Abstract
Background
Improving cardiovascular health (CVH) of all Americans by 2020 is a strategic goal of the American Heart Association. Understanding the sources of variation and identifying contextual factors associated with poor CVH may suggest important avenues for prevention.
Methods and Results
Cross-sectional data from the Behavioral Risk Factor Surveillance System for the year 2011 were linked to state-level coronary heart disease and stroke mortality data from the National Vital Statistics System and to state-level measures of median household income, income inequality, taxes on soda drinks and cigarettes, and food and physical activity environments from various administrative sources. Poor CVH was defined according to the American Heart Association definition using 7 self-reported CVH metrics (current smoking, physical inactivity, obesity, poor diet, hypertension, diabetes, and high cholesterol). Linked micromap plots and multilevel logistic models were used to examine state variation in poor CVH and to investigate the contributions of individual- and state-level factors to this variation. We found significant state-level variation in the prevalence of poor CVH (median odds ratio 1.32, P<0.001). Higher rates of poor CVH and cardiovascular disease mortality were clustered in the southern states. Minority and low socioeconomic groups were strongly associated with poor CVH and explained 51% of the state-level variation in poor CVH; state-level factors explained an additional 28%. State-level median household income (odds ratio 0.89; 95% CI 0.84–0.94), taxes on soda drinks (odds ratio 0.94; 95% CI 0.89–0.99), farmers markets (odds ratio 0.91; 95% CI 0.85–0.98), and convenience stores (odds ratio 1.09; 95% CI 1.01–1.17) were predictive of poor CVH even after accounting for individual-level factors.
Conclusions
There is significant state-level variation in poor CVH that is partly explained by individual- and state-level factors. Additional longitudinal research is warranted to examine the influence of state-level policies and food and physical activity environments on poor CVH.
Keywords: cardiovascular health, geographic variation, individual- and state-level factors, linked micromap plots, multilevel analysis
Although efforts over decades have improved the cardiovascular disease (CVD) mortality rate, CVD remains the leading cause of mortality and morbidity in the United States, accounting for >1 in 3 deaths in 2010.1,2 In addition, CVD places a large economic burden on the United States, with estimated direct and indirect health care costs of more than $500 billion in 2010 alone.1 This cost is projected to increase sharply by 2020 because of the rising prevalence of some CVD risk factors such as obesity, hypertension, type 2 diabetes, and the aging of the US population.3–5
To reverse the trend, the American Heart Association (AHA) recently outlined its strategic goal of a 20% improvement in cardiovascular health (CVH) for all Americans and a 20% reduction in CVD death by 2020.1 To evaluate progress toward this goal, the AHA introduced a new concept of ideal, intermediate, and poor CVH based on 7 health metrics: hypertension, obesity, diabetes, cholesterol, smoking, diet, and physical activity. Previous studies have demonstrated that the number of ideal CVH metrics is strong predictor of CVD mortality.6–9 Studies have shown, for example, that persons who had ≥5 ideal CVH metrics had a 78% lower risk of all-cause mortality7 and a 59% lower risk of CVD compared with those having none or 1 ideal CVH metric.8
The prevalence of ideal CVH in the United States is very low. Using data from National Health and Nutrition Examination Survey, Yang et al reported that just 1% of the US population falls into the ideal CVH category (ideal in all 7 metrics), whereas >18% of the population falls into the poor CVH category (0 to 2 ideal metrics).9 Others also found similar prevalence of ideal and poor CVH in US populations.10–12 Moreover, studies have shown considerable geographic variation in the prevalence of poor or ideal CVH across states.11–13 Fang et al found that CVH varied substantially by state, ranging from 1.2% (Oklahoma) to 6.9% (District of Columbia) for ideal CVH and from 6.7% (Colorado) to 16.2% (West Virginia) for poor CVH.12 Dong et al also found very low prevalence of ideal CVH in an urban population in which no participants had all 7 ideal CVH metrics (0%) and few participants had 5 or 6 ideal metrics (4.4%).8 In addition, the prevalence of ideal CVH has also been found to be especially low in some rural populations.13
The reasons for these large variations in CVH across states and the contributions of individual- or state-level factors to this variation remain to be determined. Although several studies have explored the effects of geographic contextual factors on CVD risk factors,14–16 most focused on 1 or 2 components of CVH rather than on the combined 7 CVH metrics. Furthermore, despite considerable state and regional variation, few studies have explored the influence of state-level socioeconomic status (SES) conditions, policy measures such as taxation of soda drinks and cigarettes, and distribution of food and physical activity environments on individual-level poor CVH. Understanding the sources of variation in CVH may suggest important avenues for prevention and achievement of the overarching goal of the AHA.
In this study, we examined state-level variations in poor CVH and the contributions of individual- and state-level factors to these variations using cross-sectional data from the Behavioral Risk Factor Surveillance System (BRFSS) for the year 2011. Specifically, the main purposes of this study were (1) to examine state-level rankings and geographic patterns of poor CVH and CVD mortality using a geovisualization technique called linked micromap (LM) plots, (2) to quantify the state-level variation in poor CVH using multilevel models, and (3) to determine the extent to which individual- and state-level factors explain variation in poor CVH.
Methods
Data and Data Sources
Data on CVH and individual-level variables were obtained from the 2011 BRFSS, sponsored by the Centers for Disease Control and Prevention (CDC).17 The BRFSS has been the primary source of state-level population health estimates from surveys and has been available in all states since 1984. It collects information on health status, health-risk behaviors, and chronic conditions related to leading causes of death and disabilities at national, state, and local levels. Using random-digit dialing and a complex multistage sampling design, the BRFSS selects a sample of noninstitutionalized adults aged ≥18 years from all US states and territories. Weights can be used to generate representative national and state-level estimates. The BRFSS has been found to provide valid and reliable national estimates comparable with other national surveys in the United States.18–20 After excluding those with missing information on CVH, demographic, and socioeconomic variables, a total of 281 198 adults remained from all 50 states and the District of Columbia for analysis.
Cardiovascular Health
The 2011 BRFSS data contain core questions on each of the 7 CVH metrics (hypertension, diabetes, obesity, hypercholesterolemia, physical activity, current smoking, and consumption of fruits and vegetables). We used the AHA definition to calculate poor CVH by recoding each CVH metric as a dichotomous variable coded as 1 for poor and 0 for other categories.1 We then calculated a summary of the poor CVH score for each participant by summing the 7 dichotomized CVH metrics ranging from 0 to 7 points. We classified participants with a score of ≥5 as meeting the criteria for poor CVH.7,8,12 Additional sensitivity analysis using a continuous CVH metric showed that the results were stable, with similar patterns of associations and unchanged statistical significance.
Self-reported hypertension, diabetes, and hypercholesterolemia status were assessed by the question, “Has a doctor or other health professional ever told you that you have high blood pressure, blood sugar, and cholesterol?” Respondents who answered yes to these questions were defined as having self-reported these conditions and were coded as 1; those who responded no were coded as 0 in our analyses. Women who were told that they had hypertension or diabetes only during pregnancy were included in the no category, and those who answered “do not know/not sure” or “refused” were excluded from our analysis. Body mass index was calculated based on self-reported weight in kilograms divided by height in square meters, and obesity was defined as a body mass index of ≥30 and coded as 1 (and 0 otherwise). Current smokers were respondents who reported they had smoked ≥100 cigarettes during their lifetime or who currently smoked every day or on some days and were coded as 1 (and 0 otherwise). Sufficient physical activity was noted if respondents reported ≥150 total minutes of moderate activity per week, the equivalent in vigorous activity, or a combination of moderate and vigorous activity. Respondents with insufficient physical activity were coded as 1 (and 0 otherwise). Consumption of fruits and vegetables was defined based on responses to 6 questions that asked how many times a day participants consumed 100% fruit juice, fruit, beans or lentils, dark green vegetables, orange-colored vegetables, and other vegetables over the past month. These questions were combined to create a composite measure of average daily fruit and vegetable consumption. Respondents who consumed <5 servings of fruits or vegetables a day were coded as 1 (and 0 otherwise).
The main focus of this study was poor CVH; however, to explore the geographic correlations between poor CVH and mortality from CHD and stroke at the state level, we extracted age-adjusted CHD and stroke mortality rates for ≥15 years by state for the study period 2011–2012 from the National Vital Statistics System (NVSS), based on the CDC’s WONDER database.21 The NVSS used death certificates to ascertain and classify the cause of death for 2011 according to codes from the International Classification of Diseases, 10th Revision (ICD-10). For this analysis, the category for CHD (ICD-10 codes I20 to I25) included acute myocardial infarction, angina pectoris, atherosclerotic cardiovascular disease, and all other forms of acute and chronic ischemic heart disease. The category for stroke (ICD-10 codes I60 to I69) included ischemic and hemorrhagic strokes, strokes not specified as ischemic or hemorrhagic, and other cerebrovascular diseases (eg, occlusion and stenosis of cerebral arteries) not resulting in cerebral infarction.
Other covariates included in our analysis were age (years), sex (male or female), race or ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, and other), education levels (less than high school diploma, high school graduate, some college or technical school, and college graduate or higher), and annual household income (less than $15 000, $15 000 to $25 000, $25 000 to $49 999, and more than $50 000). The BRFSS and CDC WONDER mortality data sets are available in the public domain, and this study was exempted from human subject review by the National Institutes of Health Office for Human Subjects Research Protections (OHSRP 12516).
State-Level Variables
Several state-level variables were examined as potential contributors to state differences in poor CVH. We selected variables that had been previously hypothesized to be related to population differences in cardiovascular risk.1,14–16
Data on 2 important economic indicators, state median household income and the Gini index, were obtained for 2011 from the American Community Survey.22 The Gini index is a measure of income inequality, and its values range between 0 to 1, with 0 representing a society with no income inequality and 1 representing a society with maximal inequality.15 These economic variables were investigated because they may serve as proxies for a variety of unmeasured environmental factors (including features of the social environment) or policies that could be related to ≥1 of the risks factors included in the CVH metrics.
We also investigated 2 variables intended to capture the presence of heart-healthy policies. Soda-drink tax and cigarette excise tax for 2010 for all states and the District of Columbia were obtained from Bridging the Gap program23 and the National Conference of State Legislatures,24 respectively. In addition, we included 4 state-level variables intended to capture the food and physical activity environments in the year 2009 from the US Department of Agriculture Economic Research Service–Food Environment Atlas:25 (1) the density of grocery stores in the state per 1000 residents, defined by North American Industry Classification System (NAICS) code 445110, which includes establishments generally known as supermarkets and smaller grocery stores; (2) the density of farmers markets in the state per 1000 residents, with farmers market defined as a retail outlet in which ≥2 vendors sell agricultural products directly to customers through a common marketing channel and at least 51% of retail sales are direct to consumers; (3) the density of convenience stores in the state per 1000 residents, defined by NAICS code 447110, which includes establishments engaged in retailing automotive fuels (eg, diesel fuel, gasohol, gasoline) in combination with convenience store or food mart items; and (4) the density of fitness and recreation facilitates in the state per 1000 residents, including establishments primarily engaged in operating fitness and recreational sports facilities, as defined by NAICS code 713940. All of these state-level variables were investigated as continuous variables in units of standard deviation. Although some of these state-level variables (eg, state taxation policies) may affect only 1 risk factor (smoking), we include them because it is of interest to quantify how a specific policy could affect overall levels of CVH, as reflected in the CVH metrics.
Statistical Analysis
We examined differences in the prevalence of poor CVH across categories of individual-level demographic, SES, and state-level factors. We then calculated age-adjusted and weighted prevalence and 95% CIs of poor CVH for each of the 50 states and the District of Columbia using the 2000 US standard population.26 Sample weights were applied in calculating prevalence to account for the probability of nonresponse and noncoverage in the complex sampling design.
Next, we used the geovisualization technique of LM plots27–29 to explore state-level rankings, variations, and geographic patterns in poor CVH. We also explored the geographic correlations between poor CVH and mortality from CHD and stroke. The basic idea of the LM plots is to display information in a sequence of small maps called micromaps that provide the opportunity to explore state rankings, state variations, regional patterns, and relationships between outcomes in a joint geospatial context and traditional statistical graphic context.27,29
We then used multilevel logistic regression30 to quantify the magnitude of state-level variations in poor CVH and to examine the extent to which individual- and state-level factors explain these variations. We fitted 5 sequential models. First, we fitted an intercept-only model (model 1) without any predictors to estimate the overall variation in poor CVH at the state level. We gradually added the individual- and state-level factors to examine their associations with poor CVH and to assess their statistical contributions to the variation in poor CVH across the states. Model 2 adjusted for demographic variables (age, sex, and race). We adjusted for individual SES variables (income and education) in model 3. We then added state-level economic indicators (median household income and Gini index) in model 4. We included policy measures (soda-drink tax and cigarette excise tax) in model 5. Finally, we added food and physical environments (density of grocery stores, convenience stores, farmers markets, and recreation and fitness facilities) in model 6.
For each model, we estimated odds ratio (OR) and 95% CI associated with covariates in the model. To quantify the presence of variation in poor CVH, we estimated the state-level variance and its standard error using multilevel logistic regression. Because the interpretation of state-level variance in logistic regression is difficult, we computed the median OR (MOR) by translating state-level variance into an odds scale.31 The MOR quantifies the variation between states by comparing 2 persons from 2 randomly chosen states (ie, the MOR is the median of all possible ORs comparing a resident of a state with higher propensity with a resident of a state with lower propensity). The values of MOR are always ≥1. If the MOR is equal to 1, then there is no variation in the probability having poor CVH between states, whereas a MOR value >1 indicates variation in the probability of having poor CVH between states—the larger the OR, the stronger the variation. In addition, we also calculated the percentage of proportional change in variance (PCV) between 2 consecutive models to examine the extent to which the variables explain the variation in poor CVH across states.
Statistical analysis for descriptive and age-adjusted and weighted prevalence of CVH at the state-level were performed using the SAS-callable version of SUDAAN 11.0.0 (RTI International). Multilevel analysis was conducted using HLM software version 7.32 The LM plot was produced using R (R Foundation), a statistical software environment, and the micromap R functions provided by Carr and Pickle.29 All analyses accounted for the complex sampling design. Statistical tests were 2-sided, and a P value <0.05 was considered statistically significant.
Results
Table1 shows the distribution of poor CVH by individual- and state-level factors. The overall prevalence of age-adjusted poor CVH was 10.4% (95% CI 10.3–10.5) after accounting for sampling weights. We found large variation in poor CVH by age, sex, and race or ethnicity. Older people reported higher prevalence of poor CVH than younger people. The prevalence of poor CVH was greater among men than women. Non-Hispanic black, Hispanic and other racial or ethnic groups reported significantly higher prevalence of poor CVH compared with the non-Hispanic white group. Those with less than a high school education and with low income had higher prevalence of poor CVH compared with those with higher educational attainment and income.
Table 1.
Weighted and Age-Standardized Prevalence of Poor CVH Across Individual- and State-Level Characteristics Among Adults, Behavioral Risk Factor Surveillance Survey 2011
| Characteristics | Percentage | Prevalence of Poor CVH, % (95% CI) |
|---|---|---|
| Overall | Weighted N=125 887 430 | 10.4 (10.3–10.5) |
| Individual-level variables | ||
| Age group | ||
| 18–45 | 41.6 | 5.4 (5.1–5.7) |
| 45–54 | 24.6 | 12.4 (11.9–13.0) |
| 54–64 | 20.4 | 17.5 (16.9–18.0) |
| 65–74 | 12.2 | 19.1 (18.5–19.8) |
| ≥75 | 18.9 (16.8–21.2) | |
| Sex | ||
| Female | 50.1 | 9.9 (9.5–10.2) |
| Male | 49.9 | 10.9 (10.5–11.4) |
| Race | ||
| Non-Hispanic white | 70.4 | 9.7 (9.6–9.9) |
| Non-Hispanic black | 11.4 | 16.5 (15.9–17.1) |
| Hispanic | 11.6 | 10.7 (10.1–11.3) |
| Other racial/ethnic groups | 7.0 | 8.7 (8.2–9.2) |
| Income | ||
| <$15 000 | 9.6 | 21.0 (19.9–22.1) |
| $15 000 to <$25 000 | 14.9 | 16.4 (15.5–17.3) |
| $25 000 to <$50 000 | 24.5 | 11.1 (10.6–11.6) |
| ≥$50 000 | 51.1 | 5.9 (5.6–6.1) |
| Education | ||
| Less than high school | 10.2 | 20.0 (18.8–21.3) |
| High school or equivalent | 26.8 | 13.1 (12.6–13.7) |
| Some college or technical school | 31.1 | 10.2 (9.7–10.6) |
| Graduated from college or technical school | 31.9 | 4.6 (4.3–4.9) |
| State-level variables* | ||
| Median household income | ||
| Low | 29.5 | 13 (12.7–13.3) |
| Medium | 32.7 | 10.5 (10.3–10.7) |
| High | 37.8 | 8.2 (8.0–8.4) |
| Gini index | ||
| Low | 12.2 | 9.2 (9.0–9.4) |
| Medium | 29.9 | 11 (10.8–11.2) |
| High | 57.9 | 10.3 (10.1–10.5) |
| Soda-drink tax | ||
| Low | 23.2 | 13.01 (12.7–13.3) |
| Medium | 49.4 | 9.9 (9.7–10.1) |
| High | 27.4 | 9.2 (9.0–9.4) |
| Cigarette tax | ||
| Low | 36.4 | 11.2 (10.9–11.5) |
| Medium | 24.5 | 11.0 (10.8–11.2) |
| High | 39.2 | 9.3 (9.1–9.5) |
| Farmers markets per 1000 | ||
| Low | 54.9 | 11.3 (11.1–11.5) |
| Medium | 34.5 | 11.2 (11.0–11.4) |
| High | 10.7 | 8.9 (8.7–9.1) |
| Grocery stores per 1000 | ||
| Low | 31.0 | 10.7 (10.5–10.9) |
| Medium | 31.8 | 10.9 (10.7–11.1) |
| High | 37.3 | 8.3 (8.1–8.5) |
| Recreation and fitness facilities per 1000 | ||
| Low | 43.1 | 10.7 (10.5–10.9) |
| Medium | 40.1 | 10.1 (9.9–10.3) |
| High | 16.8 | 9.8 (9.6–10.0) |
CVH indicates cardiovascular health.
State-level factors were categorized into tertiles of low, medium, and high.
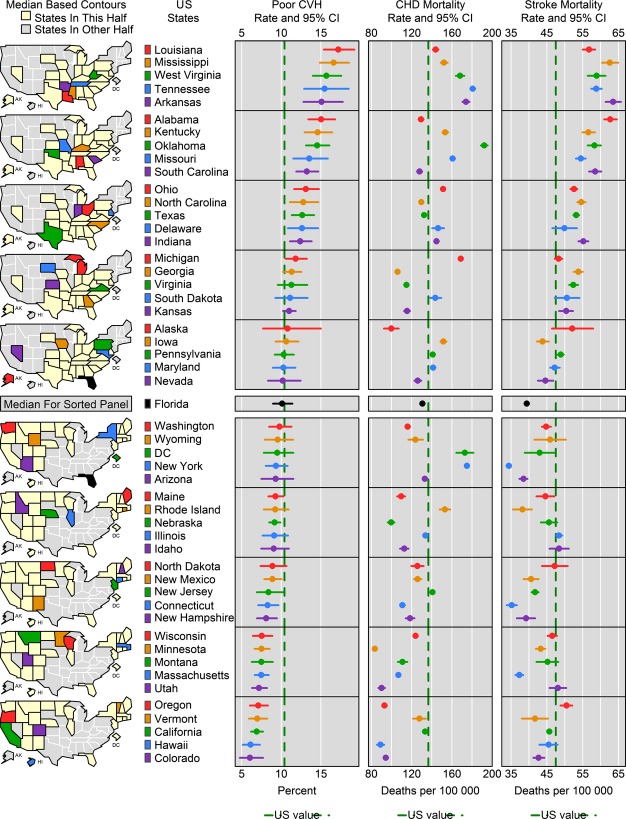
Figure 1 shows the LM plot for age-adjusted poor CVH and CHD and stroke mortality for the United States. The figure shows 5 columns linked by geographic location. The first column contains the map caricatures (micromaps) for the 50 states and the District of Columbia. The second column shows the state names. The last 3 columns are statistical panels showing age-adjusted estimates of poor CVH and mortality from CHD and stroke and their corresponding 95% CIs. All corresponding states within each micromap, state names, and statistical plots are linked through the same color designation. The micromaps are organized from top to bottom, with the top maps showing states with the highest prevalence of poor CVH and the bottom maps showing states with the lowest prevalence of poor CVH. Each map adds a set of 5 states grouped according to similarity in poor CVH. The micromaps are further divided into 2 major blocks, with Florida (black color) as the median, highlighting states that lie above and below the median. The national average is indicated with a vertical green line.
Figure 1.
Linked micromap plot showing age-adjusted prevalence of poor cardiovascular health (CVH) and mortality rates for coronary heart disease (CHD) and stroke by state in 2011. The green lines show the national average (ie, mean) of the prevalence of poor CVH (10.4%), the CHD mortality rate (136.6 per 100 000), and the stroke mortality rate (47.5 per 100 000). Florida (black color) highlights the median of poor CVH among the states and the District of Columbia. AK indicates Alaska; DC, District of Columbia; HI, Hawaii.
The LM plot reveals several interesting patterns and relationships. As shown in Figure, Louisiana (17.2%) tops the list as having the highest prevalence of poor CVH in 2011, followed by Mississippi (16.6%), West Virginia (15.7%), Tennessee (15.4%), and Arkansas (15.1%). In contrast, Colorado (6.0%) had the lowest prevalence of poor CVH, followed by Hawaii (6.1%), California (6.9%), Vermont (7.0%), and Oregon (7.1%). Overall, 22 states had higher prevalence of poor CVH than the US average of 10.4%, whereas 29 states and the District of Columbia had poor CVH lower than the US average. Furthermore, the LM plot also reveals geographic patterns in the prevalence of poor CVH: States with higher prevalence of poor CVH were primarily clustered in the South and the Midwest (states in the top panel), with the exception Minnesota, Wisconsin, and Illinois, whereas the states with lower prevalence tended to be clustered in the West and the Northeast (states in the bottom panel).
States with higher prevalence of poor CVH also tended to have higher CHD and stroke mortality, as shown in Figure 1 (Spearman’s rank correlation coefficients between poor CVH and CHD mortality: r=0.64, P<0.001; between poor CVH and stroke: r=0.81, P<0.001). The states with high CHD and stroke mortality were clustered mainly in the South (Louisiana, Mississippi, West Virginia, Tennessee, and Arkansas). The precise ranking of states in the 3 dimensions is not always consistent. The District of Columbia, New York, New Jersey, and Rhode Island, for example, ranked below the median in poor CVH but had CHD mortality rates exceeding the national average (136.6 per 100 000). Similarly, Oregon had lower poor CVH, but its stroke mortality rate exceeded the national average (47.5 per 100 000).
Table2 shows results from the multilevel analysis of poor CVH. In the random intercept-only model (model 1), we found significant variation in prevalence of poor CVH across states. The MOR was 1.32 before adjusting for individual- and state-level factors. Adjusting for individual demographic variables (model 2) reduced the variance modestly to 1.31 (PCV 7%). Further adjustment for individual-level income and education substantially reduced the variance to 1.23 (PCV 44%), as shown in model 3. Demographic variables were significantly associated with increased odds of poor CVH (OR 1.04 [95% CI 1.04–1.04] for every 1 year increase in age; OR 1.11 [95% CI 1.08–1.16] for men versus women). In addition, non-Hispanic black (OR 2.05 [95% CI 1.90–2.21]), Hispanic (OR 1.50 [95% CI 1.38–1.62]), and other racial or ethnic groups (OR 1.51 [95% CI 1.34–1.69]) had increased odds of poor CVH compared with the non-Hispanic white group (model 2). Individual-level SES variables were strongly and inversely associated with poor CVH (model 3). Adults with lower income or education had higher odds of poor CVH compared with those with higher income or education (OR 2.89 [95% CI 2.71–3.08] for low versus high income; OR 3.07 [95% CI 2.88– 3.26] for less than high school versus graduate degree).
Table 2.
Odds Ratios (95% CIs) of Poor Cardiovascular Health Associated With Individual- and State-Level Variables, Behavioral Risk Factor Surveillance Survey 2011
| Predictors* | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 |
|---|---|---|---|---|---|---|
| Fixed effects OR (95% CI) | ||||||
| Age | 1.04 (1.04–1.04) | 1.04 (1.04–1.04) | 1.04 (1.04–1.04) | 1.04 (1.04–1.04) | 1.04 (1.04–1.04) | |
| Sex (male) | 1.11 (1.08–1.16) | 1.25 (1.20–1.30) | 1.25 (1.20–1.30) | 1.25 (1.20–1.30) | 1.25 (1.20–1.30) | |
| Race | ||||||
| Non-Hispanic white | Reference | Reference | Reference | Reference | Reference | |
| Non-Hispanic black | 2.05 (1.90–2.21) | 1.36 (1.26–1.46) | 1.36 (1.26–1.46) | 1.36 (1.26–1.46) | 1.36 (1.26–1.46) | |
| Hispanic | 1.50 (1.38–1.62) | 0.85 (0.77–0.94) | 0.85 (0.77–0.94) | 0.85 (0.77–0.94) | 0.85 (0.77–0.94) | |
| Other racial/ethnic groups | 1.51 (1.34–1.69) | 1.13 (1.03–1.26) | 1.13 (1.03–1.26) | 1.13 (1.03–1.26) | 1.13 (1.03–1.25) | |
| Income | ||||||
| <$15 000 | 2.89 (2.71–3.08) | 2.89 (2.71–3.08) | 2.89 (2.71–3.08) | 2.88 (2.70–3.07) | ||
| $15 000 to <$25 000 | 2.07 (1.95–2.20) | 2.07 (1.95–2.20) | 2.07 (1.95–2.20) | 2.07 (1.95–2.20) | ||
| $25 000 to <$50 000 | 1.47 (1.39–1.56) | 1.47 (1.39–1.56) | 1.47 (1.39–1.56) | 1.47 (1.39–1.56) | ||
| ≥$50 000 | Reference | Reference | Reference | Reference | ||
| Education | ||||||
| Less than high school | 3.07 (2.88–3.26) | 3.07 (2.88–3.26) | 3.07 (2.88–3.26) | 3.05 (2.87–3.25) | ||
| High school or equivalent | 2.24 (2.12–2.37) | 2.24 (2.12–2.37) | 2.24 (2.12–2.37) | 2.24 (2.12–2.36) | ||
| Some college or technical school | 1.98 (1.86–2.10) | 1.98 (1.86–2.10) | 1.98 (1.86–2.10) | 1.97 (1.86–2.10) | ||
| Graduated from college or technical school | Reference | Reference | Reference | Reference | ||
| State-level effects† | ||||||
| Median household income, in SD units | 0.89 (0.84–0.94) | 0.92 (0.86–0.98) | 0.96 (0.89–1.04) | |||
| Gini index, in SD units | 1.04 (0.99–1.09) | 1.05 (1.00–1.11) | 1.02 (0.95–1.09) | |||
| Soda-drink tax, in SD units | 0.94 (0.89–0.99) | 0.97 (0.91–1.04) | ||||
| Cigarette tax, in SD units | 0.98 (0.93–1.03) | 0.99 (0.94–1.04) | ||||
| Density of farmers markets, in SD units | 0.91 (0.85–0.98) | |||||
| Density of RFF, in SD units | 0.97 (0.91–1.04) | |||||
| Density of grocery stores, in SD units | 1.01 (0.95–1.08) | |||||
| Density of convenience stores, in SD units | 1.09 (1.01–1.17) | |||||
| Random effects | ||||||
| Variance (SE) | 0.086 (0.29)¶ | 0.080 (0.28)¶ | 0.048 (0.22)¶ | 0.032 (0.18)¶ | 0.030 (0.17)¶ | 0.024 (0.16)¶ |
| MOR‡ | 1.32 | 1.31 | 1.23 | 1.19 | 1.18 | 1.16 |
| PCV, %§ | 6.9 | 44.2 | 62.8 | 65.1 | 72.1 | |
Model 1 is an intercept-only model. Model 2 includes model 1 plus demographic variables (age, sex, and race). Model 3 includes model 2 plus socioeconomic status variables (income and education). Model 4 includes model 3 plus state median household income and Gini index. Model 5 includes model 4 plus soda-drink tax and cigarette tax. Model 6 includes model 5 plus density of grocery stores, convenience stores, farmers markets, and RFF. MOR indicates median odds ratio; OR, odds ratio; PCV, proportional change in variance; RFF, recreational and fitness facilities.
All predictors are grand-centered at mean value.
OR estimates for state-level factors are based on population average with robust SE.
MOR =  .
.
PCV =  where, VModel1 = Variance of Model 1,
where, VModel1 = Variance of Model 1,  N, and (N = 2 – 6).
N, and (N = 2 – 6).
P<0.001.
Adjusting for state-level median household income and Gini index (model 4), the MOR decreased from 1.23 to 1.19 (PCV 63%). In model 5, the MOR was further reduced to 1.18 (PCV 65%) after adjusting for soda-drink and cigarette taxes. In model 6, adjusting for food and physical activity environments reduced the MOR to 1.16 (PCV 72%); however, the MOR is still >1 and significant, indicating the presence of residual variation unexplained by the individual-and state-level factors considered in this analysis. Of the state-level factors, median household income and soda-drink tax were statistically significantly associated with poor CVH (OR per SD increase for median household income: 0.92 [95% CI 0.86–0.98]: for soda-drinks tax: 0.94 [95% CI 0.89–0.99]; model 5). Adjusting for food and physical activity environments attenuated the associations of poor CVH with median household income and soda-drink tax (model 6). The density of convenience stores was positively associated with poor CVH (OR 1.09 [95% CI 1.01–1.17] per SD increase), whereas the density of farmers markets was inversely associated (OR 0.91 [95% CI 0.85–0.98] per SD increase). Grocery stores and recreational and fitness facilities were not associated with poor CVH.
Discussion
To our knowledge, this study is the first to demonstrate the utility of LM plots and multilevel analysis to examine state-level variations in the prevalence of poor CVH and to identify the individual- and state-level factors that may contribute to these variations. We found substantial variation in the prevalence of poor CVH across states, with an ≈3-fold difference between the high prevalence in Louisiana and the low prevalence in Colorado. Moreover, the prevalence of poor CVH showed strong geographic patterns: Higher rates of poor CVH were clustered among the southern and some midwestern states. These patterns of state-level variation in prevalence of poor CVH are consentient with prior findings.12,33 In addition, our study found strong geographic correlation between poor CVH and CVD mortality, showing that states with higher rates of poor CVH tended to have higher rates of CHD and stroke mortality. The LM plot, however, identified some exceptions to this general pattern in that some states with lower poor CVH had higher CHD mortality (the District of Columbia, New York, New Jersey, and Rhode Island) and stroke mortality (Oregon). The reasons for these discordances (which could include overreporting)34 remain to be determined, and the ecological nature of these associations does not allow individual-level causal inference.
In a second set of analyses, we used multilevel logistic models to explore variations in state-level poor CVH and the statistical contribution of both individual- and state-level factors to this variation. We observed significant variation across states. Our results indicate that both individual- and state-level factors contributed to this variation and together explained 72% of the total variation we observed. Of this 72%, 44% was explained by individual-level demographic and SES factors. Accounting for individual-level factors, an additional 28% of variation was explained by state-level factors, suggesting the importance of state-level factors in influencing poor CVH.
We found significant differences in poor CVH by race, with greater odds of poor CVH in minority groups than in the non-Hispanic white group, a finding that is consistent with the abundant evidence of higher prevalence of poor CVH in minority groups than in the non-Hispanic white group.11,35–37 Moreover, poor CVH was strongly influenced by SES; adults with lower education and income were more likely to have poor CVH than those with higher education and income. This result is consistent with several studies that found inverse graded associations of CVD risk factors with SES.38–40 We also found that state-level median household income was associated with poor CVH independently of individual-level demographic and SES factors. Our results, however, showed no significant association between income inequality and poor CVH, although the association was in the expected direction. Several studies have examined the link between income inequality and poor health, but the results have been mixed.14,15,40,41 We found no evidence that income inequality itself is associated with CVH after accounting for individual-level and other state-level factors.
We found that higher state-level soda-drink tax was associated with lower odds of poor CVH. The cross-sectional nature of our study makes it difficult to draw causal inferences, and it may be possible that other unmeasured confounding affects this association. In addition, state-level policies may be implemented in response to risk-factor levels, further limiting inferences from cross-sectional analyses. Our finding, however, is consistent with previous studies that demonstrated small but significant association between the presence of state-level taxation on soda drinks and lower obesity.42,43 Fletcher et al reported that a 1-point increase in soft-drink tax decreased adult body mass index by 0.003 point using BRFSS data.42 Soda-drink taxes could affect CVH through decreases in total caloric intake influenced by the tax itself or because of raised awareness of the negative health effects of soda-drink consumption.42,43 Cigarette tax was not significantly associated with poor CVH in our study, although the association was in the expected direction. A limitation is that our data were limited to cigarette excise taxes and did not account for other tobacco products (eg, cigars, snuff).44,45 In addition, our study did not incorporate antismoking policies such as clean air laws, quit lines, or workplace ban policies, which have been found to be effective in reducing tobacco consumption.46 Further analysis using longitudinal data is essential to understanding the potential benefits of taxation on tobacco products and soft drinks in reducing poor CVH.
We found that a higher density of farmers markets was associated with lower prevalence of poor CVH, whereas a higher density of convenience stores was associated with greater odds of poor CVH. Although our findings are cross-sectional, the results are consistent with those of prior studies showing that greater density of farmers markets was associated with greater access to fruits and vegetables and healthier eating behaviors and, in turn, lower rates of obesity and diabetes.47,48 Conversely, previous studies have also shown that greater density of convenience stores may lead to more access to energy-dense and high-fat food but less access to healthy foods, leading to higher rates of obesity and diabetes.49,50 We found no associations of grocery store density with CVH; that result is consistent with prior mixed findings16,50–53 and may be related to the fact that grocery store density is a limited measure of access to healthy foods. The density of recreational and fitness facilities was not significantly associated with poor CVH. Many studies have shown that availability of physical activity facilities is associated with greater physical activity and better health.16,54,55 An important limitation is that the measure of recreational facilities that we used did not include open-space parks and natural amenities such as climate, topography, and water area, which have been found to be inversely associated with obesity and diabetes.55
Although our findings with respect to state-level factors were mixed, our findings collectively indicate that state-level economic conditions, policy measures, and distributions of food and physical environments are associated with CVH over and above individual-level characteristics. Further research, including longitudinal evaluations of policy changes, is needed to determine whether these associations are causal and, if so, to identify the specific mechanisms involved. Previous studies have postulated that state-level factors may exert influence on individual or population CVH.14–16,56,57 State-level economic conditions, as indexed by median household income, may be proxies for a variety of environmental conditions and policies potentially related to CVD.56–60 State or local policy measures, such as taxation of sugar-sweetened beverages and tobacco products and zoning regulations and policies on land use, transportation, recreation, and availability of healthier foods, may affect levels of risky health behaviors (eg, consumption of sugar-sweetened beverages, tobacco products, and unhealthy foods or being physically inactive), which in turn have implications for overall CVH.60–62 Each of these policies may operate through a single component of the CVH metric; however, from a policy perspective, and given recent interest in global measures of overall CVH, it is desirable to understand how a specific policy may affect overall levels of risk.
Limitations and Strengths
Our study has several important limitations. First, although our multilevel design is an advance over purely ecological studies, its cross-sectional nature precludes causal inference. Second, the BRFSS data are self-reported and subject to recall bias and other measurement errors. In addition, the poor CVH measure used in this study is a proxy and may not capture the equivalent definition of poor CVH according to the AHA. Our study, for example, used only fruit and vegetable intake as a measure of diet, and that approach is less comprehensive than the AHA diet measure (which includes fruits and vegetables, whole grains, sodium, sugar-sweetened beverages, and fish).1 A third major limitation is the use of state-level variables, which may not capture important within-state variations in policies or environments. In addition, the state-level variables that we examined were limited to those with data that were easily available through public sources and do not capture the variety of state-level factors and policies that could affect CVH. For all of these reasons, our results regarding the role of specific state-level variables should be viewed as exploratory and suggestive. Nevertheless, given the important role of states as policy contexts, the investigation of state-level variations remains of interest. We found that significant state-level variation in poor CVH persisted even after all available individual- and state-level factors were included in the model, suggesting that other factors may be involved. Potential candidates include psychosocial stressors, social capital, safety, crime, quality of and access to health care, and exposure to environmental contaminants.56–59 Longitudinal analyses are needed to better understand how state-level economic conditions, policy measures, and food and physical environments affect CVH and to identity other individual- and state-level factors that may explain the geographic variation in poor CVH.
A major strength of our study is that we assessed a comprehensive set of state-level factors while controlling for individual-level confounders. Other strengths include a large sample size and the national representativeness of our findings. In addition, our study is the first, to our knowledge, to demonstrate the utility of LM plot and multilevel analysis to explore the variation in poor CVH and the contributions of individual- and state-level factors to this variation. In conclusion, our results revealed significant state-level variation in prevalence of poor CVH, with higher rates of poor CVH clustered primarily in southern states and consistent with higher rates of CHD and stroke mortality in those states. We also found that minority status and low SES were associated with poorer CVH. State-level factors including median household income, soda-drink tax, and selected food and physical environmental factors were also predictive of CVH, even after accounting for individual-level factors. These findings suggest that public health interventions to reduce CVH need to consider individual-level factors as well as the broader environmental and policy contexts in which people live.
Sources of Funding
This research is supported by Intermural Program of National Human Genomics Institute, NIH. Dr Ana Diez V. Roux is also partially supported by Michigan Center for Integrative Approaches to Health Disparities (2P60MD002249) funded by the National Institute on Minority Health and Health Disparities.
Disclosures
None.
References
- Lloyd-Jones D, Adams RJ, Brown TM, Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De SG, Ferguson TB, Ford E, Furie K, Gillespie C, Go A, Greenlund K, Haase N, Hailpern S, Ho PM, Howard V, Kissela B, Kittner S, Lackland D, Lisabeth L, Marelli A, McDermott MM, Meigs J, Mozaffarian D, Mussolino M, Nichol G, Roger VL, Rosamond W, Sacco R, Sorlie P, Roger VL, Thom T, Wasserthiel-Smoller S, Wong ND, Wylie-Rosett J on behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2010 update: a report from the American Heart Association statistics committee and stroke statistics subcommittee. Circulation. 2010;121:e1–e170. doi: 10.1161/CIRCULATIONAHA.109.192666. [DOI] [PubMed] [Google Scholar]
- Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Soliman EZ, Sorlie PD, Sotoodehnia N, Turan TN, Virani SS, Wong ND, Woo D, Turner MB American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease 246 and stroke statistics–2012 update: a report from the American Heart Association. Circulation. 2012;125:e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, Finkelstein EA, Hong Y, Johnston SC, Khera A, Lloyd-Jones DM, Nelson SA, Nichol G, Orenstein D, Wilson PW, Woo YJ American Heart Association Advocacy Coordinating Committee; Stroke Council; Council on Cardiovascular Radiology and Intervention; Council on Clinical Cardiology; Council on Epidemiology and Prevention; Council on Arteriosclerosis; Thrombosis and Vascular Biology; Council on Cardiopulmonary; Critical Care; Perioperative and Resuscitation; Council on Cardiovascular Nursing; Council on the Kidney in Cardiovascular Disease; Council on Cardiovascular Surgery and Anesthesia, and Interdisciplinary Council on Quality of Care and Outcomes Research. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123:933–944. doi: 10.1161/CIR.0b013e31820a55f5. [DOI] [PubMed] [Google Scholar]
- Huffman MD, Capewell S, Ning H, Shay CM, Ford ES, Lloyd-Jones DM. Cardiovascular health behavior and health factor changes (1988–2008) and projections to 2020: results from the National Health and Nutrition Examination Surveys. Circulation. 2012;125:2595–2602. doi: 10.1161/CIRCULATIONAHA.111.070722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- Folsom AR, Yatsuya H, Nettleton JA, Lutsey PL, Cushman M, Rosamond WD. Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J Am Coll Cardiol. 2011;57:1690–1696. doi: 10.1016/j.jacc.2010.11.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford ES, Greenlund KJ, Hong Y. Ideal cardiovascular health and mortality from all causes and diseases of the circulatory system among adults in the United States. Circulation. 2012;125:987–995. doi: 10.1161/CIRCULATIONAHA.111.049122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong C, Rundek T, Wright CB, Anwar Z, Elkind MS, Sacco RL. Ideal cardiovascular health predicts lower risks of myocardial infarction, stroke, and vascular death across whites, blacks, and Hispanics: the Northern Manhattan Study. Circulation. 2012;125:2975–2984. doi: 10.1161/CIRCULATIONAHA.111.081083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Q, Cogswell ME, Flanders WD, Hong Y, Zhang Z, Loustalot F, Gillespie C, Merritt R, Hu FB. Trends in cardiovascular health metrics and associations with all-cause and CVD mortality among US adults. JAMA. 2012;307:1273–1283. doi: 10.1001/jama.2012.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shay CM, Ning H, Allen NB, Carnethon MR, Chiuve SE, Greenlund KJ, Daviglus ML, Lloyd-Jones DM. Status of cardiovascular health in US adults/clinical Perspective: prevalence estimates from the National Health and Nutrition Examination Surveys (NHANES) 2003–2008. Circulation. 2012;125:45–56. doi: 10.1161/CIRCULATIONAHA.111.035733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bambs C, Kip KE, Dinga A, Mulukutla SR, Aiyer AN, Reis SE. Low prevalence of “ideal cardiovascular health” in a community-based population clinical perspective. Circulation. 2001;123:850–857. doi: 10.1161/CIRCULATIONAHA.110.980151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang J, Yang Q, Hong Y, Loustalot F. Status of cardiovascular health among adult Americans in the 50 states and the District of Columbia, 2009. J Am Heart Assoc. 2012;1:e005371. doi: 10.1161/JAHA.112.005371. doi: 10.1161/JAHA.112.005371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim JI, Sillah A, Boucher JL, Sidebottom AC, Knickelbine T. Prevalence of the American Heart Association’s “Ideal Cardiovascular Health” metrics in a rural, cross-sectional, community-based study: the Heart of New Ulm Project. J Am Heart Assoc. 2013;2:e000058. doi: 10.1161/JAHA.113.000058. doi: 10.1161/JAHA.113.000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez-Roux AV, Link BG, Northridge ME. A multilevel analysis of income inequality and cardiovascular disease risk factors. Soc Sci Med. 2000;50:673–687. doi: 10.1016/s0277-9536(99)00320-2. [DOI] [PubMed] [Google Scholar]
- Subramanian SV, Kawachi I, Kennedy BP. Does the state you live in make a difference? multilevel analysis of self-rated health in the US. Soc Sci Med. 2001;53:9–19. doi: 10.1016/s0277-9536(00)00309-9. [DOI] [PubMed] [Google Scholar]
- Sallis JF, Floyd MF, Rodríguez DA, Saelens BE. Role of built environments in physical activity, obesity, and cardiovascular disease. Circulation. 2012;125:729–737. doi: 10.1161/CIRCULATIONAHA.110.969022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) 2011 BRFSS summary prevalence report. Available at: http://www.cdc.gov/brfss/annual_data/annual_2011.htm. Accessed December 10, 2013.
- Nelson DE, Holtzman D, Bolen J, Stanwyck CA, Mack KA. Reliability and validity of measures from the Behavioral Risk Factor Surveillance System (BRFSS) Soz Praventivmed. 2001;46:S3–S42. [PubMed] [Google Scholar]
- Li C, Balluz LS, Ford ES, Okoro CA, Zhao G, Pierannunzi C. A comparison of prevalence estimates for selected health indicators and chronic diseases or conditions from the Behavioral Risk Factor Surveillance System, the National Health Interview Survey, and the National Health and Nutrition Examination Survey, 2007–2008. Prev Med. 2012;54:381–387. doi: 10.1016/j.ypmed.2012.04.003. [DOI] [PubMed] [Google Scholar]
- Pierannunzi C, Hu SS, Balluz LA. Systematic review of publications assessing reliability and validity of the Behavioral Risk Factor Surveillance System (BRFSS), 2004–2011. BMC Med Res Methodol. 2013;13:49. doi: 10.1186/1471-2288-13-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) US Department of Health and Human Services, CDC, National Center for Health Statistics Compressed mortality file (CMF) WONDER online database, 2011. Available at: http://wonder.cdc.gov/cmf-icd10.html. Accessed February 7, 2015.
- 2011 American Community Survey Briefs: U.S. Department of Commerce: United States Census Bureau. Available at: www.census.gov/prod/2012pubs/acsbr11-01.pdf. Accessed March 27, 2014.
- Soda drinks taxes 2010: bridging the gap: research informing policies and practice for health youth. Available at: http://www.bridgingthegapresearch.org/research/sodasnack_taxes. Accessed March 27, 2014.
- Cigarette excise tax by states: National Conference of State legislatures (NCSL). Available at: http://www.ncsl.org/research/health/2010-state-cigarette-excise-taxes.aspx. Accessed March 27, 2014.
- Food Environment Atlas data 2010: U.S. Department of Agriculture Economic Research Service, Research Service. Available at: http://www.ers.usda.gov/data-products/food-environment-atlas. Accessed March 27, 2014.
- Klein RJ, Schoenborn CA. Age adjustment using the 2000 projected US population. Healthy People 2010 Stat Notes. 2001;20:1–10. [PubMed] [Google Scholar]
- Carr DB, Wallin JF, Carr DA. Two new templates for epidemiology applications: linked micromap plots and conditioned choropleth maps. Stat Med. 2000;19:2521–2538. doi: 10.1002/1097-0258(20000915/30)19:17/18<2521::aid-sim585>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- Gebreab SY, Gillies RR, Munger RG, Symanzik J. Visualization and interpretation of birth defects data using linked micromap plots. Birth Defects Res Part A Clin Mol Teratol. 2008;82:110–119. doi: 10.1002/bdra.20419. [DOI] [PubMed] [Google Scholar]
- Carr DB, Pickle LW. Visualizing Data Patterns With Micromaps. Boca Raton: FL Chapman & Hall/CRC; 2010. [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical Linear Models: Applications and Data Analysis Methods. 2nd ed. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- Merlo J, Chaix B, Yang M, Lynch J, Rastam L. A brief conceptual tutorial of multilevel analysis in social epidemiology—linking the statistical concept of clustering to the idea of contextual phenomenon. J Epidemiol Community Health. 2005;59:443–449. doi: 10.1136/jech.2004.023473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS, Congdon R. HLM 7: Hierarchical linear & nonlinear modeling (version 7.00) [Computer software & manual] 2011. Lincolnwood, IL Scientific Software International.
- Troost JP, Rafferty AP, Luo Z, Reeves MJ. Temporal and regional trends in the prevalence of healthy lifestyle characteristics: United States, 1994-2007. Am J Public Health. 2012;102:1392–1398. doi: 10.2105/AJPH.2011.300326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agarwal R, Norton JM, Konty K, Zimmerman R, Glover M, Lekiachvili A, McGruder H, Malarcher A, Casper M, Mensah GA, Thorpe L. Overreporting of deaths from coronary heart disease in New York City hospitals, 2003. Prev Chronic Dis. 2010;7:A47. [PMC free article] [PubMed] [Google Scholar]
- Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of disparities in cardiovascular health in the United States. Circulation. 2005;111:1233–1241. doi: 10.1161/01.CIR.0000158136.76824.04. [DOI] [PubMed] [Google Scholar]
- Kramer H, Han C, Post W, Goff D, Diez Roux A, Cooper R, Jinagouda S, Shea S. Racial/ethnic differences in hypertension and hypertension treatment and control in the multi-ethnic study of atherosclerosis (MESA) Am J Hypertens. 2004;17:963–970. doi: 10.1016/j.amjhyper.2004.06.001. [DOI] [PubMed] [Google Scholar]
- McBean AM, Li S, Gilbertson DT, Collins AJ. Differences in diabetes prevalence, incidence, and mortality among the elderly of four racial/ethnic groups: whites, blacks, hispanics, and asians. Diabetes Care. 2004;27:2317–2324. doi: 10.2337/diacare.27.10.2317. [DOI] [PubMed] [Google Scholar]
- Kaplan GA, Keil JE. Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation. 1993;88:1973–1998. doi: 10.1161/01.cir.88.4.1973. [DOI] [PubMed] [Google Scholar]
- Boykin S, Diez-Roux AV, Carnethon M, Shrager S, Ni H, Whitt-Glover M. Racial/ethnic heterogeneity in the socioeconomic patterning of CVD risk factors: in the United States: the multi-ethnic study of atherosclerosis. J Health Care Poor Underserved. 2011;22:111–127. doi: 10.1353/hpu.2011.0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkman L, Kawachi I, editors. Social Epidemiology. New York, NY: Oxford University Press; 2000. [Google Scholar]
- Subramanian SV, Kawachi I. Income inequality and health: what have we learned so far? Epidemiol Rev. 2004;26:78–91. doi: 10.1093/epirev/mxh003. [DOI] [PubMed] [Google Scholar]
- Fletcher JM, Frisvold D, Tefft N. Can soft drink taxes reduce population weight? Contemp Econ Policy. 2010;28:23–35. doi: 10.1111/j.1465-7287.2009.00182.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim D, Kawachi I. Food taxation and pricing strategies to “thin out” the obesity epidemic. Am J Prev Med. 2006;30:430–437. doi: 10.1016/j.amepre.2005.12.007. [DOI] [PubMed] [Google Scholar]
- Delnevo CD, Hrywna M, Foulds J, Steinberg MB. Cigar use before and after a cigarette excise tax increase in New Jersey. Addict Behav. 2004;29:1799–1807. doi: 10.1016/j.addbeh.2004.04.024. [DOI] [PubMed] [Google Scholar]
- Nyman AL, Taylor TM, Biener L. Trends in cigar smoking and perceptions of health risks among Massachusetts adults. Tob Control. 2002;11:25–28. doi: 10.1136/tc.11.suppl_2.ii25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy DT, Friend K, Holder H, Carmona M. Effect of policies directed at youth access to smoking: results from the SimSmoke computer simulation model. Tob Control. 2001;10:108–116. doi: 10.1136/tc.10.2.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen K, Gilliland J. A farmers’ market in a food desert: evaluating impacts on the price and availability of healthy food. Health Place. 2009;15:1158–1162. doi: 10.1016/j.healthplace.2009.06.007. [DOI] [PubMed] [Google Scholar]
- Jilcott SB, Keyserling T, Crawford T, McGuirt JT, Ammerman AS. Examining associations among obesity and per capita farmers’ markets, grocery stores/supermarkets, and supercenters in US counties. J Am Diet Assoc. 2011;111:567–572. doi: 10.1016/j.jada.2011.01.010. [DOI] [PubMed] [Google Scholar]
- Sharkey JR, Dean WR, Nalty C. Convenience stores and the marketing of foods and beverages through product assortment. Am J Prev Med. 2012;43:S109–S115. doi: 10.1016/j.amepre.2012.05.012. [DOI] [PubMed] [Google Scholar]
- Salois MJ. Obesity and diabetes, the built environment, and the ‘local’ food economy in the United States, 2007. Econ Hum Biol. 2012;10:35–42. doi: 10.1016/j.ehb.2011.04.001. [DOI] [PubMed] [Google Scholar]
- Morland KB, Evenson KR. Obesity prevalence and the local food environment. Health Place. 2009;15:491–495. doi: 10.1016/j.healthplace.2008.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore LV, Diez Roux AV. Associations of neighborhood characteristics with the location and type of food stores. Am J Public Health. 2006;96:325–331. doi: 10.2105/AJPH.2004.058040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mobley LR, Root ED, Finkelstein EA, Khavjou O, Farris RP, Will JC. Environment, obesity, and cardiovascular disease risk in low-income women. Am J Prev Med. 2006;30:327–332. doi: 10.1016/j.amepre.2005.12.001. [DOI] [PubMed] [Google Scholar]
- Poortinga W. Perceptions of the environment, physical activity, and obesity. Soc Sci Med. 2006;63:2835–2846. doi: 10.1016/j.socscimed.2006.07.018. [DOI] [PubMed] [Google Scholar]
- Giles-Corti B, Broomhall M, Knuiman M, Collins C, Douglas K, Ng K, Lange A, Donovan RJ. Increasing walking: how important is distance to, attractiveness, and size of public open space? Am J Prev Med. 2005;28:169–176. doi: 10.1016/j.amepre.2004.10.018. [DOI] [PubMed] [Google Scholar]
- Mays GP, Smith SA. Geographic variation in public health spending: correlates and consequences. Health Serv Res. 2009;44:1796–1817. doi: 10.1111/j.1475-6773.2009.01014.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman JS, Witzburg R, Linov P, Campbell EG. Termination from Medicaid: how does it affect access, continuity of care, and willingness to purchase insurance? J Health Care Poor Underserved. 1999;10:122–137. doi: 10.1353/hpu.2010.0764. [DOI] [PubMed] [Google Scholar]
- Diez Roux AV, Mair C. Neighborhoods and health. Ann NY Acad Sci. 2010;1186:125–145. doi: 10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- Adler N. Overview of health disparities. In: Thomson GE, Mitchell F, Williams M, editors. Examining the Health Disparities Research Plan of the NIH: Unfinished Business. Washington, DC: National Academy Press; 2006. pp. 121–174. [Google Scholar]
- Dietz WH, Benken DE, Hunter AS. Public health law and the prevention and control of obesity. Milbank Q. 2009;87:215–227. doi: 10.1111/j.1468-0009.2009.00553.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan LK, Sobush K, Keener D, Goodman K, Lowry A, Kakietek J, Zaro S Centers for Disease Control and Prevention. Recommended community strategies and measurements to prevent obesity in the United States. MMWR Recomm Rep. 2009;58:1–26. [PubMed] [Google Scholar]
- Sallis JF, Bauman A, Pratt M. Environmental and policy interventions to promote physical activity. Am J Prev Med. 1998;15:379–397. doi: 10.1016/s0749-3797(98)00076-2. [DOI] [PubMed] [Google Scholar]