Abstract
Introduction
Numerous testosterone (T) formulations are available, each with differing effects on serum parameters.
Aim
The aim of this study was to compare the long-term effects of topical, injectable, and implantable pellet T formulations in hypogonadal men.
Methods
Retrospective review of hypogonadal men treated with a single T formulation was performed: 47 men on T gels, 57 on injectable T, and 74 on T pellets were identified. Total T (TT), calculated free T (FT), estradiol (E), hemoglobin (Hgb), hematocrit (Hct), prostate-specific antigen (PSA), total cholesterol (Tchol), triglycerides (TG), low-density lipoprotein (LDL), and high-density lipoprotein (HDL) cholesterol were evaluated at baseline and every 3–6 months for 3 years. Serum parameters were compared using a mixed model linear regression for repeated measures.
Main Outcome Measures
Effects of topical, injectable, and pellet T formulations on serum hormone levels, Hgb, Hct, lipid parameters and PSA.
Results
Men in the injectable T group were younger (42.5 ± 12.3 years) than in the gel (54.1 ± 9.8 years) or pellet groups (53.8 ± 13.0 years), and baseline FT, Hgb, and Hct were higher in the injectable T group than in gel or pellet groups. Increases in TT and FT were observed throughout follow-up in all groups. Increases in E were observed at in all T groups and throughout follow-up in injectable and gel groups. No PSA increases were observed. Erythrocytosis (Hct > 50%) was more common with injectable T (66.7%) than with T gels (12.8%) or pellets (35.1%, P < 0.0001). Transient changes in cholesterol, TG, and LDL were observed, and no significant changes were seen in HDL for any group.
Conclusions
All T formulations increase serum T and FT. More significant increases in E occur with injectable T and T gels. Changes in Hgb and Hct are most significant with injectable T, and effects on lipids are variable and inconsistent. Selection of T formulations must account for individual patient preferences and the effects of each formulation.
Keywords: . Testosterone Therapy, Testosterone Pellets, Testosterone Gel, Testosterone Injections, Erythrocytosis, Lipid Panel, Prostate Cancer
Introduction
Hypogonadism affects approximately 2–4 million men in the United States, and is characterized by low serum testosterone (T) levels in association with signs and symptoms of hypogonadism including fatigue, decreased libido, erectile dysfunction, depression, anemia, and decreased muscle mass and bone density [1],[2]. In addition to ameliorating hypogonadal symptoms [1],[3], T therapy (TTh) can lead to increased muscle mass and bone density 4–6, and reversal of the metabolic syndrome [2],[7]. However, TTh is associated with potential adverse effects including elevated serum estrogen levels, gynecomastia, local reactions, alterations in serum lipids, erythrocytosis, testicular atrophy, male infertility, and cardiovascular effects 1,2,8–11.
Numerous T formulations are Food and Drug Administration approved in the United States for the treatment of hypogonadism. Several commonly used T formulations include injectables, transdermal gels, and implantable pellets [12]. While all T preparations are effective, the likelihood of associated side effects is determined by dosage, pharmacokinetics, and method of administration [12],[13]. As such, the selection of T preparation should be a joint decision between the patient and physician, and includes consideration of treatment efficacy, cost, acceptability of the therapy by the patients, and likelihood of specific adverse effects [2],[12]. However, a relative dearth of long-term data directly comparing the effects of T formulations in men on TTh limits physicians' ability to counsel their patients. To better understand how various T formulations impact not only serum T levels, but also the likelihood of related adverse effects, we retrospectively compared the long-term effects of injectable, transdermal, and subcutaneous T pellet formulations in hypogonadal men.
Aims
We sought to compare the long-term effects of topical, injectable, and implantable pellet T formulations in hypogonadal men on serum hormone, hemoglobin (Hgb), hematocrit (Hct), lipid, and prostate-specific antigen (PSA) levels. Our goal was to assess the unique and common effects of each T formulation in order to better inform selection of T formulations for individual patients. We hypothesized that different T formulations would have varying effects on both serum hormone parameters as well as the likelihood of adverse events.
Methods
Patient Identification and Data Acquisition
After approval by the Institutional Review Board of Baylor College of Medicine, retrospective review of hypogonadal men treated with a single T formulation between 2007 and 2012 was performed. Only men that were T naïve or those who had been off of T for 3 or more months prior to restarting TTh were included in the analysis. Men were diagnosed with hypogonadism using both clinical symptoms of hypogonadism, including erectile dysfunction, decreased libido, and/or decreased energy, as well as evidence of low serum T (≤350 ng/dL). All included men were diagnosed with secondary hypogonadism. We identified 47 men treated with T gels, 57 with injectable T, and 74 with subcutaneous T pellets that met our inclusion criteria. Men using T gels applied drug daily based on manufacturer's recommendations (Testim® 50–100 mg T [one to two packets applied to the shoulder area daily; Endo, Ballsbridge, Ireland], Androgel® 1.62% 20.25–80.1 mg T [two to four pumps applied to the skin daily; AbbVie, North Chicago, IL, USA]), and men on T pellets (75 mg crystalline T/pellet) were implanted with 10–14 pellets to achieve a peak serum T level of 500–800 ng/dL every 3–6 months [14]. Men on injectable T formulations injected 100–200 mg of T cypionate or enanthate intramuscularly weekly. If men developed serum estradiol (E) levels >5 pg/mL, the upper limit of our lab's reference range, they were treated with oral aromatase inhibitor (AI).
Patient demographics, total T, free T (FT), E, Hgb, Hct, PSA, total cholesterol (Tchol), triglycerides (TG), low-density lipoprotein (LDL), and high-density lipoprotein (HDL) were evaluated at baseline and every 3–6 months for 3 years. All samples were analyzed in the Laboratory for Male Reproductive Research and Testing at Baylor College of Medicine on a single Beckman Coulter Access2 assay system (Beckman Coulter, Brea, CA, USA). Hormone levels were determined using enzyme-linked immunoassay. As the definition for erythrocytosis in the literature ranges from 50–54%, we defined erythrocytosis as Hct ≥50%, which we use in clinical practice to identify patients requiring therapeutic phlebotomy or T dose adjustment.
Statistical Analysis
Baseline and follow-up serum values were compared within each group using a mixed model linear regression for repeated measures. Erythrocytosis rates were determined and compared between groups, and the time to development of erythrocytosis in each group was determined by averaging the time it took for subjects to develop Hct ≥50%. All analyses were performed using the Statistical Package for the Social Sciences (SPSS) for Mac Version 22 (IBM Corporation, Armonk, NY, USA) with P < 0.05 considered statistically significant.
Main Outcome Measures
The primary outcomes of this study were the effects of T topical, injectable, and pellet formulations on serum hormone levels. Secondary outcomes included the effects of the above T formulations on Hgb, Hct, lipid parameters, and PSA levels.
Results
At baseline, men in the injectable T group were younger (42.5 ± 12.3 years) than in the T gel or T pellet groups (54.1 ± 9.8 and 53.8 ± 13.0 years, respectively, P < 0.001) (Table 1). More men in the T pellet group had hypertension and hyperlipidemia at baseline, and more men in the T gel group had erectile dysfunction. Baseline FT, Hgb and Hct were slightly higher in the injectable T group than in the T gel or T pellet groups (Table 2). No significant differences were observed in other serum parameters at baseline. Increases in mean T and FT levels were observed beginning at 3 months after TTh initiation and persisted throughout 3 years of follow-up in all T formulation groups (Figure 1, Supplementary Table S1). Overall, TT and FT levels were significantly higher in men receiving injectable T than in T gel or pellet groups.
Table 1.
Cohort demographics
| T gels | Injectable T | T pellets | ||
|---|---|---|---|---|
| n = 47 | n = 57 | n = 74 | P value | |
| Characteristics (mean [SD]) | ||||
| Age at start of rx (years) | 54.1 (9.8) | 42.5 (12.3) | 53.8 (13.0) | 0.001 |
| Follow-up (months) | 26.2 (10.6) | 29.8 (8.8) | 28.2 (8.6) | 0.145 |
| Range of follow-up (months) | 2.7–55.8 | 7.1–41.1 | 4.3–41.0 | |
| T naïve men | 41 (87.2) | 36 (63.2) | 33 (44.6) | |
| Men off T for ≥3 months | 6 (12.8) | 21 (36.8) | 41 (55.4) | |
| Comorbidities (n[%]) | ||||
| Diabetes mellitus | 3 (6.4) | 5 (8.8) | 11 (14.9) | 0.288 |
| Hypertension | 6 (12.8) | 3 (5.3) | 18 (24.3) | 0.009 |
| Hyperlipidemia | 5 (10.6) | 5 (8.8) | 25 (33.8) | 0.003 |
| Prostate cancer | 6 (12.8) | 4 (7.0) | 8 (10.8) | 0.609 |
| Erectile dysfunction | 32 (68.1) | 19 (33.3) | 37 (50) | 0.002 |
rx = treatment; SD = standard deviation; T = testosterone.
Table 2.
Baseline serum values
| Baseline hormones | T gels mean (SD) | Injectable T mean (SD) | T pellets mean (SD) | P value |
|---|---|---|---|---|
| Total testosterone (ng/dL) | 300 (89.6) | 306 (164.0) | 268 (167.4) | 0.297 |
| Free testosterone (ng/dL) | 5.9 (1.6) | 7.5 (5.0) | 5.7 (3.8) | 0.033 |
| Estradiol (pg/mL) | 2.66 (0.96) | 2.71 (1.36) | 2.80 (1.77) | 0.876 |
| PSA (ng/mL) | 0.879 (0.72) | 0.725 (0.53) | 1.237 (1.48) | 0.096 |
| Hemoglobin (g/dL) | 15.1 (1.1) | 15.6 (1.3) | 14.9 (1.2) | 0.008 |
| Hematocrit (%) | 44.6 (3.1) | 46.0 (3.7) | 44.3 (3.3) | 0.024 |
| Total cholesterol (mg/dL) | 191 (45.1) | 180 (40.1) | 189 (40.2) | 0.404 |
| Triglycerides (mg/dL) | 206 (205.4) | 180 (116.9) | 205 (215.2) | 0.743 |
| LDL cholesterol (mg/dL) | 106 (35.4) | 100 (37.5) | 106 (33.2) | 0.655 |
| HDL cholesterol (mg/dL) | 47 (11.1) | 43 (12.1) | 47 (11.6) | 0.16 |
HDL = high-density lipoprotein; LDL = low-density lipoprotein; PSA = prostate-specific antigen; SD = standard deviation; T = testosterone.
Figure 1.
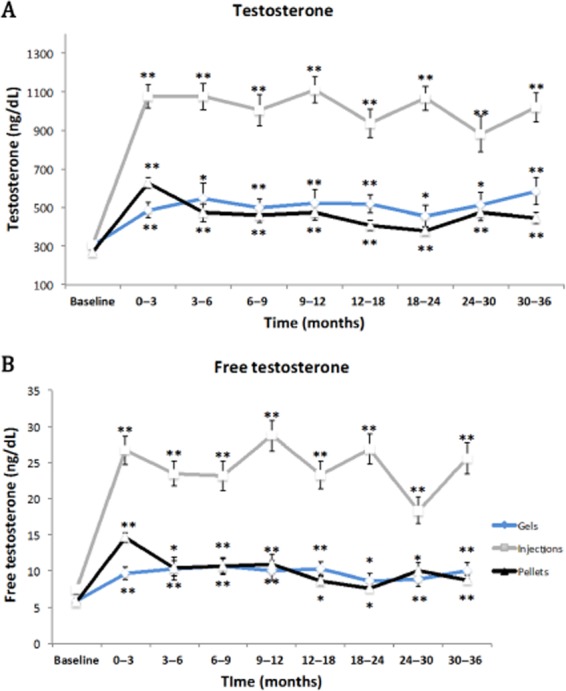
Changes in serum testosterone (T) and free testosterone (FT) levels during testosterone therapy (TTh). Changes in (A) serum total T, and (B) serum FT were assessed as a function of time and T formulation. *P < 0.05, **P < 0.001.
Significant increases in E were observed in the injectable T group beginning at 3 months and persisted throughout the follow-up period. E levels were also consistently increased from baseline in the T gel group throughout follow-up, as well as after 3–6 months of follow-up with T pellets (Figure 2). Men with E levels >5 pg/mL were treated with AIs, with 1, 12, and 22 men in the T gel, injectable T, and T pellet groups requiring therapy. A sensitivity analysis excluding AI-treated men did not significantly affect E levels during follow-up in any group (data not shown). E levels in AI-treated men normalized in all patients. Multivariate analysis demonstrated that only T level (P = 0.01), and not age (P = 0.126) or body mass index (BMI) (P = 0.813), affected E levels in all T formulation groups, with higher E levels in subjects with higher T levels.
Figure 2.
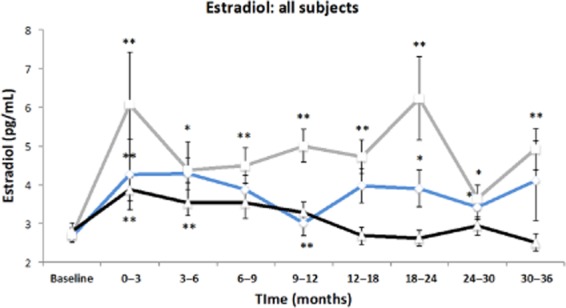
Changes in serum estradiol (E levels during testosterone therapy (TTh). Changes in serum estradiol were assessed as a function of time and testosterone (T) formulation. *P < 0.05, **P < 0.001.
A significant concern in men on TTh is that exogenous T will increase the risk of developing prostate cancer (CaP) or its progression. We evaluated the risk of CaP incidence or progression as a function of T formulation. There were 18 men in our cohort with a prior history of CaP, and all had been treated with either radical prostatectomy or radiation therapy; no men were on active surveillance. No significant PSA increases were observed in any T formulation group, regardless of whether patients had a history of CaP (Table 3). Only one subject in the T pellet group had a new diagnosis of CaP during the study, and was diagnosed with Gleason 3 + 4 CaP 2 years after TTh initiation. There were no CaP recurrences in any of the subjects with a history of CaP during the follow-up period.
Table 3.
Changes in PSA by T formulation and CaP status
| T formulation | Baseline PSA (ng/mL) | Final follow-Up PSA (ng/mL) | P value |
|---|---|---|---|
| Mean (SD) | Mean (SD) | ||
| Gels (n = 47) | 0.90 (0.72) | 1.02 (0.83) | 0.52 |
| With CaP (n = 6) | 0.06 (0.12) | 0.01(0.001) | 0.51 |
| Without CaP (n = 41) | 1.05 (0.67) | 1.23 (0.76) | 0.43 |
| Injectables (n = 57) | 0.73 (0.53) | 0.73 (0.47) | 0.99 |
| With CaP (n = 4) | 0.01 (0.00) | 0.01 (0.00) | 1.00 |
| Without CaP (n = 53) | 0.78 (0.51) | 0.86 (0.39) | 0.55 |
| Pellets (n = 74) | 1.24 (1.48) | 1.41 (1.31) | 0.54 |
| With CaP (n = 8) | 0.65 (1.45) | 0.04 (0.05) | 0.81 |
| Without CaP (n = 66) | 1.31 (1.48) | 1.46 (1.28) | 0.60 |
CaP = protstate cancer; PSA = prostate-specific antigen; SD = standard deviation; T = testosterone.
Erythrocytosis is a common adverse effect of TTh, with variable incidence as a function of T formulation. Significant increases in Hgb were observed by 6 months after TTh initiation in the injectable T and T gel groups, and by 9 months after TTh initiation in the T pellet group (Figure 3). At 9 months, when Hgb plateaus in all groups, the mean ± SD increase in Hgb was 1.06 ± 1.40 g/dL in the injectable T group, and this increase was comparable with the mean increase in the T gel and pellet groups 0.79 ± 0.94 and 0.81 ± 1.15 g/dL, respectively, (P = 0.598, Table 4). Similarly, significant increases in Hct were observed by 3 months after TTh initiation in the T pellet groups and by 6 months in the injectable T and T gel groups (Figure 3). These increases in Hgb and Hct persisted throughout follow-up. However, the rate of erythrocytosis, defined as Hct ≥50% in our study, was more common in the injectable T group (66.7%) than in the T gel (12.8%) and T pellet (35.1%) groups (P < 0.0001) (Table 5). Erythrocytosis occurred significantly earlier in the injectable T group (10.5 ± 9.1 months) when compared with the T gel (14.0 ± 12.6 months) and T pellet (16.4 ± 10.7 months) groups (P = 0.01).
Figure 3.
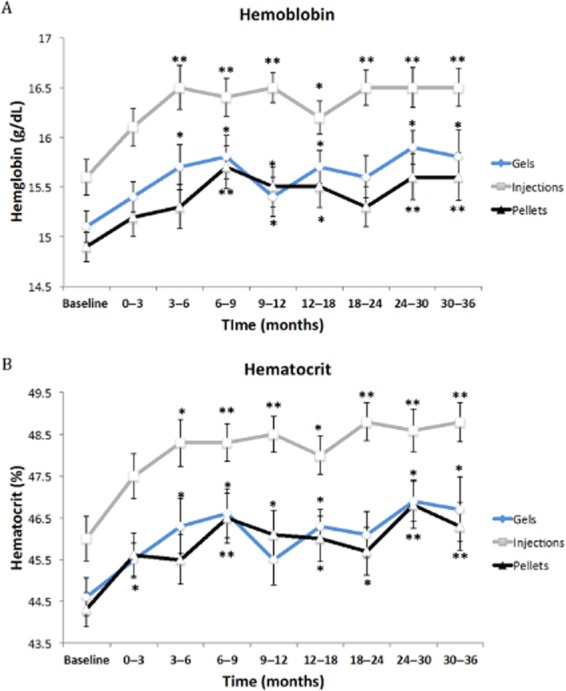
Changes in hemoglobin (Hgb) and hematocrit (Hct) during testosterone therapy (TTh). Changes in (A) Hgb and B) Hct were assessed over time as a function of testosterone (T) formulation. *P < 0.05, **P < 0.001.
Table 4.
Changes in Hgb and Hct after TTh initiation
| Group | Baseline mean (SD) | 9 months | Change | P value |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | |||
| Hgb (g/dL) | 0.598 | |||
| T gels | 15.1 (1.1) | 15.8 (1.1) | 0.79 (0.9) | |
| Injectable T | 15.6 (1.3) | 16.4 (1.1) | 1.06 (1.4) | |
| T pellets | 14.9 (1.2) | 15.7 (1.5) | 0.81 (1.2) | |
| Hct (%) | 0.074 | |||
| T gels | 44.6 (3.1) | 46.6 (3.0) | 2.55 (2.6) | |
| Injectable T | 46.0 (3.7) | 48.3 (2.7) | 6.47 (12.4) | |
| T pellets | 44.3 (3.3) | 46.5 (4.0) | 2.62 (3.5) |
Hct = hematocrit; Hgb = hemoglobin; SD = standard deviation; T = testosterone.
Table 5.
Rates and timing of erythrocytosis as a function of T formulation
| T gels | Injectable T | T pellets | ||
|---|---|---|---|---|
| n = 47 | n = 57 | n = 74 | P value | |
| Hct >50% (n[%]) | 6 (12.8) | 38 (66.7) | 26 (35.1) | <0.0001 |
| Time to increase in Hct (months) (mean [SD]) | 14.0 (12.6) | 10.5 (9.1) | 16.4 (10.7) | 0.01 |
Hct = hematocrit; Hgb = hemoglobin; SD = standard deviation; T = testosterone.
Exogenous T is known to variably affect lipid profiles, although no consistent effects have been determined as a function of T formulation. In our cohort, we observed transient decreases in mean Tchol in the T gel group at 9 and 36 months, and the T pellet group at 3, 18, and 24 months (Supplementary Figure S1). The T pellet group also demonstrated a transient decrease in TG at 36 months, and in LDL at 3 and 18 months, respectively. No significant changes were observed in HDL for any T formulation group.
Discussion
Serum T levels decline at a rate of 0.4–2.6% per year as men age, resulting in hypogonadal levels in approximately 20% of men over 60, 30% of men over 70, and 50% of men over 80 15–17. The improved recognition of the sequelae of hypogonadism coupled with an aging male population has led to a significant rise in the treatment of androgen deficiency [18]. A recent study found that 3.8% of men 60 years or older were prescribed T, and the use of T has increased by over 170% between 2007 and 2013 [2],[19],[20]. Given its widespread use, it is essential to understand the long-term benefits and adverse effects of TTh. Furthermore, because multiple TTh options are available, understanding the effect profile of each is useful when selecting T formulations for individual patients. In this study, we evaluated the long-term effects of injectable, gel, and pellet T formulations to determine the impact on serum hormones and the rates of common adverse effects of each T formulation.
As expected, all T formulations resulted in increases in serum T and FT levels, which were sustained throughout 3 years of therapy. All forms of TTh resulted in a significant increase in E levels, although this increase was present throughout follow-up in men treated with injectable T and T gels, yet lasted only up to the 6-month follow-up point in men using T pellets. These findings are supported by prior work observing an increase in E during TTh using injectable and gel T formulations [20]. The increase in E results from peripheral aromatization of T in adipose tissue and is typically more prevalent in older men on TTh, in part because of higher fat mass in older men [21]. In our study, there was no correlation between age and/or BMI and E levels, and the only variable impacting E level on multivariate analysis was T level, suggesting that higher T levels drive aromatization in our cohort. This is further supported by the decrease in E levels after initiation of AI therapy in men with elevated E levels. In our cohort 1, 12, and 22 subjects were treated with an AI in the T gel, injectable, and T pellet groups, respectively, resulting in normalization of E levels in all treated men. However, the clinical consequences of elevated E levels in men remain poorly understood. While an increase in E can lead to gynecomastia, this is uncommon (2.2%) and is often reversible upon discontinuation of TTh or treatment using an AI 22–24. Furthermore, an increase in E levels may be beneficial, as very low E levels are associated with insulin resistance, an increased risk of fractures, and a higher risk of mortality in elderly men, and elevated levels of E are associated with increased libido in men on TTh 25–28.
One significant concern with TTh is potential for the development or progression of CaP, given the androgen-responsive nature of prostate tissue. In our cohort, we found no significant increases in PSA with any T formulation, irrespective of whether treated men had a history of CaP. The apparent lack of influence of TTh on PSA levels is consistent with several prospective studies that failed to demonstrate a significant increase in PSA [1],[3],[6]. However, small increases in PSA levels in men initiating TTh during the first few months following therapy initiation have been observed [29]. Furthermore, a recent study observed overall higher PSA levels in men on T [25]. However, these increases in PSA levels are not related to the risk of CaP, and support the stimulation of prostate tissue containing unsaturated androgen receptors, as described in the prostate saturation theory proposed by Morgentaler [26]. Across numerous studies, the incidence of CaP in men on TTh is low (1.1–2.3%), similar to the prevalence in the general population 1,3–6,27,28,30. In the setting of hypogonadal men with a history of CaP treated with TTh, no definitive data supporting a detrimental effect of TTh exist. In hypogonadal men on TTh with CaP treated using radical prostatectomy or radiation, small increases in PSA have been observed, with no increases in CaP recurrence rates over those seen in eugonadal men 31–34. Similar results have been observed in men with CaP on active surveillance [35]. Overall, however, these studies have been limited by their retrospective nature and small sample sizes, precluding definitive conclusions.
Erythrocytosis is the most frequent dose-limiting adverse effect of TTh; an increase in blood viscosity can exacerbate preexisting vascular disease [9]. For this study, we defined erythrocytosis as Hct ≥ 50%, which is the cutoff value we use in clinical practice for T dose adjustment or recommendation of therapeutic phlebotomy. While all forms of TTh may lead to increases in Hct, the rate of erythrocytosis in our study was significantly higher with injectable T (66.7%) when compared with T pellets (35.1%) and T gels (12.8%). Our findings are consistent with a study by Dobs et al. comparing injectable and transdermal T formulations, in which a higher incidence of erythrocytosis (43.8%) with injectable T relative to transdermal T (15.4%) was observed [27]. However, the above study used an Hct cutoff of 52% to define erythrocytosis. When adjusting our Hct cutoff to 52%, we observe 18 (31.58%) men on injectable T, 3 (6.38%) on T gels, and 9 (12.16%) on T pellets with erythrocytosis, similar to the rates observed by Dobs et al. Our results are also comparable to a recent study examining the effects of T pellets, which observed a 20.3% rate of erythrocytosis using a Hct cutoff of 50% [14].
Erythrocytosis also occurred significantly earlier in men on injectable T formulations when compared with the other two formulations. While the mechanism of T-induced erythrocytosis is unclear, erythrocytosis is associated with supraphysiologic T and E levels [1],[2],[12],[27], as well as hepcidin, dihydrotesosterone and erythropoietin levels, and androgen receptor CAG repeat length 9,36–38. It should be noted that mean T levels in men treated with injectable T were higher than those treated with gels or pellets, which may contribute to the increased likelihood of erythroctyosis in this group. However, it is unclear whether this increased rate of erythrocytosis is related to peak T levels or overall higher serum T levels. In our cohort, men on injectable T had the highest increases in serum T and E levels, whereas data were not available for the other factors associated with erythrocytosis. Nevertheless, our data support an increased risk for erythrocytosis in men on injectable T formulations. While studies directly examining the effects of T dose on Hct are lacking, Wang et al. found a direct relationship between T gel dose and the rate of erythrocytosis, observing an increase in erythrocytosis rate from 11.3% to 17.9% when increasing T gel dose from 50 to 100 mg per day [28]. Thus, care should be taken when selecting and dosing T formulations and Hgb/Hct should be monitored regularly.
Sex steroids play a key role in the regulation of lipid metabolism. Activation of hepatic lipase (HL) leads to a decrease of LDL and HDL, and increased lipoprotein lipase (LPL) activity leads to an increase in HDL and decreased Tchol [35]. Because TTh increases HL and LPL activity, and further activation of LPL can result from elevated E levels seen with TTh, TTh may have favorable effects on lipid parameters [35]. However, studies examining the effects of TTh on lipid profiles have been variable and inconclusive, identifying both favorable (decreases in Tchol and LDL with injectable T) 39–41 and unfavorable (decreases in HDL and increases in Tchol and LDL with injectable and pellet T) [42],[43] effects on lipid parameters. A recent meta-analysis examining 51 studies using various T formulations (28 injectable T, 17 transdermal T, and 6 oral T) found that the only change in lipids during TTh was a small, but significant decrease in HDL [10]. We did not observe an effect on HDL in our cohort and no consistent, significant changes in any lipid parameter were observed. This may be due to the fact that the lipid levels in our cohort were not consistently drawn from fasting patients, as they had been in the previous study observing a decrease in Tchol and LDL levels with TTh [35]. Furthermore, changes in the diets of subjects in our study were not tracked, so the influence of diet on lipid parameters in our cohort cannot be determined.
The strengths of this study include the selection of T-naïve men or men who had been off of TTh for 3 or more months, that all men in the study were treated using a single T formulation for the duration of follow-up, the study's single-center design, the long follow-up period, and the reproducibility associated with utilizing a single laboratory for evaluation of all serum variables. Furthermore, the ability to compare T formulations within a single clinic setting is significant. Our study is limited by several factors, including its retrospective design, precluding the ability to randomize the cohort to treatment and limiting the ability to evaluate the impact of confounding factors, the lack of fasting lipid parameters in all patients, the use of AIs, and the relatively small sample size necessitated by the rigorous patient selection schema. Furthermore, the 3 T formulation groups are imperfectly matched, with differing ages and comorbidities between groups, as well as varying levels of T and FT observed during follow-up, limiting the ability to compare the groups.
In summary, this study supports prior findings associating different T formulations with variable adverse effect rates. Specifically, injectable T formulations are associated with significant increases in E and higher erythrocytosis rates relative to T gels and pellets, possibly related to elevated mean or peak T levels. PSA levels are not affected by T formulation, and inconsistent variations in lipid levels occur, also apparently independently of T formulation. Understanding the differences in effect profiles for each T formulation is useful for individualizing TTh and identifying parameters that require regular monitoring.
Conflict of Interest
The author(s) report no conflicts of interest.
Supporting Information
Figure S1 Changes in lipid parameters during TTh.
Changes in (A) total cholesterol, (B) Triglycerides, (C) LDL Cholesterol, and (D) HDL Cholesterol were assessed over time as a function of T formulation.
Table S1 Summary serum data during follow-up.
References
- Rhoden EL, Morgentaler A. Risks of testosterone-replacement therapy and recommendations for monitoring. N Engl J Med. 2004;350:482–492. doi: 10.1056/NEJMra022251. [DOI] [PubMed] [Google Scholar]
- Bassil N, Alkaade S, Morley JE. The benefits and risks of testosterone replacement therapy: A review. Ther Clin Risk Manag. 2009;5:427–448. doi: 10.2147/tcrm.s3025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder PJ, Peachey H, Berlin JA, Hannoush P, Haddad G, Dlewati A, Santanna J, Loh L, Lenrow DA, Holmes JH, Kapoor SC, Atkinson LE, Strom BL. Effects of testosterone replacement in hypogonadal men. J Clin Endocrinol Metab. 2000;85:2670–2677. doi: 10.1210/jcem.85.8.6731. [DOI] [PubMed] [Google Scholar]
- Kenny AM, Prestwood KM, Gruman CA, Marcello KM, Raisz LG. Effects of transdermal testosterone on bone and muscle in older men with low bioavailable testosterone levels. J Gerontol A Biol Sci Med Sci. 2001;56:M266–272. doi: 10.1093/gerona/56.5.m266. [DOI] [PubMed] [Google Scholar]
- Snyder PJ, Peachey H, Hannoush P, Berlin JA, Loh L, Holmes JH, Dlewati A, Staley J, Santanna J, Kapoor SC, Attie MF, Haddad JG, Jr, Strom BL. Effect of testosterone treatment on bone mineral density in men over 65 years of age. J Clin Endocrinol Metab. 1999;84:1966–1972. doi: 10.1210/jcem.84.6.5741. [DOI] [PubMed] [Google Scholar]
- Sih R, Morley JE, Kaiser FE, Perry HM, 3rd, Patrick P, Ross C. Testosterone replacement in older hypogonadal men: A 12-month randomized controlled trial. J Clin Endocrinol Metab. 1997;82:1661–1667. doi: 10.1210/jcem.82.6.3988. [DOI] [PubMed] [Google Scholar]
- Kapoor D, Goodwin E, Channer KS, Jones TH. Testosterone replacement therapy improves insulin resistance, glycaemic control, visceral adiposity and hypercholesterolaemia in hypogonadal men with type 2 diabetes. Eur J Endocrinol. 2006;154:899–906. doi: 10.1530/eje.1.02166. [DOI] [PubMed] [Google Scholar]
- Calof OM, Singh AB, Lee ML, Kenny AM, Urban RJ, Tenover J, Bhasin S. Adverse events associated with testosterone replacement in middle-aged and older men: A meta-analysis of randomized, placebo-controlled trials. J Gerontol A Biol Sci Med Sci. 2005;60:1451–1457. doi: 10.1093/gerona/60.11.1451. [DOI] [PubMed] [Google Scholar]
- Aghazadeh M, Pastuszak AW, Johnson WG, McIntyre MG, Hsieh TM, Lipshultz LI. Elevated dihydrotestosterone is associated with testosterone-induced erythrocytosis. J Urol. 2015;194:160–165. doi: 10.1016/j.juro.2015.01.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez-Balsells MM, Murad MH, Lane M, Lampropulos JF, Albuquerque F, Mullan RJ, Agrwal N, Elamin MB, Gallegos-Orozco JF, Wang AT, Erwin PJ, Bhasin S, Montori VM. Clinical review 1: Adverse effects of testosterone therapy in adult men: A systematic review and meta-analysis. J Clin Endocrinol Metab. 2010;95:2560–2575. doi: 10.1210/jc.2009-2575. [DOI] [PubMed] [Google Scholar]
- Xu L, Freeman G, Cowling BJ, Schooling CM. Testosterone therapy and cardiovascular events among men: A systematic review and meta-analysis of placebo-controlled randomized trials. BMC Med. 2013;11:108. doi: 10.1186/1741-7015-11-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tenover JL. The androgen-deficient aging male: Current treatment options. Rev Urol. 2003;5(suppl 1):S22–28. [PMC free article] [PubMed] [Google Scholar]
- Kovac JR, Rajanahally S, Smith RP, Coward RM, Lamb DJ, Lipshultz LI. Patient satisfaction with testosterone replacement therapies: The reasons behind the choices. J Sex Med. 2014;11:553–562. doi: 10.1111/jsm.12369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pastuszak AW, Mittakanti H, Liu JS, Gomez L, Lipshultz LI, Khera M. Pharmacokinetic evaluation and dosing of subcutaneous testosterone pellets. J Androl. 2012;33:927–937. doi: 10.2164/jandrol.111.016295. [DOI] [PubMed] [Google Scholar]
- Moskovic DJ, Araujo AB, Lipshultz LI, Khera M. The 20-year public health impact and direct cost of testosterone deficiency in U.S. men. J Sex Med. 2013;10:562–569. doi: 10.1111/j.1743-6109.2012.02944.x. [DOI] [PubMed] [Google Scholar]
- Feldman HA, Longcope C, Derby CA, Johannes CB, Araujo AB, Coviello AD, Bremner WJ, McKinlay JB. Age trends in the level of serum testosterone and other hormones in middle-aged men: Longitudinal results from the Massachusetts male aging study. J Clin Endocrinol Metab. 2002;87:589–598. doi: 10.1210/jcem.87.2.8201. [DOI] [PubMed] [Google Scholar]
- Harman SM, Metter EJ, Tobin JD, Pearson J, Blackman MR Baltimore Longitudinal Study of Aging. Longitudinal effects of aging on serum total and free testosterone levels in healthy men. Baltimore Longitudinal Study of Aging. J Clin Endocrinol Metab. 2001;86:724–731. doi: 10.1210/jcem.86.2.7219. [DOI] [PubMed] [Google Scholar]
- Smith RP, Khanna A, Coward RM, Rajanahally S, Kovac JR, Gonzales MA, Lipshultz LI. Factors influencing patient decisions to initiate and discontinue subcutaneous testosterone pellets (Testopel) for treatment of hypogonadism. J Sex Med. 2013;10:2326–2333. doi: 10.1111/jsm.12226. [DOI] [PubMed] [Google Scholar]
- Nigro N, Christ-Crain M. Testosterone treatment in the aging male: Myth or reality? Swiss Med Wkly. 2012;142:w13539. doi: 10.4414/smw.2012.13539. [DOI] [PubMed] [Google Scholar]
- Baillargeon J, Urban RJ, Ottenbacher KJ, Pierson KS, Goodwin JS. Trends in androgen prescribing in the United States, 2001 to 2011. JAMA Intern Med. 2013;173:1465–1466. doi: 10.1001/jamainternmed.2013.6895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakshman KM, Kaplan B, Travison TG, Basaria S, Knapp PE, Singh AB, LaValley MP, Mazer NA, Bhasin S. The effects of injected testosterone dose and age on the conversion of testosterone to estradiol and dihydrotestosterone in young and older men. J Clin Endocrinol Metab. 2010;95:3955–3964. doi: 10.1210/jc.2010-0102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajjar RR, Kaiser FE, Morley JE. Outcomes of long-term testosterone replacement in older hypogonadal males: A retrospective analysis. J Clin Endocrinol Metab. 1997;82:3793–3796. doi: 10.1210/jcem.82.11.4387. [DOI] [PubMed] [Google Scholar]
- Rhoden EL, Morgentaler A. Treatment of testosterone-induced gynecomastia with the aromatase inhibitor, anastrozole. Int J Impot Res. 2004;16:95–97. doi: 10.1038/sj.ijir.3901154. [DOI] [PubMed] [Google Scholar]
- Seftel A. Testosterone replacement therapy for male hypogonadism: Part III. Pharmacologic and clinical profiles, monitoring, safety issues, and potential future agents. Int J Impot Res. 2007;19:2–24. doi: 10.1038/sj.ijir.3901366. [DOI] [PubMed] [Google Scholar]
- Peskoe SB, Joshu CE, Rohrmann S, McGlynn KA, Nyante SJ, Bradwin G, Dobs AS, Kanarek N, Nelson WG, Platz EA. Circulating total testosterone and PSA concentrations in a nationally representative sample of men without a diagnosis of prostate cancer. Prostate. 2015;75:1167–1176. doi: 10.1002/pros.22998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgentaler A, Traish AM. Shifting the paradigm of testosterone and prostate cancer: The saturation model and the limits of androgen-dependent growth. Eur Urol. 2009;55:310–320. doi: 10.1016/j.eururo.2008.09.024. [DOI] [PubMed] [Google Scholar]
- Dobs AS, Meikle AW, Arver S, Sanders SW, Caramelli KE, Mazer NA. Pharmacokinetics, efficacy, and safety of a permeation-enhanced testosterone transdermal system in comparison with bi-weekly injections of testosterone enanthate for the treatment of hypogonadal men. J Clin Endocrinol Metab. 1999;84:3469–3478. doi: 10.1210/jcem.84.10.6078. [DOI] [PubMed] [Google Scholar]
- Wang C, Swerdloff RS, Iranmanesh A, Dobs A, Snyder PJ, Cunningham G, Matsumoto AM, Weber T, Berman N Testosterone Gel Study Group. Transdermal testosterone gel improves sexual function, mood, muscle strength, and body composition parameters in hypogonadal men. J Clin Endocrinol Metab. 2000;85:2839–2853. doi: 10.1210/jcem.85.8.6747. [DOI] [PubMed] [Google Scholar]
- Marks LS, Mazer NA, Mostaghel E, Hess DL, Dorey FJ, Epstein JI, Veltri RW, Makarov DV, Partin AW, Bostwick DG, Macairan ML, Nelson PS. Effect of testosterone replacement therapy on prostate tissue in men with late-onset hypogonadism: A randomized controlled trial. JAMA. 2006;296:2351–2361. doi: 10.1001/jama.296.19.2351. [DOI] [PubMed] [Google Scholar]
- Haider A, Zitzmann M, Doros G, Isbarn H, Hammerer P, Yassin A. Incidence of prostate cancer in hypogonadal men receiving testosterone therapy: Observations from 5-year median followup of 3 registries. J Urol. 2015;193:80–86. doi: 10.1016/j.juro.2014.06.071. [DOI] [PubMed] [Google Scholar]
- Agarwal PK, Oefelein MG. Testosterone replacement therapy after primary treatment for prostate cancer. J Urol. 2005;173:533–536. doi: 10.1097/01.ju.0000143942.55896.64. [DOI] [PubMed] [Google Scholar]
- Kaufman JM, Graydon RJ. Androgen replacement after curative radical prostatectomy for prostate cancer in hypogonadal men. J Urol. 2004;172:920–922. doi: 10.1097/01.ju.0000136269.10161.32. [DOI] [PubMed] [Google Scholar]
- Pastuszak AW, Pearlman AM, Godoy G, Miles BJ, Lipshultz LI, Khera M. Testosterone replacement therapy in the setting of prostate cancer treated with radiation. Int J Impot Res. 2013;25:24–28. doi: 10.1038/ijir.2012.29. [DOI] [PubMed] [Google Scholar]
- Pastuszak AW, Pearlman AM, Lai WS, Godoy G, Sathyamoorthy K, Liu JS, Miles BJ, Lipshultz LI, Khera M. Testosterone replacement therapy in patients with prostate cancer after radical prostatectomy. J Urol. 2013;190:639–644. doi: 10.1016/j.juro.2013.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgentaler A, Lipshultz LI, Bennett R, Sweeney M, Avila D, Jr, Khera M. Testosterone therapy in men with untreated prostate cancer. J Urol. 2011;185:1256–1260. doi: 10.1016/j.juro.2010.11.084. [DOI] [PubMed] [Google Scholar]
- Bachman E, Feng R, Travison T, Li M, Olbina G, Ostland V, Ulloor J, Zhang A, Basaria S, Ganz T, Westerman M, Bhasin S. Testosterone suppresses hepcidin in men: A potential mechanism for testosterone-induced erythrocytosis. J Clin Endocrinol Metab. 2010;95:4743–4747. doi: 10.1210/jc.2010-0864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zitzmann M, Nieschlag E. Androgen receptor gene CAG repeat length and body mass index modulate the safety of long-term intramuscular testosterone undecanoate therapy in hypogonadal men. J Clin Endocrinol Metab. 2007;92:3844–3853. doi: 10.1210/jc.2007-0620. [DOI] [PubMed] [Google Scholar]
- Bachman E, Travison TG, Basaria S, Davda MN, Guo W, Li M, Connor WestfallJ, Bae H, Gordeuk V, Bhasin S. Testosterone induces erythrocytosis via increased erythropoietin and suppressed hepcidin: Evidence for a new erythropoietin/hemoglobin set point. J Gerontol A Biol Sci Med Sci. 2014;69:725–735. doi: 10.1093/gerona/glt154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zgliczynski S, Ossowski M, Slowinska-Srzednicka J, Brzezinska A, Zgliczynski W, Soszynski P, Chotkowska E, Srzednicki M, Sadowski Z. Effect of testosterone replacement therapy on lipids and lipoproteins in hypogonadal and elderly men. Atherosclerosis. 1996;121:35–43. doi: 10.1016/0021-9150(95)05673-4. [DOI] [PubMed] [Google Scholar]
- Tenover JS. Effects of testosterone supplementation in the aging male. J Clin Endocrinol Metab. 1992;75:1092–1098. doi: 10.1210/jcem.75.4.1400877. [DOI] [PubMed] [Google Scholar]
- Morley JE, Perry HM, 3rd, Kaiser FE, Kraenzle D, Jensen J, Houston K, Mattammal M, Perry HM., Jr Effects of testosterone replacement therapy in old hypogonadal males: A preliminary study. J Am Geriatr Soc. 1993;41:149–152. doi: 10.1111/j.1532-5415.1993.tb02049.x. [DOI] [PubMed] [Google Scholar]
- Thompson PD, Cullinane EM, Sady SP, Chenevert C, Saritelli AL, Sady MA, Herbert PN. Contrasting effects of testosterone and stanozolol on serum lipoprotein levels. JAMA. 1989;261:1165–1168. [PubMed] [Google Scholar]
- Jones DB, Higgins B, Billet JS, Price WH, Edwards CR, Beastall GH, Shepherd J, Sweeting VM, Horn DB, Wenham PR. The effect of testosterone replacement on plasma lipids and apolipoproteins. Eur J Clin Invest. 1989;19:438–441. doi: 10.1111/j.1365-2362.1989.tb00256.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1 Changes in lipid parameters during TTh.
Changes in (A) total cholesterol, (B) Triglycerides, (C) LDL Cholesterol, and (D) HDL Cholesterol were assessed over time as a function of T formulation.
Table S1 Summary serum data during follow-up.


