Abstract
Objective
To determine if regions with high Medicare expenditures in a given setting remain high cost over time.
Data Sources/Study Setting
One hundred percent of national Medicare Parts A and B fee-for-service beneficiary claims data and enrollment for 1992–2010.
Study Design
Patients are classified into regions. Claims are price-standardized. Risk adjustment is performed at the beneficiary level using the CMS Hierarchical Condition Categories model. Correlation analyses are conducted.
Data Collection/Extraction Methods
The data were obtained through a contract with CMS for a study performed for the Institute of Medicine.
Principal Findings
High-cost regions in 1992 are likely to remain high cost in 2010. Stability in regional spending is highest in the home health, inpatient hospital, and outpatient hospital settings over this time period. Despite the persistence of a region's relative spending over time, a region's spending levels in all settings except home health tend to regress toward the mean.
Conclusions
Relatively high-cost regions tend to remain so over long periods of time, even after controlling for patient health status and geographic price variation, suggesting that the observed effect reflects real differences in practice patterns.
Keywords: Medicare fee-for-service, Medicare spending
Numerous studies have documented that spending on Medicare patients varies significantly across regions, even for patients with the same health conditions. The authors of the Dartmouth Atlas of Health Care, for instance, found that per capita Medicare reimbursements in Miami were more than twice as high as in Minneapolis (Center for the Evaluative Clinical Services and Dartmouth Medical School 1996). Other studies have also found significant variation in expenditures for end-of-life care (Song et al. 2010), medical and surgical inpatient admissions (Fuchs, McClellan, and Skinner 2004), Cesarean deliveries (Baicker, Buckles, and Chandra 2006), and physician practice norms (Phelps 2000). In the media, Atul Gawande's New Yorker article popularized the notion that variation in physicians' chosen practice patterns drives variation in Medicare costs observed, even in cities geographically nearby one another (Gawande 2009). Gawande uses the Texan cities of McAllen (a high-cost area) and El Paso (a low-cost area) to highlight this point.
Although many previous analyses examine regional variation in Medicare spending and the potential for cost savings cross-sectionally, this paper asks whether high-cost regions remain high cost across decades and across settings. Specifically, we investigate whether regions with high spending levels in 1992 are likely to remain high-spending regions in 2010. This report also measures whether there has been convergence or divergence in regional variation in Medicare spending over this time period to determine if geographically targeted policies could have a large effect on spending levels.
Examining regional variation in spending trends from a longitudinal perspective has a number of advantages over the cross-sectional approach. First, time series analyses can highlight whether relative per capita spending levels persist over time. If high-cost regions do not remain high cost over time, policy options targeting these areas may not be effective or may need to be modified on a regular basis. Second, using data from multiple years permits more precise measurement; panel data permit researchers to identify idiosyncratic shocks from a single year of data. Third, one can examine whether changes in Medicare policy had a similar effect on each region's Medicare spending trends.
Although this paper is not the first to evaluate trends in Medicare spending and utilization over time, this analysis offers a number of advances over prior work (Rettenmaier and Wang 2012). First, this report analyzes claims and enrollment data for 100 percent of Medicare beneficiaries. Using the complete claims history enables this study to present actual Medicare spending figures rather than statistical estimates. Second, this study includes more recent data than previous decades-long longitudinal studies, covering Medicare spending up until 2010. Third, this study applies a risk-adjustment model at the beneficiary level rather than summarized to the state or region level, relying on a detailed set of demographic, enrollment, and health status variables. This approach not only permits a more precise measurement of patient case mix, but it also allows the case mix distribution within a region—rather than region-level averages—to affect overall spending. This issue is particularly relevant, as the presence of patient comorbidities likely affects spending in a nonlinear manner. Finally, this study looks at changes in regional variation in aggregate spending over time, as well as in spending on each of the seven Medicare service types.
Methodological Approach
We calculate average monthly Medicare per capita spending for all Medicare fee-for-service beneficiaries between 1992 and 2010 in each geographic region in the United States. This analysis includes 100 percent of all Medicare claims data over this time period.1 The spending estimates do not include prescription drug coverage data, as Medicare did not cover most prescription drugs until the end of our study period (i.e., 2006). Spending is measured by the total payments made to providers by Medicare, beneficiaries, and all other sources recorded on these Medicare claims data. We also stratify results by Medicare payment setting. The seven settings examined include inpatient hospital (IP), outpatient hospital (OP), physician/carrier (PB), home health (HH), hospice (HS), skilled nursing facility (SNF), and durable medical equipment (DM).
To compare spending levels across regions, this study defines geographic regions using hospital referral regions (HRRs). The Dartmouth Atlas of Health Care team designed HRRs to represent regional health care markets surrounding a major health care center (2007-2009). In total, there are 306 HRRs in the United States.
This study also controls for two factors that may affect total spending but are outside of providers' control: regional differences in Medicare reimbursement rates and differences in patient case mix. Health care expenditures are affected by Medicare reimbursement rules, which pay providers differently based on their geographic location. For instance, Medicare uses the hospital wage index to increase reimbursement rates for hospitals located in high-wage areas and decrease reimbursement rates for hospitals in low-wage regions.
To control for these differences in reimbursement rates, we price-standardize expenditures by assigning the average price to each service type in each year by setting. Total price-adjusted costs are renormalized (at the setting and year level) so that total price-adjusted costs are equal to total unadjusted expenditures each year. Thus, price-adjusted costs reflect the actual prices paid by the Centers for Medicare and Medicaid Services (CMS). We also adjust prices for inflation in each year using the CMS market basket adjustment for each payment system or setting.2 While calculating a national average price for a given year and setting removes considerable variation in output prices, this methodology is limited. Implementing the ideal price-standardization methodology—completely removing all variation in Medicare payment rules for all settings each year by directly accounting for each payment rule—is not feasible over this time period due to the complexity and frequent adjustments in Medicare payment policy. Averaging costs by service type for each year provides a reasonable estimate of changes in payment rules over time.
After controlling for regional differences in Medicare reimbursement rates, we account for the second confounding factor—case mix—by risk-adjusting the price-standardized spending levels. The risk-adjustment model is an ordinary least-squares regression that uses monthly beneficiary spending for months the beneficiary is enrolled in Medicare A and B as the dependent variable, and patient demographics (age and sex), new enrollee status, and health status as the independent variables (Reschovsky, Hadley, and Romano 2013). We use monthly spending to maximize the number of beneficiary months that can be included in the analysis.
To account for health status, we categorize beneficiaries' claims information from the prior year into CMS's hierarchical condition categories (HCCs) (Pope et al. 2011). HCCs are a set of 70 indicator variables that measure patient comorbidities, used by CMS as part of its risk-adjustment methodology for the Medicare Advantage program.3 Our model's coefficients are reestimated for each year of data. Because beneficiaries in high-use areas may be more likely to have their diagnoses noted on their health care claims, this approach of assigning HCCs may upward-bias the estimated coefficients for these beneficiaries, as they may have more comorbidities coded than they otherwise would in a low-use area. This limitation, however, occurs whenever a study uses administrative claims data. All numbers presented in this study are both price-standardized and risk-adjusted using the methodology described above. However, no risk-adjustment approach can perfectly account for differences in patient health status, and the results of our analysis after risk adjustment may reflect demand factors unrelated to measured health status as well as supply factors.
To ensure that we capture the majority of beneficiaries' health care spending, we exclude beneficiaries with incomplete claims data. In practice, the analysis requires beneficiaries to have Medicare as their primary payer so that the study includes the vast majority of each patient's health care costs. Finally, beneficiaries with a missing ZIP code are excluded because the study cannot determine their geographic location. Excluding months in which beneficiaries do not have Medicare as their primary payer or beneficiaries who have a missing or invalid ZIP code results in a loss of less than 2 percent of beneficiaries.
To further examine regional trends, this analysis classifies HRRs into quintiles based on utilization levels in each year. For this analysis, the regions are binned such that there are an approximately equal number of regions in each quintile. Binning the regions such that there are an approximately equal number of beneficiaries in each quintile does not change any of this study's conclusions.
Results
Table1 presents the HRR-level rank correlations between each Medicare setting and total Medicare spending in 1992 and in 2010. The 1992 correlations range from −0.047 (SNF) to 0.786 (IP), while the 2010 correlations range from 0.236 (DM) to 0.853 (IP). The relationship between total spending and each setting strengthened over the study period for all settings except OP, which moved from a rank correlation of 0.308 to a weaker correlation of 0.238.
Table 1.
HRR-Level Correlation with Total Medicare Spending by Setting
| IP | OP | PB | HH | HS | SNF | DM | |
|---|---|---|---|---|---|---|---|
| Rank correlation with total Medicare spending in 1992 | 0.786 | 0.308 | 0.270 | 0.535 | 0.027 | −0.047 | 0.055 |
| Rank correlation with total Medicare spending in 2010 | 0.853 | 0.238 | 0.315 | 0.736 | 0.452 | 0.473 | 0.235 |
Table2 shows regional stability in Medicare spending for each setting using two metrics. First, Table2 shows the HRR-level rank correlation within each setting between spending in 1992 and spending in 2010. This relationship is weakest for DM (with a rank correlation of 0.039) and strongest for OP spending (rank correlation of 0.662). Second, Table2 shows the percent of HRRs ranked in the highest spending (top) quintile in 1992 that were also in the highest spending quintile in 2010. By this metric, HS has the lowest stability for high-use HRRs (21 percent of HRRs in the top quintile in 1992 were also in the top quintile in 2010), but OP again has the highest stability (66 percent of HRRs in the top quintile in 1992 were also in the top quintile in 2010).
Table 2.
HRR-Level Stability in Regional Spending by Setting
| Total Spending | IP | OP | PB | HH | HS | SNF | DM | |
|---|---|---|---|---|---|---|---|---|
| Rank correlation within setting between 1992 and 2010 spending | 0.629 | 0.635 | 0.662 | 0.582 | 0.637 | 0.181 | 0.207 | 0.039 |
| Percent of HRRs in top quintile in 1992 that stayed in top quintile in 2010 | 58% | 60% | 66% | 55% | 55% | 21% | 37% | 26% |
Table3 presents beta convergence, which determines whether regions that are high cost in 1992 are likely to have lower growth rates than regions that are low cost in 1992 (Panopoulou and Pantelidis 2013). To measure beta convergence, this report calculates the correlation between initial spending levels and growth rates between 1992 and 2010. The Pearson correlation between an HRR's total spending levels in 1992 and its growth rate from 1992 to 2010 is −0.260. The Pearson correlations in individual settings range from −0.204 (HH) to −0.780 (DM).
Table 3.
HRR-Level Evidence of Beta Convergence by Setting
| Total Spending | IP | OP | PB | HH | HS | SNF | DM | |
|---|---|---|---|---|---|---|---|---|
| Pearson's correlation between spending levels in 1992 and growth rate from 1992 to 2010 | −0.260 | −0.352 | −0.475 | −0.383 | −0.204 | −0.628 | −0.811 | −0.780 |
Figure1 graphically displays sigma convergence using the coefficient of variation (CV), which examines whether the cross-sectional distribution shrinks over time. The CV is the standard deviation of HRR-level spending divided by the mean of HRR-level spending. The variation in regional spending has been decreasing slightly overall, hinting at moderate levels of sigma convergence. Figure1 presents the CV of HRR-level spending in each year from 1992 to 2010 and shows that the CV of total Medicare spending increased slightly from 1992 to 1996 but remained fairly steady from 1997 to 2010. The CVs of inpatient hospital spending, outpatient hospital spending, and physician/carrier spending follow similar patterns and generally trend downward. These results are similar using the ratio of the 90th percentile of HRR-level utilization to the 10th percentile of HRR-level utilization, or the percent difference between the highest-spending quintile and the lowest-spending quintile as a measure of variation instead. Figure2 shows the CVs for home health, hospice, durable medical equipment, and skilled nursing facility spending, using a different axis scale than Figure1 to highlight trends. Figure2 shows that the CV in these settings has fluctuated markedly over time, with all settings except home health generally decreasing during this period.
Figure 1.
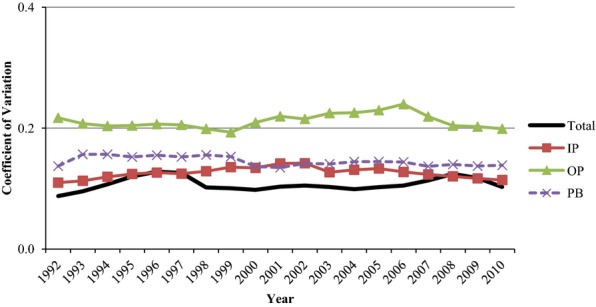
Trends in the Coefficient of Variation in HRR-Level Total, Inpatient, Outpatient, and Physician/Carrier SpendingSource: Authors' analysis of 100 percent Medicare fee-for-service claims data, 1992–2010.
Figure 2.
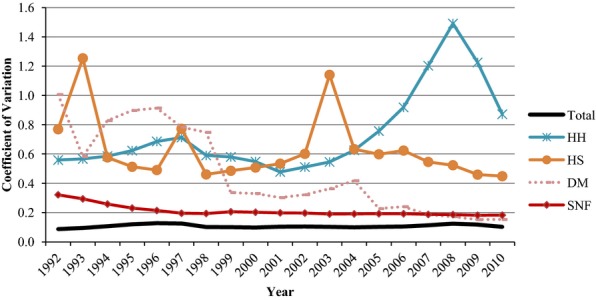
Trends in the Coefficient of Variation in HRR-Level Total, Home Health, Hospice, Durable Medical Equipment, and Skilled Nursing Facility SpendingSource: Authors' analysis of 100 percent Medicare fee-for-service claims data, 1992–2010.
Discussion
High-Use Regions Are Now More Likely to Be High Use across Settings
Regions with high total Medicare spending in 1992 are likely to be high use in different settings than regions that are high use in total Medicare spending in 2010. Table1 shows that, in 1992, high total Medicare spending regions were most likely also to be high use in inpatient hospital spending and in home health spending (rank correlations of 0.786 and 0.535, respectively); this association was further strengthened by the end of the study period, in 2010 (rank correlations of 0.853 and 0.736, respectively). However, though regions with high total Medicare spending did not tend to be high use in hospice or skilled nursing facility spending in 1992 (rank correlations of 0.027 and −0.047, respectively), high-use regions were more likely to be high use in hospice or skilled nursing facility spending in 2010 (rank correlations of 0.452 and 0.473, respectively). This trend suggests that high-use regions tend to be more high use across service areas over time.
Regions That Are High Use Tend to Remain So over Time, Particularly in Certain Settings
Regions with high levels of total Medicare spending tend to remain high use over time. The correlation between HRR-level utilization rank in 1992 and 2010 is strong (0.629), mirroring previous findings of long-term stability in Medicare spending (Cutler and Sheiner 1999).4 Furthermore, regions with high levels of Medicare spending in a given setting may also be more likely to remain high use in that setting over time. Table2 shows the correlation between HRR-level utilization ranks in 1992 and 2010 by Medicare setting. Regional stability in the inpatient hospital, outpatient hospital, or home health settings (with rank correlations of 0.635, 0.662, and 0.637, respectively) is higher than regional stability in total spending. Regions that were high use in the hospice, skilled nursing facility, and durable medical equipment settings were less likely to remain high use in that setting over time (0.181, 0.207, and 0.039, respectively).
The stability of the HRR quintiles is also fairly high; over 39 percent of regions remained in the exact same quintile for total Medicare spending in 2010 as in 1992. Furthermore, 58 percent of HRRs that ranked in the highest total Medicare spending quintile in 1992 also fell into the highest spending quintile in 2010. Table2 shows that high-cost regional stability is strongest during this period in the outpatient hospital setting; over 66 percent of HRRs that ranked in the highest spending quintile of outpatient hospital spending in 1992 also fell into the highest spending quintile of outpatient hospital spending in 2010. Regional stability is also strong in inpatient hospital spending (60 percent), physician/carrier spending (55 percent), and home health spending (55 percent). Though the results are not shown, fewer than 2 percent of HRRs in the highest total Medicare spending quintile in 1992 moved to the lowest total Medicare spending quintile by 2010. There was considerable movement in hospice spending; over 14 percent of HRRs in the highest hospice spending quintile in 1992 moved to the lowest hospice spending quintile by 2010. Notably, not a single HRR in the top quintile of inpatient hospital spending, outpatient hospital spending, or home health spending in 1992 fell to the bottom quintile of spending in that setting by 2010.
In fact, most HRRs showed little movement in their relative HRR rank from 1992 to 2010. Of the five highest spending HRRs in 2010, looking back to 1992, most were always well above the national average. Miami, FL, for example, remained in the top 10 most expensive HRRs every year between 2000 and 2010, and maintained the single highest resource use every year between 2004 and 2010. This negligible change in rank is not unique to Miami. The Monroe, LA; Baton Rouge, LA; and Alexandria, LA, HRRs all remained in the top 10 most expensive HRRs every year between 1992 and 2010. The low-cost HRRs were stable as well; Honolulu, HI, had the single lowest adjusted resource use every year between 1992 and 2010, while Santa Cruz, CA, and Santa Barbara, CA, remained in the 10 lowest spending HRRs each year from 2001 to 2010.
While most individual HRRs showed little movement in rank from 1992 to 2010, one region stood out with a remarkable change in relative spending levels: McAllen, TX. McAllen moved from the 11th lowest spending HRR in 1992 to the 5th highest spending HRR in 2010—a change of 290 ranks. McAllen's dramatic change is largely due to its increase in home health spending; in 1992, McAllen was the 33rd lowest spending HRR in home health spending, but, by 2010, McAllen was the 2nd highest spending HRR in home health spending. McAllen's relative spending rank on inpatient hospital, outpatient hospital, hospice care, and skilled nursing care actually fell over this time period.
Regional Spending Is Converging Slightly
Total spending appears to be converging slightly. The Pearson correlation between an HRR's total spending levels in 1992 and its growth rate from 1992 to 2010 (beta convergence) is −0.260, indicating that regions that are high cost in 1992 tend to have lower growth rates over that time period than regions that are low cost in 1992, mirroring previous findings (Chernew et al. 2010). Similarly, the coefficient of variation for total spending (sigma convergence) appears to increase slightly from 1992 to 1996, but it remains steady from 1997 to 2010. These findings suggest that regional spending levels are regressing toward the mean and the variation in spending is decreasing. In other words, regions that are high cost in total Medicare spending are not becoming much more high cost relative to other regions.
There is mixed evidence of convergence in the individual settings. Regions that were high cost in skilled nursing facility or hospice spending tended to be much more likely to have lower growth rates (with correlations between 1992 spending and growth rates from 1992 to 2010 of −0.811 and −0.628, respectively) and to see a decrease in their coefficient of variation, suggesting that regions that were high cost in these settings in 1992 are not becoming more high cost relative to other regions.5
Indeed, home health is the only setting that has a weaker relationship than total spending has between spending levels in 1992 and growth from 1992 to 2010, though the relationship is still negative (correlation of −0.204), suggesting slight beta convergence. The CV of home health spending trended upward from 1992 to 1997 and 2001 to 2009, suggesting an increase in regional variation in home health spending.
Regional Trends in Geographic Variation Are Dominated by National Trends
Although there is substantial regional variation in Medicare spending and trends vary across settings, national trends have a much stronger effect on per-beneficiary spending levels than trends in regional variation. Figures1 and 2 show that Medicare spending levels grew rapidly from 1992 to 1997, fell sharply in 1998 and 1999, and began a pattern of moderate growth from 2000 onward. The sudden decline in spending in 1998 and 1999 is due in part to the implementation of the Medicare Balanced Budget Act (BBA) of 1997, which reduced Medicare payments for many services, especially home health care, and restrained the update factors for payment (Crippen 1999). Congress enacted the Medicare Balanced Budget Refinement Act (BBRA) of 1999 to offset the larger-than-expected gains in Medicare savings, which contributed to slight but positive spending growth in 2000 (Lewin Group and the American Hospital Association 2000). Though not shown here, these national trends in spending levels are mirrored in both high-use and low-use regions. Regions that were low cost in 1992 and regions that were high cost in 1992 experienced increased spending from 1992 to 1997, followed by a sharp decline in 1998 due to the BBA and a moderate increase in spending after the BBRA and onward.
Conclusion
Using 100 percent of Medicare Parts A and B fee-for-service claims data from 1992 to 2010, this study reaches three principal conclusions with respect to regional variation in Medicare spending growth rates. First, drivers of Medicare spending have changed over time. High inpatient hospital and home health spending have always been associated with high total Medicare spending, but high spending on hospice care and skilled nursing facility care has become increasingly associated with high total Medicare spending from 1992 to 2010. Second, relative spending levels are persistent over time. An HRR deemed high cost in 1992 is likely to be high cost in 2010. This finding is true both for total Medicare spending as well as for spending in home health, inpatient hospital, and outpatient hospital spending. Third, there is some evidence of regression to the mean for total Medicare spending, and more for spending on certain types of postacute care (hospice and skilled nursing facility). Overall, the cross-sectional distribution of regional spending decreased over this time period in all settings except for home health.
Because regional variation in Medicare spending for certain service types is large in magnitude and persistent over time, policy makers have an opportunity to reduce Medicare spending if they could reduce spending in high-cost areas. In fact, a number of researchers have proposed implementing policies to reduce Medicare resource utilization in areas with the highest per-capita spending (Skinner and Wennberg 2000; Orszag 2008). Previous research indicates that if all metropolitan statistical areas (MSAs) in the United States had Medicare spending equal to the MSA with costs in the 10th percentile of the spending distribution, Medicare could save approximately 30 percent of costs (Cutler and Sheiner 1999). The Dartmouth Atlas investigators estimate that the United States could save 40 percent of the resources spent on chronic illness if all regions adopted the practice patterns of high-quality, low-cost regions (Wennberg 2010). However, our findings suggest that targeting specific settings may be more effective at reducing costs than targeting entire geographic regions. Effective cost reduction policies may aim to target settings with consistent or increasing associations with total spending, high levels of regional stability in spending, and/or a lack of regression-to-mean spending.
Although we control for regional differences in Medicare reimbursement and case mix, a number of other factors outside Medicare's control could also be driving spending levels. These factors include provider culture (e.g., provider preference for invasive procedures), consumer culture (e.g., patient preference for different types of treatment), market conditions (e.g., supply of nonprofits in the area or provider competition), productivity spillovers, and many other factors (Chandra and Staiger 2007). To address these issues, future work should consider specific mechanisms through which Medicare could reduce regional variation in Medicare spending, particularly in certain settings. For example, existing studies have examined options such as fraud detection, increasing Medicare's use of prior authorization, and more rapid review of local coverage decisions (Foote et al. 2008). Other studies have considered delivery-system reforms, payment reforms (such as episodes of care), and promarket strategies (Chernew et al. 2010). In summary, the persistence of high-cost Medicare spending regions for certain service types offers an opportunity to target policies to reduce spending in these service areas; determining the specific policies to achieve this goal, however, is a task that we leave for future work.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: The authors acknowledge funding from the Institute of Medicine of the National Academies for this report. The responsibility for the content of this paper rests with the authors; the content does not necessarily represent the views of the Institute of Medicine or its committees and convening bodies. The analysis that prompted this research is available online and can be found here: http://iom.edu/∼/media/Files/Report%20Files/2013/Geographic-Variation/Sub-Contractor/Acumen-Growth.pdf. All tables and figures are from the authors' analysis of 100 percent Medicare fee-for-service claims data, 1992–2010, and are reprinted with permission by the National Academy of Sciences, Courtesy of the National Academies Press, Washington, D.C. Bhattacharya's work on this paper was partially supported by the National Institute on Aging. We thank seminar participants at Stanford Institute of Theoretical Economics, numerous people at the Institute of Medicine, including Meg McCoy, Robin Graham, Michelle Mancher, and Ashna Kibria, and Rob Valletta, for their comments on early versions of this manuscript. MaCurdy is the CEO/President of Acumen, LLC and The SPHERE Institute. The remaining authors are or were employees or consultants at Acumen, LLC or The SPHERE Institute at the time this manuscript was written.
Disclosures: None.
Disclaimers: None.
Notes
This study was also repeated including prescription drug costs for beneficiaries who were continuously enrolled in Medicare Part A, B, and D from 2006 to 2010. The results of the analysis including Part D are broadly similar as those presented here.
More details of our price-standardization methodology can be found in the growth analysis report presented to the Institute of Medicine, located here: http://www.iom.edu/Reports/2013/∼/media/Files/Report%20Files/2013/Geographic-Variation/Sub-Contractor/Acumen-Growth.pdf
We performed sensitivity analyses on the risk-adjustment specifications in the report presented to the Institute of Medicine using analysis of 2007 through 2009 data, located here: http://www.iom.edu/Reports/2013/∼/media/Files/Report%20Files/2013/Geographic-Variation/Sub-Contractor/Acumen-Medicare-Medicaid.pdf
Cutler and Sheiner use metropolitan statistical areas (MSAs) and find that the correlation between MSA-level spending in 1970 and 1997 is 0.387, and the correlation between 1982 and 1997 is 0.713. MSAs and HRRs do not correspond exactly but match fairly closely.
Four HRRs with negative average risk-adjusted hospice spending were removed from the hospice calculations.
Supporting Information
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Appendix SA2: Payment Standardization Methodology.
References
- Baicker K, Buckles KS. Chandra A. Geographic Variation in the Appropriate Use of Cesarean Delivery. Health Affairs. 2006;25(5):w355–67. doi: 10.1377/hlthaff.25.w355. [DOI] [PubMed] [Google Scholar]
- Center for the Evaluative Clinical Services and Dartmouth Medical School. The Dartmouth Atlas of Health. Chicago: American Hospital Publishing Inc; 1996. [PubMed] [Google Scholar]
- Chandra A. Staiger DO. Productivity Spillovers in Health Care: Evidence from the Treatment of Heart Attacks. Journal of Political Economy. 2007;115(1):103–40. doi: 10.1086/512249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chernew ME, Sabik L, Chandra A. Newhouse JP. Ensuring the Fiscal Sustainability of Health Care Reform. New England Journal Of Medicine. 2010;362(1):1–3. doi: 10.1056/NEJMp0910194. [DOI] [PubMed] [Google Scholar]
- Cutler DM. Sheiner L. The Geography of Medicare. American Economic Review. 1999;89(2):228–33. doi: 10.1257/aer.90.2.303. [DOI] [PubMed] [Google Scholar]
- Foote SB, Virnig BA, Town RJ. Hartman L. The Impact of Medicare Coverage Policies on Health Care Utilization. Health Services Research. 2008;43(4):1285–301. doi: 10.1111/j.1475-6773.2008.00836.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuchs VR, McClellan MB. Skinner JS. Area Differences in Utilization of Medical Care and Mortality among U.S. Elderly. Perspectives on the Economics of Aging. Chicago: University of Chicago Press; 2004. pp. 367–414. [Google Scholar]
- Gawande A. The Cost Conundrum: What a Texas Town Can Teach Us about Health Care. The New Yorker. 2009;1:36–44. [Google Scholar]
- Lewin Group and the American Hospital Association. Trend Watch: The Impact of the BBA and the BBRA. Falls Church, VA: Lewin Group and the American Hospital Association; 2000. , Vol. 2. [Google Scholar]
- Orszag PR. Increasing the Value of Federal Spending on Health Care. Washington, DC: Committee on the Budget, U.S. House of Representatives; 2008. [Google Scholar]
- Panopoulou E. Pantelidis T. Cross-State Disparities in U.S. Health Care Expenditures. Health Economics. 2013;22(4):451–65. doi: 10.1002/hec.2816. [DOI] [PubMed] [Google Scholar]
- Phelps CE. Information Diffusion and Best Practice Adoption. Handbook of Health Economics. 2000;1:223–64. [Google Scholar]
- Pope GC, Kautter J, Ingber MJ, Freeman S, Sekar R. Newhart C. Evaluation of the CMS-HCC Risk Adjustment Model. 2011. , and. “ ”[accessed January 27, 2015]. Available at https://www.cms.gov/Medicare/Health-Plans/MedicareAdvtgSpecRateStats/downloads/Evaluation_Risk_Adj_Model_2011.pdf.
- Reschovsky JD, Hadley J. Romano PS. Geographic Variation in Fee-for-Service Medicare Beneficiaries' Medical Costs Is Largely Explained by Disease Burden. Medical Care Research and Review. 2013;70(5):542–63. doi: 10.1177/1077558713487771. [DOI] [PubMed] [Google Scholar]
- Rettenmaier AJ. Wang Z. Regional Variations in Medical Spending and Utilization: A Longitudinal Analysis of U.S. Medicare Population. Health Economics. 2012;21(2):67–82. doi: 10.1002/hec.1700. [DOI] [PubMed] [Google Scholar]
- Skinner J. Wennberg JE. Regional Inequality in Medicare Spending: The Key to Medicare Reform? Forum for Health Economics & Policy. 2000;3(1):1017. [Google Scholar]
- Song Y, Skinner J, et al. Regional Variations in Diagnostic Practices. New England Journal of Medicine. 2010;2010(363):45–53. doi: 10.1056/NEJMsa0910881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau. 2007. -2009. “ American Community Survey (ACS) ” [accessed on March 16, 2012]. Available at http://www.census.gov/acs/www.
- U.S. Congress, Congressional Budget Office. The Impact of the Balanced Budget Act on the Medicare Fee-for-service Program: Testimony of Dan L. Crippen, Director, Congressional Budget Office. Washington, DC: CBO; 1999. [Google Scholar]
- Wennberg JE. Tracking Medicine: A Researcher's Quest to Understand Health Care. Oxford, UK: Oxford University Press; 2010. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Appendix SA2: Payment Standardization Methodology.


