Abstract
Although cancer arises from a combination of mutations in oncogenes and tumour suppressor genes, the extent to which tumour suppressor gene loss is required for maintaining established tumours is poorly understood. p53 is an important tumour suppressor that acts to restrict proliferation in response to DNA damage or deregulation of mitogenic oncogenes, by leading to the induction of various cell cycle checkpoints, apoptosis or cellular senescence1,2. Consequently, p53 mutations increase cell proliferation and survival, and in some settings promote genomic instability and resistance to certain chemotherapies3. To determine the consequences of reactivating the p53 pathway in tumours, we used RNA interference (RNAi) to conditionally regulate endogenous p53 expression in a mosaic mouse model of liver carcinoma4,5. We show that even brief reactivation of endogenous p53 in p53-deficient tumours can produce complete tumour regressions. The primary response to p53 was not apoptosis, but instead involved the induction of a cellular senescence program that was associated with differentiation and the upregulation of inflammatory cytokines. This program, although producing only cell cycle arrest in vitro, also triggered an innate immune response that targeted the tumour cells in vivo, thereby contributing to tumour clearance. Our study indicates that p53 loss can be required for the maintenance of aggressive carcinomas, and illustrates how the cellular senescence program can act together with the innate immune system to potently limit tumour growth.
p53 mutations are common in human liver cancer6, which is typically highly aggressive and resistant to non-surgical therapies. To determine the requirement for p53 loss in the maintenance of such carcinomas, we used reversible RNAi7 to control p53 in a chimaeric liver cancer mouse model (Fig. 1a)4,5. Purified embryonic liver progenitor cells (hepatoblasts) were transduced with retroviruses expressing oncogenic ras (HrasV12), the tetracycline transactivator protein tTA (‘tet-off’) and a tet-responsive p53 miR30 design short hairpin RNA (shRNA; Supplementary Fig. 1a)7,8, and seeded into the livers of athymic nude mice following intrasplenic injection4,5. To facilitate in vivo imaging, the oncogenic ras retrovirus co-expressed green fluorescent protein (GFP) and, in some experiments, hepatoblasts were also co-transduced with a luciferase reporter.
Figure 1. Reactivation of p53 results in liver tumour regression.

a, Embryonic liver progenitor cells were transduced with a tetracycline-regulatable p53 shRNA (TRE.shp53), tTA and H-rasV12. After onset of liver tumours, p53 expression could be restored by doxycycline (Dox) treatment. b, Reactivation of p53 leads to rapid tumour regression. Tumour-bearing mice were treated with Dox starting at day 0 and imaged at the indicated time points (n = 9). c, Subcutaneous tumours derived from ras-transformed liver progenitor cells with tet-off shRNA (TRE.shp53) or a non-regulatable shRNA (MLS.shp53) were grown in nude mice. Values represent mean ± s.d. (n = 4). d, p53 reactivation is reversed by Dox withdrawal. Protein lysates from liver progenitor cells pulse-treated with Dox for 4 days were immunoblotted for p53. e, Representative mice (n = 6) as in b were pulse-treated with Dox for 4 days and imaged at the indicated time.
p53 expression was efficiently suppressed in the absence of doxycycline (Dox) and rapidly restored following Dox addition (Supplementary Fig. 1b, c). On transplantation into the livers of recipient mice, hepatoblast populations co-expressing Ras and the conditional p53 shRNA rapidly produced invasive hepatocarcinomas in the absence of Dox (Fig. 1b), whereas cells expressing each vector alone did not (data not shown). These tumours were GFP-positive and, if expressing luciferase, could be visualized externally by bioluminescence imaging (Fig. 1b).
Animals with advanced tumours were treated with Dox to re-establish p53 expression (Fig. 1b). Shortly after Dox administration, the p53 microRNA (miRNA) was shut off and p53 expression increased (Supplementary Fig. 1). Although tumours in untreated mice rapidly progressed, those in Dox-treated animals began to involute and became nearly undetectable within 12 days (Fig. 1b). Similar results were observed in a subcutaneous setting, where tumours could be accurately monitored using calliper measurements (Fig. 1c, left panel). Importantly, ras-induced liver carcinomas produced using a constitutive p53 shRNA grew similarly irrespective of Dox treatment (Fig. 1c, right), indicating that tumour regression was not due to Dox toxicity. Such regressions also occurred when p53 was reactivated in tumours co-expressing a constitutively activated Akt or an endogenous oncogenic K-ras allele and the conditional p53 shRNA (W.X., L.Z. and S.W.L., unpublished data).
To determine whether transient p53 reactivation could also cause tumour regression, we treated transformed cells in culture or tumour-bearing mice with Dox for 4 days and then removed the drug. Immunoblotting revealed that p53 could be transiently induced following Dox addition and withdrawal (Fig. 1d). In cultured cells, even two days of Dox treatment reduced colony formation to levels observed following continuous Dox treatment (Supplementary Fig. 2a). Furthermore, both in situ and subcutaneous liver carcinomas showed complete regressions after only four days of Dox treatment (Fig. 1e; Supplementary Fig. 2b). Thus, p53 can induce tumour involution through a process that, once activated, seems irreversible. These observations are analogous to results seen in murine tumours conditionally expressing various oncogenes, where silencing of the initiating oncogene often causes tumour regression9,10.
The rapid involution of hepatocarcinomas re-expressing p53 is consistent with p53's well-characterized ability to promote apoptosis. We therefore examined apoptosis and proliferation in tumours before and after p53 restoration (Fig. 2a, b). Surprisingly, we observed few cells that were TUNEL-positive or contained activated caspase 3 following p53 reactivation, suggesting that the primary response to p53 was not apoptosis. Similarly, substantial necrosis was not observed in the regressing tumours. Instead, these tumours showed a marked decrease in proliferation (Ki67) that was associated with signs of cellular differentiation (Supplementary Fig. 3).
Figure 2. The primary response to p53 reactivation is not apoptosis.

a, Haematoxylin and eosin (H&E) immunohistochemical staining for apoptotic cells (TUNEL and Caspase 3 staining) and proliferating cells (Ki67 staining) of liver tumours before (p53 off) and after Dox treatment (p53 on). Tumours showed histopathology of human hepatocellular and cholangiocellular carcinoma. Inset (P) denotes positive controls (irradiated thymus, 20Gy (20 Gray)). ‘p53 on’ shows representative tumour on day 6. Scale bar, 100 μm. b, Quantification of a. Values represent mean ± s.d. (n = 4; **P<0.002).
p53 can also promote cellular senescence, an apparently irreversible form of cell cycle arrest that is a potent barrier to tumorigenesis11–14 and can be triggered by hyperactive Ras or PI3K signalling12,15. Interestingly, hepatocarcinomas expressing either oncogenic ras or Akt showed clear signs of senescence following p53 reactivation in vivo (Fig. 3a–c; data not shown for Akt), including the accumulation of senescence-associated-β-galactosidase (SA-β-Gal) activity (Fig. 3a, b) and the senescence markers p16INK4a, DcR2 and p15INK4b (Fig. 3c)13,15. SA-β-gal activity was also observed in tumours following brief Dox treatment (Fig. 3b), indicating that a pulse of p53 activity was sufficient to trigger senescence in vivo.
Figure 3. p53 reactivation induces cellular senescence.
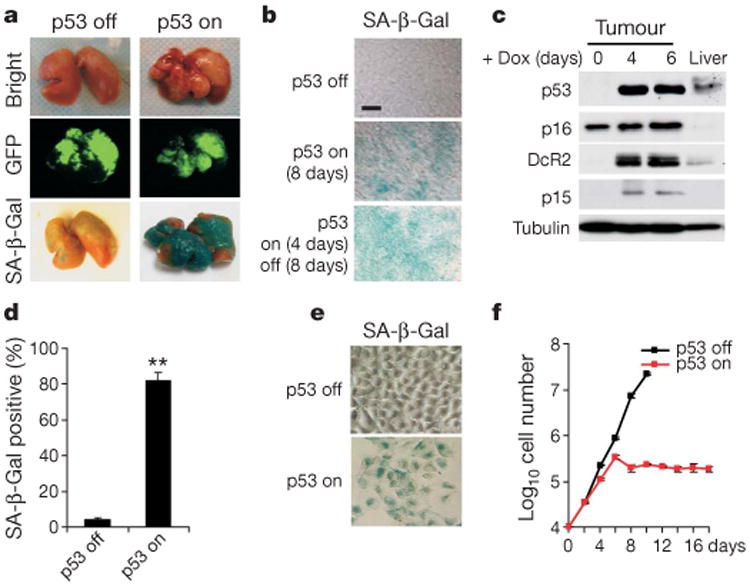
a, SA-β-Gal staining of representative tumour-bearing livers untreated (p53 off) or treated with Dox (p53 on, day 6) (n= 3). b, SA-β-Gal staining of tumour sections (n = 3). Tumours were either untreated (p53 off), constantly treated with Dox for 8 days (p53 on 8 days) or briefly treated for 4 days and left untreated for 8 days (p53 on 4 days/off 8 days). Scale bar, 25 μm. c, Immunoblotting for senescence markers in normal liver or liver tumours treated with Dox for 0, 4 and 6 days. d, Liver progenitor cells harbouring ras and tet-off shp53 were cultured in Dox-containing medium for 6 days (p53 on) and stained for SA-β-Gal. Values represent mean±s.d. (n = 3; **P < 0.0001). e, Representative pictures from d. f, Cells as in d were cultured with (p53 on, red line) or without Dox (p53 off, black line) and cell numbers were counted. Values represent mean±s.d. (n=4).
That p53 activation induces both cellular senescence and tumour involution is surprising given that senescence is a cytostatic program. Indeed, transformed cells accumulated SA-β-gal activity but subsequently remained arrested following p53 reactivation in vitro (Fig. 3d–f), suggesting that tumour regression involves non-cell-autonomous processes. Microscopic examination of tumours harvested at different times following p53 reactivation revealed a progressive inflammatory reaction involving polymorphonuclear leukocytes, initially developing in peri-tumoral regions and ultimately spreading throughout the tumour (Fig. 4a–f). We also observed an intense perivascular infiltration in regressing tumours, leading eventually to an overt vasculitis characterized by sclerosed vessels, hemorraghia and erythrophagocytosis (Supplementary Fig. 7). Morphological, immunofluorescence and flow cytometric analyses identified the infiltrating leukocytes as neutrophils, macrophages and natural killer cells (Supplementary Figures 4–6). These histopathological features support a model of sequential events, initiated by p53 reactivation in the tumour, activation of a dramatic inflammatory response, followed by destruction of tumour cells and neo-vasculature.
Figure 4. Clearance of liver tumours by an innate immune response.

a–f, Progressive immune infiltration in regressing tumours following p53 reactivation (H&E; n = 4). Arrows denote peri-tumoral polymorphonuclear (PMN) leukocytes. Arrowheads denote intra-tumoral polymorphonuclear leukocytes. Scale bar, 100 μm. e, High magnification view of d. g, p53 reactivation leads to increased expression of chemokines and adhesion molecules in senescent tumours (in vivo) and cultured liver progenitor cells (in vitro). Values represent mean± s.d. (duplicate samples with triplicate qPCR). All the D4 and D8 values are statistically significant compared with D0 (P<0.05). h, p53 reactivation is accompanied by increased immune cell transcripts in senescent tumours (in vivo) but not in cultured cells (in vitro). Values represent the average of duplicate samples from microarrays. i, Subcutaneous hepatocarcinomas were treated with Dox to induce tumour regression. The macrophage toxin GdCl (red line), an anti-neutrophil antibody (purple) or an anti-natural killer-cell antibody (blue) was administered. Saline (solid black line) or an isotype control antibody (dashed black line) served as controls. Values represent mean ± s.d. (n = 4; *P < 0.02; **P < 0.002 for day 16). j, Blockade of innate immune cells does not prevent p53-induced senescence. Frozen sections from control animals or immune antagonist treated animals were stained for SA-β-Gal activity (n = 3). Scale bar, 50 μm.
Senescent cells often acquire a gene expression signature that includes the upregulation of inflammatory cytokines and other immune modulators16,17. Accordingly, inflammatory cytokines known to attract macrophages (Csf1 and Mcp1), neutrophils (Cxcl1) and natural killer cells (Il15) were upregulated in liver tumours shortly following p53 reactivation (Fig. 4g). These genes were also induced by p53 in cultured hepatoma cells, demonstrating that they are expressed in tumour cells, not merely the infiltrating leukocytes (Fig. 4g). Moreover, several adhesion molecules including Icam1 (ref. 18) and Vcam1 were induced following p53 reactivation (Fig. 4g, and data not shown), indicating one way in which senescent cells could facilitate immune recognition. Finally, transcripts specific for neutrophils (Ncf2, Ncf4), macrophages (Mgl2, MSR2, CD68) and natural killer cells (Klrb1, Klrd1) were increased in senescent tumours but not cultured cells. Thus, multiple components of the innate immune system infiltrate the tumours following p53 reactivation.
To determine whether innate immune cells were required for tumour clearance, mice bearing subcutaneous hepatocarcinomas harbouring the conditional p53 shRNA were treated with gadolinium chloride (a macrophage toxin)19,20 or neutralizing antibodies to suppress neutrophil or natural killer cell function20,21, and monitored for tumour regression following Dox treatment. All three treatments significantly delayed tumour regression following p53 reactivation (Fig. 4i), thus confirming that components of the innate immune system were actively involved in tumour clearance, presumably through a coordinated response. Importantly, each antagonist efficiently and specifically depleted the targeted immune cells from the spleen or peripheral blood (Supplementary Fig. 8), but did not prevent tumour cell senescence (Fig. 4j). Similarly, almost no tumour regression was observed following p53 reactivation in tumours grown in NOD/SCID mice —which have a highly impaired innate immune system22—even though p53 still induced cytostasis and senescence (Supplementary Fig. 9). Therefore, the delay in tumour clearance cannot be explained by a failure of the immune system to phagocytose dead or dying cells. Instead, these results indicate that the induction of cellular senescence and the evoked immune attack cooperate to promote tumour clearance. Of note, the athymic nude mice used here lacked functional B and T cells, which typically potentiate, but can also attenuate, inflammatory responses23. However, p53 reactivation in murine sarcomas also can induce senescence and tumour clearance in a completely immunocompetent setting24.
Our study used regulatable RNAi to demonstrate that p53 loss is required for maintenance of aggressive hepatocarcinomas. We suspect that tumours harbouring p53 mutations may be hypersensitive to restoration of p53 signalling because they have oncogenic lesions or damage signals capable of potently activating p53 (refs 3, 25). Still, the consequences of restoring p53 signalling may depend on tumour origin or genotype; thus, whereas p53 reactivation induces senescence in liver carcinomas and sarcomas, lymphoid tumours respond to p53 by undergoing apoptosis24. Tumours may also eventually escape their dependence on p53 mutations, but the fact that brief reactivation can cause complete tumour regressions supports the potential of transient p53 reactivation therapies26,27, even for advanced cancers.
Our results also identify a novel mechanism of tumour suppression involving cooperative interactions between a tumour cell senescence program and the innate immune system. They further demonstrate that, despite the cytostatic nature of the senescence program, senescent cells can turn over in vivo. Whether such turnover is a general feature of senescence in vivo is not clear14,28, but when present may reinforce the tumour suppressive action of senescence in pre-malignant settings or in tumours following treatment with senescence- or differentiation-promoting therapies26,29. Conversely, our results identify a setting in which the innate immune system is provoked to coordinately attack tumour cells, presumably through both phagocytosis and direct cytotoxic killing, thereby facilitating their elimination. Although it is established that chronic inflammation triggered by senescent stromal cells or other factors can promote tumorigenesis19,30, our study illustrates how innate immune cells— when targeted against senescent tumour cells—can have anti-tumour effects as well. Strategies that specifically harness these processes may represent a promising therapeutic approach.
Methods
See Supplementary Methods for detailed experimental methods.
Generation and analysis of liver tumours
Isolation, culture and retroviral infection of murine hepatoblasts were as described4,5. Doxycycline treatment (BD Biosciences) and bioluminescence imaging (Xenogen) was performed according to the manufacturer's instructions. Histopathological evaluation was performed by an experienced pathologist (C.C.C.). Immunohistochemistry was performed as described5.
Tumour characterization
Fresh tumour tissue was lysed in Laemmli buffer using a tissue homogenizer and analysed by immunoblotting by standard procedures with the indicated antibodies. Detection of SA-β-gal activity was performed as described at pH5.5 (ref. 7). Sections (10 μm) of snap frozen tumour tissue were fixed with 1% formalin for 1 min and stained for 12h. Tumour-bearing livers were fixed with 4% formalin overnight and stained for 4h. Cultured cells were fixed with 4% formalin for 5 min and stained for 10 h.
RNA expression analyses
RNA isolation (Qiagen) and TaqMan reverse transcriptase reaction (Applied Bosystems) were according to the manufacturer's instructions. Quantitative PCR (qPCR) reactions (Bio-Rad) for each sample were done in triplicate. Microarray experiments were performed on Mouse Genome 430A 2.0 arrays (Affymetrix).
Data analysis
All the statistical analysis was done by Student's t-test.
Supplementary Material
Acknowledgments
We thank L. Bianco and M. Jiao for technical assistance. We also thank G. Evan, T. Jacks, A. Ventura, M. Narita, A. Chicas, M. Yon, G. Hannon and other members of the Lowe and Hannon laboratories for advice and discussions. We thank M. McCurrach for editorial assistance. W.X. is in the MCB graduate program at Stony Brook University. This work was generously supported by the Emmy Noether Programme of the German Research Foundation, Alan and Edith Seligson, the Don Monti Foundation, and grants from the National Institutes of Health (C.C.C, S.W.L.). This work is dedicated to our friend and colleague Dr. Enrique (Henry) Cepero.
Footnotes
Supplementary Information is linked to the online version of the paper at www.nature.com/nature.
Author Contributions W.X.: study design and conduction of experiments; L.Z.: study design and conduction of experiments; C.M.: design and conduction of flow cytometry experiments; R.A.D.: vector development; E.H.: histopathological analyses; V.K.: microarray analysis; C.C.C: histopathological analyses; S.W.L.: study design, principal investigator.
The authors declare no competing financial interests.
References
- 1.Harris SL, Levine AJ. The p53 pathway: positive and negative feedback loops. Oncogene. 2005;24:2899–2908. doi: 10.1038/sj.onc.1208615. [DOI] [PubMed] [Google Scholar]
- 2.Sherr CJ. Principles of tumor suppression. Cell. 2004;116:235–246. doi: 10.1016/s0092-8674(03)01075-4. [DOI] [PubMed] [Google Scholar]
- 3.Lowe SW, Cepero E, Evan G. Intrinsic tumour suppression. Nature. 2004;432:307–315. doi: 10.1038/nature03098. [DOI] [PubMed] [Google Scholar]
- 4.Zender L, et al. Generation and analysis of genetically defined liver carcinomas derived from bipotential liver progenitors. Cold Spring Harb Symp Quant Biol. 2005;70:251–261. doi: 10.1101/sqb.2005.70.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zender L, et al. Identification and validation of oncogenes in liver cancer using an integrative oncogenomic approach. Cell. 2006;125:1253–1267. doi: 10.1016/j.cell.2006.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Staib F, Hussain SP, Hofseth LJ, Wang XW, Harris CC. TP53 and liver carcinogenesis. Hum Mutat. 2003;21:201–216. doi: 10.1002/humu.10176. [DOI] [PubMed] [Google Scholar]
- 7.Dickins RA, et al. Probing tumor phenotypes using stable and regulated synthetic microRNA precursors. Nature Genet. 2005;37:1289–1295. doi: 10.1038/ng1651. [DOI] [PubMed] [Google Scholar]
- 8.Silva JM, et al. Second-generation shRNA libraries covering the mouse and human genomes. Nature Genet. 2005;37:1281–1288. doi: 10.1038/ng1650. [DOI] [PubMed] [Google Scholar]
- 9.Chin L, et al. Essential role for oncogenic Ras in tumour maintenance. Nature. 1999;400:468–472. doi: 10.1038/22788. [DOI] [PubMed] [Google Scholar]
- 10.Jain M, et al. Sustained loss of a neoplastic phenotype by brief inactivation of MYC. Science. 2002;297:102–104. doi: 10.1126/science.1071489. [DOI] [PubMed] [Google Scholar]
- 11.Braig M, et al. Oncogene-induced senescence as an initial barrier in lymphoma development. Nature. 2005;436:660–665. doi: 10.1038/nature03841. [DOI] [PubMed] [Google Scholar]
- 12.Chen Z, et al. Crucial role of p53-dependent cellular senescence in suppression of Pten-deficient tumorigenesis. Nature. 2005;436:725–730. doi: 10.1038/nature03918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Collado M, et al. Tumour biology: senescence in premalignant tumours. Nature. 2005;436:642. doi: 10.1038/436642a. [DOI] [PubMed] [Google Scholar]
- 14.Michaloglou C, et al. BRAFE600-associated senescence-like cell cycle arrest of human naevi. Nature. 2005;436:720–724. doi: 10.1038/nature03890. [DOI] [PubMed] [Google Scholar]
- 15.Serrano M, Lin AW, McCurrach ME, Beach D, Lowe SW. Oncogenic ras provokes premature cell senescence associated with accumulation of p53 and p16INK4a. Cell. 1997;88:593–602. doi: 10.1016/s0092-8674(00)81902-9. [DOI] [PubMed] [Google Scholar]
- 16.Minamino T, et al. Ras induces vascular smooth muscle cell senescence and inflammation in human atherosclerosis. Circulation. 2003;108:2264–2269. doi: 10.1161/01.CIR.0000093274.82929.22. [DOI] [PubMed] [Google Scholar]
- 17.Shelton DN, Chang E, Whittier PS, Choi D, Funk WD. Microarray analysis of replicative senescence. Curr Biol. 1999;9:939–945. doi: 10.1016/s0960-9822(99)80420-5. [DOI] [PubMed] [Google Scholar]
- 18.Gorgoulis VG, et al. p53-dependent ICAM-1 overexpression in senescent human cells identified in atherosclerotic lesions. Lab Invest. 2005;85:502–511. doi: 10.1038/labinvest.3700241. [DOI] [PubMed] [Google Scholar]
- 19.Maeda S, Kamata H, Luo JL, Leffert H, Karin M. IKKβ couples hepatocyte death to cytokine-driven compensatory proliferation that promotes chemical hepatocarcinogenesis. Cell. 2005;121:977–990. doi: 10.1016/j.cell.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 20.Mundt B, et al. Involvement of TRAIL and its receptors in viral hepatitis. FASEB J. 2003;17:94–96. doi: 10.1096/fj.02-0537fje. [DOI] [PubMed] [Google Scholar]
- 21.Hong F, et al. β-glucan functions as an adjuvant for monoclonal antibody immunotherapy by recruiting tumoricidal granulocytes as killer cells. Cancer Res. 2003;63:9023–9031. [PubMed] [Google Scholar]
- 22.Shultz LD, et al. Multiple defects in innate and adaptive immunologic function in NOD/LtSz-scid mice. J Immunol. 1995;154:180–191. [PubMed] [Google Scholar]
- 23.Ghiringhelli F, Menard C, Martin F, Zitvogel L. The role of regulatory T cells in the control of natural killer cells: relevance during tumor progression. Immunol Rev. 2006;214:229–238. doi: 10.1111/j.1600-065X.2006.00445.x. [DOI] [PubMed] [Google Scholar]
- 24.Ventura A, et al. Restoration of p53 function leads to tumour regression in vivo. Nature. 2007 Jan 24; doi: 10.1038/nature05541. advance online publication. [DOI] [PubMed] [Google Scholar]
- 25.Christophorou MA, Ringshausen I, Finch AJ, Swigart LB, Evan GI. The pathological response to DNA damage does not contribute to p53-mediated tumour suppression. Nature. 2006;443:214–217. doi: 10.1038/nature05077. [DOI] [PubMed] [Google Scholar]
- 26.Bykov VJ, et al. Restoration of the tumor suppressor function to mutant p53 by a low-molecular-weight compound. Nature Med. 2002;8:282–288. doi: 10.1038/nm0302-282. [DOI] [PubMed] [Google Scholar]
- 27.Vassilev LT, et al. In vivo activation of the p53 pathway by small-molecule antagonists of MDM2. Science. 2004;303:844–848. doi: 10.1126/science.1092472. [DOI] [PubMed] [Google Scholar]
- 28.Gray-Schopfer VC, et al. Cellular senescence in naevi and immortalisation in melanoma: a role for p16? Br J Cancer. 2006;95:496–505. doi: 10.1038/sj.bjc.6603283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Roninson IB. Tumor cell senescence in cancer treatment. Cancer Res. 2003;63:2705–2715. [PubMed] [Google Scholar]
- 30.Krtolica A, Parrinello S, Lockett S, Desprez PY, Campisi J. Senescent fibroblasts promote epithelial cell growth and tumorigenesis: a link between cancer and aging. Proc Natl Acad Sci USA. 2001;98:12072–12077. doi: 10.1073/pnas.211053698. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


