Abstract
Objective
To estimate the relationship between physicians' acceptance of new Medicaid patients and access to health care.
Data Sources
The National Ambulatory Medical Care Survey (NAMCS) Electronic Health Records Survey and the National Health Interview Survey (NHIS) 2011/2012.
Study Design
Linear probability models estimated the relationship between measures of experiences with physician availability among children on Medicaid or the Children's Health Insurance Program (CHIP) from the NHIS and state-level estimates of the percent of primary care physicians accepting new Medicaid patients from the NAMCS, controlling for other factors.
Principal Findings
Nearly 16 percent of children with a significant health condition or development delay had a doctor's office or clinic indicate that the child's health insurance was not accepted in states with less than 60 percent of physicians accepting new Medicaid patients, compared to less than 4 percent in states with at least 75 percent of physicians accepting new Medicaid patients. Adjusted estimates and estimates for other measures of access to care were similar.
Conclusions
Measures of experiences with physician availability for children on Medicaid/CHIP were generally good, though better in states where more primary care physicians accepted new Medicaid patients.
Keywords: State health policies, primary care, access, demand, utilization of services
Under the Affordable Care Act (ACA), states will have the option to expand Medicaid coverage to some additional adults with full federal financing from 2014 to 2016, potentially adding millions of people to the program (Supreme Court of the United States 2012). Medicaid payment rates for some primary care services provided by primary care physicians are also increasing to 100 percent of Medicare rates in 2013 and 2014. This payment change will greatly affect Medicaid payment rates in states where rates are well below Medicare rates (Zuckerman and Goin 2012). Although previous literature has found that measures of access to care are generally good for individuals on Medicaid compared to private insurance (Long, Coughlin, and King 2007; Perry and Kenney 2007), authors have posited that access measures for those on Medicaid may be related to provider reimbursement rates. In particular, a positive association between Medicaid physician fees and the percent of physicians accepting Medicaid patients has generally been found, though estimated impact sizes vary with some estimating a small effect (Sloan, Mitchell, and Cromwell 1978; Decker 2007) and others a large effect (Hadley 1979; Showalter 1997).
Although determinants of physician participation in Medicaid other than physician fees have been explored (for example, Sloan, Mitchell, and Cromwell 1978; Decker 2007, 2012; Cunningham and O'Malley 2009), the focus of research has been on Medicaid physician payment rates both because they are known to be low in some states compared to other payers and because they are changeable by state legislatures. Although the literature linking Medicaid physician payment rates to physician participation in Medicaid has a long history, the literature linking Medicaid physician payment rates to measures of access to or use of health care is smaller, has more mixed results, and mostly uses data that are fairly old (Long, Settle, and Stuart 1986; Cohen 1993; Baker and Beeson Royalty 2000; Decker 2009). One challenge is that state Medicaid physician payment rates have only been documented for some services through state surveys performed every few years (Zuckerman, Williams, and Stockley 2009; Zuckerman and Goin 2012). In contrast, state-level measures of physician participation in Medicaid are available from several data sources (Cunningham and O'Malley 2009; Decker 2013; Rhodes et al. 2014) and are now available for every state annually (Decker 2012, 2013). However, the utility of these state-level measures in predicting access to health care among Medicaid beneficiaries is not known. Lack of participation in Medicaid among some physicians not located near places where Medicaid patients live or work may not affect access measures, leaving the utility of these aggregate, state-level measures uncertain.
This study first documents state-level rates of acceptance of new Medicaid patients among primary care physicians in 2011/2012, before the Medicaid physician fees for some physicians and services began to increase in 2013. The article also analyzes the relationship between state-level rates of acceptance of new Medicaid patients during this pre-ACA period and measures of experience with physician availability among children on Medicaid or the Children's Health Insurance Program (CHIP). The focus of the analysis is on children (younger than 18) since children rely mostly on health care provided by primary care physicians, and since coverage of children by Medicaid/CHIP is common. For example, 2013 estimates indicate that nearly 43 percent of children had public health insurance coverage (almost entirely through Medicaid or the CHIP), compared to less than 17 percent of nonelderly adults (Cohen and Martinez 2013).
Data and Methods
This article used data from two annual surveys, conducted by the Centers for Disease Control and Prevention's National Center for Health Statistics (NCHS), both of which are now capable of producing state-level estimates for many states. Information on acceptance of new patients among office-based primary care physicians came from the 2011/2012 National Ambulatory Medical Care Survey (NAMCS) Electronic Health Records Survey. NAMCS is an annual, nationally representative survey of office-based physicians (M.D.s and D.O.s), excluding radiologists, anesthesiologists, and pathologists.1 The NAMCS Electronic Health Records Survey began in 2008 and, since 2010, has followed a design stratified by state and physician specialty. State-level estimates are available through the NCHS Research Data Center beginning in 2010, and questions about acceptance of new patients were added in 2011. Those who accepted new patients were questioned about which payment forms they accepted. Those who accepted no new patients were considered not to accept either privately insured or Medicaid patients. Unweighted response rates for the survey were 64 and 67 percent in 2011 and 2012, respectively. For this article, information on acceptance of new Medicaid and privately insured patients was considered for physicians in the primary care specialties of general/family practice or pediatrics,2 yielding a sample of 2,478 physicians in 2011 and 2012 combined, after dropping physicians in a few states (see below) plus 198 physicians due to missing information on acceptance of new Medicaid or privately insured patients. The final sample size by state ranged from 33 to 84 primary care physicians.
Information on measures of experiences with physician availability came from the National Health Interview Survey (NHIS), a continuing national household survey of the civilian, noninstitutionalized population that follows a stratified probability sample design.3 Information on insurance status for children came from the NHIS person files, though the analysis sample was limited to those in the sample child file in which the questions pertaining to experiences with physician availability were asked about only one child per household. Unweighted survey response rates for sample children were 75 percent in 2011 and 70 percent in 2012. For both the NHIS and the NAMCS Electronic Health Record Survey, sample weights reflect the probability of selection with adjustment for nonresponse. Two years of data were combined for analyses of both the NAMCS Electronic Health Records Survey and NHIS in order to maximize sample size by state. In both surveys, observations from a few states were dropped because of limited sample size in the state for one of the surveys. These states were Alaska, Delaware, Minnesota, and Wyoming, plus the District of Columbia. For the NHIS, the analysis sample was restricted to children younger than 18 who were on Medicaid, CHIP, or privately insured, and who were not on Medicare. Since the measures of physician availability consisted of measures related to access to health care in the year prior to the NHIS interview, the sample also excluded any children who had been uninsured at any point during the year prior to interview. The number of observations for children on Medicaid/CHIP was 9,009, after dropping less than 0.5 percent of the sample because of missing values on any of the variables used in the analysis, or because they were in Alaska, Delaware, Minnesota, and Wyoming, or the District of Columbia. The sample size for privately insured children (see below) was 11,778.
Although the focus of the article is on the relationship between state-level measures of physician participation in Medicaid and children's experience with physician availability, two supplementary analyses were also conducted. The first consisted of an analysis of measures of children's experience with physician availability as a function of one determinant of physician participation identified from previous literature, the Medicaid-to-Medicare fee ratio.4 The fee ratio was divided into three categories with at least 20 percent of the sample in each category and used information from Zuckerman and Goin (2012). The second and final analysis consisted of an analysis of NHIS sample adults. Inclusion criteria were similar to those for children, resulting in a sample of 3,915 adults on Medicaid. For this analysis, physician participation among physicians in general/family practice and internal medicine were considered, though results (data not shown) including obstetricians/gynecologists were similar. It is hypothesized that the relationship between physician participation in Medicaid and adults' experience with physician availability is similar to the relationship for children, though the relationship may be harder to identify since fewer adults than children are on Medicaid, resulting in a smaller sample size of adults compared to children on Medicaid.
The measures of experiences with physician availability consisted of three new measures added to the NHIS in 2011, plus three other measures of access to care hypothesized to be related to physician availability. The first new measure examined seemed the one most closely related to physician acceptance of new Medicaid patients. This consisted of a question asking if the sampled child's family (or similarly for adults) had been told by a doctor's office or clinic in the past year that they did not accept the child's source of health insurance coverage. The other new NHIS questions concerned whether in the past year the family had had trouble finding a general doctor or provider to see the child, and whether the family was not able to find a general doctor or provider to see the child. The three other measures consisted of whether the child had not received care in the past year because the wait to get an appointment was too long, whether the child had not received care in the past year because the wait in the doctor's office was too long, and whether the child had had at least one visit with a doctor or other health care professional in the past year (at a doctor's office, a clinic, or some other place—but not including at an emergency room, at home, or dental visits). These measures of experiences with physician availability were examined for all children younger than 18 and for the subset of children with a significant health condition or a development delay.5 Since questions about development delay were only asked for children at least 2 years old, the sample of children with a significant health condition or development delay was limited to children aged 2–17. This consisted of 1,485 such children on Medicaid/CHIP.
Using data from the NAMCS sample, the percent of primary care physicians accepting new Medicaid patients was estimated by state and compared to that for acceptance of new privately insured patients. The association between acceptance of new Medicaid patients by state in the NAMCS and measures of experiences with physician availability among children in the NHIS was then examined. Specifically, linear probability models were estimated predicting whether children in the NHIS sample had each measure of experience with physician availability as a function of the percent of physicians accepting new Medicaid patients in the state of residence.6 Some models included covariates consisting of other possible state-level predictors of experiencing problems with physician availability (the number of general/family practitioners or pediatricians per person in 20127 and the Medicaid managed care penetration rate in 20118), and child or family characteristics including child gender, race/ethnicity, general health status, and the ratio of family income to the poverty level.9 For 18 states considered to have reliable state-level estimates of the percent of children on Medicaid/CHIP with at least one visit with a physician or health care professional in the past year, the relationship between these estimates and the percent of physicians accepting new Medicaid patients by state was also graphed.10
Since this study used exclusively cross-sectional data, it is difficult to draw conclusions about causality from the associations between state-level measures of acceptance of new Medicaid patients among primary care physicians and measures of experiences with physician availability among children on Medicaid. For example, if acceptance rates for new Medicaid patients are exceptionally low in states with poor access measures in general, we might see a spurious correlation between acceptance of new Medicaid patients and the measures of experience with physician availability examined. To reduce this concern, some models including a comparison group of privately insured children were estimated. These models considered the effect of state-level measures of the acceptance of new Medicaid patients among primary care physicians on children with Medicaid/CHIP coverage compared to the effect on privately insured children and took the following general form below:
where Access measures (i.e., measures of experiences with physician availability) for child i in state s are modeled as a function of Aceptcaid, the percent of primary care physicians accepting new Medicaid patients in the child's state of residence; Medicaid, an indicator for the child being on Medicaid/CHIP rather than privately insured; and an interaction between Medicaid and Aceptcaid, measuring the differential effect of acceptance of new Medicaid patients for children on Medicaid/CHIP relative to privately insured children. The use of children on private insurance as a comparison group should help to mitigate any correlation between a state's percent of physicians accepting new Medicaid patients and other omitted state-level factors that may be correlated with children's access to health care. Control variables measured both at the state (States) and child/family levels (Childis) were also included, as listed above. In addition to estimating models with a linear measure of the percent of physicians accepting new Medicaid patients, models predicting the effect of low (<60 percent), medium (60–74 percent), and high (≥75 percent) state percentages of primary care physicians accepting new Medicaid patients were also estimated to ease interpretation. (These categories were chosen so that at least 20 percent of the NHIS sample of Medicaid/CHIP children is in each category.) All estimates used sample weights, and analyses allow for arbitrary correlation of standard errors by state (Moulton 1990; Donald and Lang 2007).
Results
Figure1a shows substantial variation in the percent of physicians accepting new Medicaid patients by state. Among the 46 states examined in this study, the percent of primary care physicians accepting new Medicaid patients ranged from a low of 42.8 percent in New Jersey to a high of 95.0 percent in Mississippi. These figures are similar to those presented in Decker (2013), which included physicians in internal medicine as primary care physicians since that paper did not focus on care of children. The percent of physicians accepting new privately insured patients varied considerably less across states than the percent accepting new Medicaid patients. The percent accepting new privately insured patients varied from a low of 69.8 percent in Maine to a high of 97.1 percent in Idaho. (Figures also presented in Appendix Table S1.)
Figure 1.
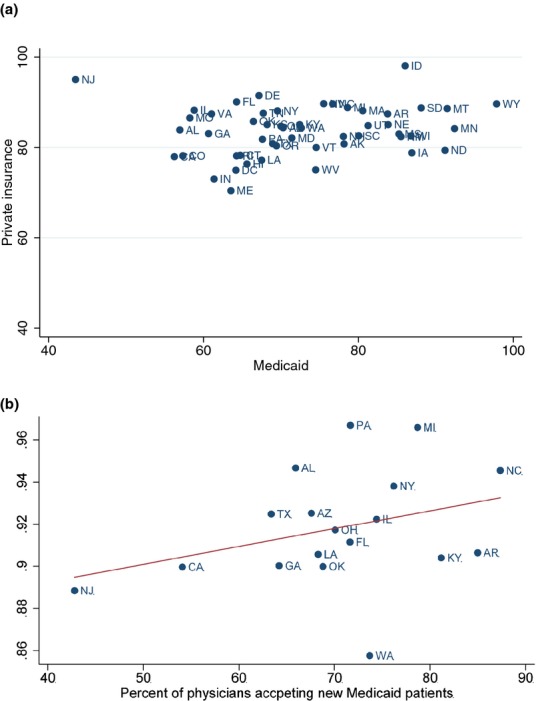
- Note: The intercept in this figure (for states pictured) is 88.9 and the slope is 0.09.
Table1 presents means of the measures of experience with physician availability from the NHIS for both children on Medicaid/CHIP and privately insured children. Although each measure shows statistically significant more access problems on Medicaid/CHIP compared to private insurance, the differences were small and the percent of children experiencing problems with physician availability according to these measures was small. For example, 4.1 percent of the families of children on Medicaid/CHIP reported having a doctor's office or clinic indicate that they did not accept the child's insurance in the past year compared to 1.0 percent for privately insured children (p < .001). The percent of children on Medicaid/CHIP whose families reported having trouble finding a provider to see the child in the past year was 2.1 percent compared to 0.6 percent for privately insured children (p < .001).
Table 1.
Measures of Experience with Physician Availability for Children on Medicaid or CHIP and Privately Insured Children (NHIS 2011/2012)
| Percents | All | Percent of Primary Care Physicians Accepting New Medicaid Patients | ||
|---|---|---|---|---|
| <60% | 60–74% | 75%+ | ||
| Children on Medicaid/CHIP (n = 9,009) | ||||
| Doctor's office or clinic indicated that they did not accept child's insurance | 4.06 (0.30) | 5.31*** (0.83) | 4.37*** (0.44) | 2.73 (0.41) |
| Had trouble finding a general doctor or provider to see the child | 2.07 (0.22) | 2.86** (0.62) | 2.33** (0.33) | 1.12 (0.26) |
| Was not able to get a general doctor or provider to see the child | 0.56 (0.12) | 1.49*** (0.40) | 0.45* (0.16) | 0.13 (0.07) |
| Did not get care in the last year because it took too long to get an appointment | 6.05 (0.33) | 7.49*** (0.69) | 6.51*** (0.53) | 4.36 (0.44) |
| Did not get care in the past year because the wait in the doctor's office was too long | 6.03 (0.42) | 8.63*** (0.90) | 6.24*** (0.65) | 3.99 (0.52) |
| At least one visit with a doctor or health care professional in the past year | 91.96 (0.42) | 89.66*** (1.06) | 91.89** (0.63) | 93.61 (0.58) |
| Privately insured children (n = 11,778) | ||||
| Doctor's office or clinic indicated that they did not accept child's insurance | 0.95 (0.11) | 0.73 (0.16) | 1.04 (0.18) | 0.94 (0.19) |
| Had trouble finding a general doctor or provider to see the child | 0.62 (0.09) | 0.67 (0.18) | 0.66 (0.12) | 0.54 (0.14) |
| Was not able to get a general doctor or provider to see the child | 0.11 (0.03) | 0.03 (0.03) | 0.16 (0.06) | 0.07 (0.04) |
| Did not get care in the last year because it took too long to get an appointment | 3.09 (0.19) | 3.56 (0.47) | 3.08 (0.29) | 2.81 (0.32) |
| Did not get care in the past year because the wait in the doctor's office was too long | 2.23 (0.17) | 2.70 (0.40) | 2.22 (0.28) | 1.95 (0.28) |
| At least one visit with a doctor or health care professional in the past year | 93.06 (0.34) | 92.02 (0.73) | 93.46 (0.51) | 93.12 (0.57) |
Notes: The table presents sample means with standard errors in parentheses.
The symbols *, **, and *** indicate that the difference relative to at least 75% is statistically significant at the 10, 5, and 1 percent levels, respectively.
Table1 also presents the percent of children experiencing problems with physician availability across different categories representing the percent of primary care physicians in the child's state of residence that reported accepting new Medicaid patients. For children on Medicaid/CHIP, each measure of physician availability suggested more access problems for children in states with low acceptance of new Medicaid patients among primary care physicians compared to children in states with higher acceptance rates. For example, 5.3 percent of children in states where less than 60 percent of primary care physicians accept new Medicaid patients had an office or clinic say they don't take the child's insurance compared to 2.7 percent in states where at least 75 percent of primary care physicians accept new Medicaid patients. About 90 percent of children in states with less than 60 percent of physicians accepting new Medicaid patients had at least one doctor visit or visit with a health care professional in the past year compared to nearly 94 percent of children in states where at least 75 percent of physicians accept new Medicaid patients. The percent of privately insured children experiencing problems with physician availability did not vary significantly according to the percent of physicians accepting new Medicaid patients.
Table2 shows the association between the percent of physicians accepting new Medicaid patients in a state and measures of experience with physician availability for children on Medicaid compared to children with private insurance, controlling for covariates. Estimates of the relationship between acceptance of new Medicaid patients by physicians and measures of experience with physician availability were similar whether controlling for covariates or not. For example, unadjusted estimates from Table1 showed that children in states where less than 60 percent of physicians accepted new Medicaid patients were about 4 percentage points less likely to have had a physician visit in the past year compared to children in states where at least 75 percent of physicians accepted new Medicaid patients. Estimates in Table2 controlling for covariates and using either the Medicaid/CHIP sample or the combined Medicaid-private insurance sample both gave estimates of about a 3 percentage point difference. Estimates (not reported) using linear measures of the percent of physicians accepting new Medicaid patients by state were similar, showing, for example, a statistically significant positive relationship between the percent of physicians accepting new Medicaid patients and the probability that a child on Medicaid had seen a physician in the past year. In order to picture this relationship by state, Figure1b shows state-level measures of the percent of physicians accepting new Medicaid patients for the NAMCS and the percent of children on Medicaid/CHIP who have had at least one visit with a doctor or health care professional in the past year for the 18 states considered to have reliable estimates of the latter measure.11
Table 2.
The Association between Low State Acceptance of New Medicaid Patients and Measures of Experience with Physician Availability for Children on Medicaid or CHIP (NHIS 2011/2012)
| Percentage Point Effect Relative to Children in States with Acceptance of at Least 75% (Standard Error in Parentheses) | Percent of Primary Care Physicians Accepting New Medicaid Patients | |
|---|---|---|
| <60% | 60–74% | |
| Adjusted using Medicaid/CHIP sample (n = 9,009) | ||
| Doctor's office or clinic indicated that they did not accept child's insurance | 4.16*** (1.15) | 1.79** (0.72) |
| Had trouble finding a general doctor or provider to see the child | 2.08*** (0.77) | 1.38*** (0.51) |
| Was not able to get a general doctor or provider to see the child | 1.57*** (0.45) | 0.37 (0.22) |
| Did not get care in the last year because it took too long to get an appointment | 2.91** (1.17) | 1.63** (0.79) |
| Did not get care in the past year because the wait in the doctor's office was too long | 1.54 (1.13) | 0.55 (0.71) |
| At least one visit with a doctor or health care professional in the past year | −2.88* (1.61) | −1.37 (0.87) |
| Adjusted using Medicaid/CHIP and private insurance sample (n = 20,787) | ||
| Doctor's office or clinic indicated that they did not accept child's insurance | 3.39*** (0.97) | 1.66** (0.64) |
| Had trouble finding a general doctor or provider to see the child | 1.72** (0.68) | 1.20** (0.45) |
| Was not able to get a general doctor or provider to see the child | 1.43*** (0.42) | 2.99 (0.19) |
| Did not get care in the last year because it took too long to get an appointment | 2.79*** (0.94) | 1.94*** (0.72) |
| Did not get care in the past year because the wait in the doctor's office was too long | 2.42** (1.01) | 1.18* (0.69) |
| At least one visit with a doctor or health care professional in the past year | −2.98** (1.40) | −1.31 (0.86) |
Notes: The symbols *, **, and *** indicate statistical significance at the 10, 5, and 1 percent levels, respectively, relative to “75%+”. The first panel of the table reports coefficients (with standard errors in parentheses) on dichotomous variables for each category of acceptance of new Medicaid patients. The second panel reports the sum of the coefficients (with standard errors in parentheses) on a dichotomous variable representing that the child is on Medicaid/CHIP (rather than privately insured) and that dichotomous variable multiplied by the measure of state acceptance of new Medicaid patients. Coefficients for control variables included are presented in Appendix Table S2.
Table3 reports means for the NHIS measures of experience with physician availability for children with a significant health condition or a development delay, and by categories measuring the percent of physicians in a child's state of residence who accept new Medicaid patients. The percent of children on Medicaid/CHIP whose families reported problems with physician availability was higher for children with one of these conditions than for the group of all children on Medicaid. For example, 6.6 percent of families with a child with a significant health condition or development delay reported having a provider not accept their child's insurance in the past year. For children with a significant health condition or development delay and on Medicaid/CHIP, families of those living in a state where less than 60 percent of doctors accept new Medicaid patients were about 12 (15.5–3.5) percentage points more likely than those living in a state where at least 75 percent of physicians accept Medicaid to have reported not having their insurance accepted and nearly 7 (8.5–1.8) percentage points more likely to have reported having trouble finding a provider to treat them. Adjusted estimates (available upon request) using either the Medicaid or the combined Medicaid-private insurance sample are very similar.
Table 3.
The Association between State Acceptance of New Medicaid Patients or the State Primary Care Medicaid-to-Medicare Fee Ratio and Measures of Experience with Physician Availability for Children on Medicaid or CHIP with a Significant Health Condition or Development Disability (NHIS 2011/2012)
| Unadjusted Percent for the Medicaid/CHIP Sample (n = 1,485) | All | Percent of Primary Care Physicians Accepting New Medicaid Patients | ||
|---|---|---|---|---|
| <60% | 60–74% | 75%+ | ||
| Doctor's office or clinic indicated that they did not accept child's insurance | 6.62 (0.91) | 15.48*** (3.45) | 6.11 (1.18) | 3.53 (1.04) |
| Had trouble finding a general doctor or provider to see the child | 3.34 (0.70) | 8.52*** (2.65) | 2.90 (0.95) | 1.82 (0.70) |
| Did not get care in the last year because it took too long to get an appointment | 8.79 (0.97) | 13.72** (2.87) | 9.38* (1.49) | 5.85 (1.22) |
| Did not get care in the past year because the wait in the doctor's office was too long | 6.99 (0.92) | 10.15** (2.24) | 7.83* (1.48) | 4.48 (1.19) |
| At least one visit with a doctor or health care professional in the past year | 95.77 (0.72) | 89.99** (3.16) | 96.86 (0.71) | 96.74 (0.96) |
| Medicaid-to-Medicare Primary Care Fee Ratio | All | <50% | 50–74% | 75%+ |
| Doctor's office or clinic indicated that they did not accept child's insurance | 6.62 (0.91) | 9.78** (2.19) | 6.19 (1.17) | 3.61 (1.34) |
| Had trouble finding a general doctor or provider to see the child | 3.34 (0.70) | 6.02* (1.65) | 2.67 (0.91) | 2.20 (1.03) |
| Did not get care in the last year because it took too long to get an appointment | 8.79 (0.97) | 9.11** (2.04) | 10.27*** (1.44) | 4.06 (1.04) |
| Did not get care in the past year because the wait in the doctor's office was too long | 6.99 (0.92) | 9.00** (1.95) | 7.34* (1.35) | 4.02 (1.36) |
| At least one visit with a doctor or health care professional in the past year | 95.77 (0.72) | 93.41 (2.04) | 96.98 (0.68) | 96.03 (1.25) |
Notes: The table presents sample means with standard errors in parentheses. The symbols *, **, and *** indicate that the difference relative to at least 75% is statistically significant at the 10, 5, and 1 percent levels, respectively.
For children with a health condition or development delay, the bottom panel of Table3 directly investigates the effect of the Medicaid-to-Medicare fee ratio on measures of experience with physician availability instead of investigating the effect of the intermediary variable—physician acceptance of new Medicaid patients. Although the fee ratio is only one predictor of physician participation in Medicaid, the relationship is statistically significant for most measures of experience with physician availability. For example, nearly 10 percent of children with a health condition or development delay had had a doctor's office or clinic indicate that they did not take the child's insurance in states with fee ratios under 50 percent compared to less than 4 percent of children in states with fee ratios of at least 75 percent. Similarly, about 9 percent of children with a health condition or development delay did not get care in the past year because the wait in the doctor's office was too long in states with a fee ratio under 50 percent compared to about 4 percent for children in states with a fee ratio of at least 75 percent. (Again, estimates adjusted using either the Medicaid sample or the combined Medicaid-private insurance sample were similar and are available upon request.)
The last table explores the relationship between primary care physicians' acceptance of new Medicaid patients and the Medicaid-to-Medicare fee ratio and measures of experience with physician availability among adults on Medicaid. Although estimates are less precise, the results show similar patterns compared to those for children. For example, nearly 10 percent of adults on Medicaid reported not receiving care in the past year because the wait in the doctor's office was too long in states with less than 60 percent of physicians accepting new Medicaid patients compared to less than 5 percent in states with at least 75 percent of physicians accepting new Medicaid patients. About 82 percent of Medicaid adults had seen a physician in the past year in states with fee ratios under 50 percent compared to nearly 87 percent in states with fee ratios of at least 75 percent (Table4).
Table 4.
The Association between State Acceptance of New Medicaid Patients or the State Primary Care Medicaid-to-Medicare Fee Ratio and Measures of Experience with Physician Availability for Adults Aged 18–64 on Medicaid (NHIS 2011/2012)
| Unadjusted Percent for the Medicaid/CHIP Sample (n = 3,915) | All | Percent of Primary Care Physicians Accepting New Medicaid Patients | ||
|---|---|---|---|---|
| <60% | 60–74% | 75%+ | ||
| Doctor's office or clinic indicated that they did not accept adult's insurance | 7.93 (0.63) | 8.45* (0.80) | 7.73 (1.05) | 5.19 (1.75) |
| Had trouble finding ha general doctor or provider to see the adult | 4.69 (0.47) | 5.00 (0.61) | 4.39 (0.79) | 4.27 (1.55) |
| Was not able to get a general doctor or provider to see the adult | 1.39 (0.26) | 1.47 (0.32) | 1.28 (0.45) | 1.40 (1.09) |
| Did not get care in the last year because it took too long to get an appointment | 8.73 (0.67) | 8.92 (0.84) | 8.33 (1.17) | 9.60 (2.06) |
| Did not get care in the past year because the wait in the doctor's office was too long | 7.97 (0.58) | 9.50*** (0.80) | 6.51*** (0.80) | 4.91 (0.92) |
| At least one visit with a doctor or health care professional in the past year | 85.40 (0.82) | 83.73*** (1.15) | 86.89 (1.30) | 89.31 (1.47) |
| Medicaid-to-Medicare Primary Care Fee Ratio | <50% | 50–74% | 75%+ | |
| Doctor's office or clinic indicated that they did not accept adult's insurance | 7.75 (1.00) | 9.00* (0.99) | 6.01 (1.41) | |
| Had trouble finding a general doctor or provider to see the adult | 4.22 (0.76) | 5.64*** (0.73) | 2.89 (0.75) | |
| Was not able to get a general doctor or provider to see the adult | 1.36** (0.44) | 1.75*** (0.41) | 0.37 (0.21) | |
| Did not get care in the last year because it took too long to get an appointment | 8.28 (1.14) | 9.18 (0.99) | 8.11 (1.28) | |
| Did not get care in the past year because the wait in the doctor's office was too long | 7.71 (0.94) | 8.00 (0.89) | 8.81 (1.45) | |
| At least one visit with a doctor or health care professional in the past year | 82.28* (1.41) | 87.81 (1.17) | 86.48 (1.83) | |
Notes:The table presents sample means with standard errors in parentheses.
The symbols *, **, and *** indicate that the difference relative to at least 75% is statistically significant at the 10, 5, and 1 percent levels, respectively.
[Correction added on 13 April 2015, after first online publication: The numbers in the “All” column of Table4 have been corrected from “9.45 (1.20), 4.66 (0.78), 1.18 (0.44), 9.13 (1.08), 8.38 (1.03), 89.72 (1.18)” to “7.93 (0.63), 4.69 (0.47), 1.39 (0.26), 8.73 (0.67), 7.97 (0.58), 85.40 (0.82)”, respectively.]
Discussion
During the 2011/2012 period prior to implementation of most ACA provisions, the percent of primary care physicians accepting new Medicaid patients varied widely by state. Among the 46 states examined in this article, the percent accepting new Medicaid patients ranged from a low of 42.8 percent in New Jersey to a high of 95.0 percent in Mississippi. The percent of primary care physicians accepting new privately insured patients varied less by state. Measures of experiences with physician availability were worse for children on Medicaid/CHIP compared to private insurance, though the differences were small and the percent of children experiencing problems with physician availability was small. This is consistent with the fact that Medicaid covers a wide variety of health care services with no copayments for children.
However, measures of experiences with physician availability were worse for children with significant health conditions or a development delay than for children overall. For example, nearly 7 percent of children on Medicaid/CHIP with a significant health condition or development delay had families report that they had had a doctor's office or clinic saying they did not accept the child's insurance source. Measures of experiences with physician availability were better for children on Medicaid/CHIP who live in states with higher rates of acceptance of new Medicaid patients compared to other children. For example, only about 4 percent of children on Medicaid/CHIP with a significant health condition or developmental delay had a doctor's office or clinic indicate that the child's health insurance was not accepted in states with at least 75 percent of primary care physicians accepting new Medicaid patients, compared to nearly 16 percent of children living in states with less than 60 percent of physicians accepting new Medicaid patients.
Although this study used purely cross-sectional data, the comparison of differences in measures of experiences with physician availability for children on Medicaid/CHIP to those for privately insured children in states with different percentages of physicians accepting new Medicaid patients helped control for any overall correlation between acceptance rates and unmeasured attributes of states affecting experiences with physician availability for children. A positive correlation was found between both higher acceptance of new Medicaid patients and higher Medicaid-to-Medicare fee ratios and improved measures of experiences with physician availability for Medicaid/CHIP patients. These findings, together with previous literature documenting a link between Medicaid physician fees and the percent of physicians accepting Medicaid patients (Sloan, Mitchell, and Cromwell 1978; Hadley 1979; Showalter 1997;Decker 2007), imply that higher physician payment rates should be expected to improve access measures for Medicaid patients, though the fact that the increases in Medicaid fees occurring in some states in 2013 and 2014 may be temporary could mitigate this effect.
Although greater acceptance of Medicaid patients among primary care physicians was found to be associated with improved measures of experiences with physician availability for children on Medicaid/CHIP, this effect in improving access is undoubtedly not as large as the effect of providing health insurance coverage itself. This study reported that about 2 percent of children on Medicaid/CHIP had families indicate that they had had trouble finding a provider to see their child and nearly 92 percent had seen a doctor or health care professional in the past year. Although not reported, comparable figures for uninsured children were 6.6 percent and less than 52 percent, respectively. Although the effect of different insurance designs and provider reimbursement policies may be important, insurance coverage of children overall is clearly correlated with measures of access to health care.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This was work was not sponsored. The findings and conclusions in this article are those of the author and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Disclosures: None.
Disclaimers: None.
Notes
More information about the survey is available at http://www.cdc.gov/nchs/ahcd.htm. Accessed September 25, 2013.
Author's analysis of the NAMCS 2010 visit data showed that 81 percent of visits to office-based physicians among children younger than 18 were to general/family practitioners or pediatricians. The next most frequently visited specialty was ophthalmology, which accounted for less than 3 percent of visits.
More information about the survey is available at http://www.cdc.gov/nchs/nhis.htm. Accessed September 25, 2013.
Although many children and adults on Medicaid are enrolled in managed care programs, about half of Medicaid enrollees are either in fee-for-service plans, plans which are prepaid only for inpatient care, or primary care case management programs which often pay on a fee-for-service basis (Centers for Medicare and Medicaid Services [CMS] 2011). Also, a recent U.S. Government Accounting Office [GAO] (2014) report found that payment rates to physicians under Medicaid managed care are highlight corrected across states with Medicaid fee-for-service payment rates for most states.
Having a significant health condition was defined as those with at least one of the following list of conditions: Down syndrome, cerebral palsy, muscular dystrophy, cystic fibrosis, sickle cell anemia, diabetes, autism, arthritis, congenital heart disease, a vision limitation even with correction, any impairment or health problem that requires the child to use special equipment, such as a brace, a wheelchair, or a hearing aid (excluding ordinary eyeglasses or corrective shoes), or any impairment or health problem that limits the child's ability to crawl, walk, run, or play that has lasted or is expected to last at least 12 months. Having a development delay was defined as the family having been told by a doctor that the child had attention deficit hyperactivity disorder, attention deficit disorder, mental retardation, or any other development delay.
Since state estimates of the percent of primary care physicians accepting new Medicaid patients obtained from the NAMCS are measured with error, estimates of their effect on outcomes in the NHIS data will be subject to attenuation bias (i.e., biased toward zero).
Data on the number of physicians by specialty and state come from the Kaiser Family Foundation's “Primary Care Physicians by Field” Available at http://kff.org/other/state-indicator/primary-care-physicians-by-field/. Accessed October 18, 2013. State population data in 2012 came from the U.S. Census Bureau, Table2: Cumulative Estimates of Resident Population Change for the United States, Regions, States, and Puerto Rico and Region and State Rankings: April 1, 2010 to July 1, 2012 (NST-EST2012-02). Released December 2012. Available at http://www.census.gov/popest/data/state/.../2012/tables/NST-EST2012-04.xls. Accessed October 18, 2013.
These data came from the Centers for Medicaid and Medicare Services, “Medicaid Managed Care Enrollment Report: Summary Statistics as of July 1, 2011.” Available at http://www.medicaid.gov/.../2011-Medicaid-MC-Enrollment-Report.pdf. Accessed October 18, 2013.
Information on income relative to the poverty level came from the NCHS imputed income files. The first of five available imputation files was used. Analyses relying on multiple-imputation methods would result in higher standard errors on the income control variable compared to single-imputation methods that do not account for the extra uncertainly due to imputation. In an analysis using NHIS 2001, for example, Schenker et al. (2006) found that standard errors for the percentage of persons aged 45–64 in fair or poor health by category of family income relative to poverty were underestimated by up to 15 percent, using a single compared to a multiple imputation method for observations missing income.
Reliable estimates were considered to be those that were based on at least 150 sampled children, to have a relative standard error (RSE) (standard error divided by the estimate itself) less than 30 percent, and an RSE of the complement of the statistic (i.e., the percent of children without at least one visit to a physician or health care professional) less than 50 percent.
These estimates are also contained in Appendix Table S3. Although precise estimates are presented, readers should be cautious not to interpret small differences between states as differences that are statistically significant.
Supporting Information
Additional supporting information may be found in the online version of this article:
Appendix SA1: Acceptance of New Medicaid and Privately Insured Patients among Office-Based Primary Care Physicians.
Appendix SA2: Association between State Acceptance of New Medicaid Patients and Other State and Child Characteristics and the Probability That a Child's Family Had Been Told by a Doctor's Office or Clinic in the Past Year That They Did Not Accept the Child's Health Insurance Coverage.
Appendix SA3: Acceptance of New Medicaid Patients among Office-Based Primary Care Physicians and the Percent of Children on Medicaid or CHIP with at Least One Physician Visit or Visit with a Health Care Professional in the Past Year.
References
- Baker LC. Beeson Royalty A. Medicaid Policy, Physician Behavior, and Health Care for the Low-Income Population. Journal of Human Resources. 2000;35(3):480–502. [Google Scholar]
- Centers for Medicare and Medicaid Services [CMS] 2011. . “ Medicaid Managed Care Enrollment Report Summary Statistics as of July 1, 2011 ” [accessed on May 23, 2014]. Available at http://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Data-and-Systems/Downloads/2011-Medicaid-MC-Enrollment-Report.pdf.
- Cohen JW. Medicaid Physician Fees and Use of Physician and Hospital Services. Inquiry. 1993;30:281–92. [PubMed] [Google Scholar]
- Cohen RA. Martinez ME. Health Insurance Coverage: Early Release of Estimates from the National Health Interview Survey, January–March 2013. National Center for Health Statistics; 2013. , and [accessed on September 25, 2013]. Available at http://www.cdc.gov/nchs/nhis/releases.htm. [Google Scholar]
- Cunningham PJ. O'Malley AS. Do Reimbursement Delays Discourage Medicaid Participation by Physicians? Health Affairs. 2009;28(1):w17–28. doi: 10.1377/hlthaff.28.1.w17. [DOI] [PubMed] [Google Scholar]
- Decker SL. The Effect of Physician Reimbursement Levels on the Primary Care of Medicaid Patients. Review of Economics of the Household. 2007;5(1):95–112. [Google Scholar]
- Decker SL. Changes in Medicaid Physician Fees and Patterns of Ambulatory Care. Inquiry. 2009;46:291–304. doi: 10.5034/inquiryjrnl_46.03.291. [DOI] [PubMed] [Google Scholar]
- Decker SL. In 2011, Nearly One-Third of Physicians Said They Would Not Accept New Medicaid Patients, but Rising Fees May Help. Health Affairs. 2012;31(8):1673–9. doi: 10.1377/hlthaff.2012.0294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Decker SL. Two-Thirds of Primary Care Physicians Accepted New Medicaid Patients in 2011-12: A Baseline to Measure Future Acceptance Rates. Health Affairs. 2013;32(7):1183–7. doi: 10.1377/hlthaff.2013.0361. [DOI] [PubMed] [Google Scholar]
- Donald SG. Lang K. Inferences with Difference in Differences and Other Panel Data. Review of Economics and Statistics. 2007;89(2):221–33. [Google Scholar]
- Hadley J. Physician Participation in Medicaid: Evidence from California. Health Services Research. 1979;14(4):266–80. [PMC free article] [PubMed] [Google Scholar]
- Long SK, Coughlin T. King J. How Well Does Medicaid Work in Improving Access to Care? Health Services Research. 2007;40(1):39–58. doi: 10.1111/j.1475-6773.2005.00341.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long S, Settle RF. Stuart BC. Reimbursement and Access to Physicians' Services under Medicaid. Journal of Health Economics. 1986;5:235–51. doi: 10.1016/0167-6296(86)90016-0. [DOI] [PubMed] [Google Scholar]
- Moulton BR. An Illustration of a Pitfall in Estimating the Effects of Aggregate Variables in Micro Units. Review of Economics and Statistics. 1990;72(2):334–8. [Google Scholar]
- Perry CD. Kenney GM. Preventive Care for Children in Low-Income Families: How Well do Medicaid and State Children's Health Insurance Programs Do? Pediatrics. 2007;I20:e1392–401. doi: 10.1542/peds.2006-3520. [DOI] [PubMed] [Google Scholar]
- Rhodes KV, Kenney GM, Friedman AB, Saloner B, Lawson CC, Chearo D, Wissoker D. Polsky D. Primary Care Access for New Patients on the Eve of Health Care Reform. JAMA Internal Medicine. 2014;174(6):861–9. doi: 10.1001/jamainternmed.2014.20. [DOI] [PubMed] [Google Scholar]
- Schenker N, Trivellore E, Raghunathan P-LC, Makuc DM, Zhang G. Cohen AJ. Multiple Imputation of Missing Income Data in the National Health Interview Survey. Journal of the American Statistical Association. 2006;101(475):924–33. [Google Scholar]
- Showalter MH. Physicians' Cost Shifting Behavior: Medicaid versus Other Patients. Contemporary Economic Policy. 1997;15(2):74–84. [Google Scholar]
- Sloan F, Mitchell J. Cromwell J. Physician Participation in State Medicaid Programs. Journal of Human Resources. 1978;13:211–45. [PubMed] [Google Scholar]
- Supreme Court of the United States. 2012. . “ National Federation of Independent Business et al. v. Sebelius, Secretary of Health and Human Services, et al ” [accessed on July 2, 2012]. Available at http://www.supremecourt.gov/opinions/11pdf/11-393c3a2.pdf.
- U.S. Government Accounting Office [GAO] Medicaid Payment: Comparisons of Selected Services under Fee-for-service, Managed Care, and Private Insurance. Washington, DC: U.S. Government Printing Office; 2014. . GAO-14-533. [Google Scholar]
- Zuckerman S. Goin D. 2012. , and. “ How Much Will Medicaid Physician Fees for Primary Care Rise in 2013? Evidence from a 2012 Survey of Medicaid Physician Fees. ” Kaiser Commission on Medicaid and the Uninsured Issue Paper [accessed on October 17, 2013]. Available at http://kff.org/medicaid/issue-brief/how-much-will-medicaid-physician-fees-for/
- Zuckerman S, Williams AF. Stockley KE. Trends in Medicaid Physician Fees, 2003-2008. Health Affairs. 2009;28(3):w510–9. doi: 10.1377/hlthaff.28.3.w510. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Acceptance of New Medicaid and Privately Insured Patients among Office-Based Primary Care Physicians.
Appendix SA2: Association between State Acceptance of New Medicaid Patients and Other State and Child Characteristics and the Probability That a Child's Family Had Been Told by a Doctor's Office or Clinic in the Past Year That They Did Not Accept the Child's Health Insurance Coverage.
Appendix SA3: Acceptance of New Medicaid Patients among Office-Based Primary Care Physicians and the Percent of Children on Medicaid or CHIP with at Least One Physician Visit or Visit with a Health Care Professional in the Past Year.


