Abstract
Introduction
Solitary plasmacytoma of bone is a local primary bone tumour consisting of malignant plasma cells without systemic involvement.
These tumours are known for large amount of blood loss, and the use of electrocautery is helpful in reducing blood loss and performing surgery in a relatively bloodless field; however, use of unipolar cautery in patients with indwelling cardiac pacemaker is known to cause arrhythmias and cardiac events.
Minimally invasive techniques offer potential advantages over open techniques particularly in patients with spinal tumours, where massive amount of blood loss is expected, if open procedure is performed.
Here, we present a case of solitary L3 plasmacytoma with progressive neurological deficit with chronic refractory anaemia with indwelling cardiac pacemaker treated by minimally invasive technique.
Materials and methods
A 71-year-old male presented with increasing back pain with Left L3 radiculopathy since 6 months and progressive left lower limb weakness since 5 days.
The patient is a known case of chronic renal failure with chronic refractory anaemia. The patient has indwelling cardiac pacemaker for cardiac arrhythmias.
Radiology was suggestive of L3 body plasmacytoma. L3 corpectomy and anterior column reconstruction with expandable cage and posterior stabilization by minimally invasive techniques were performed.
Results
Two years of follow-up showed no local recurrence. The patient is ambulatory unaided with no neurological deficit and backache.
Discussion
There is no consensus regarding appropriate surgical approach and perioperative strategies in treatment of solitary plasmacytoma. A solitary plasmacytoma was found in the spine of a patient with cardiac pacemaker where anaesthetic consideration, blood loss and the use of electrocautery were the limiting factors. Minimally invasive approach is a good option.
Keywords: Plasmacytoma, Minimally invasive approach, Corpectomy, Cardiac pacemaker, Cautery
1. Background
Solitary plasmacytoma is a local primary bone tumour consisting of malignant plasma cells without systemic involvement, constituting around 10% of all plasma cell neoplasms.1
The overall prognosis and survival of localized plasmacytomas are much better than that of an overt myeloma, with complete recovery in some, after adequate local therapy.
These tumours are known for large amount of blood loss, and the use of electrocautery is helpful in reducing blood loss and performing surgery in a relatively bloodless field; however, the use of unipolar cautery in patients with indwelling cardiac pacemaker is known to cause arrhythmias and cardiac events.2
Minimally invasive techniques offer potential advantages over open techniques, particularly in patients with spinal tumours, where massive amount of blood loss is expected, if open procedure is performed.
The incorporation of evolving minimally invasive access techniques has the potential to minimize associated morbidities without compromising the goals of surgery.3
Here, we present a case of solitary L3 plasmacytoma with progressive neurological deficit and having chronic refractory anaemia with indwelling cardiac pacemaker treated with minimally invasive technique.
There are few studies in literature highlighting the use of minimal access spinal surgeries in the treatment of plasmacytoma, but none of the studies have shown how to approach a patient with indwelling cardiac pacemaker with a comorbidity of chronic renal failure with refractory anaemia.
2. Case report
A 71-year-old male presented with increasing back pain with Left L3 radiculopathy since 6 months and progressive left lower limb weakness since 5 days. The patients’ activity of daily living was affected because of pain and sleep was disturbed because of pain at night. There was no bowel and bladder disturbance.
The patient is a known case of chronic renal failure with chronic refractory anaemia of Hb-6gm%. The patient had undergone indwelling cardiac pacemaker for cardiac arrhythmias 20 years back.
Transpedicular biopsy of vertebral lesion was suggestive of plasma cell tumour.
Clinically, midline tenderness presents at L3 region, and manual muscle testing revealed Left L3-grade 3/5 and L4, L5-grade 4/5 weakness. Hypoaesthesia was seen in Left L4 dermatome.
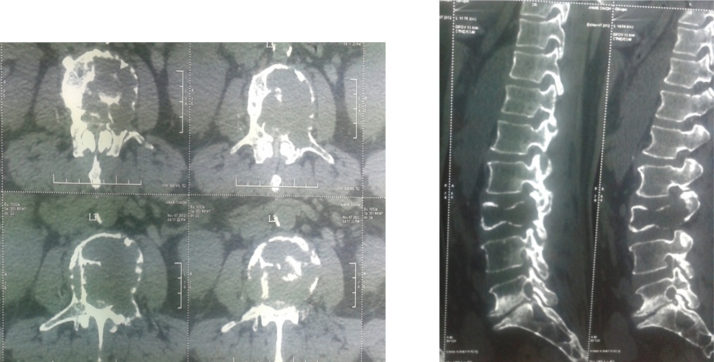
Plain radiographs (Fig. 1) and CT scan (Fig. 2) showed a single osteolytic lesion in L3 vertebral body. MR imaging was deferred in view of indwelling cardiac pacemaker. Further diagnostics following recommended algorithm for tumour screening were negative.
Fig. 1.
Pre-operative A.P. (Anterio-Posterior) and lateral X-rays showing osteolytic lesion in the L3 vertebral.
Fig. 2.
CT scan showing lytic destruction of L3 vertebral body and Left L3 pedicle.
In view of progressive neurological deficit and anaemia with indwelling cardiac pacemaker, the use of electrocautery is a limiting factor. Minimally invasive technique using stand-alone posterior approach was performed.
3. Surgical procedure
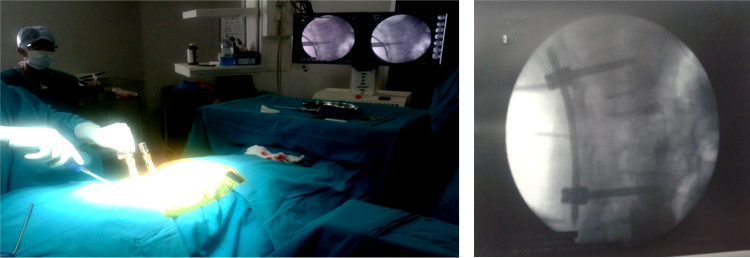
Under intraoperative neuromonitoring, the patient was placed in prone position on a radiolucent operating table. Using C-arm fluoroscopic guidance percutaneous pedicle screw fixation of L2 and L4 was performed on the right side using a stab incision (Fig. 3) and a connecting rod was inserted.
Fig. 3.
Using C-arm fluoroscopic guidance percutaneous pedicle screw fixation of L2 and L4 was performed on the right side using a stab incision.
The pedicles were cannulated on the ipsilateral side simultaneously, but K-wires were left in place during the initial portion of the operation.
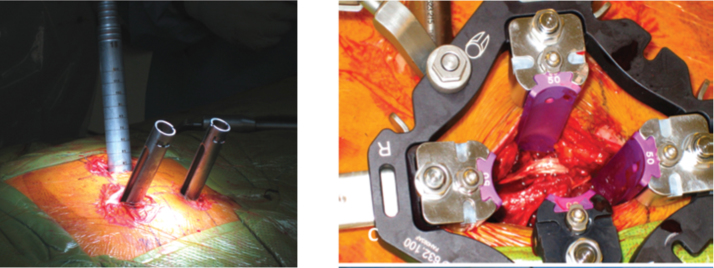
Using fluoroscopic guidance, a K-wire was then inserted percutaneously and docked on the lateral facet at the level of the pathology. Sequential soft tissue tubular dilators were used to separate the posterior musculature (Fig. 4).
Fig. 4.
Docking on the lateral facet at the level of the pathology. Sequential soft tissue tubular dilators were used to separate the posterior musculature.
Subperiosteal dissection was carried out with the help of Cobbs elevator, and the ipsilateral lamina, facet and transverse process were exposed. Facet, pedicle and lamina were then removed.
Dural sac and Left L3 nerve root were seen tangled in the tumour mass, which was freed and decompressed. The L3 corpectomy was then completed with the combined use of the high-speed drill, osteotomes, curettes and pituitary and Kerrison rongeurs.
Bleeding was controlled by bipolar cautery, surgicel and surgical patties.
Anterior column was reconstructed by inserting expandable cage. The insertion of a collapsed cage is facilitated by having performed a wide dissection of the superior and inferior nerve roots at that level. The cage was delivered in an oblique fashion via the inter nerve corridor; after it has crossed the nerve roots, the cage was rotated into the desired vertical position.
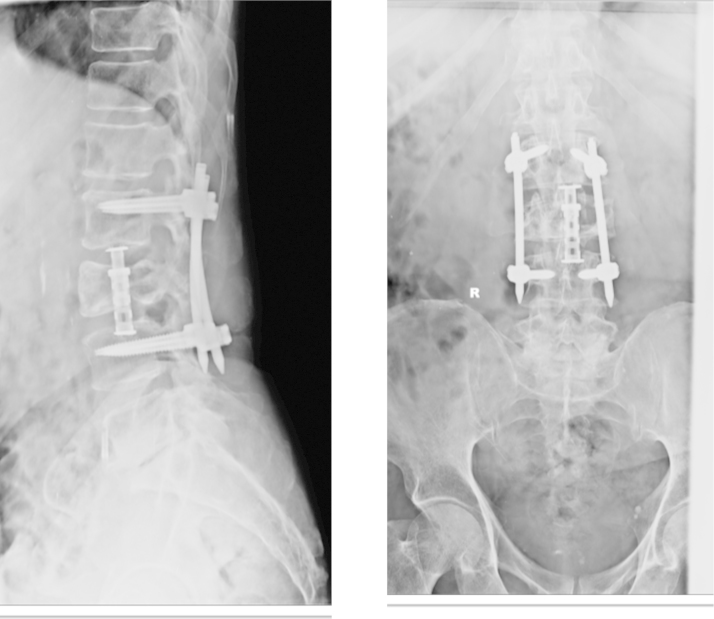
Posterior stabilization was completed by insertion of percutaneous pedicle screws in Left L2, L4 pedicles and insertion of connecting rod (Fig. 5).
Fig. 5.
Post-operative A.P. (Anterio-Posterior) and lateral view showing posterior stabilization with L2–L4 pedicle screw and L3 reconstruction with expandable cage.
The surgery lasted 5 h, the estimated blood loss was 200 ml, and there were no changes in the evoked motor potentials for the entirety of the case.
Biopsy was diagnostic of plasmacytoma.
4. Results
After surgery, the patient was examined daily while in the hospital and then at 1 and 6 weeks after discharge. Follow-up evaluations were then conducted at 3–6-month intervals for the 1st year and thereafter yearly interval showed no local recurrence or disease progression clinically and radiologically.
The patient was scheduled for localized radiotherapy and chemotherapy periodically.
The patient is ambulatory unaided with no neurological deficit or backache at end of 2 years (Fig. 6).
Fig. 6.
Two-year-old follow-up X-rays A.P. and lateral view showing no evidence of recurrence and implants are holding good without evidence of implant failure.
5. Discussion
There is no clear consensus in the literature regarding appropriate surgical approach and perioperative strategies in the treatment of solitary plasmacytoma.
The modern concept of surgery for spinal tumours involves radical excision with the primary goal of local cure and secondary goals of alleviating pain, preserving neurological status and stabilizing the spine.4
Traditional combined anterior and posterior approaches for lumbar vertebral tumours are associated with a higher complication rate than those involving single-stage surgery.
However, the conventional open surgeries are associated with increased blood loss, higher incidence of infection and longer duration of surgery.
Our patient in this study was considered a poor candidate for an open combined/single approach surgery in view of his refractory anaemia secondary to chronic renal failure with indwelling cardiac pacemaker.
Recent advances in the application of minimally invasive techniques have allowed many traditional spinal surgeries to be completed with a focus on minimizing injury to the soft tissue and decreasing blood loss.5
Minimally invasive techniques, especially in patients with spinal tumours may benefit from the option of less invasive techniques for tumour ablation, resection, reconstruction, and stabilization.6
An important advantage of minimally invasive approach, as opposed to midline posterior approaches, is the preservation of the midline posterior tension band. It also allows the ability to create longer constructs by placing percutaneous screws above and below the level of corpectomy.6
The lumbar spine poses unique challenges that make a minimal access posterior-only approach for corpectomy technically demanding because of the depth of the operative field and the need to navigate around lumbar nerve roots that need to be preserved.7,8
Reconstruction of the anterior column with expandable cage facilitates the restoration of vertebral body height and restores sagittal balance.
The small size of these cages is useful for initial placement. This is particularly relevant in the cases that involve lumbar pathology where the segmental nerve root cannot be sacrificed.9
The expandable cage protects both the exiting and traversing nerve roots and allows the surgeon to treat the anterior and posterior column via a single posterior incision.
The advantage of the expandable cage is that it is easy to place because it permits an optimal, tight fit and correction of the deformity by in vivo expansion of the device.
Electrocautery causes temporary inhibition or triggering of output, reversion to an asynchronous mode, inappropriate reprogramming, induced AF and VF and burns at lead–tissue interface.
If electrocautery is to be used, pacemakers should be placed in a triggered or asynchronous mode; ICDs should have arrhythmia detection suspended before surgery.
The solution to tackle this is to use the appropriate programming device to convert to an asynchronous mode and use electrocautery for only 1-s bursts, allowing 10 s for proper device function. When possible, bipolar electrocautery should be used.2
In our case, we did not use monopolar cautery, and the bleeding was controlled mainly by using surgicels, surgical patty and cautiously bipolar cautery in 1-s bursts.
6. Conclusions
A solitary plasmacytoma was found in the spine in a patient with progressive neurological deficit and also having chronic refractory anaemia with indwelling cardiac pacemaker where anaesthetic consideration, blood loss and the use of electrocautery (there is a concern about pacemaker inhibition) were limiting factors. Minimal access spine surgery is a good option.
Minimally invasive approaches for corpectomy in the lumbar spine offer substantial exposure-related advantages compared to their open counterparts.
Anterior column reconstruction in lumbar spine by using expandable cages by minimally invasive technique protects both exiting and traversing nerve roots, avoids the complications of combined anterior–posterior surgery and facilitates a quicker recovery and shorter hospitalization.
Conflicts of interest
All authors have none to declare.
References
- 1.Mclain R.F., Weinstein J.N. Solitary plasmacytomas of the spine: a review of 84 cases. J Spinal Disord. 1989;2:69–74. [PubMed] [Google Scholar]
- 2.John D.M., Asim F.C., Jonathan C. Surgical Management of the patient with an implanted cardiac device. Ann Surg. 2001;230(5):639–647. doi: 10.1097/00000658-199911000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Binning M.J., Gottfried O.N., Klimo J. Minimally invasive treatments for metastatic tumors of the spine. Neurosurg Clin N Am. 2004;15:459–465. doi: 10.1016/j.nec.2004.04.010. [DOI] [PubMed] [Google Scholar]
- 4.Sundaresan N., DiGiacinto G.V., Hughes J.E.O. Surgical approaches to primary and metastatic tumors of the spine. In: Schmidek H.H., Sweet W.H., editors. Operative Neurosurgical Techniques: Indications, Methods, Results. Grune & Stratton; Orlando, FL: 1988. pp. 1525–1537. [Google Scholar]
- 5.Rampersaud Y.R., Annand N., Dekutoski M.B. Use of minimally invasive surgical techniques in the management of thoracolumbar trauma: current concepts. Spine. 2006;31(suppl 11):S96–S102. doi: 10.1097/01.brs.0000218250.51148.5b. [DOI] [PubMed] [Google Scholar]
- 6.Guiot B.H., Khoo L.T., Fessler R.G. A minimally invasive technique for decompression of the lumbar spine. Spine (Phila Pa 1976) 2002;27:432–438. doi: 10.1097/00007632-200202150-00021. [DOI] [PubMed] [Google Scholar]
- 7.Jandial R., Kelly B., Chen M.Y. Posterior-only approach for lumbar vertebral column resection and expandable cage reconstruction for spinal metastases – clinical article. J Neurosurg Spine. 2013;19:27–33. doi: 10.3171/2013.4.SPINE12344. [DOI] [PubMed] [Google Scholar]
- 8.Hunt T., Shen F.H., Arlet V. Expandable cage placement via a posterolateral approach in lumbar spine reconstructions. Technical note. J Neurosurg Spine. 2006;5:271–274. doi: 10.3171/spi.2006.5.3.271. [DOI] [PubMed] [Google Scholar]
- 9.Smith Z.A., Li Z., Chen N.F., Raphael D., Khoo L.T. Minimally invasive lateral extracavitary corpectomy: cadaveric evaluation model and report of 3 clinical cases. J Neurosurg Spine. 2012;16:463–470. doi: 10.3171/2012.2.SPINE11128. [DOI] [PubMed] [Google Scholar]