Abstract
Young men who have sex with men (MSM) are substantially impacted by HIV/AIDS, and most new infections occur in serious romantic dyads. Young people experience substantial psychosocial and neurocognitive change between adolescence and emerging adulthood which impacts engagement in risk behaviors. We aimed to examine developmental change in the association between sexual partnership characteristics and condomless anal intercourse (CAI). Data were taken from an analytic sample of 114 YMSM from a longitudinal study of lesbian, gay, bisexual and transgender youth with 4-year follow-up. Rates of CAI were approximately 12 times higher in serious compared to casual partnerships, but this effect diminished in size over time. Partner age differences and violence were associated with more CAI, and these associations strengthened across development. Characteristics of serious relationships (e.g., power dynamics) were also examined. We discuss the need for HIV prevention strategies that address dyadic influences on CAI during this critical developmental period.
Keywords: young men who have sex with men, HIV/AIDS, romantic relationships, developmental change
INTRODUCTION
Men who have sex with men (MSM) are substantially impacted by HIV/AIDS in the United States (1), and this burden is especially pronounced among adolescent and young adult MSM (YMSM). In 2011, YMSM accounted for 77% of new HIV infections among all 13–24 year olds in the United States, which reflects a dramatic disparity between YMSM and other youth populations. Furthermore, YMSM are the only risk group in which rates of new infections are increasing (1, 2). Currently, there is a limited understanding of how HIV risk and the relationships of YMSM change across development, which would allow for more precise developmental tailoring of HIV prevention programs that target dyadic influences on risk.
In 2009, Sullivan and colleagues (3) published the striking finding that an estimated 68% of new HIV infections in MSM occurred in the context of serious relationships or main sex partnerships, and for YMSM (ages 18–29) this proportion was estimated to be 79–84%. These findings led to a paradigm shift in terms of what the field defined as a “high risk” sexual partnership, as much of the previous literature identified casual sex encounters as the highest risk for HIV acquisition (4, 5). Extant research indicates that both adult and YMSM are more likely to have condomless anal intercourse (CAI) with main or serious partners compared to casual sex partners (2, 6–9). In fact, a recent longitudinal study found that the rate of unprotected sex was 79% lower with casual dating partners relative to serious relationships, 84% lower with repeated sex partners (sleeping with but not dating), and 97% lower with unknown or anonymous partners (10). This lower rate of condom use in serious relationships makes intuitive sense, and evidence suggests that YMSM stop using condoms in serious relationships to express trust and intimacy and because they perceived their relationship to be monogamous (11). Unfortunately, many YMSM are unaware that they are HIV-infected and therefore perceive the risk of HIV transmission in their relationships to be low. In 2011, the CDC estimated that 51% of HIV-infected YMSM ages 18–24 were unaware of their status (12), which means that many HIV-infected YMSM may unknowingly put their serious partners at risk for HIV.
Adolescence (~age 13–17) and emerging adulthood (~age 18 to mid-20s) are periods of rapid and profound change (13, 14), including initiation of sexual behavior (15). Neurologically, the cognitive control system does not fully mature until the end of emerging adulthood (16), and adolescents and emerging adults have associated difficulties engaging in long-term planning and inhibiting impulsive behavior. This is also a period of rapid psychosocial development. One of the primary tasks of this period is the development of romantic relationship skills, and as a result, emerging adult relationships differ substantially from adult relationships. Such differences have important implications for HIV risk. For example, emerging adults have higher rates of primary partner turnover (17), which in concert with higher rates of CAI with serious partners, would provide more opportunities for HIV transmission if partners are not aware of their HIV status.
At the same time, romantic relationships provide myriad valuable tangible and intangible benefits (18–20), including promoting health and well-being by satisfying needs for intimacy and social connection (21) and increasing social support (22). However, YMSM experience delays in normative achievement of relationship milestones (e.g., age of first romantic partner) (23–26) due to lack of available partners at younger ages (27). Without the opportunity to build relationship skills during this critical developmental period, YMSM may lack the skills needed to build and maintain healthy relationships (e.g., effective communication), navigate power differentials in relationships (e.g., partner age differences), and make effective decisions about HIV risk reduction (27, 28).
Beyond simply being in a serious romantic relationship, there are several other factors that may contribute to HIV transmission risk in the sexual partnerships of YMSM. Research suggests that having older partners is associated with a higher likelihood of engaging in CAI (5, 10, 29), as well as a higher likelihood of HIV infection (30), particularly among Black YMSM (29, 31). Given that prevalence of HIV increases with age and is highest among adults aged 35– 54 (32), YMSM who have sex with older partners face higher per-sex contact transmission risk (29–31, 33). If YMSM are simultaneously more likely to have CAI with their older partners, as evidence has suggested (10, 31), then sexual partnerships between YMSM and older partners may be potentiating higher rates of HIV incidence among YMSM. Experiencing intimate partner violence (IPV) is not uncommon among young and adult MSM (34–36), and several studies have identified IPV as an important determinant of HIV risk in young and adult MSM (9, 35, 37–41). Experiencing such IPV (i.e., threats, physical violence, and forced sex) may dissuade YMSM from asserting condom use due to power differentials and/or fear of violence.
The relationship between Internet partner-seeking and engagement in sexual risk behavior is much less clear. Several studies from the early 2000s documented evidence of a link between meeting sexual partners online and engagement in sexual risk behavior, but several more recent studies found either no relationship between these variables or a negative relationship, such that meeting partners online was associated with less sexual risk behavior (for a review, see 42). One explanation for these divergent findings is that there may not be a causal relationship between Internet partner-seeking and sexual risk. Instead, young and adult MSM who have more condomless sex on average may use the Internet as an efficient means to find partners with whom to engage in condomless acts (43–48). Another possible explanation is that there is an association between Internet partner-seeking and sexual risk behavior for some MSM but not others. It may be that there are developmental differences in this association, but this has not been examined extensively in the literature.
Within romantic relationships (as opposed to casual sex partnerships), several other relationship characteristics have also been found to contribute to rates of CAI among YMSM, including expressing a stronger desire for the relationship to last, partner sexual concurrency, and having less power in the relationship (9, 10). Wanting one’s relationship to last has been found to be associated with higher rates of CAI with serious relationship partners (9). This likely results from the desire to build emotional closeness and intimacy with one’s partner, and this is corroborated by the finding that YMSM often stop using condoms in their relationships to express trust, commitment and intimacy (11). Conversely, believing that one’s serious partner was having concurrent sexual partners outside the relationship has been found to be associated with less CAI in the relationship (9, 10). Regardless of whether the dyad has a formal arrangement allowing for outside sexual partners, it is not surprising that rates of CAI are lower in dyads in which members have concurrent sexual partners given that this increases risk for HIV and other STIs. Finally, certain indicators of power differentials within serious relationships have been examined as predictors of CAI. In one study, YMSM reported higher rates of CAI with partners that “usually got their way” in arguments or other disagreements (9).
Our own work has recently documented that partnership-level influences on sexual risk behavior change as YMSM move from adolescence to emerging adulthood. More specifically, we found important developmental change for the effects of alcohol and substance use before sex on rate of CAI change in YMSM (49). The current study aimed to expand upon this work and examine developmental changes in the influence of sexual partner and relationship characteristics on sexual risk behavior in the same longitudinal sample of YMSM with 4-year follow-up that spans the developmental stages of adolescence and emerging adulthood (ages 16–25). We made the following hypotheses: 1) averaging across the entire follow-up period, higher rates of CAI would occur in serious relationships (relative to casual), with older partners, and in relationships characterized by physical and sexual IPV (we hypothesized no effect for meeting partners online); and 2) based on substantial neurocognitive and psychosocial change that occurs during adolescence and emerging adulthood (13, 14, 16), the influence of serious relationships, older partners and IPV on CAI would decrease across development. We anticipated no developmental change in the effect of having online partners on CAI.
METHODS
Participants
Participants were a subset of YMSM from a longitudinal study of LGBT youth from the Chicago area (ages 16–20 at baseline; N = 118). The largest percentage of YMSM identified as Black/African-American (48.4%), followed by White (18.9%), Latino/Hispanic (12.3%), Multiracial (11.5%), Asian/Pacific Islander (2.5%), and Other (6.5%). In terms of self-reported sexual orientation, 65.6% identified as gay, 23.0% bisexual, 3.3% heterosexual, and 8.1% other (i.e., questioning, queer, unsure) at baseline interview. Mean age of the sample at baseline was 18.53 (SD = 1.21) and 23.0% were under age 18. Participants self-reported their age and date of birth at baseline, but identification checks conducted at later waves of data collection resulted in an adjusted sample size. Table 1 displays the full demographic description of the sample.
Table 1.
Description of YMSM sample at baseline (N=118) and the 48th month follow-up (N=92)
|
N (%) |
||
|---|---|---|
| Baseline | 48th month follow-up |
|
| Gender Identity | ||
| Male | 102 (87.2%) | 76 (82.6%) |
| Transgender or Female | 15 (12.8%) | 14 (15.2%) |
| Sexual Orientation | ||
| Gay | 79 (67.5%) | 64 (69.6%) |
| Bisexual | 27 (23.1%) | 16 (17.4%) |
| Questioning/Unsure/Other | 11 (9.4%) | 9 (9.8%) |
| Race/Ethnicity | ||
| White | 23 (19.5%) | 17 (18.5%) |
| Black | 53 (44.9%) | 45 (48.9%) |
| Latino/a | 16 (13.6%) | 11 (12.0%) |
| Other | 26 (22.0%) | 19 (20.7%) |
| Living Situation | ||
| Living with parents | 64 (54.7%) | 27 (29.7%) |
| Other stable housing | 41 (35.0%) | 58 (63.7%) |
| Unstable housing | 12 (10.3%) | 6 (6.6%) |
| Highest Education | ||
| Partial high school or less | 45 (38.5%) | 14 (15.4%) |
| High school graduate | 41 (35.0%) | 28 (30.8%) |
| Partial college | 24 (20.5%) | 26 (28.6%) |
| College graduate | 7 (6.0%) | 23 (25.3%) |
Note. Demographic data was missing for one participant at baseline. Sample sizes vary for demographic items at the 48th month follow-up due to an additional response option (“I don’t want to answer this question”).
Procedure and Design
We employed an accelerated longitudinal design involving a baseline interview and six follow-up waves over four years (50). A modified respondent driven sampling approach (51) was used to recruit participants that involved an initial convenience sample (i.e., flyers in neighborhoods frequented by LGBT youth and college listserves; 38%) and subsequent waves of incentivized peer recruitment (62%). Participants were paid $25 to $40 for participation at each time point. At each visit, participants completed self-report measures of health behaviors, mental health, and psychosocial variables. Data for analyses were from seven waves (2007–2012; baseline and 6−, 12−, 18−, 30−, 42−, and 48-month follow-up), and retention at each wave for the full sample was 85%, 90%, 79%, 77%, 82%, and 83%, respectively. Retention rates may differ from previous reports based on differences between analytic samples. The Institutional Review Boards approved this protocol.
Measures
Demographics
Baseline demographics questionnaire assessed participant age, birth sex, race/ethnicity, self-reported sexual orientation, living situation, and highest achieved level of education.
Sexual risk behavior
The HIV-Risk Assessment for Sexual Partnerships (H-RASP; 52) is a computerized self-administered interview designed to assess sexual behavior and associated situational/contextual variables at the level of the sexual partnership. The sexual risk behavior outcome variable used in these analyses was a count of the total number of CAI acts within each partnership with another male.
Relationship status and characteristics of serious relationships
The H-RASP prompted participants to identify the relationship status of each sexual partnership reported by categorizing it into either a serious (coded 1) or casual (coded 0) relationship. If the relationship was categorized as serious, then participants were asked six questions about relationship power differentials, emotional dynamics, and partner concurrency. Items were adapted from the Sexual Relationship Power Scale (53) based on prior literature on HIV risk behaviors in YMSM. Items included: (1) I really wanted my relationship with this person to last; (2) I felt trapped or stuck in my relationship with this person; (3) My partner was having sex with someone else; (4) My partner paid for things I really wanted or needed; (5) When my partner and I disagreed, my partner got his way most of the time; and (6) Most of the time we did what my partner wanted to do. Response options were on a 4-point Likert scale, ranging from 0 (strongly disagree) to 3 (strongly agree).
Partnership characteristics
The H-RASP assessed age difference between partners on the following scale (centered at ‘same age’): −2=more than 2 years younger, −1=1 year younger, 0=same age, 1=1 to 2 years older, 2=3 to 4 years older, 3=5 or more years older. We assessed where participants met their partners, and venue of meeting was characterized into “online” (coded 1) or “offline” (coded 0). Finally, we assessed relationship violence during the H-RASP. Physical IPV was defined as “hit, slapped, punched, or hurt in a physical way” and sexual IPV was defined as “having sex when you didn’t want to (including physical and non-physical pressure, such as pushing, arguing or threatening)”. Participants’ response options were either yes (1) or no (0) to assess whether either of these forms of IPV had ever occurred with each partner.
Analyses
Analyses were conducted using Hierarchical Linear Modeling (HLM) 7.0 statistical software (54). HLM is well suited to account for the dependencies in data that contain a nested or multilevel structure. We ran two types of models for these analyses. First, we utilized a two-level model to examine the main effects of partner and relationship characteristics on CAI. In these models, sexual partnership data (Level 1) were nested within participants (Level 2), and HLM estimated main effects at Level 1. To examine change over time in the effects of partner and relationship characteristics on CAI, we utilized a three-level model (except where noted). In this case, sexual partnership data (Level 1) were nested within waves of data collection (Level 2), which were further nested within participants (Level 3). We analyzed developmental change in the effects of Level 1 partnership variables on the outcome variable by entering participant age at each wave at Level 2 as a moderator of Level 1 main effects. A three-level model is preferable for the analysis of developmental change in the effects of repeated measures variables because it accounts for dependency that occurs within-persons, as well as within waves of data collection as the participant ages.
Maximum likelihood estimation was used to model the frequency of CAI using a Poisson distribution that accounted for overdispersion (i.e., the standard deviation of the outcome variable was larger than the mean). As such, results are presented as event-rate ratios (ERR), which provide an estimate of the change in event-rate of the outcome variable (e.g., number of CAI acts in male partnerships) for each one unit increase in the independent variable. Estimates were made from the population-average model using robust standard errors.
RESULTS
One participant was removed due to missing data at baseline, and three participants were removed because they did not report any sexual partners in the six months prior to each wave of data collection. The remaining 114 participants reported a total of 779 sexual partnerships across all seven waves of data collection, and 693 sexual partnerships with male partners. Participants had a median of one male sexual partner per 6-month wave, and 10% reported having more than three sexual partners at any given wave. Given that we collected data on up to three partnerships per wave, the current data captures the vast majority (90%) of our participants’ sexual partnerships during the 4-year follow-up period.
Table 2 shows sexual partnership and relationship characteristics across all waves of data collection. On average, participants had 4.72 episodes of CAI in their male partnerships. The intraclass correlation coefficient (ICC) indicated that the vast majority of the variance in CAI was across partnerships (91%), as opposed to between participants. Approximately half of relationships were considered serious (49%), with participants reporting a mean of 3.00 (SD = 2.82) serious relationships across all of the reporting windows in the 4-year follow-up period (15.3% had zero, 33.1% had 1–2, 27.1% had 3–4, and 24.5% had 5 or more). Within these serious relationships, participants most strongly agreed with the feeling that they wanted their relationship to last. On average, sexual partners were described as 1–2 years older than the participant (M = 1.20), with the majority of the variance in partner age differences across partnerships (76%; ICC = .24). In terms of IPV, physical IPV occurred in 11% of partnerships, and sexual IPV in 3% of partnerships. Twenty-six percent of partners were met online. Finally, there were no significant demographic differences in rate of CAI across the entire follow-up period, including no differences by race/ethnicity or self-reported sexual orientation at baseline.
Table 2.
Sexual Partner and Relationship Characteristics Across All Sexual Partnerships
| Study Variables | Mean | SD | % | ICC | Kappa |
|---|---|---|---|---|---|
| Variables asked of all partnerships | |||||
| Condomless Anal Intercourse with Males (count) | 4.72 | 15.74 | -- | .09 | -- |
| Serious Relationship (dichotomous) | -- | -- | 49% | -- | .51 |
| Met Partner Online (dichotomous) | -- | -- | 26% | -- | .70 |
| Hit, Slapped, Punched by Partner (dichotomous) | -- | -- | 11% | -- | .88 |
| Forced Sex by Partner (dichotomous) | -- | -- | 3% | -- | .95 |
| Partner Age Difference (ordinal) | 1.20 | 1.34 | .24 | ||
| Variables asked of serious partnerships only | |||||
| Wanted Relationship to Last (ordinal) | 2.43 | 0.88 | -- | .07 | -- |
| Felt Trapped/Stuck (ordinal) | 0.79 | 0.93 | -- | .87 | -- |
| Partner Having Sex with Others (ordinal) | 0.79 | 0.98 | -- | .78 | -- |
| Partner Paid for Things (ordinal) | 1.43 | 1.06 | -- | .70 | -- |
| Partner Got His Way (ordinal) | 1.28 | 0.90 | -- | .94 | -- |
| Did What Partner Wanted (ordinal) | 1.40 | 0.86 | -- | .81 | -- |
Change Over Time in Sexual Risk Behavior and Partnership Characteristics
Age at each wave of data collection was used to evaluate the slopes of change in sexual partner and relationship characteristics over time (see Table 3). CAI did not change significantly with age for the sample as a whole (ERR = 1.02, p = .776). Additionally, we observed no change over time in the reporting of any of the sexual partnership characteristics, included no change over time in the proportion of relationship types (serious vs. casual), partner age differences, meeting partners online, partnership physical IPV and partnership sexual IPV. We also examined the slopes of change in endorsement of the relationship characteristics in serious relationships. Endorsement of the items “partner paid for things” (coefficient = −0.06, p < .05) and “did what partner wanted” (coefficient = −0.07, p < .01) decreased significantly with age. We observed no change over time in the following relationship items: “wanted relationship to last”, “felt trapped/stuck in relationship”, “partner having sex with others”, and “partner got his way”.
Table 3.
Change Over Time in Sexual Partner and Relationship Characteristics
| Change Over Time in Study Variables |
||||||
|---|---|---|---|---|---|---|
| Study Variables | Standardized Coefficient |
p-value | Odds Ratio | Confidence Interval (95%) |
Event-Rate Ratio |
Confidence Interval (95%) |
| Sexual Partnership Variables | ||||||
| Condomless Anal Intercourse | -- | -- | -- | -- | 1.02 | 0.90 – 1.16 |
| Relationship Type (Serious) | -- | -- | 0.98 | 0.90 – 1.06 | -- | -- |
| Met Partner Online | -- | -- | 1.01 | 0.90 – 1.12 | -- | -- |
| Hit, Slapped, Punched | -- | -- | 0.95 | 0.85 – 1.07 | -- | -- |
| Forced Sex | -- | -- | 1.03 | 0.84 – 1.25 | -- | -- |
| Partner Age Difference | 0.02 | .479 | -- | -- | -- | -- |
| Relationship Characteristics | ||||||
| Wanted Relationship to Last | −0.04 | .146 | -- | -- | -- | -- |
| Felt Trapped/Stuck | 0.01 | .709 | -- | -- | -- | -- |
| Partner Having Sex with Others | −0.03 | .313 | -- | -- | -- | -- |
| Partner Paid for Things | −0.06 | <.05 | -- | -- | -- | -- |
| Partner Got His Way | −0.02 | .521 | -- | -- | -- | -- |
| Did What Partner Wanted | −0.07 | <.01 | -- | -- | -- | -- |
NOTE: relationship characteristics were only assessed for partnerships there were indicated to be “serious”.
Longitudinal Correlates of Sexual Risk (2-Level Model)
Sexual partnership characteristics were entered into Level 1 of a two-level model in HLM in order to examine longitudinal partnership-level correlates of CAI (see Table 4). This model adjusted for the effects of participant demographic characteristics, including age at each wave, race/ethnicity, and self-reported sexual orientation at baseline. The strongest longitudinal correlate of CAI was relationship status (ERR = 12.50, p < .001), such that serious sexual partnerships were associated with an approximate 12-fold increase in rate of CAI relative to casual partnerships. To examine whether this effect is driven by a higher number of sex acts with serious relative to casual partners, we ran a follow-up analysis examining the odds of having CAI with serious relative to casual partners. The odds of CAI with a serious partner was about 4 times higher (OR = 3.86, p < .001). In fact, the odds of CAI with a serious partner remained more than twice as high (OR = 2.44, p < .001) even after controlling for the total number of anal sex acts, which itself was a significant predictor of CAI (OR = 1.04, p < .01). Sexual IPV was the next strongest effect (ERR = 2.04, p < .001), and the rate of CAI was approximately twice as high in partnerships in which sexual IPV had occurred. Additionally, physical IPV (ERR = 1.88, p < .05) and larger partner age differences (ERR = 1.18, p < .001) were each associated with a higher rate of CAI. Meeting partners online was not associated with CAI.
Table 4.
Effects of Sexual Partner and Relationships Characteristics on Condomless Anal Intercourse
| Fixed Effects | Event- Rate Ratio (ERR) |
Confidence Interval (95%) |
p- value |
|---|---|---|---|
| Longitudinal Correlates (2-Level Model) | |||
| Relationship Status (serious) | 12.50 | 8.30 – 18.82 | <.001 |
| Partner Age Difference | 1.18 | 1.09 – 1.28 | <.001 |
| Venue of Meeting (online) | 1.06 | 0.80 – 1.40 | 0.671 |
| Physical IPV | 1.88 | 1.11 – 3.21 | <.05 |
| Sexual IPV | 2.04 | 1.16 – 3.57 | <.05 |
| Developmental Change in Effects (3-Level Model) | |||
| Relationship Status X Age | 0.80 | 0.71 – 0.90 | <.001 |
| Partner Age Difference X Age | 1.07 | 1.02 – 1.11 | <.01 |
| Met Partner Online X Age | 1.27 | 1.16 – 1.40 | <.001 |
| Physical IPV X Age* | 1.17 | 0.99 – 1.39 | 0.061 |
| Sexual IPV X Age* | 1.56 | 1.32 – 1.83 | <.001 |
Change over time in the effects of physical violence and forced sex on sexual risk were conducted as follow-up analyses in a 2-level HLM model because there was not enough within-participant variance in these independent variables within waves of data collection. IPV = Intimate Partner Violence.
In a follow-up analysis, we examined the effects of relationship characteristics on CAI in serious partnerships (see Table 5), and this model also adjusted for participant demographic characteristics. Both “wanted the relationship to last” (ERR = 1.89, p < .001) and “felt trapped/stuck in relationship” (ERR = 1.29, p < .05) were associated with higher rates of CAI. Conversely, “partner having sex with others” (ERR = 0.78, p < .058) and “did what partner wanted” (ERR = 0.75, p < .05) were both associated with lower rates of CAI, though the former effect was a trend. “Partner paid for things” and “partner got his way” were not associated with rate of CAI.
Table 5.
Effects of Relationship Characteristics on Condomless Anal Intercourse in Serious Relationships
| Fixed Effects | Event- Rate Ratio (ERR) |
Confidence Interval (95%) |
p- value |
|---|---|---|---|
| Longitudinal Correlates (2-Level Model) | |||
| Wanted Relationship to Last | 1.89 | 1.46 – 2.44 | <.001 |
| Felt Trapped/Stuck in Relationship | 1.29 | 1.04 – 1.59 | <.05 |
| Partner Having Sex with Others | 0.78 | 0.61 – 1.01 | 0.058 |
| Partner Paid for Things | 0.92 | 0.79 – 1.07 | 0.263 |
| Partner Got His/Her Way | 1.19 | 0.89 – 1.60 | 0.245 |
| Did What Partner Wanted | 0.75 | 0.57 – 1.00 | <.05 |
| Developmental Change in Effects (2-Level Model) | |||
| Wanted Relationship to Last X Age | 1.05 | 0.94 – 1.17 | 0.414 |
| Felt Trapped/Stuck in Relationship X Age | 1.16 | 1.03 – 1.31 | <.05 |
| Partner Having Sex with Others X Age | 0.93 | 0.83 – 1.06 | 0.278 |
| Partner Paid for Things X Age | 0.98 | 0.91 – 1.05 | 0.530 |
| Partner Got His/Her Way X Age | 0.92 | 0.79 – 1.07 | 0.266 |
| Did What Partner Wanted X Age | 1.03 | 0.88 – 1.19 | 0.724 |
Change Over Time in Longitudinal Correlates of Sexual Risk (3-Level Model)
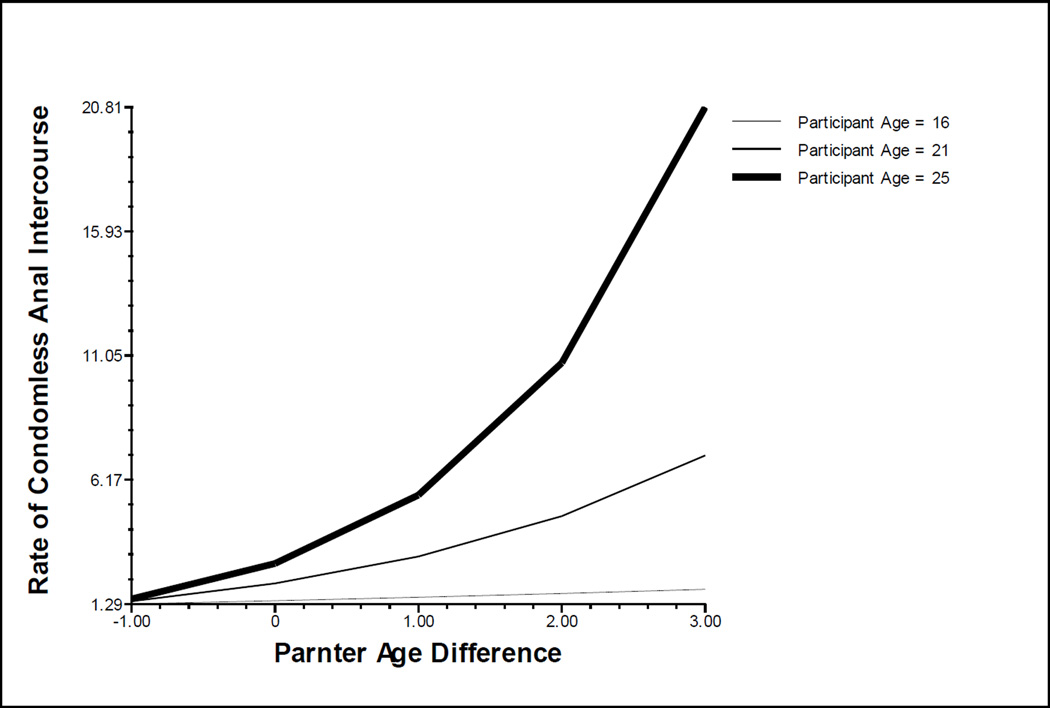
We evaluated change over time in the effects of sexual partnership characteristics on CAI in a three-level model by entering age at each wave of data collection at Level 2 as a moderator of the Level 1 effects of sexual partnership characteristics on CAI (i.e., cross-level interactions). Note that physical and sexual IPV were analyzed separately in a two-level model; because the base rate of IPV was relatively low, there was not enough variance in the endorsement of these variables within waves in order to allow for the estimation of a three-level model As such, we examined developmental change in the effects of IPV on CAI by entering the appropriate interaction terms at Level 1 in a separate two-level model (i.e., within-level interaction; partner violence X age at each wave). All effects were estimated in multivariate models that adjusted for the main effects of age at each wave of data collection, participant race/ethnicity and self-reported sexual orientation (see Table 4). There was significant change over time in the association between relationship status and CAI (ERR = 0.80, p < .001); the difference in rate of CAI with serious compared to casual partners decrease over time. Conversely, the positive association between having older partners and CAI increased significantly over time (ERR = 1.07, p < .01; see Figure 1). A similar pattern was found for the change over time in the effects of meeting partners online (ERR = 1.27, p <.001), physical IPV (ERR = 1.17, p = .061), and sexual IPV (ERR = 1.56, p < .001) on CAI.
Figure 1.
Developmental Change in the Association between Partner Age Difference and Condomless Anal Intercourse
We conducted a follow-up analysis to examine a possible explanation for the above-described effects; increases in the strength of the association between partnership characteristics and CAI across development may occur because YMSM move out from their family homes and into less restrictive and protective environments as they age. To do this, we examined the moderating effect of living situation (coded 1 = living with family; 0 = other living situation) on the relationship between each partnership characteristic and CAI in a multivariate model that contained the previously described developmental effects. Living situation significantly moderated several of the associations between partnership characteristics and CAI. The positive association between CAI and each of the partnership variables that demonstrated developmental change previously (i.e., serious partnerships, older partners, meeting partners online, and sexual IPV) was stronger among YMSM who did not live with their parents or family relative to those who lived in some other situation. Living situation did not moderate the association between physical IPV and CAI.
Analysis of change over time in the effects of relationship characteristics on CAI in serious partnerships was conducted in a separate two-level model (see Table 5). In this case, a three-level model would have required enough variance in observed variables within each wave of data collection, which is unlikely as very few participants report multiple serious partnerships within a single wave. The effect of “felt trapped/stuck in relationship” changed significantly over time (ERR = 1.16, p < .05), such that the positive association between feeling trapped or stuck and CAI increased with participant age. There was no change over time in the effects of the other relationship characteristics, including “wanted relationship to last”, “partner having sex with others”, “partner paid for things”, “partner got his/her way”, and “did what partner wanted”.
DISCUSSION
These analyses expand upon previous studies that have examined the influence of partner and relationship characteristics on engagement in sexual risk behavior (9, 10) by modeling how these influences change as YMSM move from adolescence into emerging adulthood. Our findings are consistent with previous reports indicating that the rate of CAI is substantially higher with serious compared to casual partners (3, 9, 10). However, our analyses suggest that this difference is largest in adolescence and decreases over time, largely due to a small increase in rate of CAI with casual partners during emerging adulthood. Conversely, the influence of other partner and relationship characteristics on CAI increased in strength over time, including the influence of partner age differences, meeting partners online, and physical and sexual IPV. Finally, several characteristics of serious relationships had an influence on rate of CAI. Wanting one’s relationship to last and feeling trapped or stuck in one’s relationship were both associated with higher rates of CAI, and the latter effect increased in strength over time. Partner sexual concurrency and doing what one’s partner wanted most of the time were both negatively associated with rate of CAI.
Consistent with extant research (3, 9, 10), the rate of CAI was substantially higher in serious relative to casual partnerships across all waves (approximately 12 times higher), as was the odds of CAI with a serious relative to casual partner (approximately 4 times higher). However, the strength of this effect decreased over time. The rate of CAI with casual partners increased with age relative to CAI with serious partners, thus decreasing the magnitude of the effect. This developmental change may result from the fact that adolescent relationships are more likely to follow a pattern of serial monogamy in which relationships are defined as serious more rapidly than in adulthood, but last for briefer durations (i.e., rapid primary partner turnover). Older YMSM may wait longer before defining their relationships as serious and therefore a dichotomous definition of serious vs. casual relationships may not capture the range of relationship types these young men have with their partners. It would make sense that CAI may occur with some frequency in some of the casual partnerships of older YMSM in which partners have known each other for longer and have established some amount of trust or familiarity (e.g., casual dating partners, repeated sex partners). Alternatively, CAI with casual partners may increase with age if YMSM become more comfortable with this risk behavior over time. This may result from various factors, such as becoming more familiar with HIV through increased contact with HIV-positive individuals or receiving repeated negative test results that reinforce engagement in risk (55). Regardless, the rate of CAI remains much higher in serious relationships regardless of participant age. Given that the majority of new HIV infections in YMSM come from primary partners (3), it is clear that YMSM need to be given the skills necessary to navigate the complexities of HIV prevention in serious relationships, including the integration of behavioral and biomedical approaches.
Also consistent with expectations, several other partner and relationship characteristics were associated with a higher rate of CAI with male partners, including larger partner age differences, physical IPV, and sexual IPV. Each of these partnership characteristics may reflect power differentials between YMSM and their sexual partners (9, 10), which could lead to reduced ability to negotiate safer sex practices. In the case of age discordant partnerships, the older partner may have more control or power (either perceived or actual), which could reduce agency in the younger partner. In more extreme cases, partners may exert control over younger partners through actual or threatened violence. Such violence is likely to diminish the victim’s capacity to initiate discussions about condom use or other safer sex practices. When such violence involves forced sex, it is likely that YMSM are not able to make a choice about condom use during coercive or forced sex events.
Each of the associations between these partnership characteristics and CAI increased in strength as YMSM moved from late adolescence to emerging adulthood. At first glance, these findings seem counterintuitive. One might expect that the youngest individuals would be the most vulnerable to the influence of various partnership characteristics on engagement in condomless sex, particularly when these factors set up power differentials that could be challenging for younger YMSM to navigate. Our supplementary analyses provide a possible explanation. As YMSM age into emerging adulthood, they often move into less restrictive or less protective environments (e.g., they gain independence from parents, move away from families of origin). These contextual shifts may increase vulnerability to the influence of partnership characteristics on engagement in sexual risk because there are fewer restrictions on who and in what contexts YMSM interact with their dating and sexual partners. For example, a young person living alone who meets a partner online may feel less confident in their ability to negotiate safer sex with that partner compared to a young person who lives at home in which access to support is more readily available.
With regard to the effect of older partners on sexual risk, we should note that we assessed partner age differences as a relative age difference (e.g., “5 or more years older”) which may have masked important developmental change in partner age differences that could have been observed if we had measured the actual age of the sexual partner. In other words, our measurement would categorize the age difference between an 18 and 23 year-old the same as the difference between a 22 and 40 year old. As YMSM move into their early 20s, they gain more access to MSM-specific venues and are more likely to live independently, which allows for more opportunities to meet older partners in their 30s and 40s. These larger age discrepancies could be more likely to set up power differentials that could reduce likelihood of safer sex. If in fact YMSM have more age discrepant relationships as they move into emerging adulthood, then they may also be more likely to have CAI with these older partners.
Our previous research with this sample has also found that both general alcohol use and alcohol use before sex increased developmentally (49, 56), as did the positive association between alcohol use before sex and CAI (49). It may be that normative increases in alcohol use during this developmental period, which are typically a function of moving into less restrictive environments and gaining legal access to alcohol, heighten the influence of other partnership characteristics on sexual risk. Regardless of the explanation for these developmental effects, it is clear that late adolescence and emerging adulthood are periods during which YMSM are engaging in behaviors that put them at risk for HIV acquisition, and there are various characteristics of the sexual dyad that are associated with HIV risk behavior. As such, this is a critical developmental period during which dyadic HIV prevention interventions may be especially potent in reducing HIV transmission between partners. Future observation of this cohort can determine whether the associations between partnership characteristics and CAI continue to change over time or stabilize.
Finally, several characteristics of serious relationships were associated with rate of CAI with serious partners. Consistent with previous findings (9), wanting one’s relationship to last was associated with a higher rate of CAI, which is corroborated by qualitative research that has found that YMSM stop using condoms in their serious relationship to express trust, commitment and intimacy (11). Feeling trapped or stuck in one’s relationship was also associated with a higher rate of CAI, and the strength of this effect increased as YMSM moved from adolescence to emerging adulthood. This characteristic may be another indicator of a power differential between partners that could reduce the ability of the partner with less power to negotiate condom use. As noted previously, exposure to relationships that might establish such power differentials may increase as YMSM age and move into less restrictive environments. Interestingly, doing what one’s partner wanted most of the time would also seem to be an indicator of a power differential between partners, but this characteristic was actually associated with reduced rate of CAI. It may be that the endorsement of this item actually captured YMSM who were more agreeable than others, and such agreeableness may facilitate healthier communication between partners that could reduce likelihood of HIV risk behavior. Finally, believing a partner was having sex with others was associated with a marginally lower rate of CAI with serious partners, which is consistent with previous findings (9, 10). This finding makes sense given that YMSM likely perceive themselves to be at higher risk for HIV or STIs when their partners are having sex with people outside the relationship.
Taken together, these various findings have important implications for the development of HIV prevention strategies for YMSM. What is clear is that YMSM are engaging in HIV risk behaviors in their serious relationships at higher rates compared to their casual sex encounters. Moreover, various characteristics of their partners (e.g., older partners) and relationships (e.g., wanting one’s relationship to last) influence rates of CAI. Despite mounting evidence that dyadic factors play a critical role in potentiating HIV transmission among YMSM, very few interventions are available that address such dyadic influences in order to reduce risk. It is also important to note that romantic relationships provide a multitude of mental and physical health benefits to individuals (18–22). As such, by developing a base of healthy relationship skills (e.g., effective communication, coping skills), YMSM can develop the skills to enhance their relationship functioning, navigate power differentials in their relationships, and make effective decisions about safer sex practices. Not having these skills leaves many YMSM vulnerable to HIV infection, which is contributing to the continuing rise of HIV incidence in this population.
It is important to acknowledge several limitations of the current investigation. First, the current study used a retrospective approach to examine situational predictors of risk associated with up to three sexual partners in the six months prior to each interview. While this approach allows for the examination of a wider timeframe than most other prospective designs (e.g., diary studies), as well as more variability in sexual partnerships, it may be prone to some bias in recall. Furthermore, this study used an accelerated longitudinal design in which we recruited a baseline sample with a narrow age range (ages 16–20) and followed the sample longitudinally. This approach allowed us to observe a wider developmental period across all timepoints (ages 16–25), but this sample contains fewer data points at the extremes of the developmental period, which may lead to less precision in estimation of effects at the youngest and oldest ages. Next, these data did not contain enough within-wave variability in the occurrence of certain independent variables (e.g., IPV). This precluded our ability to estimate three-level models for some effects, which means we were not able to account for within-wave (Level 2) dependency for these effects. Finally, while a major strength of our data is that we observed multiple partnerships within participants over time, these reports are from only one member of the dyad. Data from both members of the dyad would allow us to understand how characteristics of each partner influences the health and behavior of the other.
Despite these limitations, the current analyses provide novel data that has important implications for future research and prevention efforts. This is one of the first studies to examine developmental change in the effects of partner and relationship characteristics on sexual risk behavior in YMSM across adolescence and emerging adulthood. These findings are highly significant in that they point to important targets for HIV prevention interventions among YMSM. In order to curb rising rates of HIV in YMSM, prevention efforts must address dyadic influences on risk, including dynamics of serious romantic relationships, age discordant partnerships, and IPV, as well as the effects of situational alcohol and substance use on risk, which we highlighted in a previous report (49). YMSM need to be given the skills to build and maintain healthy relationships. By optimizing the functioning of their relationships, YMSM may be better able to navigate the complexities of HIV risk reduction across various types of partnerships.
ACKNOWLEDGMENTS
This research was supported by a grant from the National Institute of Mental Health (R21MH095413; PI: Mustanski), National Institute on Drug Abuse (U01DA036939), an American Foundation for Suicide Prevention grant (PI: Mustanski), the William T. Grant Foundation Scholars Award (PI: Mustanski), and the David Bohnett Foundation (PI: Mustanski). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
REFERENCES
- 1.Centers for Disease Control and Prevention. Diagnoses of HIV infection in the United States and dependent areas, 2011. HIV Surveillance Report. 2013;23 [Google Scholar]
- 2.Prejean J, Song R, Hernandez A, et al. Estimated HIV incidence in the United States, 2006–2009. PLoS One. 2011;6:e17502. doi: 10.1371/journal.pone.0017502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sullivan PS, Salazar L, Buchbinder S, Sanchez TH. Estimating the proportion of HIV transmissions from main sex partners among men who have sex with men in five US cities. AIDS. 2009;23:1153–1162. doi: 10.1097/QAD.0b013e32832baa34. [DOI] [PubMed] [Google Scholar]
- 4.Mustanski B, Parsons JT. Introduction to the special section on sexual health in gay and bisexual male couples. Arch Sex Behav. 2014;43:17–19. doi: 10.1007/s10508-013-0228-4. [DOI] [PubMed] [Google Scholar]
- 5.Mustanski BS, Newcomb ME, Du Bois SN, Garcia SC, Grov C. HIV in young men who have sex with men: a review of epidemiology, risk and protective factors, and interventions. J Sex Res. 2011;48:218–253. doi: 10.1080/00224499.2011.558645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Crepaz N, Marks G, Mansergh G, et al. Age-related risk for HIV infection in men who have sex with men: examination of behavioral, relationship, and serostatus variables. AIDS Educ Prev. 2000;12:405–415. [PubMed] [Google Scholar]
- 7.Dudley MG, Rostosky SS, Korfhage BA, Zimmerman RS. Correlates of high-risk sexual behavior among young men who have sex with men. AIDS Educ Prev. 2004;16:328–340. doi: 10.1521/aeap.16.4.328.40397. [DOI] [PubMed] [Google Scholar]
- 8.Hays RB, Kegeles SM, Coates TJ. Unprotected sex and HIV risk taking among young gay men within boyfriend relationships. AIDS Educ Prev. 1997;9:314–329. [PubMed] [Google Scholar]
- 9.Mustanski B, Newcomb ME, Clerkin EM. Relationship characteristics and sexual risk-taking in young men who have sex with men. Health Psychol. 2011;30:597–605. doi: 10.1037/a0023858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Newcomb ME, Ryan DT, Garofalo R, Mustanski B. The effects of sexual partnership and relationship characteristics on three sexual risk variables in young men who have sex with men. Arch Sex Behav. 2014;43:61–72. doi: 10.1007/s10508-013-0207-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Greene GJ, Andrews R, Kuper L, Mustanski B. Intimacy, monogamy, and condom problems drive unprotected sex among young men in serious relationships with other men: a mixed methods dyadic study. Arch Sex Behav. 2014;43:73–87. doi: 10.1007/s10508-013-0210-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. HIV among gay, bisexual, and other men who have sex with men: Unites States Department of Health and Human Services. 2013 [Google Scholar]
- 13.Jessor R. Risk behavior in adolescence: a psychosocial framework for understanding and action. Dev Rev. 1992;12:374–390. [Google Scholar]
- 14.Arnett JJ. Emerging adulthood A theory of development from the late teens through the twenties. Am Psychol. 2000;55:469–480. [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. Youth Risk Behavior Surveillance - United States, 2011. MMWR. 2012;61:1–162. [PubMed] [Google Scholar]
- 16.Steinberg L. A social neuroscience perspective on adolescent risk-taking. Dev Rev. 2008;28:78–106. doi: 10.1016/j.dr.2007.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Corbin WR, Fromme K. Alcohol use and serial monogamy as risks for sexually transmitted diseases in young adults. Health Psychol. 2002;21:229–236. doi: 10.1037//0278-6133.21.3.229. [DOI] [PubMed] [Google Scholar]
- 18.Misovich SJ, Fisher JD, Fisher WA. Close relationships and elevated HIV risk behavior: evidence and possible underlying psychological processes. Rev Gen Psychol. 1997;1:72–107. [Google Scholar]
- 19.Robles TF, Kiecolt-Glaser JK. The physiology of marriage: pathways to health. Physiol Behav. 2003;79:409–416. doi: 10.1016/s0031-9384(03)00160-4. [DOI] [PubMed] [Google Scholar]
- 20.Waite LJ, Gallagher M. The case for marriage: why married people are happer, healthier, and better off financially. Doubleday Books; 2000. [Google Scholar]
- 21.House JS, Umberson D, Landis KR. Structures and processes of social support. Ann Rev Sociol. 1988;14:293–318. [Google Scholar]
- 22.Turner RJ, Brown RL. Social support and mental health. New York, NY: Cambridge University Press; 2010. [Google Scholar]
- 23.Drasin H, Beals KP, Elliott MN, et al. Age cohort differences in the developmental milestones of gay men. J Homosex. 2008;54:381–399. doi: 10.1080/00918360801991372. [DOI] [PubMed] [Google Scholar]
- 24.Eccles TA, Sayegh MA, Fortenberry JD, Zimet GD. More normal than not: a qualitative assessment of the developmental experiences of gay male youth. J Adolesc Health. 2004;35:425, e411–e428. doi: 10.1016/j.jadohealth.2004.02.015. [DOI] [PubMed] [Google Scholar]
- 25.Rosario M, Schrimshaw EW, Hunter J. Different patterns of sexual identity development over time: implications for the psychological adjustment of lesbian, gay, and bisexual youths. J Sex Res. 2011;48:3–15. doi: 10.1080/00224490903331067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rosario M, Schrimshaw EW, Hunter J. Predicting different patterns of sexual identity development over time among lesbian, gay, and bisexual youths: a cluster analytic approach. Am J Community Psychol. 2008;42:266–282. doi: 10.1007/s10464-008-9207-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mustanski B, Birkett M, Greene GJ, Hatzenbuehler ML, Newcomb ME. Envisioning an America without sexual orientation inequities in adolescent health. Am J Public Health. 2014;104:218–225. doi: 10.2105/AJPH.2013.301625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Macapagal KR, Greene GJ, Rivera Z, Mustanski B. Relationship stages and processes among same-sex couple in emerging adulthood. Manuscript under review. doi: 10.1037/fam0000094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mustanski B, Newcomb ME. Older sexual partners may contribute to racial disparities in HIV among young men who have sex with men. J Adolesc Health. 2013;52:666–667. doi: 10.1016/j.jadohealth.2013.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Joseph HA, Marks G, Belcher L, et al. Older partner selection, sexual risk behaviour and unrecognised HIV infection among black and Latino men who have sex with men. Sex Transm Infect. 2011;87:442–447. doi: 10.1136/sextrans-2011-050010. [DOI] [PubMed] [Google Scholar]
- 31.Newcomb ME, Mustanski B. Racial differences in same-race partnering and the effects of sexual partnership characteristics on HIV Risk in MSM: a prospective sexual diary study. J Acquir Immune Defic Syndr. 2013;62:329–333. doi: 10.1097/QAI.0b013e31827e5f8c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Centers for Disease Control and Prevention. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data - United States and 6 U.S. dependent areas −2010. HIV Surveillance Supplemental Report. 2012;17 [Google Scholar]
- 33.Berry M, Raymond HF, McFarland W. Same race and older partner selection may explain higher HIV prevalence among black men who have sex with men. AIDS. 2007;21:2349–2350. doi: 10.1097/QAD.0b013e3282f12f41. [DOI] [PubMed] [Google Scholar]
- 34.Dank M, Lachman P, Zweig JM, Yahner J. Dating violence experiences of lesbian, gay, bisexual, and transgender youth. J Youth Adolesc. 2014;43:846–857. doi: 10.1007/s10964-013-9975-8. [DOI] [PubMed] [Google Scholar]
- 35.Buller AM, Devries KM, Howard LM, Bacchus LJ. Associations between intimate partner violence and health among men who have sex with men: a systematic review and meta-analysis. PLoS Med. 2014;11:e1001609. doi: 10.1371/journal.pmed.1001609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Finneran C, Stephenson R. Intimate partner violence among men who have sex with men: a systematic review. Trauma Violence Abuse. 2013;14:168–185. doi: 10.1177/1524838012470034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Finneran C, Stephenson R. Intimate partner violence, minority stress, and sexual risk-taking among U.S men who have sex with men. J Homosex. 2014;61:288–306. doi: 10.1080/00918369.2013.839911. [DOI] [PubMed] [Google Scholar]
- 38.Feldman MB, Ream GL, Diaz RM, El-Bassel N. Intimate partner violence and HIV sexual risk behavior among Latino gay and bisexual men: the role of situational factors. J LGBT Health Res. 2007;3:75–87. doi: 10.1080/15574090802226618. [DOI] [PubMed] [Google Scholar]
- 39.Houston E, McKirnan DJ. Intimate partner abuse among gay and bisexual men: risk correlates and health outcomes. J Urban Health. 2007;84:681–690. doi: 10.1007/s11524-007-9188-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Koblin BA, Torian L, Xu G, et al. Violence and HIV-related risk among young men who have sex with men. AIDS Care. 2006;18:961–967. doi: 10.1080/09540120500467182. [DOI] [PubMed] [Google Scholar]
- 41.Mustanski B, Garofalo R, Herrick A, Donenberg G. Psychosocial health problems increase risk for HIV among urban young men who have sex with men: preliminary evidence of a syndemic in need of attention. Ann Behav Med. 2007;34:37–45. doi: 10.1080/08836610701495268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Grov C, Breslow AS, Newcomb ME, Rosenberger JG, Bauermeister JA. Gay and bisexual men's use of the Internet: research from the 1990s through 2013. J Sex Res. 2014;51:390–409. doi: 10.1080/00224499.2013.871626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bauermeister JA, Leslie-Santana M, Johns MM, Pingel E, Eisenberg A. Mr. Right and Mr Right Now: romantic and casual partner-seeking online among young men who have sex with men. AIDS Behav. 2011;15:261–272. doi: 10.1007/s10461-010-9834-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Downing MJ., Jr Using the internet in pursuit of public sexual encounters: is frequency of use associated with risk behavior among MSM? Am J Mens Health. 2012;6:18–27. doi: 10.1177/1557988311407906. [DOI] [PubMed] [Google Scholar]
- 45.Garofalo R, Herrick A, Mustanski BS, Donenberg GR. Tip of the Iceberg: young men who have sex with men, the Internet, and HIV risk. Am J Public Health. 2007;97:1113–1117. doi: 10.2105/AJPH.2005.075630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Horvath KJ, Rosser BR, Remafedi G. Sexual risk taking among young internet-using men who have sex with men. Am J Public Health. 2008;98:1059–1067. doi: 10.2105/AJPH.2007.111070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mustanski BS. Are sexual partners met online associated with HIV/STI risk behaviours? Retrospective and daily diary data in conflict. AIDS Care. 2007;19:822–827. doi: 10.1080/09540120701237244. [DOI] [PubMed] [Google Scholar]
- 48.Ogilvie GS, Taylor DL, Trussler T, et al. Seeking sexual partners on the internet: a marker for risky sexual behaviour in men who have sex with men. Can J Public Health. 2008;99:185–188. doi: 10.1007/BF03405470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Newcomb ME, Mustanski B. Developmental change in the relationship between alcohol and drug use before sex and sexual risk behavior in young men who have sex with men. AIDS Behav. 2014;18:1981–1990. doi: 10.1007/s10461-014-0766-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tonry M, Ohlin LE, Farrington DP. Human development and criminal behavior: New ways of advancing knowledge. New York, NY: Springer-Verlag Publishing, 1991; [Google Scholar]
- 51.Heckathorn DD. Respondent-driven sampling: A new approach to the study of hidden populations. Soc Probl. 1997;44:174–200. [Google Scholar]
- 52.Mustanski B, Starks T, Newcomb ME. Methods for the design and analysis of relationship and partner effects on sexual health. Arch Sex Behav. 2014;43:21–33. doi: 10.1007/s10508-013-0215-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pulerwitz J, Gortmaker SL, DeJong W. Measuring sexual relationship power in HIV/STD research. Sex Roles. 2000;42:637–660. [Google Scholar]
- 54.Raudenbush SW, Bryk AS, Cheong YF, Congdon RT, du Toit M. HLM 7: Hierarchical linear and nonlinear modeling. Chicago, IL: Scientific Software International; 2011. [Google Scholar]
- 55.Mustanski B, Rendina HJ, Greene GJ, Sullivan PS, Parsons JT. Testing negative means i'm lucky, making good choices, or immune: diverse reactions to HIV test results are associated with risk behaviors. Ann Behav Med. 2014;48:371–383. doi: 10.1007/s12160-014-9612-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Newcomb ME, Heinz AJ, Mustanski B. Examining risk and protective factors for alcohol use in lesbian, gay, bisexual, and transgender youth: a longitudinal multilevel analysis. J Stud Alcohol Drugs. 2012;73:783–793. doi: 10.15288/jsad.2012.73.783. [DOI] [PMC free article] [PubMed] [Google Scholar]