Abstract
Neglected anterior dislocation of shoulder is rare in spite of the fact that the anterior dislocation of the shoulder is seen in around 90% of the acute cases. Most of the series of neglected dislocation describe posterior dislocation to be far more common.1,2 We hereby report a case of the neglected anterior shoulder dislocation in a 15 year old boy who had a history of epilepsy. There was a large Hill Sachs lesion in humeral head which was impacted in glenoid inferiorly and glenoid was eburnated at that margin. The humeral head was reconstructed with a tricortical iliac graft. Glenoid was reconstructed by transfer of coracoids process of scapula to antero-inferior glenoid (modified Latarjet procedure). This case is unique because management of humeral head defect with bone graft is not mentioned in anterior dislocation.
Keywords: Hill Sach's, Latarjet procedure, Neglected shoulder dislocation
1. Case report
A 15 years old right handed student, under treatment for epilepsy in our institution, was referred to us by his treating physician for poor function of his right shoulder of four months duration after he suffered the last epileptic fit. On examination the right upper limb was in attitude of an abduction and external rotation.
The patient did not have much pain at rest and had not been using his shoulder for the last four months. Although the patient was regularly visiting the physician for the treatment of epilepsy, he had been neglecting his shoulder ailment mainly due to lack of pain at rest.
Plain radiographs i.eAP and axillary views [Figs. 1 and 2] confirmed an anterior dislocation of the right shoulder. A CT scan was ordered further to elaborate the pathological anatomy [Fig. 3]. The extent and location of the Hill Sachs lesion could be very well elaborated.
Fig. 1.
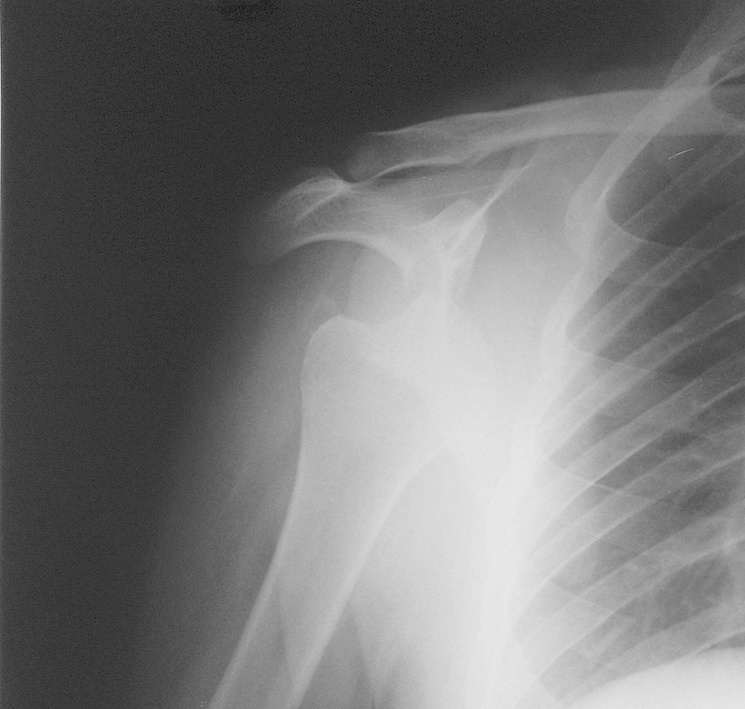
AP radiograph of neglected shoulder dislocation.
Fig. 2.

Axillary lateral radiograph showing engaging Hill Sachs.
Fig. 3.

Coronal CT cut at the level of engaging Hill Sachs lesion.
Closed reduction of the shoulder under general anaesthesia was unsuccessful and we resorted to open reduction in the beach chair position, using the delto-pectoral interval. Subscapularis and the joint capsule were incised near their attachment to humeral head leaving a cuff of tissue there for the repair later on. At the time of reduction, there was a significant Hill Sachs lesion noticed in the posterior part of the head that was engaging on the anterior glenoid margin in just five degrees of external rotation thus causing an unstable reduction. Glenoid was eburnated at that margin. This lesion was more than 40% of the humeral head in diameter. During intra-operative assessment we noticed that shoulder would dislocate and lesion would re-engage on just crossing the neutral rotation towards five degree external rotation. Tricortical iliac crest graft with thin layer of soft tissue attached to the crest part, that would replace the cartilaginous part of head was harvested, contoured and applied in the defect and fixed with a 60 mm, 4 mm partially threaded cancellous screws [Fig. 4]. After grafting the defect, shoulder would dislocate only by extreme external rotation in neutral position and at 20° of external rotation in 90° abduction. To provide a stable reduction we resorted to transferring of the coracoid process to the antero-inferior margin of the glenoid which was fixed with a screw. The joint capsule and subscapularis was repaired by double breasting on tissue sleeve which was left earlier there. Wound was closed on negative suction drain. The patient was immobilised in a cuff and collar sling for three weeks and pendular exercises were started after three weeks. Passive abduction was started at four weeks and active abduction allowed at twelve weeks. Post operative X-rays showed reduced shoulder joint with a well placed tricortical iliac graft in Hill Sach's lesion. Patient was followed at monthly intervals till 6 months and then at 3 monthly interval for 2 years. At final follow up the shoulder was well located and he had no pain at rest & abduction was upto 110° and flexion was full [Figs. 5 and 6]. Oxford instability index was 39.3
Fig. 4.
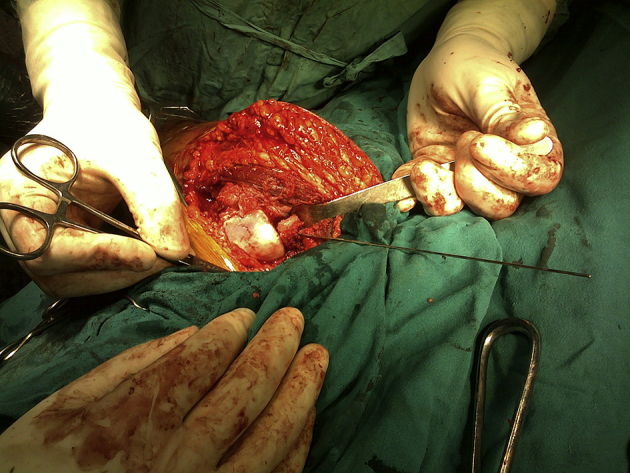
Tricortical iliac graft being fixed into Hill Sachs lesion.
Fig. 5.
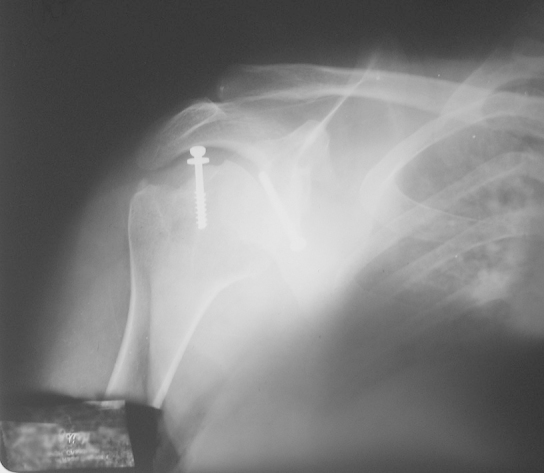
X-rays showing healing of graft in the lesion at 1 year.
Fig. 6.

Abduction at 1 year follow up.
2. Discussion
Neglected shoulder dislocations are most commonly seen in elderly patients in whom the functional demands are much less compared to young adults. Most of the neglected dislocations are posterior and cause very little functional problems due to the attitude of internal rotation1. This may also be partly due to fact that the AP radiograph of shoulder in case of anterior shoulder dislocation clearly shows the lesion, while it is often considered negative in case of posterior shoulder dislocation.2 A neglected anterior shoulder dislocation in young adult male that has been neglected for four months makes is a challenging task.
Plausible explanation for such a large defect could be recurrent dislocation leading to gradually increasing size of defect, ultimately precipitating an irreducible dislocation. Another reason could be damage caused by prolonged fits or status epilepticus, or with repeated attempts at movements of a dislocated shoulder.
Antero-inferior glenoid was eburnated which could have been due to previous dislocations which was not reported by patient to us in history.
Besides the restoration of normal anatomy of the shoulder joint the treatment focuses on the restoration of the humeral head and creating a restraint to prevent further shoulder dislocation.4 A large impression fracture has been often attributed to be a cause of failure of open reduction.5 Literature is still unclear about the management of the large humeral head bone defects. While Latarjet procedure remains gold standard researchers have reported a re-dislocation rate of 0–12% with it also.6,7 Hemiarthroplasty has been suggested as treatment for a large impression2 fracture but every attempt should be made to salvage the humeral head in a young adult.
Transfer of osteotomized coracoid process into the glenoid rim was described by Latarjet in 1958.8 This technique was popularised by Helfet9 who named it after Bristow. While in Bristow procedure only the tip of coracoid is transferred to glenoid rim in Latarjet procedure the transfer includes a portion of coracoacromial ligament which is sutured to the anterior capsule through a short horizontal incision in subscapularis. Latarjet procedure reconstructs the depth and width of the glenoid. A dynamic reinforcement is created for inferior part of the capsule through the coracobrachialis muscle which is particularly effective when arm is abducted and externally rotated.10
Osteochondral allograft transfer to the lesion has been described in literature.11,12 This procedure involves the transfer of allograft osteochondral fragment into the humeral head defect and thereby eliminating the chances of humeral head engagement. With this technique chance of disease transmission, graft resorption and cost consideration remain. Gerber described use of allograft for such dislocation with very good results. Unfortunately allograft is not used at our institution because of various reasons. Iliac crest is the choice for autogenous graft for structural purposes. Tricortical could be easily contoured into shape and packed into the defect. Autogenous graft is rapidly incorporated at the host bed compared to allograft.
While reviewing the literature we came across a few series of matched allograft13,14 usages for neglected posterior dislocation, we did not come across with any such series for neglected anterior dislocation. Although the iliac crest graft cannot be perfectly contoured to spherical humeral head; the patient did not have any signs of osteoarthritis till the final follow up. A longer follow-up is required to make a definite conclusion.
Humeral head osteotomy has also been used for treating a large hill sach lesion.15 This technique involves retroversion of the osteotomized head thereby preventing the engagement of hill sach lesion. The draw backs of this procedure are hardware problems and restriction of internal rotation.
Purchase et al16 recently have described capsulo-tenodesis of posterior capsule and infraspinatus tendon to fill hill sach lesion known as remplissage in French. This is an arthroscopic technique and we could not apply it in our case as we were dealing with a neglected shoulder dislocation of more than four month duration for which open reduction was needed.
Abdelhady17 described a technique of open remplissage technique recently in 4 cases of neglected locked anterior dislocation with good results. We have had no experience with this technique.
3. Conclusion
A rare case of neglected anterior dislocation of shoulder is presented which was managed by a novel technique using a combination of humeral head reconstruction with autogenous tricortical graft and modified Latarjet procedure.
Conflicts of interest
All authors have none to declare.
Footnotes
The work was done at Department of Orthopedics, Government Medical College and Hospital, Chandigarh, India.
References
- 1.Goga I.E. Chronic shoulder dislocations. J Shoulder Elbow Surg. 2003;12:446. doi: 10.1016/s1058-2746(03)00088-0. [DOI] [PubMed] [Google Scholar]
- 2.Rowe R.C., Zarins B. Chronic unreduced dislocation of the shoulder. J Bone Joint Surg Am. 1982;64A:494. [PubMed] [Google Scholar]
- 3.Dawson J., Fitzpatrick R., Carr A. The assessment of shoulder instability. The development and validation of a questionnaire. J Bone Joint Surg Br. 1999;81-B:420. doi: 10.1302/0301-620x.81b3.9044. [DOI] [PubMed] [Google Scholar]
- 4.Hawkins R.J., Neer C.S., 2nd, Pinta R.M., Mendoza F.X. Locked posterior dislocation of the shoulder. J Bone Joint Surg Am. 1987;69:9–18. [PubMed] [Google Scholar]
- 5.Hovelius L., Augustini B.J., Fredrin H., Johnasson O., Norlin R., Thorling J. Primary anterior dislocation in young patients. A ten year prospective study. J Bone Joint Surg Am. 1996;78:1667–1684. doi: 10.2106/00004623-199611000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Allain J., Gotallier D., Glorion C. Long term results of Latarjet procedure for treatment of anterior instability of shoulder. J Bone Joint Surg Am. 1998;80:841–852. doi: 10.2106/00004623-199806000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Bukhart S.S., De Beer J.F., Barth J.R. Results of modified latarjet reconstruction in patients with anteroinferior instability and significant bone loss. Arthroscopy. 2007;23:1033–1041. doi: 10.1016/j.arthro.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 8.Latarjet Technique of coracoid preglenoid arthroereisis in treatment of recurrent dislocation of shoulder. Lyon Chir. 1958;54:604–607. J Bone Joint Surg Br 1958;40:198–202. [PubMed] [Google Scholar]
- 9.Helfet A.J. Coracoid transplantation for recurring shoulder dislocation. J Bone Joint Surg Br. 1958;40-B:198–202. doi: 10.1302/0301-620X.40B2.198. [DOI] [PubMed] [Google Scholar]
- 10.Millet P.J., Clavert P., Warner J.J.P. Open operative treatment for anterior shoulder instability: when and why. J Bone Joint Surg Am. 2005;87:419–432. doi: 10.2106/JBJS.D.01921. [Review] [DOI] [PubMed] [Google Scholar]
- 11.Kropf E.J., Sekiya J.K. Osteoarticular allograft transplantation for large humeral head defects in gleno-humeral instability. Arthroscopy. 2007;23 doi: 10.1016/j.arthro.2006.07.032. 322.e1–322.e5. [DOI] [PubMed] [Google Scholar]
- 12.Miniaci A., Berlet G. recurrent anterior instability following failed surgical repair, allograft reconstruction of large humeral head defects. J Bone Joint Surg Br. 2001;83:19–20. [Google Scholar]
- 13.Gerber C., Lambert S.M. Allograft reconstruction of segmental defects of humeral head for the treatment of chronic locked posterior shoulder dislocation of shoulder. J Bone Joint Surg Am. 1996;78:376–382. doi: 10.2106/00004623-199603000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Chalidis B.E., Papadoupoulos P.P., Dimitriou C.G. Reconstruction of a missed posterior locked shoulder fracture-dislocation with bone graft and lesser tuberosity transfer: a case report. J Med Case Rep. 2008;2:260. doi: 10.1186/1752-1947-2-260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weber B.J., Simpson L.A., Hardegger F. Rotational humeral head osteotomy for recurrent anterior dislocation of shoulder associated with a large Hill Sach lesion. J Bone Joint Surg Am. 1984;66:1443–1450. [PubMed] [Google Scholar]
- 16.Purchase R.J., Wolf E.M., Hobgood E.R., Pollock M.E., Smalley C.C. Hill-sachs “remplissage”: an arthroscopic solution to engaging hill-sachs lesion. Arthroscopy. 2008;24:723–726. doi: 10.1016/j.arthro.2008.03.015. [DOI] [PubMed] [Google Scholar]
- 17.Abdelhady A.M. Neglected anterior shoulder dislocation: open remplissage of Hill-Sachs lesion with infraspinatus tendon. Acta Orthop Belg. 2010;76:162–165. [PubMed] [Google Scholar]


