1% (95% CI 47.5 to 52.8) in men and 18.7% (95% CI 16.7 to 20.8) in women (Figure). Among participants classified as low short-term risk, 54.0% (95% CI 51.7 to 56.3) were in the high lifetime CVD risk category. Most CVD risk factors were most prevalent in the high short-term predicted risk group, although dyslipidemia was most prevalent in the low short-term and high lifetime risk group (92%).
Figure 1.
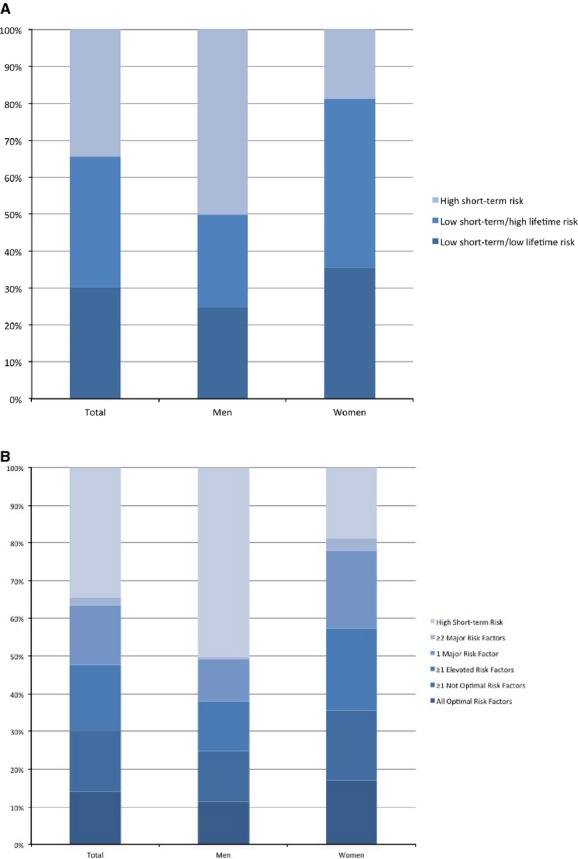
Distribution of risk in CRONICAS and PERU MIGRANT studies. A, Short-term and lifetime risk. B, Risk strata. For both panels, distribution was significantly different by sex (P<0.001).
Only 23.1% (95% CI 20.5 to 25.9) and 1.2% (95% CI 0.3 to 3.0) of participants in the youngest (40 to 49 years) and oldest (70 to 79 years) age groups, respectively, had all optimal risk factors. Prevalence of the optimal risk profile was significantly higher among participants with the lowest (14.9%) compared with the highest educational level (12.9%). Prevalence was similarly higher among those in the lowest (17.3%) compared with highest (12.1%) wealth index tertile and among rural (24.2%) compared with urban counterparts (12.0%) (P<0.01).
With regard to participants with low short-term and high lifetime predicted risk, 25.1% (95% CI 22.4 to 28.0) and 2.7% (95% CI 1.8 to 4.0) in the youngest age subgroup had ≥1 elevated and ≥2 major risk factors, respectively, whereas none of the participants in the oldest age subgroup had these risk profiles. Participants within the lowest wealth index and from rural areas had significantly lower prevalence of these risk profiles compared with the highest wealth index and urban counterparts, respectively (P<0.01).
In contrast, almost all participants in the oldest age group (96.5% [95% CI 96.2 to 99.3]) were classified as high short-term risk. This risk profile was found to be significantly higher in the lowest (40.9%) versus the highest (30.5%) educational groups, in the lowest (37.2%) versus the highest (34.9%) wealth index tertiles, and among urban (35.3%) versus rural (30.4%) participants (P<0.01) (Table 3). Results were generally consistent by sex (Table 4).
Table 3.
Distribution of Combined 10-Year (Short-Term) and Lifetime Cardiovascular Risk in the Pooled Population
| Variables | Low Short-Term/Low Lifetime Risk | Low Short-Term/High Lifetime Risk | High Short-Term Risk | N=2844 | |||
|---|---|---|---|---|---|---|---|
| All Optimal | ≥1 Not Optimal | ≥1 Elevated | 1 Major | ≥2 Major | P Value | ||
| Total, n (%) | 403 (14.2) | 455 (16.0) | 500 (17.6) | 447 (15.7) | 60 (2.1) | 979 (34.4) | |
| Age, n (%) | |||||||
| 40 to 49 | 219 (23.1) | 204 (21.5) | 238 (25.1) | 217 (22.9) | 26 (2.7) | 44 (4.6) | |
| 50 to 59 | 119 (12.5) | 201 (21.0) | 200 (20.9) | 180 (18.8) | 30 (3.1) | 226 (23.6) | |
| 60 to 69 | 61 (10.1) | 48 (8.0) | 62 (10.3) | 50 (8.3) | 4 (0.7) | 378 (62.7) | |
| 70 to 79 | 4 (1.2) | 2 (0.6) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 331 (98.2) | |
| Location, n (%) | |||||||
| Urban | 278 (12.0) | 344 (14.8) | 430 (18.5) | 395 (17.0) | 58 (2.5) | 822 (35.3) | <0.01*,†,‡ |
| Rural | 125 (24.2) | 111 (21.5) | 70 (13.5) | 52 (10.1) | 2 (0.4) | 157 (30.4) | |
| Highest educational level, n (%) | |||||||
| Primary school or less | 206 (14.9) | 207 (15.0) | 206 (14.9) | 170 (12.3) | 29 (2.1) | 565 (40.9) | <0.01*,‡ |
| Secondary school | 135 (13.8) | 172 (17.5) | 204 (20.8) | 182 (18.5) | 21 (2.1) | 268 (27.3) | |
| Superior level | 62 (12.9) | 76 (15.9) | 90 (18.8) | 95 (19.8) | 10 (2.1) | 146 (30.5) | |
| Wealth index, n (%) | |||||||
| Lowest | 154 (17.3) | 150 (16.9) | 139 (15.6) | 106 (11.9) | 9 (1.0) | 331 (37.2) | <0.01*,‡,§,¶,** |
| Middle | 130 (13.4) | 171 (17.6) | 187 (19.3) | 155 (16.0) | 23 (2.4) | 305 (31.4) | |
| Highest | 119 (12.1) | 134 (13.6) | 174 (17.7) | 186 (18.9) | 28 (2.9) | 343 (34.9) | |
P values are for the comparison between row variables (highest level of education, wealth index tertiles, or location) and cardiovascular disease risk strata, separately, and adjusted by age.
All optimal risk factors.
≥1 elevated risk factor.
High short-term risk.
≥1 nonoptimal risk factor.
1 major risk factor.
≥2 major risk factors.
Table 4.
Distribution of Combined 10-Year (Short-Term) and Lifetime Cardiovascular Risk in the Pooled Population by Sex
| Variables | Low Short-Term/Low Lifetime Risk | Low Short-Term/High Lifetime Risk | High Short-Term Risk | N=2844 | |||
|---|---|---|---|---|---|---|---|
| All Optimal | ≥1 Not Optimal | ≥1 Elevated | 1 Major | ≥2 Major | P Value | ||
| Total, n (%) | 403 (14.2) | 455 (16.0) | 500 (17.6) | 447 (15.7) | 60 (2.1) | 979 (34.4) | |
| Age range, men, n (%) | |||||||
| 40 to 49 | 89 (18.7) | 95 (19.9) | 113 (23.7) | 127 (26.6) | 9 (1.9) | 44 (9.2) | |
| 50 to 59 | 57 (12.3) | 93 (20.0) | 72 (15.5) | 30 (6.5) | 2 (0.4) | 211 (45.4) | |
| 60 to 69 | 15 (4.9) | 4 (1.3) | 3 (1.0) | 0 (0.0) | 0 (0.0) | 282 (92.8) | |
| 70 to 79 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 176 (100.0) | |
| Age range, women, n (%) | |||||||
| 40 to 49 | 130 (27.6) | 109 (23.1) | 125 (26.5) | 90 (19.1) | 17 (3.6) | 0 (0.0) | |
| 50 to 59 | 62 (12.6) | 108 (22.0) | 128 (26.1) | 150 (30.6) | 28 (5.7) | 15 (3.1) | |
| 60 to 69 | 46 (15.4) | 44 (14.7) | 59 (19.7) | 50 (16.7) | 4 (1.3) | 96 (32.1) | |
| 70 to 79 | 4 (2.5) | 2 (1.2) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 155 (96.3) | |
| Location, men, n (%) | |||||||
| Urban | 115 (9.8) | 145 (12.4) | 158 (13.5) | 137 (11.7) | 11 (0.9) | 604 (51.6) | <0.01*,†,‡ |
| Rural | 46 (18.3) | 47 (18.7) | 30 (11.9) | 20 (7.9) | 0 (0.0) | 109 (43.3) | |
| Location, women, n (%) | |||||||
| Urban | 163 (14.1) | 199 (17.2) | 272 (23.5) | 258 (22.3) | 47 (4.1) | 218 (18.8) | <0.01*,†,§,¶,** |
| Rural | 79 (29.8) | 64 (24.2) | 40 (15.1) | 32 (12.1) | 2 (0.8) | 48 (18.1) | |
| Highest level of education, men, n (%) | |||||||
| Primary school or less | 54 (10.3) | 56 (10.7) | 42 (8.0) | 31 (5.9) | 4 (0.8) | 339 (64.5) | >0.01 |
| Secondary school | 76 (12.7) | 93 (15.5) | 101 (16.8) | 87 (14.5) | 5 (0.8) | 239 (39.8) | |
| Superior level | 31 (10.5) | 43 (14.6) | 45 (15.3) | 39 (13.2) | 2 (0.7) | 135 (45.8) | |
| Highest level of education, women, n (%) | |||||||
| Primary school or less | 152 (17.7) | 151 (17.6) | 164 (19.1) | 139 (16.2) | 25 (2.9) | 226 (26.4) | <0.01*,¶ |
| Secondary school | 59 (15.5) | 79 (20.7) | 103 (27.0) | 95 (24.9) | 16 (4.2) | 29 (7.6) | |
| Superior level | 31 (16.9) | 33 (17.9) | 45 (24.5) | 56 (30.4) | 8 (4.4) | 11 (6.0) | |
| Wealth index, men, n (%) | |||||||
| Lowest | 44 (11.43) | 49 (12.73) | 44 (11.4) | 40 (10.4) | 1 (0.3) | 207 (53.8) | <0.01‡ |
| Middle | 65 (13.1) | 72 (14.5) | 78 (15.7) | 54 (10.9) | 5 (1.0) | 222 (44.8) | |
| Highest | 52 (9.6) | 71 (13.1) | 66 (12.2) | 63 (11.7) | 5 (0.9) | 284 (52.5) | |
| Wealth index, women, n (%) | |||||||
| Lowest | 110 (21.8) | 101 (20.0) | 95 (18.9) | 66 (13.1) | 8 (1.6) | 124 (24.6) | <0.01*,†,‡,¶,** |
| Middle | 65 (13.7) | 99 (20.8) | 109 (23.0) | 101 (21.3) | 18 (3.8) | 83 (17.5) | |
| Highest | 67 (15.1) | 63 (14.2) | 108 (24.4) | 123 (27.8) | 23 (5.2) | 59 (13.3) | |
P values are for the comparison between row variables (highest level of education, wealth index tertiles, or location) and cardiovascular disease risk strata, adjusted by age.
All optimal risk factors.
≥1 not optimal risk factors.
≥1 elevated risk factor.
1 major risk factor.
≥2 major risk factors.
high short-term risk.
Discussion
We found a relatively high proportion of participants classified as high short-term and high lifetime risk in a Peruvian population-based sample. A major finding of our study suggests that short-term and lifetime risks are not necessarily interdependent; specifically, the latter can be high even if the former is low. The chief implication of this finding is that approaches to prevention need to be global and target specific.
More than one-third of participants in our study were classified as high short-term CVD risk; more than half of those participants classified as low short-term predicted CVD risk, who would not likely be candidates for pharmacotherapy based on current guidelines, were classified as high lifetime CVD risk. Moreover, a higher proportion of participants were classified as high short-term and lifetime risk in low SES and urban settings, compared with high SES and rural settings, respectively. These overall findings are consistent with results from India and the United States.9,27 In addition, a relatively small proportion of participants had all optimal risk factors (12.7%), which are far from optimal for population CVD prevention efforts. In fact, only 23.1% had this optimal risk profile in our youngest age subgroup (40 to 49 years). These findings suggest potential to identify targets for future public health intervention because maintaining a healthy lifestyle throughout young adulthood has been shown to be associated with a low CVD risk profile in middle age.28
Distribution of Risk by Socioeconomic Status: Education and Wealth Index
We found that levels of education and wealth index had inverse relationships to short-term risk but direct relationships to lifetime risk. A study in India found a similar association between educational level and short-term risk.9 The relationship between SES and CVD incidence and risk factors has been well established,29–34 and it is recognized that wealthy, educated, and urban people are most affected. Several risk factors, however, such as unhealthy food and tobacco use have become more available for mass consumption, leading to a transition in which all social classes are affected. Based on our findings, we may hypothesize that in Peru, this transition may have started by having a greater initial impact on short-term rather than lifetime risk.
Although CVD-related mortality has declined steadily over past decades, socioeconomic disparities have not. Similar to developed countries, developing countries had CVD risk factors more frequently in persons with high socioeconomic status in the past.35 With social and economic development and ongoing epidemiological transition in these countries, these risk factors have become more prevalent among persons with lower SES.35 Our findings suggest that in Central and South America, there is a need to direct CVD prevention efforts to communities and persons with low SES.
Distribution of Risk by Place of Residence
We found a higher proportion of participants classified as high short-term risk among urban versus rural counterparts and a lower proportion of participants with all optimal risk factors. Similar results were found in other low- and middle-income countries.9,36,37 Using the INTERHEART risk score, Yusuf et al found that in low- and middle-income countries, the predicted cardiovascular risk was higher in urban areas.38 Similar to demographic trends throughout Central and South America, the Peruvian urban population has increased from 12.2 million to 23.2 million between 1983 and 201239,40 and is predicted to increase.41 Consequently, an increasing proportion of the population will likely face increased CVD risk.
Clinical Implications
The cutoff point for high short-term risk definition has been lowered from 10% (ATP III) to 7.5% (Pooled Cohort Risk Equations),19 thereby increasing the proportion of persons with predicted high short-term risk. Despite this decrease in the number of persons classified as low short-term risk, a great proportion among them are at high lifetime risk. Exposure to high levels of risk factors over a lifetime promotes the development and progression of atherosclerosis.42 Those with low short-term but high lifetime predicted risk have been found to have greater subclinical disease compared with those with low short-term and lifetime risk.25 This suggests a potential benefit from aggressive prevention efforts in patients with this risk profile; however, this approach has yet to be rigorously tested.
Therapeutic strategies based on lifetime risk can be troublesome because of the uncertainty of safety and efficacy of use of statins for ≥10 years and the lack of data on long-term follow-up of randomized clinical trials >15 years or treatment of persons aged <40 years.10 Nonetheless, reliance on only short-term risk estimates, as recommended by previous ATP III guidelines, may be limited because any single risk factor can produce significant cumulative damage if left untreated for many years. Consequently, lifetime risk assessment is particularly relevant for young patients, in whom attention to only short-term risk—very often found to be low—may discourage initiation of or adherence to lifestyle modification and treatment.24
Strengths and Limitations
This study uses diverse geographical settings at both low and high altitudes. In addition, this report may well be one of the earliest in Central and South American populations to use the recently published Pooled Cohort Risk Equations and one of the first to combine evaluations of short-term and predicted lifetime CVD risk in the region. Similar to the lifetime risk estimation tool, the Pooled Cohort Risk Equations assess total CVD as an outcome, which has been demonstrated to be more clinically relevant than only coronary heart disease events.43 In addition, the lifetime risk algorithm used in this study yields a better remaining lifetime risk for CVD in comparison to Kaplan–Meier cumulative incidence.24
This study also has important limitations. Scarce evidence exists to support the validity of cardiovascular prediction tools in Central and South America.16 In fact, Pooled Cohort Risk Equations have been shown to overestimate risk in non-US populations.44 Neither short-term nor lifetime risk algorithms have been validated or calibrated for Peruvian populations. Moreover, risk assessment tools are thought to overestimate risk in Central and South American populations,16 and there are not yet Peruvian, or general Central and South American, cohort studies with 10 years of follow-up to validate and recalibrate risk assessment tools.
Conclusions
In 2 Peruvian populations, about 1 in 3 persons has a high estimated risk of developing an atherosclerotic CVD event in the next 10 years. Among the low short-term risk group, which would not otherwise be considered for pharmacological therapy, a substantial proportion of participants were classified as high lifetime predicted CVD risk, suggesting that the profiles of short-term and lifetime risks are not necessarily interdependent. The chief implication of this finding is that approaches to prevention need to be global and target specific. Vulnerable persons, particularly those from low-SES and urban areas, are more likely to be classified as high short-term CVD risk. These findings demonstrate the need for comprehensive strategies for CVD prevention in Central and South America that target low-income communities.
Disclosures
Dr Huffman has research grants from World Heart Federation, via unrestricted educational grant from AstraZeneca. Other authors report no relationships that could be construed as a conflict of interest.
Appendix
CRONICAS Cohort Study Group
Cardiovascular Disease: Antonio Bernabé-Ortiz, Juan P. Casas, George Davey Smith, Shah Ebrahim, Héctor H. García, Robert H. Gilman, Luis Huicho, Germán Málaga, J. Jaime Miranda, Víctor M. Montori, Liam Smeeth; Chronic Obstructive Pulmonary Disease: William Checkley, Gregory B. Diette, Robert H. Gilman, Luis Huicho, Fabiola León-Velarde, María Rivera, Robert A. Wise; Training and Capacity Building: William Checkley, Héctor H. García, Robert H. Gilman, J. Jaime Miranda, Katherine Sacksteder.
PERU MIGRANT Study Investigators
Antonio Bernabé-Ortiz, Lilia Cabrera, Héctor H. García, Robert H. Gilman, J. Jaime Miranda, Julio A. Poterico, Renato Quispe, Candice Romero, Juan F. Sánchez, Liam Smeeth.
References
- Yusuf S, McKee M. Documenting the global burden of cardiovascular disease: a major achievement but still a work in progress. Circulation. 2014;129:1459–1462. doi: 10.1161/CIRCULATIONAHA.114.008302. [DOI] [PubMed] [Google Scholar]
- GBD 2013 Mortality and Causes of Death Collaborators; Causes of Death C. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385:117–171. doi: 10.1016/S0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim SS, Gaziano TA, Gakidou E, Reddy KS, Farzadfar F, Lozano R, Rodgers A. Prevention of cardiovascular disease in high-risk individuals in low-income and middle-income countries: health effects and costs. Lancet. 2007;370:2054–2062. doi: 10.1016/S0140-6736(07)61699-7. [DOI] [PubMed] [Google Scholar]
- Dalton AR, Bull RJ. Risk stratification could reduce costs in primary prevention of cardiovascular disease. BMJ. 2011;343:d4913. doi: 10.1136/bmj.d4913. [DOI] [PubMed] [Google Scholar]
- Conroy RM, Pyorala K, Fitzgerald AP, Sans S, Menotti A, De Backer G, De Bacquer D, Ducimetiere P, Jousilahti P, Keil U, Njolstad I, Oganov RG, Thomsen T, Tunstall-Pedoe H, Tverdal A, Wedel H, Whincup P, Wilhelmsen L, Graham IM Group Sp. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J. 2003;24:987–1003. doi: 10.1016/s0195-668x(03)00114-3. [DOI] [PubMed] [Google Scholar]
- Woodward M, Brindle P, Tunstall-Pedoe H Estimation Sgor. Adding social deprivation and family history to cardiovascular risk assessment: the ASSIGN score from the Scottish Heart Health Extended Cohort (SHHEC) Heart. 2007;93:172–176. doi: 10.1136/hrt.2006.108167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridker PM, Buring JE, Rifai N, Cook NR. Development and validation of improved algorithms for the assessment of global cardiovascular risk in women: the Reynolds Risk Score. JAMA. 2007;297:611–619. doi: 10.1001/jama.297.6.611. [DOI] [PubMed] [Google Scholar]
- Ridker PM, Paynter NP, Rifai N, Gaziano JM, Cook NR. C-reactive protein and parental history improve global cardiovascular risk prediction: the Reynolds Risk Score for men. Circulation. 2008;118:2243–2251. doi: 10.1161/CIRCULATIONAHA.108.814251. , 4p following 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeemon P, Prabhakaran D, Huffman MD, Ramakrishnan L, Goenka S, Thankappan KR, Mohan V, Joshi PP, Mohan BV, Ahmed F, Ramanathan M, Ahuja R, Chaturvedi V, Lloyd-Jones DM, Reddy KS Sentinel Surveillance in Industrial Populations Study G. Distribution of 10-year and lifetime predicted risk for cardiovascular disease in the Indian Sentinel Surveillance Study population (cross-sectional survey results) BMJ Open. 2011;1:e000068. doi: 10.1136/bmjopen-2011-000068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone NJ, Robinson J, Lichtenstein AH, Merz CN, Blum CB, Eckel RH, Goldberg AC, Gordon D, Levy D, Lloyd-Jones DM, McBride P, Schwartz JS, Shero ST, Smith SC, Jr, Watson K, Wilson PW. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 suppl 2):S1–S45. doi: 10.1161/01.cir.0000437738.63853.7a. [DOI] [PubMed] [Google Scholar]
- Board JBS. Joint British Societies’ consensus recommendations for the prevention of cardiovascular disease (JBS3) Heart. 2014;100(suppl 2):ii1–ii67. doi: 10.1136/heartjnl-2014-305693. [DOI] [PubMed] [Google Scholar]
- Wang Y, Liu J, Wang W, Wang M, Qi Y, Xie W, Li Y, Sun J, Liu J, Zhao D. Lifetime risk for cardiovascular disease in a Chinese population: the Chinese Multi-Provincial Cohort Study. Eur J Prev Cardiol. 2015;22:380–388. doi: 10.1177/2047487313516563. [DOI] [PubMed] [Google Scholar]
- Kandula NR, Kanaya AM, Liu K, Lee JY, Herrington D, Hulley SB, Persell SD, Lloyd-Jones DM, Huffman MD. Association of 10-year and lifetime predicted cardiovascular disease risk with subclinical atherosclerosis in South Asians: findings from the Mediators of Atherosclerosis in South Asians Living in America (MASALA) study. J Am Heart Assoc. 2014;3:e001117. doi: 10.1161/JAHA.114.001117. doi: 10.1161/JAHA.114.001117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz M, Laurinavicius AG, Franco FG, Conceicao RD, Carvalho JA, Pesaro AE, Wajngarten M, Santos RD. Calculated and perceived cardiovascular risk in asymptomatic subjects submitted to a routine medical evaluation: the perception gap*. Eur J Prev Cardiol. 2014 doi: 10.1177/2047487314543074. ; [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- Simao AF, Precoma DB, Andrade JP, Correa Filho H, Saraiva JF, Oliveira GM Brazilian Society of C. I cardiovascular prevention guideline of the Brazilian Society of Cardiology—executive summary. Arq Bras Cardiol. 2014;102:420–431. doi: 10.5935/abc.20140067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cortes-Bergoderi M, Thomas RJ, Albuquerque FN, Batsis JA, Burdiat G, Perez-Terzic C, Trejo-Gutierrez J, Lopez-Jimenez F. Validity of cardiovascular risk prediction models in Latin America and among Hispanics in the United States of America: a systematic review. Rev Panam Salud Publica. 2012;32:131–139. doi: 10.1590/s1020-49892012000800007. [DOI] [PubMed] [Google Scholar]
- Schargrodsky H, Hernandez-Hernandez R, Champagne BM, Silva H, Vinueza R, Silva Aycaguer LC, Touboul PJ, Boissonnet CP, Escobedo J, Pellegrini F, Macchia A, Wilson E Investigators CS. CARMELA: assessment of cardiovascular risk in seven Latin American cities. Am J Med. 2008;121:58–65. doi: 10.1016/j.amjmed.2007.08.038. [DOI] [PubMed] [Google Scholar]
- National Cholesterol Education Program Expert Panel on Detection E, Treatment of High Blood Cholesterol in A. Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- Goff DC, Jr, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB, Sr, Gibbons R, Greenland P, Lackland DT, Levy D, O’Donnell CJ, Robinson J, Schwartz JS, Shero ST, Smith SC, Jr, Sorlie P, Stone NJ, Wilson PW. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 suppl 2):S49–S73. doi: 10.1161/01.cir.0000437741.48606.98. [DOI] [PubMed] [Google Scholar]
- Miranda JJ, Gilman RH, Garcia HH, Smeeth L. The effect on cardiovascular risk factors of migration from rural to urban areas in Peru: PERU MIGRANT Study. BMC Cardiovasc Disord. 2009;9:23. doi: 10.1186/1471-2261-9-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda JJ, Bernabe-Ortiz A, Smeeth L, Gilman RH, Checkley W Group CCS. Addressing geographical variation in the progression of non-communicable diseases in Peru: the CRONICAS cohort study protocol. BMJ Open. 2012;2:e000610. doi: 10.1136/bmjopen-2011-000610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cosin J, Asin E, Marrugat J, Elosua R, Aros F, de los Reyes M, Castro-Beiras A, Cabades A, Diago JL, Lopez-Bescos L, Vila J. Prevalence of angina pectoris in Spain. PANES Study group. Eur J Epidemiol. 1999;15:323–330. doi: 10.1023/a:1007542700074. [DOI] [PubMed] [Google Scholar]
- Guariguata L, Whiting D, Weil C, Unwin N. The International Diabetes Federation diabetes atlas methodology for estimating global and national prevalence of diabetes in adults. Diabetes Res Clin Pract. 2011;94:322–332. doi: 10.1016/j.diabres.2011.10.040. [DOI] [PubMed] [Google Scholar]
- Lloyd-Jones DM, Leip EP, Larson MG, D’Agostino RB, Beiser A, Wilson PW, Wolf PA, Levy D. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation. 2006;113:791–798. doi: 10.1161/CIRCULATIONAHA.105.548206. [DOI] [PubMed] [Google Scholar]
- Berry JD, Liu K, Folsom AR, Lewis CE, Carr JJ, Polak JF, Shea S, Sidney S, O’Leary DH, Chan C, Lloyd-Jones DM. Prevalence and progression of subclinical atherosclerosis in younger adults with low short-term but high lifetime estimated risk for cardiovascular disease: the coronary artery risk development in young adults study and Multi-Ethnic Study of Atherosclerosis. Circulation. 2009;119:382–389. doi: 10.1161/CIRCULATIONAHA.108.800235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan GA, Keil JE. Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation. 1993;88(4 Pt 1):1973–1998. doi: 10.1161/01.cir.88.4.1973. [DOI] [PubMed] [Google Scholar]
- Marma AK, Berry JD, Ning H, Persell SD, Lloyd-Jones DM. Distribution of 10-year and lifetime predicted risks for cardiovascular disease in US adults: findings from the National Health and Nutrition Examination Survey 2003 to 2006. Circ Cardiovasc Qual Outcomes. 2010;3:8–14. doi: 10.1161/CIRCOUTCOMES.109.869727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu K, Daviglus ML, Loria CM, Colangelo LA, Spring B, Moller AC, Lloyd-Jones DM. Healthy lifestyle through young adulthood and the presence of low cardiovascular disease risk profile in middle age: the Coronary Artery Risk Development in (Young) Adults (CARDIA) study. Circulation. 2012;125:996–1004. doi: 10.1161/CIRCULATIONAHA.111.060681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang CL, Marmot MG, Farley TM, Poulter NR. The influence of economic development on the association between education and the risk of acute myocardial infarction and stroke. J Clin Epidemiol. 2002;55:741–747. doi: 10.1016/s0895-4356(02)00413-4. [DOI] [PubMed] [Google Scholar]
- Dray-Spira R, Gary TL, Brancati FL. Socioeconomic position and cardiovascular disease in adults with and without diabetes: United States trends, 1997–2005. J Gen Intern Med. 2008;23:1634–1641. doi: 10.1007/s11606-008-0727-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta R, Gupta VP, Ahluwalia NS. Educational status, coronary heart disease, and coronary risk factor prevalence in a rural population of India. BMJ. 1994;309:1332–1336. doi: 10.1136/bmj.309.6965.1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ribeiro S, Furtado C, Pereira J. Association between cardiovascular disease and socioeconomic level in Portugal. Rev Port Cardiol. 2013;32:847–854. doi: 10.1016/j.repc.2013.01.008. [DOI] [PubMed] [Google Scholar]
- Siren R, Eriksson JG, Peltonen M, Vanhanen H. Impact of health counselling on cardiovascular disease risk in middle aged men: influence of socioeconomic status. PLoS One. 2014;9:e88959. doi: 10.1371/journal.pone.0088959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deans KA, Bezlyak V, Ford I, Batty GD, Burns H, Cavanagh J, de Groot E, McGinty A, Millar K, Shiels PG, Tannahill C, Velupillai YN, Sattar N, Packard CJ. Differences in atherosclerosis according to area level socioeconomic deprivation: cross sectional, population based study. BMJ. 2009;339:b4170. doi: 10.1136/bmj.b4170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yusuf S, Reddy S, Ounpuu S, Anand S. Global burden of cardiovascular diseases: part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation. 2001;104:2746–2753. doi: 10.1161/hc4601.099487. [DOI] [PubMed] [Google Scholar]
- Riha J, Karabarinde A, Ssenyomo G, Allender S, Asiki G, Kamali A, Young EH, Sandhu MS, Seeley J. Urbanicity and lifestyle risk factors for cardiometabolic diseases in rural Uganda: a cross-sectional study. PLoS Med. 2014;11:e1001683. doi: 10.1371/journal.pmed.1001683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allender S, Lacey B, Webster P, Rayner M, Deepa M, Scarborough P, Arambepola C, Datta M, Mohan V. Level of urbanization and noncommunicable disease risk factors in Tamil Nadu, India. Bull World Health Organ. 2010;88:297–304. doi: 10.2471/BLT.09.065847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yusuf S, Rangarajan S, Teo K, Islam S, Li W, Liu L, Bo J, Lou Q, Lu F, Liu T, Yu L, Zhang S, Mony P, Swaminathan S, Mohan V, Gupta R, Kumar R, Vijayakumar K, Lear S, Anand S, Wielgosz A, Diaz R, Avezum A, Lopez-Jaramillo P, Lanas F, Yusoff K, Ismail N, Iqbal R, Rahman O, Rosengren A, Yusufali A, Kelishadi R, Kruger A, Puoane T, Szuba A, Chifamba J, Oguz A, McQueen M, McKee M, Dagenais G, Investigators P. Cardiovascular risk and events in 17 low-, middle-, and high-income countries. N Engl J Med. 2014;371:818–827. doi: 10.1056/NEJMoa1311890. [DOI] [PubMed] [Google Scholar]
- The World Bank. Peru: Urban Population. Available at: http://data.worldbank.org/indicator/SP.URB.TOTL.IN.ZS?page=4. Accessed January 21, 2015.
- World Health Organization. Peru: urban health profile. Available at: http://www.who.int/kobe_centre/measuring/urbanheart/peru.pdf. Accessed January 21, 2015.
- U.S. Department of Commerce. Economics and Statistics Administration. Peru: International Brief, Population Trends; 1999. Available at: https://www.census.gov/population/international/files/ib99-1.pdf. Accessed January 21, 2015. [Google Scholar]
- Loria CM, Liu K, Lewis CE, Hulley SB, Sidney S, Schreiner PJ, Williams OD, Bild DE, Detrano R. Early adult risk factor levels and subsequent coronary artery calcification: the CARDIA Study. J Am Coll Cardiol. 2007;49:2013–2020. doi: 10.1016/j.jacc.2007.03.009. [DOI] [PubMed] [Google Scholar]
- Lackland DT, Elkind MS, D’Agostino R, Sr, Dhamoon MS, Goff DC, Jr, Higashida RT, McClure LA, Mitchell PH, Sacco RL, Sila CA, Smith SC, Jr, Tanne D, Tirschwell DL, Touze E, Wechsler LR American Heart Association Stroke C, Council on E, Prevention, Council on Cardiovascular R, Intervention, Council on Cardiovascular N, Council on Peripheral Vascular D, Council on Quality of C, Outcomes R. Inclusion of stroke in cardiovascular risk prediction instruments: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2012;43:1998–2027. doi: 10.1161/STR.0b013e31825bcdac. [DOI] [PubMed] [Google Scholar]
- Chia YC, Lim HM, Ching SM. Validation of the pooled cohort risk score in an Asian population—a retrospective cohort study. BMC Cardiovasc Disord. 2014;14:163. doi: 10.1186/1471-2261-14-163. [DOI] [PMC free article] [PubMed] [Google Scholar]


