Abstract
The purpose of this cross-sectional descriptive pilot study was to describe daily intake of select nutrients important for efficient wound healing and general health in a sample of older adults (64.25 ± 9.49 years of age) with chronic venous leg ulcers (CVLUs; N = 12), compared to recommended dietary allowances (RDA). Anthropometric data were also collected. Compared to RDA, participants on average consumed lower vitamin C (60.03 ± 49.73 mg/d) and higher sodium (3197.07 ± 1455.04 mg/d), sugar (181.21 ± 115.45 g/d), and saturated fat (33.75 ± 1.06 g/d). They also demonstrated a relatively high plasma n-6/n-3 polyunsaturated fatty acid ratio, a biomarker of inflammation (11.25 ± 1.99). The mean body mass index indicated extreme obesity (41.48 ± 11.47). A multidisciplinary treatment approach that includes routine dietary assessments followed by tailored dietary interventions may improve wound healing and long-term health outcomes in this population.
Keywords: chronic venous leg ulcers, older adults, nutrition
Introduction
Chronic venous leg ulcers (CVLUs) are significant clinical problems affecting approximately 600,000 Americans annually,1 including ~3.6% of people over 65 years of age.2 Moreover, the global incidence of CVLUs is predicted to escalate dramatically, in tandem with the rising numbers of older adults because CVLUs are associated with aging.1 Currently, annual CVLU treatment-related costs to the U.S. health care system are > $3.5 billion, directly related to protracted healing times.1 Only an estimated 50%–65% of CVLUs heal within six months of diagnosis, 20% remain unhealed after two years, and 8% remain unhealed after five years.1 Further, the recurrence rate is nearly 50%.3 Thus, cost-effective adjunct treatment strategies are needed to help prevent or facilitate healing of these problematic wounds.
The pathobiology of CVLUs involves sustained venous hypertension leading to leaky vessels and high levels of activated pro-inflammatory cytokines and proteases in wound microenvironments that contribute to chronic inflammation.1 Although inflammation is the essential initial stage of healing, chronic inflammation prevents or delays subsequent healing stages.4 Treatment regimens for CVLUs include compression therapy (gold standard) and various types of wound dressings targeting excessive drainage and/or bacterial overgrowth.5 Additionally, it is important that adequate levels of oxygen and key nutrients such as vitamin C and zinc reach the site of tissue damage to facilitate reparative processes.6 Patients with chronic wounds may require higher than recommended dietary allowances (RDA) of certain nutrients to expedite healing because of a heightened metabolism triggered by chronic inflammation and increased cellular activity at wound sites.6 Thus, individuals’ overall cardiovascular health and nutritional status affect healing outcomes.6 Unfortunately, the nutritional status of older adults is often suboptimal because of comorbidities, physical limitations, damaged teeth, chewing and swallowing difficulties, multiple medication usage, or limited access to healthy foods due to a lack of social support, transportation, and income.6,7 Malnutrition among older adults has been described as a growing, but still unaddressed, epidemic.8 This could have profound effects on the incidence of chronic wounds and wound healing in the aging population.
Low intake of vitamin C, zinc, and protein has been associated with healing delays in older adults with pressure ulcers.9–12 However, few studies have evaluated the nutritional status of older adults with CVLUs, and the findings have been inconsistent.1,13 Moreover, there are limited data regarding weights of CVLU patients and how obesity may affect wound healing. Thus, the primary purpose of this cross-sectional pilot study was to describe the nutritional profile of a sample of older adults with CVLUs by comparing their average daily intake levels of nutrients known to affect wound healing, inflammation status, and general health to recommendations by public health organizations such as the Institute of Medicine (IOM) dietary reference intake (DRI) and USDA RDA (both called RDA herein). Secondary aims were to describe the group’s anthropometric measures, comorbidities, and dietary supplement use. The main hypothesis was that most participants would not meet national guidelines for daily intake levels of key nutrients important for optimal health and would have high levels of systemic inflammation that collectively could contribute to wound healing delays and other chronic diseases. This pilot study was a preliminary step to generate evidence for future studies to determine if dietary assessments should be a component of standard care for this population and whether dietary interventions in this population could promote healing.
Materials and Methods
Design
This pilot study used a descriptive, cross-sectional design to assess the dietary intake levels of nutrients important for wound healing and general health in a sample of older adults with CVLUs during one study visit wherein they self-reported nutritional data. Sociodemographic data, anthropometric data, plasma polyunsaturated fatty acid (PUFA) data and opinions about dietary supplement use were also collected. Individuals received $100 for participating in the one-visit study.
Potential participants were identified from University Wound Clinic records and approached about the study if they had an existing wound (CVLU) for at least three months, were English-speaking, and were able to sign their own consent. Exclusion criteria included taking fish oil (n-3 PUFAs) supplements or already in a study related to CVLUs. The Institutional Review Board (IRB) approved the study, which was conducted in compliance with ethical rules for human experimentation as stated in the 1975 Declaration of Helsinki.
Setting
The study was conducted in the Clinical Research Center (CRC) of a large university in the Midwest United States. The CRC provided a high-quality, ethical, safe, efficient, and cost-effective environment in which to complete the study protocol.
Participants
Data collected from 12 individuals (64.25 ± 9.49 years of age) who were diagnosed with at least one CVLU were used for analysis. Eighteen patients were approached about the study; 18 met eligibility criteria; 12 were interested in participation; 12 were consented.
Data Collection
After potential participants expressed interest in the study, a confidential screening interview was performed to confirm eligibility. Participants were instructed to consume only clear fluids during the eight hours prior to their one-time study appointment to fulfill plasma PUFA assay requirements. Study details were reviewed again when individuals arrived at the CRC, and time was allowed for questions before a consent form was presented for signature. Sociodemographic, anthropometric, and nutritional supplement data were collected; body mass index (BMI) was calculated; and a blood sample was collected to quantify plasma PUFA levels. Then study participants received instructions on completing the electronic food frequency questionnaire (FFQ) that collected data about nutrient intake from foods.
Sociodemographic and Nutritional Supplement Measures
Participants completed an electronic health and lifestyle questionnaire wherein they self-reported gender, age, income level, years of education, race/ethnicity, nutritional supplement use, and opinions about taking nutritional supplements to improve wound healing.
Nutrient Measures
Food Frequency Questionnaire
An electronic form of the FFQ validated by the Women’s Health Initiative, the VioFFQ (VIOCARE, Inc., Princeton, NJ), was used to collect nutrient data.14 It is a web-based system that allows participants to self-administer the questionnaire using a tablet via internet connection. Participants watched a nine-minute instructional video about portion size and received instruction on VioFFQ completion. The VioFFQ asks questions about type, frequency, and quantity of foods and beverages consumed in the previous 90 days. Bias and precision of the FFQ used in the current study have been assessed by comparing the intake of 30 nutrients estimated from the FFQ with means from four 24-hour dietary recalls and a 4-day food record. For most nutrients, means estimated by the FFQ were within 10% of the records or recalls. Precision, defined as the correlation between the FFQ and the records and recalls, was similar to other FFQs. Energy adjusted correlation coefficients ranged from 0.2 (vitamin B12) to 0.7 (magnesium), with a mean of 0.5. Thus, this FFQ generated nutrient estimates that were similar to those obtained from short-term dietary recall and recording methods.14 CRC Registered Dietitian Nutritionists were available to answer participants’ questions and assist as needed. Data generated included a nutrient analysis of reported diet on a per-day basis. Nutrient databases used include the Nutrition Data System for Research (NDSR), which includes all United States Department of Agriculture (USDA) databases and corresponding consumer, manufacturer, and science review board updates.
Plasma PUFA Data
Plasma PUFAs were analyzed by the well-established gas chromatography/mass spectrometry (GC/MS) method. Lipids were extracted from plasma samples with 2:1 (v/v) chloroform:methanol and 0.24 ml 0.88% KCL.15–17 Fatty acid methyl esters were prepared using tetramethylguanidine at 100°C.16, 17 Fatty acid methyl esters were analyzed by gas chromatography using a 30-m Omegawax™ 320 (Sigma-Aldrich, St. Louis, MO) capillary column. Oven temperature was started at 175°C and increased at a rate of 3°C/min until reaching 220°C. Flow rate of the carrier gas helium was 30 mL/min. Retention times were compared to standards for fatty acid methyl esters (Sigma-Aldrich, St. Louis, MO, and Matreya, LLC, Pleasant Gap, PA). The resultant values were expressed as % composition. This is routinely done to express fatty acid values and widely accepted in the field.15–17
Anthropometric Measures
Height and weight were measured, and BMI was calculated by CRC research nurses. Height was measured using the Harpenden Stadiometer (Holtain Limited, Crymych, Dyfed, UK) to the nearest 0.1 cm. Measurement of stature can be performed accurately and quickly using the Harpenden stadiometer, which delivers results reproducible within ± 0.29 cm.18 Body weight was measured using the Seca 644 digital multifunctional handrail scale, model number 6441321108, made in Hamburg, Germany, to the nearest 0.1 kg. The scale’s accuracy is verified using known masses of 10 kg and 20 kg.19 BMI was calculated as body weight (kg) divided by height (m) squared.
Data Analysis
Descriptive analysis was performed using SPSS version 20.0 (SPSS, Inc., Chicago, IL). Categorical variables were summarized using proportions, and continuous variables were summarized using means, ranges, and standard deviations (SD).
Results
Sociodemographic and Nutritional Supplement Data
In this sample of CVLU patients (n = 12), the mean age was 64.25 ± 9.49 years, and most (10 of 12) were older Caucasian males (Table 1). More than half (7 of 12) reported that they had completed 12 years of formal education. Overall, 5 of 12 participants reported an annual household income at or below the federal poverty line ($15,730 for a two-person household).20
Table 1.
Participant Characteristics
| Characteristic | Participants, n = 12 |
|---|---|
| Age, mean ± standard deviation | 64.25 ± 9.49 |
| Age, range, years | 48–80 |
| Gender: | |
| Male, n | 10 |
| Female, n | 2 |
| Race: | |
| Caucasian, n | 8 |
| African American, n | 3 |
| Other, n | 1 (Creole) |
| Education: | |
| High school graduate, n | 7 |
| Some college, n | 3 |
| College/University graduate, n | 2 |
| Annual household income: | |
| < $10.000, n | 4 |
| $10,000 – $14,999, n | 1 |
| $15,000 – $29,999, n | 3 |
| $30,000 – $44,999, n | 1 |
| $45,000 or more, n | 3 |
All participants (100%) reported that they would consider taking a dietary supplement to improve wound healing (if prescribed), but that cost and potential side effects would affect their final decision. Eight participants (67%) self-reported currently taking a vitamin and/or dietary supplement every day, such as calcium, fish oil, folic acid, ginkgo, iron, vitamin B complex, vitamin C, or vitamin D (Table 2).
Table 2.
Vitamin and Dietary Supplement Use by Participants
| Vitamin/Supplement | Participants, = 12 |
|---|---|
| Currently taking vitamin/supplement | 8 |
| Calcium | 2 |
| Fish oil | 1 |
| Folic acid | 1 |
| Ginkgo | 1 |
| Iron | 1 |
| Multivitamin | 2 |
| Vitamin B | 3 |
| Vitamin C | 1 |
| Vitamin D | 5 |
| Other | 3 |
| Multivitamin with iron | 1 |
| Mass XXX Muscle and Skin Supplement | 1 |
| Not sure | 1 |
| Consider taking dietary supplements to improve wound healing, n (%) | 12 (100) |
Nutrient Data
Food Frequency Questionnaire
The VioFFQ analysis indicated that the average vitamin C intake from foods consumed by this sample was 60.03 ± 49.73 mg/day, which is less than RDA for women (75 mg) and men (90 mg).21 However, on average, participants consumed adequate amounts of zinc (10.78 ± 5.17 mg/day) and protein (71.37 ± 31.32 g/day; Table 3).21 The mean intake of sodium (3.2 ± 1.5 g/day), total saturated fatty acid (33.75 ± 1.06 g/day), and sugar (181.21 ± 115.45 g/day) were all substantially higher than the guidelines.21,22
Table 3.
VioFood Frequency Questionnaire Data (n = 12)
| Nutrient | Mean ± SD | Recommendations |
|---|---|---|
| Vitamin C, mg/day | 60.03 ± 49.73 | 75 for women; 90 for men18 |
| Zinc, mg/day | 10.78 ± 5.17 | 8–1118 |
| Protein, g/day | 71.37 ± 31.32 | 46–5618 |
| Total Sugar, g/day | 181.21 ± 115.45 | ≤ 2522 |
| Sodium, g/day | 3.2 ± 1.5 | 1.2–1.518 |
| Total Saturated Fatty Acids, g/day | 33.75 ± 1.06 | <1627 |
| PUFA, g/day | ||
| EPA+DHA | 0.05±0.04 | 0.521 |
SD = standard deviation
EPA = eicosapentaenoic acid
DHA = docosahexaenoic acid
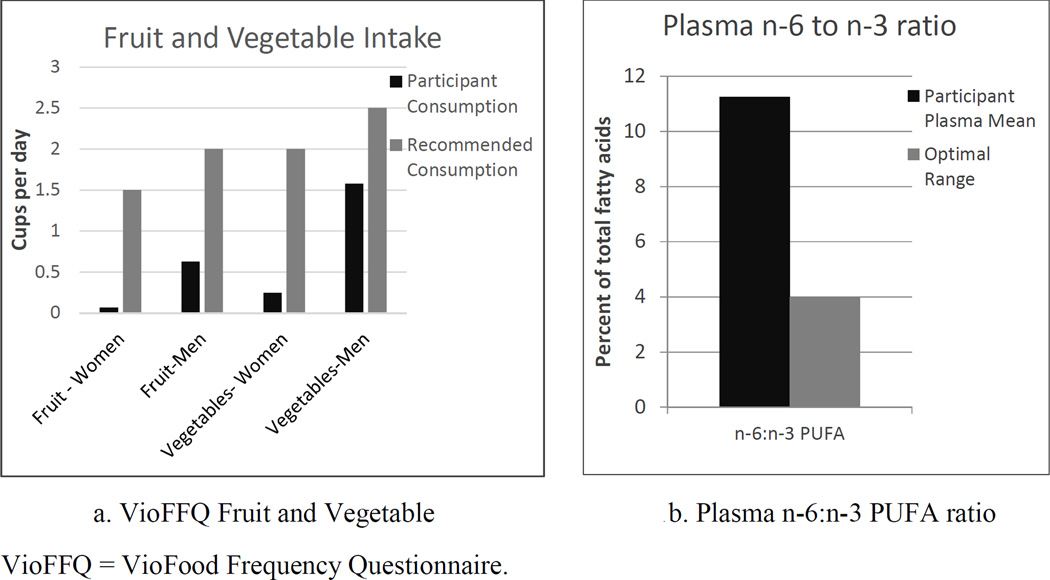
The VioFFQ also measured participants’ daily intake of fruits and vegetables, which contain numerous antioxidants important for health and tissue healing.6 Participants’ average fruit intake was 0.53 ± 0.58 cups/day, which is below recommendations for both women (1.5 cups) and men (2 cups) who are 51 years of age and older and get less than 30 minutes of physical activity per day beyond normal daily activity (Figure 1a).23 Similarly, participants’ average intake of vegetables was 1.33 ± 1.67 cups/day, also below recommendations for women (2 cups) and men (2.5 cups).23
Figure 1.
VioFFQ Fruit and Vegetable Intake and Plasma n-6 to n-3 PUFA Ratio
Also below recommendations (by the Academy of Nutrition and Dietetics) according to VioFFQ data was the combined daily intake (0.05 ± 0.04 g/day) of eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA): two specific n-3 PUFAs found almost exclusively in oily fish and known to be anti-inflammatory and inflammation-resolving.24 The VioFFQ does not allow determination of total n-6 data; therefore, we used blood samples instead to calculate n-6/n-3 ratios.
Plasma PUFAs
Plasma PUFA data are expressed as percent of total PUFAs. The average plasma n-6/n-3 ratio for the group was 11.25 ± 1.99 (Figure 1b). Additionally, on average, n-3 EPA was 0.43 ± 0.14, n-3 DHA was 2.14 ± 0.66, and n-6 was 8.64 ± 2.79.
Anthropometrics and Comorbidities
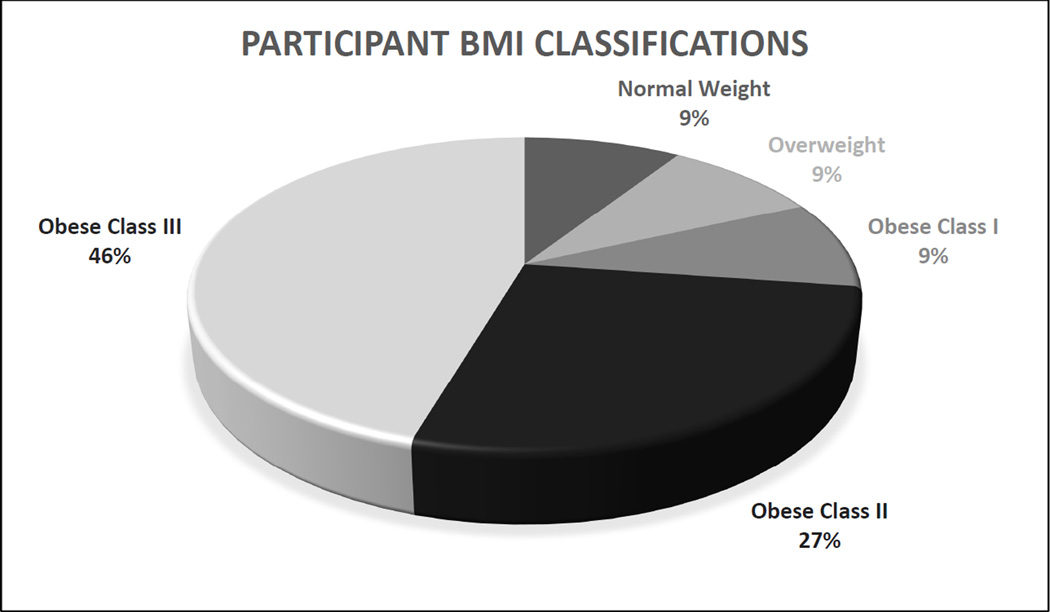
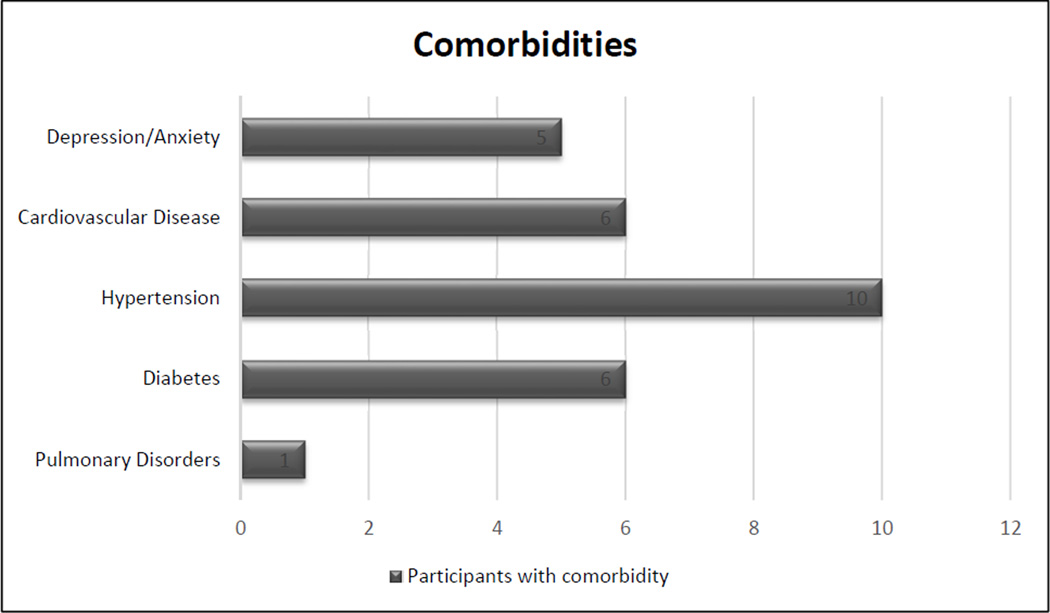
The group’s mean BMI was 41.48 ± 11.47 (Figure 2). One participant did not have data collected for BMI computation. Of the remaining 11, 9 were classified as obese according to the National Institutes of Health (BMI ≥ 30).25 Specifically, five were classified as extremely obese (class III: BMI ≥ 40), three were obese class II (BMI 35.0–39.99), one was obese class I (BMI 30–34.99); one was overweight (BMI 25.0–29.99); and one was of normal weight (BMI 18.5–24.99).25 Participants also were found to have a variety of comorbidities. According to current medical records, 6 of 12 (50%) participants had a diagnosis of diabetes, 6 of 12 (50%) had cardiovascular disease, and 8 of 12 (83.3%) had hypertension. Nearly 42% (5 of 12) were taking medications for depression and/or anxiety, and 1 of 12 (8.3%) was being treated for pulmonary disease (Figure 3).
Figure 2.
Participants’ Body Mass Index (BMI) Classifications (n = 11)
Figure 3.
Comorbidities of Participants (n = 12)
Discussion
This study measured intake levels of key nutrients important for wound healing and overall health in a population of older adults with a type of chronic wound. This study of a sample of older adults with CVLUs found that, on average, the group was consuming lower than recommended amounts of vitamin C, but adequate amounts of zinc and protein, according to IOM guidelines, and lower than recommended amounts of the n-3 PUFAs EPA and DHA according to Academy of Nutrition and Dietetics guidelines. The findings of low vitamin C intake are aligned with previous studies reporting that many patients with chronic wounds such as pressure ulcers are vitamin C-deficient.9,11
The study data also indicated that participants were consuming several nutrients in excess of RDA, and that could be detrimental to health over time. For example, the group’s average daily intake of sodium was more than double IOM guidelines.21 It was also above the more lenient recommendations by the USDA Dietary Guidelines for Americans (DGA) that state Americans should reduce daily sodium intake to < 2,300 mg and ≤ 1,500 mg if a person is 51 or older or any age if he/she is African American or has hypertension, diabetes, or chronic kidney disease.26 Consistent excessive consumption of sodium contributes to the development and/or exacerbation of hypertension, which is a major risk factor for several chronic diseases, including cardiovascular disease, congestive heart failure, and kidney disease.21
Additionally, the group’s average saturated fat intake (33.75 ± 1.06 g/day) was more than double the advised allowance of < 16 g/day established by the American Heart Association.27 These findings are aligned with the National Health and Nutrition Examination Survey (NHANES) 2011–2012 report What We Eat in America, which found high intake levels of saturated fat (23.6 g/day) and sodium (3,236 mg/day) in males and females greater than 50 years of age.28 A diet containing high quantities of saturated fat is linked to an increased risk of cardiovascular disease.27
Further, on average, the current study’s participants consumed over seven times the maximum recommended daily amount of free (added) sugar recently proposed by the WHO.22 Excessive sugar consumption is associated with a nutrient-deficient diet, weight gain and obesity, and an increased risk of developing cardiovascular disease and diabetes--risk factors for wound healing complications.22 Excessive zinc consumption has also been found to compromise the wound healing process.29 Adequate, but not excessive, amounts of zinc are fundamental for the wound healing process.29
Data also revealed that study participants were eating fewer daily servings of fruits and vegetables than the USDA advises.23 There is mounting evidence that a diet rich in fruits and vegetables reduces risk for heart disease, stroke, obesity, type 2 diabetes, and hypertension and may defend against certain cancers.10 Our results were similar to previous studies reporting that few older adults in the U.S. meet intake recommendations for vegetables, fruits, dairy, meats, and grains.7,10,13
Other nutrients important to consider in terms of inflammation status are the n-6 and n-3 PUFAs, which generate eicosanoids that regulate inflammation throughout the body.30 Generally, eicosanoids generated from n-6 PUFAs have stronger pro-inflammatory actions than those generated from n-3 PUFAs.30 This study’s blood plasma findings indicated that participants had relatively high plasma n-6/n-3 ratios, implying that they were consuming foods containing high amounts of n-6 PUFAs relative to n-3 PUFAs. These findings are aligned with previous U.S. studies reporting n-6/n-3 ratios ranging from 10:1–20:1 in the general population.30–32 High n-6/n-3 ratios, common in Western diets, are associated with chronic inflammatory conditions such as cardiovascular disease and rheumatoid arthritis, while lower n-6/n-3 ratios are linked to inflammation resolution and improvements in inflammation-related disorders.32 More balanced ratios of 2:1 to 4:1 are recommended for optimal health.32 Importantly, studies have shown that increasing n-3 PUFA intake, especially EPA and DHA (the most biologically active in terms of inflammation resolution), can help balance high n-6/n3 ratios.32,33 Thus, when indicated, EPA and DHA supplementation may help reduce the chronic inflammation associated with CVLUs.
Most participants in this study were classified as obese. Obesity is associated with increased production of proinflammatory cytokines by adipocytes and subsequently high levels of systemic inflammation.34 Moreover, obesity increases risk for developing and/or exacerbating cardiovascular disease and diabetes, risk factors for wound healing problems.25 Cardiovascular disease, diabetes, and pulmonary disorders (diagnoses noted in this study’s sample) can impede tissue oxygenation, which slows the healing process.34 Cardiovascular disease is also associated with increased numbers of leukocytes in the lower extremities and high levels of systemic inflammation, which also contribute to healing delays.4 Moreover, this study’s data indicate that almost half of the sample had concomitant diagnoses of depression and/or anxiety, which have been associated with malnutrition and subsequent impairment of tissue regeneration.10
Dietary elements such as vitamin C, zinc, and protein are known to impact wound healing and thus may be important to evaluate as part of a nutritional assessment to determine in people with CVLUs. Data from the current study did indicate that the sample was consuming lower than recommended intake levels of vitamin C. A nutritional assessment would also help identify other nutrient issues (high sodium, high sugar, etc.) which could indirectly affect healing through subsequent effects on the cardiovascular system. This sample had high intake of sodium, sugar, and fat.
Many factors such as poor nutrition contribute to the development and healing of chronic wounds such as CVLUs. Pilot data from this study profiling the nutritional status of older adults with CVLUs suggest that dietary assessments could help identify patients likely to benefit from nutritional interventions to improve overall health and wound healing. This supports the need for nutritional assessments, which might be important in guiding the plan of care, which could include nutritional interventions. Nurses and registered dieticians on the healthcare team together could initiate and implement these assessments and interventions.
Limitations
Because this was a descriptive study using a small sample and a single data collection point, causality cannot be determined. Self-report was used. Additionally, the sample consisted primarily of Midwestern Caucasian CVLU patients of lower socioeconomic status. These factors limit the generalizability of the findings because there is variability in dietary patterns across races, socioeconomic levels, and regions of the country.7
Conclusion
In summary, this study found that some older adults with CVLUs are not consuming adequate amounts of select nutrients needed for effectual wound healing. Conversely, they are eating excessive amounts of nutrients known to prolong heightened inflammation (n-6 PUFAs), which could contribute to healing delays because chronic inflammation is a characteristic of CVLUs. Further, they are at increased risk for developing or exacerbating other chronic diseases because of high BMIs and dietary intake that is low in fruits and vegetables, and high in sodium, saturated fat, and sugar. Though nutrition is only one of many factors that impact the complex process of wound healing, the current study’s findings provide evidence that dietary assessments can inform the planning of treatment strategies for older adults with CVLUs to facilitate weight loss/gain and optimize the wound environment for healing. Additional research is needed to validate the findings in a larger, more diverse population, evaluate effects of specific nutritional interventions on CVLU healing (e.g., balancing n-6/n-3 ratios with n-3 PUFA supplementation), and address barriers that can limit older adults’ intake of healthy foods. Obtaining dietary assessments and promoting nutrient-rich diets and strategies for reaching a healthy weight may improve the general health and healing outcomes for older adults with CVLUs, which may in turn reduce health care costs. Nurses and registered dieticians could facilitate these assessments and interventions.
ACKNOWLEDGMENTS
Funding was provided by the National Institutes of Health Clinical and Translational Science Award to The Ohio State University UL1RR025755 and UL1TR001070 (JM).
Sponsor’s Role: None.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: None.
References
- 1.Hankin CS, Knispel J, Lopes M, Bronstone A, Maus E. Clinical and cost efficacy of advanced wound care matrices for venous ulcers. J Manag Care Pharm. 2012;18(5):375–384. doi: 10.18553/jmcp.2012.18.5.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moor A, Vachon DJ, Gould LJ. Proteolytic activity in wound fluids and tissues derived from chronic venous leg ulcers. 2009:832. doi: 10.1111/j.1524-475X.2009.00547.x. [DOI] [PubMed] [Google Scholar]
- 3.McDaniel HB, Marston WA, Farber MA, et al. Recurrence of chronic venous ulcers on the basis of clinical, etiologic, anatomic, and pathophysiologic criteria and air plethysmography. Journal of Vascular Surgery. 2002;35(4):723–728. doi: 10.1067/mva.2002.121128. [DOI] [PubMed] [Google Scholar]
- 4.Raffetto JD. Inflammation in chronic venous ulcers. Phlebology. 2013;28(Suppl 1):61–67. doi: 10.1177/0268355513476844. [DOI] [PubMed] [Google Scholar]
- 5.Tang JC, Marston WA, Kirsner RS. Wound healing society (WHS) venous ulcer treatment guidelines: What's new in five years? Wound Repair Regen. 2012;20(5):619–637. doi: 10.1111/j.1524-475X.2012.00815.x. [DOI] [PubMed] [Google Scholar]
- 6.MacKay D, Miller AL. Nutritonal support for wound healing. Alternative Medicine Review. 2003;8(4):359–377. [PubMed] [Google Scholar]
- 7.Ervin RB. Healthy eating index scores among adults, 60 years of age and over, by sociodemographic and health characteristics: United states, 1999–2002. Adv Data. 2008:1–16. (395)(395) [PubMed] [Google Scholar]
- 8.The Gerontological Society of America. Malnutrition a hidden epidemic among elders. ScienceDaily. 2014 Dec 18; [Google Scholar]
- 9.Gray M, Whitney JD. Does vitamin C supplementation promote pressure ulcer healing? Journal of Wound Ostomy & Continence Nursing. 2003;30(5):245–249. doi: 10.1067/mjw.2003.140. [DOI] [PubMed] [Google Scholar]
- 10.Heyman H, DE J, Meijer EP, Schols J. Benefits of an oral nutritional supplement on pressure ulcer healing in long-term care residents. J Wound Care. 2008;17(11):476. doi: 10.12968/jowc.2008.17.11.31475. [DOI] [PubMed] [Google Scholar]
- 11.Langer G, Schloemer G, Knerr A, Kuss O, Behrens J. Nutritional interventions for preventing and treating pressure ulcers. Cochrane Database Syst Rev. 2003;4(4) doi: 10.1002/14651858.CD003216. [DOI] [PubMed] [Google Scholar]
- 12.Brewer RD, Jr, Leal JF, Mihaldzic N. Preliminary observations on the effect of oral zinc sulfate on the healing of decubitus ulcers. Proc Annu Clin Spinal Cord Inj Conf. 1966;15:93–96. [PubMed] [Google Scholar]
- 13.Legendre C, Debure C, Meaume S, Lok C, Golmard JL, Senet P. Impact of protein deficiency on venous ulcer healing. Journal of Vascular Surgery. 2008;48:3688–3693. doi: 10.1016/j.jvs.2008.04.012. [DOI] [PubMed] [Google Scholar]
- 14.Patterson RE, Kristal AR, Tinker LF, Carter RA, Bolton MP, Agurs-Collins T. Measurement characteristics of the Women’s health initiative food frequency questionnaire. Ann Epidemiol. 1999;9(3):178–187. doi: 10.1016/s1047-2797(98)00055-6. [DOI] [PubMed] [Google Scholar]
- 15.Folch J, Lees M, Sloane-Stanley G. A simple method for the isolation and purification of total lipids from animal tissues. J Biol Chem. 1957;226(1):497–509. [PubMed] [Google Scholar]
- 16.Shantha NC, Decker E, Hennig B. Comparison of methylation methods for the quantitation of conjugated linoleic acid isomers. J AOAC Int. 1993:76. [Google Scholar]
- 17.Kiecolt-Glaser JK, Epel ES, Belury MA, et al. Omega-3 fatty acids, oxidative stress, and leukocyte telomere length: A randomized controlled trial. Brain Behav Immun. 2013;28:16–24. doi: 10.1016/j.bbi.2012.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Renstrom SB, Andersen CS, Pedersen CH, Madsen FF. Correct measurement of height is important when assessing lung function values. Dan Med J. 2012;59(2):A4376. [PubMed] [Google Scholar]
- 19.SECA Medical Measuring Systems and Scales. SECA 664. https://us.secashop.com/products/multifunctional-and-wheelchair-scales/seca-644/6441321108. Updated 2015.
- 20.U.S. Department of Health and Human Services. 2014 poverty guidelines. Office of the Assistant Secretary for Planning and Evaluation. 2014 Updated periodically in the Federal Register by the U.S. Department of Health and Human Services under the authority of 42 U.S.C. 9902(2).
- 21.Hellwig JP, Otten JJ, Meyers LD. Dietary reference intakes: The essential guide to nutrient requirements. National Academies Press; 2006. [Google Scholar]
- 22.World Health Organization. WHO opens public consultation on draft sugars guideline. http://www.who.int/mediacentre/news/notes/2014/consultation-sugar-guideline/en/. Updated 20142014. [PubMed]
- 23.United States Department of Agriculture. ChooseMyPlate.gov. http://www.choosemyplate.gov/food-groups/. Updated 20102014.
- 24.Vannice GRH. Position of the academy of nutrition and dietetics: dietary fatty acids for healthy adults. J Acad Nutr Diet. 2014;114:136–153. doi: 10.1016/j.jand.2013.11.001. [DOI] [PubMed] [Google Scholar]
- 25.National Institutes of Health. Classification of overweight and obesity by BMI, waist circumference, and additional disease risk. National Heart, Lung, and Blood Institute. 2014 [Google Scholar]
- 26.U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary guidelines for Americans, 2010. 7th Edition. Washington, DC: U.S. Government Printing Office; 2010. Dec, [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.American Heart Association. Know your facts- cholesterol. http://www.heart.org/HEARTORG/Conditions/Cholesterol/PreventionTreatmentofHighCholeste rol/Know-Your-Fats_UCM_305628_Article.jsp. Updated 20142014.
- 28.U.S. Department of Agriculture, Agricultural Research Service. What we eat in America. NHANES; 2014. Nutrient intake from food: Mean amounts consumed per individual, by gender and age; pp. 2011–2012. [Google Scholar]
- 29.Gray M. Does oral zinc supplementation promote healing of chronic wounds? Wound, Ostomy and Continence Nurses Society. 2003;30:295–299. doi: 10.1016/S1071. [DOI] [PubMed] [Google Scholar]
- 30.McDaniel JC, Massey K, Nicolaou A. Fish oil supplementation alters levels of lipid mediators of inflammation in microenvironment of acute human wounds. Wound Repair and Regulation. 2011;19:189–200. doi: 10.1111/j.1524-475X.2010.00659.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Simopoulos AP. Importance of the omega-6/omega-3 balance in health and disease: Evolutionary aspects of diet. World Rev Nutr Diet. 2011;102:10–21. doi: 10.1159/000327785. [DOI] [PubMed] [Google Scholar]
- 32.Simopoulos AP. The importance of the omega-6/omega-3 fatty acid ratio in cardiovascular disease and other chronic diseases. Exp Biol Med (Maywood) 2008;233(6):674–688. doi: 10.3181/0711-MR-311. [DOI] [PubMed] [Google Scholar]
- 33.Grenon SM, Owens CD, Alley H, et al. n-3 polyunsaturated fatty acids supplementation in peripheral artery disease: The OMEGA-PAD trial. Vasc Med. 2013;18(5):263–274. doi: 10.1177/1358863X13503695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guo S, Dipietro LA. Factors affecting wound healing. J Dent Res. 2010;89(3):219–229. doi: 10.1177/0022034509359125. [DOI] [PMC free article] [PubMed] [Google Scholar]