Abstract
Spiritual meditation has been found to reduce the frequency of migraines and physiological reactivity to stress. However, little is known about how introducing a spirituality component into a meditation intervention impacts analgesic medication usage. In this study, 92 meditation naïve participants were randomly assigned to four groups (Spiritual Meditation (N=25), Internally Focused Secular Meditation (N=23), Externally Focused Secular Meditation (N=22), Progressive Muscle Relaxation (N=22)) and practiced their technique for 20min/day over 30 days while completing daily diaries. Headache frequency, headache severity, and pain medication use were assessed. Migraine frequency decreased in the Spiritual Meditation group compared to other groups (p<.05). Headache severity ratings did not differ across groups (p=NS). After adjusting for headache frequency, migraine medication usage decreased in the Spiritual Meditation group compared to other groups (p<.05). Spiritual Meditation was found to not affect pain sensitivity, but it does improve pain tolerance with reduced headache related analgesic medication usage.
Keywords: spirituality, meditation, migraine, medication, pain
Introduction
Migraine headaches are a serious pain disorder that affects people around the world. Migraine headaches are distinctive in that they involve intense, unilateral, and throbbing pain which is generally accompanied by nausea and either photo- or phono- phobia.1 In the United States, approximately 18% of women and 6% of men suffer from migraine headaches every year.2 For individuals with migraines, over a third (37%) experience frequent migraine attacks of five or more migraine headaches per month. In addition to the significant pain involved in a migraine attack, migraines have negative emotional and societal impacts. Up to 60% of migraineurs report that their headaches have had a negative impact on their relationships and 85% reported interference with their home life. Spread out across all Americans, migraine headaches account for the loss of 1.8 hours per week of productive time.3
A wide variety of pharmacological interventions for migraines have been described that offer partial relief to patients.4 These interventions may be either abortive or prophylactic with a range of side effects common to both methods. Opiates, benzodiazpines, and triptans are commonly employed as rescue medications for migraines, but these medications are burdened by side effects and risks such as medication-overuse headaches, abuse, and addiction.5 Prophylactic medications used in the treatment of migraine headaches tend to fall into the categories of antidepressants, anticonvulsants, and beta-blockers.6 Similar to abortive medications, prophylactic medications can carry serious side effects that can interfere with patients’ daily lives.
Reviews have described a variety of empirically supported non-pharmacological approaches to preventing or stopping headaches; some of these techniques exhibit pain management results equal to or better than medication.7 However, there has been relatively little research on the role of meditation and migraine headache pain medication use.
Multiple studies suggest that meditation has a generally global positive effect on emotional and physical health.8–10 Specifically meditation has proven effective in reducing physiological and psychological arousal to stress and pain.11,12 Further, recent randomized controlled trials have demonstrated the efficacy of meditation-based interventions as a treatment for headache pain,13 and other forms of chronic pain.14
Previous research has indicated that when patients access their spiritual resources they have greater tolerance of chronic arthritis pain.15 Our previously published research suggests that not only can naïve participants be taught how to access spiritual resources, but also to use that skill to enhance pain tolerance to acute, laboratory induced pain.11,12 However, little is known about how spiritual meditation affects in vivo pain experiences and how medication usage is impacted by integrating a spiritual component into a meditation practice. There are no known studies explicitly looking at how different meditation types impact pain medication consumption and pain tolerance during a migraine headache attack.
Present study
Spirituality and spiritual meditation may take many different formats in the research. For the purposes of this study, we are defining spirituality as “a person’s degree of orientation toward the transcendent features of life.” While spiritual outcomes were not the focus of this paper, this definition of spirituality was used as the basis for intervention development and to assess for balance between groups11,12.
Previous research has indicated that prayer and a spiritual meditation technique may be an effective tool to 1) decrease the frequency of migraine headaches among meditation naïve frequent migraineurs11,12 and 2) improve pain tolerance in a laboratory based pain-challenge task.11,12,16 When used for pain management, these spiritual tools can assist with meaning making which in turn can also be helpful in reducing the pain experience17. However, little is known about how different meditation types affect pain tolerance in vivo and analgesic medication consumption for migraine headaches. This study addresses that gap in the literature by analyzing daily diary data that was collected as part of a larger study on meditation type and migraine headache pain. The authors hypothesize that spiritual meditation will result in greater in vivo pain tolerance among frequent migraineurs resulting in less analgesic consumption for migraine headaches. There are multiple pathways through which spiritual meditation may be effective in helping frequent migraineurs cope with pain.18 As a result, spiritual meditators may able to endure higher levels of pain and prolonged exposure to uncomfortable situations.18,19 In order to test this hypothesis, we compared the daily headache diary data from meditation naïve frequent migraineurs who were randomly assigned to groups teaching one of four meditation techniques (spiritual meditation, internally focused secular meditation, externally focused secular meditation, and progressive muscle relaxation) and asked to practice the technique for 20 minutes a day for 30 days.
Method
Participants
This study included 92 meditation naïve participants with frequent migraines (≥2 per month) who completed a month long meditation protocol. All participants met the criteria for vascular headache (migraine; mixed migraine) according to the criteria of the International Headache Society and verified by the ID Migraine screener.1,20 Participants were excluded if they had been previously diagnosed with diabetes or Reynaud’s syndrome. No participants were concurrently engaged in therapy or counseling at the time of this study. Participants were comprised of 10 men (10.9%) and 82 women (89.1%), similar to the national prevalence rates for migraine headache.21 The participant population was ethnically diverse: white, 73%; black, 12%; Latino/a 6.5%; Multi-Racial/Ethnic 7.6%; and Native American 1.1%.
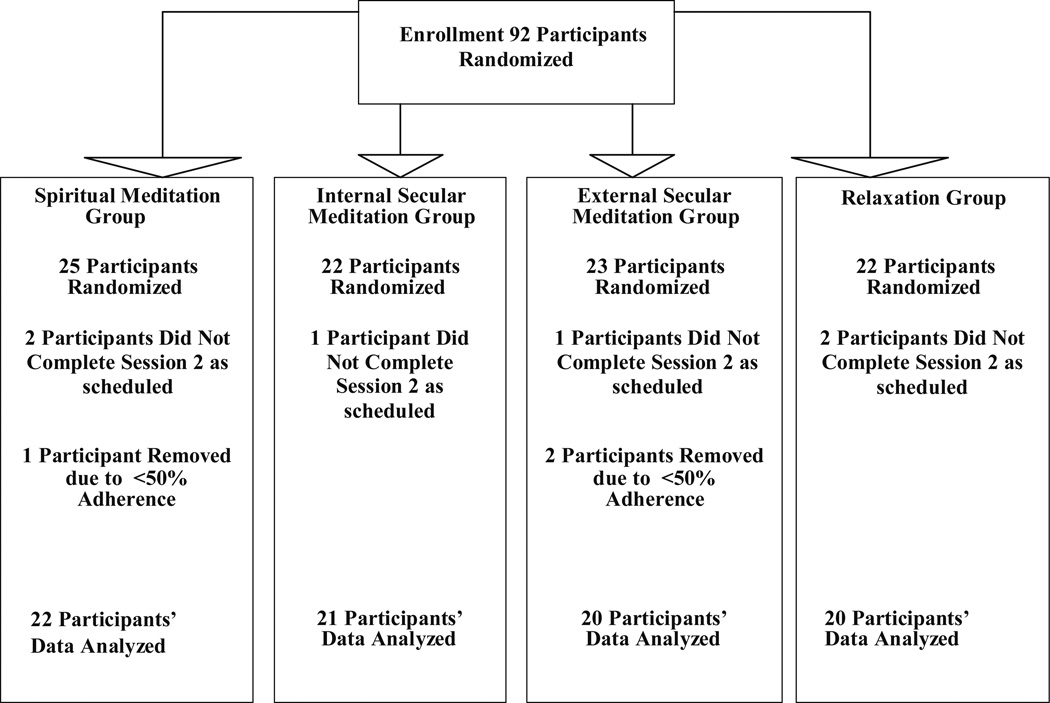
Over the course of the study, six participants dropped out of the study and three participants were dropped by the investigators due to <50% adherence to the protocol (Figure 1). Non-adhering and drop out participants did not differ statistically on pre-test variables from those who completed the study. There were no differences between the groups on number of completed meditation sessions reported via the daily diaries during the 30 day period. 83 participants completed the study protocol.
Figure 1.
Participant Flow Diagram
Participants were randomly assigned to one of four groups: Spiritual Meditation (22 participants); Internal Secular Meditation (21 participants); External Secular Meditation (20 participants); and Relaxation (20 participants). Sample size was determined by power analyses utilizing average effect/variance sizes from studies where patients meditated for less than or equal to 1 month and indicated that 20 participants per cell are required to achieve statistical significance for a power level of 0.9. There were no group differences on demographic or pre-test variables (see Table 1).
Table 1.
Demographics by Group
| Spiritual Meditation N (%) |
Internally Focused Secular Meditation N (%) |
Externally Focused Secular Meditation N (%) |
Progressive Muscle Relaxation N (%) |
|
|---|---|---|---|---|
| Gender | ||||
| Women | 19 (85.5%) | 19 (90.5%) | 19 (95%) | 18 (90%) |
| Men | 3 (13.6%) | 2 (9.5%) | 1 (5%) | 2 (10%) |
| Race | ||||
| White | 15 (68.2%) | 15 (71.4%) | 15 (75%) | 16 (80%) |
| Black | 1 (4.5%) | 3 (14.3%) | 4 (20%) | 1 (5%) |
| Hispanic | 2 (9.1%) | 1 (4.8%) | 1 (5%) | 2 (10%) |
| Native American | 1 (4.5%) | 0 | 0 | 0 |
| Middle Eastern | 0 | 1 (4.8%) | 0 | 0 |
| Multi-Racial | 3 (13.6%) | 1 (4.8%) | 0 | 1 (5%) |
| Religion | ||||
| Protestant | 11 (50.0%) | 8 (38%) | 12 (60%) | 11 (55%) |
| Catholic | 10 (45.5%) | 11 (52.4%) | 5 (25%) | 7 (35%) |
| Agnostic | 1 (4.5%) | 1 (4.8%) | 2 (10%) | 2 (10%) |
| Buddhist | 0 | 1 (4.8%) | 0 | 0 |
| Muslim | 0 | 0 | 1 (5%) | 0 |
| Self-Rated Spirituality | ||||
| None | 2 (9.1%) | 1 (4.8%) | 3 (15%) | 3 (15%) |
| Moderate | 14 (63.6%) | 17 (80.9%) | 12 (60%) | 12 (60%) |
| Very | 3 (13.6%) | 3 (14.3%) | 5 (25%) | 5 (25%) |
| M(SD) | ||||
| Headache Count/month | ||||
| Pre | 13.7 (6.36) | 12.8(5.10) | 11.1(5.24) | 11.4(6.25) |
| Post | 8.7 (5.88) | 9.7(5.48) | 10.1(5.02) | 10.4(5.08) |
| Age | 19.5 (.912) | 18.7 (.78) | 19.2 (1.67) | 18.9 (.72) |
There were no significant differences between any of the groups on any of the pre-test demographic variables.
Participants’ migraine medication use was collected upon entry to the study and medication use was assessed daily via the headache diaries. Participants reported name and dosage every headache related analgesic medication they took during the course of the study. This information was reported and submitted in their daily diaries. No participants were treated with preventative migraine medication; all migraine medication among study completers was commercially available analgesic medications. Two participants had frequent use of prescription abortive medication and benzodiazepines; both of these participants dropped out of the study prior to assessment Session 2 and were not included in the final data analysis. No participant had any changes to their medication regimens during the study.
Procedure
Participants were recruited from two primary sources: undergraduate students attending a Great Lakes region university; and flyers and advertisements in the local community. Participation was completely voluntary and participants did not receive any financial compensation. All recruitment and research procedures were approved by the university’s Human Subjects Review Board. No adverse events occurred during the course of the study.
After completing informed consent, participants were randomly assigned to a group meeting of 5–10 individuals using a random number generator. In the initial group meeting, they received basic education about the study and informed consent was completed. They then completed the initial survey (demographic, psychological, spiritual, health assessments), and were taught one of four meditation techniques. Classes were taught by Research Assistants who were trained on the study protocols but were blinded as to the hypotheses of the study. They were supervised for adherence to the protocol by the PI via audiotapes of the education sessions. Participants in each category were allowed to choose one of four phrases that they would meditate on throughout the next 30 days.
Meditation Training
Each group was trained in how to perform their assigned meditation/relaxation task using a protocol script. Participants were taught to sit in a quiet room, without any distractions (e.g. no television, radio). They were taught to wear comfortable clothing and told that they could sit in any position they would like, as long as they would not fall asleep. They were encouraged to pick a time during the day that they could use for their regular relaxation/meditation time. During the session, participants discussed problems that frequently arise among new practitioners of relaxation/meditation (e.g. losing focus) and how to solve the problem and continue relaxing/meditating.
Meditation participants were instructed to begin their meditation by softly repeating their meditation aloud a few times to help them focus, and then to continue to silently focus on the phrase, and how the phrase is reflected in their lives. If the participants felt they were losing focus, they should repeat the phrase aloud to refocus and then continue with the silent meditation. All meditation participants received the same training; the only difference was the set of meditative phrases available from which they could choose.
Meditation Groups
Spiritual Meditation participants were allowed to choose one of four spiritual meditative phrases: “God is peace,” “God is joy,” God is good,” and “God is love.” Those who were uncomfortable with the term “God” were allowed to choose another term that they felt better reflected the focus of their spirituality. Only one participant chose to use an alternate term. He chose to use “Mother Earth.”
Internal Secular Meditation participants chose from four internally focused secular phrases: “I am content,” “I am joyful,” “I am good,” “I am happy.”
In the External Secular Meditation group, participants chose from four externally focused secular meditation phrases: “Grass is green,” “Sand is soft,” “Cotton is fluffy,” “Cloth is smooth.” The participants were asked to practice their meditation for 20 minutes per day for 30 days.
Relaxation participants were taught a progressive muscle relaxation in which they tensed and released muscle groups in their bodies.20 The relaxation group was not provided a meditation phrase.
Meditation practice consisted of repeating their choice of one of the optional phrases provided within their randomly assigned meditation type. Participants were asked to use the phrase to focus their meditation and to meditate 20 minutes/daily for 30 days and complete daily headache diaries.
In pilot testing these phrases had been assessed and balanced for positivity so that there were no significant differences between the groups. Further, in the manipulation check analyses, there was also no difference on the level of relaxation reported by participants in the four groups during their assigned techniques. All groups rated the tasks ‘‘moderately’’ relaxing (F(3,78) = 0.19, p = NS).
Session 2 Assessment
After 30 days, individuals returned to the testing facility, completed another survey packet, and were tested during laboratory induced pain, while practicing their meditation technique.
Measures
Pre-Treatment Headache Measures
Patients reported their current migraine medication usage (including preventative, abortive, and analgesic forms), monthly usage of these medications, and average frequency and severity of migraine headaches.
Headache Diaries
Participants completed daily headache diaries during the 30 days of the study. Participants completed the diaries daily for each day of the 30 days. They submitted the diaries daily via email. Daily diaries consisted of questions including 1) migraine headache in the past 24 hours (Yes/No), 2) if yes, the severity of the migraine headache (1–10), and 3) if the participant consumed abortive or analgesic medications for a migraine headache including medication and dosage.
Spirituality Measures
Selected portions of the Multi-dimensional Measurement of Religiousness/Spirituality Scale were administered to screen and compare participants’ religious and spirituality levels upon entering the study and to measure group balance on spiritual measures22.
The Religious/Spiritual Intensity Scale uses a 1–10 Likert scale of self-reported spirituality, and religiousity22. The scale has an acceptable reliability (α=.77).
The five item Private Religious Activities scale was used to assess for the frequency of private spiritual activities on a 5 point Likert scale. These activities may have similar characteristics as meditation (e.g. meditative prayer) and therefore this scale was used to assess for potential confounds of activities among this meditation naïve group. Previous studies show it is a reliable measure (α=.77)22.
The Daily Spiritual Experiences Scale is a 16 item assessment to measure how frequently individuals experience the transcendent in their daily lives22,23. Items are scored on a 6 point Likert scale. Internal reliability estimates range from .91–.95 in previous research22.
Data Analysis
Data analysis used intent-to-treat and last known data pulled forward techniques. Pre-intervention spirituality assessments were compared across groups using 1×4 ANOVAs. Data analysis used SPSS 17.0, Repeated Measures GLM to assess for differences between groups in changes over time. Three analyses were performed using the following criteria: 1) headache frequency, 2) headache severity, and 3) use of headache pain medication after adjusting for headache frequency.
Results
Spirituality Results
There were no group differences in the self-reported religious intensity (F(3,78) = 1.16,ns), spiritual intensity (F(3,78) = .18, ns) or private spiritual practices (F(3,78) = 1.63, ns). Further, there was no group differences on the levels of daily spiritual experiences (F(3,78) = .08, ns).
Headache Frequency
The intervention had a noticeable impact on the frequency of headaches suffered by participants. An analysis of participants’ headaches displayed a statistically significant time period by group interaction effect in the number of reported headaches. The frequency of migraine headaches decreased significantly in the Spiritual Meditation group compared to other groups (F(87,186)=1.907, p<.05, eta2 = .64). While each of the other groups displayed some improvement in headache frequency, the improvements in the other three groups did not reach the level of statistical significance.
Headache Severity
An analysis of participant ratings of headache severity did not display a statistically significant time period by group interaction effect in the severity of reported headaches. When headaches did occur, there was no difference in headache severity ratings across groups (F(87,186)=1.182, p<NS).
Analgesic Use
Relative equi-analgesic doses and the effective analgesic dosage relationships among the participants’ migraine medications were assessed using the Oxford League Table of Analgesics in Acute Pain26. As none of the participants that completed the study used opioids, the relationships were normed to the equivalent of 1 gram of acetaminophen (paracetamol). Each headache-related medication use reported by participants in their daily diary was normed prior to further analyses.
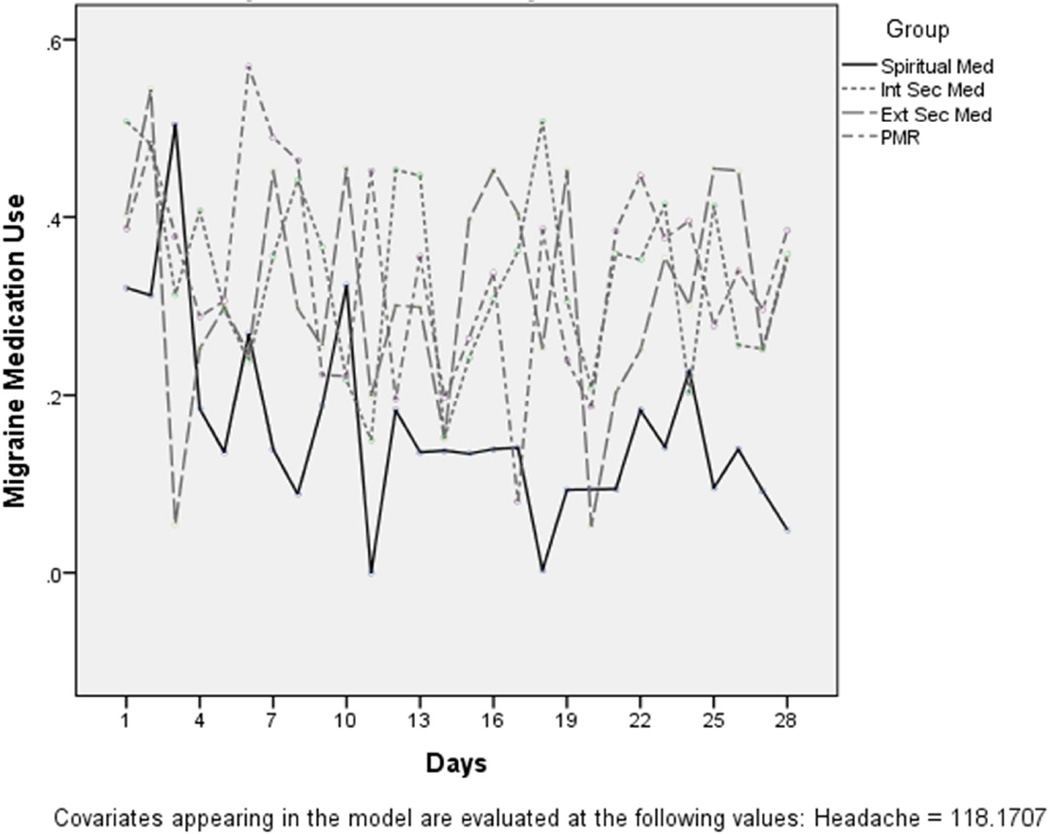
A significant interaction was observed in the levels of migraine analgesic medication consumption displayed by the separate groups (Figure 2). After adjusting for headache frequency, all four groups showed decreased analgesic medication use over time (F(81,2079)=1.317, p<.05, eta2=.34). However, medication usage for migraine headaches had a significantly sharper decline in the Spiritual Meditation group compared to other groups (p<.05).
Figure 2.
Migraine medication consumption after adjustment for headache frequency
Discussion
This study examined the impact that different forms of meditation can exert on headache frequency, headache severity, and headache analgesic medication usage. The authors hypothesized that spiritual meditation would result in less headache analgesic consumption among frequent migraineurs.
Over the course of the 30 days of the study, the frequency of migraine headaches decreased significantly among the spiritual meditators compared to the other groups. The meditation intervention did not lead to any decrease in the perception of headache severity when headaches did occur. Even with the same pain severity rating, after adjusting for headache frequency, medication usage for migraine headaches was significantly lower in the spiritual meditators compared to the other groups. The decreased analgesic use may indicate increased pain tolerance to migraine headache pain.
The results of this study indicate that while spiritual meditation does not reduce the severity of migraines among patients, it may lead to increased migraine pain tolerance. Reduced analgesic consumption in response to migraine headache pain may indicate greater pain tolerance among spiritual meditators compared to other forms of meditation or relaxation. The results of this study show that those who spiritually meditated had fewer migraine headaches, and the headaches they experienced were less likely to be deemed by the participants to require pain medication despite the migraine pain being perceived as severe.
Previous research has indicated that spiritual practices can modulate subjective pain experiences and increase laboratory-induced pain tolerance.11,12,18 Many different potential pathways for this link between spirituality and pain have been postulated and include: providing the patient with a framework by which to cope with the pain, by engendering feelings of control or self-efficacy in the patient,27 providing a distraction from the pain experience,28 or providing a source of social or spiritual support for the patient.29,30 These studies indicate that while the precise mechanisms by which spirituality impacts a patient’s pain experience have not been concretely established, spirituality needs to be recognized as an important psycho-social variable which influences the pain experience and analgesic use.
Certain meditation styles have been previously found to predict less negative appraisals of pain and a small study suggested that meditation may reduce analgesic medication usage for general pain.31,32 The effect may be enhanced with prolonged practice and familiarity with meditation practice. Long-term meditators appear to have better pain tolerance compared to meditation novices. Compared to non-meditators, long-term meditators rate pain stimuli as significantly less unpleasant despite rating the stimuli as intense of pain.33 Therefore, the improved pain tolerance among meditators may be a result of decreased pain-related distress which results in less need for pain medication.
This current study expands upon previously published research by incorporating a spirituality component into a meditation intervention. Our study is the only known investigation to have incorporated specific patient characteristics (spirituality) into a meditation intervention to assess analgesic medication consumption. Similar to previously published literature, we have found that participants are able to successfully complete a meditation regimen at home without close oversight and without interfering in their daily functioning. Our study is consistent with previous findings that meditation interventions do not reduce the perceived painfulness of the patients’ ailments and extends these studies with the unique finding that spiritual meditation is more effective at increasing pain tolerance and reducing analgesic medication use compared to other meditation styles.
Limitations
There are some limitations in the present study. The participants for this study were primarily composed of undergraduate students which limit the generalizability of this study to other individuals. Female participants also compose the vast majority of the sample of this study (89.1%), however migraine headache patients are 75% female.21 So while the gender imbalance of this study should be noted, it is similar to the gender differential of those affected by migraines. Recent findings have suggested that female hormones, specifically estrogen, may be related to migraines.34 Not controlling for female participant hormone levels may be an additional limitation to the present study however monitoring headaches for 30 days was designed to minimize the effect of hormonal cycles.
Conclusions
The results from this study support previous research suggesting that spiritual meditation may be more effective for pain tolerance and migraine coping than non-spiritual meditation alternatives. This study suggests that spiritual meditation is an effective means of mitigating the frequency of migraine headaches. Spiritual meditation has the additional benefit of leading to reduced analgesic medication use. The potential benefits of reduced analgesic use are numerous and include: reduced incidence of medication-overuse headaches, lower rates of medication abuse and addiction, and lower health care costs. The speed and ease with which patients learned to meditate provides support for the clinical applicability of using meditation as a non-pharmacological intervention for patients suffering from frequent migraines. The clinical applicability of a meditation intervention is further supported by the observation that patients are able and willing to practice meditation independently.
In light of the observed positive impact of meditation on migraine suffering as well as the cost and side effects of pharmaceutical interventions for migraine treatment,35 further research into the clinical applicability of meditation as an intervention for migraineurs is warranted. The brief spiritual meditation practice used in this study may provide mental health clinicians with a tool that can be adapted to multiple belief systems, quickly result in positive changes and can be used to integrate a patient’s spirituality into effective treatment for migraine headaches and reduced analgesic consumption. Future studies should examine the impact of this intervention on subjects drawn from pain clinics and the general population.
Acknowledgments
Funding for this study was provided by a Dissertation Fellowship from Bowling Green State University to AW and by an NIH-NIDA grant (#K23DA030397) to AW.
Footnotes
Publisher's Disclaimer: Disclaimer: This is a version of an unedited manuscript that has been accepted for publication. As a service to authors and researchers we are providing this version of the accepted manuscript (AM). Copyediting, typesetting, and review of the resulting proof will be undertaken on this manuscript before final publication of the Version of Record (VoR). During production and pre-press, errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal relate to this version also.
Taylor & Francis makes every effort to ensure the accuracy of all the information (the “Content”) contained in the publications on our platform. However, Taylor & Francis, our agents, and our licensors make no representations or warranties whatsoever as to the accuracy, completeness, or suitability for any purpose of the Content. Any opinions and views expressed in this publication are the opinions and views of the authors, and are not the views of or endorsed by Taylor & Francis. The accuracy of the Content should not be relied upon and should be independently verified with primary sources of information. Taylor and Francis shall not be liable for any losses, actions, claims, proceedings, demands, costs, expenses, damages, and other liabilities whatsoever or howsoever caused arising directly or indirectly in connection with, in relation to or arising out of the use of the Content.
This article may be used for research, teaching, and private study purposes. Any substantial or systematic reproduction, redistribution, reselling, loan, sub-licensing, systematic supply, or distribution in any form to anyone is expressly forbidden. Terms & Conditions of access and use can be found at http://www.tandfonline.com/page/terms-and-conditions
Amy Wachholtz, Christopher Malone, and Kenneth Pargament declare that they have no conflict of interest.
Contributor Information
Amy B Wachholtz, University of Massachusetts Medical School, Worcester, Massachusetts, USA, Amy.wachholtz@umassmemorial.org.
Christopher D Malone, University of Massachusetts Medical School, Worcester, Massachusetts, USA, Christopher.malone@umassmed.edu.
Kenneth I Pargament, Bowling Green State University, Bowling Green, Ohio, USA, kpargam@bgsu.edu.
References
- 1.Headache Classification Committee of The International Headache Society. The international classification of headache disorders, 2nd edition. Cephalalgia. 2004;24(Suppl 1):1–160. doi: 10.1111/j.1468-2982.2003.00824.x. [DOI] [PubMed] [Google Scholar]
- 2.Bigal M, Lipton R. The epidemiology, burden, and comorbidities of migraine. Neurol Clin. 2005;27(2):321–334. doi: 10.1016/j.ncl.2008.11.011. [DOI] [PubMed] [Google Scholar]
- 3.Stewart W, Wood G, Razzaghi H. Work impact of migraine headaches. JOEM. 2008;50(7):736–745. doi: 10.1097/JOM.0b013e31818180cb. [DOI] [PubMed] [Google Scholar]
- 4.DeMaagd G. The phamacological management of migraine, part 1. P T. 2008;33(7):404–416. [PMC free article] [PubMed] [Google Scholar]
- 5.Pesaturo KA, Wooding FG. Modern management of the migraine headache. Am J Lifestyle Med. 2009;3(2):147–159. [Google Scholar]
- 6.DeMaagd G. The pharmacological management of migraine, part 2: Preventative therapy. P T. 2008;33(8):480–487. [PMC free article] [PubMed] [Google Scholar]
- 7.Penzien DB, Rains JC, Andrasik F. Behavioral management of recurrent headache: Three decades of experience and empiricism. Appl Psychophy Biof. 2002;27:163–181. doi: 10.1023/a:1016247811416. [DOI] [PubMed] [Google Scholar]
- 8.Epel E, Daubenmier J, Moskowitz J, Folkman S, Blackburnc E. Can meditation slow rate of cellular aging? Cognitive stress, mindfulness, and telomeres. Ann N Y Acad Sci. 2009;1172:34–53. doi: 10.1111/j.1749-6632.2009.04414.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Manikonda JP, Störk S, Tögel S, et al. Contemplative meditation reduces ambulatory blood pressure and stress-induced hypertension: a randomized pilot trial. J Hum Hypertens. 2008;22(2):138–140. doi: 10.1038/sj.jhh.1002275. [DOI] [PubMed] [Google Scholar]
- 10.Oman D, Shapiro SL, Thoresen CE, Plante TG, Flinders T. Meditation lowers stress and supports forgiveness among college students: A randomized controlled trial. J Am Coll Health. 2008;56(5):569–578. doi: 10.3200/JACH.56.5.569-578. [DOI] [PubMed] [Google Scholar]
- 11.Wachholtz A, Pargament K. Is spirituality a critical ingredient of meditation? Comparing the effects of spiritual meditation, secular meditation, and relaxation on spiritual, psychological, cardiac, and pain outcomes. J Behav Med. 2005;28(4):369–384. doi: 10.1007/s10865-005-9008-5. [DOI] [PubMed] [Google Scholar]
- 12.Wachholtz A, Pargament K. Migraines and meditation: does spirituality matter? J Behav Med. 2008;31(4):351–366. doi: 10.1007/s10865-008-9159-2. [DOI] [PubMed] [Google Scholar]
- 13.Day M, Thorn B, Ward C, Rubin N, Hickman s, Scogin F, Kilgo G. Mindfulness-based cognitive therapy for the treatment of headache pain: A pilot study. Clinical Journal of Pain. 2014;30(2):152–161. doi: 10.1097/AJP.0b013e318287a1dc. [DOI] [PubMed] [Google Scholar]
- 14.Rosenzweig S, Greeson J, Reibel D, Green J, Jasser S, Beasley D. Mindfulness-based stress reduction for chronic pain conditions: Variation in treatment outcomes and role of home meditation practice. Journal of Psychosomatic Research. 2010;68:29–36. doi: 10.1016/j.jpsychores.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 15.Keefe F, Affleck G, Lefebvre J, et al. Living with rheumatoid arthritis: The role of daily spirituality and daily religious and spiritual coping. J Pain. 2001;2(2):101–110. doi: 10.1054/jpai.2001.19296. [DOI] [PubMed] [Google Scholar]
- 16.Jegindø E, Vase L, Skewes JC, Terkelsen AJ, Hansen J, Geertz AW, Roepstorff A, Jensen TS. Expectations contribute to reduced pain levels during prayer in highly religious participants. J Behav Med. 2013;36:413–426. doi: 10.1007/s10865-012-9438-9. [DOI] [PubMed] [Google Scholar]
- 17.Dezutter J, Wachholtz A, Corveleyn J. Prayer and pain: The mediating role of positive re-appraisal. Journal of Behavioral Medicine. 2011;34:542–549. doi: 10.1007/s10865-011-9348-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wachholtz AB, Pearce MJ, Koenig HG. Exploring the relationship between spirituality, coping, and pain. J Behav Med. 2007;30(4):311–318. doi: 10.1007/s10865-007-9114-7. [DOI] [PubMed] [Google Scholar]
- 19.Alexander C, Robinson D, Orme-Johnson R, Schneider R, Walton K. The effects of transcendental meditation compared to other methods of relaxation and meditation reducing risk factors, morbidity, and mortality. Homeostasis Hlth Dis. 1994;35:243–264. [Google Scholar]
- 20.Lipton RB, Dodick D, Sadovsky R, Kolodner K. A self-administered screener for migraine in primary care. Neurology. 2003;61(3):375–382. doi: 10.1212/01.wnl.0000078940.53438.83. [DOI] [PubMed] [Google Scholar]
- 21.Lipton RB, Bigal ME, Diamond M, et al. Migraine prevalence disease burden, and the need for preventive therapy. Neurology. 2007;68:343–349. doi: 10.1212/01.wnl.0000252808.97649.21. [DOI] [PubMed] [Google Scholar]
- 22.Fetzer Institute. Multidimensional Measurement of Religiousness/Spirituality for Use in Health Research. Kalamazoo, MI: John E. Fetzer Institute; 1999. [Google Scholar]
- 23.Underwood LG, Teresi JA. The daily spiritual experiences scale: Development, theoretical description, reliability, exploratory factor analysis, preliminary construct validity using health-related data. Annals of Behavioral Medicine. 2002;24:22. doi: 10.1207/S15324796ABM2401_04. [DOI] [PubMed] [Google Scholar]
- 24.Wagner TH, Patrick DL, Galer BS, Berson RA. A new instrument to assess the long-term quality of life effects from migraine: Development and psychometric testing of the MSQOL. Headache. 1996;36:484–492. doi: 10.1046/j.1526-4610.1996.3608484.x. [DOI] [PubMed] [Google Scholar]
- 25.French DJ, Holroyd KA, Pinell C, Malinoski PT, O’Donnell F, Hill KR. Perceived self-efficacy and headache related disability. Headache. 2000;40:647–656. doi: 10.1046/j.1526-4610.2000.040008647.x. [DOI] [PubMed] [Google Scholar]
- 26.Oxford Pain Site. [Retrieved May 12, 2007];Oxford League Table of Analgesics in Acute Pain. 2007 from http://www.jr2.ox.ac.uk/bandolier/booth/painpag/Acutrev/Analgesics/Leagtab.html. [Google Scholar]
- 27.Carver CS, Harris SD, Lehman JM, et al. How important is the perception of personal control? Studies of early stage breast cancer patients. Pers Soc Psychol B. 2000;26:139–150. [Google Scholar]
- 28.Alexander C, Rainforth M, Gelderloos P. Transcendental Meditation, self-actualization, and psychological health: A conceptual overview and statistical meta-analysis. J Soc Behav Pers. 1991;6:189–247. [Google Scholar]
- 29.Krause N. Church-based social support and mortality. J Gerontol B Psychol Sci Soc Sci. 2006;61B(3):S140–S146. doi: 10.1093/geronb/61.3.s140. [DOI] [PubMed] [Google Scholar]
- 30.Powell LH, Shahabi L, Thoresen C. Religion and spirituality: Linkages to physical health. Am Psychol. 2003;58(1):36–52. doi: 10.1037/0003-066x.58.1.36. [DOI] [PubMed] [Google Scholar]
- 31.Brown CA, Jones AK. Meditation experience predicts less negative appraisal of pain: electrophysiological evidence for the involvement of anticipatory neural responses. Pain. 2010;150(3):428–438. doi: 10.1016/j.pain.2010.04.017. [DOI] [PubMed] [Google Scholar]
- 32.Kabat-Zinn J, Lipworth L, Burney R. The clinical use of mindfulness meditation for the self-regulation of chronic pain. J Behav Med. 1985;8(2):163–190. doi: 10.1007/BF00845519. [DOI] [PubMed] [Google Scholar]
- 33.Perlman DM, Salomons TV, Davidson RJ, Lutz A. Differential effects on pain intensity and unpleasantness of two meditation practices. Emotion. 2010;10(1):65–71. doi: 10.1037/a0018440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chai NC, Peterlin BL, Calhoun AH. Migrain and estrogen. Curr Opin Neurol. 2014;27(3):315–324. doi: 10.1097/WCO.0000000000000091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bigal M, Borucho S, Serrano D, Lipton R. The acute treatment of episodic and chronic migraine in the USA. Cephalalgia. 2009;29(8):891–897. doi: 10.1111/j.1468-2982.2008.01819.x. [DOI] [PubMed] [Google Scholar]