Abstract
Emerging data demonstrate pivotal roles for brain insulin resistance and insulin deficiency as mediators of cognitive impairment and neurodegeneration, particularly Alzheimer’s disease (AD). Insulin and insulin-like growth factors (IGFs) regulate neuronal survival, energy metabolism, and plasticity, which are required for learning and memory. Hence, endogenous brain-specific impairments in insulin and IGF signaling account for the majority of AD-associated abnormalities. However, a second major mechanism of cognitive impairment has been linked to obesity and Type 2 diabetes (T2DM). Human and experimental animal studies revealed that neurodegeneration associated with peripheral insulin resistance is likely effectuated via a liver-brain axis whereby toxic lipids, including ceramides, cross the blood brain barrier and cause brain insulin resistance, oxidative stress, neuro-inflammation, and cell death. In essence, there are dual mechanisms of brain insulin resistance leading to AD-type neurodegeneration: one mediated by endogenous, CNS factors; and the other, peripheral insulin resistance with excess cytotoxic ceramide production.
INTRODUCTION
Alzheimer’s disease (AD) is the most common cause of dementia in the Western hemisphere. Aging is by far the most important risk factor, and in essence, a requirement for developing AD. The same is true for many other neurodegenerative diseases such as Parkinson’s disease, frontotemporal dementia, diffuse Lewy body disease, and progressive supranuclear palsy, as these syndromes seldom occur in young or even middle aged individuals. Given the requirement for an aged central nervous system (CNS) template, gaining a fuller understanding of how and why wear and tear changes develop, persist, and progress with prolonged survival is critical to the future design of therapeutic strategies to prevent neurodegeneration.
At the core of the aging process is increased DNA damage, which is mediated by oxidative stress, mitochondrial dysfunction, and reduced energy metabolism/ATP production. In AD, these same abnormalities occur but their severities are greater and their distributions broader due to involvement of targets beyond those impaired or destroyed by normal aging. For example, prominent involvement of corticolimbic structures accounts for the progressive deficits in memory, learning, and behavior in AD. Currently, it is hotly debated as to whether progressive DNA damage and oxidative stress actually trigger and/or propagate AD; or 2) if other underlying factors cause and/or contribute to the pathogenesis of AD, while also exacerbating aging associated oxidative stress and DNA damage in the CNS. Our hypothesis is that in sporadic AD, which accounts for the majority of cases, impairment of brain insulin signaling forms the core of the neurodegeneration cascade (1–3). The mechanism we propose is that brain insulin deficiency and resistance cause neuronal death due to trophic factor withdrawal, deficits in energy metabolism, and inhibition of insulin-responsive gene expression, including those required for acetylcholine homeostasis.
Insulin and igf actions in brain
Insulin and IGF modulate neuronal growth, survival, differentiation, migration, metabolism, gene expression, protein synthesis, cytoskeletal assembly, synapse formation, and plasticity (4). In addition, insulin and IGF-I regulate growth, survival, and myelin production/maintenance in oligodendrocytes (4). Correspondingly, impaired signaling through insulin/IGF receptors adversely affects a broad range of neuronal and glial functions including, glucose homeostasis, energy metabolism, and white matter fiber structure and function. Although insulin and IGF supplied in the circulation can modulate brain functions such as blood flow and energy metabolism (5), endogenous expression of the same polypeptides and their receptors in the CNS indicates that the downstream signaling pathways can be selectively regulated by local and specific activation of the said pathways (1–4, 6, 7). For example, endogenous CNS insulin is likely to be more critical for responding to local and immediate demands associated with learning and memory, than peripheral sources of the same trophic factor (4, 7).
Insulin and IGF-I mediate their effects by activating intrinsic receptor tyrosine kinases (8), which then tyrosine phosphorylate insulin receptor stubstrate (IRS) proteins (9). Tyrosine phosphorylated (TP) IRS transmits intracellular signals that mediate growth, metabolism, and viability by interacting with downstream SH2 domain-containing molecules (10), including the p85 regulatory subunit of phosphatidylinositol-3 kinase (PI3 kinase) (11). PI3 kinase stimulates glucose transport (12) and inhibits apoptosis by activating Akt/Protein kinase B and inhibiting glycogen synthase kinase-3β (GSK-3β) (13).
Positive stimulation through the PI3K/Akt pathway preserves mitochondrial membrane integrity (14), and inhibits production of free radicals that cause mitochondrial DNA damage, mitochondrial dysfunction, and pro-apoptosis mechanisms (15). Therefore, impairments of insulin and IGF signaling due to insulin/IGF resistance and/or trophic factor withdrawal leads to decreased energy metabolism manifested by reduced glucose uptake and ATP production (1). Reduced ATP adversely affects cellular homeostasis, membrane permeability, and fundamental processes required for synaptic maintenance and remodeling, which are needed for learning and establishing new memory.
Brain insulin/IGF resistance and deficiency in Alzheimer’s disease
In the early stages of AD, cerebral glucose utilization is reduced by as much as 45%, and blood flow by ~18%. In the later stages, metabolic and physiological abnormalities worsen, resulting in 55–65% reductions in cerebral blood flow (16). Therefore, altered brain metabolism with features resembling T2DM (17), is detectable soon after the onset of dementia-related symptoms. Since cerebral metabolism declines prior to cognitive deterioration, it is likely that energy failure represents one of the earliest hallmarks of AD. Together, these observations suggest that AD-associated abnormalities in energy metabolism are caused by insulin resistance or reduced insulin actions in the brain, i.e. brain diabetes (18).
Analysis of postmortem human brains demonstrated that AD is associated with significantly reduced expression of insulin/ IGF trophic factors, their receptors, and IRS proteins, and that these abnormalities increase in severity with progression of dementia and neurodegeneration (2, 7). Since IRS molecules are the primary gatekeepers regulating insulin and IGF signaling, the finding that the expression levels of all 3 IRS proteins were reduced indicates that, inability to effectively activate downstream pathways needed to stimulate growth, survival, and metabolism, represents a major abnormality in AD. The critical roles of IRS molecules in the maintenance of brain structure and function have been validated in IRS gene depletion models. IRS-1 knockout mice exhibit small but significant reductions in brain weight (19), while genetic depletion of IRS-2 impairs neuronal proliferation, and promotes intra-neuronal accumulation of phosphorylated tau and neurofibrillary tangles in the hippocampi of affected old mice (20).
In addition to reduced expression of insulin/IGF receptors, AD is associated with reduced insulin, IGF-I, and IGF-II receptor binding (2), which deteriorates as AD progresses (7). Further analyses linked the impairments in ligand-receptor binding to increased membrane cholesterol content in brain (7), possibly secondary to the ApoE4 genotype, which is prevalent in individuals with AD (21), and contributes to aging-associated perturbations in membrane lipid composition (17). Impairments in ligand-receptor binding and downstream signaling through insulin/IGF/IRS pathways, together are sufficient to cause brain insuIin/IGF resistance in AD.
In essence, there are at two main pathophysiological mechanisms of brain insulin/IGF resistance in AD: 1) progressive loss of insulin/IGF responsive neurons, caused by trophic factor withdrawal; and 2) impaired insulin/IGF ligand-receptor binding due to pathological alterations in membrane lipid composition, and probably reduced membrane receptor expression as well. The realization that AD is associated with both insulin/IGF deficiency and insulin/IGF resistance which are for the most part, confined to the CNS, led us to the conclusion that AD represents a brain-specific or brain-restricted form of diabetes mellitus, hence the term, “Type 3 Diabetes” (2).
Consequences of brain insulin and IGF-I mal-signaling in AD
Aberrant Phosphorylation of tau. Insulin and IGF-1 support neuronal cytoskeletal functions via phosphorylation (22), which is required for cytoskeleton assembly and stabilization. Erk MAPK and cyclin dependent kinase 5 are the major kinases responsible for physiological phosphorylation of tau via insulin and IGF-1 stimulation (23). Impaired insulin or IGF-1 signaling, as occurs in AD, can result in hyper-phosphorylation of tau due to inhibition of PI3K/Akt, and increased activation of GSK-3β (20). In addition, inhibition of insulin/IGF-1 signaling blocks the Wnt pathway (24), which negatively regulates GSK-3β via a PI3K/Akt-independent mechanism. In AD, both PI3K/Akt and Wnt signaling have been linked to key molecular abnormalities in AD (25). Finally, GSK-3β can be activated by oxidative stress (26), which is a consequence of insulin/IGF resistance and established feature of AD. Hyper-phosphorylated tau cannot be transported into axons, and instead accumulates and aggregates in neuronal perikarya. Aberrant intra-neuronal phospho-tau accumulation contributes to neurodegeneration by enhancing oxidative stress (27), and triggering pathophysiological cascades that lead to increased apoptosis, mitochondrial dysfunction, and necrosis.
Amyloid β precursor protein (AβPP) and AβPP-Aβ pathology
Insulin influences AβPP-Aβ peptide metabolism by accelerating its trafficking to the plasma membrane from the trans-Golgi network, where it's generated. In addition, insulin increases extracellular levels of AβPP-Aβ by promoting its secretion and inhibiting its degradation by insulin-degrading enzyme. These effects of insulin on AβPP metabolism are mediated by downstream signaling through Erk MAPK (28). Therefore, impaired insulin signaling disrupts physiological processing of AβPP-Aβ. At the same time, AβPP-Aβ can adversely affect insulin signaling by competing with and inhibiting insulin binding or reducing the affinity of insulin binding to its own receptor (29). This suggests that AβPP-Aβ accumulations can promote tau hyper-phosphorylation and formation of dementia associated paired helical filament-containing neuronal cytoskeletal lesions (neurofibrillary tangles, neuritic plaques, and neuropil threads) via functional impairment of the insulin signaling cascade, and attendant increased levels of GSK-3β activity. In addition, AβPP-Aβ exerts adverse/neurodegenerative effects because it can function as a neurotoxin (30). However, AβPP-Aβ-induced neurotoxicity can be prevented by pre-treatment with IGF-1 >>IGF-II (30), and these neuro-protective actions of IGFs are mediated by activation of PI3K/Akt, and suppression of GSK-3β (31).
Oxidative Injury
Insulin/IGF resistance leads to increased oxidative stress, mitochondrial dysfunction, DNA damage, and cell death. Correspondingly, the progressive worsening of insulin/IGF resistance with stage of AD is correlated with increased oxidative stress, DNA damage with apoptosis, incorporation of 8-OHdG, which destabilizes DNA, lipid peroxidation manifested by 4-hydroxynonenal (HNE) accumulation, activation of pro-apoptosis genes and signaling mechanisms (1, 3). Increased expression of pro-oxidant genes such as NOS and NOX, and reduced expression of mitochondria-encoded genes that are critical for ATP production, also contribute to brain insulin resistance.
Insulin degrading enzyme
Insulin degrading enzyme (IDE) catalyzes insulin degradation and negatively regulates its signaling. However, IDE can also degrade soluble AβPP-Aβ (32), and thereby regulate extracellular levels of AβPP-Aβ (33). AβPP-Aβ(1–40) and AβPPAβ (1–42), the main physiological C-terminal cleavage products of AβPP, inhibit insulin binding and insulin receptor auto- phosphorylation by reducing affinity of insulin binding to its own receptor (29). Since AβPP-Aβ competes with insulin for receptor binding, inefficient degradation of soluble AβPP-Aβ could represent an important mediator of brain insulin resistance in AD. Correspondingly, in situ studies have demonstrated increased IDE immunoreactivity surrounding senile plaques (34), and reduced IDE expression in AD hippocampi (35). Moreover, transgenic mice that over-express mutant IDE develop hyperinsulinemia, glucose intolerance, and increased levels of AβPP-Aβ in the brain. These findings support the hypothesis that AβPP-Aβ contributes to AD neurodegeneration by impairing insulin signaling, and promoting insulin resistance. One caveat in this argument is that, if AβPP-Aβ interferes with IDE function, the outcome should be to increase rather than decrease insulin levels and actions in the CNS. In AD, the opposite is true-- increased levels of AβPP-Aβ are associated with reduced levels of CNS insulin and IGF-1 (2, 7).
Type 3 diabetes model of AD
Reflection on some of the earlier findings in AD, including the impaired glucose utilization, mitochondrial dysfunction, reduced ATP production, and energy shortage, led to the hypothesis that these abnormalities were mediated by desensitization of the neuronal insulin receptor (36). The stated metabolic abnormalities, as well as several of the classical histopathological lesions of AD, could be attributed, in part, to reduced insulin levels and reduced insulin receptor function in AD. Hoyer was among the first to suggest that reduced levels of brain insulin may precipitate a cascade resulting in disturbances in cellular glucose, acetylcholine, cholesterol, and ATP levels, impaired membrane function, accumulation of amyloidogenic derivatives, and hyper-phosphorylation of tau, i.e. that AD may represent a brain form of Type 2 diabetes mellitus (36).
Streptozotocin (STZ) is a nitrosamide methylnitrosourea linked to D-glucose, and taken up by insulin-producing cells such as beta cells in pancreatic islets. Once metabolized, the N-nitrosoureido is liberated and causes DNA damage and cell death through generation of reactive oxygen species (37). Intracerebroventricular (ic) injection of STZ impairs brain glucose utilization oxidative metabolism (38), insulin receptor function (39), and spatial learning and memory (6, 40). Moreover, ic-STZ treatments produced long-term and progressive deficits in learning, memory, cognition, behavior, and cerebral energy balance (6, 40).
Rat brains treated by ic-STZ had striking histopathological, biochemical, and molecular neurodegenerative abnormalities that overlapped with AD. The ic-STZ-injected brains became atrophic due to neuronal and oligodendroglial cell loss mediated by apoptosis, mitochondrial dysfunction, neuro-inflammation, and oxidative stress (6). In addition, the brains had significantly increased expression of AβPP and acetylcholinesterase (40), increased levels of GSK-3β activity, phospho-tau, ubiquitin, and AβPP-Aβ, and decreased expression of choline acetyltransferase (6, 40), similar to the findings in AD. Importantly, ic-STZ induced neurodegenerative abnormalities and neurocognitive deficits were associated reduced expression of genes encoding insulin, IGF-II, insulin receptor, IGF-I receptor, and insulin receptor substrate-1 (IRS-1), and reduced binding to the insulin and IGF-II receptors. The combined effects of decreased expression of insulin/IGF polypeptides, insulin/IGF receptors, and IRS, and impaired receptor binding, reflect failure of brain insulin/IGF signaling mechanisms. Importantly, many molecular abnormalities that characteristically occur in AD and produced by ic-STZ, including increased GSK-3β activation, increased tau phosphorylation, and decreased neuronal survival, energy metabolism, and cholinergic homeostasis, are mediated by downstream effects of impaired insulin and IGF signaling. Therefore, the ic-STZ model recapitulates many characteristic features of AD, and demonstrates a cause-effect relationship between insulin deficiency and resistance and AD-type neurodegeneration, i.e. Type 3 diabetes (2, 7).
Contributions of type 2 diabetes
Interest in clarifying the roles of T2DM, peripheral insulin resistance, and hyperinsulinemia in relation to cognitive impairment and its progression to AD began 5 to 10 years ago (1, 18, 20, 41). Currently, this field is exploding with new information about mechanisms of brain insulin resistance and deficiency, and how they contribute to cognitive impairment and neurodegeneration (2, 6, 7, 40, 41). There is now solid evidence that tau expression and phosphorylation are regulated by insulin and IGF signaling cascades (20), and that many critical aspects of AD can be explained on the basis of impaired insulin signaling (1, 3).
That peripheral insulin resistance diseases, including obesity, T2DM, and non-alcoholic steatohepatitis (NASH), which is caused by lipid accumulation in liver with inflammation and insulin resistance, contribute to cognitive impairment and neurodegeneration, is supported by the findings that: 1) morbidity and mortality from AD, T2DM, obesity, and NASH have all increased rapidly over the past 2–3 decades (42); 2) individuals with T2DM (43) or obesity/dyslipidemic disorders (44) are at increased risk of developing mild cognitive impairment (MCI), dementia, or AD (43); 3) AD is associated with progressive brain insulin resistance and insulin deficiency (2, 7, 41); 4) experimental T2DM and obesity cause cognitive impairment (45); 5) experimental induction of brain insulin resistance and insulin deficiency cause AD-type neurodegeneration and cognitive impairment (6); 6) treatment with insulin sensitizer agents or intranasal insulin improves cognitive performance in experimental models and human cases of AD or MCI (40, 46, 47); and 7) molecular, biochemical, and mechanistic abnormalities in T2DM and AD are shared (48).
To experimentally interrogate the roles of obesity and T2DM as mediators of neurodegeneration, we utilized models of high fat diet (HFD) feeding which doubled mean body weight and caused T2DM, NASH, and mild brain atrophy in C57BL/6 mice (49). Molecular and biochemical analyses revealed the obesity/T2DM induced neurodegeneration was associated with brain insulin resistance, gliosis, neuronal cytoskeletal abnormalities, and oxidative stress, although the overall magnitude of these effects was modest compared with AD (2, 7) or ic-STZ treatment (6, 40). These results support the hypothesis that obesity with T2DM serve as co-factors in neurodegeneration, but are not sufficient to cause AD.
Additional studies and a literature review focused on identifying critical factors linking cognitive impairment or brain insulin resistance to obesity and/or T2DM revealed that, irrespective of etiology, steatohepatitis can be associated with cognitive impairment and neuropsychiatric dysfunction in humans (50, 51) and experimental animal models (6, 40, 49, 52). In fact, the critical variable seemed to be hepatic steatosis or steatohepatitis with hepatic insulin resistance. This suggests that dysregulated lipid metabolism in liver mediates cognitive impairment and neurodegeneration. Mechanistically, insulin normally stimulates lipogenesis, which increases triglyceride storage in the liver (53). However, if the process proceeds unchecked, hepatocytes suffer ER stress, oxidative damage, mitochondrial dysfunction, and inflammatory reactions. Attendant alterations in membrane lipid composition shift the liver cells toward insulin resistance (53). Insulin resistance promotes lipolysis, and lipolysis generates toxic lipids, i.e. ceramides, which further impair insulin signaling, mitochondrial function, and cell viability (54).
Ceramides are lipid signaling molecules with wide-ranging modulatory effects, including cell proliferation, motility, plasticity, inflammation, apoptosis, and insulin resistance (55). Cytotoxic ceramides cause insulin resistance by activating pro-inflammatory cytokines and inhibiting insulin-stimulated signaling through PI3 kinase-Akt (56). In brain, ceramides have similar inhibitory effects on insulin signaling (57) and pro-inflammatory cytokine activation (55). In diet-induced obesity, enhanced ceramide production in adipocytes leads to insulin resistance (55). However, more recent studies indicate that ceramide generation is significantly increased in livers with steatosis and insulin resistance, irrespective of co-existing obesity (40, 49, 52).
Since ceramides, sphingosines, and other toxic lipids are lipid soluble and therefore can readily cross the blood-brain barrier, we hypothesized that ceramides generated in the context of hepatic steatosis or steatohepatitis mediate neurodegeneration by precipitating a cascade leading to brain insulin resistance. Correspondingly, in vitro exposure to bioactive ceramides causes neuronal insulin resistance, reduced viability, neurotransmitter function, and mitochondrial function, and increased oxidative stress, DNA damage, and lipid peroxidation (58). Further preliminary studies showed that intraperitoneal injection of bioactive ceramides impairs learning and causes brain insulin resistance, similar to the effects of T2DM and NASH. These observations support the hypothesis that ceramides generated in extra-CNS tissues, particularly liver, can cause brain insulin resistance and thereby mediate neurodegeneration.
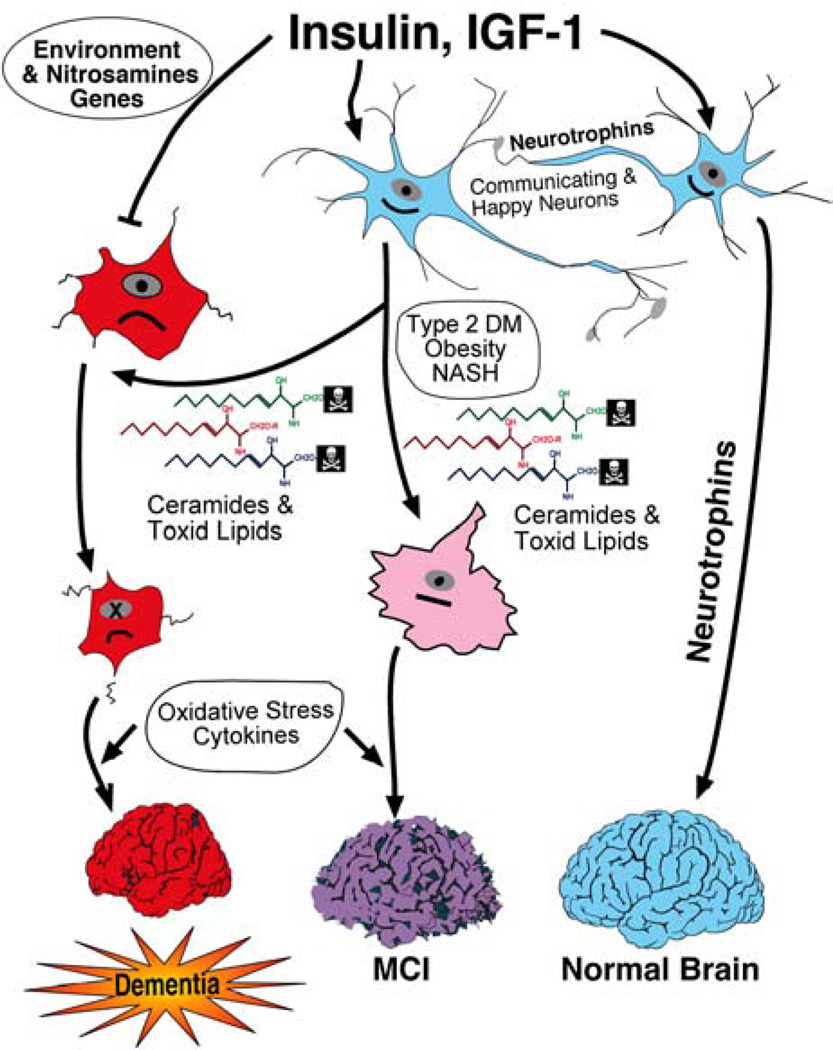
Hypothesis (Fig. 1)
Fig. 1.
Dual and overlapping pathways of insulin/IGF resistance mediated neurodegeneration. CNS neuronal survival, metabolic activity, and homeostasis are stimulated by insulin and IGF-1, which promote neurotrophin expression and plasticity for maintenance of normal brain structure, learning, and memory. Peripheral insulin resistance diseases such as T2DM and NASH, contribute to neurodegeneration through increased production of cytotoxic ceramides and other toxic lipids, which cause insulin resistance, mild cognitive impairment (MCI), and limited neurodegeneration. Environmental exposures, including nitrosamines, plus genetic factors, cause insulin and IGF resistance, which leads to neurodegeneration. T2DM and other peripheral insulin resistance diseases exacerbate the neurodegeneration cascade due to increased production of toxic lipids and ceramides. Finally, oxidative stress and cytokine activation contribute to neurodegeneration and dementia, but alone are not sufficient to cause dementia.
The aggregate findings in human and experimental investigations provide strong evidence in favor of dual mechanisms of cognitive impairment and neurodegeneration mediated by brain insulin resistance. In the absence of peripheral insulin resistance, AD most likely represents a brain-specific form of diabetes mellitus, i.e. T3DM, and due to the combined effects of brain insulin deficiency and insulin resistance. Although etiological factors responsible for T3DM have not been proven, recent studies, based on the structural relationship between STZ and nitrosamines, which contaminate preserved foods, point toward a role for environmental, food, and tobacco exposures as causative agents (42). Among individuals with peripheral insulin resistance due to obesity, T2DM, NASH, or metabolic syndrome, excess generation of cytotoxic lipids, including ceramides, cross the blood-brain barrier and cause brain insulin resistance, neuro-inflammation, and oxidative stress. The magnitude of disease process is considerably less than in T3DM because the primary disease focus is outside the CNS. Nonetheless, the "hit" is sufficient to precipitate, propagate, and increase the severity of T3DM, thereby reconciling epidemiologic data demonstrating increased risk of MCI or AD among individuals with T2DM, and the consistent human and experimental evidence that peripheral insulin resistance diseases alone are not sufficient to cause AD.
Acknowledgements
Research Supported by Grants AA-11431, AA-12908, and AA-16126 from the National Institutes of Health.
REFERENCES
- 1.de la Monte SM, Wands JR. Review of insulin and insulin-like growth factor expression, signaling, and malfunction in the central nervous system: relevance to Alzheimer's disease. J. Alzheimers. Dis. 2005;7:45–61. doi: 10.3233/jad-2005-7106. [DOI] [PubMed] [Google Scholar]
- 2.Steen E, Terry BM, Rivera EJ, Cannon JL, Neely TR, Tavares R, Xu XJ, Wands JR, de la Monte SM. Impaired insulin and insulin-like growth factor expression and signaling mechanisms in Alzheimer's disease--is this type 3 diabetes? J. Alzheimers. Dis. 2005;7:63–80. doi: 10.3233/jad-2005-7107. [DOI] [PubMed] [Google Scholar]
- 3.de la Monte SM, Wands JR. Alzheimer's disease is type 3 diabetes: evidence reviewed. J. Diabetes. Sci. Tech. 2008;2:1101–1113. doi: 10.1177/193229680800200619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.D'Ercole AJ, Ye P, Calikoglu AS, Gutierrez-Ospina G. The role of the insulin-like growth factors in the central nervous system. Mol. Neurobiol. 1996;13:227–255. doi: 10.1007/BF02740625. [DOI] [PubMed] [Google Scholar]
- 5.Wozniak M, Rydzewski B, Baker SP, Raizada MK. The cellular and physiological actions of insulin in the central nervous system. Neurochem. Int. 1993;22:1–10. doi: 10.1016/0197-0186(93)90062-a. [DOI] [PubMed] [Google Scholar]
- 6.Lester-Coll N, Rivera EJ, Soscia SJ, Doiron K, Wands JR, de la Monte SM. Intracerebral streptozotocin model of type 3 diabetes: relevance to sporadic Alzheimer's disease. J. Alzheimers. Dis. 2006;9:13–33. doi: 10.3233/jad-2006-9102. [DOI] [PubMed] [Google Scholar]
- 7.Rivera EJ, Goldin A, Fulmer N, Tavares R, Wands JR, de la Monte SM. Insulin and insulin-like growth factor expression and function deteriorate with progression of Alzheimer's disease: link to brain reductions in acetylcholine. J. Alzheimers. Dis. 2005;8:247–268. doi: 10.3233/jad-2005-8304. [DOI] [PubMed] [Google Scholar]
- 8.Ullrich A, Bell JR, Chen EY, Herrera R, Petruzzelli LM, Dull TJ, Gray A, Coussens L, Liao YC, Tsubokawa M. Human insulin receptor and its relationship to the tyrosine kinase family of oncogenes. Nature. 1985;313:756–761. doi: 10.1038/313756a0. [DOI] [PubMed] [Google Scholar]
- 9.Shpakov AO, Pertseva MN. Structural and functional characterization of insulin receptor substrate proteins and the molecular mechanisms of their interaction with insulin superfamily tyrosine kinase receptors and effector proteins. Membr. Cell. Biol. 2000;13:455–484. [PubMed] [Google Scholar]
- 10.Giovannone B, Scaldaferri ML, Federici M, Porzio O, Lauro D, Fusco A, Sbraccia P, Borboni P, Lauro R, Sesti G. Insulin receptor substrate (IRS) transduction system: distinct and overlapping signaling potential. Diabetes. Metab. Res. Rev. 2000;16:434–441. doi: 10.1002/1520-7560(2000)9999:9999<::aid-dmrr159>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 11.Sun XJ, Crimmins DL, Myers MJ, Miralpeix M, White MF. Pleiotropic insulin signals are engaged by multisite phosphorylation of IRS-1. Mol. Cell. Biol. 1993;13:7418–7428. doi: 10.1128/mcb.13.12.7418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lam K, Carpenter CL, Ruderman NB, Friel JC, Kelly KL. The phosphatidylinositol 3-kinase serine kinase phosphorylates IRS-1. Stimulation by insulin and inhibition by Wortmannin. J. Biol. Chem. 1994;269:20648–20652. [PubMed] [Google Scholar]
- 13.Dudek H, Datta SR, Franke TF, Birnbaum MJ, Yao R, Cooper GM, Segal RA, Kaplan DR, Greenberg ME. Regulation of neuronal survival by the serine-threonine protein kinase Akt. Science. 1997;275:661–665. doi: 10.1126/science.275.5300.661. [see comments]. [DOI] [PubMed] [Google Scholar]
- 14.Condorelli F, Salomoni P, Cotteret S, Cesi V, Srinivasula SM, Alnemri ES, Calabretta B. Caspase cleavage enhances the apoptosis-inducing effects of BAD. Mol. Cell. Biol. 2001;21:3025–3036. doi: 10.1128/MCB.21.9.3025-3036.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Halestrap AP, Doran E, Gillespie JP, O'Toole A. Mitochondria and cell death. Biochem. Soc. Trans. 2000;28:170–177. doi: 10.1042/bst0280170. [DOI] [PubMed] [Google Scholar]
- 16.Hoyer S, Nitsch R. Cerebral excess release of neurotransmitter amino acids subsequent to reduced cerebral glucose metabolism in early-onset dementia of Alzheimer type. J. Neural. Transm. 1989;75:227–232. doi: 10.1007/BF01258634. [DOI] [PubMed] [Google Scholar]
- 17.Hoyer S. Brain glucose and energy metabolism abnormalities in sporadic Alzheimer disease. Causes and consequences: an update. Exp. Gerontol. 2000;35:1363–1372. doi: 10.1016/s0531-5565(00)00156-x. [DOI] [PubMed] [Google Scholar]
- 18.Hoyer S. Glucose metabolism and insulin receptor signal transduction in Alzheimer disease. Eur. J. Pharmacol. 2004;490:115–125. doi: 10.1016/j.ejphar.2004.02.049. [DOI] [PubMed] [Google Scholar]
- 19.Pete G, Fuller CR, Oldham JM, Smith DR, D'Ercole AJ, Kahn CR, Lund PK. Postnatal growth responses to insulin-like growth factor I in insulin receptor substrate-1-deficient mice. Endocrinology. 1999;140:5478–5487. doi: 10.1210/endo.140.12.7219. [DOI] [PubMed] [Google Scholar]
- 20.Schubert M, Brazil DP, Burks DJ, Kushner JA, Ye J, Flint CL, Farhang-Fallah J, Dikkes P, Warot XM, Rio C, Corfas G, White MF. Insulin receptor substrate-2 deficiency impairs brain growth and promotes tau phosphorylation. J. Neurosci. 2003;23:7084–7092. doi: 10.1523/JNEUROSCI.23-18-07084.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ait-Ghezala G, Abdullah L, Crescentini R, Crawford F, Town T, Singh S, Richards D, Duara R, Mullan M. Confirmation of association between D10S583 and Alzheimer's disease in a case--control sample. Neurosci. Lett. 2002;325:87–90. doi: 10.1016/s0304-3940(02)00243-4. [DOI] [PubMed] [Google Scholar]
- 22.Hong M, Lee VM. Insulin and insulin-like growth factor-1 regulate tau phosphorylation in cultured human neurons. J. Biol. Chem. 1997;272:19547–19553. doi: 10.1074/jbc.272.31.19547. [DOI] [PubMed] [Google Scholar]
- 23.Lovestone S, Reynolds CH, Latimer D, Davis DR, Anderton BH, Gallo JM, Hanger D, Mulot S, Marquardt B, Stabel S, et al. Alzheimer's disease-like phosphorylation of the microtubule-associated protein tau by glycogen synthase kinase-3 in transfected mammalian cells. Curr. Biol. 1994;4:1077–1086. doi: 10.1016/s0960-9822(00)00246-3. [DOI] [PubMed] [Google Scholar]
- 24.Doble BW, Woodgett JR. GSK-3: tricks of the trade for a multi-tasking kinase. J. Cell. Sci. 2003;116:1175–1186. doi: 10.1242/jcs.00384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.De Ferrari GV, Inestrosa NC. Wnt signaling function in Alzheimer's disease. Brain. Res. Brain. Res. Rev. 2000;33:1–12. doi: 10.1016/s0165-0173(00)00021-7. [DOI] [PubMed] [Google Scholar]
- 26.Chen GJ, Xu J, Lahousse SA, Caggiano NL, de la Monte SM. Transient hypoxia causes Alzheimer-type molecular and biochemical abnormalities in cortical neurons: potential strategies for neuroprotection. J. Alzheimers. Dis. 2003;5:209–228. doi: 10.3233/jad-2003-5305. [DOI] [PubMed] [Google Scholar]
- 27.Mandelkow EM, Stamer K, Vogel R, Thies E, Mandelkow E. Clogging of axons by tau, inhibition of axonal traffic and starvation of synapses. Neurobiol. Aging. 2003;24:1079–1085. doi: 10.1016/j.neurobiolaging.2003.04.007. [DOI] [PubMed] [Google Scholar]
- 28.Gasparini L, Netzer WJ, Greengard P, Xu H. Does insulin dysfunction play a role in Alzheimer's disease? Trends. Pharmacol. Sci. 2002;23:288–293. doi: 10.1016/s0165-6147(02)02037-0. [DOI] [PubMed] [Google Scholar]
- 29.Xie L, Helmerhorst E, Taddei K, Plewright B, Van Bronswijk W, Martins R. Alzheimer's beta-amyloid peptides compete for insulin binding to the insulin receptor. J. Neurosci. 2002;22:RC221. doi: 10.1523/JNEUROSCI.22-10-j0001.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dore S, Kar S, Quirion R. Insulin-like growth factor I protects and rescues hippocampal neurons against beta-amyloid- and human amylin-induced toxicity. Proc. Natl. Acad. Sci. U.S.A. 1997;94:4772–4777. doi: 10.1073/pnas.94.9.4772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zheng WH, Kar S, Dore S, Quirion R. Insulin-like growth factor-1 (IGF-1): a neuroprotective trophic factor acting via the Akt kinase pathway. J. Neural. Transm. Suppl. 2000:261–272. doi: 10.1007/978-3-7091-6301-6_17. [DOI] [PubMed] [Google Scholar]
- 32.McDermott JR, Gibson AM. Degradation of Alzheimer's beta-amyloid protein by human and rat brain peptidases: involvement of insulin-degrading enzyme. Neurochem. Res. 1997;22:49–56. doi: 10.1023/a:1027325304203. [DOI] [PubMed] [Google Scholar]
- 33.Balasubramanian AS. Amyloid beta peptide processing, insulin degrading enzyme, and butyrylcholinesterase. Neurochem. Res. 2001;26:453–456. doi: 10.1023/a:1010967602362. [DOI] [PubMed] [Google Scholar]
- 34.Bernstein HG, Ansorge S, Riederer P, Reiser M, Frolich L, Bogerts B. Insulin-degrading enzyme in the Alzheimer's disease brain: prominent localization in neurons and senile plaques. Neurosci. Lett. 1999;263:161–164. doi: 10.1016/s0304-3940(99)00135-4. [DOI] [PubMed] [Google Scholar]
- 35.Cook DG, Leverenz JB, McMillan PJ, Kulstad JJ, Ericksen S, Roth RA, Schellenberg GD, Jin LW, Kovacina KS, Craft S. Reduced hippocampal insulin-degrading enzyme in late-onset Alzheimer's disease is associated with the apolipoprotein E-epsilon4 allele. Am. J. Pathol. 2003;162:313–319. doi: 10.1016/s0002-9440(10)63822-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hoyer S. The aging brain. Changes in the neuronal insulin/insulin receptor signal transduction cascade trigger late-onset sporadic Alzheimer disease (SAD). A mini-review. J. Neural. Transm. 2002;109:991–1002. doi: 10.1007/s007020200082. [DOI] [PubMed] [Google Scholar]
- 37.Szkudelski T. The mechanism of alloxan and streptozotocin action in B cells of the rat pancreas. Physiol. Res. 2001;50:537–546. [PubMed] [Google Scholar]
- 38.Duelli R, Schrock H, Kuschinsky W, Hoyer S. Intracerebroventricular injection of streptozotocin induces discrete local changes in cerebral glucose utilization in rats. Int. J. Dev. Neurosci. 1994;12:737–743. doi: 10.1016/0736-5748(94)90053-1. [DOI] [PubMed] [Google Scholar]
- 39.Hoyer S, Lee SK, Loffler T, Schliebs R. Inhibition of the neuronal insulin receptor. An in vivo model for sporadic Alzheimer disease? Ann. N. Y. Acad. Sci. 2000;920:256–258. doi: 10.1111/j.1749-6632.2000.tb06932.x. [DOI] [PubMed] [Google Scholar]
- 40.de la Monte SM, Tong M, Lester-Coll N, Plater M, Jr, Wands JR. Therapeutic rescue of neurodegeneration in experimental type 3 diabetes: relevance to Alzheimer's disease. J. Alzheimers. Dis. 2006;10:89–109. doi: 10.3233/jad-2006-10113. [DOI] [PubMed] [Google Scholar]
- 41.Craft S. Insulin resistance and Alzheimer's disease pathogenesis: potential mechanisms and implications for treatment. Curr. Alzheimer. Res. 2007;4:147–152. doi: 10.2174/156720507780362137. [DOI] [PubMed] [Google Scholar]
- 42.de la Monte SM, Neusner A, Chu J, Lawton M. Epidemilogical trends strongly suggest exposures as etiologic agents in the pathogenesis of sporadic Alzheimer's disease, diabetes mellitus, and non- alcoholic steatohepatitis. J. Alzheimers. Dis. 2009 doi: 10.3233/JAD-2009-1070. (In Press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pasquier F, Boulogne A, Leys D, Fontaine P. Diabetes mellitus and dementia. Diabetes. Metab. 2006;32:403–414. doi: 10.1016/s1262-3636(07)70298-7. [DOI] [PubMed] [Google Scholar]
- 44.Martins IJ, Hone E, Foster JK, Sunram-Lea SI, Gnjec A, Fuller SJ, Nolan D, Gandy SE, Martins RN. Apolipoprotein E, cholesterol metabolism, diabetes, and the convergence of risk factors for Alzheimer's disease and cardiovascular disease. Mol. Psychiatry. 2006;11:721–736. doi: 10.1038/sj.mp.4001854. [DOI] [PubMed] [Google Scholar]
- 45.Winocur G, Greenwood CE, Piroli GG, Grillo CA, Reznikov LR, Reagan LP, McEwen BS. Memory impairment in obese Zucker rats: an investigation of cognitive function in an animal model of insulin resistance and obesity. Behav. Neurosci. 2005;119:1389–1395. doi: 10.1037/0735-7044.119.5.1389. [DOI] [PubMed] [Google Scholar]
- 46.Landreth G. Therapeutic use of agonists of the nuclear receptor PPARgamma in Alzheimer's disease. Curr. Alzheimer. Res. 2007;4:159–164. doi: 10.2174/156720507780362092. [DOI] [PubMed] [Google Scholar]
- 47.Reger MA, Watson GS, Green PS, Wilkinson CW, Baker LD, Cholerton B, Fishel MA, Plymate SR, Breitner JC, Degroodt W, Mehta P, Craft S. Intranasal insulin improves cognition and modulates {beta}-amyloid in early AD. Neurology. 2008;70:440–448. doi: 10.1212/01.WNL.0000265401.62434.36. [DOI] [PubMed] [Google Scholar]
- 48.Nicolls MR. The clinical and biological relationship between Type II diabetes mellitus and Alzheimer's disease. Curr. Alzheimer. Res. 2004;1:47–54. doi: 10.2174/1567205043480555. [DOI] [PubMed] [Google Scholar]
- 49.Lyn-Cook LE, Lawton M, Tong M, Silbermann E, Longato L, Jiao P, Mark P, Wands JR, Xu H, de la Monte SM. Hepatic ceramide mediates brain insulin resistance and neurodegeneration in obesity with type 2 diabetes mellitus and Non-alcoholoic steatohepatitis. J. Alzheimer's Dis. 2008 doi: 10.3233/JAD-2009-0984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Elwing JE, Lustman PJ, Wang HL, Clouse RE. Depression, anxiety, and nonalcoholic steatohepatitis. Psychosom. Med. 2006;68:563–569. doi: 10.1097/01.psy.0000221276.17823.df. [DOI] [PubMed] [Google Scholar]
- 51.Perry W, Hilsabeck RC, Hassanein TI. Cognitive dysfunction in chronic hepatitis C: a review. Dig. Dis. Sci. 2008;53:307–321. doi: 10.1007/s10620-007-9896-z. [DOI] [PubMed] [Google Scholar]
- 52.Tong M, Lawton M, Neusner A, Longato L, Wands JR, de la Monte SM. Nitrosamine-mediated type 2 diabetes mellitus, hepatic steatosis, and alzheimer-type neurodegeneration: potential role of environmental exposures in our insulin resistance diseases pandemic. J. Alzheimers. Dis. 2009 (In Press) [Google Scholar]
- 53.Capeau J. Insulin resistance and steatosis in humans. Diabetes. Metab. 2008;34:649–657. doi: 10.1016/S1262-3636(08)74600-7. [DOI] [PubMed] [Google Scholar]
- 54.Holland WL, Summers SA. Sphingolipids, insulin resistance, and metabolic disease: new insights from in vivo manipulation of sphingolipid metabolism. Endocr. Rev. 2008;29:381–402. doi: 10.1210/er.2007-0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Summers SA. Ceramides in insulin resistance and lipotoxicity. Prog. Lipid. Res. 2006;45:42–72. doi: 10.1016/j.plipres.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 56.Hajduch E, Balendran A, Batty IH, Litherland GJ, Blair AS, Downes CP, Hundal HS. Ceramide impairs the insulin-dependent membrane recruitment of protein kinase B leading to a loss in downstream signalling in L6 skeletal muscle cells. Diabetologia. 2001;44:173–183. doi: 10.1007/s001250051596. [DOI] [PubMed] [Google Scholar]
- 57.Arboleda G, Huang TJ, Waters C, Verkhratsky A, Fernyhough P, Gibson RM. Insulin-like growth factor-1-dependent maintenance of neuronal metabolism through the phosphatidylinositol 3-kinase-Akt pathway is inhibited by C2-ceramide in CAD cells. Eur. J. Neurosci. 2007;25:3030–3038. doi: 10.1111/j.1460-9568.2007.05557.x. [DOI] [PubMed] [Google Scholar]
- 58.Tong M, de la Monte SM. Ceramide- mediated neurodegeneration: relevance to Diabetes-associated neurodegeneration. J. Alzheimers. Dis. 2009 (In Press) [Google Scholar]