Abstract
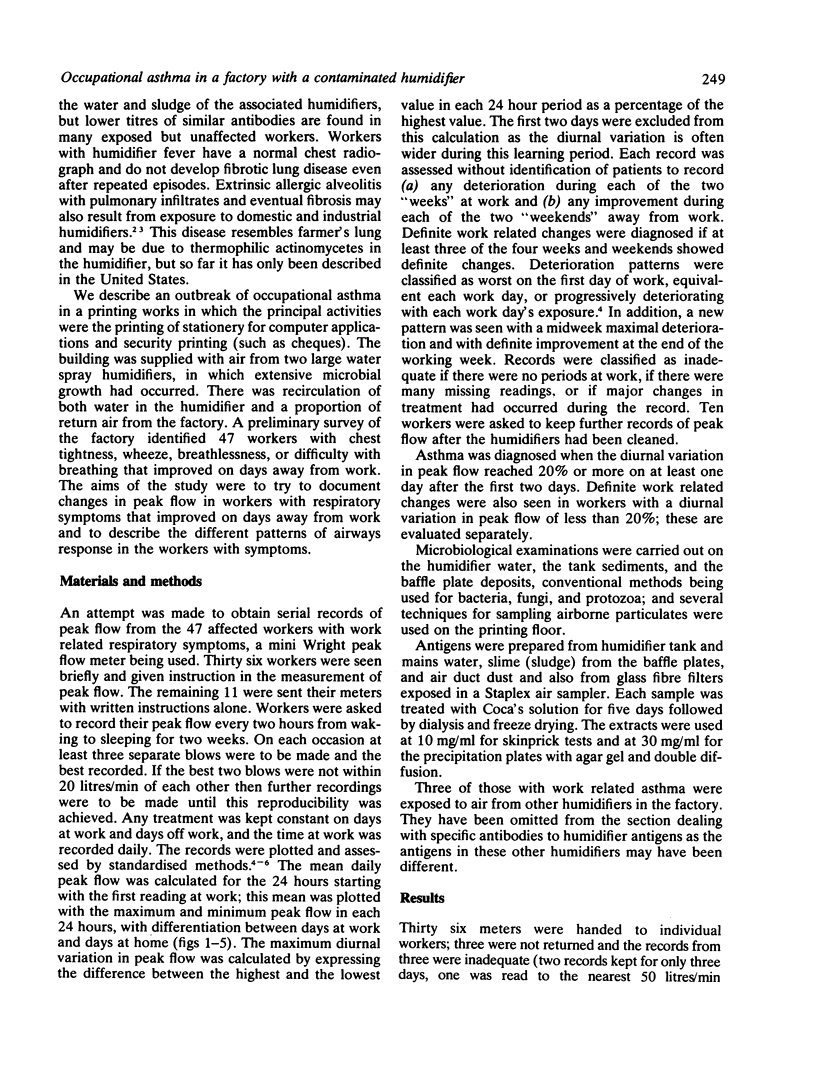
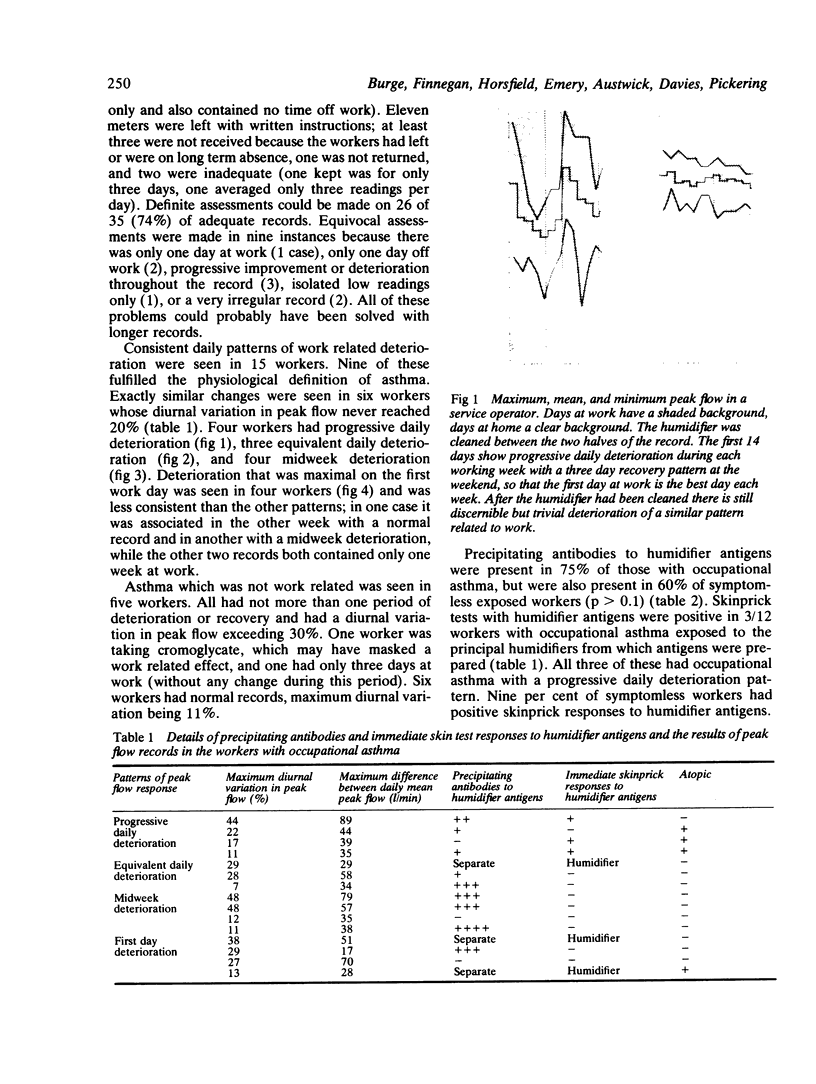
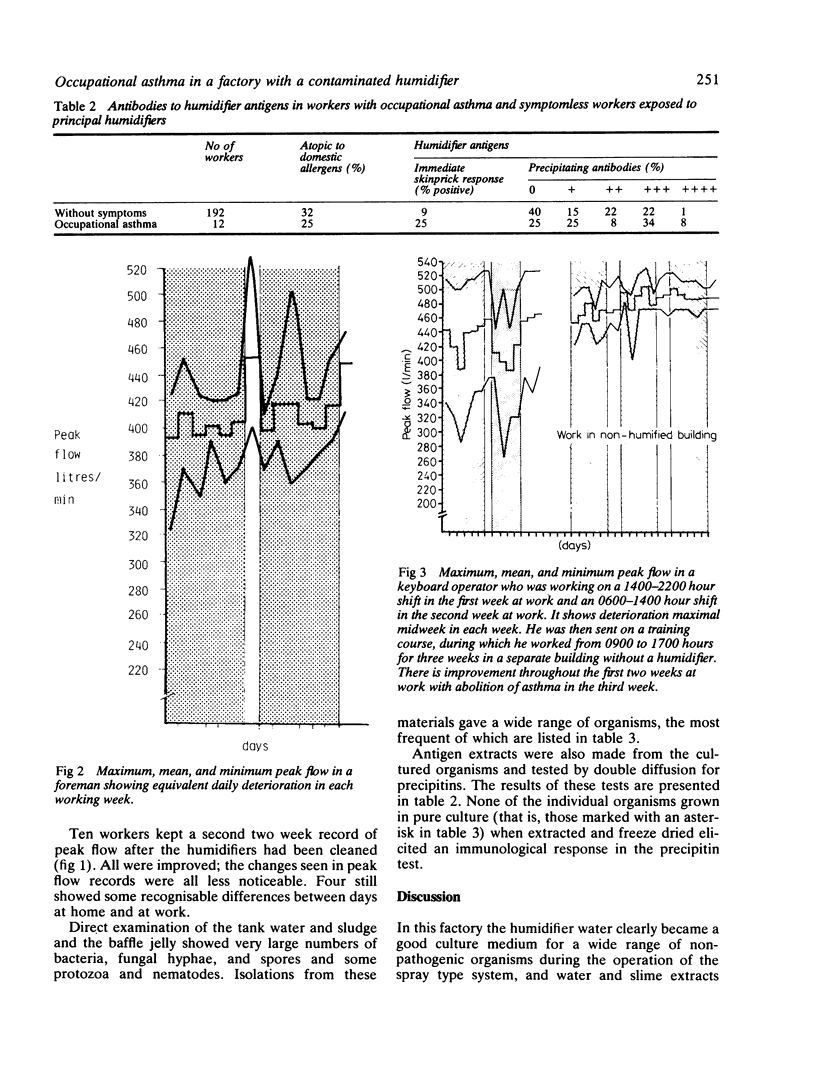
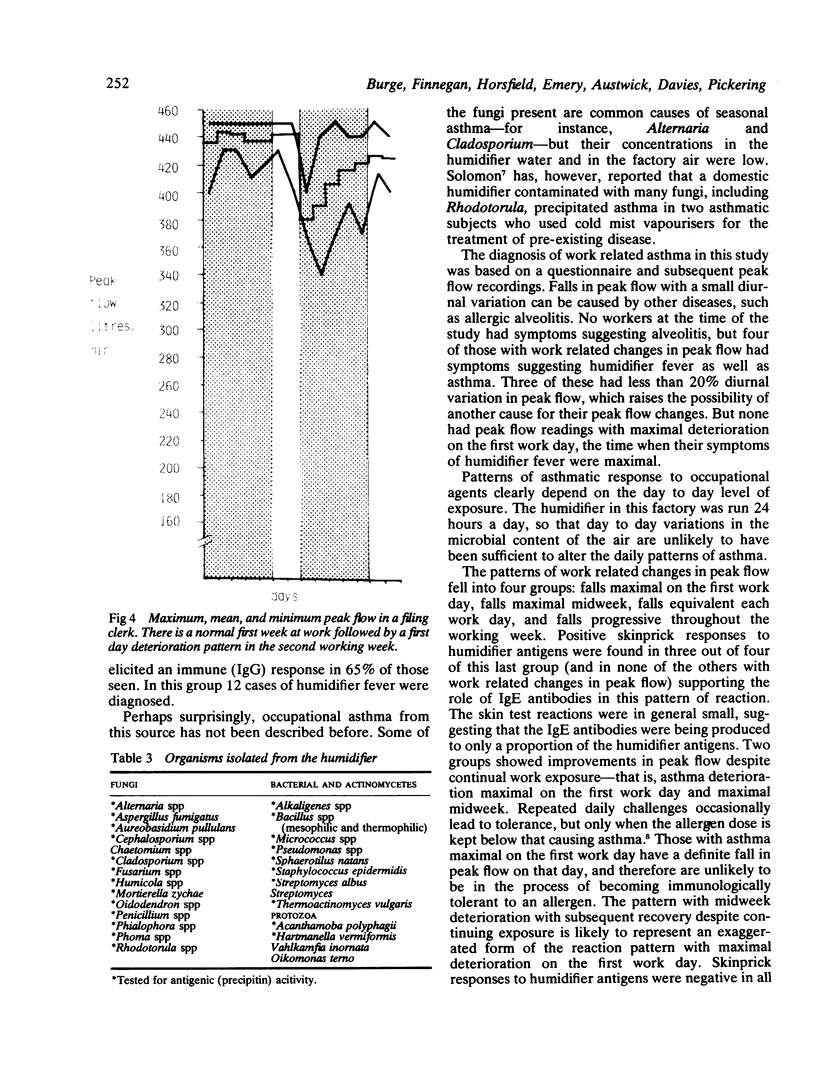
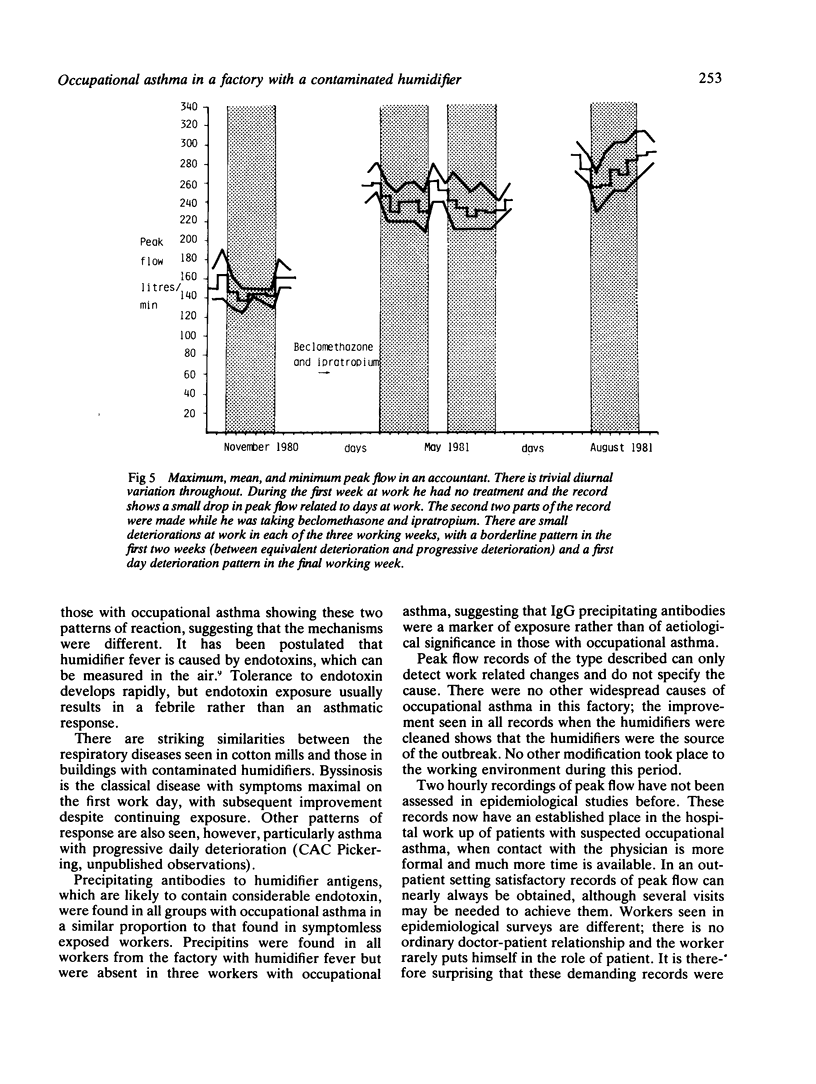
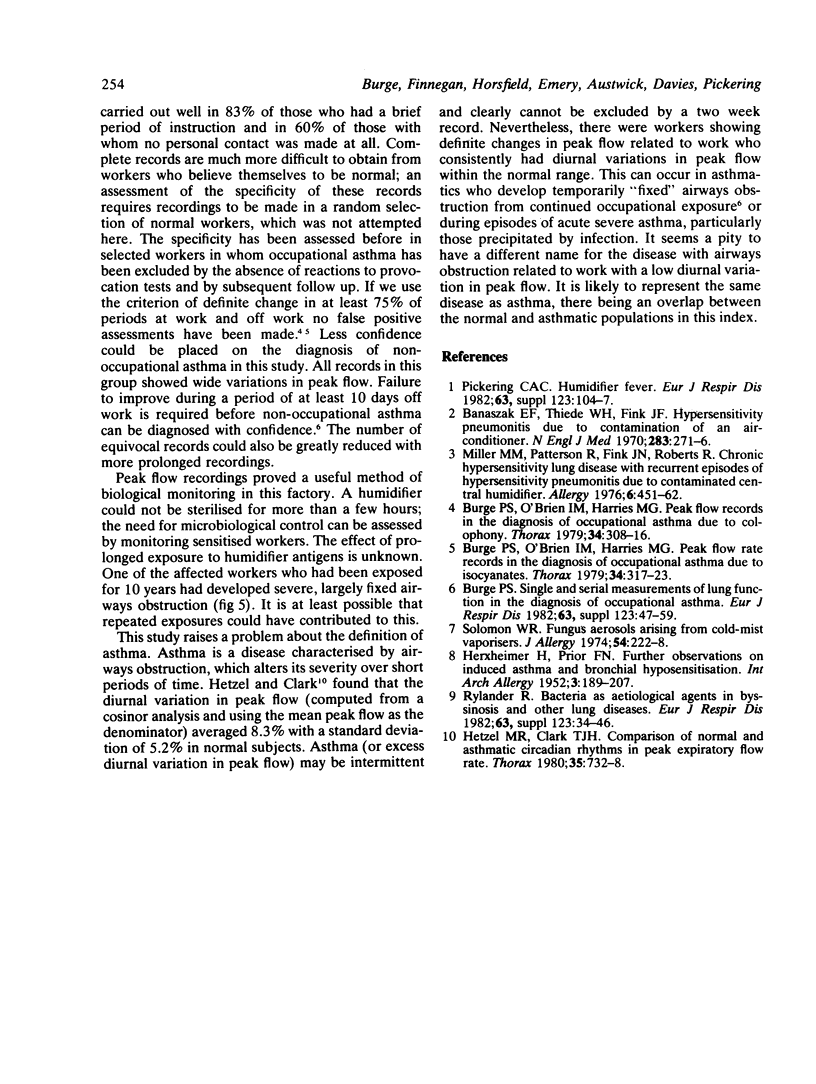
Thirty five printers who had work related wheeze, chest tightness, or breathlessness kept two hourly records of their peak expiratory flow for at least two weeks. They all worked in a factory supplied by air from contaminated humidifiers. The peak flow records showed consistent work related deterioration in 15 workers, nine of whom had a diurnal variation in peak flow exceeding 20%. Ten workers kept further records after the humidifiers had been cleaned, other work practices remaining unchanged. There was substantial improvement in all 10 workers, implying that material from the contaminated humidifier was the cause of the work related changes in peak flow. The patterns of work related changes in peak flow fell into four groups: falls maximal on the first work day, falls maximal midweek, falls equivalent each work day, and falls progressive throughout the working week. Three quarters of this last group had immediate prick test responses to humidifier antigen, which were negative in all the others with work related changes in peak flow. This suggests that the progressive daily deterioration pattern alone is due to an IgE mediated response to humidifier antigens. A large range of microorganisms was identified in the humidifiers. No single microorganism appeared to be the antigen responsible for the precipitating antibody seen in 75% of the study population.
Full text
PDF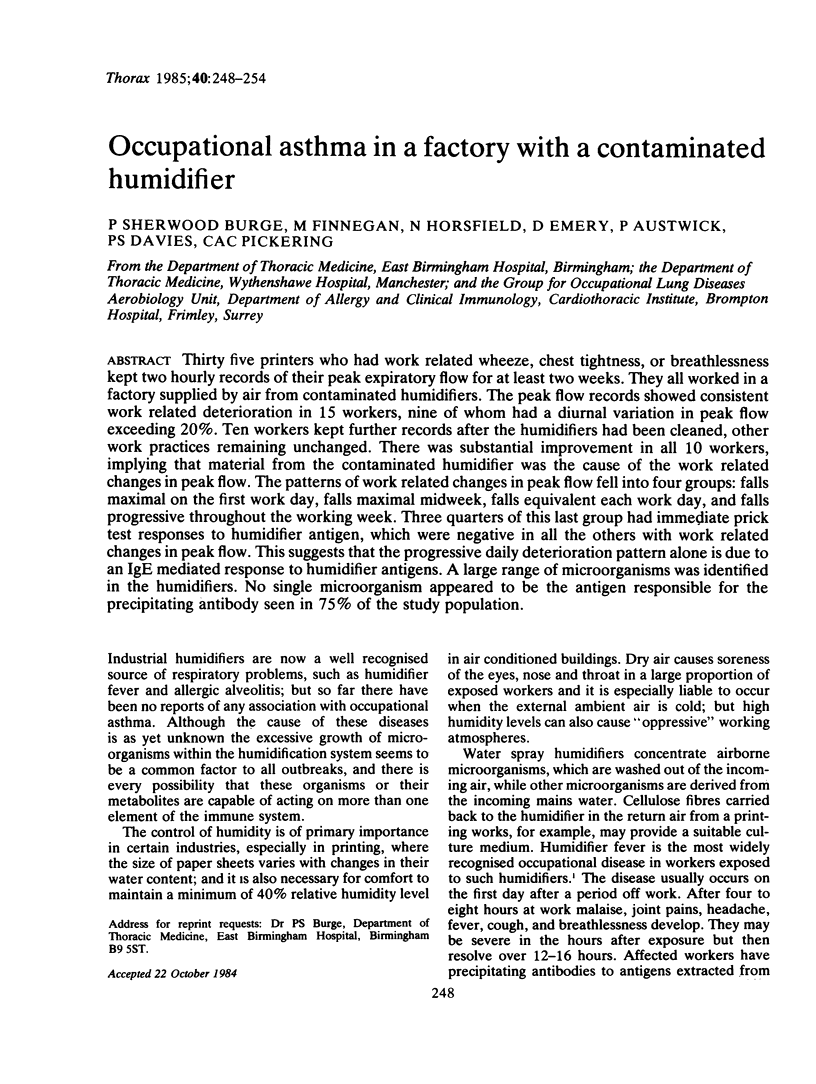
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Banaszak E. F., Thiede W. H., Fink J. N. Hypersensitivity pneumonitis due to contamination of an air conditioner. N Engl J Med. 1970 Aug 6;283(6):271–276. doi: 10.1056/NEJM197008062830601. [DOI] [PubMed] [Google Scholar]
- Burge P. S., O'Brien I. M., Harries M. G. Peak flow rate records in the diagnosis of occupational asthma due to colophony. Thorax. 1979 Jun;34(3):308–316. doi: 10.1136/thx.34.3.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burge P. S., O'Brien I. M., Harries M. G. Peak flow rate records in the diagnosis of occupational asthma due to isocyanates. Thorax. 1979 Jun;34(3):317–323. doi: 10.1136/thx.34.3.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burge P. S. Single and serial measurements of lung function in the diagnosis of occupational asthma. Eur J Respir Dis Suppl. 1982;123:47–59. [PubMed] [Google Scholar]
- HERXHEIMER H., PRIOR F. N. Further observations on induced asthma and bronchial hyposensitization. Int Arch Allergy Appl Immunol. 1952;3(3):189–207. doi: 10.1159/000227963. [DOI] [PubMed] [Google Scholar]
- Hetzel M. R., Clark T. J. Comparison of normal and asthmatic circadian rhythms in peak expiratory flow rate. Thorax. 1980 Oct;35(10):732–738. doi: 10.1136/thx.35.10.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller M. M., Patterson R., Fink J. N., Roberts M. Chronic hypersensitivity lung disease with recurrent episodes of hypersensitivity pneumonitis due to a contaminated central humidifer. Clin Allergy. 1976 Sep;6(5):451–462. doi: 10.1111/j.1365-2222.1976.tb01929.x. [DOI] [PubMed] [Google Scholar]
- Pickering C. A. Humidifier fever. Eur J Respir Dis Suppl. 1982;123:104–107. [PubMed] [Google Scholar]
- Rylander R. Bacteria as etiological agents in byssinosis and other lung disease. Eur J Respir Dis Suppl. 1982;123:34–46. [PubMed] [Google Scholar]
- Solomon W. R. Fungus aerosols arising from cold-mist vaporizers. J Allergy Clin Immunol. 1974 Oct;54(4):222–228. doi: 10.1016/0091-6749(74)90064-5. [DOI] [PubMed] [Google Scholar]