Abstract
Background
Although mortality rates for acute myocardial infarction (AMI) have declined for men and women, prior studies have reported a sex gap in mortality such that younger women were most likely to die after an AMI.
Methods and Results
We sought to explore the impact of race and ethnicity on the sex gap in AMI patterns of care and mortality for younger women in a contemporary patient cohort. We constructed multivariable hierarchical logistic regression models to examine trends in AMI hospitalizations, procedures, and in-hospital mortality by sex, age (<65 and ≥65 years), and race/ethnicity (white, black, and Hispanic). Analyses were derived from 194 071 patients who were hospitalized for an AMI with available race and ethnicity data from the 2009–2010 National Inpatient Sample. Hospitalization rates, procedures (coronary angiography, percutaneous coronary interventions, and cardiac bypass surgery), and inpatient mortality were analyzed across age, sex, and race/ethnic groups. There was significant variation in hospitalization rates by age and race/ethnicity. All racial/ethnic groups were less likely to undergo invasive procedures compared with white men (P<0.001). After adjustment for comorbidities, younger Hispanic women experienced higher in-hospital mortality compared with younger white men, with an odds ratio of 1.5 (95% CI 1.2 to 1.9), adjusted for age and comorbidities.
Conclusion
We found significant racial and sex disparities in AMI hospitalizations, care patterns, and mortality, with higher in-hospital mortality experienced by younger Hispanic women. Future studies are necessary to explore determinants of these significant racial and sex disparities in outcomes for AMI.
Keywords: acute myocardial infarction, disparities, outcomes, race/ethnicity, sex-based differences
Cardiovascular disease remains the leading cause of death for women,1 and considerable attention has been paid to understanding sex-based differences in coronary heart disease. Although mortality rates for acute myocardial infarction (AMI) have declined for both men and women,2 studies have reported a significant sex–age interaction and short-term mortality such that women aged <75 years were most likely to die after an AMI.3–6 Women presenting with signs and symptoms of AMI continue to experience disparities in evidence-based treatment strategies, including delayed reperfusion times, and more procedural complications.7–9 Similarly, although strides have been made in narrowing the differences in AMI management by race and ethnicity,10,11 it remains unclear if these efforts have translated to improved outcomes for diverse minority groups in the United States. Most studies exploring cardiovascular disease disparities have focused exclusively on black–white differences, and less is known about patterns of care and outcomes for Hispanic patients, one of the fastest growing segments of the US population.8 We evaluated whether the reported sex–age mortality interaction was influenced by patient race (black or white) and ethnicity (Hispanic or non-Hispanic). We also explored how AMI hospitalizations and treatment patterns differed by race/ethnicity in a contemporary patient cohort.
Methods
We used 2009 and 2010 combined data from the Nationwide Inpatient Sample (NIS), a database developed as part of the Healthcare Cost and Utilization Project (HCUP) sponsored by the Agency for Healthcare Research and Quality (AHRQ). NIS data aim to measure utilization, hospitalizations, and length of stay (LOS) by populations with a given discharge diagnosis. It is designed to approximate a stratified 20% sample of all nonfederal, general, and specialty hospitals serving adults in the United States.9 Importantly, NIS hospitalization data have all payer information, including Medicaid and other nonfederal payers. The sampling frame includes ≈90% of discharges from US hospitals and selects hospitals within states that have state inpatient databases according to defined strata based on ownership, bed size, teaching status, urban/rural location, and region. Detailed information on HCUP and NIS is available online (http://www.hcup-us.ahrq.gov). We excluded patients with missing information on race/ethnicity (13.2%, n=1 708 180) or sex (0.11%, n=14 600) and further restricted the study sample to patients who were aged ≥18 years, reported as white or black race or Hispanic ethnicity, discharged from a short-term care hospital, and had LOS <30 days.
Our main outcomes were AMI hospitalizations, patterns of care, and in-hospital mortality stratified by age. Younger patients were defined as aged <65 years, and older patients were defined as aged ≥65 years. The NIS database provides up to 25 diagnoses for each discharge record. AMI hospitalizations were defined as a discharge from an acute care hospital for a principal discharge diagnosis of AMI (International Classification of Diseases, 9th revision, clinical modification [ICD-9-CM] code 410.xx) from January 1, 2009, to December 31, 2010, across the 42 states available in the HCUP data. Prior research has found that the diagnosis of AMI using the ICD-9-CM codes has a specificity of 99.5% with a sensitivity of 72.4%, a negative predictive value of 96.1%, and a positive predictive value of 95.9%.12 AMI in-hospital mortality was defined as all-cause death during an index AMI hospitalization. The pattern of care included LOS and in-hospital procedures defined as in-hospital coronary angiography (ICD-9-CM codes 8850, 8853, 8858, 3722, and 3723), percutaneous coronary intervention (PCI; ICD-9-CM codes 3601, 3602, 3605, 3606, 3607, 0066), or coronary artery bypass grafting (CABG; ICD-9-CM codes 3610 to 3616). All outcomes were calculated for the 2 age groups of interest (18 to 64 or ≥65 years), by sex (female or male), and by race/ethnicity (white, black, and Hispanic). Specifically, we defined 6 sex–race subgroups: black men, black women, white men, white women, Hispanic men, and Hispanic women. This approach allowed us to account for the positive interaction between race and sex. Patient demographics and comorbidities included age, sex, history of heart failure, prior AMI, diabetes, hypertension, chronic obstructive pulmonary disease, depression, liver disease, peripheral vascular disease, renal failure, and/or metastatic cancer. Pertinent comorbidities were defined by the AHRQ definitions and then extracted from the HCUP data sets (http://www.hcup-us.ahrq.gov/toolssoftware/comorbidity/comorbidity.jsp). The software uses a comorbidity indexed developed by Elixhauser et al for the use of large administrative data based on diagnosis-related group and ICD-9 codes for secondary diagnosis that was found to predict in-hospital mortality, costs, and LOS. These comorbidity indicators were entered as dummy indicators in the our regression models and included age, sex, history of heart failure, diabetes (complicated and uncomplicated), hypertension, chronic obstructive pulmonary disease, pulmonary circulation disorders, depression, liver disease, peripheral vascular disease, renal failure, rheumatologic disorders, hypothyroidism, neurological disorders, weight loss, cancer, anemia, substance abuse, and coagulopathies.13
Statistical Analysis
We conducted bivariate analysis to evaluate the sex–race differences in patient characteristics and outcomes. We used the chi-square test to compare dichotomous and categorical variables and the Cuzick nonparametric test for continuous variables. We fitted a mixed-effects model with a logit link function and hospital-specific random intercepts to evaluate racial/ethnic disparities in AMI hospitalizations, adjusting for patient age and comorbidities. We included 5 dummy variables (white female, black male, black female, Hispanic male, and Hispanic female) in the model and used the white male subgroup as a reference. We fitted the same model for in-hospital procedures and mortality. Tests of significance were 2-sided at a significance level of 0.05. All analyses were conducted using SAS 64-bit version 9.3 (SAS Institute Inc). Institutional review board approval was obtained through the Brigham and Women’s Hospital Human Investigation Committee. Patient confidentiality was protected through a data use agreement with AHRQ.
Results
AMI Hospitalizations
The study population consisted of 10 567 625 all-cause hospitalizations, of which 194 071 (1.84%) were AMI in the HCUP database from 2009 to 2010 with available race/ethnicity data. Approximately 57% of AMI patients were aged ≥65 years. There was remarkable variation in the AMI hospitalization rate across the 6 race–sex subgroups. Compared with white men aged <65 years, the odds ratios (ORs) of AMI hospitalizations adjusted for age and comorbidities were 0.36 (95% CI 0.35 to 0.36), 0.53 (95% CI 0.51 to 0.55), 0.28 (95% CI 0.27 to 0.29), 0.79 (95% CI 0.77 to 0.82), and 0.23 (95% CI 0.22 to 0.24) for white women, black men, black women, Hispanic men, and Hispanic women, respectively. Similarly, compared with white men aged ≥65 years, the ORs of AMI hospitalizations adjusted for age and comorbidities were 0.75 (95% CI 0.74 to 0.76), 0.64 (95% CI 0.62 to 0.64), 0.57 (95% CI 0.55 to 0.58), 0.93 (95% CI 0.91 to 0.96), and 0.63 (95% CI 0.61 to 0.66) for white women, black men, black women, Hispanic men, and Hispanic women, respectively.
Significant variations in patient age and comorbidities were also observed among patients hospitalized for AMI across the 6 race–gender subgroups (Tables1 and 2). There were 9926 AMI hospitalizations for black women and 5482 for Hispanic women. Both black and Hispanic women were significantly younger at time of index hospitalization for AMI compared with their white counterparts (mean age 65.9 [SD 14.2] and 68.6 [SD 14.2] years compared with 72.9 [14.2] years for white women, P<0.001). Table1 describes the characteristics of hospitalizations for adults aged <65 years. Younger women hospitalized for AMI had more comorbidities than their male counterparts, with higher rates of comorbid disease among minority women. Younger Hispanic women had the highest prevalence of diabetes at 55.9% compared with 46.1% of black women and 35.9% of white women (P<0.001). Similarly, Hispanic women were more likely to suffer from hypertension and chronic kidney disease compared with both their male counterparts and non-Hispanic white women. Younger black women similarly had a higher prevalence of heart failure, hypertension, and chronic kidney disease compared with white women. The differences in comorbidities were less pronounced among adults hospitalized for AMI who were aged >65 years (Table2).
Table 1.
Characteristics of AMI Hospitalizations by Race/Ethnicity and Sex (Age <65 Years)
| Age <65 Years | |||||||
|---|---|---|---|---|---|---|---|
| White | Black | Hispanic | |||||
| Characteristics | Female (n=17 455) | Male (n=46 670) | Female (n=4694) | Male (n=7004) | Female (n=2116) | Male (n=5320) | P Value |
| Age, y (mean, SD) | 54.5 (7.6) | 53.8 (7.5) | 52.9 (8.1) | 52.1 (8.3) | 53.8 (7.9) | 52.5 (8.1) | |
| Heart failure | 19.5 | 14.2 | 26.4 | 23.4 | 22.6 | 18.7 | <0.001 |
| Diabetes | 35.9 | 26.8 | 46.1 | 34.2 | 55.9 | 43.0 | <0.001 |
| Hypertension | 62.8 | 61.4 | 78.4 | 74.5 | 70.8 | 66.3 | <0.001 |
| Chronic kidney disease | 9.5 | 7.0 | 20.0 | 19.2 | 18.8 | 12.4 | <0.001 |
| COPD | 24.6 | 15.0 | 20.2 | 12.2 | 14.8 | 9.4 | <0.001 |
| Obesity | 22.3 | 16.3 | 25.7 | 12.1 | 21.3 | 14.6 | <0.001 |
| PVD | 8.9 | 6.8 | 9.5 | 8.1 | 8.4 | 4.9 | <0.001 |
| Prior AMI | 1.4 | 1.3 | 1.7 | 1.7 | 1.1 | 1.0 | 0.01 |
| LOS, days (mean, SD) | 4.0 (3.8) | 3.8 (3.6) | 4.6 (4.1) | 4.3 (4.9) | 4.7 (4.4) | 4.3 (4.0) | <0.001 |
Data are shown as percentage except as indicated. AMI indicates acute myocardial infarction; COPD, chronic obstructive pulmonary disease; LOS, length of stay; PVD, peripheral vascular disease.
Table 2.
Characteristics of AMI Hospitalizations by Race/Ethnicity and Sex (Age ≥65 Years)
| Age ≥65 Years | |||||||
|---|---|---|---|---|---|---|---|
| White | Black | Hispanic | |||||
| Characteristics | Female (n=44 677) | Male (n=49 701) | Female (n=5232) | Male (n=3963) | Female (n=3366) | Male (n=3873) | P Value |
| Age, y (mean, SD) | 80.2 (8.5) | 76.8 (7.9) | 77.7 (8.4) | 74.8 (7.5) | 77.8 (8.1) | 75.4 (7.5) | |
| Heart failure | 43.2 | 36.1 | 45.1 | 42.1 | 42.8 | 38.9 | <0.001 |
| Diabetes | 32.3 | 34.7 | 49.8 | 42.6 | 53.2 | 49.8 | <0.001 |
| Hypertension | 72.9 | 69.8 | 80.2 | 78.2 | 77.6 | 74.5 | <0.001 |
| CKD | 21.3 | 25.0 | 34.5 | 38.9 | 24.8 | 29.7 | <0.001 |
| COPD | 24.3 | 23.0 | 18.8 | 23.0 | 19.6 | 19.7 | <0.001 |
| Obesity | 8.3 | 8.0 | 11.4 | 6.0 | 11.1 | 7.9 | <0.001 |
| PVD | 13.5 | 15.5 | 16.0 | 15.9 | 13.4 | 15.2 | <0.001 |
| Prior AMI | 1.4 | 1.3 | 1.7 | 1.6 | 1.2 | 1.3 | 0.05 |
| LOS, days (mean, SD) | 4.9 (4.2) | 4.0 (3.8) | 5.7 (4.6) | 4.3 (3.9) | 5.5 (4.7) | 4.3 (4.0) | <0.001 |
Data are shown as percentage except as indicated. AMI indicates acute myocardial infarction; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; LOS, length of stay; PVD, peripheral vascular disease.
On average, younger Hispanic and black women had longer LOS (4.6 and 4.7 days, respectively) compared with younger white men (3.8 days). Similarly, women aged >65 years had longer LOS compared with their male counterparts.
In-Hospital Procedures
Table3 outlines the procedure rates (cardiac catheterization with or without intervention, PCI, or CABG) by race/ethnicity and age group for patients during an index hospitalization for AMI. Younger patients were more likely to undergo invasive procedures compared with older adults. Overall, 47.7% of black women, 50.1% of Hispanic women, and 58.0% of white women underwent PCI or CABG during index hospitalization compared with 73.3% of white men. Figure1 shows the ORs adjusted for age and comorbidities for patients undergoing PCI or CABG. All racial/ethnic groups had lower risk-adjusted odds of an invasive procedure for AMI compared with white men within the same age category. Younger black women had significantly lower odds of undergoing PCI or CABG (OR 0.39, 95% CI 0.37 to 0.42), followed by younger Hispanic women (OR 0.41, 95% CI 0.38 to 0.45) and white women (OR 0.55, 95% CI 0.53 to 0.58), compared with white men. The pattern was similar for older women and nonwhite men (Figure1).
Table 3.
Receipt of Coronary Angiography, PCI, or CABG by Race/Ethnicity During Index Hospitalization for AMI
| White | Black | Hispanic | |||||
|---|---|---|---|---|---|---|---|
| Procedure | Female | Male | Female | Male | Female | Male | P Value |
| Age <65 Years | |||||||
| Angiography | 75.2 | 79.3 | 68.3 | 70.1 | 69.8 | 76.1 | <0.001 |
| PCI | 51.1 | 63.9 | 41.5 | 49.6 | 41.7 | 58.0 | <0.001 |
| CABG | 8.0 | 10.9 | 6.5 | 7.3 | 9.3 | 11.5 | <0.001 |
| Age ≥65 Years | |||||||
| Angiography | 45.8 | 56.3 | 43.0 | 50.8 | 50.9 | 57.7 | <0.001 |
| PCI | 29.2 | 38.0 | 23.5 | 31.8 | 28.7 | 36.9 | <0.001 |
| CABG | 5.0 | 9.9 | 4.4 | 7.0 | 6.3 | 10.5 | <0.001 |
Data are shown as percentage except as indicated. AMI indicates acute myocardial infarction; CABG, coronary artery bypass grafting; PCI, percutaneous coronary intervention.
Figure 1.
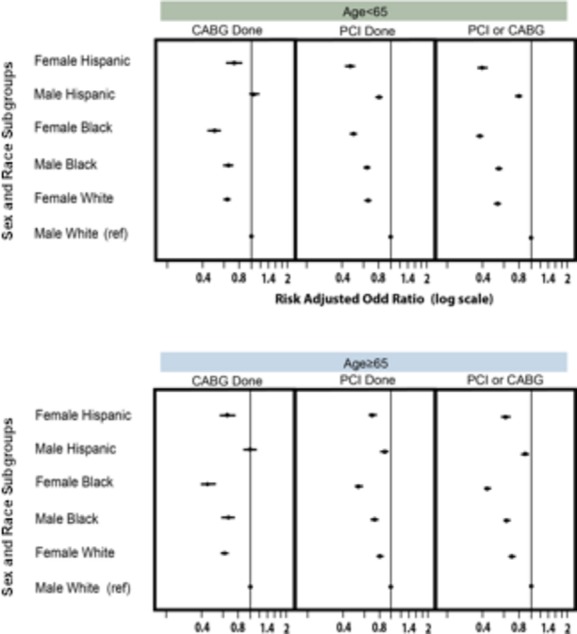
Multivariable risk-adjusted odds ratios of CABG or PCI by race/ethnicity, sex, and age. The figure depicts the adjusted odds ratios for CABG and/or PCI during an index hospitalization by sex, race/ethnicity, and age group. Comorbidities defined by Agency for Healthcare Research and Quality definitions and then extracted from the Healthcare Cost and Utilization Project data sets included the following conditions: neurological disorders, congestive heart failure, hypertension, metastatic cancer, chronic anemia, fluid and electrolyte disorders, coagulopathy, renal failure, paralysis, pulmonary circulation disorders, substance abuse, valvular disease, drug abuse, peripheral vascular disorders, hypothyroidism, obesity, and psychiatric illness. CABG indicates coronary artery bypass surgery; PCI, percutaneous coronary intervention; ref, reference.
In-Hospital Mortality
The unadjusted mortality rates by age group and racial/ethnic group are shown in Figure2. Older white women had the highest in-hospital mortality rate for AMI at 8.0%. Younger Hispanic women experienced overall higher in-hospital mortality at 3.7% compared with 3.1% for black women and 2.5% for white women. Men experienced slightly lower mortality for all groups. Figure3 shows the ORs for in-hospital mortality adjusted for age and comorbidities with white men as the reference group. Younger Hispanic, black, and white women were 1.5, 1.4, and 1.2 times more likely, respectively, to experience higher in-hospital mortality compared with younger white men, although this finding was statistically significant only for Hispanic women (Figure3). This pattern was not observed for older Hispanic women.
Figure 2.
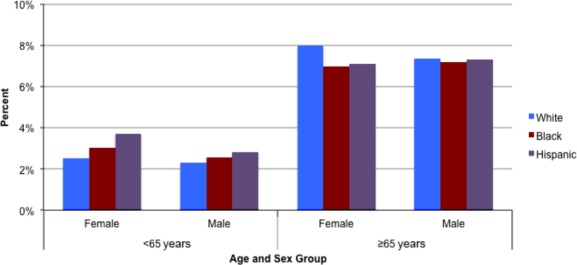
Unadjusted in-hospital mortality by sex, race/ethnicity, and age. Unadjusted in-hospital mortality rates by sex, race/ethnicity, and age group during an index hospitalization for acute myocardial infarction.
Figure 3.
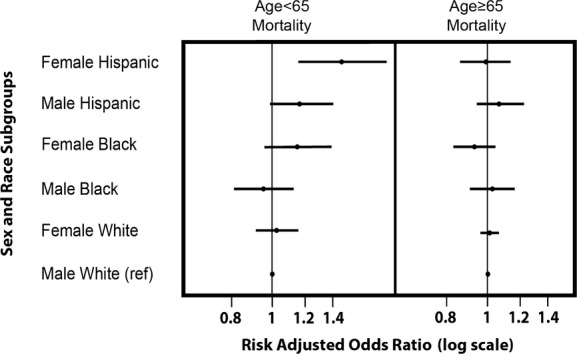
Multivariable risk-adjusted odds ratios of in-hospital mortality by race/ethnicity, sex, and age. The figure depicts the risk-adjusted odds ratios for in-hospital mortality following an index admission for an acute myocardial infarction by sex, race/ethnicity, and age group. Comorbidities defined by Agency for Healthcare Research and Quality definitions and then extracted from the Healthcare Cost and Utilization Project data sets included the following conditions: neurological disorders, congestive heart failure, hypertension, metastatic cancer, chronic anemia, fluid and electrolyte disorders, coagulopathy, renal failure, paralysis, pulmonary circulation disorders, substance abuse, valvular disease, drug abuse, peripheral vascular disorders, hypothyroidism, obesity, and psychiatric illness. This was further adjusted for in-hospital procedures (coronary angiography, percutaneous coronary angiography, or cardiac bypass surgery) as well as length of stay. Ref indicates reference.
Discussion
Using 2009–2010 data from a large inpatient sample, we found that younger Hispanic women had higher in-hospital mortality rates for AMI compared with their male counterparts. In addition, we found that persistent disparities exist by race, ethnicity, and sex in the rates of cardiac procedures performed, with women and minorities being much less likely to receive coronary angiography, PCI, or CABG during an index admission for AMI. There were also significant racial/ethnic differences in comorbid conditions, with a high prevalence of comorbidities particularly among young minority women.
Our finding that, after adjustment for comorbidities, younger Hispanic women were more likely to experience in-hospital mortality is noteworthy. Many studies have focused exclusively on black–white differences in cardiovascular disease disparities because Hispanic patients have been underrepresented in clinical trials focusing on AMI. Using data from the New York State Department of Health Statewide Planning and Research Cooperate System (SPARCS), a study showed that Hispanic participants experienced lower in-hospital mortality compared with both white and black participants, but the study sample consisted only of older Hispanic adults in New York City.14 We found no differences in mortality among those aged >65 years in a nationally representative data set. Several other studies have found that Hispanic patients presenting with AMI are younger, have more metabolic risk factors, and experience longer door-to-balloon times compared with non-Hispanic white patients.15–18 These differences, however, have not necessarily translated to worse outcomes following acute coronary syndromes in prior studies.17,19
Our study is complementary to other studies that have reported a sex–age interaction for AMI short-term mortality, for which younger women experience higher mortality compared with men.4,6,9,20,21 The persistence of this sex–age interaction for AMI is not attributable to the many demographic and clinical comorbidities included in our multivariable regression models and risk adjustment methods. There are several possible explanations. First, there is under-recognition of ischemic symptoms for women, particularly young and minority women, despite national efforts to improve awareness.22–24 Second, women have been shown to present more often with atypical symptoms than men.25,26 These factors may be exacerbated by additional barriers to care faced by Hispanic women including limited English proficiency, lack of regular access to care, and distrust of the medical system.27 Third, the likelihood that the pathophysiology of coronary heart disease is different with microvascular disease predominance contributes to our findings. A recent study from the Women’s Ischemia Syndrome Evaluation (WISE) study group found that, even in the absence of obstructive coronary artery disease, women presenting with ischemic symptoms experienced adverse long-term cardiovascular outcomes.28 Nonobstructive coronary disease, as measured by an angiographic severity score, was associated with linear increases in cardiovascular death or myocardial infarction with rates of 6.7%, 12.8%, and 25.9% for no, nonobstructive, and obstructive coronary artery disease, respectively.
Similar to other studies dating back 2 decades,10,15,29–34 we found a disparity in the rate of cardiac procedures and outcomes by race/ethnicity and sex. We found that black and Hispanic women, in both older and younger age groups, were less likely to undergo invasive procedures during an index hospitalization for AMI compared with both white women and men. Studies that have examined both sex and race have consistently found less aggressive management of coronary disease for black women,10,29,35 but data for Hispanic women are limited. Reasons for this disparity are complex, and some studies have suggested not only underuse of revascularization for minorities and women but also overuse among white men.31,36,37 It is also possible that patient preferences, eligibility for treatment, and other unmeasured characteristics partly account for this disparity, but significant racial/ethnic differences in preferences for other invasive procedures have not been found.38 Differences in institutional quality and availability of services may also play a role in these disparities. Finally, as seen in our study, younger Hispanic women experience a high burden of comorbid disease with a high prevalence of diabetes and cardiometabolic risks that may make them particularly high risk for both revascularization and unfavorable outcomes.
Our study has several strengths. First, we used contemporary data that included patients of all ages and all payers, a major limitation of prior studies was that they were limited to Medicare data. Second, our study not only compared black–white disparities but also included an in-depth study of AMI patterns of cares and outcomes in Hispanic patients, an important and growing population in the United States that has traditionally been understudied. Finally, our study included a large sample of both black and Hispanic patients hospitalized for AMI across the United States, allowing for meaningful comparisons both between and within racial and ethnic groups.
There are several limitations to our study. First, the data are administrative, which limits our ability to adjust for important clinical characteristics such as ejection fraction, distinction between ST-elevation myocardial infarction and non–ST-elevation myocardial infarction, and medication use and thus may affect our findings. Similar to other studies based on large administrative data sets, we were unable to fully account for the appropriateness of cardiac interventions of angioplasty, PCI, or CABG or detailed patient-level characteristics; however, our findings are consistent and complementary to prior studies. Furthermore, not all states report race and ethnicity information, limiting the full generalizability for our findings. Because we used ICD-9-CM coding to define AMI hospitalizations, it is possible that coding errors may over- or underreport true AMI hospitalization rates and outcomes. Finally, due to the administrative nature of the data, we were unable to disaggregate Hispanic patients into subgroups that have demonstrated significant heterogeneity in cardiovascular risk by country of origin and acculturation metrics.39 Future studies should collect disaggregated data for this important and growing US demographic group.
In conclusion, our study highlights striking and persistent racial/ethnic, sex, and age disparities in AMI treatment and mortality in a contemporary inpatient cohort. Although younger Hispanic women were less likely to be hospitalized for AMI, once they were hospitalized for an AMI, they were less likely to undergo invasive procedures and more likely to experience in-hospital mortality. Understanding why these disparities exist is important for developing targeted interventions. Future studies exploring ischemia pathogenesis, presentation, and outcomes in diverse populations are necessary to ultimately eliminate these observed disparities.
Disclosures
Dr Foody has received funding for this work through the Linda Joy Pollin Cardiovascular Wellness Center at Brigham and Women’s Hospital. Drs Rodriguez, Lopez, and Wang have no conflicts to declare. Dr López thanks the Robert Wood Johnson Foundation Harold Amos Faculty Development Program and NIDDK 1K23DK098280-01.
References
- Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, Carnethon MR, Dai S, de Simone G, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Greenlund KJ, Hailpern SM, Heit JA, Ho PM, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, McDermott MM, Meigs JB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Rosamond WD, Sorlie PD, Stafford RS, Turan TN, Turner MB, Wong ND, Wylie-Rosett J. Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation. 2011;123:e18–e209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krumholz HM, Wang Y, Chen J, Drye EE, Spertus JA, Ross JS, Curtis JP, Nallamothu BK, Lichtman JH, Havranek EP, Masoudi FA, Radford MJ, Han LF, Rapp MT, Straube BM, Normand SL. Reduction in acute myocardial infarction mortality in the United States: risk-standardized mortality rates from 1995–2006. JAMA. 2009;302:767–773. doi: 10.1001/jama.2009.1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaccarino V, Krumholz HM, Yarzebski J, Gore JM, Goldberg RJ. Sex differences in 2-year mortality after hospital discharge for myocardial infarction. Ann Intern Med. 2001;134:173–181. doi: 10.7326/0003-4819-134-3-200102060-00007. [DOI] [PubMed] [Google Scholar]
- Vaccarino V, Chen YT, Wang Y, Radford MJ, Krumholz HM. Sex differences in the clinical care and outcomes of congestive heart failure in the elderly. Am Heart J. 1999;138:835–842. doi: 10.1016/s0002-8703(99)70007-4. [DOI] [PubMed] [Google Scholar]
- Vaccarino V, Parsons L, Every NR, Barron HV, Krumholz HM. Sex-based differences in early mortality after myocardial infarction. National Registry of Myocardial Infarction 2 Participants. N Engl J Med. 1999;341:217–225. doi: 10.1056/NEJM199907223410401. [DOI] [PubMed] [Google Scholar]
- Canto JG, Rogers WJ, Goldberg RJ, Peterson ED, Wenger NK, Vaccarino V, Kiefe CI, Frederick PD, Sopko G, Zheng ZJ Investigators N. Association of age and sex with myocardial infarction symptom presentation and in-hospital mortality. JAMA. 2012;307:813–822. doi: 10.1001/jama.2012.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanghavi M, Gulati M. Sex differences in the pathophysiology, treatment, and outcomes in IHD. Curr Atheroscler Rep. 2015;17:511. doi: 10.1007/s11883-015-0511-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jneid H, Fonarow GC, Cannon CP, Hernandez AF, Palacios IF, Maree AO, Wells Q, Bozkurt B, Labresh KA, Liang L, Hong Y, Newby LK, Fletcher G, Peterson E, Wexler L Get With the Guidelines Steering C, Investigators. Sex differences in medical care and early death after acute myocardial infarction. Circulation. 2008;118:2803–2810. doi: 10.1161/CIRCULATIONAHA.108.789800. [DOI] [PubMed] [Google Scholar]
- Lichtman JH, Wang Y, Jones SB, Leifheit-Limson EC, Shaw LJ, Vaccarino V, Rumsfeld JS, Krumholz HM, Curtis JP. Age and sex differences in inhospital complication rates and mortality after percutaneous coronary intervention procedures: evidence from the NCDR((R)) Am Heart J. 2014;167:376–383. doi: 10.1016/j.ahj.2013.11.001. [DOI] [PubMed] [Google Scholar]
- Vaccarino V, Rathore SS, Wenger NK, Frederick PD, Abramson JL, Barron HV, Manhapra A, Mallik S, Krumholz HM. Sex and racial differences in the management of acute myocardial infarction, 1994 through 2002. N Engl J Med. 2005;353:671–682. doi: 10.1056/NEJMsa032214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yancy CW, Wang TY, Ventura HO, Pina IL, Vijayaraghavan K, Ferdinand KC, Hall LL. The coalition to reduce racial and ethnic disparities in cardiovascular disease outcomes (CREDO): why CREDO matters to cardiologists. J Am Coll Cardiol. 2011;57:245–252. doi: 10.1016/j.jacc.2010.09.027. [DOI] [PubMed] [Google Scholar]
- Quan H, Li B, Saunders LD, Parsons GA, Nilsson CI, Alibhai A, Ghali WA IMECCHI Investigators. Assessing validity of ICD-9-CM and ICD-10 administrative data in recording clinical conditions in a unique dually coded database. Health Serv Res. 2008;43:1424–1441. doi: 10.1111/j.1475-6773.2007.00822.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- Barnhart JM, Fang J, Alderman MH. Differential use of coronary revascularization and hospital mortality following acute myocardial infarction. Arch Intern Med. 2003;163:461–466. doi: 10.1001/archinte.163.4.461. [DOI] [PubMed] [Google Scholar]
- Shaw LJ, Shaw RE, Merz CN, Brindis RG, Klein LW, Nallamothu B, Douglas PS, Krone RJ, McKay CR, Block PC, Hewitt K, Weintraub WS, Peterson ED. Impact of ethnicity and gender differences on angiographic coronary artery disease prevalence and in-hospital mortality in the American College of Cardiology-National Cardiovascular Data Registry. Circulation. 2008;117:1787–1801. doi: 10.1161/CIRCULATIONAHA.107.726562. [DOI] [PubMed] [Google Scholar]
- Bradley EH, Herrin J, Wang Y, McNamara RL, Webster TR, Magid DJ, Blaney M, Peterson ED, Canto JG, Pollack CV, Jr, Krumholz HM. Racial and ethnic differences in time to acute reperfusion therapy for patients hospitalized with myocardial infarction. JAMA. 2004;292:1563–1572. doi: 10.1001/jama.292.13.1563. [DOI] [PubMed] [Google Scholar]
- Cohen MG, Roe MT, Mulgund J, Peterson ED, Sonel AF, Menon V, Smith SC, Jr, Saucedo JF, Lytle BL, Pollack CV, Jr, Garza L, Gibler WB, Ohman EM. Clinical characteristics, process of care, and outcomes of Hispanic patients presenting with non-ST-segment elevation acute coronary syndromes: results from can rapid risk stratification of unstable angina patients suppress adverse outcomes with early implementation of the ACC/AHA Guidelines (CRUSADE) Am Heart J. 2006;152:110–117. doi: 10.1016/j.ahj.2005.09.003. [DOI] [PubMed] [Google Scholar]
- Krim SR, Vivo RP, Krim NR, Cox M, Hernandez AF, Peterson ED, Fonarow GC, Pina IL, Schwamm LH, Bhatt DL. Regional differences in clinical profile, quality of care, and outcomes among Hispanic patients hospitalized with acute myocardial infarction in the get with guidelines-coronary artery disease (GWTG-CAD) registry. Am Heart J. 2011;162:988–995.e984. doi: 10.1016/j.ahj.2011.09.006. [DOI] [PubMed] [Google Scholar]
- Canto JG, Taylor HA, Jr, Rogers WJ, Sanderson B, Hilbe J, Barron HV. Presenting characteristics, treatment patterns, and clinical outcomes of non-black minorities in the National Registry of Myocardial Infarction 2. Am J Cardiol. 1998;82:1013–1018. doi: 10.1016/s0002-9149(98)00590-6. [DOI] [PubMed] [Google Scholar]
- Vaccarino V, Horwitz RI, Meehan TP, Petrillo MK, Radford MJ, Krumholz HM. Sex differences in mortality after myocardial infarction: evidence for a sex-age interaction. Arch Intern Med. 1998;158:2054–2062. doi: 10.1001/archinte.158.18.2054. [DOI] [PubMed] [Google Scholar]
- Bucholz EM, Butala NM, Rathore SS, Dreyer RP, Lansky AJ, Krumholz HM. Sex differences in long-term mortality after myocardial infarction: a systematic review. Circulation. 2014;130:757–767. doi: 10.1161/CIRCULATIONAHA.114.009480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diercks DB, Owen KP, Kontos MC, Blomkalns A, Chen AY, Miller C, Wiviott S, Peterson ED. Gender differences in time to presentation for myocardial infarction before and after a national women’s cardiovascular awareness campaign: a temporal analysis from the can rapid risk stratification of unstable angina patients suppress adverse outcomes with early implementation (CRUSADE) and the national cardiovascular data registry acute coronary treatment and intervention outcomes network-get with the guidelines (NCDR ACTION Registry-GWTG) Am Heart J. 2010;160:80–87.e83. doi: 10.1016/j.ahj.2010.04.017. [DOI] [PubMed] [Google Scholar]
- Mosca L, Hammond G, Mochari-Greenberger H, Towfighi A, Albert MA. Fifteen-year trends in awareness of heart disease in women: results of a 2012 American Heart Association national survey. Circulation. 2013;127:1254–1263. doi: 10.1161/CIR.0b013e318287cf2f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez F, Foody JM. Is cardiovascular disease in young women overlooked? Womens Health (Lond Engl) 2013;9:213–215. doi: 10.2217/whe.13.18. [DOI] [PubMed] [Google Scholar]
- Lopez L, Wilper AP, Cervantes MC, Betancourt JR, Green AR. Racial and sex differences in emergency department triage assessment and test ordering for chest pain, 1997–2006. Acad Emerg Med. 2010;17:801–808. doi: 10.1111/j.1553-2712.2010.00823.x. [DOI] [PubMed] [Google Scholar]
- Vaccarino V, Badimon L, Corti R, de Wit C, Dorobantu M, Manfrini O, Koller A, Pries A, Cenko E, Bugiardini R. Presentation, management, and outcomes of ischaemic heart disease in women. Nat Rev Cardiol. 2013;10:508–518. doi: 10.1038/nrcardio.2013.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson JA, Kannel WB, Lopez-Candales A, Morales L, Moreno PR, Ovalle F, Rodriguez CJ, Rodbard HW, Rosenson RS, Stern M. Avoiding the looming Latino/Hispanic cardiovascular health crisis: a call to action. J Cardiometab Syndr. 2007;2:238–243. doi: 10.1111/j.1559-4564.2007.07534.x. [DOI] [PubMed] [Google Scholar]
- Sharaf B, Wood T, Shaw L, Johnson BD, Kelsey S, Anderson RD, Pepine CJ, Bairey Merz CN. Adverse outcomes among women presenting with signs and symptoms of ischemia and no obstructive coronary artery disease: findings from the National Heart, Lung, and Blood Institute-Sponsored Women’s Ischemia Syndrome Evaluation (WISE) angiographic core laboratory. Am Heart J. 2013;166:134–141. doi: 10.1016/j.ahj.2013.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giles WH, Anda RF, Casper ML, Escobedo LG, Taylor HA. Race and sex differences in rates of invasive cardiac procedures in US hospitals. Data from the National Hospital Discharge Survey. Arch Intern Med. 1995;155:318–324. [PubMed] [Google Scholar]
- Peterson ED, Shaw LK, DeLong ER, Pryor DB, Califf RM, Mark DB. Racial variation in the use of coronary-revascularization procedures. Are the differences real? Do they matter? N Engl J Med. 1997;336:480–486. doi: 10.1056/NEJM199702133360706. [DOI] [PubMed] [Google Scholar]
- Epstein AM, Weissman JS, Schneider EC, Gatsonis C, Leape LL, Piana RN. Race and gender disparities in rates of cardiac revascularization: do they reflect appropriate use of procedures or problems in quality of care? Med Care. 2003;41:1240–1255. doi: 10.1097/01.MLR.0000093423.38746.8C. [DOI] [PubMed] [Google Scholar]
- Ayanian JZ, Udvarhelyi IS, Gatsonis CA, Pashos CL, Epstein AM. Racial differences in the use of revascularization procedures after coronary angiography. JAMA. 1993;269:2642–2646. [PubMed] [Google Scholar]
- Freund KM, Jacobs AK, Pechacek JA, White HF, Ash AS. Disparities by race, ethnicity, and sex in treating acute coronary syndromes. J Womens Health (Larchmt) 2012;21:126–132. doi: 10.1089/jwh.2010.2580. [DOI] [PubMed] [Google Scholar]
- Conigliaro J, Whittle J, Good CB, Hanusa BH, Passman LJ, Lofgren RP, Allman R, Ubel PA, O’Connor M, Macpherson DS. Understanding racial variation in the use of coronary revascularization procedures: the role of clinical factors. Arch Intern Med. 2000;160:1329–1335. doi: 10.1001/archinte.160.9.1329. [DOI] [PubMed] [Google Scholar]
- Schulman KA, Berlin JA, Harless W, Kerner JF, Sistrunk S, Gersh BJ, Dube R, Taleghani CK, Burke JE, Williams S, Eisenberg JM, Escarce JJ. The effect of race and sex on physicians’ recommendations for cardiac catheterization. N Engl J Med. 1999;340:618–626. doi: 10.1056/NEJM199902253400806. [DOI] [PubMed] [Google Scholar]
- Schneider EC, Leape LL, Weissman JS, Piana RN, Gatsonis C, Epstein AM. Racial differences in cardiac revascularization rates: does “overuse” explain higher rates among white patients? Ann Intern Med. 2001;135:328–337. doi: 10.7326/0003-4819-135-5-200109040-00009. [DOI] [PubMed] [Google Scholar]
- Cromwell J, McCall NT, Burton J, Urato C. Race/ethnic disparities in utilization of lifesaving technologies by Medicare ischemic heart disease beneficiaries. Med Care. 2005;43:330–337. doi: 10.1097/01.mlr.0000156864.80880.aa. [DOI] [PubMed] [Google Scholar]
- Ayanian JZ, Cleary PD, Weissman JS, Epstein AM. The effect of patients’ preferences on racial differences in access to renal transplantation. N Engl J Med. 1999;341:1661–1669. doi: 10.1056/NEJM199911253412206. [DOI] [PubMed] [Google Scholar]
- Daviglus ML, Talavera GA, Aviles-Santa ML, Allison M, Cai J, Criqui MH, Gellman M, Giachello AL, Gouskova N, Kaplan RC, LaVange L, Penedo F, Perreira K, Pirzada A, Schneiderman N, Wassertheil-Smoller S, Sorlie PD, Stamler J. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. JAMA. 2012;308:1775–1784. doi: 10.1001/jama.2012.14517. [DOI] [PMC free article] [PubMed] [Google Scholar]


