Abstract
Persistent left superior vena cava (PLSVC) can be incidentally detected during pacemaker implantation from the left pectoral side. Optimal site pacing is technically difficult, and lead stability of the right ventricle (RV) can lead to such a situation. We describe a case of successful single-chamber pacemaker implantation in a 76-year-old woman with a PLSVC and concomitant agenesis of the right-sided superior vena cava, after failed attempts with the conventional procedure. The pacemaker had been working well after 12 months of follow-up.
Abbreviations: CS, coronary sinus; PLSVC, persistent left superior vena cava; RV, right ventricle; SVC, superior vena cava
Keywords: Persistent left superior vena cava, Agenesis of the right-sided superior vena cava, Sinus node disease
1. Introduction
Persistent left superior vena cava (PLSVC) is an uncommon finding during pacemaker implantation and creates difficulties in device implantation, leading to complications. Few reports on successful pacemaker implantation have been published. We report a case of successful and uncomplicated pacemaker implantation in a 76-year-old woman with a PLSVC and concomitant agenesis of the right-sided superior vena cava (SVC).
2. Case report
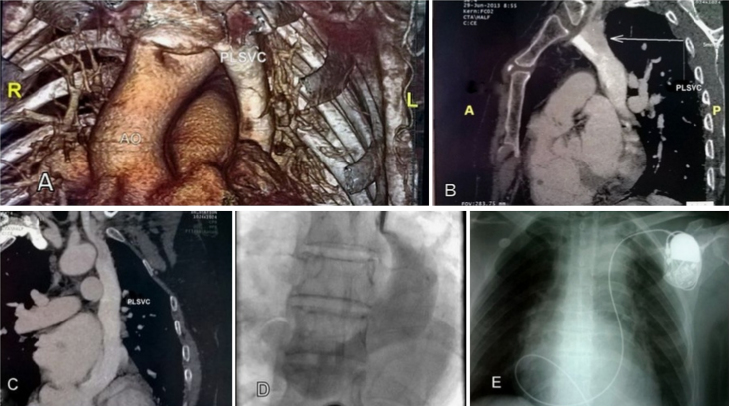
A 76-year-old woman presented to our department with sinus bradycardia-induced asthenia (38 beats/min). There were multiple pauses up to 7 s on telemetry monitoring with frequent episodes of paroxysmal atrial fibrillation. A sinus node dysfunction was made, and a single-chamber pacemaker was required. Her height was 150 cm. A first attempt for temporary pacing via the right subclavian vein failed because of the abnormal path of the wire, which made PLSVC possible. The patient was given isoprenaline and scheduled for a left-sided permanent pacemaker implantation. A thoracic computed tomography (CT) scan was thus performed, showing clearly the PLSVC with a posterior target behind the left atrium, ending in a dilated coronary sinus (CS) with an absent right SVC (Fig. 1A–C). After an easy puncture of the left subclavian vein, a wire was introduced, toward the left downward pathway. We used a catheter to visualize the CS that was drained into the right atrium (Fig. 1D). A 58 cm St Jude Medical active-fixation pacing lead (model 2088TC/58) was inserted through the left superior vena cava by using a steerable stylet. A wide loop of the lead was made in the right atrium, and the tip of the lead was directed toward the tricuspid valve using the curved stylet. After a few manipulations, the lead could be positioned in the RV apex (Fig. 1E). The lead parameters were satisfactory, with a pacing threshold of 0.7 V at a 0.5-ms pulse width, a pacing impedance of 564 Ω, and R-wave amplitude of 10.2 mV. The device was connected to the lead and implanted in the left pectoral region. The total fluoroscopy time for the procedure was 14 min. The pacing thresholds were good, and no complication occurred intra- and post-procedurally. The patient was doing well 1 year post-pacemaker implantation. Transthoracic echocardiography (TTE) ruled out any associated complications.
Fig. 1.
(A–C) A thoracic CT scan showing the PLSVC and absent right superior vena cava. (D) A venoogram showing a large coronary sinus drained in the right atrium. (E) A radiograph in the antero-posterior view showing a ventricular lead implanted in the right ventricle via atrial loop. PLSVC: persistent left superior vena cava, Ao: aorta.
3. Discussion
PLSVC with an absent right superior vena cava is a rare anatomic variation (0.07–0.13%) [1]. It represents the most common variation of the thoracic venous system, typically asymptomatic and discovered incidentally during device implantation.
In normal embryogenesis, the left cardinal vein involutes to form the ligament of Marshall, the right cardinal vein and the superior connection between the left and right cardinal veins persist to form the superior vena cava and the brachiocephalic vein, respectively. PLSVC is when involution of the anterior cardinal vein does not occur. It is more frequently connected to the coronary sinus (92%) rather than the left atrium (8%). In most cases, a normal right-sided SVC is present, as well as a left brachiocephalic vein [2]. Associated cardiac abnormalities such as atrial septal defect and bicuspid aortic valve commonly occur. PLSVC is even more frequent (12%) in the presence of other congenital heart abnormalities [2].
PLSVC is a rare finding during pacemaker implantation. The number of detected cases has increased with the increasing number of pacemaker implantation. The operator should be aware of the anatomic particularities, difficulties in lead fixation, and potential complications.
When present, a PLSVC shows a left downward course before connection to the CS. An abnormal path of the leads should raise this possibility.
Most patients have a right SVC, which represents an option for pacemaker implantation; in our case, the right SVC was absent.
Jiang et al. recommended that in such cases, a PLSVC should be identified preoperatively, to avoid the cephalic vein, as the lead may be short and not reach the target site [3].
In daily practice, the diagnosis may be suspected on TTE that reveals CS dilatation and confirmed by CT scan or magnetic resonance imaging. Injecting an agitated saline (bubble study) or contrast dye into the arms’ vein confirms easily the TTE diagnosis avoiding further invasive examinations and favoring correct planning of the implantation technique.
Conflict of interest statement
The authors have no conflict of interest.
References
- 1.Heye T., Wengenroth M., Schipp A. Persistent left superior vena cava with absent right superior vena cava: morphological CT features and clinical implications. Int J Cardiol. 2007;116(3):e103–e105. doi: 10.1016/j.ijcard.2006.08.067. [DOI] [PubMed] [Google Scholar]
- 2.Povoski S.P., Khabiri H. Persistent left superior vena cava: review of the literature, clinical implications, and relevance of alterations in thoracic central venous anatomy as pertaining to the general principles of central venous access device placement and venography in cancer patients. World J Surg Oncol. 2011;9:173. doi: 10.1186/1477-7819-9-173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jiang M., Shen X., Zhou S. Clinical consideration of cardiac pacemaker implantation through a persistent left superior vena cava with an absent right superior vena cava. Int J Cardiol. 2012;159(3):e59–e60. doi: 10.1016/j.ijcard.2011.12.029. [DOI] [PubMed] [Google Scholar]