Abstract
Objectives
To assess the impact of ambulatory surgery centers (ASCs) on rates of hospital-based outpatient procedures and adverse events.
Data Sources
Twenty percent national sample of Medicare beneficiaries.
Study Design
A retrospective study of beneficiaries undergoing outpatient surgery between 2001 and 2010. Health care markets were sorted into three groups—those with ASCs, those without ASCs, and those where one opened for the first time. Generalized linear mixed models were used to assess the impact of ASC opening on rates of hospital-based outpatient surgery, perioperative mortality, and hospital admission.
Principal Findings
Adjusted hospital-based outpatient surgery rates declined by 7 percent, or from 2,333 to 2,163 procedures per 10,000 beneficiaries, in markets where an ASC opened for the first time (p < .001 for test between slopes). Within these markets, procedure use at ASCs outpaced the decline observed in the hospital setting. Perioperative mortality and admission rates remained flat after ASC opening (both p > .4 for test between slopes).
Conclusions
The opening of an ASC in a Hospital Service Area resulted in a decline in hospital-based outpatient surgery without increasing mortality or admission. In markets where facilities opened, procedure growth at ASCs was greater than the decline in outpatient surgery use at their respective hospitals.
Keywords: Ambulatory surgery, ambulatory surgery center, utilization
Pressures for improved efficiency and enhancements in perioperative care have prompted considerable growth in outpatient surgery in the United States. Of the 100 million procedures performed in 2006, approximately two-thirds were performed in the outpatient setting (Cullen, Hall, and Golosinskiy 2009). Concurrent with this evolution, there has been a proliferation of freestanding ambulatory surgery centers (ASCs) that are designed to offload volume from the more expensive hospital-based outpatient department (MedPAC 2013a,b).
Because ASCs provide outpatient surgery at a lower cost per episode (Centers for Medicare and Medicaid Services 2008; MedPAC 2013b), they have the potential to improve the efficiency of the delivery system insofar as they are able to reduce rates of hospital-based surgery without negatively impacting quality. Previous work in this area demonstrated modest declines in hospital-based surgery after ASC entry (Lynk and Longley 2002; Bian and Morrisey 2007; Courtemanche and Plotzke 2010), although these studies predated the proliferation of facilities that occurred in the last decade. Further, some worry that ASCs lack oversight and accountability, raising concerns about the quality of care delivered in these facilities (Office of Inspector General 2002). For instance, lapses in infection control (Schaefer et al. 2010) have further amplified these concerns and are partly responsible for the recent implementation of a value-based purchasing program for ASC payments by the Centers for Medicare and Medicaid Services (2010). The recent increase in surgeon-owned freestanding facilities (Ambulatory Surgery Center Association 2012), and their associated financial incentives, has the potential to exacerbate gaps in quality by encouraging the redistribution of less suitable patients (i.e., those with multiple medical problems) to ASCs.
For these reasons, we used national Medicare data to assess the extent to which freestanding ASCs have had their intended effects on the delivery system. In particular, we were interested in the impact of ASCs on rates of hospital-based outpatient surgery and quality, as measured by perioperative mortality and hospital admission.
Methods
Study Subjects
We performed a retrospective cohort study of fee-for-service Medicare beneficiaries undergoing outpatient surgical procedures between 2001 and 2010. We used a 20 percent national sample of claims in the Carrier, Outpatient, Medicare Provider Analysis and Review, and Denominator files. We included only those patients aged 65–99 years who underwent a procedure at either a hospital-based facility or freestanding ASC and who were eligible for Medicare Part B. Information on age, race, and gender of patients was obtained from the Denominator file. Comorbidity was assessed using International Classification of Diseases, Ninth Revision, Clinical Modification diagnoses codes submitted in the year preceding the index outpatient procedure and categorized into groups using established methods (Klabunde et al. 2000). Additional detail on the local health care and regulatory milieu was specified using data from the Area Resource File (Health Resources and Services Administration 2013) and the American Health Planning Association's National Directory (American Health Planning Association 2012). Specifically, we included measures of socioeconomic class, education, capacity for surgery (i.e., surgeons per capita and hospital discharges per capita), presence of certificate of need regulations, and population density.
Surgical procedures were enumerated using Healthcare Common Procedure Coding Systems codes. The type of procedure (inpatient vs. outpatient) and setting (hospital outpatient department vs. ASC) were determined using explicit codes in the Medicare files. We used Hospital Service Areas (HSAs), as described by the Dartmouth Atlas (Wennberg 1999), to reflect distinct health care markets. We chose HSAs, as opposed to another unit of geography, because outpatient surgery is elective, discretionary, and low risk. Thus, patients are likely to undergo such procedures where they commonly receive most of their primary health care (i.e., locally) as opposed to where they would be referred to for tertiary care.
Freestanding ASCs were identified in each HSA using the Provider of Services Extract reported by the Centers for Medicare and Medicaid Services (CMS). These files, released annually, provide detailed information on all Medicare-certified ASCs in the United States, including the facility location. HSAs were sorted into one of three mutually exclusive categories: (1) those with at least one ASC present as of January 1, 2001; (2) those initially without an ASC but in which at least one opened between 2001 and 2010; and (3) those without an ASC throughout the study. A small number of HSAs (n = 190, or 5.5 percent) had ASCs open and close during the study and were excluded from the analysis.
Outcomes
The primary objective was to assess the extent to which the opening of an ASC in a health care market had its intended effects of offloading surgery from the hospital without compromising quality. Our first outcome was population rates of hospital-based outpatient surgery, which includes all surgical procedures (i.e., Healthcare Common Procedure Coding System codes between 10,000 and 69,999) that were performed in either the hospital or ASC over the study period. Ideally, the opening of an ASC would facilitate the migration of outpatient surgery from the more expensive hospital to these facilities. For this measure, the numerator consisted of annual counts of hospital-based outpatient procedures within an HSA, and the denominator was comprised of Medicare beneficiaries eligible for Medicare part B residing in each HSA. Because of the stark differences in population size of the two ASC-containing HSA types (e.g., in 2010, a mean of 21,266 beneficiaries in HSAs where ASCs were always present and 9,020 beneficiaries in HSAs where ASCs were added for the first time), we secondarily examined changes in ASC surgery rates within these markets. One concern is that patient migration across HSA boundaries might explain some of the observed changes in procedure use at the hospital. That is, boundary crossing for surgery by a few beneficiaries in the relatively small HSAs where ASCs opened for the first time (e.g., to nearby larger markets with greater ASC capacity) could have a large impact on rates of hospital procedure use. To address this issue, we examined the direct effect of facility opening on procedures performed in the ASC and contrasted them with the observed change in hospital use within each HSA.
In addition to measuring procedure use, we also assessed the impact of ASC opening on quality, as measured by rates of hospital admission and mortality following outpatient surgery. Preferably, the opening of a new facility within a health care market would have no effect on rates of these events. That is, redistribution from the hospital to the ASC should occur without added patient risk. For these aspects of perioperative quality, we examined the impact of ASC opening on the entire population undergoing outpatient surgery (i.e., procedures performed in both the hospital and ASC). One outcome was hospital admission within 30 days after the index surgery. For this measure, the numerator consisted of counts of admissions. The denominator was the amount of time “at risk,” expressed in person years, among eligible beneficiaries undergoing outpatient surgery annually. A similar measure was developed for perioperative mortality, in which the numerator consisted of all patients dying within 30 days of an outpatient procedure. Due to concerns that procedure selection might artificially lead to more favorable findings for ASCs (i.e., ASCs would preferentially select procedures with the lowest likelihood of adverse events), we also contrasted rates of mortality between hospitals and ASCs for the 10 most common procedures performed in both settings.
Statistical Analysis
The three groups of HSAs (ASC always present, ASC never present, ASC opens for the first time) were contrasted according to beneficiary and regional characteristics using nonparametric statistics. To address differences between HSAs, we used multiple propensity score methods (Spreeuwenberg et al. 2010). To this end, we fit a multinomial logistic regression model in which the dependent variable was the HSA group and the independent variables were the aforementioned beneficiary and regional characteristics. The Hausman test was used to verify that the multinomial model met the Irrelevant Alternatives Assumption, and overlapping of the distributions was visually confirmed. For this model, the Wald χ2 was 789.2 with 24 degrees of freedom (p < .0001) and the pseudo R2 was 0.38. This approach enabled us to effectively calculate the predicted probability of each HSA of being assigned to one of the three market types. These probabilities were then included in subsequent models assessing relationships between HSA group and outcomes.
Longitudinal rates of hospital-based outpatient surgery were estimated after adjustment for their multiple propensity scores, aggregated patient, and regional characteristics using generalized linear mixed models. The unit of analysis was the HSA. We incorporated a random effect for each HSA to account for the correlation between repeated measures within a market. For HSAs where an ASC opened for the first time, “baseline” was classified as the year prior to the first facility opening within its boundaries. For the other two categories of HSAs, “baseline” was randomly assigned and proportionally matched to the “opened for the first time” category so that the distribution of baseline years matched the distribution of baseline years in the “opened for the first time” category. We accounted for temporal trends by introducing the calendar year as a fixed effect and contrasted changes in rates over time both within and between HSA groups. These models were fit using splines with a knot at baseline, which allowed for different linear trends to be assessed in the pre- and post-ASC introduction phases. Splines, interactions, and all adjustment variables were included as fixed effects. In addition to looking at overall rates of hospital-based outpatient surgery, we also sorted patients into groups of procedures (i.e., ophthalmologic, gastrointestinal, and musculoskeletal) commonly performed in ASCs (see Appendix for listing of codes) (MedPAC 2013b).
A similar modeling strategy was used to assess the impact of ASC opening on quality (i.e., hospital admission and mortality) among those undergoing an outpatient procedure. However, for these models, the patient was the unit of analysis.
All analyses were performed using SAS v9.2 (Cary, NC, USA). The probability of a type I error was set at .05 and all testing was two-sided. The institutional review board at the University of Michigan approved this study.
Results
An ASC was introduced into a previously naïve market in 255 HSAs. As shown in Table1, aggregate beneficiary and regional characteristics varied across the three HSA types. While statistically significant differences were evident across market type for most characteristics, many of these were relatively small in magnitude. Of note, HSAs without ASCs had significantly fewer surgeons per capita and lower population densities (i.e., much more likely to be in a rural setting). All differences between markets abated after multiple propensity score adjustment.
Table 1.
Characteristics of the Population Undergoing Outpatient Surgery Based on National Medicare Data
| Hospital Service Area Type | p-value | ||||
|---|---|---|---|---|---|
| ASC Always Present | ASC Never Present | ASC Added for the First Time | Before Multiple PS Correction | After Multiple PS Correction | |
| No. HSAs | 837 | 2,154 | 255 | – | – |
| No. patients in 2010 | 17,793,686 | 6,295,820 | 2,308,790 | – | – |
| Age, mean | 70.6 | 70.5 | 70.5 | .55 | .97 |
| Gender, % female | 55.0 | 53.8 | 54.9 | <.001 | .97 |
| Race, % non-white | 14.8 | 10.3 | 11.3 | <.001 | .41 |
| Charlson score, % 2 or higher | 25.8 | 23.1 | 25.0 | <.001 | .81 |
| Living below poverty, % | 14.0 | 16.0 | 13.6 | <.001 | .60 |
| College education or more among those 25 years and older, % | 23.5 | 16.2 | 23.1 | <.001 | .42 |
| Log of hospital discharges per 10,000 population | 8.8 | 8.4 | 8.8 | <.001 | .94 |
| Log of surgeons per 10,000 population | 4.4 | 2.9 | 4.4 | <.001 | .45 |
| Certificate of need, % | 64.8 | 67.7 | 62.1 | .09 | .88 |
| Urban, % | 79.6 | 28.0 | 65.8 | <.001 | .30 |
As shown in Figure1, adjusted rates of hospital-based outpatient surgery remained stable in all HSA types in the 2 years preceding baseline (p = .22 for test between the three slopes). However, in HSAs where an ASC opened for the first time, hospital-based outpatient surgery rates declined by 7.4 percent, or from 2,333 to 2,163 procedures per 10,000 beneficiaries (p < .0001 for test between the three slopes) during the 4-year period after opening. In contrast, rates of hospital-based outpatient surgery in HSAs where ASCs were always or never present increased by 7.8 percent and 6.6 percent, respectively. The declines in these two market types occurred at a similar pace with one another (p = .11 for test between the two slopes).
Figure 1.

Adjusted Rates of Hospital-Based Outpatient Surgery in Markets Where ASCs Were Always Present, Never Present, and in Those Where an ASC Opened for the First Time. In the period prior to baseline, the rate of change in outpatient surgery across the three market groups was similar (p = .22). However, for the 4-year period following baseline, rates of outpatient surgery decreased more rapidly in markets where an ASC was added for the first time (p < .001 for change over time relative to HSAs always with and without ASCs)
In terms of outpatient surgery use at ASCs themselves, rates in markets where they were always present remained relatively stable over time, increasing by 52 procedures per 10,000 between baseline and 4 years after baseline (p = .60 for trend). In contrast, rates of outpatient surgery in ASCs in HSAs where they opened for the first time increased by 624 procedures per 10,000 during the 4-year period after opening (p < .001 for trend). This increase was more than twofold greater than the decline in hospital-based outpatient surgery observed over the same period in these HSAs (i.e., a decrease of 299 procedures per 10,000 between baseline and 4 years after baseline).
The effect of ASC opening to lower rates of hospital-based outpatient surgery held true for each of the common procedures groups (Figure2). Notably, the strongest relative impact was observed for ophthalmologic surgery (Figure2a). Adjusted rates of hospital-based surgery declined by 53.9 percent by 4 years in HSAs where an ASC opened for the first time, or from 408.4 to 188.3 procedures per 10,000 beneficiaries (p < .0001 for test between the three slopes). Conversely, hospital-based rates of ophthalmologic surgery actually increased at a similar pace over the 4-year period after baseline in HSAs where ASCs were always and never present, or by 5.7 percent and 6.2 percent, respectively (p = .11 for test between the two slopes).
Figure 2.
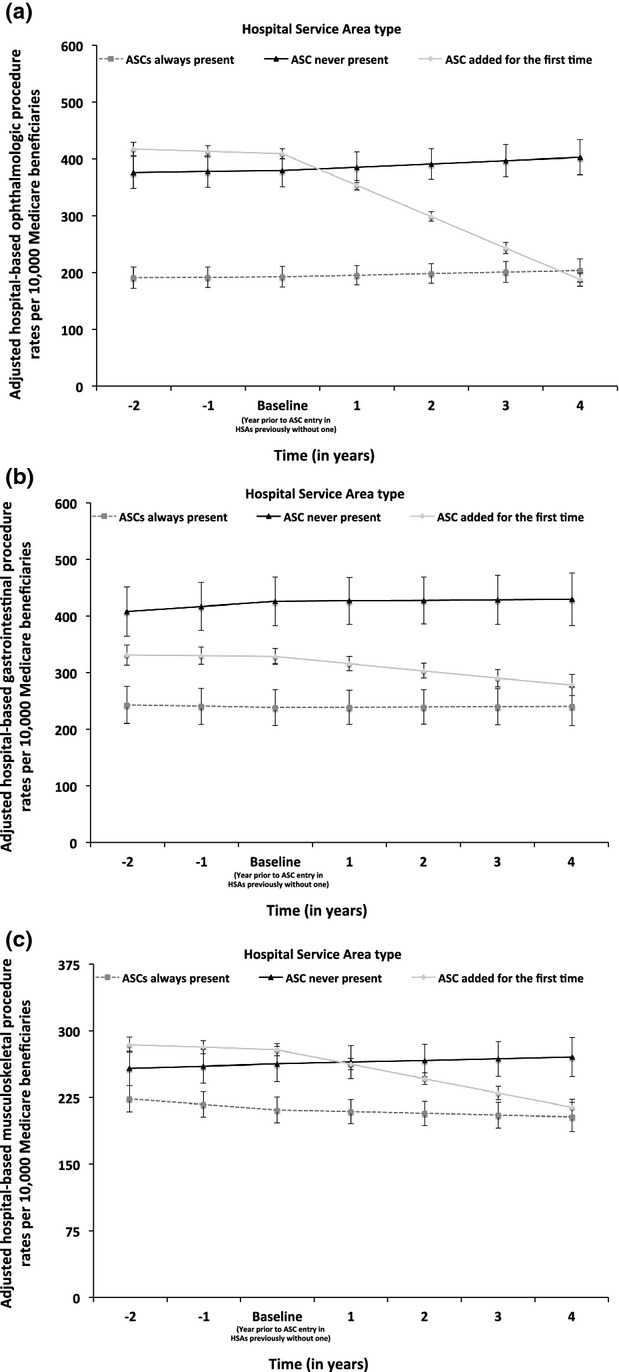
Adjusted Rates of Ophthalmologic (a), Gastrointestinal (b), and Musculoskeletal (c) Hospital-Based Outpatient Surgery in Markets Where ASCs Were Always Present, Never Present, and in Those Where an ASC Opened for the First Time. In the period after baseline, adjusted rates of hospital-based outpatient surgery declined more sharply in markets where an ASC opened for the first time compared to HSAs with and without ASCs (p < .01 for all three specialty groups)
As shown in Figure3, changes in mortality within 30 days for the 4-year period after baseline did not vary significantly across the three market types (p = .43 for test between the three slopes). For each of the 10 most common procedures performed in both settings, rates of mortality were similar or significantly lower for those performed in the ASC compared to the hospital. We found no significant change in hospital admission within 30 days of the index procedure (Figure4) across the three market types. Rates of admission in markets where an ASC opened for the first time were flat during the 4-year period after baseline (7.6 admissions per 1,000 person years at baseline and 7.6 admissions per 1,000 person years at 4 years after baseline; p = .56 for test between three slopes).
Figure 3.
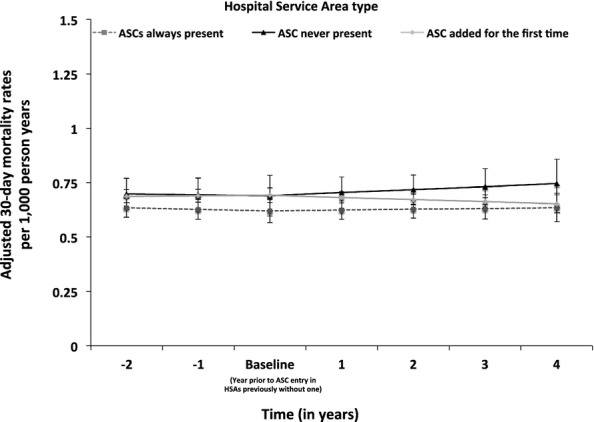
Adjusted Thirty-Day Mortality Rates among Patients Undergoing Outpatient Surgery in Markets with ASCs, Those without and Those Where ASCs Were Added for the First Time. Rates of mortality were similar across HSA groups before (p = .84 for test between three slopes) and after (p = .43 for test between three slopes) baseline
Figure 4.
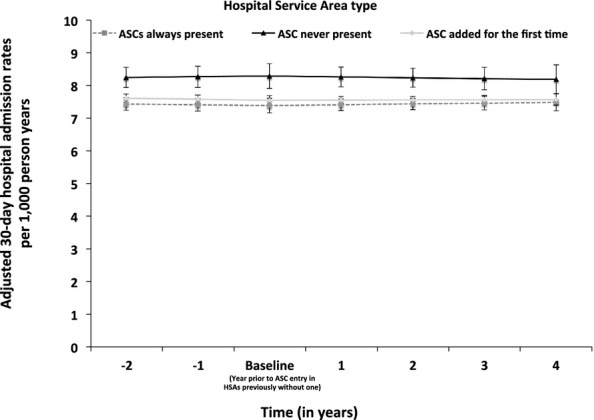
Adjusted Thirty-Day Hospital Admission Rates among Patients Undergoing Outpatient Surgery in Markets with ASCs, Those without ASCs, and Those Where ASCs Were Added for the First Time. Rates of hospital admission were similar across HSA groups before (p = .43 for test between three slopes) and after (p = .56 for test between three slopes) baseline
Comment
The opening of a freestanding ASC was associated with significant reductions in hospital-based surgery within a health care market. In contrast to markets without ASCs, in which hospital-based outpatient surgery rates increased by 7 percent, those where an ASC opened for the first time experienced a 7 percent reduction. This redistribution was even more evident in some surgical disciplines, particularly ophthalmology. Importantly, the shift of outpatient surgery from the hospital to the ASC was not associated with higher rates of hospital admission or mortality. Collectively, our findings suggest that freestanding ASCs can safely achieve their intended effects of outpatient procedure redistribution to a less expensive setting without sacrificing quality, as measured by hospital admission or mortality.
Since the 1980s, the volume of outpatient procedures has grown considerably. Concurrent with this growth, there has been a sea change in the setting for these procedures, with movement out of the hospital and into the ASC (Ambulatory Surgery Center Association 2012). These freestanding facilities were originally championed by the federal government and payers as a means to curtail rising health care expenditures (Davis 1987). While previous studies have demonstrated the ability of these facilities to achieve their desired effects on hospital utilization (Lynk and Longley 2002; Bian and Morrisey 2007; Courtemanche and Plotzke 2010) and outpatient surgery quality (Hollingsworth et al. 2012) in some contexts, they were generally limited in scope or predated the recent proliferation of ASCs. Indeed, the number of ASCs essentially doubled during the first part of the last decade, with nearly 5,500 facilities in 2011 (American Hospital Association 2012). Because these facilities tend to be owned by the physicians who staff them (Ambulatory Surgery Center Association 2012), some worry that inherent financial incentives might spur utilization (i.e., induced demand).
Implicit in the possibility of induced demand by owners of ASCs is the notion that there is an asymmetry of information between the physician and the patient such that the latter cannot make a rationale choice as to the health “value” of the procedure (Wennberg, Barnes, and Zubkoff 1982). Rather, the physician serves in the agency role for the patient. While several factors (e.g., patient preference, medical liability pressures) may cause surgeons to lower their threshold for surgery, many believe that the financial incentives associated with increased productivity (Conrad et al. 2002) and ASC ownership may fuel the use of outpatient surgery. While our study does not address the question of induced demand directly, we did observe that ASCs did not simply offload procedures from the hospitals within markets where new facilities opened for the first time. Four years after opening in these markets, the increase in outpatient surgery at ASCs was more than double the decline in such procedures performed in the hospital setting.
While unmet clinical need might explain this differential, prior empirical work in this area has suggested the possibility of induced demand. First, rates of discretionary outpatient surgery (e.g., knee arthroscopy, cataract surgery) are strongly correlated with the penetration of ASCs (i.e., the proportion of outpatient surgery delivered by ASCs) within a market (Hollenbeck et al. 2010). Second, physician owners of ASCs uniformly perform higher volumes of outpatient procedures (Hollingsworth et al. 2009, 2010; Strope et al. 2009) and patients who see these physicians are much more likely to have surgery compared to those of nonowners (Mitchell 2010). Third, physician owners preferentially manage well-insured patients (Gabel et al. 2008) and perform well-reimbursed procedures (Plotzke and Courtemanche 2011) at ASCs. Finally, the opening of an ASC in a health care market has been associated with significantly higher rates of outpatient surgery relative to markets without them (Hollingsworth et al. 2011; Hollenbeck et al. 2014). Importantly, this growth appears to be driven by procedures with less stringent clinical indications for their use (Hollingsworth et al. 2011).
In addition to concerns surrounding induced demand, other implications of financially motivated procedure redistribution are untoward outcomes and poor quality. As per CMS Conditions for Coverage (Centers for Medicare and Medicaid Services 2011), ASCs are intended for procedures that do not require hospitalization. Unlike hospital outpatient departments, ASCs have limited access to specialty physicians and ancillary services that may be necessary to care for complicated surgical patients undergoing outpatient procedures. A potential consequence of procedure offloading to ASCs after their opening is that some patients may be inappropriately selected for treatment in these facilities, thereby inadvertently leading to higher rates of hospital admission and perioperative mortality.
This study is the first of its kind to comprehensively assess the impact of ASCs on their intended effects on broad indicators of ASC quality. As opposed to comparing quality between hospitals and ASCs, which would clearly bias against the hospital due to favorable patient selection, we instead focused on the effects of ASC opening on rates of adverse events for the entire population undergoing outpatient surgery. Importantly, procedure redistribution to the ASC was not associated with higher population-based rates of unexpected admission or mortality. Further, even within the most common procedures, we observed similar or lower rates of these adverse events at ASCs, implying that our population-level findings were not simply due to favorable procedure-mix selection by the ASCs. Collectively, our data suggest that the observed procedure redistribution from hospitals to ASCs had a negligible impact on these aspects of quality.
Our findings should be interpreted in the context of three limitations. First, because of our reliance on claims data, our measures of ambulatory surgical quality, though well accepted, are limited in scope. While we observed no ill effects of procedure redistribution on unanticipated hospital admission and mortality, there may have been improvements (or decrements) in quality that are underappreciated. For instance, due to their laser-sharp focus on specific procedure lines, ASCs may enhance quality by achieving better clinical outcomes. Second, because we are using Medicare claims, our findings do not reflect the effects of non-Medicare-certified ASCs on procedure redistribution and quality. However, as approximately 80 percent of all ASCs are Medicare-certified, our findings include facilities where the vast majority of outpatient surgery is performed. Third, although ASC opening was able to successfully offload procedures from the hospital, the subsequent utilization by these facilities outpaced the declines at hospitals within their respective markets. Thus, the broader effects of ASCs on utilization and overall health care spending remain unclear and are the focus of our ongoing research efforts. For instance, some worry that the cost savings garnered by ASC efficiency may be offset by financial incentives to increase procedure utilization.
These limitations notwithstanding, our findings have important implications with respect to ambulatory surgery. First and foremost, the rapid proliferation of ASCs in the 2000s was associated with significant reductions in hospital-based outpatient surgery. Because ASCs can provide similar care at a lower cost (Centers for Medicare and Medicaid Services 2008), such procedure redistribution could yield substantial cost savings to the Medicare program, at least on a per episode basis. These savings have the potential to be further amplified by the recent implementation of provisions in the Medicare Prescription Drug, Improvement and Modernization Act of 2003 that greatly expanded the types of procedures eligible for payment in ASCs. Second, the observed redistribution did not come at the expense of quality as measured by population-based rates of mortality and hospital admission, suggesting that patient selection did not negatively impact these outcomes. However, procedure volumes at new ASCs were substantially greater than the declines in volumes at local hospitals.
The dissemination of freestanding ASCs results in a decline in outpatient surgery in the hospital. Insofar as thresholds for intervention remain constant, additional redistribution to these facilities may alleviate latent need and further reduce the use of the more costly hospital setting. Unfortunately, the within-market discrepancy between hospital volume declines and ASC volume increases raises the possibility of induced demand. Additional research surrounding the net effects of ASCs on outpatient surgery expenditures would be helpful for gauging their overall value to the health care system. Given the economics surrounding outpatient surgery and their importance to spending growth for Medicare, understanding the gains in health productivity relative to what is spent is of paramount importance to improving the efficiency of the delivery system.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This work was supported by funding from the Agency for Healthcare Research and Quality (R01 HS18726) to Dr. Hollenbeck. The views expressed herein do not necessarily represent the views of Center for Medicare and Medicaid Services or the United States Government.
Disclosures: None.
Disclaimers: None.
Supporting Information
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Appendix SA2: Common Procedures Performed in Both the Hospital and ASC That Comprised the Three Specialty Group Analyses.
References
- Ambulatory Surgery Center Association. 2012. . “ Ambulatory Surgery Centers: A Positive Trend in Health Care ” [accessed on July 28, 2014]. Available at http://www.ascassociation.org/AdvancingSurgicalCare/aboutascs/industryoverview/apositivetrendinhealthcare.
- American Health Planning Association. 2012. . “ National Directory ” [accessed on January 15, 2013]. Available at http://www.ahpanet.org/national_directory.html.
- American Hospital Association. 2012. . “ Trends Affecting Hospitals and Health Systems ” [accessed on January 1, 2012]. Available at http://www.aha.org/research/reports/tw/chartbook/index.shtml.
- Bian J. Morrisey MA. Free-Standing Ambulatory Surgery Centers and Hospital Surgery Volume. Inquiry. 2007;44(2):200–10. doi: 10.5034/inquiryjrnl_44.2.200. [DOI] [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services. 2008. . “ Calendar Year 2008 Revised Ambulatory Surgical Center Payment System ” [accessed on October 13, 2013]. Available at http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/ASCPayment/downloads/ASC_QAs_03072008.pdf.
- Centers for Medicare and Medicaid Services. 2010. . “ Report to Congress: Medicare Ambulatory Surgery Center Value-Based Purchasing Implementation Plan ” [accessed on March 27, 2013]. Available at http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/ASCPayment/Downloads/C_ASC_RTC-2011.pdf.
- Centers for Medicare and Medicaid Services. 2011. . “ Medicare Ambulatory Surgical Center Value-Based Purchasing Implementation Plan ” [accessed on November 20, 2013]. Available at http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/ASCPayment/Downloads/C_ASC_RTC-2011.pdf.
- Conrad DA, Sales A, Liang SY, Chaudhuri A, Maynard C, Pieper L, Weinstein L, Gans D. Piland N. The Impact of Financial Incentives on Physician Productivity in Medical Groups. Health Services Research. 2002;37(4):885–906. doi: 10.1034/j.1600-0560.2002.57.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtemanche C. Plotzke M. Does Competition from Ambulatory Surgical Centers Affect Hospital Surgical Output? Journal of Health Economics. 2010;29(5):765–73. doi: 10.1016/j.jhealeco.2010.07.003. [DOI] [PubMed] [Google Scholar]
- Cullen KA, Hall MJ. Golosinskiy A. Ambulatory Surgery in the United States, 2006. 2009. , and. National Health Statistics Reports [accessed January 5, 2015]. Available at http://www.cdc.gov/nchs/data/nhsr/nhsr011.pdf. [PubMed] [Google Scholar]
- Davis JE. The Major Ambulatory Surgical Center and How It Is Developed. Surgical Clinics of North America. 1987;67(4):671–92. doi: 10.1016/s0039-6109(16)44279-9. [DOI] [PubMed] [Google Scholar]
- Gabel JR, Fahlman C, Kang R, Wozniak G, Kletke P. Hay JW. Where Do I Send Thee? Does Physician-Ownership Affect Referral Patterns to Ambulatory Surgery Centers? Health Affairs. 2008;27(3):w165–74. doi: 10.1377/hlthaff.27.3.w165. [DOI] [PubMed] [Google Scholar]
- Health Resources and Services Administration. 2013. . “ Area Resource File ” [accessed on March 21, 2013]. Available at http://arf.hrsa.gov.
- Hollenbeck BK, Hollingsworth JM, Dunn RL, Zaojun Y. Birkmeyer JD. Ambulatory Surgery Center Market Share and Rates of Outpatient Surgery in the Elderly. Surgical Innovation. 2010;51:340–5. doi: 10.1177/1553350610377211. [DOI] [PubMed] [Google Scholar]
- Hollenbeck BK, Dunn RL, Suskind AM, Zhang Y, Hollingsworth JM. Birkmeyer JB. Ambulatory Surgery Centers and Outpatient Procedure Use among Medicare Beneficiaries. Medical Care. 2014;52(10):926–31. doi: 10.1097/MLR.0000000000000213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollingsworth JM, Ye Z, Strope SA, Krein SL, Hollenbeck AT. Hollenbeck BK. Urologist Ownership of Ambulatory Surgery Centers and Urinary Stone Surgery Use. Health Services Research. 2009;44(4):1370–84. doi: 10.1111/j.1475-6773.2009.00966.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollingsworth JM, Ye Z, Strope SA, Krein SL, Hollenbeck AT. Hollenbeck BK. Physician-Ownership of Ambulatory Surgery Centers Linked to Higher Volume of Surgeries. Health Affairs. 2010;29(4):683–9. doi: 10.1377/hlthaff.2008.0567. [DOI] [PubMed] [Google Scholar]
- Hollingsworth JM, Krein SL, Ye Z, Kim HM. Hollenbeck BK. Opening of Ambulatory Surgery Centers and Procedure Use in Elderly Patients: Data from Florida. Archives of Surgery. 2011;146(2):187–93. doi: 10.1001/archsurg.2010.335. [DOI] [PubMed] [Google Scholar]
- Hollingsworth JM, Saigal CS, Lai JC, Dunn RL, Strope SA, Hollenbeck BK Urologic Diseases in America Project. Surgical Quality among Medicare Beneficiaries Undergoing Outpatient Urological Surgery. Journal of Urology. 2012;188(4):1274–8. doi: 10.1016/j.juro.2012.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klabunde CN, Potosky AL, Legler JM. Warren JL. Development of a Comorbidity Index Using Physician Claims Data. Journal of Clinical Epidemiology. 2000;53(12):1258–67. doi: 10.1016/s0895-4356(00)00256-0. [DOI] [PubMed] [Google Scholar]
- Lynk WJ. Longley CS. The Effect of Physician-Owned Surgicenters on Hospital Outpatient Surgery. Health Affairs. 2002;21(4):215–21. doi: 10.1377/hlthaff.21.4.215. [DOI] [PubMed] [Google Scholar]
- MedPAC. 2013a. . “ A Data Book: Healthcare Spending and the Medicare Program ” [accessed on November 8, 2013]. Available at http://www.medpac.gov/documents/Jun13DataBookEntireReport.pdf.
- MedPAC. 2013b. . “ Medicare Payment Policy ” [accessed on November 7, 2013]. Available at http://www.medpac.gov/documents/Mar13_EntireReport.pdf.
- Mitchell JM. Effect of Physician Ownership of Specialty Hospitals and Ambulatory Surgery Centers on Frequency of Use of Outpatient Orthopedic Surgery. Archives of Surgery. 2010;145(8):732–8. doi: 10.1001/archsurg.2010.149. [DOI] [PubMed] [Google Scholar]
- Office of Inspector General. Quality Oversight of Ambulatory Surgery Centers: A System in Neglect. 2002. . Department of Health and Human Services Report OEI-01-00-0450 [accessed January 5, 2015]. Available at http://oig.hhs.gov/oei/reports/oei-01-00-00450.pdf. [Google Scholar]
- Plotzke MR. Courtemanche C. Does Procedure Profitability Impact Whether an Outpatient Surgery is Performed at an Ambulatory Surgery Center or Hospital? Health Economics. 2011;20(7):817–30. doi: 10.1002/hec.1646. [DOI] [PubMed] [Google Scholar]
- Schaefer MK, Jhung M, Dahl M, Schillie S, Simpson C, Llata E, Link-Gelles R, Sinkowitz-Cochran R, Patel P, Bolyard E, Sehulster L, Srinivasan A. Perz JF. Infection Control Assessment of Ambulatory Surgical Centers. Journal of the American Medical Association. 2010;303(22):2273–9. doi: 10.1001/jama.2010.744. [DOI] [PubMed] [Google Scholar]
- Spreeuwenberg MD, Bartak A, Croon MA, Hagenaars JA, Busschbach JJV, Andrea H, Twisk J. Stijnen T. The Multiple Propensity Score as Control for Bias in the Comparison of more than Two Treatment Arms: An Introduction from a Case Study in Mental Health. Medical Care. 2010;48(2):166–74. doi: 10.1097/MLR.0b013e3181c1328f. [DOI] [PubMed] [Google Scholar]
- Strope SA, Daignault S, Hollingsworth JM, Ye Z, Wei JT. Hollenbeck BK. Physician Ownership of Ambulatory Surgery Centers and Practice Patterns for Urological Surgery: Evidence from the State of Florida. Medical Care. 2009;47(4):403–10. doi: 10.1097/mlr.0b013e31818af92e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wennberg JE. The Dartmouth Atlas of Health Care in the United States. Chicago, IL: AHA Press; 1999. [Google Scholar]
- Wennberg JE, Barnes BA. Zubkoff M. Professional Uncertainty and the Problem of Supplier-Induced Demand. Social Science & Medicine. 1982;16(7):811–24. doi: 10.1016/0277-9536(82)90234-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Appendix SA2: Common Procedures Performed in Both the Hospital and ASC That Comprised the Three Specialty Group Analyses.


