Abstract
One of the hallmarks of malignant cell populations is the ability to undergo continuous proliferation. This property allows clonal lineages to acquire sequential aberrations that can fuel increasingly autonomous growth, invasiveness, and therapeutic resistance. Innate cellular mechanisms have evolved to regulate replicative potential as a hedge against malignant progression. When activated in the absence of normal terminal differentiation cues, these mechanisms can result in a state of persistent cytostasis. This state, termed “senescence,” can be triggered by intrinsic cellular processes such as telomere dysfunction and oncogene expression, and by exogenous factors such as DNA damaging agents or oxidative environments. Despite differences in upstream signaling, senescence often involves convergent interdependent activation of tumor suppressors p53 and p16/pRB, but can be induced, albeit with reduced sensitivity, when these suppressors are compromised. Doses of conventional genotoxic drugs required to achieve cancer cell senescence are often much lower than doses required to achieve outright cell death. Additional therapies, such as those targeting cyclin dependent kinases or components of the PI3K signaling pathway, may induce senescence specifically in cancer cells by circumventing defects in tumor suppressor pathways or exploiting cancer cells’ heightened requirements for telomerase. Such treatments sufficient to induce cancer cell senescence could provide increased patient survival with fewer and less severe side effects than conventional cytotoxic regimens. This positive aspect is countered by important caveats regarding senescence reversibility, genomic instability, and paracrine effects that may increase heterogeneity and adaptive resistance of surviving cancer cells. Nevertheless, agents that effectively disrupt replicative immortality will likely be valuable components of new combinatorial approaches to cancer therapy.
Keywords: Senescence, Telomerase, Oncogenic stress, p53, pRB
1. Introduction
Among the notable feats of evolution is the remarkable protection from cancer that is enjoyed by long-lived species such as humans. Despite billions of cell divisions and trillions of cells, humans remain, on average, cancer-free for more than 50 years. One of nature's notable tumor suppressive mechanisms is cellular senescence, a response to nonlethal stress that results in persistent cytostasis. In the absence of normal growth arrest accompanying differentiation, senescence imposes limits on the proliferative capacity of clonal cell lineages. Senescence can be induced by multiple stimuli, including intrinsic cellular processes such as telomere dysfunction and oncogene expression, but also by exogenous factors such as DNA damaging agents or oxidative environments. Abundant published evidence now supports the concept that senescence is a significant impediment to malignancy, and that it is ordinarily very stringent. Indeed, as a number of investigations have shown, many cell types in which one or more senescence pathway components are functionally inactivated remain susceptible to senescence – an indication that robust compensatory mechanisms exist for this important stress response. Despite the resiliency of the senescence response, however, it is prone to failure to varying degrees, depending upon genetic/epigenetic context. Failure of senescence in cells that have undergone oncogene activation, telomere dysfunction, and/or DNA damage can result in changes favoring malignancy and drug resistance. Elucidation of mechanisms that enforce senescence has been sought in expectation that such knowledge should lead to measures that prevent or reverse its failure in susceptible pre-malignant and malignant cell populations. In this review, we focus on telomeres and other mediators of senescence induction as candidate targets for the prevention and treatment of cancers.
2. Causes of senescence
Proliferating cells can respond to genotoxic and non-genotoxic stresses in a number of ways, including transient cell-cycle arrest, senescence, and cell death. Senescence is operationally broadly defined as a viable growth arrest characterized by the inability of affected cells to resume proliferation in the presence of appropriate mitogenic factors. While multiple cellular and molecular features, including increased cell size, accumulation of lysosomes, upregulation of cell cycle inhibitors, presence of senescence-associated heterochromatic foci (SAHF), and positive staining for senescence-associated beta-galactosidase (SA-βGal) activity, have been associated with senescent cells, no single feature is a universal and specific marker of senescence. Experimental and clinical evidence indicate that an intact senescence response is important for preventing unregulated growth and malignant transformation. In addition, the ability to undergo senescence can determine the efficacy of targeted cancer therapies. As described below, however, senescence is not a discrete mechanism or pathway that can be easily classified as either intact or entirely non-functional. Instead, it is a process that can result from many different inputs with degrees of sensitivity dictated by intrinsic as well as extrinsic factors.
2.1. Telomerase repression
In the absence of externally or oncogenically induced stresses, telomerase repression may be the only physiological impediment to indefinite replication. Replicative senescence, as originally described by Hayflick in cultures of cells from non-malignant tissues, is due to natural repression of telomerase and the resulting DNA damage response that occurs when the number of telomeric TTAGGG repeat sequences on the ends of chromosomes becomes too few to support the assembly of stable telomere complexes [1], [2]. Structures formed through interactions of TTAGGG repeat sequences with a protein complex referred to as shelterin function to “cap” the chromosome ends, protecting against DNA degradation, recombination, and chromosome fusion [3]. The telomeric TTAGGG repeats are replenished by telomerase [4], a ribonucleoprotein complex that consists of a catalytic reverse transcriptase protein subunit (hTERT, TERT) [5], [6], [7], an RNA template (hTR, TERC) [8], [9], [10], and other accessory proteins, including the RNA-modifying protein dyskerin [11], [12]. The presence of hTERT and hTR are the minimum requirements for recapitulation of telomerase activity in vitro. Telomerase activity and telomere length elongation in cancer are associated with up-regulation of both hTR and hTERT, while overexpression of hTR has been shown to boost telomerase activity and more dramatically extend telomere length in cells that express endogenous or ectopic hTERT [13], [14], [15]. Thus both telomerase components restrict telomerase activity and telomere length in vitro, illustrating the fact that both components are required for a functional telomerase holoenzyme. Although hTERT was initially considered as the limiting component of telomerase, evidence from biochemistry, promoter studies, mouse models, and human tumors has demonstrated contexts where hTR limits telomerase enzyme levels and telomere maintenance [13], [14], [15], [16], [17], [18]. At early embryonic stages, the hTERT gene and telomerase activity are expressed at high levels in many tissues [19], [20]. The hTERT gene then undergoes repression as embryonic cells differentiate into adult somatic cells [21]. From the neonatal period onward, hTERT transcripts and telomerase activity are nearly or completely undetectable in most human tissues [19], [22], [23], except in some highly proliferative tissues, such as lymphoid cells and tissue stem and progenitor cells [24], [25], [26], [27]. In vitro, attrition of TTAGGG repeats upon successive divisions in cells lacking sufficient telomerase activity ultimately results in DNA damage responses including growth arrest, followed by cell enlargement, chromatin condensation, and vacuolization – characteristic features of senescent cells. Multiple and distinct human cancer precursor lesions, but not corresponding malignant cancers, are composed of cells that display signs of telomere dysfunction-induced senescence [28]. Ectopic hTERT expression in many cell types prevents these senescent changes by stabilizing telomeres and extending replicative lifespan [29], [30], [31], [32]. While not intrinsically essential for malignancy [33], an extended lifespan or “immortalization” permits clonal cell lineages to accumulate rare genetic and epigenetic aberrations that together can cause malignant transformation.
In the absence of a telomere maintenance mechanism, telomeres shorten with each round of cellular replication to eventually reach critically short lengths that are unable to support stable formation of shelterin protein complexes that protect telomeres from DNA damage surveillance mechanisms [34]. In normal cells, dysfunctional telomeres and abnormal chromosomal structures initiate a p53-mediated DNA damage response [35]. The p16/pRB tumor suppressor pathway is also activated during replicative senescence in response to telomere dysfunction and DNA damage [36], [37]. Activation of these tumor suppressors halts cell cycle progression, initiates senescence, and prevents the propagation of abnormal chromosomes. However, genetic or epigenetic aberrations in p53 and/or p16/pRB pathways enable otherwise normal cells to continue to proliferate. Cells that bypass senescence as a result of defects in these pathways are subject to continued telomere shortening and telomere dysfunction with consequential evolution of complex karyotypes [38], [39], [40]. Critically short telomeres are fusogenic, resulting in formation of unstable structures, such as dicentric and ring chromosomes [38], [41]. Continued telomere dysfunction promotes the development of abnormal chromosomes through breakage-fusion-bridge (BFB) cycles, which are initiated by fused chromatids [40], [42]. During BFB cycles, fused chromatids form bridges during anaphase. Chromatin bridges break as cells continue through mitosis, resulting in uneven segregation of genetic material and unstable chromosome structures, which fuel further BFB events in daughter cells. BFB cycles continue until abnormal chromosome structures are lost or stabilized [43]. Resulting chromosome abnormalities include non-reciprocal translocations, deletions, gene amplifications, and whole chromosome losses [43]. These types of chromosomal aberrations have been demonstrated in association with telomere dysfunction in cell culture models, p53-null mice, tumor-derived cell lines, and pre-malignant conditions [38], [40], [42], [44], [45], [46], [47], [48], [49]. They are also the hallmarks of human carcinomas that feature chromosomal instability [46], [50], [51], [52], [53], [54]. By accelerating the rate and accumulation of molecular changes, telomere dysfunction-driven chromosomal instability may result in activation of telomerase, activation of oncogenes and/or silencing of tumor suppressor genes, which ultimately cooperate to promote malignant transformation, tumor progression, and drug resistance [44], [45], [46], [47], [48], [52], [54], [55].
2.2. Oncogenic stress
In contrast to replicative senescence, oncogene-induced senescence (OIS) often occurs independently of telomere status [56], [57], but shares many of the same morphological and biochemical features [36], [58], [59], [60], [61]. OIS is observed after ectopic expression of oncogenic RAS, and many of its effectors, including activated mutants of RAF, MEK, B-RAF, PI3K, AKT, and PIM [62], [63], [64], [65], [66], and other oncogenes such as CDC6, cyclin E and STAT5 [67]. Also, functional abrogation of tumor suppressors such as PTEN, pRB, Spn, and NF1, induces senescence-like responses [68]. Stress associated with aberrant DNA replication caused by these oncogenic changes appears involved in OIS [69], [70], [71], [72]. Although the mechanism is not fully understood, it may be due to increased expression of positive regulators of S-phase. Consequently, replicons refire or terminate prematurely, generating DNA breaks that initiate a DNA damage response and phosphorylation of p53 by DNA damage response kinases. Components of the MAPK cascade also increase the expression of the tumor suppressor ARF [73], and initiate a negative feedback loop that ultimately inhibits H/MDM2 [65], resulting in p53 stabilization.
The presence of senescent cells induced by oncogenic signaling has been documented in several precancerous tissues of both human and mouse, indicating that OIS occurs in vivo [74], [75], [76], [77], [78]. The first direct evidence of cellular senescence in a growth-arrested human neoplasm was reported in benign human melanocytic nevi (moles) [77]. Cells in nevi carry an activated oncogene product (B-Raf-E600), express elevated levels of the tumor suppressor p16, undergo long-term cell-cycle arrest, and display abundant SA-β-Gal activity. In addition, they do not show detectable signs of telomere erosion, suggesting that they have undergone OIS rather than replicative senescence. These and similar results reported by others [79] suggest that OIS in nevi acts as a barrier to melanoma development.
2.3. External agent-induced stress
Conventional genotoxic radiotherapy and chemotherapeutic regimens are potent inducers of senescence in cancer cells in vitro and in vivo (reviewed in [80]). Although this senescence response has been shown to involve many of the same DNA damage response mediators (e.g., ATM, ATR, Chk1, Chk2) as those activated by telomere dysfunction and oncogene activation, it is noteworthy therapeutically that cancer cells lacking functional tumor suppressors such as p53 or pRB often retain the capacity to undergo external agent-induced senescence. While in some cases, senescence-inducing drugs clearly act through the generation of DNA damage, in other cases the mechanisms involve only alterations in DNA structure and function (e.g., inhibition of DNA methylation or histone acetylation). Still other compounds may induce senescence through direct or indirect stimulation of stress sensitive kinases, creating imbalances in mitogen signaling pathways [81].
The chief clinical advantage of targeting senescence rather than outright cell death as a desired endpoint is that drug doses required to achieve cancer cell senescence are often much lower than doses required to achieve outright cell death. In prostate cancer cell lines, for example, a dose of 25 nM doxorubicin is sufficient to induce senescence, while doses >250 nM are necessary to cause cell death [82]. In practical terms, treatment with lower doses of genotoxic drugs that are sufficient to induce senescence but not cell death could provide equivalent or prolonged patient survival with fewer and less severe side effects. There are caveats to this approach, however, as mentioned elsewhere in this review. Chief among them are the questions of senescence reversibility and pro-tumorigenic paracrine effects of senescent cells that are not cleared by the immune system.
3. Mediators of senescence
Gene expression profiling has revealed that there is limited overlap among genes exhibiting altered expression in cells induced to undergo senescence by telomere shortening, oncogene induction, or external agents [83], [84], [85], [86], [87], [88]. The data indicate that fundamental differences exist in gene regulation during senescence activated by various signals in different cell types, despite similarity in the resulting phenotypes. Despite differences in upstream signaling, however, induction of senescence often involves convergent interdependent activation of tumor suppressors p53 and p16, the former protein initiating and the latter maintaining the response [89], [90]. While this sequence is demonstrable in lymphoma cells exposed to cyclophosphamide [91] and fibroblasts exposed to activated Ras [59], in other cases, such as human mammary epithelial cells exposed to suboptimal culture conditions [48], [92] and melanocytes which acquire B-RAF mutations [93], p16 activation and senescence occur independently of p53 activation. Although p53 and p16 are clearly involved in establishing senescence growth arrest, their precise roles in this process are incompletely understood.
3.1. p53
The importance of p53 in senescence was determined by inhibiting p53 function with dominant negative mutants, specific p53 antisense mRNA, oligonucleotides or viral oncoproteins (such as SV40 T antigen or HPV16 E6); such treatments were sufficient to substantially extend the lifespan of several cell types in culture [94]. Consistent with these findings, senescence is associated with the transactivation of p53 in cultured cells [95]. Coincident with telomere shortening and DNA-damage checkpoint activation, p53 is also activated in vivo [45]. Deletion of p53 attenuated the cellular and organismal effects of telomere dysfunction [45], [96]. Proteins that regulate p53 have also been implicated in senescence. MDM2 has p53 ubiquitin ligase activity and forms an autoregulatory loop with p53 [97]. Overexpression of MDM2 targets p53 for degradation and induces functional p53 depletion [98]. Expression of another factor upregulated in senescence, ARF, can release p53 from MDM2 inhibition and cause growth arrest in young fibroblasts [98]. Seeding mouse embryonic fibroblasts (MEFs) into culture induces ARF synthesis, which continues to accumulate until the cells enter senescence [99]. MEFs derived from ARF-disrupted mice [99] or wild type fibroblasts expressing an ARF antisense construct [100] are efficiently immortalized. Consistent with this observation, overexpression of MDM2 in MEFs produces efficient immortalization [100].
Senescence effects of p53 are mediated in part through increased expression of the CDK inhibitor p21WAF1 [101], [102], [103]. p21, in turn, prevents hyperphosphorylation and inactivation of pRB [104], [105]. In some human cells, elimination of p21 is sufficient to bypass senescence [101]. However, in MEFs, the absence of p21 does not prevent senescence [106], [107]. This finding indicates that at least one additional downstream effector can independently mediate p53-induced senescence. Candidate p53 effectors include 14-3-3 and GADD45, which inhibit G2/M transition, or p53-dependent transcriptional repression of c-Myc, which results in G1 cell cycle arrest [108]. Other signals may cooperate with p53 to induce senescence. For example, Ras-induced activation of PPP1CA, the catalytic subunit of PP1α, has been shown to be necessary for Ras-dependent senescence [109]. Independently of p53, PPP1CA can stabilize the active unphosphorylated form of pRB. In MEFs, E2F transcription factor associated repressor complexes are downstream targets of p53-induced proliferation arrest [110], indicating a convergence of the p53 and p16/pRB pathways at the level of E2F. However, in many human cells, inactivation of either p53 or pRB (e.g., by viral oncoproteins or anti-sense oligonucleotides) independently and synergistically extends replicative life span [111], [112], [113]. These findings suggest that although the p53 and pRB pathways interact, they may also act separately to establish senescence.
3.2. p16/pRB
While the causes of p16 induction remain to be defined, its mechanism of action has been well characterized. The binding of p16 to cyclin dependent kinases (CDKs) 4 and 6 induces allosteric conformational changes that disrupt the interaction of these kinases with D-type cyclins [114], thus antagonizing activation of the CDKs. Through binding and inactivation of CDKs, p16 prevents phosphorylation and inactivation of pRB and similar “pocket” proteins, p107 and p130. This canonical description, while valid, obscures the differences in RB family functions that distinguish reversible cell cycle arrest from irreversible senescence-associated changes. Despite the similarities among RB family proteins, defects in pRB, but not in p107 or p130, have been associated with human cancers. This suggests that pRB has unique tumor suppressor properties not attributable to p107 or p130. In support of this concept, pRB has been shown to be preferentially associated with E2F targets involved in DNA replication during OIS, and suppression of pRB, but not p107 or p130, allowed continued DNA synthesis after induction of oncogenic RAS [115]. The pRB protein contains multiple phosphorylation sites and interacts with multiple protein complexes. It remains to be determined whether the spectrum of pRB dependent changes in a given cell type under specific conditions is simply determined by the duration of pRB activation or by qualitative differences in pRB modifications/binding interactions. Changes initiated by p16 expression are qualitatively and quantitatively distinct from those in cells undergoing transient pRB-dependent growth arrest. For example, in U2OS cells exposed to p16, pRB augments p130 at E2F-regulated promoters. Dean and co-workers [116] used chromatin immunoprecipitation (ChIP) assays to assess protein association with the E2F responsive cyclin E and A promoters. A 6-day induction of p16 resulted in a dramatic increase in pRB and E2F-4 associated with these promoters. Additional promoter-specific changes in the extent of binding to histone deacetylase HDAC1, SWI/SNF chromatin remodeling complex components BRG1 and Brm, and polycomb group protein HPC2 were noted.
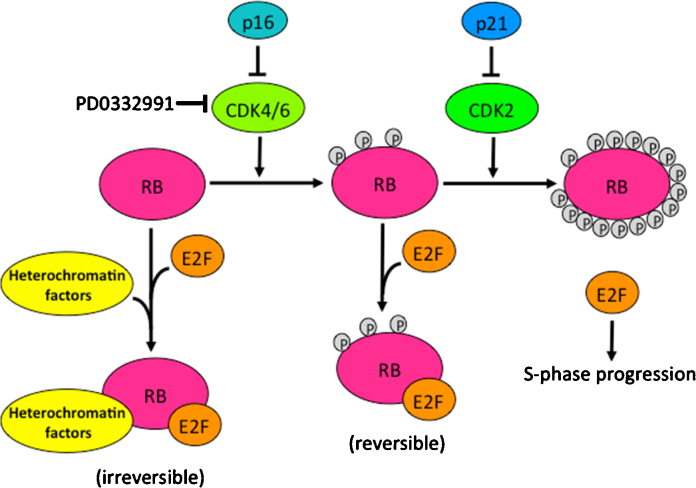
Distinctions in pRB-associated phenotypes may be due to differences in the functionality of different phosphorylated forms of pRB (Fig. 1). Although growth factors are required for cyclin D1 synthesis, transiently growth-arrested cells often contain significant amounts of cyclin D3 associated with CDK4, and the level of CDK4 activity is sufficient for cell cycle progression if CDK inhibitors are removed [117]. Thus in transiently growth-arrested cells, pRB may be held preferentially in a hypophosphorylated rather than an unphosphorylated state. While many past studies have relied on the effect of hyperphosphorylation on the electrophoretic mobility of pRB to distinguish the hyperphosphorylated from the hypophosphorylated form, few have distinguished the unphosphorylated from the hypophosphorylated form [118]. E2Fs are more easily co-immunoprecipitated with the hypophosphorylated form of pRB than the unphosphorylated form of pRB in peripheral blood lymphocytes (PBLs) during early G1 [119]. Interestingly, transduction of p16 protein into PBLs leads to loss of pRB hypophosphorylation and loss of detectable pRB association with E2F-4. The lack of detectable association might be due to reduced affinity of the unphosphorylated form of pRB for E2F-4, or alternatively to relative insolubility of larger chromatin complexes containing both pRB and E2F-4. Regardless of the interpretation, the results suggest that pRB maintained in a minimally or completely unphosphorylated state in the presence of p16, is likely to have properties that differ from those of the hypophosphorylated form. Confirmation of this concept is apparent in the results of an expression profiling study of rat fibroblast cell lines [120]. In this study, the effects on global gene expression of a pRB allele refractory to cyclin-CDK phosphorylation (the presumed state of pRB in the presence of p16) were compared to those of E2F-2 overexpression. The targets of unphosphorylated pRB were consistent with genes downregulated by p16 overexpression, but showed lower correspondence to genes stimulated by E2F-2. Similar results using human U2OS cells were reported [121].
Fig. 1.
A simplified scheme is presented of hypothetical alternative phosphorylation states and growth arrest functions of RB family proteins. Gray circles represent phosphate groups added to RB family proteins by different cyclin-CDK complexes. The primary sites of action of endogenous CDK inhibitors, p16 and p21, as well as the small molecule inhibitor, PD0332991, are also shown.
3.3. pRB-mediated heterochromatin formation during cellular senescence
pRB can play an active role in the formation of senescence-induced heterochromatic foci (SAHF) in human cells. Originally characterized in senescent fibroblasts [122], these foci consist of reorganized DNA and are enriched for proteins normally associated with heterochromatin, such as histone H3 methylated on lysine 9 (H3-K9Me), and heterochromatin protein 1 (HP1) proteins α, β, and γ. The formation of SAHF was slow, taking several days or weeks, depending on the initiating stimulus, and was reported to coincide with the enhanced association of E2F-target promoters with heterochromatin proteins. Notably, these changes were blocked by expression of the adenoviral E1A protein, which inactivates pRB and prevents senescence. Interestingly, senescent BJ fibroblasts, which poorly express p16 and were less stably arrested [122], displayed fewer SAHFs than senescent fibroblasts that express higher amounts of p16 [123].
The chromatin-based role of pRB in transcriptional repression is complicated, with multiple factors cooperating for transcriptional repression of specific promoters. For example, repression of cyclin A has been shown to be dependent on SWI/SNF chromatin remodeling, whereas other forms of transcriptional repression have been shown to be dependent on histone deacetylases or polycomb repressor components [116], [124], [125], [126]. In addition to the E2Fs, pRB can also associate with HP1 and histone methyltransferases such as SUV3-9H1, raising the possibility that pRB helps direct the process of histone methylation and HP1 recruitment to E2F responsive promoters during senescence. Consistent with this possibility, pRB showed colocalization with SAHFs in the nuclei of senescent cells, which was greater than that observed for p107 and p130 [122]. Additional work [127] has shown that p16-dependent repression by pRB at E2F target gene promoters involves the establishment of a stable repressor complex that is not displaced by the overexpression of E2F-1. Rather than displacing pRB, excess E2F-1 instead recruits more pRB, leading to direct transcriptional repression. In contrast, Rb family members, p130 and p107, which have not been demonstrated to be tumor suppressors, bind preferentially to target promoters in the absence of growth factors and in proliferating cells, respectively, and these repressor complexes are displaceable by E2F-1. HP1, which interacts with pRB, is associated with these distinct repressor complexes and follows a similar pattern of stability/displaceability. Efficient growth arrest by p16/pRB in MEFs is dependent on H3-K9Me, which provides a binding site for HP1. Differences in the stability of repressor complexes at promoters may underlie the different roles of pRB versus p130 and p107 in cell cycle regulation and tumor suppression [127].
Although the mechanisms responsible for formation and propagation of heterochromatin remain to be characterized, H3-K9Me, trimethylation of histone H4 lysine 20 (H4-K20Me), and recruitment of HP1 appear to be involved [128], [129]. Trimethylation of heterochromatic histone H3-K9 is accomplished by Suv3-9H1 and Suv3-9H2 [130], while Suv4-20H1 and Suv4-20H2 trimethylate histone H4-K20 [129]. pRB physically interacts with both these methyltransferase complexes, although the biological significance of these interactions remains unclear [131], [132]. Importantly, H3-K9Me was enriched at proliferation-associated gene promoters specifically in senescent cells, concomitant with the appearance of SAHFs, but not in quiescent cells [122]. In addition, Suv3-9, which is responsible for H3-K9Me, has been found to be required for OIS in murine lymphocyes, and for suppression of lymphoma [64]. Therefore senescent cells are thought to maintain growth arrest through the formation of heterochromatin at proliferation-promoting gene loci.
Molecular details of SAHF formation and stability remain to be determined. In addition to pRB, H3-K9Me, and HP1, SAHFs are known to be enriched in a histone H2A variant, macroH2A, previously associated with silenced chromatin [133], and HMGA proteins, which appear to be essential for SAHF formation [123]. Two evolutionarily conserved histone chaperones, HIRA and ASF1a, are also known to cooperate with pRB in the formation of SAHFs [134]. These proteins, human orthologs of proteins known to create transcriptionally silent heterochromatin in yeast, flies, and plants, may generate more extensive heterochromatin domains at positions designated by pRB. In WI38 human fibroblasts induced to undergo senescence by the introduction of an activated Ras oncogene, each chromosome condenses into a single SAHF focus [135]. The chromosome condensation is hypothesized to depend, in part, on increased nucleosome density due to HIRA/ASF1a-mediated nucleosome deposition. This chromatin condensation occurs prior to the accumulation of H3-K9Me and deposition of HP1 and macroH2A in chromatin, leading to speculation that HP1 proteins do not contribute to the acute onset of the senescent phenotype, but that instead, they might be required for the long-term maintenance of SAHF and the senescent state. Similarly, recent work using the same inducible OIS model has shown that the global pattern of repressive histone marks was largely unchanged during senescence, indicating that SAHF formation largely involves repositioning of chromatin bearing pre-existing marks rather than de novo formation of new marks [136]. This work also showed that H3-K9Me and H3-K27Me marks were not necessary for SAHF formation. However, the contribution of these individual components to senescence irreversibility remains to be determined.
4. Evidence that senescence is tumor suppressive
A protective role of senescence has been inferred in murine models of lung adenomas, T-cell lymphomas, prostate tumors, and pituitary tumors [74], [75], [76], [78]. In one example, Ras-V12 knock-in mice were shown to develop lung adenomas that were characterized by low proliferative indices, elevation of SA-β-Gal activity, and other senescence markers [137]. By contrast, the few adenocarcinomas that did emerge showed considerable proliferative activity and lacked senescence markers. In another example, Ras-V12-driven mouse T-cell lymphoma cells in which apoptosis was blocked entered senescence after drug therapy, and senescence was shown to be dependent on the chromatin-remodeling enzyme Suv3-9H1 [74]. In another study, p53 and p16 were found to cooperate in murine lymphoma cells, engaging a program of prolonged cell-cycle arrest in response to the alkylating agent, cyclophosphamide [91]. Mice bearing tumors capable of p16-induced senescence had a much better prognosis following chemotherapy than those harboring tumors with p16 defects. The study showed further that p16 loss and disruption of apoptosis by Bcl2 act independently to promote drug resistance. In a prostate tumor model, p53-dependent cellular senescence could be triggered by inactivation of the tumor suppressor, PTEN [75]. Similar findings have been reported in E2F-3 driven pituitary gland tumors [138].
Direct evidence that senescence is tumor suppressive has been generated using inducible murine models. In a model for p53-dependent liver cancer, the effect of p53 restoration was studied in established liver carcinomas [139]. Hepatoblasts expressing a conditional p53 shRNA produced invasive hepatocarcinomas. Soon after re-expression of p53, the tumors underwent dramatic regression associated with cellular senescence. The senescent cells acquired a specific gene expression profile that included upregulation of inflammatory cytokines; this led to activation of the innate immune system, which was responsible for clearing the tumor. This work established a link between the cellular senescence program and the innate immune system in suppressing tumorigenesis. Similar work by others using a mouse osteosarcoma model has also shown that re-expression of endogenous p53 leads to a senescence-like cell-cycle arrest and complete tumor regression [140].
Correlative data indicate that stress-induced senescence is tumor suppressive in human tissues as well. In malignant cells, senescence is a well-documented consequence of various chemotherapeutic regimens [80]. In a specific example in which SA-βgal activity was used as a marker of senescence, 15/36 breast tumor resections after neoadjuvant chemotherapy (cyclophosphamide, doxorubicin, and 5-fluorouracil) were found positive for SA-βgal, while only 2/20 untreated tumors showed any SA-βgal staining, suggesting that the induction of senescence may be favorably related to treatment outcome [141]. The senescence response was associated with those tumors bearing wild-type p53 alleles and exhibiting p16 expression. Interestingly, the normal tissue of chemotherapy-treated patients was completely negative for SA-βgal, indicating potential selectivity in the senescence response. Similar observations have been made in lung tumors resected from patients receiving neoadjuvant chemotherapy [142].
5. Evidence that senescence can promote malignancy – the senescence associated secretory phenotype
Unlike cells that are removed by other tumor suppressor mechanisms such as programmed cell death, senescent cells can persist and continue to actively interact with surrounding cells and tissues for extended periods of time. Defective elimination of senescent cells may lead to unregulated accumulation in aging tissues and at sites of age-associated pathologies including cancer [75], [86], [93], [143], [144], [145], [146], [147], [148], [149], [150], [151], [152], [153], [154]. Experimental removal of accumulated p16 positive senescent cells in a progeroid mouse model was sufficient to reverse some age-associated pathologies, demonstrating that accumulation of senescent cells is responsible for some tissue dysfunctions [155]. In the context of tissue repair, current evidence suggests that senescent cells are normally eliminated in a process that involves immune system functions [156], [157], [158], [159], [160], [161]. Whether to stimulate tissue repair or their own elimination, senescent cells actively interact with their tissue microenvironment, possibly through direct cell–cell contacts, and undoubtedly using paracrine signals (secretion). Protein secretion by senescent cells has been collectively termed the Senescence-Associated Secretory Phenotype (SASP) [162]. Current data support the idea that senescent cells interact with and modify their microenvironment using this secretory program. Signaling elements regulating the SASP include the DNA damage response (DDR), p38MAPK, the JAK/STAT pathway and transcription factors such as NF-κB and C/EBPβ [163], [164], [165], [166], [167], [168].
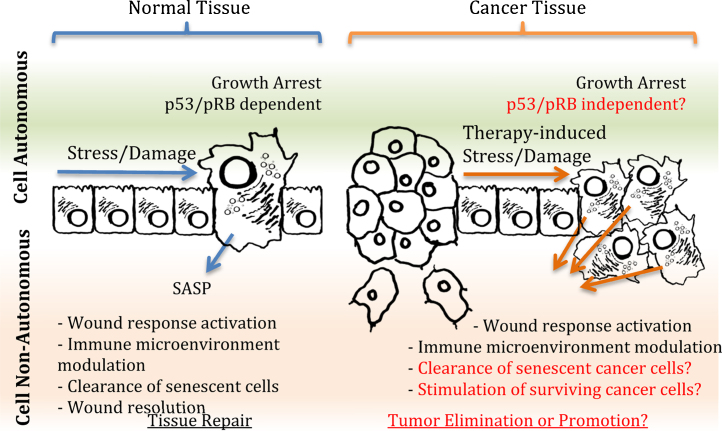
The SASP was originally documented indirectly through the ability of senescent cells to influence the biology of other cells [169]. Subsequently, mRNA profiling, targeted proteomics (antibody arrays), and genome-wide RNA interference screens have been used to characterize SASP factors and their effects [163], [164], [170], [171], [172], [173], [174]. Multiple SASP factors have been directly validated for their ability to modulate the biology of senescent cells or that of surrounding cells [175], [176], [177]. While individual SASP components may vary depending on cell type and context, a few ubiquitous SASP factors have emerged, including pro-inflammatory IL6 and IL8, extracellular matrix remodeling MMP3, and growth promoting GroA [170]. The SASP supports positive aspects of cellular senescence such as growth arrest and proper tissue repair (Fig. 2). Autocrine activities include reinforcement of p53-dependent growth arrest via cytokine signaling loops [163], [164]. Paracrine activities include orchestrating the activity of specialized repair cells, including activated stellate cells, fibroblasts and immune cells, which are responsible for the resolution of wound responses [156], [157], [159]. The SASP is also believed to modulate the clearance of senescent cells by the immune system [157], [159].
Fig. 2.
The senescence associated secretory phenotype (SASP) aids in the clearance of senescent cells, but can potentially promote proliferation of tumor cells that are not stably growth arrested. Cell-autonomous growth arrest associated with senescence prevents the proliferation of damaged cells and is at least partially dependent on p53/pRB pathways. In normal tissues, senescence also results in the activation of non-autonomous secretory factors that participate in wound response signaling, culminating in senescent cell clearance and tissue repair (left panel). In cancer tissues (right panel), activation of non-autonomous secretory factors can be altered and/or increased by treatment with therapeutic agents. However, cancer cells often harbor compromised p53/pRB pathways, and as a result, growth arrest may not occur or may be less stable. Alterations in the types or abundance of secretory factors released by such cells may interfere with immune clearance and/or stimulate the growth of nearby cancer cells that have escaped cell death. Important questions regarding the impact of senescence in the context of cancer therapy are highlighted in red.
In some contexts, however, presumably when senescent cells cannot be properly cleared by the immune system, negative consequences can occur [153], [178], [179], [180]. Senescent cells may gradually accumulate and displace normal cells, rendering affected tissues dysfunctional. Senescent cells may also modify the local microenvironment making it more supportive of survival and/or growth of potential pre-neoplastic cells. Following cancer therapy, surviving cells exhibiting the SASP could create a protective microenvironment, or a niche, for subsets of cancer cells that can initiate cancer recurrence. Cancer promoting effects of specific SASP factors have been shown in vitro and in vivo. For example, MMP3 secretion by senescent cells perturbed the proliferation and differentiation of cultured normal breast epithelial cells [181] while secretion of HGF, AREG, or GroA increased proliferation of cultured cancer cells [173], [174], [182]. Cytokines IL6 and IL8 promoted invasiveness and epithelial to mesenchymal transition (EMT) of established cancer cell lines [173]. In xenograft models, senescent cells accelerated the growth of weakly tumorigenic human cell lines [169]. This was attributed to MMP3 [183], but may also involve other MMPs secreted by senescent cells [160]. Secretion of VEGF may be responsible for increased vascularization observed in xenograft models incorporating senescent cells [184]. Additional data support a role of the SASP in cancer recurrence. For example, IL6 secretion by senescent cells in post-chemotherapy murine thymus was sufficient to create a protective niche for subsets of lymphoma cells [167], [185]. Similarly, SASP factors were linked to recurrence of chemotherapy treated murine mammary cancers [186]. Finally, in another murine cancer model, secretion of SASP factor WNT16B by senescent stromal cells supported continued growth of prostatic epithelial cancer cells after chemotherapy [187]. Importantly, increased WNT16B levels were also detected in post-therapy human prostate, ovarian, and breast cancers.
6. Determinants of senescence stability
Contrary to popular belief, the senescence growth arrest is not always irreversible. Since senescence is a response to stress, genomic and epigenomic aberrations that ameliorate stress (e.g., telomerase activation) or compromise cellular ability to sense or transduce stress-related signals (e.g., p53 inactivation) have the potential to promote immortalization and resistance to therapeutically induced senescence. Evidence obtained using cell sorting and videomicroscopy showed that fully senescent non-malignant human keratinocytes are capable of spontaneously yielding mitotically competent progeny [188]. Similarly, fluorogenic tracer and video microscopy were used to show that morphologically senescent cells in cultures of human mammary epithelial cells expressing the NeuT oncogene are capable of dividing [189]. In addition, fully senescent human fibroblasts and human mammary epithelial cells could be stimulated to resume proliferation by inactivating p53 – provided the cells had not expressed p16 [122]. Human mammary epithelial cells lacking the ability to express functional p16 are prone to unstable growth arrest and chromosomal rearrangements during telomere dysfunction-induced senescence [48]. The genomic instability generated by telomere dysfunction can complement pre-existing genetic aberrations to yield immortal cells [190], [191]. Cells that emerge from such cultures display gross genetic aberrations, many of which are also seen in human cancers [54], suggesting that the same molecular lesions that enable escape or circumvention of senescence in vitro occur during oncogenesis in vivo.
Determinants of the stability of the senescence response have not been well characterized. Yet, the implications of delayed cell cycle re-entry or permanent senescence for patient prognoses are profound. In the former case, transient senescence may allow tumor cells time to repair or accommodate the chemotherapeutic stress (e.g., damaged DNA), effectively conferring drug resistance [192]. Conversely, therapeutic efficacy would be enhanced by enforcement of stable senescence in cancer cells that manage to retain viability in the face of a therapeutic challenge. The mechanisms determining these exclusive outcomes are poorly understood, although clinical and experimental data indicate that the status of p21 and p16, and associated tumor suppressors (e.g., p53, pRB) play critical roles.
The reversibility of p16-induced growth arrest has been examined in human U2OS cells in which the transcription of an exogenously introduced p16 gene was regulated by tetracycline [193]. Induction of p16 for one day arrested most cells in the G1 phase of the cell cycle; if the inducer was then removed, p16 levels returned to baseline and growth resumed within 3–5 days. If, however, p16 was induced for 6 days, DNA synthesis remained strongly inhibited and the cells acquired morphological features of senescence. These results demonstrated that sustained p16 expression is sufficient to impose a stable block to cell proliferation that becomes independent of p16 expression after a defined period of time.
In another model employing breast cancer cell lines stably expressing shRNAs against each of the individual RB family proteins, p16 induction still resulted in irreversible G1 growth arrest in each case [194]. This finding suggests that there is some redundancy in the ability of the individual RB family proteins to mediate irreversible growth arrest. Cases of functional redundancy within this gene family have been reported in a number of murine and human cell types [195], [196]. This finding may explain why aberrations in upstream regulators such as p16, cyclin D1 and CDK4, which presumably affect the regulation of all three RB family proteins simultaneously, are more common than aberrations in the individual RB family proteins themselves in some cancers. From a clinical standpoint, it is encouraging that even aggressive cancer cells lacking both p53 and pRB tumor suppressors, are susceptible to induction of irreversible senescence. This suggests that therapies employing small-molecule inhibitors of CDK4/6 may be effective even in some tumors lacking functional pRB.
A representative small molecule CDK inhibitor that has recently been approved for clinical use is PD0332991 (Palbociclib; Supplementary Table 1). This drug has been tested against 39 individual serine, threonine, and tyrosine kinases, representing most of the primary protein kinase families, and has shown highly selective inhibition of CDK4 and CDK6 [197], [198], [199]. Importantly, oral PD0332991 administration alone at doses that were well tolerated by host animals was sufficient to cause regression of a variety of human tumor xenografts [197]. The mechanism by which this small molecule causes tumor regression in xenograft studies has been unclear, since in short-term cell culture studies (72 h) it has been shown to cause cytostasis rather than cytotoxicity [197]. Recent assessment of PD0332991 using short-term growth assays indicated that it was effective in inducing growth arrest of many estrogen receptor (ER) positive breast cancer cell lines, but that a number of ER(−) lines were able to maintain pRB phosphorylation and proliferation in its presence [200]. Several of the ER(−) cell lines exhibiting resistance to the CDK4/6 inhibitor retained phosphorylated pRB in the presence of the CDK4/6 inhibitor. This indicates that another kinase, most likely CDK1 or CDK2, was capable of phosphorylating and inactivating pRB in the absence of CDK4/6 activity in these cell lines. Thus, in many ER(−) breast cancer cells, targeting of CDK1 or CDK2 instead of, or in addition to, CDK4 may be required to initiate senescence. However, if the resulting senescence response is not stable, this may be clinically counterproductive. Indeed this danger was illustrated in a recent report that showed CDK4/6 inhibition protected ER(−) breast cancer cells from doxorubicin-mediated cytotoxicity [201].
Supplementary table related to this article can be found, in the online version, at doi:10.1016/j.semcancer.2015.03.007.
7. Defects in telomerase regulation
Telomerase is almost universally re-expressed in cancer cells and is regulated at multiple levels involving genetic, epigenetic, transcriptional, post-transcriptional, post-translational, and sub-cellular shuttling mechanisms. At the genetic level, both hTR and hTERT genes have been reported to be amplified in some tumors. Increased hTR gene copy number was detected frequently in head and neck and cervical carcinomas [202] while hTERT gene amplifications have been found in primary cancers and cell lines, including those of brain, breast, cervix, liver, and lung [203], [204], [205], as well as primary and metastatic melanomas [206]. In most cases, the amplified region encompassed most or all of chromosome 5p [13], [203], [206]. However in several cases, chromosomal break points were mapped to regions close to the hTERT promoter, suggesting that chromosomal rearrangements could either relieve the promoter from its stringent repressive epigenetic environment or place it in the proximity of enhancers at different chromosomal sites [207]. Genetic polymorphisms may also contribute to variations in telomere length and cancer development. In a recent genome wide association study, single nucleotide polymorphisms (SNPs) in seven loci were found to be associated with differences in mean leukocyte telomere length and risks of cancer and other age-related diseases [208]. These loci corresponded to genes encoding hTERT and hTR, as well as other proteins involved in telomerase complex assembly and telomere maintenance. SNPs in multiple regions of the hTERT locus, including the promoter and downstream introns, were shown to be associated with telomere length and risks of various malignancies, including breast, ovarian, and prostate, glioma, lung, and urinary bladder cancer [209], [210], [211].
Both the hTR and hTERT genes are subject to tumor specific epigenetic regulation. H3-K9Me marks were increased at the hTR promoter in normal fibroblasts and in several ALT cell lines with low hTR expression in comparison with telomerase positive cancer cell lines, suggesting a role in hTR suppression, while H3-K4Ac, H4-K4Ac, H3-K9Ac and H3-K4Me were associated with hTR expression. Similar analysis of the hTERT promoter also revealed H3-K9Me associated with transcriptional suppression and higher levels of H3-K4Ac, H4-K4Ac and H3-K9Ac in cancer cells compared with normal fibroblasts, though H3-K4Me was not strongly associated with expression in the panel tested [212].
In cancer cells lacking chromatin mediated silencing present in normal cells, both genes are subject to regulation by a wide variety of distinct, but overlapping, transcription factors. hTR is generally expressed at low levels in normal cells and is substantially up-regulated in cancer cells as shown both by fluorescence in situ studies of a wide range of tumor samples [213] and by tumor specific expression of hTR promoter-driven transgenes in the setting of gene therapy studies [214], [215]. The hTR gene promoter is activated by NF-Y, Sp1, pRB and HIF1, and is suppressed by Sp3, MDM2 and active JNK signaling which causes a switch from Sp1 to Sp3 binding at the endogenous promoter [216], [217], [218]. However, beyond these findings, relatively little attention has been paid in the literature to hTR transcriptional mechanisms.
In contrast, the hTERT gene has been intensely studied since its molecular cloning in 1997 (Fig. 3). hTERT transcripts are nearly or completely undetectable in most normal cells, but are expressed at low levels which are sufficient to drive telomere maintenance in cancer cells. Substantial work has focused on the core promoter region, which is sufficient for tumor specific activity. This region contains a number of binding sites for known transcription factors including c-Myc, HIF1, ETS, E2F and Sp1/Sp3, which integrate hTERT transcriptional responses with a number of important pathways that are dysregulated in various tumor types [219], [220], [221]. Interestingly, HIF1 is also involved in post-transcriptional regulation of hTERT splicing [222].
Fig. 3.
Mediators of hTERT activation and repression. Green arrows (top panel) indicate reported interactions that activate, while red arrows (bottom panel) indicate reported interactions that inhibit hTERT. Letters indicate mechanism (TR, transcriptional regulation; B, binding; -/+P, de/phosphorylation; IE, influence on expression).
In general, oncogenic growth promoting pathways have usually been found to activate telomerase expression and promoter activity, while pathways controlling growth suppression, cell death and senescence have the opposite effect. For example, growth factor signaling through MAPK pathways increases hTERT expression in part via ETS factors [223]. Interestingly, recent studies have shown that telomerase can be activated by point mutations in the hTERT core promoter occurring with particularly high frequency in both familial and sporadic melanoma samples [224], [225]. These mutations occurred more frequently than BRAF or NRAS mutations and each generated a binding site for ETS family transcription factors, including the TCF subgroup activated by MAPK and BRAF signaling.
Other hTERT activation pathways that are frequently deregulated in various cancer settings include those influenced by CDK2 and CDK4 [226] and AKT [227], whereas deregulated repression pathways include those influenced by TGFβ [228], TNFα [229], and other cell cycle inhibitors [230]. Disrupted developmental pathways can cause hTERT expression. For example, the hTERT gene has been found to be a direct target of the Wnt signaling [231], [232], [233]. The Wnt signaling pathway is known to play essential roles in development and stem cell renewal. Binding of Wnt ligand to its receptor Frizzled activates GSK3β kinase, which blocks ubiquitin-dependent degradation of β-catenin. Stabilized β-catenin enters the nucleus, forms a complex with LEF/TCF, and activates a set of target genes including c-Myc. Myc protein binds to an E-box element in the hTERT core promoter and activates hTERT transcription. In addition, β-catenin can also form a complex with transcription factor Klf4 and bind to the hTERT promoter directly [231].
Recently, a whole kinome siRNA screen in ovarian cancer cells for regulators of the hTERT promoter revealed at least 68 kinases that participate in pathways upstream of hTERT regulatory transcription factors, underscoring the complexity of the signaling environment [234]. Hence, it is perhaps more useful and realistic to consider hTERT regulation in a systems context as a dynamic network, in which cell-specific mechanisms are likely to come into play, than to focus on individual factors. For example, while c-Myc has been shown to activate hTERT transcription in cancer cells and some normal cells [235], moderate overexpression of c-Myc by itself is not sufficient for activation of endogenous hTERT genes in normal human mammary epithelial cells [191]; in the latter case, additional genomic alterations were needed for telomerase activation and cellular immortalization. Many other factors bind the extended hTERT promoter region, co-operating with those at the core promoter and with upstream pathways. Different combinations of transcription factors may activate telomerase expression in specific cancer cells. Given this complexity, there is clearly a need for approaches to study telomerase regulation at the systems level. A possible positive implication of the complexity is that, if sufficiently well understood, it could lead to precise therapeutic ablation of telomerase expression in cancer cells through combinatorial targeting of cooperating factors in specific cancer cell contexts.
8. Therapeutic targeting of telomerase
Intrinsic differences in telomere maintenance between normal and cancer cells provide an attractive therapeutic opportunity. Several direct strategies to exploit the dependence of cancer cells on aberrant telomerase expression for telomere homeostasis and immortality have been reported. The key advantages of targeting telomerase in comparison with most other cancer targets are its relative universality, criticality and specificity for cancer cells, including putative cancer stem cells [236]. Approximately 90% of human cancers and virtually all adenocarcinomas display significantly higher levels of telomerase compared to normal cells, thereby implicating telomerase as an intriguing target of potential anticancer therapeutics [22]. No other tumor-associated marker is as widely expressed. Moreover, telomerase, encoded by non-redundant genes, is the most efficient known mechanism for maintenance of telomeres and replicative immortality. Although a telomerase-independent alternative lengthening of telomeres (ALT) mechanism exists for telomere maintenance in cell lines and cancers in which telomerase is not active or is suppressed [237], [238], some studies suggest that ALT cells are not as biologically robust as telomerase-positive cancer cells, and may have heightened susceptibility to drug regimens that induce oxidative stress [239], [240]. Thus cancers may be less likely to develop resistance to telomerase-based therapies than to other targeted therapies whose targets may be compensated for by functionally similar proteins and pathways. In addition, the low or transient expression of telomerase in normal tissues, including normal stem cells, and the generally longer telomeres in normal stem cells versus cancer cells, provide degrees of specificity to telomerase-based drugs and reduce the probability of toxicity to normal tissues [241]. All of these factors suggest that cancer drugs based on telomerase might have a high therapeutic index.
Many distinct classes of anticancer compounds directed toward telomerase can conceivably be developed because of the varied cellular processes that regulate telomerase expression and activity. For example, cellular telomerase activity can be controlled through changes in gene transcription and alternative splicing of the telomerase components, and by the nuclear translocation, phosphorylation, folding and turnover of individual components that lead to and regulate the rate of telomerase complex assembly and accessibility to telomeres [242], [243]. The therapeutic potential of targeting telomerase-mediated telomere maintenance in cancer cells was first demonstrated by expression of a dominant negative mutant form of hTERT (DN-hTERT) in tumor-derived cell lines [31], [244]. These studies showed that inhibition of telomerase in solid tumor and leukemia cell lines induced progressive telomere shortening and eventual proliferative arrest or cell death via apoptosis. They also demonstrated that expression of DN-hTERT inhibited anchorage independent growth and impeded the development of malignancies in xenografted mice [245], [246], [247], [248]. The inhibitory effects of DN-hTERT were also experimentally demonstrated using primary AML cells in vitro and in vivo using a murine model [248].
8.1. Oligonucleotide inhibitors
Studies that utilized antisense oligonucleotides, including chemically modified nucleic acids (PNA) that target hTR, provided proof-of-principle evidence of the effectiveness of this approach as a means of specifically inhibiting telomerase and inducing telomere shortening [249], [250], [251], [252], [253], [254]. In human tumor cell lines, 2′-O-MeRNA, phosphoramidate and PNA oligomers induced telomere shortening with the subsequent onset of apoptosis over long-term culture periods [252], [254], [255], [256]. In particular, a N3′–P5′ thio-phosphoroamidate oligonucleotide targeted to the template region of human hTR (GRN163) was shown to have efficacy against multiple myeloma and non-Hodgkin's lymphoma cell lines, as well as activity toward patient-derived cells [256], [257], [258]. The specificity of this compound was evidenced by telomere shortening, and by the relatively high sensitivity of multiple myeloma cells with short telomeres in comparison to cells with longer telomeres [257], [258]. A lipid conjugated form of GRN163, referred to as GRN163L or imetelstat, exhibited improved cell uptake and was shown to more effectively inhibit telomerase, cause more rapid telomere shortening and thus elicit more rapid growth arrest than the non-lipidated compound [259], [260]. Although one study reported that imetelstat caused cultured mesenchymal stem cells (MSCs) to arrest in G1 phase of the cell cycle, the MSCs were able to resume growth after imetelstat was removed [261]. Therefore, short-term imetelstat exposure did not appear to induce senescence or cell death in MSCs. The efficacy of imetelstat against cancer cells was demonstrated in a variety of preclinical models, including mice xenografted with human cell lines derived from liver, breast, lung and prostate cancers, as well as multiple myeloma [259], [262], [263], [264], [265]. Together, the preclinical studies of imetelstat validated targeting the template region of hTR as an effective approach to telomerase inhibition. However, evidence also emerged from these studies suggesting that in addition to inhibiting telomerase, imetelstat also has off target effects that disrupt the cytoskeleton and alter adhesive properties of tumor cells [266], [267]. Inhibition of breast and lung cancer metastases in an animal model was attributed to this telomerase-independent action of imetelstat [266].
Following the success of the preclinical investigations of imetelstat, phase 1 clinical trials were initiated in which imetelstat was tested as a single agent in patients with various aggressive liquid and solid tumors (Supplementary Table 1). The limited information that was released following the completion of those studies suggested that imetelstat presented minimal adverse effects, with thrombocytopenia and neutropenia being the dose limiting toxicity [236] (http://www.geron.com/imetelstat). Subsequent phase II trials have focused on hematologic disease, childhood CNS malignancies and the application of imetelstat in maintenance therapy for non-small cell lung cancer and metastatic breast cancer patients previously treated by standard chemotherapy and surgical debulking. Data emerging from these trials suggest limited benefit in these specific clinical settings. Disappointing progression-free survival results from a phase 2 trial of imetelstat as maintenance therapy following platinum chemotherapy in patients with non-small cell lung cancer have led the Geron Corp. to suspend further development of imetelstat in solid tumors. However, it has been argued that results from the lung cancer trial showed improved outcomes for a small subset of patients with tumors that had short telomere lengths. Among the trials for hematologic disorders, encouraging data from 13 patients treated with imetelstat for essential thrombocythemia were presented at the annual meeting of the American Society for Hematology in December 2012. The ability of imetelstat to reduce platelet counts in essential thrombocythemia is consistent with earlier trials that reported thrombocytopenia as an adverse effect.
While imetelstat, targeting hTR, was the first telomerase inhibitor to undergo trials in patients, modified antisense oligonucleotides targeting hTERT mRNA have also been shown to impede the proliferation of tumor cells. However, in contrast to the lag period observed in preclinical investigations of imetelstat, the proliferative defect induced by hTERT inhibition was immediate, and occurred in the absence of apparent telomere shortening [268], [269], [270]. A modified oligonucleotide directed toward hTERT mRNA was also shown to sensitize leukemic cell lines and primary cultures established from AML and CML patients to the drug cis-diamminedichloroplatinum. Ribozymes and small interfering RNAs (siRNAs) targeting hTERT have also been employed to suppress telomerase activity, impede proliferation, and sensitize tumor cells to cytotoxic drugs [271], [272], [273], [274], [275]. The potent anti-proliferative effects that have been demonstrated in tumor cells depleted of hTERT are consistent with a body of evidence that describe telomere-length independent functions of hTERT and gene expression changes induced by repression of hTERT [276], [277], [278], [279], [280], [281]. These observations further highlight the potential benefit of direct therapeutic targeting of hTERT, although the translation of these findings to the clinic await the development of new technologies for efficient delivery of siRNA and ribozymes to tumor cells.
8.2. Small molecule telomerase inhibitors
Small molecular weight compounds that inhibit telomerase activity have been identified in screens of chemical libraries or synthesized based on the structure of the tea catechin, epigallocatechin-3-gallate (EGCG; see Section 8.4), which is a known naturally occurring telomerase inhibitor [282], [283], [284], [285], [286], [287]. Small molecular weight telomerase inhibitors characterized to date belong to a range of chemical classes and include 2-[3-(trifluoromethyl)phenyl]isothiazolin-3-one (TMPI), Rhodacyanine (FJ5002), N-[3-[(2,3-dihydroxybenzoyl)amino]phenyl]-2,3-dihydroxybenzamide (MST-312) and (E)-2-(3-(naphthalene-2-yl)but-2enamido)benzoic acid (BIBR1532). BIBR1532 is one of the more extensively used inhibitors and was shown to induce telomere shortening, impede proliferation of tumor cell lines in vitro and limit tumor formation in xenografted mice [284], [288], [289]. At a low concentration (10 μm), BIBR1532 had no effect on short-term proliferation or survival, whereas higher concentrations (50–80 μm) were acutely cytotoxic. Notably, toxicity was also observed when telomerase-negative leukemia cells were treated with a high concentration of the BIBR1532. The cytotoxic effects of BIBR1532 were attributed to telomere uncapping, however non-telomeric effects have not been ruled out. Limited bioavailability of this compound has prevented its translation to clinical trials in patients.
Other indirect approaches to targeting telomerase can and are being considered. A range of pathways and mechanisms may be tractable for such inhibition. For example, the PI3K-Akt-mTOR pathway regulates cell size, progression of the cell cycle, and cell survival, and is considered a master regulator of protein synthesis [290]. mTOR – a serine/threonine kinase – is frequently dysregulated in cancer cells [291]. An association between mTOR and telomerase activity has been shown using the prototypical mTOR inhibitor rapamycin that, in addition to its other effects, causes inhibition of telomerase activity [292], [293], [294], [295], [296]. Some phytochemicals (see below) act in a similar manner to rapamycin with respect to telomerase inhibition [294], [297].
8.3. Immunotherapeutic approaches
Studies that demonstrated telomerase antigens on the surface of tumor cells provided impetus for pursuing telomerase immunotherapy as a therapeutic approach to the treatment of the broad spectrum of human malignancies that express telomerase [298], [299], [300]. Following preclinical studies of telomerase immunotherapy for treatment of leukemia and other malignancies [301], [302], immunotherapy products were developed for use in telomerase vaccination clinical trials [236], [303] (Suppl. Table 1). Indeed one product, GV1001, has progressed to phase III clinical trials, in which it is being used in combination with gemcitabine for the treatment of pancreatic cancer [236]. Concerns that telomerase immunotherapy may be detrimental to normal hematopoietic progenitor cells were somewhat allayed by investigations that showed there was no significant reduction in the frequency of clonogenic progenitor cells or NOD/SCID repopulating cells within the bone marrow of cancer patients after vaccination [304]. In accordance with this result, limited hematologic toxicity, such as grade I anemia and thrombocytopenia, were reported to occur during telomerase vaccine trials [236].
8.4. Telomerase-directed gene therapy
The general aim of most tumor specific gene therapy is to selectively kill cancer cells while leaving normal cells unharmed by expressing high concentrations of a therapeutic protein only in malignant cells. Transcriptional targeting, in which a therapeutic gene is placed under transcriptional control of a tumor-specific promoter, is a potentially powerful tool to achieve this aim. Although their activities are quite different, the promoters for hTERT and hTR are attractive candidates for use in gene therapy since they are both active in the vast majority of cancer cells tested [17]. Most telomerase gene therapy strategies that have been tested can be broadly categorized as cytotoxic gene therapy or oncolytic virotherapy approaches, both of which aim directly to kill cells expressing telomerase while sparing normal cells that do not, thereby circumventing the issue of the phenotypic lag in cells in which telomerase activity is merely blocked [17]. Using these gene therapy approaches, cell lines covering most of the major common malignancies have been targeted effectively in vitro. Critically, almost all of these studies have shown specificity using normal cell strains. Efficacy against xenograft models has also been repeatedly shown across multiple tumor cell types. Although there is a concern that the activities of the core telomerase promoters in normal mouse tissues may not reflect their activities in human, several groups have shown that systemic delivery of telomerase-specific gene therapy constructs does not result in significant off-target liver toxicity. In addition, the biodistribution of systemically delivered hTR and hTERT-specific transgene expression has been investigated by imaging and reporter assays; activity appears to be low or absent in normal tissues (for a review of efficacy and selectivity data, the reader is referred to tables in [17]). Therefore, proof-of-principle broad spectrum, selective targeting by the telomerase promoters has been convincingly shown in preclinical models.
8.5. Phytochemicals
Attractive anticancer agents due to their low cost and accessibility in diets, phytochemicals may have selective telomerase-inhibiting and senescence-inducing properties. Experimental evidence obtained in cultured human cancer cells suggests that a variety of natural phytochemicals from dietary and non-dietary sources represent promising sources of chemotherapeutic agents that can potentially target telomerase with few side effects (reviewed in [242], [297], [305]). Regulation of telomerase activity and/or expression, localization of specific components of the telomerase protein–RNA complex or posttranslational modifications by phytochemicals have been observed. Among the first phytochemicals reported to repress telomerase was the compound berberine, leading to identification of the more potent anti-telomerase analogue FJ5002 [282], though this was not further developed. Indicative of the complexities of understanding the precise mechanism of action of natural products, tested phytochemicals appear to disrupt different telomerase-associated processes in cancer cells from different tissue sources [242]. Also, a few studies have shown that certain phytochemicals can inhibit or stimulate expression of telomerase components in different cancer cells [242]. Because of the varied effects on telomerase, specific sets of phytochemicals could conceivably be used alone or as complementary agents in combinational therapeutic strategies with established protocols for the prevention and/or treatment of human cancers. Examples of phytochemicals with demonstrated bioactivity against telomerase include (a) isoprenoids – such as perillyl alcohol, genistein, and fisetin, (b) polyphenols – such as curcumin, resveratrol, and EGCG, (c) indole-3-carbinol, and (d) sulforaphane (Table 1).
Table 1.
Therapeutic targeting by select phytochemicals.
| Phytochemical | Targets | Current state of evidence |
|---|---|---|
| Perillyl alcohol | mTOR [292], [293], [294], [295], [296], [310], [314] Telomerase [292], [293], [294], [295], [296] Ras-Erk [309], [310] |
Cell lines [292], [293], [294], [295], [296], [310], [311], [314], [368] Animal models [307], [308], [309], [310], [311] Clinical trials [369], [370], [371], [372] |
| Curcumin | mTOR [326], [327], [373], [374] Telomerase [322], [323], [324], [325], [375] Akt [326], [373] Hsp90 [325] NF-κB [328], [375] JAK/STAT [328], [376] MAPK [328], [329] |
Cell lines [322], [323], [324], [325], [326], [327], [373], [375], [376] Animal models [334], [373], [374], [375] Clinical trials [377], [378], [379], [380] |
| Resveratrol | mTOR [334], [381] Telomerase [332], [333] Akt [334], [382] MAPK [383], [384] |
Cell lines [332], [333] Animal models [334], [381], [384] Clinical trials [385], [386], [387] |
| EGCG | mTOR [335], [388] Telomerase[336], [337], [338], [339] PI3K[335], [388] NF-κB [335], [389] JAK/STAT [335], [390] MAPK [335], [391] |
Cell lines [336], [337], [338], [339], [389], [390], [392], [393] Animal models [337], [338], [394] Clinical trials [395], [396], [397] |
| Genistein | mTOR [314], [398] Telomerase [315], [316] Akt [314] |
Cell lines [314], [315], [316] Clinical trials [399] |
| Fisetin | mTOR [319], [320] PI3K/Akt [319], [320] |
Cell lines [319], [320] Animal models [321] |
Among the isoprenoids, perillyl alcohol, a small, lipophilic product of the plant mevalonate biosynthetic pathway [306], [307], [308], suppresses the growth of tumor cells in culture as well as in rodent models [309], [310], [311], [312], [313]. Perillyl alcohol acts on protein translation through modulation of mTOR signaling in cultured prostate cancer cells [314] and in mice with intracranial gliomas [310]. Mechanistically, perillyl alcohol has been shown to disrupt complex formation between mTOR and hTERT, causing p70 S6 kinase (S6K), heat shock protein 90 (Hsp90), and hTERT to dissociate from the regulatory-associated protein of mTOR (RAPTOR) [293], [294].
Genistein – another isoprenoid found in soy and fava beans – has independently been shown to down-regulate telomerase activity and attenuate 4E-BP1 phosphorylation, an indicator of mTOR signaling [314], [315], [316]. Genistein down-regulates hTERT levels by the inhibiting hTERT gene promoter activity in human prostate cancer cells [315]. This study also showed that exposure to genistein inhibited expression of the c-Myc, possibly attenuating its transcriptional activation of the hTERT promoter; however, the inhibitory effects of genistein on hTERT promoter activity likely require the disruption of one or more factors in addition to c-Myc. One contrasting study showed that genistein stimulated hTERT expression in reproductive cancer cells by enhancing STAT3 activity [317], however, the biological context of this observation is not well understood. Consistent with the transcriptional inhibitory effects of genistein, treatment of lung cancer cells with the ethyl acetate fraction of ginger extracts concurrently down regulated hTERT and c-Myc expression, which resulted in a loss of telomerase activity [318]. Genistein also has a strong posttranslational effect on telomerase compartmentalization in prostate cancer cells where it caused down-regulation of the Akt dependent phosphorylation of hTERT and thereby inhibited hTERT translocation into the nucleus [315]. Another structurally similar phytochemical, fisetin, decreases phosphorylation of multiple proteins within the Akt and mTOR pathway, including PI3K, mTOR, S6K and 4E-BP1 [319], [320]. Furthermore, fisetin has shown antitumor efficacy in Lewis mouse lung tumor models [321].
Among polyphenolic compounds, curcumin – a component of the spice turmeric, has also been shown to inhibit telomerase directly and indirectly in human brain, breast, cervical, and leukemic cell lines [322], [323], [324], [325]. This phytochemical reduces mTOR signaling by inhibiting phosphorylation of S6K and 4E-BP1, and disrupts the mTOR–RAPTOR interaction [326], [327], [328]. Like other phytochemicals, curcumin has a range of pleiotropic effects and has been reported to modulate the expression and/or activity of a range of pro- and anti-apoptotic proteins as well as telomerase regulatory factors such as c-Myc and the p53 family [324]. In addition to its effects on mTOR, curcumin modulates additional cellular pathways, including JAK-STAT, NF-κB, and MAPK, that impact telomerase regulation and cancer cell growth [328], [329]. In breast cancer cells, curcumin down-regulation of the levels of the NFkB transcription factor has been proposed to attenuate hTERT expression [330]. In lung cancer cells, curcumin stimulates the level of reactive oxygen species, which triggers the proteasome degradation of the Sp1 transcription factor leading to the loss of hTERT gene expression [331]. Curcumin exposure was also shown to stimulate the cytoplasmic retention of hTERT protein by causing dissociation of hTERT from its chaperone p23 [325]. Resveratrol, another natural phenol produced in many plants including grapes, has been found to decrease hTERT protein levels and inhibit telomerase activity [332], [333]. The combination of curcumin and resveratrol reduced cancer incidence in PTEN knockout mice [334]. EGCG is similar to curcumin in that it was found to modulate multiple oncogenic signaling pathways such as JAK/STAT, MAPK, and PI3K/Akt/mTOR [335]. EGCG down-regulated telomerase activity in multiple carcinoma cell lines and in mouse xenograft tumors [336], [337], [338], [339].
Other phytochemicals with demonstrated telomerase regulatory properties include indole-3-carbinol, a naturally occurring hydrolysis product of glucobrassicin, and the dietary isothiocyanate, sulforaphane, both from cruciferous vegetables such as broccoli and Brussels sprouts. Treatment of cultured breast cancer cells with indole-3-carbinol induced cell cycle arrest and disrupted combined estrogen receptor-alpha and Sp1-driven transcription of the hTERT gene [340]. Chromatin immunoprecipitation analysis of the endogenous hTERT promoter showed that indole-3-carbinol inhibited binding of both estrogen receptor-alpha and Sp1 to a composite estrogen response-Sp1 element in the hTERT promoter [340]. Similar to curcumin, exposure to sulforaphane elevated intracellular reactive oxygen species in hepatocellular carcinoma cells and this process was functionally linked to the inhibition of hTERT gene expression [341]. In hepatocellular carcinoma cells and in breast cancer cells, sulforaphane suppressed Akt kinase activity, which resulted in the loss of hTERT phosphorylation [341].
Candidate telomerase inhibitory natural products are not restricted to phytochemicals. Axinelloside A, a sulphated lipopolysaccharide isolated from the marine sponge Axinella infundibula, is found to inhibit telomerase [342]. However, no further studies in relation to telomerase have been reported using this highly complex compound. Telomestatin is a natural macrocyclic pentaoxazole isolated from Streptomyces anulatus that inhibits telomerase activity and causes telomere shortening and apoptosis in a range of cancer cell lines in vitro as well as leukemia xenografts. Telomestatin also augments apoptosis induced by various chemotherapeutic agents [343], [344], [345], [346]. However, its purification is inefficient and total synthesis is highly complex [347], [348].
9. Therapeutic targeting of telomeres
Another plausible approach to the inhibition of telomere maintenance is to directly target telomeres, or to manipulate the shelterin proteins that provide telomere secondary structure and telomerase access (reviewed in [3]). One potential target that has attracted considerable interest is tankyrase 1, a poly(ADP-ribose) polymerase (PARP) family protein that modifies the shelterin protein TRF1 [349], [350]. By modifying TRF1, tankyrase 1 causes displacement of TRF1 from the telomere, thereby promoting telomere unfolding and enabling telomerase to access and lengthen the telomere. General PARP inhibitors have been shown to impede telomere length maintenance and augment the activity of the telomerase inhibitor MTS-312 in experimental systems [349]. Compounds that specifically inhibit the PARP activity of tankyrase 1 are now available for experimental purposes and provide a starting point for the development of tankyrase inhibitors for advancement to clinical trials [351]. Since tankyrase 1 is known to modulate the activity of pathways that that contribute to cancer cell proliferation independently of telomerase (e.g., the WNT/β-catenin pathway), this area of investigation holds considerable promise.
There is a body of evidence that suggests that the 3′ G-rich single stranded overhang of the telomere forms a G-quadruplex structure that is not accessible to telomerase [352], [353]. G-quadruplex stabilizers therefore present a possible alternate means of manipulating telomere maintenance in cancer cells. Molecules that stabilize G-quadruplexes and have been tested for telomere effects include porphyrins (TMPyP4), perylenes (PIPER), acridine derivatives (BRACO19, RHPS4), quinoline-substituted triazines and natural products, such as telomestatin [354], [355], [356], [357], [358]. At non-toxic concentrations, these compounds diminished telomerase enzyme activity, induced telomere shortening and arrested tumor cell proliferation after a lag period [358], [359]. Decreased tumor growth rates were also demonstrated in mice xenografted with leukemia cells [343], [344], [360]. G-quadruplex stabilizing agents may also facilitate the action of standard chemotherapeutic agents and molecular targeted treatments [356], [359]. For instance, telomestatin was shown to enhance the sensitivity of acute myeloid leukemia cells to danunorubicin and cytosine-arabinoside, and was effectively combined with the tyrosine kinase inhibitor imatinib to kill chronic myeloid leukemia progenitor cells [247], [344], [361]. These results clearly illustrate the potential of G-quadruplex stabilizing agents for the treatment of malignancy.
10. Other potential therapeutic targets
Because of a lack of definitive molecular criteria, there is currently no consensus regarding properties that contribute to efficient senescence induction. Conceivably, any compound or agent that causes DNA damage or otherwise alters replication may cause senescence at doses that are not cytotoxic. Additionally, agents that stimulate differentiation pathways (such as retinoic acid [362]), may induce senescence in cancer cells that are not able to respond appropriately; this phenomenon which so far has received little attention, can potentially be the basis of truly non-toxic alternative therapies. The therapeutic utility of specific compounds will depend on standard factors such as whether activation is required, uptake and retention, as well as detoxification and repair capacities of the target cells versus those of normal cells providing vital functions. Beyond these considerations, however, the specific genetic and epigenetic traits of prospective target cells are likely to have large influences on senescence susceptibility and stability. For example, while conventional genotoxic chemotherapy is often effective at inducing senescence when used at maximally tolerated doses, tumor resistance and recurrences remain significant clinical problems, particularly in patients whose tumors retain intact p53 responses [363], [364]. When treated with genotoxins, wild-type p53 tumors show induction of p21 and SA-βgal, but not p16, and tumor growth often recurs after treatment [364]. Tumor recurrence might be significantly impeded in these cases through the concurrent administration of CDK inhibitors that circumvent defects in the p16/pRB pathway, causing the activation of RB-family dependent heterochromatin formation at E2F-dependent promoters, and stabilization of the senescent phenotype in target cells. Similarly, telomere and telomerase targeting therapies might be improved by the inclusion of agents that induce oxidative stress to discourage the selective outgrowth of ALT+ cells [240].
11. Opportunities for senescence drug discovery
In terms of drug discovery, components of the various senescence pathways represent potential targets. To determine whether or not accelerated senescence is a desirable clinical outcome of cancer therapy, it will be necessary to develop efficient and specific approaches to modulate relevant pathways in order to activate the response in a predictable fashion. Thus, ‘proof of concept’ and target validation are necessary before senescence will be seriously considered as an area for widespread commercial drug discovery. Progress in this area has been made through the application of cell-based screening approaches [365]. Cell-based assays offer potential to identify partially validated hits with improved lead-like qualities at the earliest stages of discovery and offer a number of critical advantages over conventional biochemical screening assays. Purification of the target protein in a functional conformation is not required. Instead, the key requirement is a measurable marker of endogenous target inhibition such as a change in reporter activity, protein phosphorylation, or cell morphology. Importantly, cell-based assays may also discriminate between different drug effects, such as antagonism versus agonism, and identify hits that interact with different target conformations that may be present in a physiological setting. The characteristic morphological changes associated with cell senescence including cell enlargement and SA-βGal activity are suitable for cell based screening approaches using high content automated imaging. The validity of this approach has recently been demonstrated in both normal and cancer cell-based screening strategies using siRNA or small molecule libraries to identify compounds that modulate senescence and targets for further validation [366], [367]. Interestingly, in these studies, senescence occurs in a matter of days post treatment, an advantage over the longer lag time generally associated with telomerase inhibition.
Thus senescence is already beginning to show great promise as an endpoint for drug targeting. Cell-based senescence models and assays have contributed considerably to advancing new approaches to drug development. Importantly, a number of agents already used in the management of human cancers also show associations with senescence phenotypes, opening up opportunities for drug re-positioning [80], [365]. However, the key questions as to which patient group will benefit from such agents and clinical trial design are still open to debate and likely to revolve around the specific target in question.
12. Cross-validation
Given the heterogeneity present in most cancers, complete arrest/eradication of the various subpopulations of cells in any given cancer will likely require simultaneous targeting of several molecules and mechanisms that contribute to the malignant phenotype. It is therefore important to anticipate complementary as well as antagonistic effects on different cancer hallmarks that might be achieved using agents directed against specific targets. Accordingly, a literature search has been conducted by a “cross-validation” team to identify potential consequences of the use of selected agents targeting protein complexes involved in the maintenance of replicative immortality on other hallmarks of cancer. The results of this survey are listed in Table 2. The table indicates that not all interactions are favorable; some agents efficacious against replicative immortality may exacerbate other hallmarks (e.g., genetic instability), and their utility may be context-dependent.
Table 2.
Cross-validation of selected targets and agents.
| Targets for replicative immortality | Telomerase (inhibit) | hTERT (inhibit) | mTOR (inhibit) | CDK4/6 (inhibit) | CDK1/2/5/9 (inhibit) | Akt (inhibit) | PI3K (inhibit) |
|---|---|---|---|---|---|---|---|
| Other cancer hallmarksa | |||||||
| Genomic instability | +/− [400], [401], [402]c |
+/− [400], [401], [402] |
0 | − [403] |
+ [404], [405] |
+ [406], [407], [408] |
+ [409] |
| Sustained proliferative signaling | + [410] |
+ [411], [412], [413] |
+ [414], [415], [416] |
+ [417], [418] |
+ [419], [420], [421] |
+ [415], [422], [423] |
+ [424], [425] |
| Tumor promoting inflammation | + [410] |
+ [410] |
+ [426], [427] |
+ [428] |
+ [429], [430] |
+ [431], [432] |
+ [433], [434] |
| Evasion of anti-growth signaling | + [258], [276], [435] |
+ [258], [276], [435] |
+/− [436], [437] |
+ [438], [439] |
+ [440], [441], [442] |
+ [443], [444] |
+ [445], [446] |
| Resistance to apoptosis | + [447] |
+ [448] |
+ [449] |
+ [450] |
+ [451] |
+ [452] |
+ [452] |
| Dysregulated metabolism | + [453] |
0 | + [454] |
+ [455] |
+ [456] |
+ [457], [458] |
+ [459], [460] |
| Immune system evasion | 0 | 0 | +/− [461] |
0 | 0 | + [462] |
+/− [463], [464] |
| Angiogenesis | + [465] |
+ [465] |
+ [466], [467] |
+ [468], [469] |
+ [470], [471] |
+ [466] |
+ [466] |
| Tissue invasion and metastasis | + [472], [473] |
+ [472], [473] |
+ [474], [475] |
+/− [476], [477] |
+ [478], [479] |
+ [480] |
+ [475] |
| Tumor microenvironment | + [481] |
+ [482] |
+ [483] |
+ [484] |
− [485], [486] |
+ [487], [488] |
+ [488], [489] |
| Approaches | GRN163L (imetelstat) | Genistein | Perillyl alcohol | PD 0332991 (palbociclib) | SCH 727965 (dinacicilib) | Curcumin | EGCG (epigallocatechin-3-gallate) |
|---|---|---|---|---|---|---|---|
| Other cancer hallmarksb | |||||||
| Genomic instability | +/− [490], [491] |
+/− [492], [493] |
+ [494] |
0 | 0 | + [495], [496] |
+/− [497], [498] |
| Sustained proliferative signaling | 0 | +/− [499], [500] |
+ [501], [309] |
+ [502] |
+ [503] |
+ [504], [505] |
+ [506], [507] |
| Tumor promoting inflammation | 0 | +/− [508], [509], [510] |
+ [309], [511] |
0 | 0 | + [512], [513], [514] |
+ [515], [516] |
| Evasion of anti-growth signaling | + [258] |
+ [517], [518], [519] |
+ [520] |
+ [502], [521] |
+ [522] |
+ [523], [524] |
+ [525], [526] |
| Resistance to apoptosis | + [276] |
+ [527], [528] |
+ [529], [530] |
+ [502], [531] |
+ [522], [532] |
+ [533], [534] |
+ [535], [536] |
| Dysregulated metabolism | 0 | + [537] |
+ [310] |
0 | 0 | + [538] |
+ [539], [540] |
| Immune system evasion | 0 | + [541] |
0 | 0 | 0 | + [542], [543] |
+/− [544], [545], [546] |
| Angiogenesis | 0 | + [547], [548], [549] |
+ [550] |
0 | 0 | + [551] |
+ [552], [553] |
| Tissue invasion and metastasis | 0 | +/− [554], [555], [556] |
+ [310] |
− [476] |
+ [503] |
+ [557], [558] |
+ [559], [560], [561] |
| Tumor microenvironment | + [562] |
+ [563] |
+ [550] |
0 | + [564] |
+ [565], [566] |
+ [567] |
Potential consequences of targeting indicated protein complexes involved in the maintenance of replicative immortality on other hallmarks of cancer: +, inhibition of indicated target has beneficial consequences for hallmark; −, inhibition of indicated target exacerbates hallmark; +/−, inhibition of indicated target has both positive and negative effects on hallmark; 0, no published evidence of any effect on hallmark.
Potential consequences of the use of selected agents targeting pathways involved in the maintenance of replicative immortality on other hallmarks of cancer: +, indicated agent has beneficial consequences for hallmark; −, indicated agent exacerbates hallmark; +/−, indicated agent has both positive and negative effects on hallmark; 0, no published evidence of any effect of indicated agent on hallmark.
Numbers in brackets refer to references containing evidence for potential consequences listed.
13. Conclusions
Developing optimized and truly holistic cancer prevention and treatment regimens will likely incorporate strategies that target replicative immortality. The chief advantage to be gained by the use of these senescence-inducing regimens is elimination of tumor repopulating ability with reduced collateral damage compared to conventional cytotoxic regimens. There are certain questions and risks associated with this strategy that must be addressed before its wholesale adoption in clinical settings. In the case of telomere and telomerase based strategies, replicative senescence may occur more readily in cancer cells bearing short telomeres than in vital normal cells with long telomeres, but telomere lengths in cancer cells may still be long enough to permit sufficient population doublings for invasion and metastases to occur. Moreover, telomere dysfunction promotes the development of chromosomal instability, which in turn can generate mutations that enable cells to become drug resistant and/or activate ALT mechanisms for telomere maintenance and/or become more malignant. High priority should be given to further research into the determinants of senescence stability, as the implications of delayed cell cycle re-entry, permanent cytostasis, or eventual clearance may be profoundly different. Lower doses of genotoxic drugs needed to induce senescence may reduce collateral damage, but allow establishment of dormancy by resistant cells. Conversely, since it is almost impossible to kill all the cells in a tumor even at the highest tolerated doses of chemotherapy, addition of a complementary agent that induces or enhances stable senescence in the cancer cells that manage to retain viability might additively or synergistically increase therapeutic efficacy. The microenvironmental and systemic effects of senescent cells also need further clarification. While senescent cells have been shown to secrete proteins that aid in their own clearance and tissue repair, persistent senescent cells can disrupt niches, causing the depletion of healthy stem cells, and can promote aging and cancerous phenotypes in surrounding tissues. Given that some senescence-associated secretory phenotypes can be pro-tumorigenic, is senescence still a good objective? Can a proper immune response be counted on to clear senescent cells? Ultimately, given the hypermutability and heterogeneity of most human cancers, it is often unlikely that targeting any single gene product or pathway will provide lasting remission. However, developing agents with good mechanistic understanding, that effectively disrupt replicative immortality, may well add to the arsenal available for combinatorial approaches.
Conflict of interest
Dr. Keith has collaborative agreements with AstraZeneca and Geron Corporations, and is founder and director of Senectus Therapeutics.
Acknowledgments
The authors thank members of Getting to Know Cancer for insightful discussion. Funding was provided by the United States National Institutes of Health (PY: ES019458, GF: CA164095, JZ: GM071725), California Breast Cancer Research Program (PY: 17UB-8708), Cancer Research UK (WNK: C301/A14762), University of Glasgow (WNK), Canadian Institute for Health Research (FR: MOP114962), Fonds de Recherche Québec Santé (FR: 22624), W.W. Smith Charitable Trust (JZ), Carlos III Health Institute (AM: CP10/00539), Basque Foundation for Science (IKERBASQUE) and Marie Curie CIG grant (AM: 2012/712404), the Spanish Ministry of Economy and Competitivity, ISCIII (AC: PI12/00137, RTICC: RD12/0036/0028), Regional Development European Funds (AC), Consejeria de Ciencia e Innovacion (AC: CTS-1848), and Consejeria de Salud of the Junta de Andalucia (AC: PI-0306-2012). Children's Cancer Institute Australia is affiliated with the University of New South Wales and Sydney Children's Hospital Network (KM).
Funding for the cross-validation team was provided by EU Marie Curie Reintegration grant MC-CIG-303514 (AGG), Greek National funds grant MIS 379346 (AGG), COST Action grant CM1201 (AGG), Italian Ministry of University and the University of Italy (AA, EN), Japan Ministry of Education Culture Sports Science and Technology grant 24590493 (KH), Italian Ministry of Education Universities and Research grant MIUR-PRIN 20125S38FA_002 (KA), Italian Ministry of Health grant GR-2011-02348047 (KA), Italian Association for Cancer Research (MRC), Ovarian and Prostate Cancer Research Trust in the United Kingdom (SC), Terry Fox Foundation (AA), Zayed Center for Health Sciences (AA), and Al-Jalila Foundation (AA).
Contributor Information
Paul Yaswen, Email: p_yaswen@lbl.gov.
Karen L. MacKenzie, Email: k.mackenzie@unsw.edu.au.
W. Nicol Keith, Email: nicol.keith@glasgow.ac.uk.
Patricia Hentosh, Email: hentoshp@hotmail.com.
Francis Rodier, Email: rodierf@mac.com.
Jiyue Zhu, Email: jiyue.zhu@wsu.edu.
Gary L. Firestone, Email: glfire@berkeley.edu.
Ander Matheu, Email: ander.matheu@biodonostia.org.
Amancio Carnero, Email: acarnero@us.es.
Alan Bilsland, Email: Alan.Bilsland@glasgow.ac.uk.
Tabetha Sundin, Email: trsundin@sentara.com.
References
- 1.Wright W.E., Shay J.W. Time, telomeres and tumors: is cellular senescence more than an anticancer mechanism. Trends Cell Biol. 1995;5:293–297. doi: 10.1016/s0962-8924(00)89044-3. [DOI] [PubMed] [Google Scholar]
- 2.Kipling D., Wynford-Thomas D., Jones C.J., Akbar A., Aspinall R., Bacchetti S. Telomere-dependent senescence. Nat Biotechnol. 1999;17:313–314. doi: 10.1038/7827. [DOI] [PubMed] [Google Scholar]
- 3.Bilsland A.E., Cairney C.J., Keith W.N. Targeting the telomere and shelterin complex for cancer therapy: current views and future perspectives. J Cell Mol Med. 2011;15:179–186. doi: 10.1111/j.1582-4934.2010.01253.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morin G.B. The human telomere terminal transferase enzyme is a ribonucleoprotein that synthesizes TTAGGG repeats. Cell. 1989;59:521–529. doi: 10.1016/0092-8674(89)90035-4. [DOI] [PubMed] [Google Scholar]
- 5.Lingner J., Hughes T.R., Shevchenko A., Mann M., Lundblad V., Cech T.R. Reverse transcriptase motifs in the catalytic subunit of telomerase. Science. 1997;276:561–567. doi: 10.1126/science.276.5312.561. [DOI] [PubMed] [Google Scholar]
- 6.Meyerson M., Counter C.M., Eaton E.N., Ellisen L.W., Steiner P., Caddle S.D. hEST2, the putative human telomerase catalytic subunit gene, is up-regulated in tumor cells and during immortalization. Cell. 1997;90:785–795. doi: 10.1016/s0092-8674(00)80538-3. [DOI] [PubMed] [Google Scholar]
- 7.Harrington L., McPhail T., Mar V., Zhou W., Oulton R., Bass M.B. A mammalian telomerase-associated protein. Science. 1997;275:973–977. doi: 10.1126/science.275.5302.973. [DOI] [PubMed] [Google Scholar]
- 8.Shippen-Lentz D., Blackburn E.H. Functional evidence for an RNA template in telomerase. Science. 1990;247:546–552. doi: 10.1126/science.1689074. [DOI] [PubMed] [Google Scholar]
- 9.Blasco M.A., Funk W., Villeponteau B., Greider C.W. Functional characterization and developmental regulation of mouse telomerase RNA. Science. 1995;269:1267–1270. doi: 10.1126/science.7544492. [DOI] [PubMed] [Google Scholar]
- 10.Collins K. Mammalian telomeres and telomerase. Curr Opin Cell Biol. 2000;12:378–383. doi: 10.1016/s0955-0674(00)00103-4. [DOI] [PubMed] [Google Scholar]
- 11.Venteicher A.S., Abreu E.B., Meng Z., McCann K.E., Terns R.M., Veenstra T.D. A human telomerase holoenzyme protein required for Cajal body localization and telomere synthesis. Science. 2009;323:644–648. doi: 10.1126/science.1165357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cohen S.B., Graham M.E., Lovrecz G.O., Bache N., Robinson P.J., Reddel R.R. Protein composition of catalytically active human telomerase from immortal cells. Science. 2007;315:1850–1853. doi: 10.1126/science.1138596. [DOI] [PubMed] [Google Scholar]
- 13.Cao Y., Bryan T.M., Reddel R.R. Increased copy number of the TERT and TERC telomerase subunit genes in cancer cells. Cancer Sci. 2008;99:1092–1099. doi: 10.1111/j.1349-7006.2008.00815.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cristofari G., Lingner J. Telomere length homeostasis requires that telomerase levels are limiting. EMBO J. 2006;25:565–574. doi: 10.1038/sj.emboj.7600952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Napier C.E., Veas L.A., Kan C.Y., Taylor L.M., Yuan J., Wen V.W. Mild hyperoxia limits hTR levels, telomerase activity, and telomere length maintenance in hTERT-transduced bone marrow endothelial cells. Biochim Biophys Acta. 2010;1803:1142–1153. doi: 10.1016/j.bbamcr.2010.06.010. [DOI] [PubMed] [Google Scholar]
- 16.Chiang Y.J., Hemann M.T., Hathcock K.S., Tessarollo L., Feigenbaum L., Hahn W.C. Expression of telomerase RNA template, but not telomerase reverse transcriptase, is limiting for telomere length maintenance in vivo. Mol Cell Biol. 2004;24:7024–7031. doi: 10.1128/MCB.24.16.7024-7031.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Keith W.N., Bilsland A., Hardie M., Evans T.R. Drug insight: cancer cell immortality-telomerase as a target for novel cancer gene therapies. Nat Clin Pract Oncol. 2004;1:88–96. doi: 10.1038/ncponc0044. [DOI] [PubMed] [Google Scholar]
- 18.Cairney C.J., Keith W.N. Telomerase redefined: integrated regulation of hTR and hTERT for telomere maintenance and telomerase activity. Biochimie. 2008;90:13–23. doi: 10.1016/j.biochi.2007.07.025. [DOI] [PubMed] [Google Scholar]
- 19.Wright W.E., Piatyszek M.A., Rainey W.E., Byrd W., Shay J.W. Telomerase activity in human germline and embryonic tissues and cells. Dev Genet. 1996;18:173–179. doi: 10.1002/(SICI)1520-6408(1996)18:2<173::AID-DVG10>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 20.Jia W., Wang S., Horner J.W., Wang N., Wang H., Gunther E.J. A BAC transgenic reporter recapitulates in vivo regulation of human telomerase reverse transcriptase in development and tumorigenesis. FASEB J. 2011;25:979–989. doi: 10.1096/fj.10-173989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang S., Hu C., Zhu J. Transcriptional silencing of a novel hTERT reporter locus during in vitro differentiation of mouse embryonic stem cells. Mol Biol Cell. 2007;18:669–677. doi: 10.1091/mbc.E06-09-0840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim N.W., Piatyszek M.A., Prowse K.R., Harley C.B., West M.D., Ho P.L. Specific association of human telomerase activity with immortal cells and cancer. Science. 1994;266:2011–2015. doi: 10.1126/science.7605428. [see comments] [DOI] [PubMed] [Google Scholar]
- 23.Masutomi K., Yu E.Y., Khurts S., Ben-Porath I., Currier J.L., Metz G.B. Telomerase maintains telomere structure in normal human cells. Cell. 2003;114:241–253. doi: 10.1016/s0092-8674(03)00550-6. [DOI] [PubMed] [Google Scholar]
- 24.Yasumoto S., Kunimura C., Kikuchi K., Tahara H., Ohji H., Yamamoto H. Telomerase activity in normal human epithelial cells. Oncogene. 1996;13:433–439. [PubMed] [Google Scholar]
- 25.Weng N.P., Levine B.L., June C.H., Hodes R.J. Regulated expression of telomerase activity in human T lymphocyte development and activation. J Exp Med. 1996;183:2471–2479. doi: 10.1084/jem.183.6.2471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chiu C.P., Dragowska W., Kim N.W., Vaziri H., Yui J., Thomas T.E. Differential expression of telomerase activity in hematopoietic progenitors from adult human bone marrow. Stem Cells. 1996;14:239–248. doi: 10.1002/stem.140239. [DOI] [PubMed] [Google Scholar]
- 27.Engelhardt M., Kumar R., Albanell J., Pettengell R., Han W., Moore M.A.S. Telomerase regulation, cell cycle, and telomere stability in primitive hematopoietic cells. Blood. 1997;90:182–193. [PubMed] [Google Scholar]
- 28.Suram A., Kaplunov J., Patel P.L., Ruan H., Cerutti A., Boccardi V. Oncogene-induced telomere dysfunction enforces cellular senescence in human cancer precursor lesions. EMBO J. 2012;31:2839–2851. doi: 10.1038/emboj.2012.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bodnar A.G., Ouellette M., Frolkis M., Holt S.E., Chiu C.-P., Morin G.B. Extension of life-span by introduction of telomerase into normal human cells. Science. 1998;279:349–352. doi: 10.1126/science.279.5349.349. [DOI] [PubMed] [Google Scholar]
- 30.Counter C.M., Hahn W.C., Wei W., Caddle S.D., Beijersbergen R.L., Lansdorp P.M. Dissociation among in vitro telomerase activity, telomere maintenance, and cellular immortalization. Proc Natl Acad Sci U S A. 1998;95:14723–14728. doi: 10.1073/pnas.95.25.14723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hahn W.C., Counter C.M., Lundberg A.S., Beijersbergen R.L., Brooks M.W., Weinberg R.A. Creation of human tumor cells with defined genetic elements. Nature. 1999;400:464–468. doi: 10.1038/22780. [DOI] [PubMed] [Google Scholar]
- 32.Zhu J., Wang H., Bishop J.M., Blackburn E.H. Telomerase extends the lifespan of virus-transformed human cells without net telomere lengthening. Proc Natl Acad Sci U S A. 1999;96:3723–3728. doi: 10.1073/pnas.96.7.3723. [see comments] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Seger Y.R., Garcia-Cao M., Piccinin S., Cunsolo C.L., Doglioni C., Blasco M.A. Transformation of normal human cells in the absence of telomerase activation. Cancer Cell. 2002;2:401–413. doi: 10.1016/s1535-6108(02)00183-6. [DOI] [PubMed] [Google Scholar]
- 34.de Lange T. Shelterin: the protein complex that shapes and safeguards human telomeres. Genes Dev. 2005;19:2100–2110. doi: 10.1101/gad.1346005. [DOI] [PubMed] [Google Scholar]
- 35.d’Adda di Fagagna F., Reaper P.M., Clay-Farrace L., Fiegler H., Carr P., Von Zglinicki T. A DNA damage checkpoint response in telomere-initiated senescence. Nature. 2003;426:194–198. doi: 10.1038/nature02118. [DOI] [PubMed] [Google Scholar]
- 36.Robles S.J., Adami G.R. Agents that cause DNA double strand breaks lead to p16INK4 enrichment and the premature senescence of normal fibroblasts. Oncogene. 1998;16:1113–1123. doi: 10.1038/sj.onc.1201862. [DOI] [PubMed] [Google Scholar]
- 37.Jacobs J.J., de Lange T. Significant role for p16INK4a in p53-independent telomere-directed senescence. Curr Biol. 2004;14:2302–2308. doi: 10.1016/j.cub.2004.12.025. [DOI] [PubMed] [Google Scholar]
- 38.Counter C.M., Avilion A.A., LeFeuvre C.E., Stewart N.G., Greider C.W., Harley C.B. Telomere shortening associated with chromosome instability is arrested in immortal cells which express telomerase activity. EMBO J. 1992;11:1921–1929. doi: 10.1002/j.1460-2075.1992.tb05245.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ray F.A., Peabody D.S., Cooper J.L., Cram L.S., Kraemer P.M. SV40 T antigen alone drives karyotype instability that precedes neoplastic transformation of human diploid fibroblasts. J Cell Biochem. 1990;42:13–31. doi: 10.1002/jcb.240420103. [DOI] [PubMed] [Google Scholar]
- 40.Ducray C., Pommier J.P., Martins L., Boussin F.D., Sabatier L. Telomere dynamics, end-to-end fusions and telomerase activation during the human fibroblast immortalization process. Oncogene. 1999;18:4211–4223. doi: 10.1038/sj.onc.1202797. [DOI] [PubMed] [Google Scholar]
- 41.Blasco M.A., Lee H.W., Hande M.P., Samper E., Lansdorp P.M., DePinho R.A. Telomere shortening and tumor formation by mouse cells lacking telomerase RNA. Cell. 1997;91:25–34. doi: 10.1016/s0092-8674(01)80006-4. [DOI] [PubMed] [Google Scholar]
- 42.Gisselsson D., Pettersson L., Hoglund M., Heidenblad M., Gorunova L., Wiegant J. Chromosomal breakage-fusion-bridge events cause genetic intratumor heterogeneity. Proc Natl Acad Sci U S A. 2000;97:5357–5362. doi: 10.1073/pnas.090013497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Murnane J.P., Sabatier L. Chromosome rearrangements resulting from telomere dysfunction and their role in cancer. Bioessays. 2004;26:1164–1174. doi: 10.1002/bies.20125. [DOI] [PubMed] [Google Scholar]
- 44.Rudolph K.L., Millard M., Bosenberg M.W., DePinho R.A. Telomere dysfunction and evolution of intestinal carcinoma in mice and humans. Nat Genet. 2001;28:155–159. doi: 10.1038/88871. [DOI] [PubMed] [Google Scholar]
- 45.Chin L., Artandi S.E., Shen Q., Tam A., Lee S.-L., Gottlieb G.J. p53 deficiency rescues the adverse effects of telomere loss and cooperates with telomere dysfunction to accelerate carcinogenesis. Cell. 1999;97:527–538. doi: 10.1016/s0092-8674(00)80762-x. [DOI] [PubMed] [Google Scholar]
- 46.Artandi S.E., Chang S., Lee S.L., Alson S., Gottlieb G.J., Chin L. Telomere dysfunction promotes non-reciprocal translocations and epithelial cancers in mice. Nature. 2000;406:641–645. doi: 10.1038/35020592. [DOI] [PubMed] [Google Scholar]
- 47.O'Sullivan J.N., Bronner M.P., Brentnall T.A., Finley J.C., Shen W.T., Emerson S. Chromosomal instability in ulcerative colitis is related to telomere shortening. Nat Genet. 2002;32:280–284. doi: 10.1038/ng989. [DOI] [PubMed] [Google Scholar]
- 48.Romanov S.R., Kozakiewicz B.K., Holst C.R., Stampfer M.R., Haupt L.M., Tlsty T.D. Normal human mammary epithelial cells spontaneously escape senescence and acquire genomic changes. Nature. 2001;409:633–637. doi: 10.1038/35054579. [DOI] [PubMed] [Google Scholar]
- 49.Wen V.W., Wu K., Baksh S., Hinshelwood R.A., Lock R.B., Clark S.J. Telomere-driven karyotypic complexity concurs with p16INK4a inactivation in TP53-competent immortal endothelial cells. Cancer Res. 2006;66:10691–10700. doi: 10.1158/0008-5472.CAN-06-0979. [DOI] [PubMed] [Google Scholar]
- 50.Stewenius Y., Gorunova L., Jonson T., Larsson N., Hoglund M., Mandahl N. Structural and numerical chromosome changes in colon cancer develop through telomere-mediated anaphase bridges, not through mitotic multipolarity. Proc Natl Acad Sci U S A. 2005;102:5541–5546. doi: 10.1073/pnas.0408454102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gisselsson D., Jonson T., Petersen A., Strombeck B., Dal Cin P., Hoglund M. Telomere dysfunction triggers extensive DNA fragmentation and evolution of complex chromosome abnormalities in human malignant tumors. Proc Natl Acad Sci U S A. 2001;98:12683–12688. doi: 10.1073/pnas.211357798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gisselsson D., Jonson T., Yu C., Martins C., Mandahl N., Wiegant J. Centrosomal abnormalities, multipolar mitoses, and chromosomal instability in head and neck tumours with dysfunctional telomeres. Br J Cancer. 2002;87:202–207. doi: 10.1038/sj.bjc.6600438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Saunders W.S., Shuster M., Huang X., Gharaibeh B., Enyenihi A.H., Petersen I. Chromosomal instability and cytoskeletal defects in oral cancer cells. Proc Natl Acad Sci U S A. 2000;97:303–308. doi: 10.1073/pnas.97.1.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chin K., de Solorzano C.O., Knowles D., Jones A., Chou W., Rodriguez E.G. In situ analyses of genome instability in breast cancer. Nat Genet. 2004;36:984–988. doi: 10.1038/ng1409. [DOI] [PubMed] [Google Scholar]
- 55.Woo R.A., Poon R.Y. Activated oncogenes promote and cooperate with chromosomal instability for neoplastic transformation. Genes Dev. 2004;18:1317–1330. doi: 10.1101/gad.1165204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wei S., Sedivy J.M. Expression of catalytically active telomerase does not prevent premature senescence caused by overexpression of oncogenic Ha-Ras in normal human fibroblasts. Cancer Res. 1999;59:1539–1543. [PubMed] [Google Scholar]
- 57.Shay J.W., Wright W.E. Telomerase: a target for cancer therapeutics. Cancer Cell. 2002;2:257–265. doi: 10.1016/s1535-6108(02)00159-9. [DOI] [PubMed] [Google Scholar]
- 58.Di Leonardo A., Linke S.P., Clarkin K., Wahl G.M. DNA damage triggers a prolonged p53-dependent G1 arrest and long-term induction of Cip1 in normal human fibroblasts. Genes Dev. 1994;8:2540–2551. doi: 10.1101/gad.8.21.2540. [DOI] [PubMed] [Google Scholar]
- 59.Serrano M., Lin A.W., McCurrach M.E., Beach D., Lowe S.W. Oncogenic ras provokes premature cell senescence associated with accumulation of p53 and p16INK4a. Cell. 1997;88:593–602. doi: 10.1016/s0092-8674(00)81902-9. [DOI] [PubMed] [Google Scholar]
- 60.Serrano M., Blasco M.A. Putting the stress on senescence. Curr Opin Cell Biol. 2001;13:748–753. doi: 10.1016/s0955-0674(00)00278-7. [DOI] [PubMed] [Google Scholar]
- 61.Sharpless N.E., DePinho R.A. Telomeres, stem cells, senescence, and cancer. J Clin Invest. 2004;113:160–168. doi: 10.1172/JCI20761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Carnero A., Link W., Martinez J.F., Renner O., Castro M.E., Blanco F. Cellular senescence and cancer. Res Adv Cancer. 2003;3:183–198. [Google Scholar]
- 63.Chandeck C., Mooi W.J. Oncogene-induced cellular senescence. Adv Anat Pathol. 2010;17:42–48. doi: 10.1097/PAP.0b013e3181c66f4e. [DOI] [PubMed] [Google Scholar]
- 64.Braig M., Schmitt C.A. Oncogene-induced senescence: putting the brakes on tumor development. Cancer Res. 2006;66:2881–2884. doi: 10.1158/0008-5472.CAN-05-4006. [DOI] [PubMed] [Google Scholar]
- 65.Courtois-Cox S., Jones S.L., Cichowski K. Many roads lead to oncogene-induced senescence. Oncogene. 2008;27:2801–2809. doi: 10.1038/sj.onc.1210950. [DOI] [PubMed] [Google Scholar]
- 66.Narlik-Grassow M., Blanco-Aparicio C., Cecilia Y., Perez M., Munoz-Galvan S., Canamero M. Conditional transgenic expression of PIM1 kinase in prostate induces inflammation-dependent neoplasia. PLOS ONE. 2013;8:e60277. doi: 10.1371/journal.pone.0060277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Vergel M., Carnero A. Bypassing cellular senescence by genetic screening tools. Clin Transl Oncol. 2010;12:410–417. doi: 10.1007/s12094-010-0528-2. [DOI] [PubMed] [Google Scholar]
- 68.Bringold F., Serrano M. Tumor suppressors and oncogenes in cellular senescence. Exp Gerontol. 2000;35:317–329. doi: 10.1016/s0531-5565(00)00083-8. [DOI] [PubMed] [Google Scholar]
- 69.Bartek J., Bartkova J., Lukas J. DNA damage signalling guards against activated oncogenes and tumour progression. Oncogene. 2007;26:7773–7779. doi: 10.1038/sj.onc.1210881. [DOI] [PubMed] [Google Scholar]
- 70.Ruzankina Y., Asare A., Brown E.J. Replicative stress, stem cells and aging. Mech Ageing Dev. 2008;129:460–466. doi: 10.1016/j.mad.2008.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kenyon J., Gerson S.L. The role of DNA damage repair in aging of adult stem cells. Nucleic Acids Res. 2007;35:7557–7565. doi: 10.1093/nar/gkm1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Di Micco R., Fumagalli M., Cicalese A., Piccinin S., Gasparini P., Luise C. Oncogene-induced senescence is a DNA damage response triggered by DNA hyper-replication. Nature. 2006;444:638–642. doi: 10.1038/nature05327. [DOI] [PubMed] [Google Scholar]
- 73.Lin A.W., Lowe S.W. Oncogenic ras activates the ARF-p53 pathway to suppress epithelial cell transformation. Proc Natl Acad Sci U S A. 2001;98:5025–5030. doi: 10.1073/pnas.091100298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Braig M., Lee S., Loddenkemper C., Rudolph C., Peters A.H., Schlegelberger B. Oncogene-induced senescence as an initial barrier in lymphoma development. Nature. 2005;436:660–665. doi: 10.1038/nature03841. [DOI] [PubMed] [Google Scholar]
- 75.Chen Z., Trotman L.C., Shaffer D., Lin H.K., Dotan Z.A., Niki M. Crucial role of p53-dependent cellular senescence in suppression of Pten-deficient tumorigenesis. Nature. 2005;436:725–730. doi: 10.1038/nature03918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Collado M., Serrano M. The power and the promise of oncogene-induced senescence markers. Nat Rev Cancer. 2006;6:472–476. doi: 10.1038/nrc1884. [DOI] [PubMed] [Google Scholar]
- 77.Michaloglou C., Vredeveld L.C., Mooi W.J., Peeper D.S. BRAF(E600) in benign and malignant human tumours. Oncogene. 2008;27:877–895. doi: 10.1038/sj.onc.1210704. [DOI] [PubMed] [Google Scholar]
- 78.Blanco-Aparicio C., Canamero M., Cecilia Y., Pequeno B., Renner O., Ferrer I. Exploring the gain of function contribution of AKT to mammary tumorigenesis in mouse models. PLoS ONE. 2010;5:e9305. doi: 10.1371/journal.pone.0009305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Gray-Schopfer V.C., Cheong S.C., Chong H., Chow J., Moss T., Abdel-Malek Z.A. Cellular senescence in naevi and immortalisation in melanoma: a role for p16? Br J Cancer. 2006;95:496–505. doi: 10.1038/sj.bjc.6603283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ewald J.A., Desotelle J.A., Wilding G., Jarrard D.F. Therapy-induced senescence in cancer. J Natl Cancer Inst. 2010;102:1536–1546. doi: 10.1093/jnci/djq364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Cozzi S.J., Parsons P.G., Ogbourne S.M., Pedley J., Boyle G.M. Induction of senescence in diterpene ester-treated melanoma cells via protein kinase C-dependent hyperactivation of the mitogen-activated protein kinase pathway. Cancer Res. 2006;66:10083–10091. doi: 10.1158/0008-5472.CAN-06-0348. [DOI] [PubMed] [Google Scholar]
- 82.Schwarze S.R., Fu V.X., Desotelle J.A., Kenowski M.L., Jarrard D.F. The identification of senescence-specific genes during the induction of senescence in prostate cancer cells. Neoplasia. 2005;7:816–823. doi: 10.1593/neo.05250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Shelton D.N., Chang E., Whittier P.S., Choi D., Funk W.D. Microarray analysis of replicative senescence. Curr Biol. 1999;9:939–945. doi: 10.1016/s0960-9822(99)80420-5. [DOI] [PubMed] [Google Scholar]
- 84.Schwarze S.R., DePrimo S.E., Grabert L.M., Fu V.X., Brooks J.D., Jarrard D.F. Novel pathways associated with bypassing cellular senescence in human prostate epithelial cells. J Biol Chem. 2002;277:14877–14883. doi: 10.1074/jbc.M200373200. [DOI] [PubMed] [Google Scholar]
- 85.de Magalhaes J.P., Chainiaux F., de Longueville F., Mainfroid V., Migeot V., Marcq L. Gene expression and regulation in H2O2-induced premature senescence of human foreskin fibroblasts expressing or not telomerase. Exp Gerontol. 2004;39:1379–1389. doi: 10.1016/j.exger.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 86.Collado M., Gil J., Efeyan A., Guerra C., Schuhmacher A.J., Barradas M. Tumour biology: senescence in premalignant tumours. Nature. 2005;436:642. doi: 10.1038/436642a. [DOI] [PubMed] [Google Scholar]
- 87.Darbro B.W., Schneider G.B., Klingelhutz A.J. Co-regulation of p16INK4A and migratory genes in culture conditions that lead to premature senescence in human keratinocytes. J Invest Dermatol. 2005;125:499–509. doi: 10.1111/j.0022-202X.2005.23844.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Franco N., Lamartine J., Frouin V., Le Minter P., Petat C., Leplat J.J. Low-dose exposure to gamma rays induces specific gene regulations in normal human keratinocytes. Radiat Res. 2005;163:623–635. doi: 10.1667/rr3391. [DOI] [PubMed] [Google Scholar]
- 89.Alcorta D.A., Xiong Y., Phelps D., Hannon G., Beach D., Barrett J.C. Invovement of the cyclin-dependent kinase inhibitor p16 (INK4a) in replicative senescence of normal human fibroblasts. Proc Natl Acad Sci U S A. 1996;93:13742–13747. doi: 10.1073/pnas.93.24.13742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Stein G.H., Drullinger L.F., Soulard A., Dulic V. Differential roles for cyclin-dependent kinase inhibitors p21 and p16 in the mechanisms of senescence and differentiation in human fibroblasts. Mol Cell Biol. 1999;19:2109–2117. doi: 10.1128/mcb.19.3.2109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Schmitt C.A., Fridman J.S., Yang M., Lee S., Baranov E., Hoffman R.M. A senescence program controlled by p53 and p16INK4a contributes to the outcome of cancer therapy. Cell. 2002;109:335–346. doi: 10.1016/s0092-8674(02)00734-1. [DOI] [PubMed] [Google Scholar]
- 92.Yaswen P., Stampfer M.R. Molecular changes accompanying senescence and immortalization of cultured human mammary epithelial cells. Int J Biochem Cell Biol. 2002;34:1382–1394. doi: 10.1016/s1357-2725(02)00047-x. [DOI] [PubMed] [Google Scholar]
- 93.Michaloglou C., Vredeveld L.C., Soengas M.S., Denoyelle C., Kuilman T., van der Horst C.M. BRAFE600-associated senescence-like cell cycle arrest of human naevi. Nature. 2005;436:720–724. doi: 10.1038/nature03890. [DOI] [PubMed] [Google Scholar]
- 94.Wynford-Thomas D. p53: guardian of cellular senescence. J Pathol. 1996;180:118–121. doi: 10.1002/(SICI)1096-9896(199610)180:2<118::AID-PATH673>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 95.Bond J., Haughton M., Blaydes J., Gire V., Wynford-Thomas D., Wyllie F. Evidence that transcriptional activation by p53 plays a direct role in the induction of cellular senescence. Oncogene. 1996;13:2097–2104. [PubMed] [Google Scholar]
- 96.Feldser D.M., Greider C.W. Short telomeres limit tumor progression in vivo by inducing senescence. Cancer Cell. 2007;11:461–469. doi: 10.1016/j.ccr.2007.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ashcroft M., Taya Y., Vousden K.H. Stress signals utilize multiple pathways to stabilize p53. Mol Cell Biol. 2000;20:3224–3233. doi: 10.1128/mcb.20.9.3224-3233.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Blaydes J.P., Wynford-Thomas D. The proliferation of normal human fibroblasts is dependent upon negative regulation of p53 function by mdm2. Oncogene. 1998;16:3317–3322. doi: 10.1038/sj.onc.1201880. [DOI] [PubMed] [Google Scholar]
- 99.Kamijo T., Zindy F., Roussel M.F., Quelle D.E., Downing J.R., Ashmun R.A. Tumor suppression at the mouse INK4a locus mediated by the alternative reading frame product p19ARF. Cell. 1997;91:649–659. doi: 10.1016/s0092-8674(00)80452-3. [DOI] [PubMed] [Google Scholar]
- 100.Carnero A., Hudson J.D., Price C.M., Beach D.H. p16INK4A and p19ARF act in overlapping pathways in cellular immortalization. Nat Cell Biol. 2000;2:148–155. doi: 10.1038/35004020. [DOI] [PubMed] [Google Scholar]
- 101.Brown J.P., Wei W., Sedivy J.M. Bypass of senescence after disruption of p21CIP1/WAF1 gene in normal diploid human fibroblasts. Science. 1997;277:831–834. doi: 10.1126/science.277.5327.831. [DOI] [PubMed] [Google Scholar]
- 102.el-Deiry W.S., Tokino T., Velculescu V.E., Levy D.B., Parsons R., Trent J.M. WAF1, a potential mediator of p53 tumor suppression. Cell. 1993;75:817–825. doi: 10.1016/0092-8674(93)90500-p. [DOI] [PubMed] [Google Scholar]
- 103.Harper J.W., Adami G.R., Wei N., Keyomarsi K., Elledge S.J. The p21 Cdk-interacting protein Cip1 is a potent inhibitor of G1 cyclin-dependent kinases. Cell. 1993;75:805–816. doi: 10.1016/0092-8674(93)90499-g. [DOI] [PubMed] [Google Scholar]
- 104.Sherr C.J., Roberts J.M. CDK inhibitors: positive and negative regulators of G1-phase progression. Genes Dev. 1999;13:1501–1512. doi: 10.1101/gad.13.12.1501. [DOI] [PubMed] [Google Scholar]
- 105.Malumbres M., Carnero A. Cell cycle deregulation: a common motif in cancer. Prog Cell Cycle Res. 2003;5:5–18. [PubMed] [Google Scholar]
- 106.Carnero A., Beach D.H. Absence of p21WAF1 cooperates with c-myc in bypassing Ras-induced senescence and enhances oncogenic cooperation. Oncogene. 2004;23:6006–6011. doi: 10.1038/sj.onc.1207839. [DOI] [PubMed] [Google Scholar]
- 107.Pantoja C., Serrano M. Murine fibroblasts lacking p21 undergo senescence and are resistant to transformation by oncogenic Ras. Oncogene. 1999;18:4974–4982. doi: 10.1038/sj.onc.1202880. [DOI] [PubMed] [Google Scholar]
- 108.Ho J.S., Ma W., Mao D.Y., Benchimol S. p53-Dependent transcriptional repression of c-myc is required for G1 cell cycle arrest. Mol Cell Biol. 2005;25:7423–7431. doi: 10.1128/MCB.25.17.7423-7431.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Castro M.E., Ferrer I., Cascon A., Guijarro M.V., Lleonart M., Cajal S.R. PPP1CA contributes to the senescence program induced by oncogenic Ras. Carcinogenesis. 2008;29:491–499. doi: 10.1093/carcin/bgm246. [DOI] [PubMed] [Google Scholar]
- 110.Rowland B.D., Denissov S.G., Douma S., Stunnenberg H.G., Bernards R., Peeper D.S. E2F transcriptional repressor complexes are critical downstream targets of p19(ARF)/p53-induced proliferative arrest. Cancer Cell. 2002;2:55–65. doi: 10.1016/s1535-6108(02)00085-5. [DOI] [PubMed] [Google Scholar]
- 111.Hara E., Tsuri H., Shinozaki S., Oda K. Cooperative effect of antisense-Rb and antisense-p53 oligomers on the extension of lifespan in human diploid fibroblasts, TIG-1. Biochem Biophys Res Commun. 1991;179:528–534. doi: 10.1016/0006-291x(91)91403-y. [DOI] [PubMed] [Google Scholar]
- 112.Shay J.W., Pereira-Smith O.M., Wright W.E. A role for both RB and p53 in the regulation of human cellular senescence. Exp Cell Res. 1991;196:33–39. doi: 10.1016/0014-4827(91)90453-2. [DOI] [PubMed] [Google Scholar]
- 113.Lundberg A.S., Hahn W.C., Gupta P., Weinberg R.A. Genes involved in senescence and immortalization. Curr Opin Cell Biol. 2000;12:705–709. doi: 10.1016/s0955-0674(00)00155-1. [DOI] [PubMed] [Google Scholar]
- 114.Pavletich N.P. Mechanisms of cyclin-dependent kinase regulation: structures of Cdks, their cyclin activators, and Cip and INK4 inhibitors. J Mol Biol. 1999;287:821–828. doi: 10.1006/jmbi.1999.2640. [DOI] [PubMed] [Google Scholar]
- 115.Chicas A., Wang X., Zhang C., McCurrach M., Zhao Z., Mert O. Dissecting the unique role of the retinoblastoma tumor suppressor during cellular senescence. Cancer Cell. 2010;17:376–387. doi: 10.1016/j.ccr.2010.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Dahiya A., Wong S., Gonzalo S., Gavin M., Dean D.C. Linking the Rb and polycomb pathways. Mol Cell. 2001;8:557–569. doi: 10.1016/s1097-2765(01)00346-x. [DOI] [PubMed] [Google Scholar]
- 117.Pajalunga D., Mazzola A., Salzano A.M., Biferi M.G., De Luca G., Crescenzi M. Critical requirement for cell cycle inhibitors in sustaining nonproliferative states. J Cell Biol. 2007;176:807–818. doi: 10.1083/jcb.200608109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Ezhevsky S.A., Nagahara H., Vocero-Akbani A.M., Gius D.R., Wei M.C., Dowdy S.F. Hypo-phosphorylation of the retinoblastoma protein (pRb) by cyclin D:Cdk4/6 complexes results in active pRb. Proc Natl Acad Sci U S A. 1997;94:10699–10704. doi: 10.1073/pnas.94.20.10699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Ezhevsky S.A., Ho A., Becker-Hapak M., Davis P.K., Dowdy S.F. Differential regulation of retinoblastoma tumor suppressor protein by G(1) cyclin-dependent kinase complexes in vivo. Mol Cell Biol. 2001;21:4773–4784. doi: 10.1128/MCB.21.14.4773-4784.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Markey M.P., Angus S.P., Strobeck M.W., Williams S.L., Gunawardena R.W., Aronow B.J. Unbiased analysis of RB-mediated transcriptional repression identifies novel targets and distinctions from E2F action. Cancer Res. 2002;62:6587–6597. [PubMed] [Google Scholar]
- 121.Vernell R., Helin K., Muller H. Identification of target genes of the p16INK4A-pRB-E2F pathway. J Biol Chem. 2003;278:46124–46137. doi: 10.1074/jbc.M304930200. [DOI] [PubMed] [Google Scholar]
- 122.Beausejour C.M., Krtolica A., Galimi F., Narita M., Lowe S.W., Yaswen P. Reversal of human cellular senescence: roles of the p53 and p16 pathways. EMBO J. 2003;22:4212–4222. doi: 10.1093/emboj/cdg417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Narita M., Narita M., Krizhanovsky V., Nunez S., Chicas A., Hearn S.A. A novel role for high-mobility group a proteins in cellular senescence and heterochromatin formation. Cell. 2006;126:503–514. doi: 10.1016/j.cell.2006.05.052. [DOI] [PubMed] [Google Scholar]
- 124.Zhang H.S., Gavin M., Dahiya A., Postigo A.A., Ma D., Luo R.X. Exit from G1 and S phase of the cell cycle is regulated by repressor complexes containing HDAC-Rb-hSWI/SNF and Rb-hSWI/SNF. Cell. 2000;101:79–89. doi: 10.1016/S0092-8674(00)80625-X. [DOI] [PubMed] [Google Scholar]
- 125.Strobeck M.W., Knudsen K.E., Fribourg A.F., DeCristofaro M.F., Weissman B.E., Imbalzano A.N. BRG-1 is required for RB-mediated cell cycle arrest. Proc Natl Acad Sci U S A. 2000;97:7748–7753. doi: 10.1073/pnas.97.14.7748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Brehm A., Miska E.A., McCance D.J., Reid J.L., Bannister A.J., Kouzarides T. Retinoblastoma protein recruits histone deacetylase to repress transcription. Nature. 1998;391:597–601. doi: 10.1038/35404. [DOI] [PubMed] [Google Scholar]
- 127.Young A.P., Longmore G.D. Differences in stability of repressor complexes at promoters underlie distinct roles for Rb family members. Oncogene. 2004;23:814–823. doi: 10.1038/sj.onc.1207187. [DOI] [PubMed] [Google Scholar]
- 128.Grewal S.I., Moazed D. Heterochromatin and epigenetic control of gene expression. Science. 2003;301:798–802. doi: 10.1126/science.1086887. [DOI] [PubMed] [Google Scholar]
- 129.Schotta G., Lachner M., Sarma K., Ebert A., Sengupta R., Reuter G. A silencing pathway to induce H3-K9 and H4-K20 trimethylation at constitutive heterochromatin. Genes Dev. 2004;18:1251–1262. doi: 10.1101/gad.300704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Rea S., Eisenhaber F., O’Carroll D., Strahl B.D., Sun Z.W., Schmid M. Regulation of chromatin structure by site-specific histone H3 methyltransferases. Nature. 2000;406:593–599. doi: 10.1038/35020506. [DOI] [PubMed] [Google Scholar]
- 131.Nielsen S.J., Schneider R., Bauer U.M., Bannister A.J., Morrison A., O’Carroll D. Rb targets histone H3 methylation and HP1 to promoters. Nature. 2001;412:561–565. doi: 10.1038/35087620. [DOI] [PubMed] [Google Scholar]
- 132.Gonzalo S., Blasco M.A. Role of Rb family in the epigenetic definition of chromatin. Cell Cycle. 2005;4:752–755. doi: 10.4161/cc.4.6.1720. [DOI] [PubMed] [Google Scholar]
- 133.Zhang R., Poustovoitov M.V., Ye X., Santos H.A., Chen W., Daganzo S.M. Formation of MacroH2A-containing senescence-associated heterochromatin foci and senescence driven by ASF1a and HIRA. Dev Cell. 2005;8:19–30. doi: 10.1016/j.devcel.2004.10.019. [DOI] [PubMed] [Google Scholar]
- 134.Ye X., Zerlanko B., Zhang R., Somaiah N., Lipinski M., Salomoni P. Definition of pRB- and p53-dependent and -independent steps in HIRA/ASF1a-mediated formation of senescence-associated heterochromatin foci. Mol Cell Biol. 2007;27:2452–2465. doi: 10.1128/MCB.01592-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Zhang R., Chen W., Adams P.D. Molecular dissection of formation of senescence-associated heterochromatin foci. Mol Cell Biol. 2007;27:2343–2358. doi: 10.1128/MCB.02019-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Chandra T., Kirschner K., Thuret J.Y., Pope B.D., Ryba T., Newman S. Independence of repressive histone marks and chromatin compaction during senescent heterochromatic layer formation. Mol Cell. 2012;47:203–214. doi: 10.1016/j.molcel.2012.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Guerra C., Mijimolle N., Dhawahir A., Dubus P., Barradas M., Serrano M. Tumor induction by an endogenous K-ras oncogene is highly dependent on cellular context. Cancer Cell. 2003;4:111–120. doi: 10.1016/s1535-6108(03)00191-0. [DOI] [PubMed] [Google Scholar]
- 138.Lazzerini Denchi E., Attwooll C., Pasini D., Helin K. Deregulated E2F activity induces hyperplasia and senescence-like features in the mouse pituitary gland. Mol Cell Biol. 2005;25:2660–2672. doi: 10.1128/MCB.25.7.2660-2672.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Xue W., Zender L., Miething C., Dickins R.A., Hernando E., Krizhanovsky V. Senescence and tumour clearance is triggered by p53 restoration in murine liver carcinomas. Nature. 2007;445:656–660. doi: 10.1038/nature05529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Ventura A., Kirsch D.G., McLaughlin M.E., Tuveson D.A., Grimm J., Lintault L. Restoration of p53 function leads to tumour regression in vivo. Nature. 2007;445:661–665. doi: 10.1038/nature05541. [DOI] [PubMed] [Google Scholar]
- 141.te Poele R.H., Okorokov A.L., Jardine L., Cummings J., Joel S.P. DNA damage is able to induce senescence in tumor cells in vitro and in vivo. Cancer Res. 2002;62:1876–1883. [PubMed] [Google Scholar]
- 142.Roberson R.S., Kussick S.J., Vallieres E., Chen S.Y., Wu D.Y. Escape from therapy-induced accelerated cellular senescence in p53-null lung cancer cells and in human lung cancers. Cancer Res. 2005;65:2795–2803. doi: 10.1158/0008-5472.CAN-04-1270. [DOI] [PubMed] [Google Scholar]
- 143.Jeyapalan J.C., Ferreira M., Sedivy J.M., Herbig U. Accumulation of senescent cells in mitotic tissue of aging primates. Mech Ageing Dev. 2007;128:36–44. doi: 10.1016/j.mad.2006.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Herbig U., Ferreira M., Condel L., Carey D., Sedivy J.M. Cellular senescence in aging primates. Science. 2006;311:1257. doi: 10.1126/science.1122446. [DOI] [PubMed] [Google Scholar]
- 145.Ressler S., Bartkova J., Niederegger H., Bartek J., Scharffetter-Kochanek K., Jansen-Durr P. p16INK4A is a robust in vivo biomarker of cellular aging in human skin. Aging cell. 2006;5:379–389. doi: 10.1111/j.1474-9726.2006.00231.x. [DOI] [PubMed] [Google Scholar]
- 146.Melk A., Schmidt B.M., Takeuchi O., Sawitzki B., Rayner D.C., Halloran P.F. Expression of p16INK4a and other cell cycle regulator and senescence associated genes in aging human kidney. Kidney Int. 2004;65:510–520. doi: 10.1111/j.1523-1755.2004.00438.x. [DOI] [PubMed] [Google Scholar]
- 147.Nielsen G.P., Stemmer-Rachamimov A.O., Shaw J., Roy J.E., Koh J., Louis D.N. Immunohistochemical survey of p16INK4A expression in normal human adult and infant tissues. Lab Invest. 1999;79:1137–1143. [PubMed] [Google Scholar]
- 148.Molofsky A.V., Slutsky S.G., Joseph N.M., He S., Pardal R., Krishnamurthy J. Increasing p16INK4a expression decreases forebrain progenitors and neurogenesis during ageing. Nature. 2006;443:448–452. doi: 10.1038/nature05091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Janzen V., Forkert R., Fleming H.E., Saito Y., Waring M.T., Dombkowski D.M. Stem-cell ageing modified by the cyclin-dependent kinase inhibitor p16INK4a. Nature. 2006;443:421–426. doi: 10.1038/nature05159. [DOI] [PubMed] [Google Scholar]
- 150.Krishnamurthy J., Ramsey M.R., Ligon K.L., Torrice C., Koh A., Bonner-Weir S. p16INK4a induces an age-dependent decline in islet regenerative potential. Nature. 2006;443:453–457. doi: 10.1038/nature05092. [DOI] [PubMed] [Google Scholar]
- 151.Krishnamurthy J., Torrice C., Ramsey M.R., Kovalev G.I., Al-Regaiey K., Su L. Ink4a/Arf expression is a biomarker of aging. J Clin Invest. 2004;114:1299–1307. doi: 10.1172/JCI22475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Dimri G.P., Lee X., Basile G., Acosta M., Scott G., Roskelley C. A biomarker that identifies senescent human cells in culture and in aging skin in vivo. Proc Natl Acad Sci U S A. 1995;92:9363–9367. doi: 10.1073/pnas.92.20.9363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Ohtani N., Takahashi A., Mann D.J., Hara E. Cellular senescence: a double-edged sword in the fight against cancer. Exp Dermatol. 2012;21(Suppl. 1):1–4. doi: 10.1111/j.1600-0625.2012.01493.x. [DOI] [PubMed] [Google Scholar]
- 154.Bartkova J., Horejsi Z., Koed K., Kramer A., Tort F., Zieger K. DNA damage response as a candidate anticancer barrier in early human tumorigenesis. Nature. 2005;434:864–870. doi: 10.1038/nature03482. [DOI] [PubMed] [Google Scholar]
- 155.Baker D.J., Wijshake T., Tchkonia T., LeBrasseur N.K., Childs B.G., van de Sluis B. Clearance of p16Ink4a-positive senescent cells delays ageing-associated disorders. Nature. 2011;479:232–236. doi: 10.1038/nature10600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Jun J.I., Lau L.F. The matricellular protein CCN1 induces fibroblast senescence and restricts fibrosis in cutaneous wound healing. Nat Cell Biol. 2010;12:676–685. doi: 10.1038/ncb2070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Krizhanovsky V., Xue W., Zender L., Yon M., Hernando E., Lowe S.W. Implications of cellular senescence in tissue damage response, tumor suppression, and stem cell biology. Cold Spring Harb Symp Quant Biol. 2008;73:513–522. doi: 10.1101/sqb.2008.73.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Kang T.W., Yevsa T., Woller N., Hoenicke L., Wuestefeld T., Dauch D. Senescence surveillance of pre-malignant hepatocytes limits liver cancer development. Nature. 2011;479:547–551. doi: 10.1038/nature10599. [DOI] [PubMed] [Google Scholar]
- 159.Lujambio A., Akkari L., Simon J., Grace D., Tschaharganeh D.F., Bolden J.E. Non-cell-autonomous tumor suppression by p53. Cell. 2013;153:449–460. doi: 10.1016/j.cell.2013.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Pitiyage G.N., Slijepcevic P., Gabrani A., Chianea Y.G., Lim K.P., Prime S.S. Senescent mesenchymal cells accumulate in human fibrosis by a telomere-independent mechanism and ameliorate fibrosis through matrix metalloproteinases. J Pathol. 2011;223:604–617. doi: 10.1002/path.2839. [DOI] [PubMed] [Google Scholar]
- 161.Hoenicke L., Zender L. Immune surveillance of senescent cells – biological significance in cancer- and non-cancer pathologies. Carcinogenesis. 2012;33:1123–1126. doi: 10.1093/carcin/bgs124. [DOI] [PubMed] [Google Scholar]
- 162.Coppe J.P., Rodier F., Patil C.K., Freund A., Desprez P.Y., Campisi J. Tumor suppressor and aging biomarker p16(INK4a) induces cellular senescence without the associated inflammatory secretory phenotype. J Biol Chem. 2011;286:36396–36403. doi: 10.1074/jbc.M111.257071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Acosta J.C., O’Loghlen A., Banito A., Guijarro M.V., Augert A., Raguz S. Chemokine signaling via the CXCR2 receptor reinforces senescence. Cell. 2008;133:1006–1018. doi: 10.1016/j.cell.2008.03.038. [DOI] [PubMed] [Google Scholar]
- 164.Kuilman T., Michaloglou C., Vredeveld L.C., Douma S., van Doorn R., Desmet C.J. Oncogene-induced senescence relayed by an interleukin-dependent inflammatory network. Cell. 2008;133:1019–1031. doi: 10.1016/j.cell.2008.03.039. [DOI] [PubMed] [Google Scholar]
- 165.Novakova Z., Hubackova S., Kosar M., Janderova-Rossmeislova L., Dobrovolna J., Vasicova P. Cytokine expression and signaling in drug-induced cellular senescence. Oncogene. 2010;29:273–284. doi: 10.1038/onc.2009.318. [DOI] [PubMed] [Google Scholar]
- 166.Rodier F., Munoz D.P., Teachenor R., Chu V., Le O., Bhaumik D. DNA-SCARS: distinct nuclear structures that sustain damage-induced senescence growth arrest and inflammatory cytokine secretion. J Cell Sci. 2011;124:68–81. doi: 10.1242/jcs.071340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Rodier F., Coppé J.P., Patil C.K., Hoeijmakers W.A., Munoz D.P., Raza S.R. Persistent DNA damage signalling triggers senescence-associated inflammatory cytokine secretion. Nat Cell Biol. 2009;11:973–979. doi: 10.1038/ncb1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Freund A., Patil C.K., Campisi J. p38MAPK is a novel DNA damage response-independent regulator of the senescence-associated secretory phenotype. EMBO J. 2011;30:1536–1548. doi: 10.1038/emboj.2011.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Krtolica A., Parrinello S., Lockett S., Desprez P.Y., Campisi J. Senescent fibroblasts promote epithelial cell growth and tumorigenesis: a link between cancer and aging. Proc Natl Acad Sci U S A. 2001;98:12072–12077. doi: 10.1073/pnas.211053698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Freund A., Orjalo A.V., Desprez P.Y., Campisi J. Inflammatory networks during cellular senescence: causes and consequences. Trends Mol Med. 2010;16:238–246. doi: 10.1016/j.molmed.2010.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Davalos A.R., Coppé J.P., Campisi J., Desprez P.Y. Senescent cells as a source of inflammatory factors for tumor progression. Cancer Metastasis Rev. 2010;29:273–283. doi: 10.1007/s10555-010-9220-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Coppé J.P., Desprez P.Y., Krtolica A., Campisi J. The senescence-associated secretory phenotype: the dark side of tumor suppression. Annu Rev Pathol. 2010;5:99–118. doi: 10.1146/annurev-pathol-121808-102144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Coppé J.P., Patil C.K., Rodier F., Sun Y., Munoz D.P., Goldstein J. Senescence-associated secretory phenotypes reveal cell-nonautonomous functions of oncogenic RAS and the p53 tumor suppressor. PLoS Biol. 2008;6:2853–2868. doi: 10.1371/journal.pbio.0060301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Coppé J.P., Patil C.K., Rodier F., Krtolica A., Beauséjour C.M., Parrinello S. A human-like senescence-associated secretory phenotype is conserved in mouse cells dependent on physiological oxygen. PLoS ONE. 2010;5:e9188. doi: 10.1371/journal.pone.0009188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Rodier F. Detection of the senescence-associated secretory phenotype (SASP) Methods Mol Biol. 2013;965:165–173. doi: 10.1007/978-1-62703-239-1_10. [DOI] [PubMed] [Google Scholar]
- 176.Hubackova S., Krejcikova K., Bartek J., Hodny Z. IL1- and TGFbeta-Nox4 signaling, oxidative stress and DNA damage response are shared features of replicative, oncogene-induced, and drug-induced paracrine ‘bystander senescence’. Aging. 2012;4:932–951. doi: 10.18632/aging.100520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Acosta J.C., Banito A., Wuestefeld T., Georgilis A., Janich P., Morton J.P. A complex secretory program orchestrated by the inflammasome controls paracrine senescence. Nat Cell Biol. 2013;15:978–990. doi: 10.1038/ncb2784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Rodier F., Campisi J. Four Faces of cellular senescence. J Cell Biol. 2011;192:547–556. doi: 10.1083/jcb.201009094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Naylor R.M., Baker D.J., van Deursen J.M. Senescent cells: a novel therapeutic target for aging and age-related diseases. Clin Pharmacol Ther. 2013;93:105–116. doi: 10.1038/clpt.2012.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Tchkonia T., Zhu Y., van Deursen J., Campisi J., Kirkland J.L. Cellular senescence and the senescent secretory phenotype: therapeutic opportunities. J Clin Invest. 2013;123:966–972. doi: 10.1172/JCI64098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Parrinello S., Coppé J.P., Krtolica A., Campisi J. Stromal-epithelial interactions in aging and cancer: senescent fibroblasts alter epithelial cell differentiation. J Cell Sci. 2005;118:485–496. doi: 10.1242/jcs.01635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Bavik C., Coleman I., Dean J.P., Knudsen B., Plymate S., Nelson P.S. The gene expression program of prostate fibroblast senescence modulates neoplastic epithelial cell proliferation through paracrine mechanisms. Cancer Res. 2006;66:794–802. doi: 10.1158/0008-5472.CAN-05-1716. [DOI] [PubMed] [Google Scholar]
- 183.Liu D., Hornsby P.J. Senescent human fibroblasts increase the early growth of xenograft tumors via matrix metalloproteinase secretion. Cancer Res. 2007;67:3117–3126. doi: 10.1158/0008-5472.CAN-06-3452. [DOI] [PubMed] [Google Scholar]
- 184.Coppe J.P., Kauser K., Campisi J., Beausejour C.M. Secretion of vascular endothelial growth factor by primary human fibroblasts at senescence. J Biol Chem. 2006;281:29568–29574. doi: 10.1074/jbc.M603307200. [DOI] [PubMed] [Google Scholar]
- 185.Gilbert L.A., Hemann M.T. DNA damage-mediated induction of a chemoresistant niche. Cell. 2010;143:355–366. doi: 10.1016/j.cell.2010.09.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Jackson J.G., Pant V., Li Q., Chang L.L., Quintas-Cardama A., Garza D. p53-mediated senescence impairs the apoptotic response to chemotherapy and clinical outcome in breast cancer. Cancer Cell. 2012;21:793–806. doi: 10.1016/j.ccr.2012.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Sun Y., Campisi J., Higano C., Beer T.M., Porter P., Coleman I. Treatment-induced damage to the tumor microenvironment promotes prostate cancer therapy resistance through WNT16B. Nat Med. 2012;18:1359–1368. doi: 10.1038/nm.2890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Gosselin K., Martien S., Pourtier A., Vercamer C., Ostoich P., Morat L. Senescence-associated oxidative DNA damage promotes the generation of neoplastic cells. Cancer Res. 2009;69:7917–7925. doi: 10.1158/0008-5472.CAN-08-2510. [DOI] [PubMed] [Google Scholar]
- 189.Sherman M.Y., Meng L., Stampfer M., Gabai V.L., Yaglom J.A. Oncogenes induce senescence with incomplete growth arrest and suppress the DNA damage response in immortalized cells. Aging Cell. 2011;10:949–961. doi: 10.1111/j.1474-9726.2011.00736.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Nonet G.H., Stampfer M.R., Chin K., Gray J.W., Collins C.C., Yaswen P. The ZNF217 gene amplified in breast cancers promotes immortalization of human mammary epithelial cells. Cancer Res. 2001;61:1250–1254. [PubMed] [Google Scholar]
- 191.Bazarov A.V., Hines W.C., Mukhopadhyay R., Beliveau A., Melodyev S., Zaslavsky Y. Telomerase activation by c-Myc in human mammary epithelial cells requires additional genomic changes. Cell Cycle. 2009;8:3373–3378. doi: 10.4161/cc.8.20.9856. [DOI] [PubMed] [Google Scholar]
- 192.Bosco E.E., Wang Y., Xu H., Zilfou J.T., Knudsen K.E., Aronow B.J. The retinoblastoma tumor suppressor modifies the therapeutic response of breast cancer. J Clin Invest. 2007;117:218–228. doi: 10.1172/JCI28803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Dai C.Y., Enders G.H. p16 INK4a can initiate an autonomous senescence program. Oncogene. 2000;19:1613–1622. doi: 10.1038/sj.onc.1203438. [DOI] [PubMed] [Google Scholar]
- 194.Bazarov A.V., Lee W.J., Bazarov I., Bosire M., Hines W.C., Stankovich B. The specific role of pRb in p16 (INK4A) -mediated arrest of normal and malignant human breast cells. Cell Cycle. 2012;11:1008–1013. doi: 10.4161/cc.11.5.19492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Viatour P., Somervaille T.C., Venkatasubrahmanyam S., Kogan S., McLaughlin M.E., Weissman I.L. Hematopoietic stem cell quiescence is maintained by compound contributions of the retinoblastoma gene family. Cell Stem Cell. 2008;3:416–428. doi: 10.1016/j.stem.2008.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Jackson J.G., Pereira-Smith O.M. Primary and compensatory roles for RB family members at cell cycle gene promoters that are deacetylated and downregulated in doxorubicin-induced senescence of breast cancer cells. Mol Cell Biol. 2006;26:2501–2510. doi: 10.1128/MCB.26.7.2501-2510.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Fry D.W., Harvey P.J., Keller P.R., Elliott W.L., Meade M., Trachet E. Specific inhibition of cyclin-dependent kinase 4/6 by PD 0332991 and associated antitumor activity in human tumor xenografts. Mol Cancer Ther. 2004;3:1427–1438. [PubMed] [Google Scholar]
- 198.Saab R., Bills J.L., Miceli A.P., Anderson C.M., Khoury J.D., Fry D.W. Pharmacologic inhibition of cyclin-dependent kinase 4/6 activity arrests proliferation in myoblasts and rhabdomyosarcoma-derived cells. Mol Cancer Ther. 2006;5:1299–1308. doi: 10.1158/1535-7163.MCT-05-0383. [DOI] [PubMed] [Google Scholar]
- 199.Marzec M., Kasprzycka M., Lai R., Gladden A.B., Wlodarski P., Tomczak E. Mantle cell lymphoma cells express predominantly Cyclin D1a isoform and are highly sensitive to selective inhibition of CDK4 kinase activity. Blood. 2006;108:1744–1750. doi: 10.1182/blood-2006-04-016634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Finn R.S., Dering J., Conklin D., Kalous O., Cohen D.J., Desai A.J. PD 0332991, a selective cyclin D kinase 4/6 inhibitor, preferentially inhibits proliferation of luminal estrogen receptor-positive human breast cancer cell lines in vitro. Breast Cancer Res. 2009;11:R77. doi: 10.1186/bcr2419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.McClendon A.K., Dean J.L., Rivadeneira D.B., Yu J.E., Reed C.A., Gao E. CDK4/6 inhibition antagonizes the cytotoxic response to anthracycline therapy. Cell Cycle. 2012;11:2747–2755. doi: 10.4161/cc.21127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Soder A.I., Hoare S.F., Muir S., Going J.J., Parkinson E.K., Keith W.N. Amplification, increased dosage and in situ expression of the telomerase RNA gene in human cancer. Oncogene. 1997;14:1013–1021. doi: 10.1038/sj.onc.1201066. [DOI] [PubMed] [Google Scholar]
- 203.Zhang A., Zheng C., Lindvall C., Hou M., Ekedahl J., Lewensohn R. Frequent amplification of the telomerase reverse transcriptase gene in human tumors. Cancer Res. 2000;60:6230–6235. [PubMed] [Google Scholar]
- 204.Zhang A., Zheng C., Hou M., Lindvall C., Wallin K.L., Angstrom T. Amplification of the telomerase reverse transcriptase (hTERT) gene in cervical carcinomas. Genes Chromosomes Cancer. 2002;34:269–275. doi: 10.1002/gcc.10071. [DOI] [PubMed] [Google Scholar]
- 205.Takuma Y., Nouso K., Kobayashi Y., Nakamura S., Tanaka H., Matsumoto E. Telomerase reverse transcriptase gene amplification in hepatocellular carcinoma. J Gastroenterol Hepatol. 2004;19:1300–1304. doi: 10.1111/j.1440-1746.2004.03447.x. [DOI] [PubMed] [Google Scholar]
- 206.Pirker C., Holzmann K., Spiegl-Kreinecker S., Elbling L., Thallinger C., Pehamberger H. Chromosomal imbalances in primary and metastatic melanomas: over-representation of essential telomerase genes. Melanoma Res. 2003;13:483–492. doi: 10.1097/00008390-200310000-00007. [DOI] [PubMed] [Google Scholar]
- 207.Zhao Y., Wang S., Popova E.Y., Grigoryev S.A., Zhu J. Rearrangement of upstream sequences of the hTERT gene during cellular immortalization. Genes Chromosomes Cancer. 2009;48:963–974. doi: 10.1002/gcc.20698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Codd V., Nelson C.P., Albrecht E., Mangino M., Deelen J., Buxton J.L. Identification of seven loci affecting mean telomere length and their association with disease. Nat Genet. 2013;45:422–427. doi: 10.1038/ng.2528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Bojesen S.E., Pooley K.A., Johnatty S.E., Beesley J., Michailidou K., Tyrer J.P. Multiple independent variants at the TERT locus are associated with telomere length and risks of breast and ovarian cancer. Nat Genet. 2013;45:371–384. doi: 10.1038/ng.2566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Melin B.S., Nordfjall K., Andersson U., Roos G. hTERT cancer risk genotypes are associated with telomere length. Genet Epidemiol. 2012;36:368–372. doi: 10.1002/gepi.21630. [DOI] [PubMed] [Google Scholar]
- 211.Kote-Jarai Z., Saunders E.J., Leongamornlert D.A., Tymrakiewicz M., Dadaev T., Jugurnauth-Little S. Fine-mapping identifies multiple prostate cancer risk loci at 5p15, one of which associates with TERT expression. Hum Mol Genet. 2013;22:2520–2528. doi: 10.1093/hmg/ddt086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Atkinson S.P., Hoare S.F., Glasspool R.M., Keith W.N. Lack of telomerase gene expression in alternative lengthening of telomere cells is associated with chromatin remodeling of the hTR and hTERT gene promoters. Cancer Res. 2005;65:7585–7590. doi: 10.1158/0008-5472.CAN-05-1715. [DOI] [PubMed] [Google Scholar]
- 213.Soder A.I., Going J.J., Kaye S.B., Keith W.N. Tumour specific regulation of telomerase RNA gene expression visualized by in situ hybridization. Oncogene. 1998;16:979–983. doi: 10.1038/sj.onc.1201620. [DOI] [PubMed] [Google Scholar]
- 214.Plumb J.A., Bilsland A., Kakani R., Zhao J., Glasspool R.M., Knox R.J. Telomerase-specific suicide gene therapy vectors expressing bacterial nitroreductase sensitize human cancer cells to the pro-drug CB1954. Oncogene. 2001;20:7797–7803. doi: 10.1038/sj.onc.1204954. [DOI] [PubMed] [Google Scholar]
- 215.Bilsland A.E., Anderson C.J., Fletcher-Monaghan A.J., McGregor F., Evans T.R., Ganly I. Selective ablation of human cancer cells by telomerase-specific adenoviral suicide gene therapy vectors expressing bacterial nitroreductase. Oncogene. 2003;22:370–380. doi: 10.1038/sj.onc.1206168. [DOI] [PubMed] [Google Scholar]
- 216.Zhao J.Q., Glasspool R.M., Hoare S.F., Bilsland A., Szatmari I., Keith W.N. Activation of telomerase rna gene promoter activity by NF-Y, Sp1, and the retinoblastoma protein and repression by Sp3. Neoplasia. 2000;2:531–539. doi: 10.1038/sj.neo.7900114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Zhao J., Bilsland A., Jackson K., Keith W.N. MDM2 negatively regulates the human telomerase RNA gene promoter. BMC Cancer. 2005;5:6. doi: 10.1186/1471-2407-5-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Bilsland A.E., Stevenson K., Atkinson S., Kolch W., Keith W.N. Transcriptional repression of telomerase RNA gene expression by c-Jun-NH2-kinase and Sp1/Sp3. Cancer Res. 2006;66:1363–1370. doi: 10.1158/0008-5472.CAN-05-1941. [DOI] [PubMed] [Google Scholar]
- 219.Wu K.J., Grandori C., Amacker M., Simon-Vermot N., Polack A., Lingner J. Direct activation of TERT transcription by c-MYC. Nat Genet. 1999;21:220–224. doi: 10.1038/6010. [DOI] [PubMed] [Google Scholar]
- 220.Wick M., Zubov D., Hagen G. Genomic organization and promoter characterization of the gene encoding the human telomerase reverse transcriptase (hTERT) Gene. 1999;232:97–106. doi: 10.1016/s0378-1119(99)00108-0. [DOI] [PubMed] [Google Scholar]
- 221.Horikawa I., Cable P.L., Afshari C., Barrett J.C. Cloning and characterization of the promoter region of human telomerase reverse transcriptase gene. Cancer Res. 1999;59:826–830. [PubMed] [Google Scholar]
- 222.Anderson C.J., Hoare S.F., Ashcroft M., Bilsland A.E., Keith W.N. Hypoxic regulation of telomerase gene expression by transcriptional and post-transcriptional mechanisms. Oncogene. 2006;25:61–69. doi: 10.1038/sj.onc.1209011. [DOI] [PubMed] [Google Scholar]
- 223.Maida Y., Kyo S., Kanaya T., Wang Z., Yatabe N., Tanaka M. Direct activation of telomerase by EGF through Ets-mediated transactivation of TERT via MAP kinase signaling pathway. Oncogene. 2002;21:4071–4079. doi: 10.1038/sj.onc.1205509. [DOI] [PubMed] [Google Scholar]
- 224.Huang F.W., Hodis E., Xu M.J., Kryukov G.V., Chin L., Garraway L.A. Highly recurrent TERT promoter mutations in human melanoma. Science. 2013;339:957–959. doi: 10.1126/science.1229259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Horn S., Figl A., Rachakonda P.S., Fischer C., Sucker A., Gast A. TERT promoter mutations in familial and sporadic melanoma. Science. 2013;339:959–961. doi: 10.1126/science.1230062. [DOI] [PubMed] [Google Scholar]
- 226.Crowe D.L., Nguyen D.C. Rb and E2F-1 regulate telomerase activity in human cancer cells. Biochim Biophys Acta. 2001;1518:1–6. doi: 10.1016/s0167-4781(00)00296-7. [DOI] [PubMed] [Google Scholar]
- 227.Chou C.K., Lee D.F., Sun H.L., Li L.Y., Lin C.Y., Huang W.C. The suppression of MAD1 by AKT-mediated phosphorylation activates MAD1 target genes transcription. Mol Carcinog. 2009;48:1048–1058. doi: 10.1002/mc.20557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Wu S., Hultquist A., Hydbring P., Cetinkaya C., Oberg F., Larsson L.G. TGF-beta enforces senescence in Myc-transformed hematopoietic tumor cells through induction of Mad1 and repression of Myc activity. Exp Cell Res. 2009;315:3099–3111. doi: 10.1016/j.yexcr.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 229.Beyne-Rauzy O., Recher C., Dastugue N., Demur C., Pottier G., Laurent G. Tumor necrosis factor alpha induces senescence and chromosomal instability in human leukemic cells. Oncogene. 2004;23:7507–7516. doi: 10.1038/sj.onc.1208024. [DOI] [PubMed] [Google Scholar]
- 230.Henderson Y.C., Breau R.L., Liu T.J., Clayman G.L. Telomerase activity in head and neck tumors after introduction of wild-type p53, p21, p16, and E2F-1 genes by means of recombinant adenovirus. Head Neck. 2000;22:347–354. doi: 10.1002/1097-0347(200007)22:4<347::aid-hed6>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 231.Hoffmeyer K., Raggioli A., Rudloff S., Anton R., Hierholzer A., Del Valle I. Wnt/beta-catenin signaling regulates telomerase in stem cells and cancer cells. Science. 2012;336:1549–1554. doi: 10.1126/science.1218370. [DOI] [PubMed] [Google Scholar]
- 232.Zhang Y., Toh L., Lau P., Wang X. Human telomerase reverse transcriptase (hTERT) is a novel target of the Wnt/beta-catenin pathway in human cancer. J Biol Chem. 2012;287:32494–32511. doi: 10.1074/jbc.M112.368282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Jaitner S., Reiche J.A., Schaffauer A.J., Hiendlmeyer E., Herbst H., Brabletz T. Human telomerase reverse transcriptase (hTERT) is a target gene of beta-catenin in human colorectal tumors. Cell Cycle. 2012;11:3331–3338. doi: 10.4161/cc.21790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Bilsland A.E., Hoare S., Stevenson K., Plumb J., Gomez-Roman N., Cairney C. Dynamic telomerase gene suppression via network effects of GSK3 inhibition. PLoS ONE. 2009;4:e6459. doi: 10.1371/journal.pone.0006459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Wang J., Xie L.Y., Allan S., Beach D., Hannon G.J. Myc activates telomerase. Genes Dev. 1998;12:1769–1774. doi: 10.1101/gad.12.12.1769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Harley C.B. Telomerase and cancer therapeutics. Nat Rev Cancer. 2008;8:167–179. doi: 10.1038/nrc2275. [DOI] [PubMed] [Google Scholar]
- 237.Bryan T.M., Englezou A., Gupta J., Bacchetti S., Reddel R.R. Telomere elongation in immortal human cells without detectable telomerase activity. EMBO J. 1995;14:4240–4248. doi: 10.1002/j.1460-2075.1995.tb00098.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Bryan T.M., Englezou A., Dalla-Pozza L., Dunham M.A., Reddel R.R. Evidence for an alternative mechanism for maintaining telomere length in human tumors and tumor-derived cell lines. Nat Med. 1997;3:1271–1274. doi: 10.1038/nm1197-1271. [DOI] [PubMed] [Google Scholar]
- 239.Chang S., Khoo C.M., Naylor M.L., Maser R.S., DePinho R.A. Telomere-based crisis: functional differences between telomerase activation and ALT in tumor progression. Genes Dev. 2003;17:88–100. doi: 10.1101/gad.1029903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Hu J., Hwang S.S., Liesa M., Gan B., Sahin E., Jaskelioff M. Antitelomerase therapy provokes ALT and mitochondrial adaptive mechanisms in cancer. Cell. 2012;148:651–663. doi: 10.1016/j.cell.2011.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Shay J.W., Wright W.E. Telomeres and telomerase in normal and cancer stem cells. FEBS Lett. 2010;584:3819–3825. doi: 10.1016/j.febslet.2010.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Sprouse A.A., Steding C.E., Herbert B.S. Pharmaceutical regulation of telomerase and its clinical potential. J Cell Mol Med. 2012;16:1–7. doi: 10.1111/j.1582-4934.2011.01460.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Podlevsky J.D., Chen J.J. It all comes together at the ends: telomerase structure, function, and biogenesis. Mutat Res. 2012;730:3–11. doi: 10.1016/j.mrfmmm.2011.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Zhang X., Mar V., Zhou W., Harrington L., Robinson M. Telomere shortening and apoptosisin telomerase-inhibited human tumor cells. Genes Dev. 1999;13:2388–2399. doi: 10.1101/gad.13.18.2388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Tauchi T., Nakajima A., Sashida G., Shimamoto T., Ohyashiki J.H., Abe K. Inhibition of human telomerase enhances the effect of the tyrosine kinase inhibitor, imatinib, in BCR-ABL-positive leukemia cells. Clin Cancer Res. 2002;8:3341–3347. [PubMed] [Google Scholar]
- 246.Delhommeau F., Thierry A., Feneux D., Lauret E., Leclercq E., Courtier M.H. Telomere dysfunction and telomerase reactivation in human leukemia cell lines after telomerase inhibition by the expression of a dominant-negative hTERT mutant. Oncogene. 2002;21:8262–8271. doi: 10.1038/sj.onc.1206054. [DOI] [PubMed] [Google Scholar]
- 247.Nakajima A., Tauchi T., Sashida G., Sumi M., Abe K., Yamamoto K. Telomerase inhibition enhances apoptosis in human acute leukemia cells: possibility of antitelomerase therapy. Leukemia. 2003;17:560–567. doi: 10.1038/sj.leu.2402825. [DOI] [PubMed] [Google Scholar]
- 248.Roth A., Vercauteren S., Sutherland H.J., Lansdorp P.M. Telomerase is limiting the growth of acute myeloid leukemia cells. Leukemia. 2003;17:2410–2417. doi: 10.1038/sj.leu.2403177. [DOI] [PubMed] [Google Scholar]
- 249.Feng J., Funk W.D., Wang S.-S., Weinrich S.L., Avilion A.A., Chiu C.-P. The RNA component of human telomerase. Science. 1995;269:1236–1241. doi: 10.1126/science.7544491. [DOI] [PubMed] [Google Scholar]
- 250.Norton J.C., Piatyszek M.A., Wright W.E., Shay J.W., Corey D.R. Inhibition of human telomerase activity by peptide nucleic acids. Nat Biotechnol. 1996;14:615–619. doi: 10.1038/nbt0596-615. [DOI] [PubMed] [Google Scholar]
- 251.Kondo S., Tanaka Y., Kondo Y., Hitomi M., Barnett G.H., Ishizaka Y. Antisense telomerase treatment: induction of two distinct pathways, apoptosis and differentiation. FASEB J. 1998;12:801–811. doi: 10.1096/fasebj.12.10.801. [DOI] [PubMed] [Google Scholar]
- 252.Pitts A.E., Corey D.R. Inhibition of human telomerase by 2′-O-methyl-RNA. Proc Natl Acad Sci U S A. 1998;95:11549–11554. doi: 10.1073/pnas.95.20.11549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Herbert B., Pitts A.E., Baker S.I., Hamilton S.E., Wright W.E., Shay J.W. Inhibition of human telomerase in immortal human cells leads to progressive telomere shortening and cell death. Proc Natl Acad Sci U S A. 1999;96:14276–14281. doi: 10.1073/pnas.96.25.14276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Herbert B.S., Pongracz K., Shay J.W., Gryaznov S.M. Oligonucleotide N3′ → P5′ phosphoramidates as efficient telomerase inhibitors. Oncogene. 2002;21:638–642. doi: 10.1038/sj.onc.1205064. [DOI] [PubMed] [Google Scholar]
- 255.Corey D.R. Telomerase inhibition, oligonucleotides, and clinical trials. Oncogene. 2002;21:631–637. doi: 10.1038/sj.onc.1205063. [DOI] [PubMed] [Google Scholar]
- 256.Asai A., Oshima Y., Yamamoto Y., Uochi T.A., Kusaka H., Akinaga S. A novel telomerase template antagonist (GRN163) as a potential anticancer agent. Cancer Res. 2003;63:3931–3939. [PubMed] [Google Scholar]
- 257.Wang E.S., Wu K., Chin A.C., Chen-Kiang S., Pongracz K., Gryaznov S. Telomerase inhibition with an oligonucleotide telomerase template antagonist: in vitro and in vivo studies in multiple myeloma and lymphoma. Blood. 2004;103:258–266. doi: 10.1182/blood-2003-02-0546. [DOI] [PubMed] [Google Scholar]
- 258.Akiyama M., Hideshima T., Shammas M.A., Hayashi T., Hamasaki M., Tai Y.T. Effects of oligonucleotide N3′ → P5′ thio-phosphoramidate (GRN163) targeting telomerase RNA in human multiple myeloma cells. Cancer Res. 2003;63:6187–6194. [PubMed] [Google Scholar]
- 259.Djojosubroto M.W., Chin A.C., Go N., Schaetzlein S., Manns M.P., Gryaznov S. Telomerase antagonists GRN163 and GRN163L inhibit tumor growth and increase chemosensitivity of human hepatoma. Hepatology. 2005;42:1127–1136. doi: 10.1002/hep.20822. [DOI] [PubMed] [Google Scholar]
- 260.Herbert B.S., Gellert G.C., Hochreiter A., Pongracz K., Wright W.E., Zielinska D. Lipid modification of GRN163, an N3′ → P5′ thio-phosphoramidate oligonucleotide, enhances the potency of telomerase inhibition. Oncogene. 2005;24:5262–5268. doi: 10.1038/sj.onc.1208760. [DOI] [PubMed] [Google Scholar]
- 261.Tokcaer-Keskin Z., Dikmen Z.G., Ayaloglu-Butun F., Gultekin S., Gryaznov S.M., Akcali K.C. The effect of telomerase template antagonist GRN163L on bone-marrow-derived rat mesenchymal stem cells is reversible and associated with altered expression of cyclin d1, cdk4 and cdk6. Stem Cell Rev. 2010;6:224–233. doi: 10.1007/s12015-010-9124-7. [DOI] [PubMed] [Google Scholar]
- 262.Gellert G.C., Dikmen Z.G., Wright W.E., Gryaznov S., Shay J.W. Effects of a novel telomerase inhibitor, GRN163L, in human breast cancer. Breast Cancer Res Treat. 2006;96:73–81. doi: 10.1007/s10549-005-9043-5. [DOI] [PubMed] [Google Scholar]
- 263.Hochreiter A.E., Xiao H., Goldblatt E.M., Gryaznov S.M., Miller K.D., Badve S. Telomerase template antagonist GRN163L disrupts telomere maintenance, tumor growth, and metastasis of breast cancer. Clin Cancer Res. 2006;12:3184–3192. doi: 10.1158/1078-0432.CCR-05-2760. [DOI] [PubMed] [Google Scholar]
- 264.Dikmen Z.G., Gellert G.C., Jackson S., Gryaznov S., Tressler R., Dogan P. In vivo inhibition of lung cancer by GRN163L: a novel human telomerase inhibitor. Cancer Res. 2005;65:7866–7873. doi: 10.1158/0008-5472.CAN-05-1215. [DOI] [PubMed] [Google Scholar]
- 265.Shammas M.A., Koley H., Bertheau R.C., Neri P., Fulciniti M., Tassone P. Telomerase inhibitor GRN163L inhibits myeloma cell growth in vitro and in vivo. Leukemia. 2008;22:1410–1418. doi: 10.1038/leu.2008.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Jackson S.R., Zhu C.H., Paulson V., Watkins L., Dikmen Z.G., Gryaznov S.M. Antiadhesive effects of GRN163L – an oligonucleotide N3′→P5′ thio-phosphoramidate targeting telomerase. Cancer Res. 2007;67:1121–1129. doi: 10.1158/0008-5472.CAN-06-2306. [DOI] [PubMed] [Google Scholar]
- 267.Mender I., Senturk S., Ozgunes N., Akcali K.C., Kletsas D., Gryaznov S. Imetelstat (a telomerase antagonist) exerts offtarget effects on the cytoskeleton. Int J Oncol. 2013;42:1709–1715. doi: 10.3892/ijo.2013.1865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Kraemer K., Fuessel S., Schmidt U., Kotzsch M., Schwenzer B., Wirth M.P. Antisense-mediated hTERT inhibition specifically reduces the growth of human bladder cancer cells. Clin Cancer Res. 2003;9:3794–3800. [see comment] [PubMed] [Google Scholar]
- 269.Folini M., Brambilla C., Villa R., Gandellini P., Vignati S., Paduano F. Antisense oligonucleotide-mediated inhibition of hTERT, but not hTERC, induces rapid cell growth decline and apoptosis in the absence of telomere shortening in human prostate cancer cells. Eur J Cancer. 2005;41:624–634. doi: 10.1016/j.ejca.2004.12.002. [DOI] [PubMed] [Google Scholar]
- 270.Yuan Z., Mei H.D. Inhibition of telomerase activity with hTERT antisense increases the effect of CDDP-induced apoptosis in myeloid leukemia. Hematol J. 2002;3:201–205. doi: 10.1038/sj.thj.6200177. [DOI] [PubMed] [Google Scholar]
- 271.Kosciolek B.A., Kalantidis K., Tabler M., Rowley P.T. Inhibition of telomerase activity in human cancer cells by RNA interference. Mol Cancer Ther. 2003;2:209–216. [PubMed] [Google Scholar]
- 272.Kanazawa Y., Ohkawa K., Ueda K., Mita E., Takehara T., Sasaki Y. Hammerhead ribozyme-mediated inhibition of telomerase activity in extracts of human hepatocellular carcinoma cells. Biochem Biophys Res Commun. 1996;225:570–576. doi: 10.1006/bbrc.1996.1213. [DOI] [PubMed] [Google Scholar]
- 273.Folini M., Colella G., Villa R., Lualdi S., Daidone M.G., Zaffaroni N. Inhibition of telomerase activity by a hammerhead ribozyme targeting the RNA component of telomerase in human melanoma cells. J Invest Dermatol. 2000;114:259–267. doi: 10.1046/j.1523-1747.2000.00870.x. [DOI] [PubMed] [Google Scholar]
- 274.Yokoyama Y., Takahashi Y., Shinohara A., Wan X., Takahashi S., Niwa K. The 5′-end of hTERT mRNA is a good target for hammerhead ribozyme to suppress telomerase activity. Biochem Biophys Res Commun. 2000;273:316–321. doi: 10.1006/bbrc.2000.2939. [DOI] [PubMed] [Google Scholar]
- 275.Ludwig A., Saretzki G., Holm P.S., Tiemann F., Lorenz M., Emrich T. Ribozyme cleavage of telomerase mRNA sensitizes breast epithelial cells to inhibitors of topoisomerase. Cancer Res. 2001;61:3053–3061. [PubMed] [Google Scholar]
- 276.Shammas M.A., Koley H., Batchu R.B., Bertheau R.C., Protopopov A., Munshi N.C. Telomerase inhibition by siRNA causes senescence and apoptosis in Barrett's adenocarcinoma cells: mechanism and therapeutic potential. Mol Cancer. 2005;4:24. doi: 10.1186/1476-4598-4-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Masutomi K., Possemato R., Wong J.M., Currier J.L., Tothova Z., Manola J.B. The telomerase reverse transcriptase regulates chromatin state and DNA damage responses. Proc Natl Acad Sci U S A. 2005;102:8222–8227. doi: 10.1073/pnas.0503095102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Yuan J., Yang B.M., Zhong Z.H., Shats I., Milyavsky M., Rotter V. Upregulation of survivin during immortalization of nontransformed human fibroblasts transduced with telomerase reverse transcriptase. Oncogene. 2009;28:2678–2689. doi: 10.1038/onc.2009.136. [DOI] [PubMed] [Google Scholar]
- 279.Li S., Rosenberg J.E., Donjacour A.A., Botchkina I.L., Hom Y.K., Cunha G.R. Rapid inhibition of cancer cell growth induced by lentiviral delivery and expression of mutant-template telomerase RNA and anti-telomerase short-interfering RNA. Cancer Res. 2004;64:4833–4840. doi: 10.1158/0008-5472.CAN-04-0953. [DOI] [PubMed] [Google Scholar]
- 280.Smith L.L., Coller H.A., Roberts J.M. Telomerase modulates expression of growth-controlling genes and enhances cell proliferation. Nat Cell Biol. 2003;5:474–479. doi: 10.1038/ncb985. [DOI] [PubMed] [Google Scholar]
- 281.Stewart S.A., Hahn W.C., O’Connor B.F., Banner E.N., Lundberg A.S., Modha P. Telomerase contributes to tumorigenesis by a telomere length-independent mechanism. Proc Natl Acad Sci U S A. 2002;99:12606–12611. doi: 10.1073/pnas.182407599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Naasani I., Seimiya H., Yamori T., Tsuruo T. FJ5002: a potent telomerase inhibitor identified by exploiting the disease-oriented screening program with COMPARE analysis. Cancer Res. 1999;59:4004–4011. [PubMed] [Google Scholar]
- 283.Hayakawa N., Nozawa K., Ogawa A., Kato N., Yoshida K., Akamatsu K. Isothiazolone derivatives selectively inhibit telomerase from human and rat cancer cells in vitro. Biochemistry. 1999;38:11501–11507. doi: 10.1021/bi982829k. [DOI] [PubMed] [Google Scholar]
- 284.Damm K., Hemmann U., Garin-Chesa P., Hauel N., Kauffmann I., Priepke H. A highly selective telomerase inhibitor limiting human cancer cell proliferation. EMBO J. 2001;20:6958–6968. doi: 10.1093/emboj/20.24.6958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Kleideiter E., Piotrowska K., Klotz U. Screening of telomerase inhibitors. Methods Mol Biol. 2007;405:167–180. doi: 10.1007/978-1-60327-070-0_13. [DOI] [PubMed] [Google Scholar]
- 286.Wong L.H., Unciti-Broceta A., Spitzer M., White R., Tyers M., Harrington L. A yeast chemical genetic screen identifies inhibitors of human telomerase. Chem Biol. 2013;20:333–340. doi: 10.1016/j.chembiol.2012.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Seimiya H., Oh-hara T., Suzuki T., Naasani I., Shimazaki T., Tsuchiya K. Telomere shortening and growth inhibition of human cancer cells by novel synthetic telomerase inhibitors MST-312, MST-295, and MST-1991. Mol Cancer Ther. 2002;1:657–665. [PubMed] [Google Scholar]
- 288.Pascolo E., Wenz C., Lingner J., Hauel N., Priepke H., Kauffmann I. Mechanism of human telomerase inhibition by BIBR1532, a synthetic, non-nucleosidic drug candidate. J Biol Chem. 2002;277:15566–15572. doi: 10.1074/jbc.M201266200. [DOI] [PubMed] [Google Scholar]
- 289.El-Daly H., Kull M., Zimmermann S., Pantic M., Waller C.F., Martens U.M. Selective cytotoxicity and telomere damage in leukemia cells using the telomerase inhibitor BIBR1532. Blood. 2005;105:1742–1749. doi: 10.1182/blood-2003-12-4322. [DOI] [PubMed] [Google Scholar]
- 290.Sengupta S., Peterson T.R., Sabatini D.M. Regulation of the mTOR complex 1 pathway by nutrients, growth factors, and stress. Mol Cell. 2010;40:310–322. doi: 10.1016/j.molcel.2010.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Jiang B.H., Liu L.Z. Role of mTOR in anticancer drug resistance: perspectives for improved drug treatment. Drug Resist Updat. 2008;11:63–76. doi: 10.1016/j.drup.2008.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Bu X., Jia F., Wang W., Guo X., Wu M., Wei L. Coupled down-regulation of mTOR and telomerase activity during fluorouracil-induced apoptosis of hepatocarcinoma cells. BMC Cancer. 2007;7:208. doi: 10.1186/1471-2407-7-208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Sundin T., Peffley D.M., Gauthier D., Hentosh P. The isoprenoid perillyl alcohol inhibits telomerase activity in prostate cancer cells. Biochimie. 2012;94:2639–2648. doi: 10.1016/j.biochi.2012.07.028. [DOI] [PubMed] [Google Scholar]
- 294.Sundin T., Peffley D.M., Hentosh P. Disruption of an hTERT-mTOR-RAPTOR protein complex by a phytochemical perillyl alcohol and rapamycin. Mol Cell Biochem. 2013;375:97–104. doi: 10.1007/s11010-012-1532-3. [DOI] [PubMed] [Google Scholar]
- 295.Zhao Y.M., Zhou Q., Xu Y., Lai X.Y., Huang H. Antiproliferative effect of rapamycin on human T-cell leukemia cell line Jurkat by cell cycle arrest and telomerase inhibition. Acta Pharmacol Sin. 2008;29:481–488. doi: 10.1111/j.1745-7254.2008.00767.x. [DOI] [PubMed] [Google Scholar]
- 296.Zhou C., Gehrig P.A., Whang Y.E., Boggess J.F. Rapamycin inhibits telomerase activity by decreasing the hTERT mRNA level in endometrial cancer cells. Mol Cancer Ther. 2003;2:789–795. [PubMed] [Google Scholar]
- 297.Sundin T., Hentosh P. InTERTesting association between telomerase, mTOR and phytochemicals. Expert Rev Mol Med. 2012;14:e8. doi: 10.1017/erm.2012.1. [DOI] [PubMed] [Google Scholar]
- 298.Filaci G., Fravega M., Setti M., Traverso P., Millo E., Fenoglio D. Frequency of telomerase-specific CD8+ T lymphocytes in patients with cancer. Blood. 2006;107:1505–1512. doi: 10.1182/blood-2005-01-0258. [DOI] [PubMed] [Google Scholar]
- 299.Gannage M., Abel M., Michallet A.S., Delluc S., Lambert M., Giraudier S. Ex vivo characterization of multiepitopic tumor-specific CD8 T cells in patients with chronic myeloid leukemia: implications for vaccine development and adoptive cellular immunotherapy. J Immunol. 2005;174:8210–8218. doi: 10.4049/jimmunol.174.12.8210. [DOI] [PubMed] [Google Scholar]
- 300.Vonderheide R.H., Hahn W.C., Schultze J.L., Nadler L.M. The telomerase catalytic subunit is a widely expressed tumor-associated antigen recognized by cytotoxic T lymphocytes. Immunity. 1999;10:673–679. doi: 10.1016/s1074-7613(00)80066-7. [DOI] [PubMed] [Google Scholar]
- 301.Vonderheide R.H. Telomerase as a universal tumor-associated antigen for cancer immunotherapy. Oncogene. 2002;21:674–679. doi: 10.1038/sj.onc.1205074. [DOI] [PubMed] [Google Scholar]
- 302.Nair S.K., Heiser A., Boczkowski D., Majumdar A., Naoe M., Lebkowski J.S. Induction of cytotoxic T cell responses and tumor immunity against unrelated tumors using telomerase reverse transcriptase RNA transfected dendritic cells. Nat Med. 2000;6:1011–1017. doi: 10.1038/79519. [DOI] [PubMed] [Google Scholar]
- 303.Cortez-Gonzalez X., Zanetti M. Telomerase immunity from bench to bedside: round one. J Transl Med. 2007;5:12. doi: 10.1186/1479-5876-5-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Danet-Desnoyers G.A., Luongo J.L., Bonnet D.A., Domchek S.M., Vonderheide R.H. Telomerase vaccination has no detectable effect on SCID-repopulating and colony-forming activities in the bone marrow of cancer patients. Exp Hematol. 2005;33:1275–1280. doi: 10.1016/j.exphem.2005.07.011. [DOI] [PubMed] [Google Scholar]
- 305.Holysz H., Lipinska N., Paszel-Jaworska A., Rubis B. Telomerase as a useful target in cancer fighting-the breast cancer case. Tumour Biol. 2013;34:1371–1380. doi: 10.1007/s13277-013-0757-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Elson C.E., Peffley D.M., Hentosh P., Mo H. Isoprenoid-mediated inhibition of mevalonate synthesis: potential application to cancer. Proc Soc Exp Biol Med. 1999;221:294–311. doi: 10.1046/j.1525-1373.1999.d01-87.x. [DOI] [PubMed] [Google Scholar]
- 307.Jahangir T., Sultana S. Perillyl alcohol protects against Fe-NTA-induced nephrotoxicity and early tumor promotional events in rat experimental model. Evid Based Complement Alternat Med. 2007;4:439–445. doi: 10.1093/ecam/nel104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Liston B.W., Nines R., Carlton P.S., Gupta A., Aziz R., Frankel W. Perillyl alcohol as a chemopreventive agent in N-nitrosomethylbenzylamine-induced rat esophageal tumorigenesis. Cancer Res. 2003;63:2399–2403. [PubMed] [Google Scholar]
- 309.Chaudhary S.C., Alam M.S., Siddiqui M.S., Athar M. Perillyl alcohol attenuates Ras-ERK signaling to inhibit murine skin inflammation and tumorigenesis. Chem Biol Interact. 2009;179:145–153. doi: 10.1016/j.cbi.2008.12.016. [DOI] [PubMed] [Google Scholar]
- 310.Cho H.Y., Wang W., Jhaveri N., Torres S., Tseng J., Leong M.N. Perillyl alcohol for the treatment of temozolomide-resistant gliomas. Mol Cancer Ther. 2012;11:2462–2472. doi: 10.1158/1535-7163.MCT-12-0321. [DOI] [PubMed] [Google Scholar]
- 311.Farazuddin M., Sharma B., Khan A.A., Joshi B., Owais M. Anticancer efficacy of perillyl alcohol-bearing PLGA microparticles. Int J Nanomed. 2012;7:35–47. doi: 10.2147/IJN.S24920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Lebedeva I.V., Su Z.Z., Vozhilla N., Chatman L., Sarkar D., Dent P. Chemoprevention by perillyl alcohol coupled with viral gene therapy reduces pancreatic cancer pathogenesis. Mol Cancer Ther. 2008;7:2042–2050. doi: 10.1158/1535-7163.MCT-08-0245. [DOI] [PubMed] [Google Scholar]
- 313.Mo H., Elson C.E. Studies of the isoprenoid-mediated inhibition of mevalonate synthesis applied to cancer chemotherapy and chemoprevention. Exp Biol Med (Maywood) 2004;229:567–585. doi: 10.1177/153537020422900701. [DOI] [PubMed] [Google Scholar]
- 314.Peffley D.M., Sharma C., Hentosh P., Buechler R.D. Perillyl alcohol and genistein differentially regulate PKB/Akt and 4E-BP1 phosphorylation as well as eIF4E/eIF4G interactions in human tumor cells. Arch Biochem Biophys. 2007;465:266–273. doi: 10.1016/j.abb.2007.05.022. [DOI] [PubMed] [Google Scholar]
- 315.Jagadeesh S., Kyo S., Banerjee P.P. Genistein represses telomerase activity via both transcriptional and posttranslational mechanisms in human prostate cancer cells. Cancer Res. 2006;66:2107–2115. doi: 10.1158/0008-5472.CAN-05-2494. [DOI] [PubMed] [Google Scholar]
- 316.Ouchi H., Ishiguro H., Ikeda N., Hori M., Kubota Y., Uemura H. Genistein induces cell growth inhibition in prostate cancer through the suppression of telomerase activity. Int J Urol. 2005;12:73–80. doi: 10.1111/j.1442-2042.2004.00973.x. [DOI] [PubMed] [Google Scholar]
- 317.Chau M.N., El Touny L.H., Jagadeesh S., Banerjee P.P. Physiologically achievable concentrations of genistein enhance telomerase activity in prostate cancer cells via the activation of STAT3. Carcinogenesis. 2007;28:2282–2290. doi: 10.1093/carcin/bgm148. [DOI] [PubMed] [Google Scholar]
- 318.Tuntiwechapikul W., Taka T., Songsomboon C., Kaewtunjai N., Imsumran A., Makonkawkeyoon L. Ginger extract inhibits human telomerase reverse transcriptase and c-Myc expression in A549 lung cancer cells. J Med Food. 2010;13:1347–1354. doi: 10.1089/jmf.2010.1191. [DOI] [PubMed] [Google Scholar]
- 319.Khan N., Afaq F., Khusro F.H., Adhami V.M., Suh Y., Mukhtar H. Dual inhibition of PI3K/AKT and mTOR signaling in human non-small cell lung cancer cells by a dietary flavonoid fisetin. Int J Cancer. 2011;130:1695–1705. doi: 10.1002/ijc.26178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Syed D.N., Adhami V.M., Khan M.I., Mukhtar H. Inhibition of Akt/mTOR signaling by the dietary flavonoid fisetin. Anticancer Agents Med Chem. 2012;13:995–1001. doi: 10.2174/18715206113139990129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Seguin J., Brulle L., Boyer R., Lu Y.M., Ramos Romano M., Touil Y.S. Liposomal encapsulation of the natural flavonoid fisetin improves bioavailability and antitumor efficacy. Int J Pharm, 2013;444:146–154. doi: 10.1016/j.ijpharm.2013.01.050. [DOI] [PubMed] [Google Scholar]
- 322.Khaw A.K., Hande M.P., Kalthur G. Curcumin inhibits telomerase and induces telomere shortening and apoptosis in brain tumour cells. J Cell Biochem. 2012;114:1257–1270. doi: 10.1002/jcb.24466. [DOI] [PubMed] [Google Scholar]
- 323.Mukherjee Nee Chakraborty S., Ghosh U., Bhattacharyya N.P., Bhattacharya R.K., Dey S., Roy M. Curcumin-induced apoptosis in human leukemia cell HL-60 is associated with inhibition of telomerase activity. Mol Cell Biochem. 2007;297:31–39. doi: 10.1007/s11010-006-9319-z. [DOI] [PubMed] [Google Scholar]
- 324.Singh M., Singh N. Molecular mechanism of curcumin induced cytotoxicity in human cervical carcinoma cells. Mol Cell Biochem. 2009;325:107–119. doi: 10.1007/s11010-009-0025-5. [DOI] [PubMed] [Google Scholar]
- 325.Lee J.H., Chung I.K. Curcumin inhibits nuclear localization of telomerase by dissociating the Hsp90 co-chaperone p23 from hTERT. Cancer Lett. 2010;290:76–86. doi: 10.1016/j.canlet.2009.08.026. [DOI] [PubMed] [Google Scholar]
- 326.Beevers C.S., Chen L., Liu L., Luo Y., Webster N.J., Huang S. Curcumin disrupts the mammalian target of rapamycin–raptor complex. Cancer Res. 2009;69:1000–1008. doi: 10.1158/0008-5472.CAN-08-2367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Chakravarti N., Kadara H., Yoon D.J., Shay J.W., Myers J.N., Lotan D. Differential inhibition of protein translation machinery by curcumin in normal, immortalized, and malignant oral epithelial cells. Cancer Prev Res (Phila) 2010;3:331–338. doi: 10.1158/1940-6207.CAPR-09-0076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Shehzad A., Lee Y.S. Molecular mechanisms of curcumin action: signal transduction. Biofactors. 2013;39:27–36. doi: 10.1002/biof.1065. [DOI] [PubMed] [Google Scholar]
- 329.Hasima N., Aggarwal B.B. Cancer-linked targets modulated by curcumin. Int J Biochem Mol Biol. 2012;3:328–351. [PMC free article] [PubMed] [Google Scholar]
- 330.Ramachandran C., Fonseca H.B., Jhabvala P., Escalon E.A., Melnick S.J. Curcumin inhibits telomerase activity through human telomerase reverse transcritpase in MCF-7 breast cancer cell line. Cancer Lett. 2002;184:1–6. doi: 10.1016/s0304-3835(02)00192-1. [DOI] [PubMed] [Google Scholar]
- 331.Hsin I.L., Sheu G.T., Chen H.H., Chiu L.Y., Wang H.D., Chan H.W. N-acetyl cysteine mitigates curcumin-mediated telomerase inhibition through rescuing of Sp1 reduction in A549 cells. Mutat Res. 2010;688:72–77. doi: 10.1016/j.mrfmmm.2010.03.011. [DOI] [PubMed] [Google Scholar]
- 332.Fuggetta M.P., Lanzilli G., Tricarico M., Cottarelli A., Falchetti R., Ravagnan G. Effect of resveratrol on proliferation and telomerase activity of human colon cancer cells in vitro. J Exp Clin Cancer Res. 2006;25:189–193. [PubMed] [Google Scholar]
- 333.Lanzilli G., Fuggetta M.P., Tricarico M., Cottarelli A., Serafino A., Falchetti R. Resveratrol down-regulates the growth and telomerase activity of breast cancer cells in vitro. Int J Oncol. 2006;28:641–648. [PubMed] [Google Scholar]
- 334.Narayanan N.K., Nargi D., Randolph C., Narayanan B.A. Liposome encapsulation of curcumin and resveratrol in combination reduces prostate cancer incidence in PTEN knockout mice. Int J Cancer. 2009;125:1–8. doi: 10.1002/ijc.24336. [DOI] [PubMed] [Google Scholar]
- 335.Singh B.N., Shankar S., Srivastava R.K. Green tea catechin, epigallocatechin-3-gallate (EGCG): mechanisms, perspectives and clinical applications. Biochem Pharmacol. 2011;82:1807–1821. doi: 10.1016/j.bcp.2011.07.093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336.Lin S.C., Li W.C., Shih J.W., Hong K.F., Pan Y.R., Lin J.J. The tea polyphenols EGCG and EGC repress mRNA expression of human telomerase reverse transcriptase (hTERT) in carcinoma cells. Cancer Lett. 2006;236:80–88. doi: 10.1016/j.canlet.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 337.Meeran S.M., Patel S.N., Chan T.H., Tollefsbol T.O. A novel prodrug of epigallocatechin-3-gallate: differential epigenetic hTERT repression in human breast cancer cells. Cancer Prev Res (Phila) 2011;4:1243–1254. doi: 10.1158/1940-6207.CAPR-11-0009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Naasani I., Oh-Hashi F., Oh-Hara T., Feng W.Y., Johnston J., Chan K. Blocking telomerase by dietary polyphenols is a major mechanism for limiting the growth of human cancer cells in vitro and in vivo. Cancer Res. 2003;63:824–830. [PubMed] [Google Scholar]
- 339.Wang X., Hao M.W., Dong K., Lin F., Ren J.H., Zhang H.Z. Apoptosis induction effects of EGCG in laryngeal squamous cell carcinoma cells through telomerase repression. Arch Pharm Res. 2009;32:1263–1269. doi: 10.1007/s12272-009-1912-8. [DOI] [PubMed] [Google Scholar]
- 340.Marconett C.N., Sundar S.N., Tseng M., Tin A.S., Tran K.Q., Mahuron K.M. Indole-3-carbinol downregulation of telomerase gene expression requires the inhibition of estrogen receptor-alpha and Sp1 transcription factor interactions within the hTERT promoter and mediates the G1 cell cycle arrest of human breast cancer cells. Carcinogenesis. 2011;32:1315–1323. doi: 10.1093/carcin/bgr116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Moon D.O., Kang S.H., Kim K.C., Kim M.O., Choi Y.H., Kim G.Y. Sulforaphane decreases viability and telomerase activity in hepatocellular carcinoma Hep3B cells through the reactive oxygen species-dependent pathway. Cancer Lett. 2010;295:260–266. doi: 10.1016/j.canlet.2010.03.009. [DOI] [PubMed] [Google Scholar]
- 342.Warabi K., Hamada T., Nakao Y., Matsunaga S., Hirota H., van Soest R.W. Axinelloside A, an unprecedented highly sulfated lipopolysaccharide inhibiting telomerase, from the marine sponge, Axinella infundibula. J Am Chem Soc. 2005;127:13262–13270. doi: 10.1021/ja052688r. [DOI] [PubMed] [Google Scholar]
- 343.Tauchi T., Shin-ya K., Sashida G., Sumi M., Okabe S., Ohyashiki J.H. Telomerase inhibition with a novel G-quadruplex-interactive agent, telomestatin: in vitro and in vivo studies in acute leukemia. Oncogene. 2006;25:5719–5725. doi: 10.1038/sj.onc.1209577. [DOI] [PubMed] [Google Scholar]
- 344.Tauchi T., Shin-Ya K., Sashida G., Sumi M., Nakajima A., Shimamoto T. Activity of a novel G-quadruplex-interactive telomerase inhibitor, telomestatin (SOT-095), against human leukemia cells: involvement of ATM-dependent DNA damage response pathways. Oncogene. 2003;22:5338–5347. doi: 10.1038/sj.onc.1206833. [DOI] [PubMed] [Google Scholar]
- 345.Kim M.Y., Vankayalapati H., Shin-Ya K., Wierzba K., Hurley L.H. Telomestatin, a potent telomerase inhibitor that interacts quite specifically with the human telomeric intramolecular g-quadruplex. J Am Chem Soc. 2002;124:2098–2099. doi: 10.1021/ja017308q. [DOI] [PubMed] [Google Scholar]
- 346.Binz N., Shalaby T., Rivera P., Shin-ya K., Grotzer M.A. Telomerase inhibition, telomere shortening, cell growth suppression and induction of apoptosis by telomestatin in childhood neuroblastoma cells. Eur J Cancer. 2005;41:2873–2881. doi: 10.1016/j.ejca.2005.08.025. [DOI] [PubMed] [Google Scholar]
- 347.Deeley J., Bertram A., Pattenden G. Novel polyoxazole-based cyclopeptides from Streptomyces sp. total synthesis of the cyclopeptide YM-216391 and synthetic studies towards telomestatin. Org Biomol Chem. 2008;6:1994–2010. doi: 10.1039/b802477d. [DOI] [PubMed] [Google Scholar]
- 348.Doi T., Yoshida M., Shin-ya K., Takahashi T. Total synthesis of (R)-telomestatin. Org Lett. 2006;8:4165–4167. doi: 10.1021/ol061793i. [DOI] [PubMed] [Google Scholar]
- 349.Seimiya H., Muramatsu Y., Ohishi T., Tsuruo T. Tankyrase 1 as a target for telomere-directed molecular cancer therapeutics. Cancer Cell. 2005;7:25–37. doi: 10.1016/j.ccr.2004.11.021. [DOI] [PubMed] [Google Scholar]
- 350.Smith S., Giriat I., Schmitt A., de Lange T. Tankyrase, a poly(ADP-ribose) polymerase at human telomeres. Science. 1998;282:1484–1487. doi: 10.1126/science.282.5393.1484. [see comments] [DOI] [PubMed] [Google Scholar]
- 351.Huang S.M., Mishina Y.M., Liu S., Cheung A., Stegmeier F., Michaud G.A. Tankyrase inhibition stabilizes axin and antagonizes Wnt signalling. Nature. 2009;461:614–620. doi: 10.1038/nature08356. [DOI] [PubMed] [Google Scholar]
- 352.Zahler A.M., Williamson J.R., Cech T.R., Prescott D.M. Inhibition of telomerase by G-quartet DNA structures. Nature. 1991;350:718–720. doi: 10.1038/350718a0. [DOI] [PubMed] [Google Scholar]
- 353.Tang J., Kan Z.Y., Yao Y., Wang Q., Hao Y.H., Tan Z. G-quadruplex preferentially forms at the very 3′ end of vertebrate telomeric DNA. Nucleic Acids Res. 2008;36:1200–1208. doi: 10.1093/nar/gkm1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 354.Mergny J.L., Lacroix L., Teulade-Fichou M.P., Hounsou C., Guittat L., Hoarau M. Telomerase inhibitors based on quadruplex ligands selected by a fluorescence assay. Proc Natl Acad Sci U S A. 2001;98:3062–3067. doi: 10.1073/pnas.051620698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355.Izbicka E., Nishioka D., Marcell V., Raymond E., Davidson K.K., Lawrence R.A. Telomere-interactive agents affect proliferation rates and induce chromosomal destabilization in sea urchin embryos. Anticancer Drug Des. 1999;14:355–365. [PubMed] [Google Scholar]
- 356.Gowan S.M., Harrison J.R., Patterson L., Valenti M., Read M.A., Neidle S. A G-quadruplex-interactive potent small-molecule inhibitor of telomerase exhibiting in vitro and in vivo antitumor activity. Mol Pharmacol. 2002;61:1154–1162. doi: 10.1124/mol.61.5.1154. [DOI] [PubMed] [Google Scholar]
- 357.Shin-ya K., Wierzba K., Matsuo K., Ohtani T., Yamada Y., Furihata K. Telomestatin, a novel telomerase inhibitor from Streptomyces anulatus. J Am Chem Soc. 2001;123:1262–1263. doi: 10.1021/ja005780q. [DOI] [PubMed] [Google Scholar]
- 358.Gowan S.M., Heald R., Stevens M.F., Kelland L.R. Potent inhibition of telomerase by small-molecule pentacyclic acridines capable of interacting with G-quadruplexes. Mol Pharmacol. 2001;60:981–988. doi: 10.1124/mol.60.5.981. [DOI] [PubMed] [Google Scholar]
- 359.Cookson J.C., Dai F., Smith V., Heald R.A., Laughton C.A., Stevens M.F. Pharmacodynamics of the G-quadruplex-stabilizing telomerase inhibitor 3,11-difluoro-6,8,13-trimethyl-8H-quino[4,3,2-kl]acridinium methosulfate (RHPS4) in vitro: activity in human tumor cells correlates with telomere length and can be enhanced, or antagonized, with cytotoxic agents. Mol Pharmacol. 2005;68:1551–1558. doi: 10.1124/mol.105.013300. [DOI] [PubMed] [Google Scholar]
- 360.Shammas M.A., Shmookler Reis R.J., Li C., Koley H., Hurley L.H., Anderson K.C. Telomerase inhibition and cell growth arrest after telomestatin treatment in multiple myeloma. Clin Cancer Res. 2004;10:770–776. doi: 10.1158/1078-0432.ccr-0793-03. [DOI] [PubMed] [Google Scholar]
- 361.Sumi M., Tauchi T., Sashida G., Nakajima A., Gotoh A., Shin-Ya K. A G-quadruplex-interactive agent, telomestatin (SOT-095), induces telomere shortening with apoptosis and enhances chemosensitivity in acute myeloid leukemia. Int J Oncol. 2004;24:1481–1487. [PubMed] [Google Scholar]
- 362.Chen Y., Dokmanovic M., Stein W.D., Ardecky R.J., Roninson I.B. Agonist and antagonist of retinoic acid receptors cause similar changes in gene expression and induce senescence-like growth arrest in MCF-7 breast carcinoma cells. Cancer Res. 2006;66:8749–8761. doi: 10.1158/0008-5472.CAN-06-0581. [DOI] [PubMed] [Google Scholar]
- 363.Moreno-Aspitia A., Perez E.A. Anthracycline- and/or taxane-resistant breast cancer: results of a literature review to determine the clinical challenges and current treatment trends. Clin Ther. 2009;31:1619–1640. doi: 10.1016/j.clinthera.2009.08.005. [DOI] [PubMed] [Google Scholar]
- 364.Varna M., Lehmann-Che J., Turpin E., Marangoni E., El-Bouchtaoui M., Jeanne M. p53 dependent cell-cycle arrest triggered by chemotherapy in xenografted breast tumors. Int J Cancer. 2009;124:991–997. doi: 10.1002/ijc.24049. [DOI] [PubMed] [Google Scholar]
- 365.Cairney C.J., Bilsland A.E., Evans T.R., Roffey J., Bennett D.C., Narita M. Cancer cell senescence: a new frontier in drug development. Drug Discov Today. 2012;17:269–276. doi: 10.1016/j.drudis.2012.01.019. [DOI] [PubMed] [Google Scholar]
- 366.Lahtela J., Corson L.B., Hemmes A., Brauer M.J., Koopal S., Lee J. A high-content cellular senescence screen identifies candidate tumor suppressors, including EPHA3. Cell Cycle. 2013;12:625–634. doi: 10.4161/cc.23515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 367.Ewald J.A., Peters N., Desotelle J.A., Hoffmann F.M., Jarrard D.F. A high-throughput method to identify novel senescence-inducing compounds. J Biomol Screen. 2009;14:853–858. doi: 10.1177/1087057109340314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 368.Samaila D., Toy B.J., Wang R.C., Elegbede J.A. Monoterpenes enhanced the sensitivity of head and neck cancer cells to radiation treatment in vitro. Anticancer Res. 2004;24:3089–3095. [PubMed] [Google Scholar]
- 369.da Fonseca C.O., Schwartsmann G., Fischer J., Nagel J., Futuro D., Quirico-Santos T. Preliminary results from a phase I/II study of perillyl alcohol intranasal administration in adults with recurrent malignant gliomas. Surg Neurol. 2008;70:259–266. doi: 10.1016/j.surneu.2007.07.040. discussion 66–7. [DOI] [PubMed] [Google Scholar]
- 370.da Fonseca C.O., Simao M., Lins I.R., Caetano R.O., Futuro D., Quirico-Santos T. Efficacy of monoterpene perillyl alcohol upon survival rate of patients with recurrent glioblastoma. J Cancer Res Clin Oncol. 2011;137:287–293. doi: 10.1007/s00432-010-0873-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 371.Morgan-Meadows S., Dubey S., Gould M., Tutsch K., Marnocha R., Arzoomanin R. Phase I trial of perillyl alcohol administered four times daily continuously. Cancer Chemother Pharmacol. 2003;52:361–366. doi: 10.1007/s00280-003-0684-y. [DOI] [PubMed] [Google Scholar]
- 372.Stratton S.P., Alberts D.S., Einspahr J.G., Sagerman P.M., Warneke J.A., Curiel-Lewandrowski C. A phase 2a study of topical perillyl alcohol cream for chemoprevention of skin cancer. Cancer Prev Res (Phila) 2010;3:160–169. doi: 10.1158/1940-6207.CAPR-09-0183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 373.Aoki H., Takada Y., Kondo S., Sawaya R., Aggarwal B.B., Kondo Y. Evidence that curcumin suppresses the growth of malignant gliomas in vitro and in vivo through induction of autophagy: role of Akt and extracellular signal-regulated kinase signaling pathways. Mol Pharmacol. 2007;72:29–39. doi: 10.1124/mol.106.033167. [DOI] [PubMed] [Google Scholar]
- 374.Phillips J.M., Clark C., Herman-Ferdinandez L., Moore-Medlin T., Rong X., Gill J.R. Curcumin inhibits skin squamous cell carcinoma tumor growth in vivo. Otolaryngol Head Neck Surg. 2011;145:58–63. doi: 10.1177/0194599811400711. [DOI] [PubMed] [Google Scholar]
- 375.Royt M., Mukherjee S., Sarkar R., Biswas J. Curcumin sensitizes chemotherapeutic drugs via modulation of PKC, telomerase, NF-kappaB and HDAC in breast cancer. Ther Deliv. 2011;2:1275–1293. doi: 10.4155/tde.11.97. [DOI] [PubMed] [Google Scholar]
- 376.Seo J.H., Jeong K.J., Oh W.J., Sul H.J., Sohn J.S., Kim Y.K. Lysophosphatidic acid induces STAT3 phosphorylation and ovarian cancer cell motility: their inhibition by curcumin. Cancer Lett. 2010;288:50–56. doi: 10.1016/j.canlet.2009.06.023. [DOI] [PubMed] [Google Scholar]
- 377.Bayet-Robert M., Kwiatkowski F., Leheurteur M., Gachon F., Planchat E., Abrial C. Phase I dose escalation trial of docetaxel plus curcumin in patients with advanced and metastatic breast cancer. Cancer Biol Ther. 2010;9:8–14. doi: 10.4161/cbt.9.1.10392. [DOI] [PubMed] [Google Scholar]
- 378.Carroll R.E., Benya R.V., Turgeon D.K., Vareed S., Neuman M., Rodriguez L. Phase IIa clinical trial of curcumin for the prevention of colorectal neoplasia. Cancer Prev Res (Phila) 2011;4:354–364. doi: 10.1158/1940-6207.CAPR-10-0098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 379.Dhillon N., Aggarwal B.B., Newman R.A., Wolff R.A., Kunnumakkara A.B., Abbruzzese J.L. Phase II trial of curcumin in patients with advanced pancreatic cancer. Clin Cancer Res. 2008;14:4491–4499. doi: 10.1158/1078-0432.CCR-08-0024. [DOI] [PubMed] [Google Scholar]
- 380.Kanai M., Yoshimura K., Asada M., Imaizumi A., Suzuki C., Matsumoto S. A phase I/II study of gemcitabine-based chemotherapy plus curcumin for patients with gemcitabine-resistant pancreatic cancer. Cancer Chemother Pharmacol. 2011;68:157–164. doi: 10.1007/s00280-010-1470-2. [DOI] [PubMed] [Google Scholar]
- 381.Leontieva O.V., Paszkiewicz G., Demidenko Z.N., Blagosklonny M.V. Resveratrol potentiates rapamycin to prevent hyperinsulinemia and obesity in male mice on high fat diet. Cell Death Dis. 2013;4:e472. doi: 10.1038/cddis.2012.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 382.Um H.J., Bae J.H., Park J.W., Suh H., Jeong N.Y., Yoo Y.H. Differential effects of resveratrol and novel resveratrol derivative, HS-1793, on endoplasmic reticulum stress-mediated apoptosis and Akt inactivation. Int J Oncol. 2010;36:1007–1013. doi: 10.3892/ijo_00000581. [DOI] [PubMed] [Google Scholar]
- 383.Colin D., Limagne E., Jeanningros S., Jacquel A., Lizard G., Athias A. Endocytosis of resveratrol via lipid rafts and activation of downstream signaling pathways in cancer cells. Cancer Prev Res (Phila) 2011;4:1095–1106. doi: 10.1158/1940-6207.CAPR-10-0274. [DOI] [PubMed] [Google Scholar]
- 384.Juan M.E., Alfaras I., Planas J.M. Colorectal cancer chemoprevention by trans-resveratrol. Pharmacol Res. 2012;65:584–591. doi: 10.1016/j.phrs.2012.03.010. [DOI] [PubMed] [Google Scholar]
- 385.Cottart C.H., Nivet-Antoine V., Laguillier-Morizot C., Beaudeux J.L. Resveratrol bioavailability and toxicity in humans. Mol Nutr Food Res. 2010;54:7–16. doi: 10.1002/mnfr.200900437. [DOI] [PubMed] [Google Scholar]
- 386.Nguyen A.V., Martinez M., Stamos M.J., Moyer M.P., Planutis K., Hope C. Results of a phase I pilot clinical trial examining the effect of plant-derived resveratrol and grape powder on Wnt pathway target gene expression in colonic mucosa and colon cancer. Cancer Manag Res. 2009;1:25–37. [PMC free article] [PubMed] [Google Scholar]
- 387.Patel K.R., Brown V.A., Jones D.J., Britton R.G., Hemingway D., Miller A.S. Clinical pharmacology of resveratrol and its metabolites in colorectal cancer patients. Cancer Res. 2010;70:7392–7399. doi: 10.1158/0008-5472.CAN-10-2027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 388.Van Aller G.S., Carson J.D., Tang W., Peng H., Zhao L., Copeland R.A. Epigallocatechin gallate (EGCG), a major component of green tea, is a dual phosphoinositide-3-kinase/mTOR inhibitor. Biochem Biophys Res Commun. 2011;406:194–199. doi: 10.1016/j.bbrc.2011.02.010. [DOI] [PubMed] [Google Scholar]
- 389.Gupta S., Hastak K., Afaq F., Ahmad N., Mukhtar H. Essential role of caspases in epigallocatechin-3-gallate-mediated inhibition of nuclear factor kappa B and induction of apoptosis. Oncogene. 2004;23:2507–2522. doi: 10.1038/sj.onc.1207353. [DOI] [PubMed] [Google Scholar]
- 390.Tang S.N., Fu J., Shankar S., Srivastava R.K. EGCG enhances the therapeutic potential of gemcitabine and CP690550 by inhibiting STAT3 signaling pathway in human pancreatic cancer. PLoS ONE. 2012;7:e31067. doi: 10.1371/journal.pone.0031067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 391.Khan N., Afaq F., Saleem M., Ahmad N., Mukhtar H. Targeting multiple signaling pathways by green tea polyphenol (−)-epigallocatechin-3-gallate. Cancer Res. 2006;66:2500–2505. doi: 10.1158/0008-5472.CAN-05-3636. [DOI] [PubMed] [Google Scholar]
- 392.McLarty J., Bigelow R.L., Smith M., Elmajian D., Ankem M., Cardelli J.A. Tea polyphenols decrease serum levels of prostate-specific antigen, hepatocyte growth factor, and vascular endothelial growth factor in prostate cancer patients and inhibit production of hepatocyte growth factor and vascular endothelial growth factor in vitro. Cancer Prev Res (Phila) 2009;2:673–682. doi: 10.1158/1940-6207.CAPR-08-0167. [DOI] [PubMed] [Google Scholar]
- 393.Zou C., Liu H., Feugang J.M., Hao Z., Chow H.H., Garcia F. Green tea compound in chemoprevention of cervical cancer. Int J Gynecol Cancer. 2010;20:617–624. doi: 10.1111/IGC.0b013e3181c7ca5c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 394.Wu H., Xin Y., Xu C., Xiao Y. Capecitabine combined with (−)-epigallocatechin-3-gallate inhibits angiogenesis and tumor growth in nude mice with gastric cancer xenografts. Exp Ther Med. 2012;3:650–654. doi: 10.3892/etm.2012.448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 395.Bettuzzi S., Brausi M., Rizzi F., Castagnetti G., Peracchia G., Corti A. Chemoprevention of human prostate cancer by oral administration of green tea catechins in volunteers with high-grade prostate intraepithelial neoplasia: a preliminary report from a one-year proof-of-principle study. Cancer Res. 2006;66:1234–1240. doi: 10.1158/0008-5472.CAN-05-1145. [DOI] [PubMed] [Google Scholar]
- 396.Shanafelt T.D., Call T.G., Zent C.S., LaPlant B., Bowen D.A., Roos M. Phase I trial of daily oral polyphenon E in patients with asymptomatic Rai stage 0 to II chronic lymphocytic leukemia. J Clin Oncol. 2009;27:3808–3814. doi: 10.1200/JCO.2008.21.1284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 397.Shanafelt T.D., Call T.G., Zent C.S., Leis J.F., Laplant B., Bowen D.A. Phase 2 trial of daily, oral polyphenon E in patients with asymptomatic, Rai stage 0 to II chronic lymphocytic leukemia. Chemioterapia. 2013;119:363–370. doi: 10.1002/cncr.27719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 398.Peffley D., Hentosh P. Plant-derived isoprenoids mediate regulation of mTOR signaling in tumor cells. In: Diederich M., editor. Natural compounds as inducers of cell death. Springer Publishing; 2012. [Google Scholar]
- 399.Lazarevic B., Boezelijn G., Diep L.M., Kvernrod K., Ogren O., Ramberg H. Efficacy and safety of short-term genistein intervention in patients with localized prostate cancer prior to radical prostatectomy: a randomized, placebo-controlled, double-blind Phase 2 clinical trial. Nutr Cancer. 2011;63:889–898. doi: 10.1080/01635581.2011.582221. [DOI] [PubMed] [Google Scholar]
- 400.Roger L., Jones R.E., Heppel N.H., Williams G.T., Sampson J.R., Baird D.M. Extensive telomere erosion in the initiation of colorectal adenomas and its association with chromosomal instability. J Natl Cancer Inst. 2013;105:1202–1211. doi: 10.1093/jnci/djt191. [DOI] [PubMed] [Google Scholar]
- 401.Chou W.C., Hawkins A.L., Barrett J.F., Griffin C.A., Dang C.V. Arsenic inhibition of telomerase transcription leads to genetic instability. J Clin Investig. 2001;108:1541–1547. doi: 10.1172/JCI14064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 402.Lu R., Pal J., Buon L., Nanjappa P., Shi J., Fulciniti M. Targeting homologous recombination and telomerase in Barrett's adenocarcinoma: impact on telomere maintenance, genomic instability and tumor growth. Oncogene. 2014;33:1495–1505. doi: 10.1038/onc.2013.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 403.Lu Y., Wu Y., Feng X., Shen R., Wang J.H., Fallahi M. CDK4 deficiency promotes genomic instability and enhances Myc-driven lymphomagenesis. J Clin Investig. 2014;124:1672–1684. doi: 10.1172/JCI63139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 404.Hughes B.T., Sidorova J., Swanger J., Monnat R.J., Jr., Clurman B.E. Essential role for Cdk2 inhibitory phosphorylation during replication stress revealed by a human Cdk2 knockin mutation. Proc Natl Acad Sci U S A. 2013;110:8954–8959. doi: 10.1073/pnas.1302927110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 405.Ma Y., Yuan X., Wyatt W.R., Pomerening J.R. Expression of constitutively active CDK1 stabilizes APC-Cdh1 substrates and potentiates premature spindle assembly and checkpoint function in G1 cells. PLoS ONE. 2012;7:e33835. doi: 10.1371/journal.pone.0033835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 406.Xu N., Hegarat N., Black E.J., Scott M.T., Hochegger H., Gillespie D.A. Akt/PKB suppresses DNA damage processing and checkpoint activation in late G2. J Cell Biol. 2010;190:297–305. doi: 10.1083/jcb.201003004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 407.Nelson A.C., Lyons T.R., Young C.D., Hansen K.C., Anderson S.M., Holt J.T. AKT regulates BRCA1 stability in response to hormone signaling. Mol Cell Endocrinol. 2010;319:129–142. doi: 10.1016/j.mce.2010.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 408.Plo I., Lopez B. AKT1 represses gene conversion induced by different genotoxic stresses and induces supernumerary centrosomes and aneuploidy in hamster ovary cells. Oncogene. 2009;28:2231–2237. doi: 10.1038/onc.2009.85. [DOI] [PubMed] [Google Scholar]
- 409.Nam H.J., Chae S., Jang S.H., Cho H., Lee J.H. The PI3K-Akt mediates oncogenic Met-induced centrosome amplification and chromosome instability. Carcinogenesis. 2010;31:1531–1540. doi: 10.1093/carcin/bgq133. [DOI] [PubMed] [Google Scholar]
- 410.Ghosh A., Saginc G., Leow S.C., Khattar E., Shin E.M., Yan T.D. Telomerase directly regulates NF-kappaB-dependent transcription. Nat Cell Biol. 2012;14:1270–1281. doi: 10.1038/ncb2621. [DOI] [PubMed] [Google Scholar]
- 411.Beck S., Jin X., Sohn Y.W., Kim J.K., Kim S.H., Yin J. Telomerase activity-independent function of TERT allows glioma cells to attain cancer stem cell characteristics by inducing EGFR expression. Mol Cells. 2011;31:9–15. doi: 10.1007/s10059-011-0008-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 412.Jiang Y., Chen C., Chen S.M., Wang Y.Q., Xu Y., Wang Y. Telomerase reverse transcriptase promotes the proliferation of human laryngeal carcinoma cells through activation of the activator protein 1. Oncol Lett. 2013;6:75–80. doi: 10.3892/ol.2013.1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 413.Kraemer K., Schmidt U., Fuessel S., Herr A., Wirth M.P., Meye A. Microarray analyses in bladder cancer cells: inhibition of hTERT expression down-regulates EGFR. Int J Cancer. 2006;119:1276–1284. doi: 10.1002/ijc.21975. [DOI] [PubMed] [Google Scholar]
- 414.Dong S., Zhang X.C., Cheng H., Zhu J.Q., Chen Z.H., Zhang Y.F. Everolimus synergizes with gefitinib in non-small-cell lung cancer cell lines resistant to epidermal growth factor receptor tyrosine kinase inhibitors. Cancer Chemother Pharmacol. 2012;70:707–716. doi: 10.1007/s00280-012-1946-3. [DOI] [PubMed] [Google Scholar]
- 415.Grabinski N., Ewald F., Hofmann B.T., Staufer K., Schumacher U., Nashan B. Combined targeting of AKT and mTOR synergistically inhibits proliferation of hepatocellular carcinoma cells. Mol Cancer. 2012;11:85. doi: 10.1186/1476-4598-11-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 416.Hou X., Zhao M., Wang T., Zhang G. Upregulation of estrogen receptor mediates migration, invasion and proliferation of endometrial carcinoma cells by regulating the PI3K/AKT/mTOR pathway. Oncol Rep. 2014;31:1175–1182. doi: 10.3892/or.2013.2944. [DOI] [PubMed] [Google Scholar]
- 417.Mao C.Q., Xiong M.H., Liu Y., Shen S., Du X.J., Yang X.Z. Synthetic lethal therapy for KRAS mutant non-small-cell lung carcinoma with nanoparticle-mediated CDK4 siRNA delivery. Mol Ther J Am Soc Gene Ther. 2014;22:964–973. doi: 10.1038/mt.2014.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 418.Witkiewicz A.K., Cox D.W., Rivadeneira D., Ertel A.E., Fortina P., Schwartz G.F. The retinoblastoma tumor suppressor pathway modulates the invasiveness of ErbB2-positive breast cancer. Oncogene. 2013;33:3980–3991. doi: 10.1038/onc.2013.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 419.Rea K., Sensi M., Anichini A., Canevari S., Tomassetti A. EGFR/MEK/ERK/CDK5-dependent integrin-independent FAK phosphorylated on serine 732 contributes to microtubule depolymerization and mitosis in tumor cells. Cell Death Dis. 2013;4:e815. doi: 10.1038/cddis.2013.353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 420.Xie W., Wang H., He Y., Li D., Gong L., Zhang Y. CDK5 and its activator P35 in normal pituitary and in pituitary adenomas: relationship to VEGF expression. Int J Biol Sci. 2014;10:192–199. doi: 10.7150/ijbs.7770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 421.Held J.M., Britton D.J., Scott G.K., Lee E.L., Schilling B., Baldwin M.A. Ligand binding promotes CDK-dependent phosphorylation of ER-alpha on hinge serine 294 but inhibits ligand-independent phosphorylation of serine 305. Mol Cancer Res. 2012;10:1120–1132. doi: 10.1158/1541-7786.MCR-12-0099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 422.Kunter I., Erdal E., Nart D., Yilmaz F., Karademir S., Sagol O. Active form of AKT controls cell proliferation and response to apoptosis in hepatocellular carcinoma. Oncol Rep. 2014;31:573–580. doi: 10.3892/or.2013.2932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 423.He Z., Deng Y., Li W., Chen Y., Xing S., Zhao X. Overexpression of PTEN suppresses lipopolysaccharide-induced lung fibroblast proliferation, differentiation and collagen secretion through inhibition of the PI3-K-Akt-GSK3beta pathway. Cell Biosci. 2014;4:2. doi: 10.1186/2045-3701-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 424.Chen X., Qin Q., Zhang W., Zhang Y., Zheng H., Liu C. Activation of the PI3K-AKT-mTOR signaling pathway promotes DEHP-induced Hep3B cell proliferation. Food Chem Toxicol. 2013;59:325–333. doi: 10.1016/j.fct.2013.06.016. [DOI] [PubMed] [Google Scholar]
- 425.Bodo J., Zhao X., Sharma A., Hill B.T., Portell C.A., Lannutti B.J. The phosphatidylinositol 3-kinases (PI3K) inhibitor GS-1101 synergistically potentiates histone deacetylase inhibitor-induced proliferation inhibition and apoptosis through the inactivation of PI3K and extracellular signal-regulated kinase pathways. Br J Haematol. 2013;163:72–80. doi: 10.1111/bjh.12498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 426.Garbers C., Kuck F., Aparicio-Siegmund S., Konzak K., Kessenbrock M., Sommerfeld A. Cellular senescence or EGFR signaling induces Interleukin 6 (IL-6) receptor expression controlled by mammalian target of rapamycin (mTOR) Cell Cycle. 2013;12:3421–3432. doi: 10.4161/cc.26431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 427.Yuan H., Lu J., Xiao J., Upadhyay G., Umans R., Kallakury B. PPARdelta induces estrogen receptor-positive mammary neoplasia through an inflammatory and metabolic phenotype linked to mTOR activation. Cancer Res. 2013;73:4349–4361. doi: 10.1158/0008-5472.CAN-13-0322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 428.Handschick K., Beuerlein K., Jurida L., Bartkuhn M., Muller H., Soelch J. Cyclin-dependent kinase 6 is a chromatin-bound cofactor for NF-kappaB-dependent gene expression. Mol Cell. 2014;53:193–208. doi: 10.1016/j.molcel.2013.12.002. [DOI] [PubMed] [Google Scholar]
- 429.Du J., Wei N., Guan T., Xu H., An J., Pritchard K.A., Jr. Inhibition of CDKS by roscovitine suppressed LPS-induced *NO production through inhibiting NFkappaB activation and BH4 biosynthesis in macrophages. Am J Physiol Cell Physiol. 2009;297:C742–C749. doi: 10.1152/ajpcell.00138.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 430.Berberich N., Uhl B., Joore J., Schmerwitz U.K., Mayer B.A., Reichel C.A. Roscovitine blocks leukocyte extravasation by inhibition of cyclin-dependent kinases 5 and 9. Br J Pharmacol. 2011;163:1086–1098. doi: 10.1111/j.1476-5381.2011.01309.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 431.Dong Y.L., Kabir S.M., Lee E.S., Son D.S. CXCR2-driven ovarian cancer progression involves upregulation of proinflammatory chemokines by potentiating NF-kappaB activation via EGFR-transactivated Akt signaling. PLOS ONE. 2013;8:e83789. doi: 10.1371/journal.pone.0083789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 432.Smith D.A., Kiba A., Zong Y., Witte O.N. Interleukin-6 and oncostatin-M synergize with the PI3K/AKT pathway to promote aggressive prostate malignancy in mouse and human tissues. Mol Cancer Res. 2013;11:1159–1165. doi: 10.1158/1541-7786.MCR-13-0238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 433.Wang Y., Wang W., Wang L., Wang X., Xia J. Regulatory mechanisms of interleukin-8 production induced by tumour necrosis factor-alpha in human hepatocellular carcinoma cells. J Cell Mol Med. 2012;16:496–506. doi: 10.1111/j.1582-4934.2011.01337.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 434.Zhang Y., Wang L., Zhang M., Jin M., Bai C., Wang X. Potential mechanism of interleukin-8 production from lung cancer cells: an involvement of EGF-EGFR-PI3K-Akt-Erk pathway. J Cell Physiol. 2012;227:35–43. doi: 10.1002/jcp.22722. [DOI] [PubMed] [Google Scholar]
- 435.Xue Y., Li L., Zhang D., Wu K., Guo P., Zeng J. Telomerase suppression initiates PML-dependent p53 activation to inhibit bladder cancer cell growth. Oncol Rep. 2010;24:1551–1559. doi: 10.3892/or_00001017. [DOI] [PubMed] [Google Scholar]
- 436.Wall M., Poortinga G., Stanley K.L., Lindemann R.K., Bots M., Chan C.J. The mTORC1 inhibitor everolimus prevents and treats Emu-Myc lymphoma by restoring oncogene-induced senescence. Cancer Discov. 2013;3:82–95. doi: 10.1158/2159-8290.CD-12-0404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 437.Beuvink I., Boulay A., Fumagalli S., Zilbermann F., Ruetz S., O’Reilly T. The mTOR inhibitor RAD001 sensitizes tumor cells to DNA-damaged induced apoptosis through inhibition of p21 translation. Cell. 2005;120:747–759. doi: 10.1016/j.cell.2004.12.040. [DOI] [PubMed] [Google Scholar]
- 438.Gogolin S., Ehemann V., Becker G., Brueckner L.M., Dreidax D., Bannert S. CDK4 inhibition restores G(1)-S arrest in MYCN-amplified neuroblastoma cells in the context of doxorubicin-induced DNA damage. Cell Cycle. 2013;12:1091–1104. doi: 10.4161/cc.24091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 439.Rader J., Russell M.R., Hart L.S., Nakazawa M.S., Belcastro L.T., Martinez D. Dual CDK4/CDK6 inhibition induces cell-cycle arrest and senescence in neuroblastoma. Clin Cancer Res. 2013;19:6173–6182. doi: 10.1158/1078-0432.CCR-13-1675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 440.Dai L., Liu Y., Liu J., Wen X., Xu Z., Wang Z. A novel cyclinE/cyclinA-CDK inhibitor targets p27(Kip1) degradation, cell cycle progression and cell survival: implications in cancer therapy. Cancer Lett. 2013;333:103–112. doi: 10.1016/j.canlet.2013.01.025. [DOI] [PubMed] [Google Scholar]
- 441.De Leon G., Cavino M., D’Angelo M., Krucher N.A. PNUTS knockdown potentiates the apoptotic effect of Roscovitine in breast and colon cancer cells. Int J Oncol. 2010;36:1269–1275. doi: 10.3892/ijo_00000611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 442.Zhang C., Lundgren K., Yan Z., Arango M.E., Price S., Huber A. Pharmacologic properties of AG-012986, a pan-cyclin-dependent kinase inhibitor with antitumor efficacy. Mol Cancer Ther. 2008;7:818–828. doi: 10.1158/1535-7163.MCT-07-0440. [DOI] [PubMed] [Google Scholar]
- 443.Jiao P., Zhou Y.S., Yang J.X., Zhao Y.L., Liu Q.Q., Yuan C. MK-2206 induces cell cycle arrest and apoptosis in HepG2 cells and sensitizes TRAIL-mediated cell death. Mol Cell Biochem. 2013;382:217–224. doi: 10.1007/s11010-013-1737-0. [DOI] [PubMed] [Google Scholar]
- 444.Xu X., Lu Z., Qiang W., Vidimar V., Kong B., Kim J.J. Inactivation of AKT induces cellular senescence in uterine leiomyoma. Endocrinology. 2014;155:1510–1519. doi: 10.1210/en.2013-1929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 445.Cotrim C.Z., Fabris V., Doria M.L., Lindberg K., Gustafsson J.A., Amado F. Estrogen receptor beta growth-inhibitory effects are repressed through activation of MAPK and PI3K signalling in mammary epithelial and breast cancer cells. Oncogene. 2013;32:2390–2402. doi: 10.1038/onc.2012.261. [DOI] [PubMed] [Google Scholar]
- 446.Li C., Liu V.W., Chan D.W., Yao K.M., Ngan H.Y. LY294002 and metformin cooperatively enhance the inhibition of growth and the induction of apoptosis of ovarian cancer cells. Int J Gynecol Cancer. 2012;22:15–22. doi: 10.1097/IGC.0b013e3182322834. [DOI] [PubMed] [Google Scholar]
- 447.Mukherjee S., Bhattacharya R.K., Roy M. Targeting protein kinase C (PKC) and telomerase by phenethyl isothiocyanate (PEITC) sensitizes PC-3 cells towards chemotherapeutic drug-induced apoptosis. J Environ Pathol Toxicol Oncol. 2009;28:269–282. doi: 10.1615/jenvironpatholtoxicoloncol.v28.i4.30. [DOI] [PubMed] [Google Scholar]
- 448.Wang T., Xue Y., Wang M., Sun Q. Silencing of the hTERT gene through RNA interference induces apoptosis via bax/bcl-2 in human glioma cells. Oncol Rep. 2012;28:1153–1158. doi: 10.3892/or.2012.1952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 449.Ge J., Liu Y., Li Q., Guo X., Gu L., Ma Z.G. Resveratrol induces apoptosis and autophagy in T-cell acute lymphoblastic leukemia cells by inhibiting Akt/mTOR and activating p38-MAPK. Biomed Environ Sci. 2013;26:902–911. doi: 10.3967/bes2013.019. [DOI] [PubMed] [Google Scholar]
- 450.Zhang X.H., Cheng Y., Shin J.Y., Kim J.O., Oh J.E., Kang J.H. A CDK4/6 inhibitor enhances cytotoxicity of paclitaxel in lung adenocarcinoma cells harboring mutant KRAS as well as wild-type KRAS. Cancer Biol Ther. 2013;14:597–605. doi: 10.4161/cbt.24592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 451.Zolnierczyk J.D., Blonski J.Z., Robak T., Kilianska Z.M., Wesierska-Gadek J. Roscovitine triggers apoptosis in B-cell chronic lymphocytic leukemia cells with similar efficiency as combinations of conventional purine analogs with cyclophosphamide. Ann N Y Acad Sci. 2009;1171:124–131. doi: 10.1111/j.1749-6632.2009.04903.x. [DOI] [PubMed] [Google Scholar]
- 452.Cassinelli G., Zuco V., Gatti L., Lanzi C., Zaffaroni N., Colombo D. Targeting the Akt kinase to modulate survival, invasiveness and drug resistance of cancer cells. Curr Med Chem. 2013;20:1923–1945. doi: 10.2174/09298673113209990106. [DOI] [PubMed] [Google Scholar]
- 453.Bagheri S., Nosrati M., Li S., Fong S., Torabian S., Rangel J. Genes and pathways downstream of telomerase in melanoma metastasis. Proc Natl Acad Sci U S A. 2006;103:11306–11311. doi: 10.1073/pnas.0510085103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 454.Liu L.L., Long Z.J., Wang L.X., Zheng F.M., Fang Z.G., Yan M. Inhibition of mTOR pathway sensitizes acute myeloid leukemia cells to aurora inhibitors by suppression of glycolytic metabolism. Mol Cancer Res. 2013;11:1326–1336. doi: 10.1158/1541-7786.MCR-13-0172. [DOI] [PubMed] [Google Scholar]
- 455.Zanuy M., Ramos-Montoya A., Villacanas O., Canela N., Miranda A., Aguilar E. Cyclin-dependent kinases 4 and 6 control tumor progression and direct glucose oxidation in the pentose cycle. Metabolomics. 2012;8:454–464. doi: 10.1007/s11306-011-0328-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 456.Yalcin A., Clem B.F., Simmons A., Lane A., Nelson K., Clem A.L. Nuclear targeting of 6-phosphofructo-2-kinase (PFKFB3) increases proliferation via cyclin-dependent kinases. J Biol Chem. 2009;284:24223–24232. doi: 10.1074/jbc.M109.016816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 457.Liu Z., Zhang Y.Y., Zhang Q.W., Zhao S.R., Wu C.Z., Cheng X. 3-Bromopyruvate induces apoptosis in breast cancer cells by downregulating Mcl-1 through the PI3K/Akt signaling pathway. Anticancer Drugs. 2014;25:447–455. doi: 10.1097/CAD.0000000000000081. [DOI] [PubMed] [Google Scholar]
- 458.Liu P.P., Liao J., Tang Z.J., Wu W.J., Yang J., Zeng Z.L. Metabolic regulation of cancer cell side population by glucose through activation of the Akt pathway. Cell Death Differ. 2014;21:124–135. doi: 10.1038/cdd.2013.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 459.Gershon T.R., Crowther A.J., Tikunov A., Garcia I., Annis R., Yuan H. Hexokinase-2-mediated aerobic glycolysis is integral to cerebellar neurogenesis and pathogenesis of medulloblastoma. Cancer Metab. 2013;1:2. doi: 10.1186/2049-3002-1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 460.Polivka J., Jr., Janku F. Molecular targets for cancer therapy in the PI3K/AKT/mTOR pathway. Pharmacol Ther. 2014;142:164–175. doi: 10.1016/j.pharmthera.2013.12.004. [DOI] [PubMed] [Google Scholar]
- 461.Wang Y., Sparwasser T., Figlin R., Kim H.L. Foxp3+ T cells inhibit antitumor immune memory modulated by mTOR inhibition. Cancer Res. 2014;74:2217–2228. doi: 10.1158/0008-5472.CAN-13-2928. [DOI] [PubMed] [Google Scholar]
- 462.Noh K.H., Kim B.W., Song K.H., Cho H., Lee Y.H., Kim J.H. Nanog signaling in cancer promotes stem-like phenotype and immune evasion. J Clin Investig. 2012;122:4077–4093. doi: 10.1172/JCI64057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 463.Webb L.M., Vigorito E., Wymann M.P., Hirsch E., Turner M. Cutting edge: T cell development requires the combined activities of the p110gamma and p110delta catalytic isoforms of phosphatidylinositol 3-kinase. J Immunol. 2005;175:2783–2787. doi: 10.4049/jimmunol.175.5.2783. [DOI] [PubMed] [Google Scholar]
- 464.Hemon P., Jean-Louis F., Ramgolam K., Brignone C., Viguier M., Bachelez H. MHC class II engagement by its ligand LAG-3 (CD223) contributes to melanoma resistance to apoptosis. J Immunol. 2011;186:5173–5183. doi: 10.4049/jimmunol.1002050. [DOI] [PubMed] [Google Scholar]
- 465.Pallini R., Pierconti F., Falchetti M.L., D’Arcangelo D., Fernandez E., Maira G. Evidence for telomerase involvement in the angiogenesis of astrocytic tumors: expression of human telomerase reverse transcriptase messenger RNA by vascular endothelial cells. J Neurosurg. 2001;94:961–971. doi: 10.3171/jns.2001.94.6.0961. [DOI] [PubMed] [Google Scholar]
- 466.Karar J., Maity A. PI3K/AKT/mTOR pathway in angiogenesis. Front Mol Neurosci. 2011;4:51. doi: 10.3389/fnmol.2011.00051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 467.Chen Z., Zhang Y., Jia C., Wang Y., Lai P., Zhou X. mTORC1/2 targeted by n-3 polyunsaturated fatty acids in the prevention of mammary tumorigenesis and tumor progression. Oncogene. 2014;33:4548–4557. doi: 10.1038/onc.2013.402. [DOI] [PubMed] [Google Scholar]
- 468.Kollmann K., Heller G., Schneckenleithner C., Warsch W., Scheicher R., Ott R.G. A kinase-independent function of CDK6 links the cell cycle to tumor angiogenesis. Cancer Cell. 2013;24:167–181. doi: 10.1016/j.ccr.2013.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 469.Abedin Z.R., Ma Z., Reddy E.P. Increased angiogenesis in Cdk4(R24C/R24C):Apc(+/Min) intestinal tumors. Cell Cycle. 2010;9:2456–2463. doi: 10.4161/cc.9.12.12055. [DOI] [PubMed] [Google Scholar]
- 470.Warfel N.A., Dolloff N.G., Dicker D.T., Malysz J., El-Deiry W.S. CDK1 stabilizes HIF-1alpha via direct phosphorylation of Ser668 to promote tumor growth. Cell Cycle. 2013;12:3689–3701. doi: 10.4161/cc.26930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 471.Liebl J., Krystof V., Vereb G., Takacs L., Strnad M., Pechan P. Anti-angiogenic effects of purine inhibitors of cyclin dependent kinases. Angiogenesis. 2011;14:281–291. doi: 10.1007/s10456-011-9212-6. [DOI] [PubMed] [Google Scholar]
- 472.Chen P.C., Peng J.R., Huang L., Li W.X., Wang W.Z., Cui Z.Q. Overexpression of human telomerase reverse transcriptase promotes the motility and invasiveness of HepG2 cells in vitro. Oncol Rep. 2013;30:1157–1164. doi: 10.3892/or.2013.2563. [DOI] [PubMed] [Google Scholar]
- 473.Yu S.T., Chen L., Wang H.J., Tang X.D., Fang D.C., Yang S.M. hTERT promotes the invasion of telomerase-negative tumor cells in vitro. Int J Oncol. 2009;35:329–336. [PubMed] [Google Scholar]
- 474.Zong H., Yin B., Zhou H., Cai D., Ma B., Xiang Y. Inhibition of mTOR pathway attenuates migration and invasion of gallbladder cancer via EMT inhibition. Mol Biol Rep. 2014;41:4507–4512. doi: 10.1007/s11033-014-3321-4. [DOI] [PubMed] [Google Scholar]
- 475.Lin G., Gai R., Chen Z., Wang Y., Liao S., Dong R. The dual PI3K/mTOR inhibitor NVP-BEZ235 prevents epithelial-mesenchymal transition induced by hypoxia and TGF-beta1. Eur J Pharmacol. 2014;729:45–53. doi: 10.1016/j.ejphar.2014.02.011. [DOI] [PubMed] [Google Scholar]
- 476.Liu F., Korc M. Cdk4/6 inhibition induces epithelial–mesenchymal transition and enhances invasiveness in pancreatic cancer cells. Mol Cancer Ther. 2012;11:2138–2148. doi: 10.1158/1535-7163.MCT-12-0562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 477.Wu A., Wu B., Guo J., Luo W., Wu D., Yang H. Elevated expression of CDK4 in lung cancer. J Transl Med. 2011;9:38. doi: 10.1186/1479-5876-9-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 478.Strock C.J., Park J.I., Nakakura E.K., Bova G.S., Isaacs J.T., Ball D.W. Cyclin-dependent kinase 5 activity controls cell motility and metastatic potential of prostate cancer cells. Cancer Res. 2006;66:7509–7515. doi: 10.1158/0008-5472.CAN-05-3048. [DOI] [PubMed] [Google Scholar]
- 479.Huang C., Rajfur Z., Yousefi N., Chen Z., Jacobson K., Ginsberg M.H. Talin phosphorylation by Cdk5 regulates Smurf1-mediated talin head ubiquitylation and cell migration. Nat Cell Biol. 2009;11:624–630. doi: 10.1038/ncb1868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 480.Barrette K., Van Kelst S., Wouters J., Marasigan V., Fieuws S., Agostinis P. Epithelial–mesenchymal transition during invasion of cutaneous squamous cell carcinoma is paralleled by AKT activation. Br J Dermatol. 2014;171:1014–1021. doi: 10.1111/bjd.12967. [DOI] [PubMed] [Google Scholar]
- 481.Falchetti M.L., Mongiardi M.P., Fiorenzo P., Petrucci G., Pierconti F., D’Agnano I. Inhibition of telomerase in the endothelial cells disrupts tumor angiogenesis in glioblastoma xenografts. Int J Cancer. 2008;122:1236–1242. doi: 10.1002/ijc.23193. [DOI] [PubMed] [Google Scholar]
- 482.Liu Z., Li Q., Li K., Chen L., Li W., Hou M. Telomerase reverse transcriptase promotes epithelial–mesenchymal transition and stem cell-like traits in cancer cells. Oncogene. 2013;32:4203–4213. doi: 10.1038/onc.2012.441. [DOI] [PubMed] [Google Scholar]
- 483.Saito K., Matsumoto S., Yasui H., Devasahayam N., Subramanian S., Munasinghe J.P. Longitudinal imaging studies of tumor microenvironment in mice treated with the mTOR inhibitor rapamycin. PLoS ONE. 2012;7:e49456. doi: 10.1371/journal.pone.0049456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 484.Al-Ansari M.M., Hendrayani S.F., Shehata A.I., Aboussekhra A. p16(INK4A) represses the paracrine tumor-promoting effects of breast stromal fibroblasts. Oncogene. 2013;32:2356–2364. doi: 10.1038/onc.2012.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 485.Chatzistamou I., Dioufa N., Trimis G., Sklavounou A., Kittas C., Kiaris H. p21/waf1 and smooth-muscle actin alpha expression in stromal fibroblasts of oral cancers. Cell Oncol. 2011;34:483–488. doi: 10.1007/s13402-011-0044-6. [DOI] [PubMed] [Google Scholar]
- 486.Capparelli C., Guido C., Whitaker-Menezes D., Bonuccelli G., Balliet R., Pestell T.G. Autophagy and senescence in cancer-associated fibroblasts metabolically supports tumor growth and metastasis via glycolysis and ketone production. Cell Cycle. 2012;11:2285–2302. doi: 10.4161/cc.20718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 487.Subramaniam K.S., Tham S.T., Mohamed Z., Woo Y.L., Mat Adenan N.A., Chung I. Cancer-associated fibroblasts promote proliferation of endometrial cancer cells. PLOS ONE. 2013;8:e68923. doi: 10.1371/journal.pone.0068923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 488.Lin B.Q., Zeng Z.Y., Yang S.S., Zhuang C.W. Dietary restriction suppresses tumor growth, reduces angiogenesis, and improves tumor microenvironment in human non-small-cell lung cancer xenografts. Lung Cancer. 2013;79:111–117. doi: 10.1016/j.lungcan.2012.11.001. [DOI] [PubMed] [Google Scholar]
- 489.Rosich L., Saborit-Villarroya I., Lopez-Guerra M., Xargay-Torrent S., Montraveta A., Aymerich M. The phosphatidylinositol-3-kinase inhibitor NVP-BKM120 overcomes resistance signals derived from microenvironment by regulating the Akt/FoxO3a/Bim axis in chronic lymphocytic leukemia cells. Haematologica. 2013;98:1739–1747. doi: 10.3324/haematol.2013.088849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 490.Wu X., Smavadati S., Nordfjall K., Karlsson K., Qvarnstrom F., Simonsson M. Telomerase antagonist imetelstat inhibits esophageal cancer cell growth and increases radiation-induced DNA breaks. Biochim Biophys Acta. 2012;1823:2130–2135. doi: 10.1016/j.bbamcr.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 491.Uziel O., Reshef H., Ravid A., Fabian I., Halperin D., Ram R. Oxidative stress causes telomere damage in Fanconi anaemia cells – a possible predisposition for malignant transformation. Br J Haematol. 2008;142:82–93. doi: 10.1111/j.1365-2141.2008.07137.x. [DOI] [PubMed] [Google Scholar]
- 492.Kim Y.M., Yang S., Xu W., Li S., Yang X. Continuous in vitro exposure to low-dose genistein induces genomic instability in breast epithelial cells. Cancer Genet Cytogenet. 2008;186:78–84. doi: 10.1016/j.cancergencyto.2008.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 493.Pugalendhi P., Manoharan S., Panjamurthy K., Balakrishnan S., Nirmal M.R. Antigenotoxic effect of genistein against 7,12-dimethylbenz[a]anthracene induced genotoxicity in bone marrow cells of female Wistar rats. Pharmacol Rep. 2009;61:296–303. doi: 10.1016/s1734-1140(09)70035-0. [DOI] [PubMed] [Google Scholar]
- 494.Chan N.L., Wang H., Wang Y., Leung H.Y., Leung L.K. Polycyclic aromatic hydrocarbon-induced CYP1B1 activity is suppressed by perillyl alcohol in MCF-7 cells. Toxicol Appl Pharmacol. 2006;213:98–104. doi: 10.1016/j.taap.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 495.Ogiwara H., Ui A., Shiotani B., Zou L., Yasui A., Kohno T. Curcumin suppresses multiple DNA damage response pathways and has potency as a sensitizer to PARP inhibitor. Carcinogenesis. 2013;34:2486–2497. doi: 10.1093/carcin/bgt240. [DOI] [PubMed] [Google Scholar]
- 496.Thomas P., Wang Y.J., Zhong J.H., Kosaraju S., O’Callaghan N.J., Zhou X.F. Grape seed polyphenols and curcumin reduce genomic instability events in a transgenic mouse model for Alzheimer's disease. Mutat Res. 2009;661:25–34. doi: 10.1016/j.mrfmmm.2008.10.016. [DOI] [PubMed] [Google Scholar]
- 497.Durgo K., Kostic S., Gradiski K., Komes D., Osmak M., Franekic J. Genotoxic effects of green tea extract on human laryngeal carcinoma cells in vitro. Arh Hig Rada Toksikol. 2011;62:139–146. doi: 10.2478/10004-1254-62-2011-2105. [DOI] [PubMed] [Google Scholar]
- 498.Tobi S.E., Gilbert M., Paul N., McMillan T.J. The green tea polyphenol, epigallocatechin-3-gallate, protects against the oxidative cellular and genotoxic damage of UVA radiation. Int J Cancer. 2002;102:439–444. doi: 10.1002/ijc.10730. [DOI] [PubMed] [Google Scholar]
- 499.Chiyomaru T., Yamamura S., Fukuhara S., Hidaka H., Majid S., Saini S. Genistein up-regulates tumor suppressor microRNA-574-3p in prostate cancer. PLOS ONE. 2013;8:e58929. doi: 10.1371/journal.pone.0058929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 500.Nakamura H., Wang Y., Kurita T., Adomat H., Cunha G.R., Wang Y. Genistein increases epidermal growth factor receptor signaling and promotes tumor progression in advanced human prostate cancer. PLoS ONE. 2011;6:e20034. doi: 10.1371/journal.pone.0020034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 501.Fischer Jde S., Liao L., Carvalho P.C., Barbosa V.C., Domont G.B., Carvalho Mda G. Dynamic proteomic overview of glioblastoma cells (A172) exposed to perillyl alcohol. J Proteomics. 2010;73:1018–1027. doi: 10.1016/j.jprot.2010.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 502.Logan J.E., Mostofizadeh N., Desai A.J., Von Euw E., Conklin D., Konkankit V. PD-0332991, a potent and selective inhibitor of cyclin-dependent kinase 4/6, demonstrates inhibition of proliferation in renal cell carcinoma at nanomolar concentrations and molecular markers predict for sensitivity. Anticancer Res. 2013;33:2997–3004. [PubMed] [Google Scholar]
- 503.Feldmann G., Mishra A., Bisht S., Karikari C., Garrido-Laguna I., Rasheed Z. Cyclin-dependent kinase inhibitor Dinaciclib (SCH727965) inhibits pancreatic cancer growth and progression in murine xenograft models. Cancer Biol Ther. 2011;12:598–609. doi: 10.4161/cbt.12.7.16475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 504.Ono M., Higuchi T., Takeshima M., Chen C., Nakano S. Antiproliferative and apoptosis-inducing activity of curcumin against human gallbladder adenocarcinoma cells. Anticancer Res. 2013;33:1861–1866. [PubMed] [Google Scholar]
- 505.Cai X.Z., Wang J., Li X.D., Wang G.L., Liu F.N., Cheng M.S. Curcumin suppresses proliferation and invasion in human gastric cancer cells by downregulation of PAK1 activity and cyclin D1 expression. Cancer Biol Ther. 2009;8:1360–1368. doi: 10.4161/cbt.8.14.8720. [DOI] [PubMed] [Google Scholar]
- 506.Lim Y.C., Cha Y.Y. Epigallocatechin-3-gallate induces growth inhibition and apoptosis of human anaplastic thyroid carcinoma cells through suppression of EGFR/ERK pathway and cyclin B1/CDK1 complex. J Surg Oncol. 2011;104:776–780. doi: 10.1002/jso.21999. [DOI] [PubMed] [Google Scholar]
- 507.Ma Y.C., Li C., Gao F., Xu Y., Jiang Z.B., Liu J.X. Epigallocatechin gallate inhibits the growth of human lung cancer by directly targeting the EGFR signaling pathway. Oncol Rep. 2014;31:1343–1349. doi: 10.3892/or.2013.2933. [DOI] [PubMed] [Google Scholar]
- 508.Khan A.Q., Khan R., Rehman M.U., Lateef A., Tahir M., Ali F. Soy isoflavones (daidzein & genistein) inhibit 12-O-tetradecanoylphorbol-13-acetate (TPA)-induced cutaneous inflammation via modulation of COX-2 and NF-kappaB in Swiss albino mice. Toxicology. 2012;302:266–274. doi: 10.1016/j.tox.2012.08.008. [DOI] [PubMed] [Google Scholar]
- 509.D’Alessandro T., Prasain J., Benton M.R., Botting N., Moore R., Darley-Usmar V. Polyphenols, inflammatory response, and cancer prevention: chlorination of isoflavones by human neutrophils. J Nutr. 2003;133:3773S–3777S. doi: 10.1093/jn/133.11.3773S. [DOI] [PubMed] [Google Scholar]
- 510.Hall J.M., Korach K.S. Endocrine disrupting chemicals promote the growth of ovarian cancer cells via the ER-CXCL12-CXCR4 signaling axis. Mol Carcinog. 2013;52:715–725. doi: 10.1002/mc.21913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 511.Magkouta S., Stathopoulos G.T., Psallidas I., Papapetropoulos A., Kolisis F.N., Roussos C. Protective effects of mastic oil from Pistacia lentiscus variation chia against experimental growth of lewis lung carcinoma. Nutr Cancer. 2009;61:640–648. doi: 10.1080/01635580902825647. [DOI] [PubMed] [Google Scholar]
- 512.Vaughan R.A., Garcia-Smith R., Dorsey J., Griffith J.K., Bisoffi M., Trujillo K.A. Tumor necrosis factor alpha induces Warburg-like metabolism and is reversed by anti-inflammatory curcumin in breast epithelial cells. Int J Cancer. 2013;133:2504–2510. doi: 10.1002/ijc.28264. [DOI] [PubMed] [Google Scholar]
- 513.Killian P.H., Kronski E., Michalik K.M., Barbieri O., Astigiano S., Sommerhoff C.P. Curcumin inhibits prostate cancer metastasis in vivo by targeting the inflammatory cytokines CXCL1 and -2. Carcinogenesis. 2012;33:2507–2519. doi: 10.1093/carcin/bgs312. [DOI] [PubMed] [Google Scholar]
- 514.Nonn L., Duong D., Peehl D.M. Chemopreventive anti-inflammatory activities of curcumin and other phytochemicals mediated by MAP kinase phosphatase-5 in prostate cells. Carcinogenesis. 2007;28:1188–1196. doi: 10.1093/carcin/bgl241. [DOI] [PubMed] [Google Scholar]
- 515.Hardtner C., Multhoff G., Falk W., Radons J. (−)-Epigallocatechin-3-gallate, a green tea-derived catechin, synergizes with celecoxib to inhibit IL-1-induced tumorigenic mediators by human pancreatic adenocarcinoma cells Colo357. Eur J Pharmacol. 2012;684:36–43. doi: 10.1016/j.ejphar.2012.03.039. [DOI] [PubMed] [Google Scholar]
- 516.Hoffmann J., Junker H., Schmieder A., Venz S., Brandt R., Multhoff G. EGCG downregulates IL-1RI expression and suppresses IL-1-induced tumorigenic factors in human pancreatic adenocarcinoma cells. Biochem Pharmacol. 2011;82:1153–1162. doi: 10.1016/j.bcp.2011.07.063. [DOI] [PubMed] [Google Scholar]
- 517.Zhang Z., Wang C.Z., Du G.J., Qi L.W., Calway T., He T.C. Genistein induces G2/M cell cycle arrest and apoptosis via ATM/p53-dependent pathway in human colon cancer cells. Int J Oncol. 2013;43:289–296. doi: 10.3892/ijo.2013.1946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 518.Li Y., Chen H., Hardy T.M., Tollefsbol T.O. Epigenetic regulation of multiple tumor-related genes leads to suppression of breast tumorigenesis by dietary genistein. PLOS ONE. 2013;8:e54369. doi: 10.1371/journal.pone.0054369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 519.Majid S., Kikuno N., Nelles J., Noonan E., Tanaka Y., Kawamoto K. Genistein induces the p21WAF1/CIP1 and p16INK4a tumor suppressor genes in prostate cancer cells by epigenetic mechanisms involving active chromatin modification. Cancer Res. 2008;68:2736–2744. doi: 10.1158/0008-5472.CAN-07-2290. [DOI] [PubMed] [Google Scholar]
- 520.Yuri T., Danbara N., Tsujita-Kyutoku M., Kiyozuka Y., Senzaki H., Shikata N. Perillyl alcohol inhibits human breast cancer cell growth in vitro and in vivo. Breast Cancer Res Treat. 2004;84:251–260. doi: 10.1023/B:BREA.0000019966.97011.4d. [DOI] [PubMed] [Google Scholar]
- 521.Konecny G.E., Winterhoff B., Kolarova T., Qi J., Manivong K., Dering J. Expression of p16 and retinoblastoma determines response to CDK4/6 inhibition in ovarian cancer. Clin Cancer Res. 2011;17:1591–1602. doi: 10.1158/1078-0432.CCR-10-2307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 522.Desai B.M., Villanueva J., Nguyen T.T., Lioni M., Xiao M., Kong J. The anti-melanoma activity of dinaciclib, a cyclin-dependent kinase inhibitor, is dependent on p53 signaling. PLOS ONE. 2013;8:e59588. doi: 10.1371/journal.pone.0059588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 523.Mosieniak G., Adamowicz M., Alster O., Jaskowiak H., Szczepankiewicz A.A., Wilczynski G.M. Curcumin induces permanent growth arrest of human colon cancer cells: link between senescence and autophagy. Mech Ageing Dev. 2012;133:444–455. doi: 10.1016/j.mad.2012.05.004. [DOI] [PubMed] [Google Scholar]
- 524.Abusnina A., Keravis T., Yougbare I., Bronner C., Lugnier C. Anti-proliferative effect of curcumin on melanoma cells is mediated by PDE1A inhibition that regulates the epigenetic integrator UHRF1. Mol Nutr Food Res. 2011;55:1677–1689. doi: 10.1002/mnfr.201100307. [DOI] [PubMed] [Google Scholar]
- 525.Zhang X., Min K.W., Wimalasena J., Baek S.J. Cyclin D1 degradation and p21 induction contribute to growth inhibition of colorectal cancer cells induced by epigallocatechin-3-gallate. J Cancer Res Clin Oncol. 2012;138:2051–2060. doi: 10.1007/s00432-012-1276-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 526.Thakur V.S., Gupta K., Gupta S. Green tea polyphenols increase p53 transcriptional activity and acetylation by suppressing class I histone deacetylases. Int J Oncol. 2012;41:353–361. doi: 10.3892/ijo.2012.1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 527.Phan V., Walters J., Brownlow B., Elbayoumi T. Enhanced cytotoxicity of optimized liposomal genistein via specific induction of apoptosis in breast, ovarian and prostate carcinomas. J Drug Target. 2013;21:1001–1011. doi: 10.3109/1061186X.2013.847099. [DOI] [PubMed] [Google Scholar]
- 528.Prietsch R.F., Monte L.G., da Silva F.A., Beira F.T., Del Pino F.A., Campos V.F. Genistein induces apoptosis and autophagy in human breast MCF-7 cells by modulating the expression of proapoptotic factors and oxidative stress enzymes. Mol Cell Biochem. 2014;390:235–242. doi: 10.1007/s11010-014-1974-x. [DOI] [PubMed] [Google Scholar]
- 529.Yeruva L., Pierre K.J., Elegbede A., Wang R.C., Carper S.W. Perillyl alcohol and perillic acid induced cell cycle arrest and apoptosis in non small cell lung cancer cells. Cancer Lett. 2007;257:216–226. doi: 10.1016/j.canlet.2007.07.020. [DOI] [PubMed] [Google Scholar]
- 530.Gomez-Contreras P.C., Hernandez-Flores G., Ortiz-Lazareno P.C., Del Toro-Arreola S., Delgado-Rizo V., Lerma-Diaz J.M. In vitro induction of apoptosis in U937 cells by perillyl alcohol with sensitization by pentoxifylline: increased BCL-2 and BAX protein expression. Chemotherapy. 2006;52:308–315. doi: 10.1159/000096003. [DOI] [PubMed] [Google Scholar]
- 531.Chiron D., Martin P., Di Liberto M., Huang X., Ely S., Lannutti B.J. Induction of prolonged early G1 arrest by CDK4/CDK6 inhibition reprograms lymphoma cells for durable PI3Kdelta inhibition through PIK3IP1. Cell Cycle. 2013;12:1892–1900. doi: 10.4161/cc.24928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 532.Fu W., Ma L., Chu B., Wang X., Bui M.M., Gemmer J. The cyclin-dependent kinase inhibitor SCH 727965 (dinacliclib) induces the apoptosis of osteosarcoma cells. Mol Cancer Ther. 2011;10:1018–1027. doi: 10.1158/1535-7163.MCT-11-0167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 533.Yu L.L., Wu J.G., Dai N., Yu H.G., Si J.M. Curcumin reverses chemoresistance of human gastric cancer cells by downregulating the NF-kappaB transcription factor. Oncol Rep. 2011;26:1197–1203. doi: 10.3892/or.2011.1410. [DOI] [PubMed] [Google Scholar]
- 534.Cao A., Li Q., Yin P., Dong Y., Shi H., Wang L. Curcumin induces apoptosis in human gastric carcinoma AGS cells and colon carcinoma HT-29 cells through mitochondrial dysfunction and endoplasmic reticulum stress. Apoptosis. 2013;18:1391–1402. doi: 10.1007/s10495-013-0871-1. [DOI] [PubMed] [Google Scholar]
- 535.Li J.J., Gu Q.H., Li M., Yang H.P., Cao L.M., Hu C.P. Role of Ku70 and Bax in epigallocatechin-3-gallate-induced apoptosis of A549 cells in vivo. Oncol Lett. 2013;5:101–106. doi: 10.3892/ol.2012.972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 536.Manohar M., Fatima I., Saxena R., Chandra V., Sankhwar P.L., Dwivedi A. (−)-Epigallocatechin-3-gallate induces apoptosis in human endometrial adenocarcinoma cells via ROS generation and p38 MAP kinase activation. J Nutr Biochem. 2013;24:940–947. doi: 10.1016/j.jnutbio.2012.06.013. [DOI] [PubMed] [Google Scholar]
- 537.Boros L.G., Bassilian S., Lim S., Lee W.N. Genistein inhibits nonoxidative ribose synthesis in MIA pancreatic adenocarcinoma cells: a new mechanism of controlling tumor growth. Pancreas. 2001;22:1–7. doi: 10.1097/00006676-200101000-00001. [DOI] [PubMed] [Google Scholar]
- 538.Bayet-Robert M., Morvan D. Metabolomics reveals metabolic targets and biphasic responses in breast cancer cells treated by curcumin alone and in association with docetaxel. PLOS ONE. 2013;8:e57971. doi: 10.1371/journal.pone.0057971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 539.Moreira L., Araujo I., Costa T., Correia-Branco A., Faria A., Martel F. Quercetin and epigallocatechin gallate inhibit glucose uptake and metabolism by breast cancer cells by an estrogen receptor-independent mechanism. Exp Cell Res. 2013;319:1784–1795. doi: 10.1016/j.yexcr.2013.05.001. [DOI] [PubMed] [Google Scholar]
- 540.Relat J., Blancafort A., Oliveras G., Cufi S., Haro D., Marrero P.F. Different fatty acid metabolism effects of (−)-epigallocatechin-3-gallate and C75 in adenocarcinoma lung cancer. BMC Cancer. 2012;12:280. doi: 10.1186/1471-2407-12-280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 541.Guo T.L., Chi R.P., Hernandez D.M., Auttachoat W., Zheng J.F. Decreased 7,12-dimethylbenz[a]anthracene-induced carcinogenesis coincides with the induction of antitumor immunities in adult female B6C3F1 mice pretreated with genistein. Carcinogenesis. 2007;28:2560–2566. doi: 10.1093/carcin/bgm223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 542.Bhattacharyya S., Md Sakib Hossain D., Mohanty S., Sankar Sen G., Chattopadhyay S., Banerjee S. Curcumin reverses T cell-mediated adaptive immune dysfunctions in tumor-bearing hosts. Cell Mol Immunol. 2010;7:306–315. doi: 10.1038/cmi.2010.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 543.Chang Y.F., Chuang H.Y., Hsu C.H., Liu R.S., Gambhir S.S., Hwang J.J. Immunomodulation of curcumin on adoptive therapy with T cell functional imaging in mice. Cancer Prev Res. 2012;5:444–452. doi: 10.1158/1940-6207.CAPR-11-0308. [DOI] [PubMed] [Google Scholar]
- 544.Mantena S.K., Roy A.M., Katiyar S.K. Epigallocatechin-3-gallate inhibits photocarcinogenesis through inhibition of angiogenic factors and activation of CD8+ T cells in tumors. Photochem Photobiol. 2005;81:1174–1179. doi: 10.1562/2005-04-11-RA-487. [DOI] [PubMed] [Google Scholar]
- 545.Kawai K., Tsuno N.H., Kitayama J., Okaji Y., Yazawa K., Asakage M. Epigallocatechin gallate attenuates adhesion and migration of CD8+ T cells by binding to CD11b. J Allergy Clin Immunol. 2004;113:1211–1217. doi: 10.1016/j.jaci.2004.02.044. [DOI] [PubMed] [Google Scholar]
- 546.Kang T.H., Lee J.H., Song C.K., Han H.D., Shin B.C., Pai S.I. Epigallocatechin-3-gallate enhances CD8+ T cell-mediated antitumor immunity induced by DNA vaccination. Cancer Res. 2007;67:802–811. doi: 10.1158/0008-5472.CAN-06-2638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 547.Fotsis T., Pepper M., Adlercreutz H., Fleischmann G., Hase T., Montesano R. Genistein, a dietary-derived inhibitor of in vitro angiogenesis. Proc Natl Acad Sci U S A. 1993;90:2690–2694. doi: 10.1073/pnas.90.7.2690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 548.Guo Y., Wang S., Hoot D.R., Clinton S.K. Suppression of VEGF-mediated autocrine and paracrine interactions between prostate cancer cells and vascular endothelial cells by soy isoflavones. J Nutr Biochem. 2007;18:408–417. doi: 10.1016/j.jnutbio.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 549.Kang X., Jin S., Zhang Q. Antitumor and antiangiogenic activity of soy phytoestrogen on 7,12-dimethylbenz[alpha]anthracene-induced mammary tumors following ovariectomy in Sprague-Dawley rats. J Food Sci. 2009;74:H237–H242. doi: 10.1111/j.1750-3841.2009.01278.x. [DOI] [PubMed] [Google Scholar]
- 550.Loutrari H., Hatziapostolou M., Skouridou V., Papadimitriou E., Roussos C., Kolisis F.N. Perillyl alcohol is an angiogenesis inhibitor. J Pharmacol Exp Ther. 2004;311:568–575. doi: 10.1124/jpet.104.070516. [DOI] [PubMed] [Google Scholar]
- 551.Arbiser J.L., Klauber N., Rohan R., van Leeuwen R., Huang M.T., Fisher C. Curcumin is an in vivo inhibitor of angiogenesis. Mol Med. 1998;4:376–383. [PMC free article] [PubMed] [Google Scholar]
- 552.Jung Y.D., Ellis L.M. Inhibition of tumour invasion and angiogenesis by epigallocatechin gallate (EGCG), a major component of green tea. Int J Exp Pathol. 2001;82:309–316. doi: 10.1046/j.1365-2613.2001.00205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 553.Deng P.B., Hu C.P., Xiong Z., Yang H.P., Li Y.Y. Treatment with EGCG in NSCLC leads to decreasing interstitial fluid pressure and hypoxia to improve chemotherapy efficacy through rebalance of Ang-1 and Ang-2. Chin J Nat Med. 2013;11:245–253. doi: 10.1016/S1875-5364(13)60023-0. [DOI] [PubMed] [Google Scholar]
- 554.El Touny L.H., Banerjee P.P. Identification of a biphasic role for genistein in the regulation of prostate cancer growth and metastasis. Cancer Res. 2009;69:3695–3703. doi: 10.1158/0008-5472.CAN-08-2958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 555.Nakamura H., Wang Y., Xue H., Romanish M.T., Mager D.L., Helgason C.D. Genistein versus ICI 182, 780: an ally or enemy in metastatic progression of prostate cancer. Prostate. 2013;73:1747–1760. doi: 10.1002/pros.22712. [DOI] [PubMed] [Google Scholar]
- 556.Yu D., Shin H.S., Lee Y.S., Lee D., Kim S., Lee Y.C. Genistein attenuates cancer stem cell characteristics in gastric cancer through the downregulation of Gli1. Oncol Rep. 2014;31:673–678. doi: 10.3892/or.2013.2893. [DOI] [PubMed] [Google Scholar]
- 557.Cheng T.S., Chen W.C., Lin Y.Y., Tsai C.H., Liao C.I., Shyu H.Y. Curcumin-targeting pericellular serine protease matriptase role in suppression of prostate cancer cell invasion, tumor growth, and metastasis. Cancer Prev Res. 2013;6:495–505. doi: 10.1158/1940-6207.CAPR-12-0293-T. [DOI] [PubMed] [Google Scholar]
- 558.Soung Y.H., Chung J. Curcumin inhibition of the functional interaction between integrin alpha6beta4 and the epidermal growth factor receptor. Mol Cancer Ther. 2011;10:883–891. doi: 10.1158/1535-7163.MCT-10-1053. [DOI] [PubMed] [Google Scholar]
- 559.Deb G., Thakur V.S., Limaye A.M., Gupta S. Epigenetic induction of tissue inhibitor of matrix metalloproteinase-3 by green tea polyphenols in breast cancer cells. Mol Carcinog. 2014 doi: 10.1002/mc.22121. [DOI] [PubMed] [Google Scholar]
- 560.Maruyama T., Murata S., Nakayama K., Sano N., Ogawa K., Nowatari T. (−)-Epigallocatechin-3-gallate suppresses liver metastasis of human colorectal cancer. Oncol Rep. 2014;31:625–633. doi: 10.3892/or.2013.2925. [DOI] [PubMed] [Google Scholar]
- 561.Takahashi A., Watanabe T., Mondal A., Suzuki K., Kurusu-Kanno M., Li Z. Mechanism-based inhibition of cancer metastasis with (−)-epigallocatechin gallate. Biochem Biophys Res Commun. 2014;443:1–6. doi: 10.1016/j.bbrc.2013.10.094. [DOI] [PubMed] [Google Scholar]
- 562.Lou D., Wang B., Wang Y., Cao Y. Selective killing of cancer stem cells by a novel dual-targeting strategy. Med Hypotheses. 2012;79:430–432. doi: 10.1016/j.mehy.2012.06.012. [DOI] [PubMed] [Google Scholar]
- 563.Dai W., Wang F., He L., Lin C., Wu S., Chen P. Genistein inhibits hepatocellular carcinoma cell migration by reversing the epithelial-mesenchymal transition: Partial mediation by the transcription factor NFAT. Mol Carcinog. 2015;54:301–311. doi: 10.1002/mc.22100. [DOI] [PubMed] [Google Scholar]
- 564.Johnson A.J., Yeh Y.Y., Smith L.L., Wagner A.J., Hessler J., Gupta S. The novel cyclin-dependent kinase inhibitor dinaciclib (SCH727965) promotes apoptosis and abrogates microenvironmental cytokine protection in chronic lymphocytic leukemia cells. Leukemia. 2012;26:2554–2557. doi: 10.1038/leu.2012.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 565.Vishvakarma N.K., Kumar A., Singh S.M. Role of curcumin-dependent modulation of tumor microenvironment of a murine T cell lymphoma in altered regulation of tumor cell survival. Toxicol Appl Pharmacol. 2011;252:298–306. doi: 10.1016/j.taap.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 566.Ghosh A.K., Kay N.E., Secreto C.R., Shanafelt T.D. Curcumin inhibits prosurvival pathways in chronic lymphocytic leukemia B cells and may overcome their stromal protection in combination with EGCG. Clinical Cancer Res. 2009;15:1250–1258. doi: 10.1158/1078-0432.CCR-08-1511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 567.Suzuki Y., Isemura M. Binding interaction between (−)-epigallocatechin gallate causes impaired spreading of cancer cells on fibrinogen. Biomed Res. 2013;34:301–308. doi: 10.2220/biomedres.34.301. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.