Abstract
Drug Rash with Eosinophilia and Systemic Symptoms (DRESS) syndrome is characterised by fever, rash, eosinophilia and organ damage that develops 2–6 weeks after the initiation of a medication. We report a case of DRESS syndrome in a 79-year-old man that developed after the introduction of rifabutin, ethambutol and clarithromycin used to treat Mycobacterium avium complex (MAC) vertebral osteomyelitis. This case highlights treatment and management challenges in a patient with known MAC vertebral osteomyelitis requiring prolonged steroids. Steroids are the mainstays of treatment for moderate to severe cases of DRESS syndrome. Initiation of steroids for the treatment of DRESS syndrome among patients with concomitant infections requires multidisciplinary collaboration for optimal management.
Background
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS) syndrome is characterised by fever, eosinophilia, leucocytosis, lymphadenopathy, involvement of internal organs and a morbilliform eruption that progresses to a confluent rash or exfoliative dermatitis.1 DRESS syndrome results in a mortality rate as high as 10% mostly due to fulminant hepatitis.2 3
Reports of DRESS syndrome related to antimycobacterial therapy are few and are limited to cases related to tuberculosis treatment.4–6 A review of the literature shows that this is the first reported case of a patient with DRESS syndrome related to the treatment of Mycobacterium avium complex (MAC).
Case presentation
A 79-year-old man with a medical history of panhypopituitarism on chronic steroids, atrial fibrillation, coronary artery disease and chronic back pain, who was recently admitted 6 weeks prior to admission for MAC lumbar osteomyelitis related to steroid injections, was transferred to our hospital with fevers, altered mental status, generalised weakness and a diffuse rash.
Six weeks prior to admission, the patient was discharged on clarithromycin, rifabutin and ethambutol for MAC osteomyelitis. Two weeks prior to presentation, he noticed swelling and joint pains of the right hand. The week prior to presentation, a circular erythematous rash erupted on the dorsal surface of both forearms, followed by fever (38.1°C) and confusion. The rash spread to the trunk of his body, and the patient experienced daily fevers. The severity of his weakness, fatigue and debility prompted his family to bring him to an outside hospital, resulting in subsequent transfer to our hospital.
The patient's medications included clarithromycin, rifabutin, ethambutol, levothyroxine, hydrocortisone, tramadol, lisinopril, acetaminophen and carvedilol. He had a temperature of 39.1°C with a pulse of 105 bpm, a respiratory rate of 28 breaths/min, and a blood pressure of 147/22 mm Hg with an oxygen saturation of 97% on pulse oximetry on room air. On physical examination, the patient was toxic appearing and oriented only to person. He had a diffuse morbilliform eruption that was raised, erythematous and pruritic on the upper body extending from his face to his thighs bilaterally. He had swelling of his hands bilaterally with non-pitting oedema and tenderness to passive movement of his digits. On neurological examination, the patient had generalised weakness but no focal abnormalities.
Investigations.
Initial laboratory studies revealed a leucocytosis of 17×109/L with a neutrophilic predominance and an elevated eosinophil count of 1.2×109/L, C reactive protein was greater than the upper limit of 270 mg/L with normal transaminases aspartate aminotransferase (AST) 41 U/L and alanine transaminase (ALT) 56 U/L. Serum human herpesvirus 6 (HHV-6) PCR was not sent because it was decided that the result would not have changed our management.
Differential diagnosis
In the presence of fever, eosinophilia, rash and leucocytosis after 6 weeks of taking antimycobacterial drugs, the patient's presentation was consistent with DRESS syndrome. The time frame between the onset of the recently introduced antibiotics and the development of the patient's symptoms also supported this diagnosis. DRESS syndrome clinically presents 2–6 weeks after exposure to the inciting medication. In our case, the most likely inciting agents, the three antibiotics (rifabutin, ethambutol and clarithromycin), were introduced about 4 weeks prior to onset of the symptoms making the other drug-related syndromes unlikely. Establishing a time frame is critical for making a diagnosis and differentiating from other syndromes such as Stevens Johnson syndrome/toxic epidermal necrolysis and erythroderma, which occur 1–3 weeks after the inciting agent, or acute generalised exanthematous pustulosis, which occurs at 48 h after the drug exposure.7 Other differential diagnoses include viral infections or lymphoma.
Treatment
We consulted dermatology, allergy and infectious disease and discontinued all home medications including rifabutin and ethambutol. Patient was briefly on broad-spectrum coverage which was discontinued given stabilisation of vital signs and no growth in urine or blood cultures. We continued the patient's hydrocortisone (20 mg by mouth in the morning and 10 mg by mouth at night) for panhypopituitarism. Given the patient showed signs of improvement after withdrawal of the suspected offending medications and a known MAC infection of his spine with no initial signs of organ involvement, he was initially treated with topical steroids with no increase in his outpatient oral steroid dosage.
However, 5 days after admission the patient became confused and had fevers of 39.4°C and 38.4°C with increasing confusion and doubling of his AST and ALT to 86 and 104 U/L, respectively (figures 1 and 2). There was also an increase in his total eosinophil count compared to the prior day (figure 3). Given the patient's clinical deterioration, we started prednisone 40 mg daily to treat DRESS syndrome and discontinued the relatively lower steroid dose of oral hydrocortisone. This resulted in dramatic improvement and the patient became conversant, more alert and oriented to person, place and time with significant fading of his rash. He also had resolution of his eosinophilia and his liver function tests returned to normal.
Figure 1.
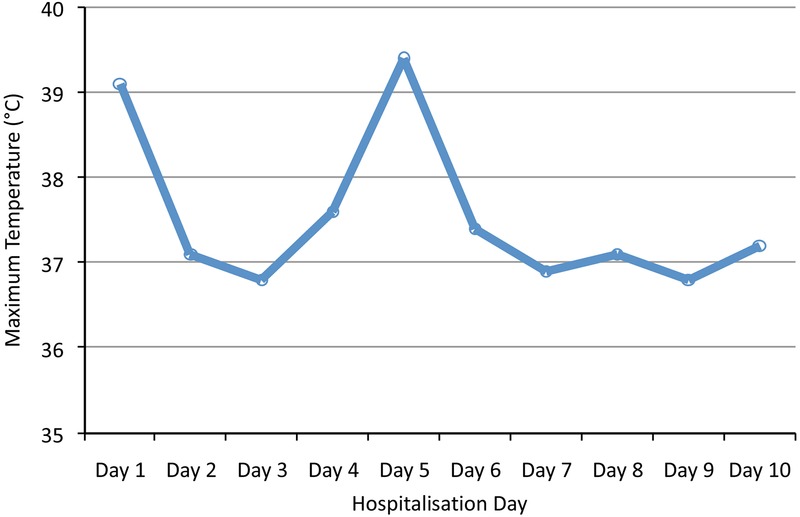
Temperature trend before and after steroids were administered on day 5.
Figure 2.
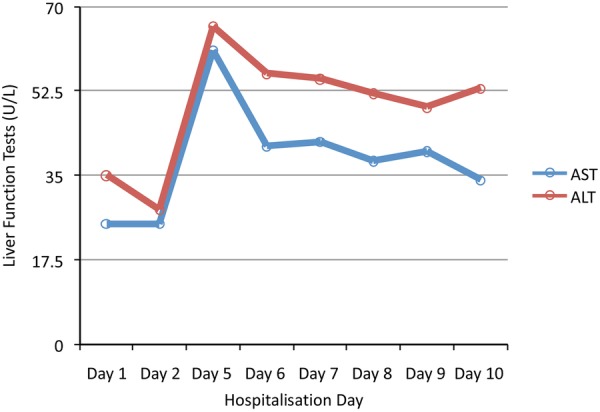
Transaminases before and after steroids administered on day 5 of hospitalisation.
Figure 3.
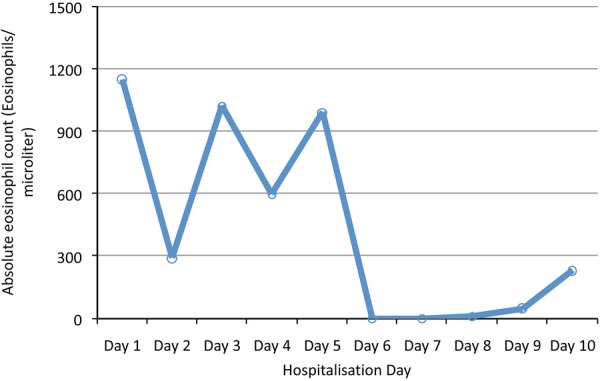
Improvement of eosinophilia after steroids administered on day 5.
Outcome and follow-up
The patient continued to have gradual improvement in his strength and he was discharged to an outpatient rehabilitation facility. His steroids were tapered with plans for reintroduction of his MAC antibiotics one at a time as managed by his allergy and immunology physician in collaboration with his infectious disease physician.
Discussion
DRESS syndrome was initially described in relation to anticonvulsants but has been associated with over 50 different medications including sulfonamides.8 The incidence has not been well studied but estimates range between 1 in 1000 to 1 in 10 000 drug exposures.8 DRESS has also been referred to as drug-induced hypersensitivity syndrome (DIHS) to place an emphasis on recent proposed pathophysiological mechanisms of the disease. These include genetic alterations in detoxification of medications with a resulting accumulation in toxic metabolites. Alternatively, viral activation of herpesviruses, HHV-6 in particular and the resulting interaction with T cells has been well described as a mechanism for disease.
Patients with DRESS initially have prodromal symptoms of fevers of 38.8°C to 40°C and pruritus preceding the rash by several days. The rash can be varied but is most commonly morbilliform and can mimic erythroderma. It usually develops on the face, upper torso and upper extremities and later spreads to the lower extremities as described in our patient. The rash can cover almost the entire skin and produce an exfoliative dermatitis with or without mucosal involvement.9
DRESS/DIHS related to antibiotics against tuberculosis has been described most frequently with the use of rifampin. There have also been cases related to ethambutol as in our patient.8 Given that our patient was initiated on an antibiotic regimen of three medications, it is difficult to determine which medication was the inciting drug. However, ethambutol is the only antibiotic that the patient was exposed to that has been clearly associated with DRESS syndrome.8 9 Reports of DRESS related to tuberculosis therapy have highlighted the difficulty in management due to uncertainty about the provoking antibiotic agent in addition to the requirement for prolonged steroid therapy during lapses in antibiotic treatment. These issues mirror our initial concerns about potentially worsening the patient's MAC osteomyelitis. Surprisingly, one case study found no worsening of tuberculosis during prolonged steroid therapy for DRESS syndrome in 11 patients.6 Our case exemplifies the need for multidisciplinary collaboration to provide the appropriate care for patients with DRESS.
Learning points.
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS) syndrome is characterised by fever, eosinophilia, leucocytosis, lymphadenopathy, involvement of internal organs and a morbilliform rash that develops 2–6 weeks after a drug exposure.
DRESS syndrome can be fatal and should be on the differential for patients presenting with altered mental status and a rash.
Many antibiotics including ethambutol have been associated with DRESS syndrome.
Clinicians must have a high index of suspicion and immediately suspend culprit drugs.
Steroids are the mainstay of treatment for moderate to severe cases of DRESS syndrome.
Footnotes
Contributors: PB is the guarantor of the paper, wrote the preliminary drafts and developed the idea for the paper. DH performed additional literatures searches, provided edits and added to the planning of the subject matter of the article. NA provided edits and helped with the clinical data gathering. WF provided edits and helped with the planning and overall concept of the manuscript. All authors were involved in the management of the patient.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Kano Y, Ishida T, Hirahara K et al. Visceral involvements and long-term sequelae in drug-induced hypersensitivity syndrome. Med Clin North Am 2010;94:743–59. 10.1016/j.mcna.2010.03.004 [DOI] [PubMed] [Google Scholar]
- 2.Walsh SA, Creamer D. Drug reaction with eosinophilia and systemic symptoms (DRESS): a clinical update and review of current thinking. Clin Exp Dermatol 2011;36:6–11. 10.1111/j.1365-2230.2010.03967.x [DOI] [PubMed] [Google Scholar]
- 3.Revuz J, Valeyrie-Allanore L. Drug reactions. In: Bolognia J, Jorizzo J, Schaffer J, eds. Dermatology. 3rd edn Elsevier, 2012:335. [Google Scholar]
- 4.Lee JH, Park HK, Heo J et al. Drug Rash with Eosinophilia and Systemic Symptoms (DRESS) syndrome induced by celecoxib and anti-tuberculosis drugs. J Korean Med Sci 2008;23:521–5. 10.3346/jkms.2008.23.3.521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Naziha K, Maha BS, Dorsaf M et al. DRESS syndrome caused by pyrazinamide. Egypt Dermatol Online J 2010;6:9–11. [Google Scholar]
- 6.Palmero D, Castagnino J, Musella RM et al. Difficult clinical management of anti-tuberculosis DRESS syndrome. Int J Tuberc Lung Dis 2013;17:76–8. 10.5588/ijtld.12.0441 [DOI] [PubMed] [Google Scholar]
- 7.Husain Z, Reddy BY, Schwartz RA. DRESS syndrome: part II. Management and therapeutics. J Am Acad Dermatol 2013;68:709.e1–9. 10.1016/j.jaad.2013.01.032 [DOI] [PubMed] [Google Scholar]
- 8.Cacoub P, Musette P, Descamps V et al. The DRESS syndrome: a literature review. Am J Med 2011;124:588–97. 10.1016/j.amjmed.2011.01.017 [DOI] [PubMed] [Google Scholar]
- 9.Husain Z, Reddy BY, Schwartz RA. DRESS syndrome: part I. Clinical perspectives. J Am Acad Dermatol 2013;68:693.e1–14. 10.1016/j.jaad.2013.01.033 [DOI] [PubMed] [Google Scholar]


