Abstract
Introduction
Premature ejaculation (PE) is defined by short ejaculatory latency and inability to delay ejaculation causing distress. Management may involve behavioral and/or pharmacological approaches.
Aim
To systematically review the randomized controlled trial (RCT) evidence for behavioral therapies in the management of PE.
Methods
Nine databases including MEDLINE were searched up to August 2014. Included RCTs compared behavioral therapy against waitlist control or another therapy, or behavioral plus drug therapy against drug treatment alone. [Correction added on 10 September 2015, after first online publication: Search period has been amended from August 2013 to August 2014.]
Main Outcome Measure
Intravaginal ejaculatory latency time (IELT), sexual satisfaction, ejaculatory control, and anxiety and adverse effects.
Results
Ten RCTs (521 participants) were included. Overall risk of bias was unclear. All studies assessed physical techniques, including squeeze and stop-start, sensate focus, stimulation device, and pelvic floor rehabilitation. Only one RCT included a psychotherapeutic approach (combined with stop-start and drug treatment). Four trials compared behavioral therapies against waitlist control, of which two (involving squeeze, stop-start, and sensate focus) reported IELT differences of 7–9 minutes, whereas two (web-based sensate focus, stimulation device) reported no difference in ejaculatory latency posttreatment. For other outcomes (sexual satisfaction, desire, and self-confidence), some waitlist comparisons significantly favored behavioral therapy, whereas others were not significant. Three trials favored combined behavioral and drug treatment over drug treatment alone, with small but significant differences in IELT (0.5–1 minute) and significantly better results on other outcomes (sexual satisfaction, ejaculatory control, and anxiety). Direct comparisons of behavioral therapy vs. drug treatment gave mixed results, mostly either favoring drug treatment or showing no significant difference. No adverse effects were reported, though safety data were limited.
Conclusions
There is limited evidence that physical behavioral techniques for PE improve IELT and other outcomes over waitlist and that behavioral therapies combined with drug treatments give better outcomes than drug treatments alone. Further RCTs are required to assess psychotherapeutic approaches to PE.
Keywords: Review, Systematic, Premature Ejaculation, Behavior Therapy, Psychological Therapy
Introduction
Premature ejaculation (PE) is a male sexual dysfunction characterized by short ejaculatory latency. PE can be either lifelong (primary, present since first sexual experiences) or acquired (secondary, beginning later). The 2014 update of the International Society for Sexual Medicine (ISSM) Guidelines for the Diagnosis and Treatment of Premature Ejaculation define PE as a combination of (i) ejaculation usually occurring within about 1 minute of vaginal penetration (for lifelong PE) or a clinically significant reduction in latency time, often to around 3 minutes or less (for acquired PE); (ii) inability to delay ejaculation; and (iii) negative personal consequences such as distress, bother, frustration, and/or the avoidance of sexual intimacy [1]. PE is similarly defined by Diagnostic and Statistical Manual of Mental Disorders 5 (DSM 5) (2013) as ejaculation usually occurring within about 1 minute of vaginal penetration and before the individual wishes it and causing clinically significant distress [1]. Estimating the prevalence of PE is not straightforward due to the difficulty in defining what constitutes clinically relevant PE. Surveys have estimated the prevalence of Diagnostic and Statistical Manual of Mental Disorders IV-defined PE as 20–30% 2–4; however, these estimates are likely to include men who have some concern about their ejaculatory function but do not meet the current diagnostic criteria for PE [1]. It has been suggested that the prevalence of lifelong PE according to the ISSM and DSM-5 definitions (with an ejaculatory latency of about 1 minute) is unlikely to exceed 4% [1]. Men with PE are more likely to report lower levels of sexual functioning and satisfaction, and higher levels of personal distress and interpersonal difficulty, than men without PE [5]. They may also rate their overall quality of life as lower than that of men without PE [5]. In addition, their partner's satisfaction with the sexual relationship has been reported to decrease with increasing severity of the condition [6]. Management of PE may involve a range of interventions. These include systemic drug treatments (such as selective serotonin reuptake inhibitors, tricyclic antidepressants, phosphodiesterase type 5 inhibitors, and analgesics), topical anesthetic creams and sprays, and behavioral therapies (BTs) [7],[8].
Behavioral and psychological therapies for PE include two main classes of therapy, with overlapping elements [1]. The first consists of psychotherapy (such as psychosexual or relationship counselling) for men and/or couples, to address psychological and interpersonal issues that may be contributing to PE. The second consists of physical techniques to help men develop sexual skills to delay ejaculation and improve sexual self-confidence. Specific physical techniques include the following. The “stop-start” technique, developed by Semans, involves the man or his partner stimulating the penis until he feels the urge to ejaculate, then stopping until the sensation passes; this is repeated a few times before allowing ejaculation to occur [9]. The aim is to learn to recognize the feelings of arousal in order to improve control over ejaculation. With the related “squeeze” technique, proposed by Masters and Johnson, the man's partner stimulates the penis until he feels the urge to ejaculate, then squeezes the glans of the penis until the sensation passes; this is repeated before allowing ejaculation to occur [9]. Within sensate focus or sensate focusing [7], the man and his partner begin by focusing on touch, which excludes breasts, genitals, and intercourse, to encourage body awareness while reducing performance anxiety; this is followed by gradual reintroduction of genital touching and then full intercourse [10]. Pelvic floor muscle rehabilitation exercises may also assist with ejaculatory control [11].
The aim of this study was to systematically review the evidence base for BTs in the management of PE.
Methods
Review Methods
The review was undertaken in accordance with the general principles recommended in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement (http://www.prisma-statement.org/). The review protocol is available from the Health Technology Assessment Programme website (http://www.nets.nihr.ac.uk/projects/hta/131201).
Literature Searches
The following databases were searched up to August 2014: MEDLINE; Embase; Cumulative Index to Nursing and Allied Health Literature; The Cochrane Library including the Cochrane Systematic Reviews Database, Cochrane Controlled Trials Register, Database of Abstracts of Reviews of Effects and the Health Technology Assessment database; ISI Web of Science, including Science Citation Index, and the Conference Proceedings Citation Index-Science. The Medline search strategy is provided in Supplementary Appendix S1; it should be noted that the search was undertaken as part of a wider project assessing a variety of treatments for PE [12], and for this reason, the search was not specific to BTs. The U.S. Food and Drug Administration website and the European Medicines Agency website were also searched. Existing systematic reviews and relevant studies were also checked for eligible studies.
Eligibility Criteria
Randomized controlled trials (RCTs) in adult men with PE that evaluated BTs were eligible for inclusion. Studies comparing a BT against a waitlist control or against another therapy were eligible, as were studies comparing a combination of BT plus drug treatment against drug treatment alone. Studies were not included if the same BT was provided in both arms, as these were not considered to be assessing the effect of the BT (e.g., studies of drug plus behavioral treatment vs. behavioral alone). Theses and dissertations were not included. Non-English publications were included where sufficient data could be extracted from an English-language abstract or tables.
Outcomes
Relevant outcomes included intravaginal ejaculatory latency time (IELT), other measures of ejaculatory latency, and other outcomes such as sexual satisfaction, control over ejaculation, relationship satisfaction, self-esteem, quality of life, treatment acceptability, and adverse events.
Data Extraction and Synthesis
One reviewer performed data extraction of each study; all numerical data were then checked by a second reviewer. Where possible, data were presented as forest plots using Cochrane RevMan software (version 5.2; The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark) (RevMan 2014) [13].
Assessment of Methodological Quality of Studies
Methodological quality of included RCTs was assessed using the Cochrane Collaboration risk of bias assessment criteria [14]. Completeness of outcome data was considered low risk if the percentage of randomized participants excluded from the primary analysis was less than 30%. Selective reporting was considered low risk if IELT or ejaculatory latency was reported, and all outcomes referred to in the study methods were reported. Overall risk of bias for each study was classed as “low” or “high” if they were rated as such for each of three key domains: allocation concealment, blinding of outcome assessment, and completeness of outcome data; otherwise, overall risk of bias was classed as “unclear.”
Results
Quantity of Evidence
The searches identified 2,283 citations (as part of a wider project assessing a variety of treatments for PE). Eighteen full-text articles were obtained as potentially relevant. A total of 10 RCTs (521 randomized participants) evaluating a BT for PE were included in the review.
Characteristics of Included Studies
Details of the included study characteristics are presented in Table 1. As noted earlier, BTs for PE include two main types of therapy: first, psychotherapeutic or counseling approaches, and second physical techniques. Interestingly, this review identified only one RCT involving psychotherapy for PE: a Chinese study [19] in which one group received a combination of drug treatment (chlorpromazine) plus psychotherapy (to reduce anxiety, sadness, and negative thoughts and rebuild confidence) plus the stop-start technique, whereas the other group received chlorpromazine alone. All other included RCTs focused on physical techniques, either individually or in combination. The specific BTs that were evaluated included: the squeeze technique [22]; the stop-start technique [21],[23]; the stop-start and squeeze techniques [15]; the stop-start technique plus psychotherapy [19]; functional-sexological treatment involving education on sensuality, movement of the body, speed of sexual activity, muscular tension and breathing [15]; self-help material (covering squeeze technique, pause technique, and sensate focusing) with or without therapist phone contact [17]; sexual therapy for couples (sensate focus, stop-start technique, and communication exercises) [17]; pelvic floor muscle rehabilitation (awareness of muscle contraction) plus electrical stimulation of perineal floor [11]; squeeze technique, sensate focus, and Chinese traditional Qigong treatment (penis swinging and acupoint tapping) [20]; web-based sex therapy based on sensate-focus [18]; and the stop-start technique using a handheld vibrating stimulation device [16].
Table 1.
Study characteristics and risk of bias
| RCT Country Duration N randomized | Treatments (N randomized) | PE definition Lifelong/acquired | Risk of bias assessment | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Random sequence generation | Allocation concealment | Blinding of participants/personnel | Blinding of outcome assessment | Completeness of outcome data* | Selective reporting† | Overall risk‡ | |||
| Behavioral therapy vs. waitlist | |||||||||
| de Carufel and Trudel [15] Canada NR n = 36 couples |
|
IELT < 2 minutes NR | Unclear | Unclear | Not possible | Unclear | Unclear | Low | Unclear |
| Jern [16] Finland 6 weeks n = 11 |
|
NR Lifelong | Unclear | Unclear | Not possible | Unclear | Low | Low | Unclear |
| Trudel and Proulx [17] Canada 12 weeks n = 25 couples |
|
IELT ≤ 5 minutes NR | Unclear | Unclear | Not possible | Unclear | Unclear | Low | Unclear |
| van Lankveld et al. [18] Netherlands 12 weeks n = 40 |
|
NR NR | Low | Unclear | Not possible | Unclear | Low | Low | Unclear |
| Combined therapies vs. monotherapy | |||||||||
| Li et al. [19] China 6 weeks n = 90 |
|
IELT < 1 minute NR | Unclear in English language text | Unclear in English language text | Not possible | Unclear in English language text | Low | Low | Unclear |
| Shao and Li [20] China 8 weeks n = 120 |
|
NR NR | Unclear in English language text | Unclear in English language text | Not possible | Unclear in English language text | Low | Low | Unclear |
| Yuan et al. [21] China 6 weeks n = 96 |
|
NR NR | Unclear in English language text | Unclear in English language text | Not possible | Unclear in English language text | Low | Low | Unclear |
| Behavioral therapy vs. drug treatment | |||||||||
| Abdel-Hamid et al. [22] Egypt Crossover, 4 weeks each, 2-week washouts n = 31 |
|
IELT ≤ 2 minutes Lifelong | Unclear | Low | Not possible | Unclear | Low | Low | Unclear |
| Oguzhanglu et al. [23] Turkey 8 weeks N = 32 |
|
Ejaculation within several minutes Lifelong and acquired | Unclear | Unclear | Not possible | Unclear | Low | High | Unclear |
| Pastore et al. [11] Italy 12 weeks n = 40 |
|
ISSM definition PE Lifelong | Low | Unclear | Not possible | Unclear | Low | Low | Unclear |
CIPE-5 = Chinese Index of Premature Ejaculation-5; GRISS = Golombok Rust Inventory of Sexual Satisfaction; IELT = intravaginal ejaculatory latency time; ISSM = International Society for Sexual Medicine; NR = not reported; PE = premature ejaculation; RCT = randomized controlled trial.
Completeness of outcome data = low risk if <30% excluded from primary analysis.
Selective reporting = low risk if reported IELT/ejaculatory latency and all outcomes referred to in methods.
Overall risk of bias = “low” or “high” if rated as such for allocation concealment, blinding of outcome assessment, and completeness of outcome data.
Duration of the behavioral intervention in the included studies ranged from 2 to 12 weeks. Four studies compared one or more behavioral techniques with a waitlist control 15–18. Three further studies compared a BT with one or more drug treatments [11],[22],[23], whereas another three studies compared combined therapy (behavioral and drug) vs. drug treatment alone 19–21. Studies were conducted in a range of countries: three in China (published in Chinese language) 19–21, two in Canada [15],[17], and one each in Egypt [22], Turkey [23], Italy [11], the Netherlands [18], and Finland [16]. The definition of PE was an IELT of <1 minute in one study [19], ≤2 minutes in two studies [15],[22], ≤5 minutes in one study [17], defined according to the ISSM definition in one study [11], “before or within several minutes” in one study [23], and was not reported (or not available in the English language text) in four studies [16],[18],[20],[21]. Three studies reported that participants had lifelong PE [11],[16],[22], whereas in one study participants had lifelong or acquired PE [23]; for the remaining studies, this was not reported (or not available in the English language text). Of the 10 studies, one did not report IELT [23], whereas the remaining nine reported either IELT (in minutes) or another measure of ejaculatory latency (Table 2). Of these, four studies reported stopwatch-assessed IELT [11],[15],[16],[22]; three studies reported IELT in minutes, but the measurement method was not reported (or not available in English-language text) [17],[19],[21]; one study reported tendency to ejaculate too soon as measured via the Golombok Rust Inventory of Sexual Satisfaction (GRISS) PE subscale [18]; and one study reported ejaculatory latency as measured on the Chinese Index of Premature Ejaculation-5 (CIPE-5) five-point Likert scale [20].
Table 2.
Results for IELT and ejaculatory latency
| RCT Country Duration N randomized | Treatments (N randomized per group) | Outcome: IELT or ejaculatory latency | Results | Effect estimate (95% CI) | Significant difference? |
|---|---|---|---|---|---|
| Behavioral therapy vs. waitlist | |||||
| De Carufel and Trudel [15] Canada NR n = 36 couples |
|
IELT (stopwatch) | Posttreatment mean (minutes):
|
BT vs. waitlist (posttreatment):
|
Yes (favors BT groups) |
| Jern [16] Finland 6 weeks n = 11 |
|
IELT (stopwatch) | Posttreatment mean (mins):
|
BT vs. waitlist (posttreatment):
|
No (but improved from baseline) |
| Trudel and Proulx [17] Canada 12 weeks n = 25 couples |
|
IELT (method NR) | Posttreatment mean (mins):
|
BT vs. waitlist:
|
Yes (favors BT groups) |
| (No SDs reported) | Significant change baseline to posttreatment, BT (P < 0.01) but not waitlist (P = NS). Changes (BT) maintained at 3-month follow-up | ||||
| van Lankveld et al. [18] Netherlands 12 weeks n = 40 |
|
Tendency to ejaculate too soon (GRISS-PE subscale) | Posttreatment mean (GRISS-PE):
|
BT vs. waitlist: MD = −0.20 (−1.75 to 1.35), P = 0.80) | No (but improved from baseline) |
3-month follow-up (GRISS-PE):
|
Significant change from baseline (P < 0.001, both groups). Change in sex therapy group maintained at 3- and 6-month follow-up | ||||
| Behavioral + drug therapies vs. drug alone | |||||
| Li et al. [19] China 6 weeks n = 90 |
|
IELT (method NR) | Posttreatment mean (mins):
|
Combined vs. drug: MD = 1.11 (0.86–1.36), P < 0.0001 | Yes (favors combined) |
| Shao and Li [20] China 8 weeks n = 80 for this comparison |
|
Ejaculatory latency (CIPE-5, five-point scale, higher = improved) | Posttreatment mean (CIPE-5):
|
Combined vs. drug: MD = 0.40 (0.18–0.62), P = 0.0003 | Yes (favors combined) |
| Yuan et al. [21] China 6 weeks n = 64 for this comparison |
|
IELT (method NR) | Post-treatment mean (mins):
|
Combined vs. drug: MD = 0.46 (0.04–0.88), P = 0.03 | Yes (favors combined) |
| Behavioral therapy vs. drug treatment | |||||
| Abdel-Hamid et al. [22] Egypt Crossover, 4 weeks each, 2-week washouts n = 31 |
|
IELT (stopwatch) | Posttreatment, median (mins):
|
Favors sildenafil or paroxetine vs. pause-squeeze; other comparisons not significant (no further data) | Yes (favors drug for 2 of 4 drugs) |
| Pastore et al. [11] Italy 12 weeks n = 40 |
|
IELT (stopwatch) | Posttreatment, geometric mean (mins):
|
BT vs. drug: MD = −1.22 (−1.65 to −0.79), P < 0.00001 | Yes (favors drug) |
| Shao and Li [20] China 8 weeks n = 80 for this comparison |
|
Ejaculatory latency (CIPE-5, five-point scale, higher = improved) | Post-treatment mean (CIPE-5):
|
BT vs. drug: MD = −0.20 (−0.40 to 0.00), P = 0.05 | Yes (favors drug) |
| Yuan et al. [21] China 2 weeks n = 64 for this comparison |
|
IELT (method NR) | Posttreatment mean (mins):
|
BT vs. drug: MD = −3.55 (−3.88 to −3.22), P < 0.00001) | Yes (favors drug) |
BT = behavioral therapy; CI = confidence interval; CIPE-5 = Chinese Index of Premature Ejaculation-5; FS = functional-sexological therapy; GRISS = Golombok Rust Inventory of Sexual Satisfaction; IELT = intra-vaginal ejaculatory latency time; MD = mean difference; NR = not reported; PE = premature ejaculation; RCT = randomized controlled trial; RR = relative risk; SD = standard deviation.
Risk of Bias in Included Studies
The risk of bias within included studies is shown in Table 1. All 10 studies were classed as overall unclear risk of bias due to limited reporting of methodological details (three studies 19–21 were reported in Chinese, and some details were unavailable from the English language text). In total, eight studies 15–17,19–23 were unclear in terms of randomization sequence generation and nine 11,15–21,23 were unclear in terms of allocation concealment. Due to the nature of the interventions, blinding of participants and personnel was not possible in any study. Blinding of outcome assessment was unclear in all studies. Eight studies 11,16,18–23 were considered at low risk of bias for completeness of outcome data (<30% excluded from primary analysis), whereas two [15],[17] were unclear on this point. All studies scored low for selective reporting (based on the fact that they reported IELT or ejaculatory latency as well as all outcomes referred to in the methods sections), with the exception of one study [23] that did not report IELT or ejaculatory latency.
Assessment of Effectiveness: IELT and Ejaculatory Latency
BT vs. Waitlist
Four studies assessed BTs vs. waitlist control 15–18. Two significantly favored BTs in terms of IELT, whereas one showed no difference on another measure of ejaculatory latency (Table 2; Figures 3).
Figure 3.
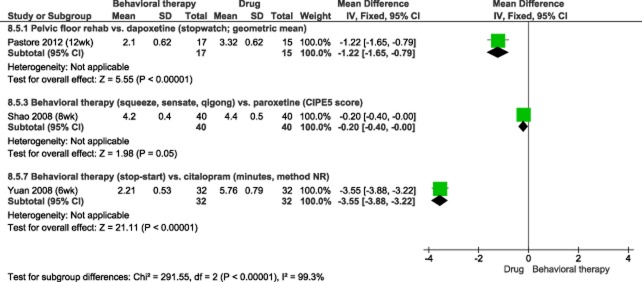
Behavioral therapy vs. drug treatment: IELT and ejaculatory latency
Functional-Sexological Treatment or Squeeze/Stop-Start vs. Waitlist
A study by de Carufel and Trudel (2006; n = 36 couples) [15] assessed two types of BT vs. waitlist control: functional-sexological therapy (FS, involving education on sensuality, movement of the body, speed of sexual activity, muscular tension and breathing) and BT (involving the squeeze and stop-start techniques). Duration of treatment was not reported. Both treatments improved stopwatch-measured IELT significantly more than waitlist at posttreatment, by almost 7 minutes (Table 2; Figure 1). Follow-up data 3 months posttreatment was available for the FS and BT groups (though not for waitlist); in both groups, the significant change in IELT from baseline to posttreatment remained significant 3 months after treatment cessation.
Figure 1.
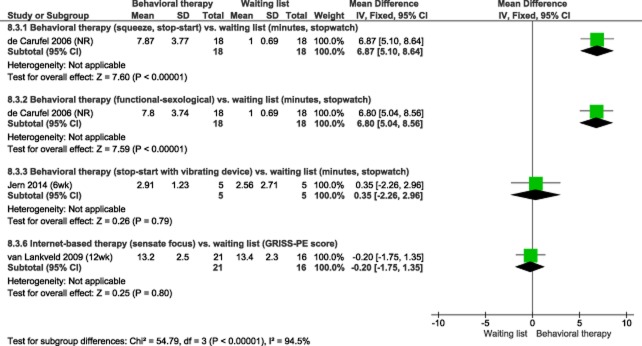
Behavioral therapies vs. waitlist: IELT and ejaculatory latency
Stop-Start Using Handheld Device vs. Waitlist
A small study by Jern (n = 11 participants) [16] assessed the stop-start technique aided by a handheld vibrating stimulation device vs. waitlist control. Participants used the device, alone or with a partner, three times per week for 6 weeks. After 6 weeks, ejaculatory latency improved slightly more in the treatment group (improvement of 1.6 minutes; P = 0.019 for change from baseline) than in the waitlist group (0.9 minutes; P = 0.075 for change); however, the posttreatment scores were not significantly different (mean difference [MD] 0.35 minutes, 95% confidence interval [CI] −2.26 to 2.96; P = 0.79; Table 2 and Figure 1). At follow-up 6 months after all patients undertook treatment, IELT had improved by 1.7 minutes from baseline (P = 0.008 for change).
Self-Help Book with/Without Therapist Contact or Couples' Sexual Therapy vs. Waitlist
A further RCT by Trudel and Proulx (n = 25 couples) [17] assessed three types of BT vs. waitlist control: self-help book alone (described as bibliotherapy); self-help book plus therapist phone contact; and sexual therapy for couples. After 12 weeks, all gave improvements in IELT of between 7 and 9 minutes over that of the waitlist group, though the method of IELT measurement was not stated, with changes from baseline significant for all treatment groups (P < 0.01) but not for the waitlist group (P value not reported; Table 2). These data could not be presented on the forest plot as no standard deviations were reported. Changes from baseline in the treatment groups remained significant 3 and 6 months after treatment cessation.
Web-Based Sex Therapy vs. Waitlist
A third RCT by van Lankveld et al. [18] (n = 40 participants) assessed web-based sex therapy (using sensate focus) vs. waitlist. The GRISS-PE subscale was used to measure the extent to which a man has the tendency to ejaculate too soon. There was almost no difference between groups at 12 weeks (score of 13 in both groups; P = 0.80; Table 2 and Figure 1). Both groups improved from baseline (P < 0.001), and the change in the sex therapy group remained significant at 3 and 6 months after treatment cessation (no follow-up data were available for waitlist).
Combined Behavioral and Drug Therapy vs. Drug Alone
Three studies compared behavioral and drug combination therapy vs. drug treatment alone; all showed small but significant differences in IELT or ejaculatory latency favoring the combined approach 19–21.
BT Plus Chlorpromazine vs. Chlorpromazine
One RCT by Li et al. (n = 90 participants) [19] assessed combined therapy (BT plus chlorpromazine, a dopamine antagonist; 50 mg/day) vs. chlorpromazine alone. BT consisted of the stop-start technique plus psychotherapy (to reduce anxiety, sadness, and negative thoughts and rebuild confidence). Combined therapy gave a greater increase in IELT at 6 weeks, though the difference was only 1 minute, and the measurement method was not reported (MD 1.11 minutes, 95% CI 0.86 to 1.36; P < 0.00001; Table 2 and Figure 2).
Figure 2.
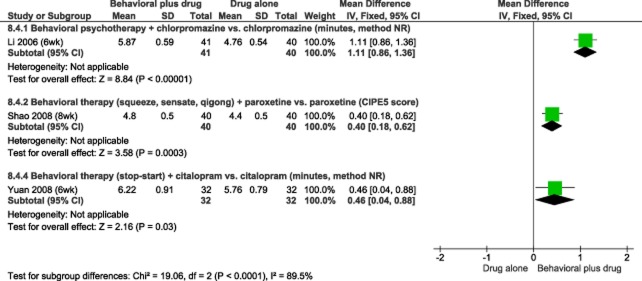
Behavioral plus drug therapy vs. drug alone: IELT and ejaculatory latency
BT Plus Paroxetine vs. Paroxetine
Another RCT by Shao et al. (n = 80 participants for this comparison) [20] assessed BT plus paroxetine (a selective serotonin reuptake inhibitor [SSRI]) vs. paroxetine alone. BT included squeeze technique, sensate focus, Qigong and acupoint tapping and was provided for 8 weeks. The paroxetine dose was 10 mg/day for 4 weeks in the combined therapy group and 20 mg/day for 8 weeks in the paroxetine-only group. Combined therapy was superior to paroxetine alone in increasing ejaculatory latency at 8 weeks as measured on a five-point Likert scale via the CIPE-5, though the difference was small (MD 0.40, 95% CI 0.18 to 0.62; P = 0.0003; Table 2 and Figure 2).
BT Plus Citalopram vs. Citalopram
A further RCT by Yuan et al. (n = 64 participants for this comparison) [21] reported that BT (stop-start technique) plus citalopram (an SSRI; 20 mg/day) was superior to citalopram alone in increasing IELT at 6 weeks, though the IELT difference was only 0.5 minutes, and the measurement method was not reported (MD 0.46 minutes, 95% CI 0.04 to 0.88; P = 0.03; Table 2 and Figure 2).
BT vs. Drug Treatment
Four studies compared BT alone vs. drug treatment alone; all showed small but significant differences in IELT or ejaculatory latency favoring drug treatment 11,20–22.
Pelvic Floor Rehabilitation vs. Dapoxetine
One RCT by Pastore et al. (n = 40 participants) [11] compared pelvic floor rehabilitation (plus electrical stimulation of the perineum) vs. dapoxetine (an SSRI, 30 or 60 mg taken prior to intercourse). The between-group difference in geometric mean stopwatch-assessed IELT at 12 weeks was 1.22 minutes in favor of dapoxetine (MD 1.22, 95% CI 0.79 to 1.65; P < 0.0001; Table 2 and Figure 3).
BT vs. Paroxetine
The RCT by Shao et al. (n = 80 participants for this comparison) [20] compared paroxetine (20 mg/day) against BT (squeeze technique, sensate focus, Qigong and acupoint tapping). The between-group difference in the CIPE-5 ejaculatory latency score at 8 weeks significantly favored paroxetine (MD 0.20, 95% CI 0.00 to 0.40; P = 0.05; Table 2 and Figure 3).
BT vs. Citalopram
The RCT by Yuan et al. (n = 64 participants for this comparison) [21] reported a between-group difference in IELT at 6 weeks of 3.55 minutes in favor of citalopram (20 mg/day) compared with BT (stop-start technique); MD 3.55, 95% CI 3.22 to 3.88; P < 0.00001; Table 2 and Figure 3). The measurement method was not reported.
Squeeze Technique vs. SSRIs or Tricyclic Antidepressants (TCA)
The between-group difference in median stopwatch-measured IELT following a 4-week randomized crossover comparison (Abdel-Hamid et al.; n = 31 participants) [22] significantly favored sildenafil or paroxetine over BT (pause-squeeze technique), whereas comparisons with sertraline and clomipramine were not significant (Table 2). Data were not presented on the forest plot due to the reporting of median rather than mean values.
Assessment of Effectiveness: Non-IELT Outcomes
With the exception of the RCT by Pastore et al. [24], all of the included trials were reported as evaluating one or more outcomes other than IELT (Table 3). However, these were diverse across the included trials and were not reported in sufficient detail to permit any pooling across trials.
Table 3.
Results for outcomes other than IELT
| RCT Country Duration N randomized | Treatments (N randomized per group) | Outcome measure | Results | Significant difference? |
|---|---|---|---|---|
| Behavioral therapy vs. waitlist | ||||
| De Carufel and Trudel [15] Canada NR n = 36 couples |
|
Sexual satisfaction (Hudson's index) | Both treatment groups had significant improvements over waitlist (men and partners) | Yes (favors BT groups) |
| Perception of duration of intercourse | Improved significantly with both treatments (men; P < 0.05) but not waitlist | Yes (favors BT groups) | ||
| Jern [16] Finland 6 weeks n = 11 |
|
Ejaculatory control, latency, relationship problems (CHEES) | Posttreatment, no significant between-group difference or change from baseline | No (also no improvement from baseline) |
| At 6 months, significant improvement from baseline after all patients undertook BT (P = 0.006) | Significant improvement from baseline | |||
| Trudel and Proulx [17] Canada 12 weeks n = 25 couples |
|
Sexual satisfaction (SII) | Improved in all three treatment groups for men and partners (P < 0.05); no data for waitlist group | Unclear (BT vs. waitlist) |
| Self-help book + phone contact better than self-help book alone (P < 0.05) | Better with phone contact | |||
| van Lankveld et al. [18] Netherlands 12 weeks n = 40 |
|
Sexual desire (IIEF) | Favored sex therapy vs. waitlist (P < 0.05). Improved from baseline across groups (P < 0.05); maintained at 3- and 6-month follow-up | Yes (also improved from baseline) |
| Overall satisfaction (IIEF) | No between-group difference. Improved from baseline across groups (P = 0.005); maintained at 3- and 6-month follow-up | No (both groups improved from baseline) | ||
| Self-confidence (SEAR) | No between-group difference. No significant change from baseline to post-treatment | No (also no improvement from baseline) | ||
| Behavioral + drug therapies vs. drug alone | ||||
| Li et al. [19] China 6 weeks n = 90 |
|
Sexual satisfaction (patient & partner), ejaculatory control, ejaculatory latency (CIPE) | Chlorpromazine + BT superior to chlorpromazine alone for all outcomes (P < 0.05) | Yes (favors combined) |
| Anxiety (SAS and CIPE) | Chlorpromazine + BT superior to chlorpromazine alone (CIPE P < 0.05, SAS P < 0.01) | Yes (favors combined) | ||
| Shao and Li [20] China 8 weeks n = 80 for this comparison |
|
Ejaculatory control (CIPE-5) | BT + paroxetine better than paroxetine (P < 0.01) | Yes (favors combined) |
| Patient/partner satisfaction (CIPE-5) | BT + paroxetine better than paroxetine (P < 0.05) | Yes (favors combined) | ||
| Sexual anxiety (CIPE-5) | BT + paroxetine better than paroxetine (P < 0.01) | Yes (favors combined) | ||
| Yuan et al. [21] China 2 weeks n = 64 for this comparison |
|
Sexual satisfaction (measure NR) | Favored BT + citalopram vs. citalopram alone (P = NR) | Unclear |
| Behavioral therapy vs. drug treatment | ||||
| Abdel-Hamid et al. [22] Egypt Crossover, 4 weeks each, 2-week washouts n = 31 |
|
Sexual satisfaction (modified EDITS) | Medians: squeeze technique, 6; clomipramine, 11; sertraline, 10 sildenafil, 30; paroxetine, 12 | Yes (sildenafil or paroxetine superior to BT; others not significant) |
| Anxiety (AAI, scale 0 to 30) | Medians: squeeze technique, 12; clomipramine, 11; sertraline, 11; sildenafil, 8; paroxetine, 9 | No | ||
| Oguzhanglu et al. [23] Turkey 8 weeks N = 32 |
|
Sexual satisfaction (latency and control in 75% coitus) | No difference between groups (P > 0.05); significantly improved in both groups | No (improved from baseline) |
| Anxiety (STAI) | Anxiety (state and trait) improved from baseline in both groups (P < 0.05) | No (improved from baseline) | ||
| Pastore et al. [11] Italy 12 weeks n = 40 |
|
No other outcomes reported | — | — |
| Shao and Li [20] China 8 weeks n = 80 for this comparison |
|
Ejaculatory control (CIPE-5) | Paroxetine better than BT (P < 0.01) | Yes (favors drug) |
| Patient/partner satisfaction (CIPE-5) | BT better than paroxetine (P < 0.01) | Yes (favors BT) | ||
| Sexual anxiety (CIPE-5) | BT vs. paroxetine, P = nonsignificant (value NR) | No difference | ||
| Yuan et al. [21] China 2 weeks n = 64 |
|
Sexual satisfaction (measure NR) | Citalopram significantly superior to BT (P = 0.015) | Yes (favors drug) |
AAI = Arabic Anxiety Inventory; BT = behavioral therapy; CHEES = Checklist for Early Ejaculation Symptoms; CIPE-5 = Chinese Index of Premature Ejaculation-5; EDITS = Erectile Dysfunction Inventory of Treatment Satisfaction; IIEF = International Index of Erectile Function; NR = not reported; RCT = randomized controlled trial; SAS = Self-rating Anxiety Scale; SEAR = Self-Esteem and Relationship; SII = Sexual Interaction Inventory; STAI = State-Trait Anxiety Index.
BT vs. Waitlist Control
Four RCTs assessed non-IELT outcomes for BTs vs. waitlist control; one significantly favored BTs [15], whereas the other two were unclear as to whether there was a significant difference between groups 16–18. One RCT (de Carufel and Trudel) [15] showed significant improvements in male perception of duration of intercourse and couples' sexual satisfaction with either functional sexological treatment (sensual education) or BT (stop-start technique and squeeze technique) compared with waitlist control. Another RCT (Trudel and Proulx) [17] reported a significant increase from baseline in sexual satisfaction for all three BT groups (self-help book, self-help book plus therapist phone contact, and sexual therapy) with better results for self-help plus phone contact vs. self-help alone; however, no data were reported for the waitlist group. A further RCT (van Lankveld et al.) [18] reported that sexual desire improved significantly more with web-based sensate focus than waitlist control, whereas sexual satisfaction improved from baseline but showed no significant difference between groups; conversely, self-confidence showed no significant difference either between groups or from baseline. A small RCT using the stop-start technique aided by a handheld stimulation device (Jern) [16] showed no significant improvement over waitlist or from baseline post-treatment (via a composite score for ejaculatory latency, control and relationship problems); however, a significant improvement from baseline was observed at 6-month follow-up (at which point all patients had received treatment so there was no waitlist comparison).
Combined Behavioral + Drug Therapy vs. Drug Alone
Three RCTs reported better results for combined therapy (behavioral plus drug) than drug treatment alone on a range of non-IELT outcomes 19–21. BT (stop-start plus psychotherapy) combined with chlorpromazine was reported by one RCT as being more effective than chlorpromazine alone on a self-rated measure of anxiety and CIPE measures of sexual anxiety, sexual satisfaction, and ejaculatory control (Li et al.) [19]. Another RCT (Shao et al.) [20] reported that combined treatment with paroxetine plus BT (squeeze, sensate focus, Qigong and acupoint tapping) was superior to paroxetine alone on CIPE measures of ejaculatory control, patient/partner satisfaction, and sexual anxiety. A further RCT (Yuan et al.) [21] reported that BT (stop-start technique) combined with citalopram was more effective at improving sexual satisfaction than citalopram alone, though significance level was not reported.
BT vs. Drug Treatment
Four RCTs 20–23 comparing BTs vs. drug treatment reported non-IELT outcomes, with mixed results (some outcomes favoring drug treatment, some behavioral, and some showing no difference). One RCT (Shao et al.) [20] reported mixed results; results for CIPE-assessed ejaculatory control significantly favored paroxetine over BT, whereas results for patient/partner satisfaction significantly favored BT, and there was no significant difference in sexual anxiety. Yuan et al. [21] reported that citalopram significantly improved sexual satisfaction compared with BT (stop-start). Oguzhanglu et al. [23] reported no significant between-group difference in sexual satisfaction for stop-start technique compared with fluoxetine (though both groups improved from baseline). A crossover RCT (Abdel-Hamid et al.) [22] reported significantly better sexual satisfaction with sildenafil or paroxetine compared with the squeeze technique but no significant differences compared with clomipramine or sertraline, whereas anxiety was not significantly different between groups.
Assessment of Adverse Effects and Withdrawals from Treatment
Adverse effect data were available for six of 10 studies [11],[16],[17],[20],[22],[23]. None reported any adverse effects for BTs. One study (Trudel and Proulx) [17] reported that dropout rates from treatment were higher for the group receiving self-help material alone (45%) than for the two groups with therapist contact (14% and 33%; unclear which data relate to which of the two therapist-contact groups). Adverse event rates reported for groups receiving drug treatment or combined drug and behavioral treatment were as follows: 10% for paroxetine 10 mg/day (plus BT) [20]; 40% for paroxetine 20 mg/day [20]; 17% for paroxetine 20 mg taken pre-coitus [22]; 10% for sertraline 50 mg pre-coitus [22], 13% for fluoxetine [23]; 13% for dapoxetine 30 mg pre-coitus [11]; 29% for dapoxetine 60 mg pre-coitus [11]; 25% for clomipramine 25 mg pre-coitus [22]; and 18% for sildenafil 50 mg pre-coitus [22]. Where reported, adverse effects of SSRIs included nausea, diarrhea, dry mouth, anorexia, drowsiness, and yawning [11],[22],[23], whereas adverse effects of sildenafil (phosphodiesterase type 5 inhibitors) included headache, flushing, and nasal congestion [22].
Summary of Effectiveness Results
The effectiveness results across trials are summarized in Table 4. Four trials compared BTs against waitlist 15–18. Of these, two trials assessing five types of BT reported posttreatment differences in IELT of 7–9 minutes compared with the waitlist groups, with changes in the treatment groups maintained 3 months after treatment cessation [15],[17]. However, a further trial showed no difference in ejaculatory latency via the GRISS-PE scale between web-based sensate focus and waitlist, though both groups improved from baseline [18]. Another trial showed no posttreatment difference in IELT between the stop-start technique aided by a stimulation device vs. waitlist, though there was a significant improvement from baseline at 6-month follow-up [16]. Results were mixed for other outcomes (sexual satisfaction, desire, and self-confidence), with some waitlist comparisons significantly favoring BT while others were not significant 15–18.
Table 4.
Summary of results
| Outcome | RCTs | N ptps | Intervention | Comparator | Mean diff. (95% CI), P value | Favors |
|---|---|---|---|---|---|---|
| Behavioral therapy vs. waitlist | ||||||
| IELT (minutes) | de Carufel and Trudel [15] | 36 | BT (squeeze, stop-start) | Waitlist | 6.87 (5.10 to 8.64), P < 0.00001 | BT |
| BT (FS) | Waitlist | 6.80 (5.04 to 8.56), P < 0.00001 | BT | |||
| Trudel and Proulx [17] | 25 | BT (self-help) | Waitlist | 9.11 (NR) | BT | |
| BT (self-help + phone) | Waitlist | 7.29 (NR) | BT | |||
| BT (couples therapy) | Waitlist | 8.84 (NR) | BT | |||
| Jern [16] | 11 | BT (stop-start + device) | Waitlist | 0.35 (−2.26 to 2.96), P = 0.79 | Not significant | |
| Ejaculatory latency (GRISS-PE) | van Lankveld et al. [18] | 40 | BT (web-based sensate focus) | Waitlist | −0.20 (−1.75 to 1.35), p=0.80 | Not significant |
| Sexual satisfaction | de Carufel and Trudel [15] | 36 | BT (two types; see above) | Waitlist | P = NR | BT |
| Trudel and Proulx [17] | 25 | BT (three types; see above) | Waitlist | P = NR | Unclear | |
| van Lankveld et al. [18] | 40 | BT (web-based sensate focus) | Waitlist | P = NR | Not significant | |
| Perception of duration | de Carufel and Trudel [15] | 36 | BT (two types; see above) | Waitlist | P < 0.05 | BT |
| Sexual desire | van Lankveld et al. [18] | 40 | BT (web-based sensate focus) | Waitlist | P < 0.05 | BT |
| Self-confidence | van Lankveld et al. [18] | 40 | BT (web-based sensate focus) | Waitlist | P = NR | Not significant |
| Ejaculatory control, latency, problems | Jern [16] | 11 | BT (stop-start + device) | Waitlist | P = NR | Not significant |
| Behavioral + drug therapies vs. drug alone | ||||||
| IELT (minutes) | Li et al. [19] | 90 | BT (PS + SS) + chlorpromazine | Chlorpromazine | 1.11 (0.86 to 1.36), P < 0.0001 | BT + drug |
| Yuan et al. [21] | 64 | BT (stop-start) + citalopram | Citalopram | 0.46 (0.04 to 0.88), P = 0.03 | BT + drug | |
| Ejaculatory latency (CIPE-5) | Li et al. [19] | 90 | BT (PS + SS) + chlorpromazine | Chlorpromazine | P < 0.05 | BT + drug |
| Shao and Li [20] | 80 | BT (various) + paroxetine | Paroxetine | 0.46 (0.04 to 0.88), P = 0.03 | BT + drug | |
| Sexual satisfaction | Li et al. [19] | 90 | BT (PS + SS) + chlorpromazine | Chlorpromazine | P < 0.05 | BT + drug |
| Shao and Li [20] | 80 | BT (various) + paroxetine | Paroxetine | P < 0.05 | BT + drug | |
| Yuan et al. [21] | 64 | BT (stop-start) + citalopram | Citalopram | P = NR (states favors BT + drug) | Unclear | |
| Ejaculatory control | Li et al. [19] | 90 | BT (PS + SS) + chlorpromazine | Chlorpromazine | P < 0.05 | BT + drug |
| Shao and Li [20] | 80 | BT (various) + paroxetine | Paroxetine | P < 0.01 | BT + drug | |
| Anxiety | Li et al. [19] | 90 | BT (PS + SS) + chlorpromazine | Chlorpromazine | P < 0.05 | BT + drug |
| Shao and Li [20] | 80 | BT (various) + paroxetine | Paroxetine | P < 0.01 | BT + drug | |
| Behavioral therapy vs. drug treatment | ||||||
| IELT (minutes) | Abdel-Hamid et al. [22] | 31 | BT (squeeze) | Paroxetine | Not reported | Drug |
| Sertraline | Not significant | |||||
| Clomipramine | Not significant | |||||
| Sildenafil | Drug | |||||
| Pastore et al. [11] | 40 | BT (pelvic floor) | Dapoxetine | −1.22 (−1.65 to −0.79), P < 0.00001 | Drug | |
| Yuan et al. [21] | 64 | BT (stop-start) | Citalopram | −3.55 (−3.88 to −3.22), P < 0.00001 | Drug | |
| Ejaculatory latency (CIPE-5) | Shao and Li [20] | 80 | BT (various) | Paroxetine | −0.20 (−0.40 to 0.00), p=0.05 | Drug |
| Sexual satisfaction | Abdel-Hamid et al. [22] | 31 | BT (squeeze) | Paroxetine | Not reported | Drug |
| Sertraline | Not significant | |||||
| Clomipramine | Not significant | |||||
| Sildenafil | Drug | |||||
| Oguzhanglu et al. [23] | 32 | BT (stop-start) | Fluoxetine | P > 0.05 | Not significant | |
| Shao and Li [20] | 80 | BT (various) | Paroxetine | P < 0.01 | BT | |
| Yuan et al. [21] | 64 | BT (stop-start) | Citalopram | P = 0.015 | Drug | |
| Ejaculatory control | Shao and Li [20] | 80 | BT (various) | Paroxetine | P < 0.01 | Drug |
| Anxiety | Abdel-Hamid et al. [22] | 31 | BT (squeeze) | See above | Not reported | Not significant |
| Oguzhanglu et al. [23] | 32 | BT (stop-start) | Fluoxetine | Not reported | Not significant | |
| Shao and Li [20] | 80 | BT (various) | Paroxetine | P = NR | Not significant | |
BT = behavioral therapy; CI = confidence interval; CIPE-5 = Chinese Index of Premature Ejaculation-5; FS = functional-sexological; GRISS = Golombok Rust Inventory of Sexual Satisfaction; IELT = intra-vaginal ejaculatory latency time; MD = mean difference; NR = not reported; NS = nonsignificant; PE = premature ejaculation; PS = psychotherapy; RCT = randomized controlled trial; RR = risk ratio; SS = stop-start.
Three trials favored combined behavioral and drug treatment over drug treatment alone 19–21, with small but significant differences in IELT favoring combined treatment (0.5–1 minute across two trials) [19],[21] and significantly better results for combined treatment on other outcomes (sexual satisfaction, ejaculatory control, and anxiety) 19–21. Direct comparisons of BT alone or drug treatment alone gave mixed results both for IELT and other outcomes, with most findings either favoring drug treatment or showing no significant difference.
Discussion
This systematic review assesses the effectiveness of BTs for the treatment of PE, based on RCT evidence. Ten trials were identified; these were conducted across various countries and the overall risk of bias was unclear in all studies. The included studies assessed various types of BT either individually or in combination, including the squeeze and stop-start techniques, stop-start aided by a stimulation device, education on sensuality and movement, sensate focus, and pelvic floor muscle rehabilitation. All the above showed some evidence of effectiveness either over waitlist or as an addition to drug treatment. No adverse effects were reported for BTs, though these were not well reported across trials. There were generally only one or two trials of each specific type of therapy, which limits the conclusions that can be drawn. Results of two trials each comparing either two or three different types of BT indicated that all were similarly effective [15],[17]. Only one RCT, Li et al. [19], included a psychotherapeutic approach, comparing chlorpromazine plus the stop-start technique plus psychotherapy against chlorpromazine alone. The effectiveness of psychotherapy in this study was unclear due to the combined intervention and the use of an active control. All remaining RCTs focused on physical techniques as outlined above. Indeed, current PE guidelines note that the majority of psychotherapy studies are uncontrolled and nonblinded [1]. Therefore, there remains a need for well-conducted RCTs of psychotherapeutic approaches to PE. Study treatments were relatively well-described in most studies, though some simply referred to an established technique (such as stop-start or sensate focus). Three of the included studies were in Chinese language. This review used robust methodology including thorough literature searching and data checking by two reviewers. Non-RCT studies were not included within this review as these were considered to be of lower methodological quality and would have provided limited information on effectiveness. Duration of the behavioral interventions in the included studies ranged from 2 to 12 weeks. Three studies reported that IELT improvements were maintained 3–6 months after treatment cessation; however, in general, there is limited data regarding how long any positive effects would be maintained after treatment finishes and whether additional follow-up treatments might be required. This is a consideration both for BTs and for drug treatments within PE studies. The majority of RCTs included an assessment of either IELT or another measure of ejaculatory latency, though the method of IELT measurement (e.g., via stopwatch) was not always reported. Many RCTs also reported other outcomes such as ejaculatory control, sexual satisfaction, and anxiety, though various different measures were used to assess these, and data were not always clearly reported. It is important that clinical studies aim to assess non-IELT aspects of PE, as highlighted in the recently updated ISSM definition of PE, which includes inability to delay ejaculation and negative personal consequences in addition to reduced latency time [1]. In comparison with a pharmacological treatment, most BTs require a willingness of the man and his partner to engage with the therapy and practice the relevant techniques. The suitability of a BT is likely to depend on individual patient (and partner) preference; some people may prefer a behavioral option, whereas others may prefer a pharmacological approach. Combinations of medical and psychological approaches may be useful where there is a clear psychosocial or relationship issue [1]. In order to increase consistency in outcome data and facilitate meta-analyses, future studies should aim to recruit men meeting the ISSM definition of PE, measure stopwatch-assessed IELT, and report other aspects of PE in addition to IELT using validated instruments. Further research may focus on psychotherapeutic or counseling approaches for PE, for which few RCTs were identified in the current evidence base. Combination therapy may also be worthy of further study; this may include combinations of physical techniques and counseling approaches, and/or behavioral and drug treatments. Additional areas for further study may include assessment of differences between types of BT, optimum duration of therapy, and how effects might best be maintained long-term.
Conclusions
There is limited evidence that physical behavioral techniques for PE improve IELT and other outcomes over waitlist control. There is also some evidence that BTs combined with drug treatments improve IELT and other outcomes compared with drug treatments alone. Areas for further research might include: RCTs of psychotherapeutic or counseling approaches to PE; further studies of combination therapy (physical/behavioral and/or counseling and/or drug); and assessment of how effects of therapy might be maintained long-term.
Acknowledgments
Thanks to Shijie Ren for translation of articles.
Conflict of Interest
No conflicts of interest occurred for any author.
Funding
This work was funded by the UK National Institute for Health Research (NIHR) Health Technology Assessment (HTA) Programme, project number 13-12.
Supporting Information
Appendix S1 Medline search strategy (August 2014).
References
- Althof SE, McMahon CG, Waldinger MD, Serefoglu EC, Shindel AW, Adaikan PG, Becher E, Dean J, Giuliano F, Hellstrom WJ, Giraldi A, Glina S, Incrocci L, Jannini E, McCabe M, Parish S, Rowland D, Segraves RT, Sharlip I, Torres LO. An update of the International Society of Sexual Medicine's guidelines for the diagnosis and treatment of premature ejaculation (PE) J Sex Med. 2014;11:1392–1422. doi: 10.1111/jsm.12504. [DOI] [PubMed] [Google Scholar]
- Laumann EO, Nicolosi A, Glasser DB, Paik A, Gingell C, Moreira ED, Wang T GSSAB Investigators' Group. Sexual problems among women and men aged 40–80 y: Prevalence and correlates identified in the Global Study of Sexual Attitudes and Behaviors. Int J Impot Res. 2005;17:39–57. doi: 10.1038/sj.ijir.3901250. [DOI] [PubMed] [Google Scholar]
- Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: Prevalence and predictors. J Am Med Assoc. 1999;281:537–544. doi: 10.1001/jama.281.6.537. [DOI] [PubMed] [Google Scholar]
- Porst H, Montorsi F, Rosen RC, Gaynor L, Grupe S, Alexander J. The Premature Ejaculation Prevalence and Attitudes (PEPA) survey: Prevalence, comorbidities, and professional help-seeking. Eur Urol. 2013;51:816–823. doi: 10.1016/j.eururo.2006.07.004. [DOI] [PubMed] [Google Scholar]
- Rowland DL, Patrick DL, Rothman M, Gagnon DD. The psychological burden of premature ejaculation. J Urol. 2007;177:1065–1070. doi: 10.1016/j.juro.2006.10.025. [DOI] [PubMed] [Google Scholar]
- Byers ES, Grenier G. Premature or rapid ejaculation: Heterosexual couples' perceptions of men's ejaculatory behavior. Arch Sex Behav. 2003;32:261–270. doi: 10.1023/a:1023417718557. [DOI] [PubMed] [Google Scholar]
- Richardson D, Goldmeier D, Green J, Lamba H, Harris JRW. Recommendations for the management of premature ejaculation: BASHH Special Interest Group for Sexual Dysfunction. Int J STD AIDS. 2006;17:1–6. doi: 10.1258/095646206775220540. [DOI] [PubMed] [Google Scholar]
- Wespes E, Eardley I, Giuliano F, Hatzichristou D, Hatzimouratidis K, Moncada I, Salonia A, Vardi Y. Guidelines on male sexual dysfunction: Erectile dysfunction and premature ejaculation. Arnhem, the Netherlands: European Association of Urology; 2013. [DOI] [PubMed] [Google Scholar]
- Melnik T, Althof S, Atallah AN, Puga MEDS, Glina S, Riera R. Psychosocial interventions for premature ejaculation. Cochrane Database Syst Rev. 2011;(8) doi: 10.1002/14651858.CD008195.pub2. CD008195. [DOI] [PubMed] [Google Scholar]
- McMahon CG, Abdo C, Incrocci L, Perelman M, Rowland D, Waldinger M, et al. Disorders of orgasm and ejaculation in men. J Sex Med. 2004;1:58–65. doi: 10.1111/j.1743-6109.2004.10109.x. [DOI] [PubMed] [Google Scholar]
- Pastore AL, Palleschi G, Leto A, Pacini L, Iori F, Leonardo C, et al. A prospective randomized study to compare pelvic floor rehabilitation and dapoxetine for treatment of lifelong premature ejaculation. Int J Androl. 2012;35:528–533. doi: 10.1111/j.1365-2605.2011.01243.x. [DOI] [PubMed] [Google Scholar]
- Cooper K, Martyn-St James M, Kaltenthaler E, Dickinson K, Cantrell A. Interventions to treat premature ejaculation. Health Technol Assess. 2013;19 doi: 10.3310/hta19210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Review Manager (RevMan) [Computer program] The Nordic Cochrane Centre The Cochrane Collaboration Version 5.3. Copenhagen2014
- Higgins JPT, Altman DG, Sterne JAC. the Cochrane Bias Methods Group, on behalf of the Cochrane Statistical Methods Group. Assessing risk of bias in included studies. In: Higgins JPT, Green S, editors. Cochrane handbook for systematic reviews of interventions version 5.1.0 (updated March 2011) The Cochrane Collaboration; 2011. Available at: http://www.cochrane-handbook.org (accessed February 5, 2015) [Google Scholar]
- de Carufel F, Trudel G. Effects of a new functional-sexological treatment for premature ejaculation. J Sex Marital Ther. 2006;32:97–114. doi: 10.1080/00926230500442292. [DOI] [PubMed] [Google Scholar]
- Jern P. Evaluation of a behavioral treatment intervention for premature ejaculation using a handheld stimulating device. J Sex Marital Ther. 2014;40:358–366. doi: 10.1080/0092623X.2013.857376. [DOI] [PubMed] [Google Scholar]
- Trudel G, Proulx S. Treatment of premature ejaculation by bibliotherapy: An experimental study. Sex Marital Ther. 1987;2:163–167. [Google Scholar]
- van Lankveld JJDM, Leusink P, van Diest S, Gijs L, Slob AK. Internet-based brief sex therapy for heterosexual men with sexual dysfunctions: A randomized controlled pilot trial. J Sex Med. 2009;6:2224–2236. doi: 10.1111/j.1743-6109.2009.01321.x. [DOI] [PubMed] [Google Scholar]
- Li P, Zhu GS, Xu P, Sun LH, Wang P. Interventional effect of behaviour psychotherapy on patients with premature ejaculation. Zhonghua Nan Ke Xue. 2006;12:717–719. [PubMed] [Google Scholar]
- Shao X, Li J. [Clinical study on treatment of premature ejaculation with Paroxetine and behavior-therapy] Nan Xing Xue Za Zhi. 2008;22:18–20. [Google Scholar]
- Yuan P, Dai J, Yang Y, Guo J, Liang R. [A comparative study on treatment for premature ejaculation: Citalopram used in combination with behavioral therapy versus either Citalopram or behavioral therapy alone] Nan Xing Xue Za Zhi. 2008;22:35–38. [Google Scholar]
- Abdel-Hamid IA, El Naggar EA, El Gilany AH. Assessment of as needed use of pharmacotherapy and the pause-squeeze technique in premature ejaculation. Int J Impot Res. 2001;13:41–45. doi: 10.1038/sj.ijir.3900630. [DOI] [PubMed] [Google Scholar]
- Oguzhanoglu NK, Ozdel O, Aybek Z. The efficacy of fluoxetine and a stop-start technique in the treatment of premature ejaculation and anxiety. J Clin Psychopharmacol. 2005;25:192–194. doi: 10.1097/01.jcp.0000161449.50969.28. [DOI] [PubMed] [Google Scholar]
- Eassa BI, El-Shazly MA. Safety and efficacy of tramadol hydrochloride on treatment of premature ejaculation. Asian J Androl. 2013;15:138–142. doi: 10.1038/aja.2012.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1 Medline search strategy (August 2014).


