Abstract
Background
Surgical repair of a torn rotator cuff is based on the belief that repairing the tear is necessary to restore normal glenohumeral joint (GHJ) mechanics and achieve a satisfactory clinical outcome.
Hypothesis
Dynamic joint function is not completely restored by rotator cuff repair, thus compromising shoulder function and potentially leading to long-term disability.
Study Design
Controlled laboratory study and Case series; Level of evidence, 4.
Methods
Twenty-one rotator cuff patients and 35 control participants enrolled in the study. Biplane radiographic images were acquired bilaterally from each patient during coronal-plane abduction. Rotator cuff patients were tested at 3, 12, and 24 months after repair of a supraspinatus tendon tear. Control participants were tested once. Glenohumeral joint kinematics and joint contact patterns were accurately determined from the biplane radiographic images. Isometric shoulder strength and patient-reported outcomes were measured at each time point. Ultrasound imaging assessed rotator cuff integrity at 24 months after surgery.
Results
Twenty of 21 rotator cuff repairs appeared intact at 24 months after surgery. The humerus of the patients’ repaired shoulder was positioned more superiorly on the glenoid than both the patients’ contralateral shoulder and the dominant shoulder of control participants. Patient-reported outcomes improved significantly over time. Shoulder strength also increased over time, although strength deficits persisted at 24 months for most patients. Changes over time in GHJ mechanics were not detected for either the rotator cuff patients’ repaired or contralateral shoulders. Clinical outcome was associated with shoulder strength but not GHJ mechanics.
Conclusion
Surgical repair of an isolated supraspinatus tear may be sufficient to keep the torn rotator cuff intact and achieve satisfactory patient-reported outcomes, but GHJ mechanics and shoulder strength are not fully restored with current repair techniques.
Clinical Relevance
The study suggests that current surgical repair techniques may be effective for reducing pain but have not yet been optimized for restoring long-term shoulder function.
Keywords: rotator cuff, glenohumeral joint, biomechanics, kinematics
Rotator cuff tears are a common clinical condition that occur in up to 50% of people over the age of 65 years and have a major effect on function, pain, and medical care costs.48 Symptomatic tears are often repaired surgically. Rotator cuff repairs have been reported to fail structurally in 20% to 70% of cases, with large tears having a much higher failure rate after repair than small tears.13,19,21,27 Thus, opinions vary regarding the optimal treatment of rotator cuff tears. Surgical treatment is implicitly based on the belief that repairing the torn rotator cuff is necessary to restore normal glenohumeral joint (GHJ) mechanics and achieve a satisfactory clinical outcome.
Previous studies have investigated the effect of rotator cuff tears or rotator cuff repair on joint mechanics both in vitro and in vivo. Cadaveric studies have shown that GHJ mechanics are altered in the presence of rotator cuff tears and that these alterations correlate with tear size.60 Other cadaveric studies have investigated the effect of simulated rotator cuff repair and have shown that repair resulted in an inferior shift in the humeral head position.71 However, cadaveric studies cannot accurately simulate in vivo conditions because muscle forces and joint forces that occur under in vivo conditions are unknown. Glenohumeral joint mechanics have also been investigated under in vivo conditions. Paletta and colleagues55 used static radiographs in 2 planes to investigate shoulder kinematics before rotator cuff repair and at 2 years after repair. They found that mechanics were indeed altered before surgery compared with healthy control participants but that mechanics were normalized to those of controls in 86% of patients at 2 years after surgery. However, the accuracy and reliability of the measurement technique were not discussed, and it is possible that small changes in joint positioning that were too small to be detected by the measurement technique were present even 2 years after rotator cuff repair. Yamaguchi and colleagues69 also used static radiographs to investigate GHJ positioning in patients with both asymptomatic and symptomatic rotator cuff tears and found that both groups of patients demonstrated superior translation of the humeral head with increasing arm elevation. While these studies have contributed to our understanding of rotator cuff injury, the experimental approach of using conventional radiographs requires that images be collected under static conditions at specific arm positions. Consequently, these studies were not designed to assess dynamic, 3-dimensional (3-D) GHJ function.
Previous research has also examined the extent to which patient-reported outcomes after rotator cuff repair are associated with measures of shoulder function. For example, a study by Nho and colleagues53 reported that shoulder strength was predictive of patients’ American Shoulder and Elbow Surgeons (ASES) score. However, the relationship between patient-reported outcomes and shoulder function is not necessarily well understood. For example, satisfactory patient-reported outcomes are sometimes reported even when surgical rotator cuff repair fails.17,18,30,39,54,72 In the case of a failed repair, it is difficult to imagine that normal shoulder function has been restored. Conversely, successful surgical repair of a torn rotator cuff can sometimes result in poor patient-reported outcomes.12 This apparent discrepancy underscores our lack of understanding and suggests that the relationship between patient-reported outcomes and restoration of shoulder function—specifically, shoulder strength and joint mechanics—after surgical treatment is not well understood.
The objectives of this study were to (1) determine the extent to which rotator cuff repair restores and maintains dynamic GHJ mechanics, (2) quantify changes over time in clinical outcomes and shoulder strength, and (3) determine the extent to which clinical outcomes are associated with shoulder strength and GHJ mechanics. Given that it is not uncommon for patients to have poor shoulder function after rotator cuff repair, our central hypothesis was that dynamic joint function is not completely restored by rotator cuff repair, with altered GHJ mechanics associated with poor clinical outcomes. Specifically, we hypothesized that GHJ mechanics would be significantly different between (1) the repaired shoulder of patients undergoing rotator cuff repair and their uninjured, contralateral shoulder and (2) the repaired shoulder of patients undergoing rotator cuff repair and the dominant shoulder of participants with normal shoulder function. In addition, we hypothesized that differences in GHJ mechanics between the repaired and contralateral shoulders would decrease over time and that measures of shoulder strength and GHJ mechanics would be significantly associated with conventional patient-reported measures of clinical outcome.
MATERIALS AND METHODS
Patients
After Institutional Review Board approval and informed consent were obtained, 21 patients (14 men, 7 women; age, 63.5 ± 9.7 years; range, 39-77 years) enrolled in this study. Each patient had an arthroscopic surgical repair of a full-thickness rotator cuff tear involving only the supraspinatus tendon. The dominant shoulder was involved in 15 of the 21 patients. Patients with multitendon tears were excluded from participating in the study. All tears were small crescent or L-shaped tears of similar size and architecture that required reattachment to their native footprint. All tears were off the insertion site of the supraspinatus with no intrasubstance tears noted. Therefore, no margin convergence or intrasubstance suturing was required. The insertion site of the supraspinatus tendon was debrided in each case, with the placement of nonmetallic anchors in the footprint. Sutures were placed in the tendon to allow for appropriate reapproximation of the tendon back to its native insertion. A minimal acromioplasty was also performed in each patient to remove any anterior subacromial spurring. Each patient’s contralateral shoulder was asymptomatic. Additionally, 35 healthy control participants (21 men, 14 women; age, 30.2 ± 7.9 years) enrolled in the study. Each control participant reported normal bilateral shoulder function, with no history of shoulder injury or upper extremity surgery that could potentially compromise shoulder function. Given that rotator cuff pathology is prevalent in individuals over age 60 years and that joint function is generally observed to change with age, younger individuals were selected as controls because they are the best representation of qualitatively “normal” shoulder function.
Postoperative Rehabilitation
Postoperatively, all patients were enrolled in a rehabilitation program that corresponded to the standard of care for our institution. The program consists of 4 phases: an immediate postoperative phase (weeks 0-4) that emphasized shoulder passive range of motion (ROM) and scapular retraining; a muscle re-education phase (weeks 4-8) that emphasized active assisted to active ROM and submaximal pain-free isometrics of the shoulder girdle muscles; an early strengthening phase (8-12 weeks) that focused on strengthening of the rotator cuff and scapular muscles; and a return to function phase (>12 weeks) that included strengthening of the rotator cuff and scapular stabilizers and progression to pain-free functional activities. All patients were given a comprehensive home management program that was consistent with their specific phase of the rehabilitation protocol. Patients were seen by a physical therapist twice a week for an average of 3 to 5 months.
Testing Procedures
Participants were positioned with the GHJ centered within the 3-D imaging volume of a biplane radiography system.9 All participants wore a lead-lined thyroid shield and protective vest during testing to minimize radiation exposure. Biplane radiographic images were acquired at 60 Hz as patients performed coronal-plane abduction while holding a 3-lb hand weight. Patients began this motion with their arm in a position of adduction and neutral rotation (ie, arm at their side) and then abducted their shoulder to approximately 120° over 2 seconds. The rate of shoulder motion was controlled using a metronome. Patients performed 3 trials, with a minimum of 3 minutes between trials to minimize fatigue. Both shoulders were tested, and the testing order was randomized. For the rotator cuff repair patients, all data were collected at 3, 12, and 24 months postoperatively.
After testing, bilateral computed tomography (CT) scans of the entire humerus and scapula were acquired (LightSpeed16, GE Medical Systems, Piscataway, New Jersey). The scans were acquired with a slice thickness of 1.25 mm and an in-plane resolution of approximately 0.5 mm per pixel. The humerus and scapula were manually segmented from other bones and soft tissue and reconstructed into a 3-D bone model (Mimics 13.1, Materialise, Leuven, Belgium).
Conventional Joint Kinematics
The 3-D motions of both the humerus and scapula were determined from the biplane radiographic images using an accurate (±0.4 mm, ±0.5°) CT model–based tracking technique.10 With use of these data, conventional GHJ kinematics (ie, translations and rotations of the humerus relative to the scapula) were determined for each shoulder using anatomic landmarks based on the International Society of Biomechanics standard.9,66 The conventional kinematic outcome measures included the anterior/posterior (A/P) and superior/inferior (S/I) translation of the center of the humeral head relative to the scapula.66 To account for differences in patient size, the humeral head translation data were normalized relative to the glenoid height as determined from the patient-specific bone models.
Joint Contact Patterns
Next, GHJ contact patterns were also estimated for each shoulder. This technique has been used extensively to estimate joint contact patterns by combining joint motion measured from the biplane radiographic images with the patient-specific bone models.3,4,6,26,44,46,50 Briefly, the GHJ contact center was estimated by first calculating the minimum distance between the glenoid and the humerus at every point on the glenoid and then determining the centroid of this distance map. The contact center position was expressed relative to a glenoid-based coordinate system, and the process was repeated for all frames of every trial. The glenoid-based coordinate system was defined with custom software that created a best-fit plane to the points on the glenoid rim, identified the glenoid’s centroid as the origin, created the S/I axis that bisected the glenoid into anterior and posterior regions of equal area, and created the A/P axis as the cross-product of the S/I axis and a laterally directed vector perpendicular to the plane defined by the glenoid rim. These calculations resulted in a contact path, that is, a time series of GHJ contact center data. To account for differences in patient size, these estimates of the joint contact center were normalized relative to each shoulder’s glenoid height and width as determined from the patient-specific bone models.
Using these joint contact center data, we determined the dynamic contact location—that is, an estimate of the average position of the humerus on the glenoid during shoulder abduction—by calculating the average A/P contact center and the average S/I contact center over each trial. To assess dynamic joint excursion (ie, the amount of GHJ translation that occurred during shoulder motion), we calculated the A/P axis contact center range, the S/I contact center range, and the contact center path length over each trial. Lastly, the subacromial space was estimated by calculating the acromiohumeral distance (ie, the shortest distance between the humeral and acromial surfaces) for every frame of data and then computing the average distance over the entire trial.8 For each parameter, the data were then averaged over the 3 trials for each patient. To account for differences in ROM across patients and control participants, the data were reported for the range of 20° to 70° of glenohumeral abduction.
Shoulder Strength
Isometric shoulder strength was tested using an isokinetic dynamometer (Biodex System 2, Shirley, New York). Following the protocol described by Hughes and colleagues,28 strength testing was performed at the following joint positions: coronal-plane abduction (ABD) at 30° of abduction, sagittal-plane elevation (ELEV) at 30° of elevation, internal rotation (IR) at 15° of frontal-plane elevation and 0° of humeral rotation, and external rotation (ER) at 15° of frontal-plane elevation and 0° of humeral rotation. To isolate shoulder strength and minimize the likelihood of compensation with other muscle groups, patients were secured to the Biodex system with 2 hook-and-loop straps diagonally across their torso. Three trials were performed at each position, with at least 2 minutes of rest between each trial. The average of the 3 trials was calculated and recorded as the patient’s maximum isometric strength. All patients were tested at 3, 12, and 24 months after surgery. Both shoulders were tested, and the testing order was randomized. To account for any inherent differences in strength between patients, normalized shoulder strength was determined by computing the maximum isometric strength of the surgically repaired shoulder as a percentage of the maximum isometric strength of the contralateral shoulder.
Subjective Assessment
Upon completion of all strength testing, patients provided a subjective assessment of their shoulder function by completing the Western Ontario Rotator Cuff (WORC) Index. The WORC Index is a disease-specific quality-of-life measurement tool that provides a cumulative score based on the domains of physical symptoms, sport/recreation, work function, lifestyle function, and emotional function. There are a total of 21 questions, and patients indicate their response to each question along a 10-cm visual analog scale, where lower scores indicate a more satisfactory clinical outcome. The WORC is a valid and reliable measurement tool for patients with rotator cuff disease.37 This survey was given at 3, 12, and 24 months after surgery.
Ultrasound Analysis
For the rotator cuff repair patients, rotator cuff tendon integrity was assessed with ultrasound at 24 months after surgery. The examinations were performed by an experienced radiologist (MVH) with extensive experience in musculoskeletal ultrasound.2,61,62 The ultrasound examinations were performed using a 12-MHz matrix linear transducer (GE Logic 9, Milwaukee, Wisconsin) and included transverse and longitudinal images of the supraspinatus, subscapularis, infraspinatus, and biceps tendons. Rotator cuff repair integrity was assessed by evaluating the supraspinatus tendon for abnormalities such as tendon nonvisualization, abnormal echogenicity, and tendon thinning.
Statistical Analysis
Differences in dynamic contact location (ie, average A/P contact center, average S/I contact center), dynamic joint excursion (ie, A/P contact center range, S/I contact center range, contact center path length), and average acromiohumeral distance were assessed separately between the repaired and contralateral shoulders with a paired t test and between the repaired and control participants’ shoulders with an independent t test. The control participant data were compared with the repaired data at only 24 months after surgery because previous research has suggested that shoulder function at 24 months after surgery is predictive of longer term outcome.20 Comparisons were made to the control participants’ dominant shoulders only because of the majority of rotator cuff tears occurring in the patients’ dominant shoulders. Changes over time in WORC Index scores, normalized shoulder strength, and GHJ mechanics were assessed using repeated-measures 1-way ANOVAs followed by a Bonferroni test for pairwise comparisons. The relationship between the WORC Index and measures of GHJ mechanics or shoulder strength was assessed for all shoulders with linear regression and correlation. Significance was set at P < .05 for all statistical tests.
RESULTS
Rotator Cuff Integrity
The average tear size (anterior-to-posterior width) was manually measured intraoperatively and was found to be 1.6 ± 0.6 cm. At the 24-month follow-up, ultrasound imaging found 20 of 21 repairs to be intact. In the contralateral shoulders at the 24-month follow-up, 3 patients were found to have a full-thickness tear, and 7 patients had a partial-thickness tear. All of the full- or partial-thickness tears involved only the supraspinatus tendon. The remaining 11 of the 21 patients had no tear in their contralateral shoulder. At 24 months after surgery, none of the patients had sought treatment at our institution for their contralateral shoulder. However, patients were not asked if they had sought treatment anywhere else for their contralateral shoulder.
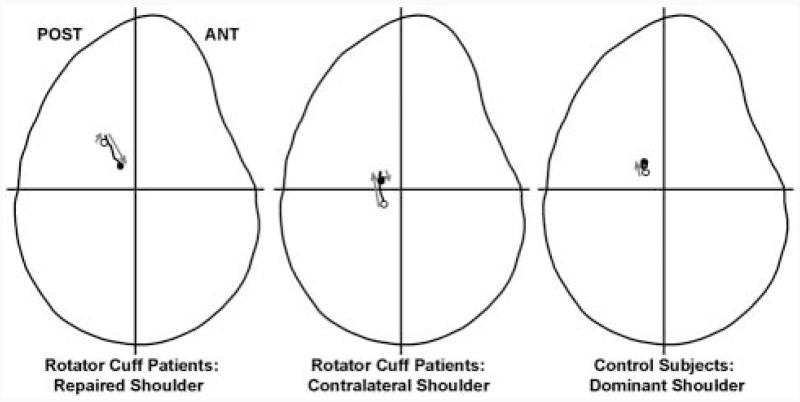
Joint Contact Paths
Marked differences in the GHJ contact paths were noted between the repaired, contralateral, and control participant shoulders after 24 months (Figure 1). In the rotator cuff repair shoulders, the contact center was located superior to the glenoid’s centroid at 20° of glenohumeral abduction and moved superiorly relative to the glenoid up to 30° of glenohumeral abduction. The contact path then reversed direction and moved inferiorly on the glenoid as glenohumeral abduction increased to 70°. In contrast, the contact center in the contralateral shoulders of the rotator cuff repair patients began inferior to the glenoid’s centroid at 20° glenohumeral abduction and moved superiorly on the glenoid up to 45° of glenohumeral abduction. Similar to the repaired shoulders, the contact center then moved inferiorly on the glenoid as glenohumeral abduction increased to 70°. For the controls, the contact center began slightly superior and posterior to the glenoid’s centroid. Although the contact center moved superiorly on the glenoid during shoulder abduction, the control participants’ contact center position varied by less than 7% of the glenoid’s width in the A/P direction and less than 14% of the glenoid’s height in the S/I direction. For all shoulders, the contact path was located on the posterior half of the glenoid and had relatively little variability in the A/P direction.
Figure 1.
The average contact center path at 24 months for repaired (left), contralateral (center), and control (right) shoulders is shown on the lateral view of the glenoid. For each contact path, the open circle (○) indicates the contact center at 20° of glenohumeral abduction, and the closed circle (●) indicates the contact center at 70° of glenohumeral abduction. The gray arrows indicate the general direction of the contact center path throughout shoulder abduction. ANT, anterior; POST, posterior.
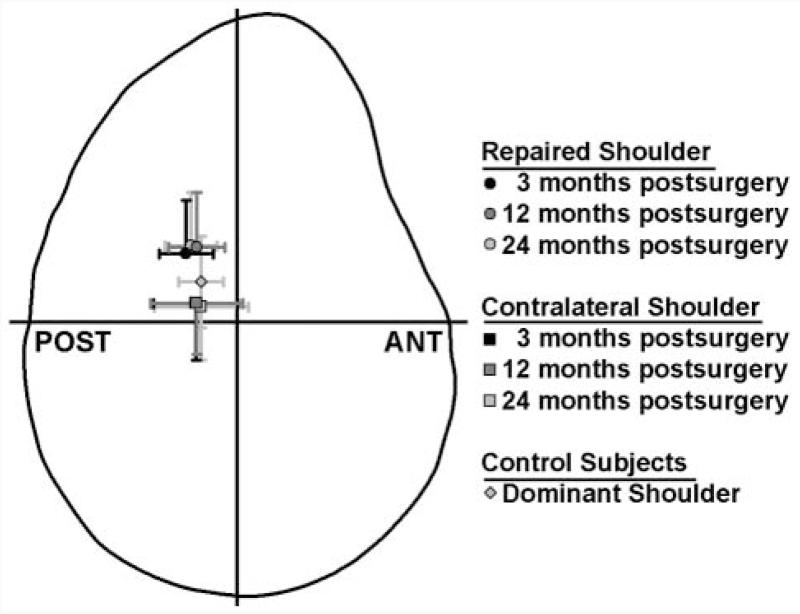
Dynamic Contact Location
There were significant differences in the dynamic contact location between the rotator cuff patients’ repaired and contralateral shoulders. Specifically, the average S/I contact center was higher in the repaired shoulder, indicating that the humerus was positioned more superiorly relative to the position of the glenoid than in the contralateral shoulder (P < .001 at all time points) (Figure 2). The difference between repaired and contralateral shoulders in the average S/I contact center was 9.0% ± 10.1%, 9.8% ± 11.7%, and 10.5% ± 11.5% of the glenoid height at 3, 12, and 24 months, respectively. In contrast, no statistically significant differences were detected between the repaired and contralateral shoulders in the average A/P contact center (P > .4 at all time points) (Figure 2).
Figure 2.
The average contact center for repaired and contralateral shoulders at 24 months after surgery and the dominant shoulder of the control participants are shown on the lateral view of a glenoid. The repaired shoulders’ average contact center was located more superiorly on the glenoid than both the contralateral shoulder (P < .001) and the control participants’ dominant shoulder (P = .007). ANT, anterior; POST, posterior.
Relative to the control participants, the rotator cuff patients’ average S/I contact center was located significantly more superiorly on the glenoid at 24 months after surgery (P = .007) (Figure 2). In contrast, no difference in the average A/P contact center was detected between repaired and control shoulders (P = .13) (Figure 2).
Over time after surgery, there were relatively few changes in the joint contact patterns of the repaired shoulder. There was a statistical trend for a more anteriorly located average A/P contact center at 12 months compared with 3 months after surgery (P = .06), but differences in the average S/I contact center were not detected over time (P = .23) (Figure 2).
Dynamic Joint Excursion
Differences in dynamic joint excursion were not detected between the rotator cuff patients’ repaired and contralateral shoulders at any of the 3 postsurgical time points. Specifically, differences were not detected in terms of the A/P contact center range (P ≥ .13) (Table 1), S/I contact center range (P ≥ .48) (Table 1), or contact center path length (P ≥ .19) (Table 1).
TABLE 1.
Comparison of Dynamic Joint Excursion Between Repaired, Contralateral, and Control Shoulders
| Rotator Cuff Patients |
Control Participants |
||||
|---|---|---|---|---|---|
| Repaired Shoulder | Contralateral Shoulder | P | Dominant Shoulder | Pa | |
| Anterior/posterior contact center range (% of glenoid width) | |||||
| 3 mo | 10.0 ± 6.2 | 9.2 ± 5.0 | .91 | 7.3 ± 4.5 | .01 |
| 12 mo | 12.7 ± 8.2b | 10.2 ± 5.6 | .13 | ||
| 24 mo | 11.7 ± 6.4c | 10.3 ± 5.5 | .38 | ||
| Superior/inferior contact center range (% of glenoid height) | |||||
| 3 mo | 13.1 ± 10.9 | 13.3 ± 7.0 | .48 | 13.6 ± 8.2 | .58 |
| 12 mo | 13.1 ± 7.3 | 14.4 ± 5.7 | .79 | ||
| 24 mo | 12.3 ± 6.8 | 14.0 ± 6.2 | .55 | ||
| Contact center path length (% of glenoid height) | |||||
| 3 mo | 20.8 ± 12.5 | 23.0 ± 7.1 | .19 | 21.5 ± 10.4 | .85 |
| 12 mo | 25.4 ± 9.8b | 24.5 ± 6.7 | .70 | ||
| 24 mo | 22.2 ± 8.0 | 24.7 ± 7.3 | .30 | ||
Control shoulders compared with repaired shoulders at 24 months after surgery.
Significantly different compared with 3 months after surgery (P < .05).
Statistical trend compared with 3 months after surgery (P = .07).
Relative to the control participants, the rotator cuff patients’ repaired shoulder demonstrated only minor differences in dynamic joint excursion. Although statistically significant differences were not detected in terms of the S/I contact center range (P = .58) or contact center path length (P = .85), the A/P contact center range of the repaired shoulders was significantly greater than that of control shoulders (P = .01) (Table 1).
Over time after surgery, changes in dynamic joint excursion were detected in the repaired shoulders in terms of the A/P contact center range and contact center path length but not in the S/I contact center range (Table 1). Specifically, the A/P contact center range was significantly greater at 12 months after surgery than at 3 months after surgery (P = .02) (Table 1), and there was a statistical trend for increased A/P contact center range at 24 months after surgery compared with 3 months after surgery (P = .07) (Table 1). The contact center path length at 12 months after surgery was significantly greater than at 3 months after surgery (P = .01) (Table 1). However, no significant difference in contact center path length was detected between 24 months after surgery and either the 3-month (P = .20) or 12-month (P = .16) postsurgical time points (Table 1).
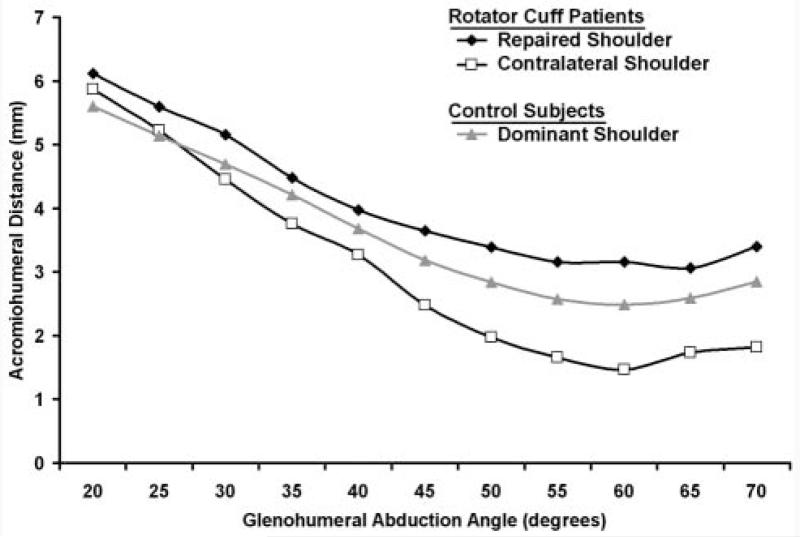
Subacromial Space
In general, the acromiohumeral distance decreased with increasing abduction angle in all groups (Figure 3). The acromiohumeral distance steadily decreased from 20° to 50° of abduction and then remained relatively constant until the end of the motion at 70°. The difference in acromiohumeral distance between the groups also became more apparent with increasing abduction angle. The repaired shoulders’ average acromiohumeral distance was significantly greater than the contralateral shoulders at 3, 12, and 24 months after surgery (P < .001). The average acromiohumeral distance of the repaired shoulders was 4.5 ± 1.6 mm, 4.3 ± 1.5 mm, and 4.2 ± 1.6 mm at 3, 12, and 24 months after surgery, respectively. In contrast, the average acromiohumeral distance of the rotator cuff patients’ contralateral shoulder was 3.1 ± 1.3 mm, 3.1 ± 1.4 mm, and 3.1 ± 1.4 mm at 3, 12, and 24 months after surgery, respectively. Relative to the control participants’ average acromiohumeral distance (3.6 ± 1.5 mm), the rotator cuff patients’ average acromiohumeral distance in their repaired shoulder at 24 months after surgery was not found to be significantly different (P = .18). Over time after surgery, no differences were detected in the repaired shoulders’ average acromiohumeral distance (P = .6).
Figure 3.
The acromiohumeral distance decreased from 20° to 50° of glenohumeral abduction and then remained relatively constant. The difference in acromiohumeral distance between the rotator cuff patients’ repaired and contralateral shoulders ranged from 0.25 mm at 20° of abduction to 1.6 mm at 70° of abduction. Acromiohumeral distance did not change over time in either the repaired or contralateral shoulders of the rotator cuff repair patients, so only the data from 24 months after surgery are shown.
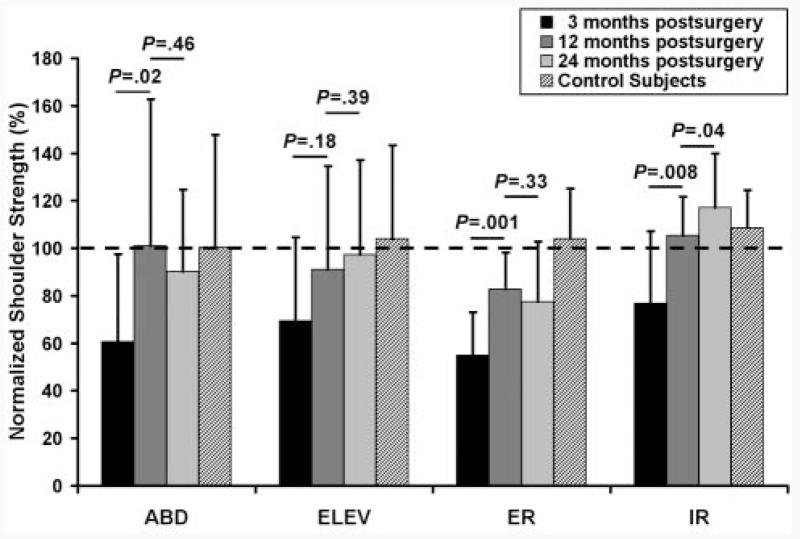
Shoulder Strength
In general, normalized shoulder strength increased over time after surgery. Specifically, shoulder strength increased over time for ABD (P = .02), ER (P < .001), and IR (P = .01), but the overall change over time for ELEV was not found to be statistically significant (P = .18) (Figure 4). There were statistically significant increases in shoulder strength from 3 months to 12 months after surgery for ABD (P = .02), ER (P = .001), and IR (P = .008). The IR was the only activity in which shoulder strength demonstrated a statistically significant increase from 12 months to 24 months after surgery (P = .04) (Figure 4).
Figure 4.
Normalized shoulder strength, defined as strength of the repaired shoulder as a percentage of the strength of the asymptomatic contralateral shoulder, improved from 3 to 12 months after surgery for abduction (ABD), external rotation (ER), and internal rotation (IR) but not for elevation (ELEV). Changes in normalized shoulder strength from 12 to 24 months after surgery were only detected for internal rotation.
Despite the increases over time in shoulder strength, strength of the repaired shoulder was less than strength of the contralateral shoulder at 24 months after surgery in 52% (11/21) of the patients during ABD, 57% (12/21) of patients during ELEV, 81% (17/21) of patients during ER, and 24% (5/21) of patients during IR. The percentage of patients who did not achieve the average control subject strength ratios (Figure 4) at 24 months after surgery was 52% (11/21) during ABD, 62% (13/21) during ELEV, 86% (18/21) during ER, and 38% (8/21) during IR.
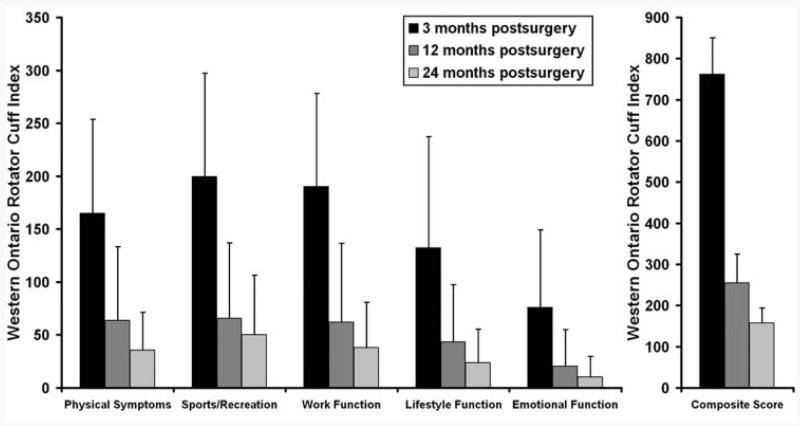
Subjective Assessment
The patients’ subjective assessment demonstrated a statistically significant improvement over time after rotator cuff repair (Figure 5). Specifically, all 5 domains of the WORC Index and the WORC Index composite score decreased significantly with time (P < .001). The WORC Index (both the composite score and the individual domains) was significantly higher at 3 months after surgery than at 12 months after surgery (P < .001) and 24 months after surgery (P < .001). However, neither the WORC composite score nor the WORC individual domains changed from 12 to 24 months after surgery (P > .18) (Figure 5).
Figure 5.
The patients’ subjective assessment of shoulder pain and function improved significantly after rotator cuff repair. The individual domains and the composite score of the Western Ontario Rotator Cuff (WORC) Index were all significantly higher at 3 months after surgery than at 12 months after surgery (P < .001) and 24 months after surgery (P < .001). However, neither the WORC composite score nor the individual domains changed from 12 to 24 months after surgery (P > .18).
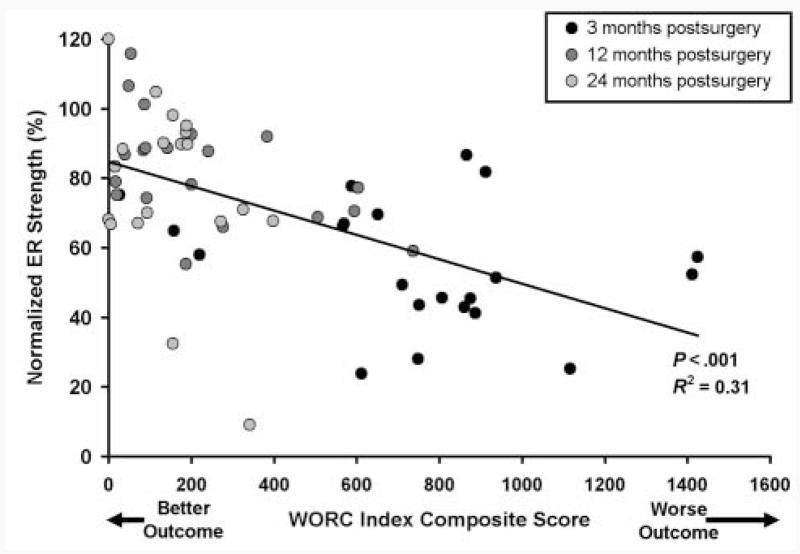
Subjective Assessment Versus Shoulder Strength
There were statistically significant associations between the WORC Index composite score and normalized shoulder strength for ABD (r = −.4, P < .001), ER (r = −.47, P < .001) (Figure 6), and IR (r = −.48, P < .001). The association between the WORC Index composite score and normalized ELEV strength was not statistically significant (r = −.20, P = .11).
Figure 6.
Normalized external rotation (ER) strength was significantly associated with the Western Ontario Rotator Cuff (WORC) Index composite score.
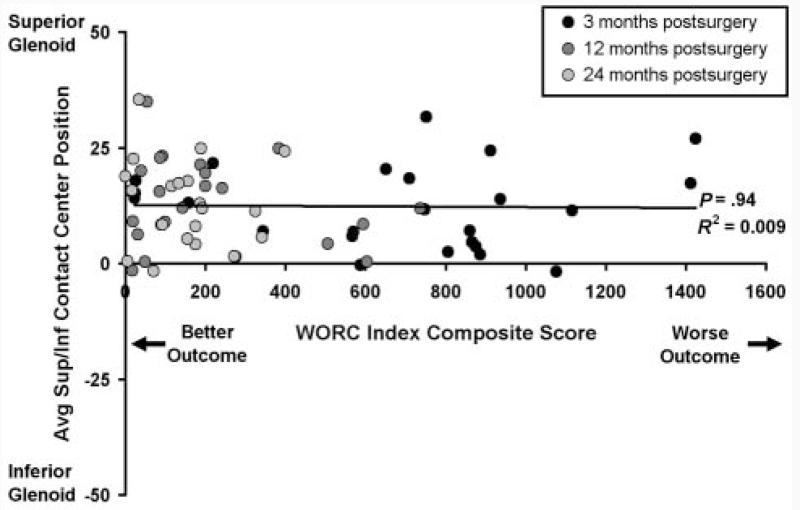
Subjective Assessment Versus GHJ Motion
The study failed to detect associations between the WORC Index composite score and the reported measures of dynamic contact location or dynamic joint excursion. Specifically, the WORC Index composite score was not found to be significantly associated with the S/I contact center position (P = .94) (Figure 7), A/P contact center position (P = .32), S/I contact center range (P = .83), A/P contact center range (P = .36), or contact center path length (P = .24).
Figure 7.
The average superior/inferior (S/I) contact center position during coronal-plane abduction was not found to be significantly associated with the Western Ontario Rotator Cuff (WORC) Index composite score.
DISCUSSION
This study demonstrated that there were significant differences between rotator cuff repair patients’ repaired and contralateral shoulders in terms of the joint contact path, the average S/I contact center, and the average acromiohumeral distance. The study also demonstrated significant differences between the rotator cuff patients’ repaired shoulder and the control participants’ dominant shoulder in terms of the joint contact path, the average S/I contact center, and the A/P contact center range. Changes over time in the rotator cuff patients’ repaired shoulders were observed in terms of the A/P contact center range and contact center path length. The study found improvements over time in shoulder strength ratios, but deficits in strength of the repaired shoulder relative to the contralateral shoulder persisted in most patients at 24 months after surgery. Ultrasound imaging indicated that 20 of 21 patients had an intact rotator cuff repair at 24 months after surgery, and the patients’ subjective assessment improved over time. There were significant associations between shoulder strength and the patients’ subjective assessment, but the patients’ subjective assessments were not significantly associated with measures of GHJ mechanics.
One of the most apparent differences reported in this study was that the repaired shoulders’ average contact center was located more superiorly on the glenoid than both the contralateral shoulders and the control shoulders (Figure 2). The explanation for this finding is unclear. It is possible that this finding may reflect an etiological factor that may have contributed to the development of the rotator cuff tear. This explanation would be consistent with the well-established theory of subacromial impingement.51,52 However, in the absence of preoperative data, this explanation is speculative. It is also possible that this finding reflects differences in scapulothoracic motion between the 3 patient populations. Specifically, it is plausible that changes in the amount of scapular rotation relative to the torso could shift the humeral contact location more superiorly on the glenoid. Lastly, it is possible that the surgical repair procedure may overtighten the tendon. Although the double-row technique has been advocated to avoid gap formation,34 it has also been suggested that single- and double-row repairs are equivalent for small tears such as the ones in this study.58 Thus, it is possible that for small tears, the double-row technique puts unnecessarily high tension on the tendon and leads to superior migration of the contact center. Regardless of the explanation for this finding, the data in this study strongly suggest that GHJ mechanics are not restored to the condition of the patient’s contralateral shoulder or to the condition of this particular control population after rotator cuff repair.
One interesting finding from this study was that the contact path changed direction in both the repaired and contralateral shoulders. Specifically, the contact center in the repaired shoulders moved superiorly on the glenoid from 20° to 30° of abduction and then moved inferiorly as the shoulder continued to abduct from 30° to 70° (Figure 1). For the contralateral shoulders, the contact center moved superiorly on the glenoid from 20° to 50° of abduction and then moved inferiorly as the shoulder continued to abduct from 50° to 70° (Figure 1). For the repaired shoulders, it is possible that initial contact between the medial aspect of the greater tuberosity and the acromion may be forcing the humeral head to translate inferiorly relative to the glenoid. However, this seems unlikely because the acromiohumeral distance is increased in the repaired shoulders (Figure 3). Alternatively, this change in direction of the contact path could be explained by underlying rotator cuff weakness, with neuromuscular compensation to accomplish elevation. Another potential explanation is that this phenomenon may reflect muscular activation in force couples to create humeral head depression. Prior cadaveric studies have suggested that the rotator cuff stabilizes the GHJ through midranges of motion by centering the humerus against the glenoid, thus preventing excessive translation of the humerus relative to the glenoid.1,25,29,36,43,67,68 Furthermore, previous research has also demonstrated that the rotator cuff contributes approximately 25% to 50% of total elevation strength.40 Although it is generally believed that loss of rotator cuff strength will result in increased GHJ excursion and superior translation of the humeral head, this belief is based on cadaveric studies that are unable to accurately simulate muscle forces and joint forces. Indeed, recent in vivo studies have suggested that paralysis of the supraspinatus and infraspinatus muscles results in neither superior migration of the humerus65 nor an increase in subacromial space pressure.64 Thus, rotator cuff weakness may not necessarily result in superior humeral translation and could instead result in the humeral head translating inferiorly relative to the glenoid.
Glenohumeral joint contact patterns have been quantified in a number of cadaveric studies. For example, the effects of shoulder position on GHJ contact patterns have been studied in cadaveric specimens using stereophotogrammetry.5,31,59 Soslowsky and colleagues59 indicated that the glenoid contact location was primarily in the anterior half of the glenoid with the shoulder adducted but moved posteriorly with increasing elevation. Although the current study demonstrated that the average contact center was located on the posterior half of the glenoid, the trend toward glenoid contact location moving posteriorly with increasing abduction was observed in the repaired shoulders (Figure 1). Furthermore, while the current study demonstrated significant changes in the S/I contact center location with increasing abduction (Figure 1), the study by Soslowsky and colleagues59 reported no clear shift in glenoid contact patterns with elevation in the S/I direction. One plausible explanation that may help to reconcile these differences is that these previous cadaveric studies simulated scapular-plane elevation, whereas the patients in the current study elevated their shoulders in the coronal plane. The effects of shoulder position, joint contact forces, muscle forces, and various simulated clinical conditions on joint contact area and joint contact pressures have been also studied by inserting thin pressure-sensitive films or similar devices (eg, Fuji film, Tokyo, Japan, or Tekscan sensors, South Boston, Massachusetts) between the humerus and glenoid of cadaveric specimens.15,23,24,63,71 Although these types of cadaveric experiments have provided the bulk of existing knowledge about GHJ mechanics, it is difficult to compare the results of the current in vivo study with cadaveric experiments that cannot reproduce muscle and joint forces because the magnitude, direction, and timing of these forces are still largely unknown.
Despite the profound differences in the average contact paths between the repaired and control shoulders at 24 months after surgery (Figure 1), it is interesting that the study failed to detect significant differences in their S/I contact center range or contact path length (Table 1). The statistical explanation for this finding is that there was tremendous variability in the joint contact patterns for the control subjects, and this variability is not adequately captured when reporting only the average contact paths (Figure 1). For example, the S/I contact center range in the control shoulders ranged from 2.2% to 39.5% of glenoid height. In contrast, the S/I contact center range of the repair shoulders at 24 months after surgery ranged from 3.0% to 27.4% of glenoid height. Similarly, the contact path length ranged from 6.7% to 51.7% of glenoid height in the control participants, whereas the path length ranged from only 5.6% to 36.0% of glenoid height in the repair patients. These data clearly suggest that there is significant variability in GHJ mechanics even among young healthy subjects with qualitatively normal shoulder function. This finding supports the clinical observation of a wide range of GHJ laxity across patients with clinically stable shoulders.
In contrast to the lack of differences in S/I contact center range or path length, the study demonstrated that the A/P contact center range was smaller in the control participants’ dominant shoulder than in the rotator cuff patients’ repaired shoulders (P = .01) (Table 1). Previous research has demonstrated that the glenoid has a higher radius of curvature in the A/P direction than in the S/I direction, indicating that the glenoid is “flatter” in the A/P direction.47 Consequently, dynamic joint excursion in the A/P direction may be less influenced by bony shape and more dependent on the glenoid labrum, relative bony positioning between the humerus and scapula, and dynamic muscle function. Therefore, the finding of a smaller A/P contact center range in the control participants may suggest that young, healthy subjects have less A/P joint excursion because of differences in muscle strength or neuromuscular control between these 2 subject populations.
The finding of a greater acromiohumeral distance in the repaired shoulders versus the contralateral shoulders (Figure 3) likely reflects the acromioplasty that was performed at the time of rotator cuff repair. The amount of the anterior acromion that is resected varies between patients and is dependent on factors such as the acromion shape and presence of osteophytes, but clinical observation suggests that it is common to remove approximately 1 to 7 mm of the acromion during an acromioplasty. Although the difference in average acromiohumeral distance between the rotator cuff patients’ repaired and contralateral shoulders was found to be only 1.2 mm, it is important to keep in mind that the humerus in the repaired shoulder is positioned, on average, approximately 10% or 3.2 mm more superiorly on the glenoid than the contralateral shoulder (Figure 2). If the humerus in the repaired shoulder would have been located at the same position on the glenoid as the contralateral shoulder, then the acromiohumeral distance would likely be in the range of 4 to 5 mm. Thus, the acromiohumeral distance data reported here are consistent with the clinical observation of the amount of bone resected during an acromioplasty.
Despite the general increase over time in the shoulder strength ratios (Figure 4), most patients had strength deficits in their repaired shoulder relative to their contralateral shoulder at 24 months after surgery. Specifically, 52% of patients had a strength deficit relative to their contralateral shoulder during ABD, 57% of patients had a strength deficit in ELEV, and 81% of patients had a strength deficit in ER. This outcome is disappointing particularly because the strength of the contralateral shoulder was likely lower by being the nondominant shoulder in 71% of the patients and was further compromised by the presence of a rotator cuff tear in 48% of the patients.35 Factors that may have contributed to this poor outcome include (1) altered GHJ (and potentially scapulothoracic) mechanics providing an inadequate or unstable base of support necessary to generate high forces, (2) muscle atrophy limiting the supraspinatus’ intrinsic ability to generate high forces, (3) inadequate or ineffective rehabilitation, or (4) the patients’ motivation and/or expectation levels relative to their activities of daily living.
The improvement in subjective outcomes (ie, the decrease in the WORC Index composite score) over time is consistent with previously published results. For example, Cools and colleagues14 reported that patient-reported outcomes improved from presurgery to 18 months after surgery as indicated by a 68% increase in the Constant-Murley score. Similarly, Bigoni et al11 demonstrated a 43% to 93% increase (depending on repair technique) in the Constant score from presurgery to 12 months after rotator cuff repair. Similar improvements in subjective assessment after rotator cuff repair have been reported by Klintberg and colleagues.38 By comparison, the current study shows a relative decrease of 70% in the WORC composite score from 3 months to 12 months after surgery (Figure 5).
The finding that the study was unable to detect significant differences in GHJ mechanics, shoulder strength, or subjective outcome between 12 and 24 months after surgery was not surprising. Although physical therapy has been shown to play an important role in the nonsurgical treatment33,41,45 and postsurgical rehabilitation after rotator cuff repair,7,38 previous research has shown that most gains in function and strength, and presumably the patient’s subjective assessment as well, will be realized within the first year after surgery.22,57 Patients were encouraged to continue their home-based strengthening program, but it is unknown if they did or if activities of daily living were sufficient to maintain the strength levels that they had achieved by 12 months after surgery. It is certainly plausible that altered glenohumeral motion and strength deficits after rotator cuff repair are not a reflection of the surgical technique but rather a limitation in the postsurgical rehabilitation protocol. Although each patient in this study was treated with a postsurgical rehabilitation protocol consistent with the standard of care at our institution, it is possible that variations in patient outcomes are a reflection of differences in compliance with rehabilitation protocol. However, this explanation is speculative because patient adherence to the postoperative rehabilitation protocol was not documented as a part of this study.
Changes in shoulder strength and subjective outcomes showed similar trends over time (ie, improvements from 3 to 12 months, but no change from 12 to 24 months), and there were statistically significant associations between these outcome measures. Specifically, the study indicated a statistically significant association between ABD, ER, and IR strength and the WORC composite score (Figure 6). Of the 21 questions in the WORC questionnaire, approximately one third of them either directly or indirectly assess the patient’s perception of his or her shoulder strength. Consequently, it is perhaps not surprising that this study would show a statistically significant association between the WORC score and measures of shoulder strength. In particular, the statistically significant association between ER strength and the WORC Index (Figure 6) was not surprising because external rotation strengthening exercises are an important component of many previously published rehabilitation protocols49,56 including the one used in this study.
In contrast to the significant associations between shoulder strength and subjective outcome, the study failed to detect any statistically significant associations between joint mechanics and subjective outcome (Figure 7). This was unexpected as we hypothesized that improved subjective assessments would reflect, at least to some extent, improvements in joint mechanics. However, there are several potential explanations for the lack of association between WORC scores and joint mechanics. First, joint mechanics were assessed during coronal-plane abduction with a 3-lb weight, and this activity may have not been sufficiently challenging (even for patients recovering from rotator cuff surgery) to provoke differences in joint mechanics as healing progressed. Second, the presurgical joint mechanics of these patients are unknown. The patients in this study had chronic rotator cuff tears and therefore may have been living with altered joint mechanics for a number of years before repair surgery. Thus, it is possible that the altered joint mechanics (eg, altered scapulothoracic motion) present after surgery reflect a presurgical condition that was not corrected through surgical repair. Alternatively, it is also plausible that the joint mechanics after surgery represent an unintended consequence of the surgical procedure—specifically, overtightening the repair—that is not resolved within the first 2 years after surgery. Lastly, it is possible that subjective assessments may simply be more heavily influenced by pain relief than by changes in GHJ function. For example, from 3 to 12 months after surgery, this study demonstrated a 71% improvement in the WORC composite score. In contrast, there was a relative increase in shoulder strength of only 47% (range, 32%-68%, depending on the activity) without any detected change in joint mechanics. These data would support the contention that a patient’s subjective assessment of shoulder function after rotator cuff surgery is more heavily influenced by a reduction in pain than increases in strength37 and that the surgery is successful in reducing pain but does not necessarily fully restore shoulder function. Furthermore, these data suggest that the complex interplay between pain, strength, and joint mechanics is poorly understood and warrants further study.
The approach used here for quantifying joint contact patterns has been used to report functional differences associated with specific clinical conditions (distal radius malunion,16,46 anterior cruciate ligament injury,4 or osteoarthritis3,26) and offers some specific advantages over conventional techniques for describing GHJ kinematics. First, the estimates of joint contact provide a more robust measurement of joint motion compared with conventional techniques. Specifically, the joint contact outcome measures are based on thousands of tessellated surface points that compose the patient-specific CT-based bone model. The estimated joint contact patterns use the entire geometry of the glenoid and humerus, and therefore, the outcome measures are not influenced by the potentially inaccurate selection of individual anatomic landmarks. In contrast, the conventional kinematic outcome measures are typically based on a small number of anatomic landmarks per bone (3 landmarks for the humerus, 4 landmarks for the scapula). Consequently, it has been shown that the calculation of conventional kinematic outcome measures can be adversely affected by the inaccurate or inconsistent identification of these specific landmarks.42 In addition, the joint contact patterns have additional clinical and physical significance in that the joint contact center provides an estimate of the location where joint contact forces are centered on the glenoid. In contrast, the center of the humeral head has limited clinical and physical significance because orthopaedic surgeons do not routinely characterize pathologic shoulder conditions with respect to the center of the humeral head. Thus, joint contact patterns provide a technically robust description of joint motion in a context that is of clinical relevance.
There are several limitations to this study. First, the experimental technique relies upon CT-based bone models that do not include articular cartilage. Consequently, the estimates of joint contact are not based on measures of cartilage overlap. However, this study was not designed to measure joint contact areas or estimate joint forces from measures of cartilage deformation. Furthermore, the same measurement technique was applied to all patients so the relative differences between the 3 groups are not compromised. Another limitation is that the study does not report preoperative data for any of the rotator cuff repair patients. However, the study was not designed to assess the effects of surgery but rather the extent to which GHJ mechanics after rotator cuff repair are consistent with that of the contralateral shoulder or a young, healthy control population. Another limitation of the study was the status of the rotator cuff in the contralateral shoulders as assessed with ultrasound at 24 months postsurgery. However, the finding of 48% (10 of 21) of the contralateral shoulders having a partial-thickness or full-thickness rotator cuff tear is consistent with previous research.70 It is important to note ultrasound imaging was performed at only 24 months after surgery, and therefore, these tears may have been present at the 3-month time point. However, the patients’ contralateral shoulders were asymptomatic at the start of the study, and none of the patients had sought treatment at our institution for their contralateral shoulder. However, the extent to which asymptomatic partial- or full-thickness tears influence the outcome measures reported here remains unknown. Additionally, the control group participants are significantly younger than the rotator cuff repair patients, and it is possible that GHJ mechanics may change as part of the aging process. However, it should be noted that differences were still observed in the patients’ repaired shoulder compared with their contralateral side. Lastly, it is possible that scapular motion patterns may have contributed to differences observed between the repaired and contralateral shoulders,32 but the field of view of our biplane radiograph system prevented us from simultaneously acquiring accurate radiograph-based measures of glenohumeral and scapulothoracic joint motion. A lack of data on scapulothoracic motion is a limitation of this study.
In summary, this study indicates that subjective outcomes and shoulder strength improve over time after surgical repair of a 1-tendon rotator cuff tear and that 95% of repairs appear intact at 2 years postsurgery. However, deficits in shoulder strength persist over time, and GHJ mechanics are not restored to the condition of either the patients’ contralateral shoulder or healthy control participants. The study also demonstrated that, in general, there are associations between patients’ subjective assessment and shoulder strength but that subjective outcomes are not associated with GHJ mechanics. Future efforts will investigate the preoperative condition of patients with rotator cuff tears, simultaneously measure glenohumeral and scapulothoracic motions, and assess the extent to which optimizing physical therapy protocols (both preoperative and postsurgical) and surgical repair techniques to restore normal GHJ mechanics improves clinical outcomes. In addition, future research should focus on testing additional patient populations (eg, young patients with rotator cuff tears, older subjects with an intact rotator cuff, older patients with asymptomatic tears) to address the extent to which factors such as age, gender, arm dominance, rotator cuff condition, and symptoms affect GHJ function.
ACKNOWLEDGMENT
One or more of the authors has declared the following potential conflict of interest or source of funding: Research support for this study was received by NIH/NIAMS AR091512.
The authors graciously acknowledge the assistance of Jeffrey Haladik, Scott Hoffman, Michael McDonald, Nicole Ramo, and Kasey Simons.
REFERENCES
- 1.Abboud JA, Soslowsky LJ. Interplay of the static and dynamic restraints in glenohumeral instability. Clin Orthop Relat Res. 2002;400:48–57. doi: 10.1097/00003086-200207000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Anderson K, Boothby M, Aschenbrener D, van Holsbeeck M. Outcome and structural integrity after arthroscopic rotator cuff repair using 2 rows of fixation: minimum 2-year follow-up. Am J Sports Med. 2006;34(12):1899–1905. doi: 10.1177/0363546506290187. [DOI] [PubMed] [Google Scholar]
- 3.Anderst WJ, Tashman S. The association between velocity of the center of closest proximity on subchondral bones and osteoarthritis progression. J Orthop Res. 2009;27(1):71–77. doi: 10.1002/jor.20702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anderst WJ, Tashman S. A method to estimate in vivo dynamic articular surface interaction. J Biomech. 2003;36(9):1291–1299. doi: 10.1016/s0021-9290(03)00157-x. [DOI] [PubMed] [Google Scholar]
- 5.Ateshian GA, Kwak SD, Soslowsky LJ, Mow VC. A stereophotogrammetric method for determining in situ contact areas in diarthrodial joints, and a comparison with other methods. J Biomech. 1994;27(1):111–124. doi: 10.1016/0021-9290(94)90038-8. [DOI] [PubMed] [Google Scholar]
- 6.Baeyens JP, Van Glabbeek F, Goossens M, Gielen J, Van Roy P, Clarys JP. In vivo 3D arthrokinematics of the proximal and distal radioulnar joints during active pronation and supination. Clin Biomech (Bristol, Avon) 2006;21(Suppl 1):S9–S12. doi: 10.1016/j.clinbiomech.2005.09.008. [DOI] [PubMed] [Google Scholar]
- 7.Baysal D, Balyk R, Otto D, Luciak-Corea C, Beaupre L. Functional outcome and health-related quality of life after surgical repair of full-thickness rotator cuff tear using a mini-open technique. Am J Sports Med. 2005;33(9):1346–1355. doi: 10.1177/0363546505275130. [DOI] [PubMed] [Google Scholar]
- 8.Bey MJ, Brock SK, Beierwaltes WN, Zauel R, Kolowich PA, Lock TR. In vivo measurement of subacromial space width during shoulder elevation: technique and preliminary results in patients following unilateral rotator cuff repair. Clin Biomech (Bristol, Avon) 2007;22(7):767–773. doi: 10.1016/j.clinbiomech.2007.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bey MJ, Kline SK, Zauel R, Lock TR, Kolowich PA. Measuring dynamic in-vivo glenohumeral joint kinematics: technique and preliminary results. J Biomech. 2007;41(3):711–714. doi: 10.1016/j.jbiomech.2007.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bey MJ, Zauel R, Brock SK, Tashman S. Validation of a new model-based tracking technique for measuring three-dimensional, in vivo glenohumeral joint kinematics. J Biomech Eng. 2006;128(4):604–609. doi: 10.1115/1.2206199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bigoni M, Gorla M, Guerrasio S, et al. Shoulder evaluation with isokinetic strength testing after arthroscopic rotator cuff repairs. J Shoulder Elbow Surg. 2009;18(2):178–183. doi: 10.1016/j.jse.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 12.Borgmastars N, Paavola M, Remes V, Lohman M, Vastamaki M. Pain relief, motion, and function after rotator cuff repair or reconstruction may not persist after 16 years. Clin Orthop Relat Res. 2010;468(10):2678–2689. doi: 10.1007/s11999-010-1403-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cofield RH, Parvizi J, Hoffmeyer PJ, Lanzer WL, Ilstrup DM, Rowland CM. Surgical repair of chronic rotator cuff tears: a prospective long-term study. J Bone Joint Surg Am. 2001;83(1):71–77. doi: 10.2106/00004623-200101000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Cools AM, Declercq G, Sneyers C, Witvrouw EE. Isokinetic muscle strength and functional restoration following surgical repair of the rotator cuff: a prospective study. Isokinet Exerc Sci. 2006;14:291–300. [Google Scholar]
- 15.Creighton RA, Cole BJ, Nicholson GP, Romeo AA, Lorenz EP. Effect of lateral meniscus allograft on shoulder articular contact areas and pressures. J Shoulder Elbow Surg. 2007;16:367–372. doi: 10.1016/j.jse.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 16.Crisco JJ, Moore DC, Marai GE, et al. Effects of distal radius malunion on distal radioulnar joint mechanics: an in vivo study. J Orthop Res. 2007;25(4):547–555. doi: 10.1002/jor.20322. [DOI] [PubMed] [Google Scholar]
- 17.DeFranco MJ, Bershadsky B, Ciccone J, Yum JK, Iannotti JP. Functional outcome of arthroscopic rotator cuff repairs: a correlation of anatomic and clinical results. J Shoulder Elbow Surg. 2007;16(6):759–765. doi: 10.1016/j.jse.2007.03.020. [DOI] [PubMed] [Google Scholar]
- 18.Fuchs B, Gilbart MK, Hodler J, Gerber C. Clinical and structural results of open repair of an isolated one-tendon tear of the rotator cuff. J Bone Joint Surg Am. 2006;88(2):309–316. doi: 10.2106/JBJS.E.00117. [DOI] [PubMed] [Google Scholar]
- 19.Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86(2):219–224. doi: 10.2106/00004623-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Galatz LM, Griggs S, Cameron BD, Iannotti JP. Prospective longitudinal analysis of postoperative shoulder function: a ten-year follow-up study of full-thickness rotator cuff tears. J Bone Joint Surg Am. 2001;83(7):1052–1056. [PubMed] [Google Scholar]
- 21.Gazielly DF, Gleyze P, Montagnon C. Functional and anatomical results after rotator cuff repair. Clin Orthop Relat Res. 1994;304:43–53. [PubMed] [Google Scholar]
- 22.Goutallier D, Postel JM, Radier C, Bernageau J, Zilber S. Long-term functional and structural outcome in patients with intact repairs 1 year after open transosseous rotator cuff repair. J Shoulder Elbow Surg. 2009;18(4):521–528. doi: 10.1016/j.jse.2008.11.006. [DOI] [PubMed] [Google Scholar]
- 23.Greis PE, Scuderi MG, Mohr A, Bachus KN, Burks RT. Glenohumeral articular contact areas and pressures following labral and osseous injury to the anteroinferior quadrant of the glenoid. J Shoulder Elbow Surg. 2002;11(5):442–451. doi: 10.1067/mse.2002.124526. [DOI] [PubMed] [Google Scholar]
- 24.Gupta R, Lee TQ. Positional-dependent changes in glenohumeral joint contact pressure and force: possible biomechanical etiology of posterior glenoid wear. J Shoulder Elbow Surg. 2005;14(1 Suppl S):105S–110S. doi: 10.1016/j.jse.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 25.Halder AM, Zhao KD, O’Driscoll SW, Morrey BF, An KN. Dynamic contributions to superior shoulder stability. J Orthop Res. 2001;19(2):206–212. doi: 10.1016/S0736-0266(00)00028-0. [DOI] [PubMed] [Google Scholar]
- 26.Hamai S, Moro-oka TA, Miura H, et al. Knee kinematics in medial osteoarthritis during in vivo weight-bearing activities. J Orthop Res. 2009;27(12):1555–1561. doi: 10.1002/jor.20928. [DOI] [PubMed] [Google Scholar]
- 27.Harryman DT, 2nd, Mack LA, Wang KY, Jackins SE, Richardson ML, Matsen FA., 3rd Repairs of the rotator cuff: correlation of functional results with integrity of the cuff. J Bone Joint Surg Am. 1991;73(7):982–989. [PubMed] [Google Scholar]
- 28.Hughes RE, Johnson ME, O’Driscoll SW, An KN. Age-related changes in normal isometric shoulder strength. Am J Sports Med. 1999;27(5):651–657. doi: 10.1177/03635465990270051801. [DOI] [PubMed] [Google Scholar]
- 29.Itoi E, Newman SR, Kuechle DK, Morrey BF, An KN. Dynamic anterior stabilisers of the shoulder with the arm in abduction. J Bone Joint Surg Br. 1994;76(5):834–836. [PubMed] [Google Scholar]
- 30.Jost B, Pfirrmann CW, Gerber C. Clinical outcome after structural failure of rotator cuff repairs. J Bone Joint Surg Am. 2000;82(3):304–314. doi: 10.2106/00004623-200003000-00002. [DOI] [PubMed] [Google Scholar]
- 31.Kelkar R, Wang VM, Flatow EL, et al. Glenohumeral mechanics: a study of articular geometry, contact, and kinematics. J Shoulder Elbow Surg. 2001;10(1):73–84. doi: 10.1067/mse.2001.111959. [DOI] [PubMed] [Google Scholar]
- 32.Kibler WB. Scapular involvement in impingement: signs and symptoms. Instr Course Lect. 2006;55:35–43. [PubMed] [Google Scholar]
- 33.Kibler WB, McMullen J, Uhl T. Shoulder rehabilitation strategies, guidelines, and practice. Orthop Clin North Am. 2001;32(3):527–538. doi: 10.1016/s0030-5898(05)70222-4. [DOI] [PubMed] [Google Scholar]
- 34.Kim DH, Elattrache NS, Tibone JE, et al. Biomechanical comparison of a single-row versus double-row suture anchor technique for rotator cuff repair. Am J Sports Med. 2006;34(3):407–414. doi: 10.1177/0363546505281238. [DOI] [PubMed] [Google Scholar]
- 35.Kim HM, Teefey SA, Zelig A, Galatz LM, Keener JD, Yamaguchi K. Shoulder strength in asymptomatic individuals with intact compared with torn rotator cuffs. J Bone Joint Surg Am. 2009;91(2):289–296. doi: 10.2106/JBJS.H.00219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kim KJ, Lee SB, An KN, Morrey BF. A method to determine the effect of the individual rotator cuff muscles to dynamic jont stability of the shoulder. ASME Advances in Bioengineering. 1998;39:385–386. [Google Scholar]
- 37.Kirkley A, Alvarez C, Griffin S. The development and evaluation of a disease-specific quality-of-life questionnaire for disorders of the rotator cuff: the Western Ontario Rotator Cuff Index. Clin J Sport Med. 2003;13(2):84–92. doi: 10.1097/00042752-200303000-00004. [DOI] [PubMed] [Google Scholar]
- 38.Klintberg IH, Gunnarsson AC, Svantesson U, Styf J, Karlsson J. Early loading in physiotherapy treatment after full-thickness rotator cuff repair: a prospective randomized pilot-study with a two-year follow-up. Clin Rehabil. 2009;23(7):622–638. doi: 10.1177/0269215509102952. [DOI] [PubMed] [Google Scholar]
- 39.Knudsen HB, Gelineck J, Sojbjerg JO, Olsen BS, Johannsen HV, Sneppen O. Functional and magnetic resonance imaging evaluation after single-tendon rotator cuff reconstruction. J Shoulder Elbow Surg. 1999;8(3):242–246. doi: 10.1016/s1058-2746(99)90136-2. [DOI] [PubMed] [Google Scholar]
- 40.Kuhlman JR, Iannotti JP, Kelly MJ, Riegler FX, Gevaert ML, Ergin TM. Isokinetic and isometric measurement of strength of external rotation and abduction of the shoulder. J Bone Joint Surg Am. 1992;74(9):1320–1333. [PubMed] [Google Scholar]
- 41.Kuhn JE. Exercise in the treatment of rotator cuff impingement: a systematic review and a synthesized evidence-based rehabilitation protocol. J Shoulder Elbow Surg. 2009;18(1):138–160. doi: 10.1016/j.jse.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 42.Langenderfer JE, Rullkoetter PJ, Mell AG, Laz PJ. A multi-subject evaluation of uncertainty in anatomical landmark location on shoulder kinematic description. Comput Methods Biomech Biomed Engin. 2009;12(2):211–216. doi: 10.1080/10255840903093441. [DOI] [PubMed] [Google Scholar]
- 43.Lee SB, Kim KJ, O’Driscoll SW, Morrey BF, An KN. Dynamic glenohumeral stability provided by the rotator cuff muscles in the mid-range and end-range of motion: a study in cadavera. J Bone Joint Surg Am. 2000;82(6):849–857. doi: 10.2106/00004623-200006000-00012. [DOI] [PubMed] [Google Scholar]
- 44.Lu TW, Tsai TY, Kuo MY, Hsu HC, Chen HL. In vivo three-dimensional kinematics of the normal knee during active extension under unloaded and loaded conditions using single-plane fluoroscopy. Med Eng Phys. 2008;30(8):1004–1012. doi: 10.1016/j.medengphy.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 45.Ludewig PM, Braman JP. Shoulder impingement: biomechanical considerations in rehabilitation. Man Ther. 2011;16(1):33–39. doi: 10.1016/j.math.2010.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Marai GE, Laidlaw DH, Demiralp C, Andrews S, Grimm CM, Crisco JJ. Estimating joint contact areas and ligament lengths from bone kinematics and surfaces. IEEE Trans Biomed Eng. 2004;51(5):790–799. doi: 10.1109/TBME.2004.826606. [DOI] [PubMed] [Google Scholar]
- 47.McPherson EJ, Friedman RJ, An YH, Chokesi R, Dooley RL. Anthropometric study of normal glenohumeral relationships. J Shoulder Elbow Surg. 1997;6(2):105–112. doi: 10.1016/s1058-2746(97)90030-6. [DOI] [PubMed] [Google Scholar]
- 48.Milgrom C, Schaffler M, Gilbert S, van Holsbeeck M. Rotator-cuff changes in asymptomatic adults: the effect of age, hand dominance and gender. J Bone Joint Surg Br. 1995;77(2):296–298. [PubMed] [Google Scholar]
- 49.Millett PJ, Wilcox RB, 3rd, O’Holleran JD, Warner JJ. Rehabilitation of the rotator cuff: an evaluation-based approach. J Am Acad Orthop Surg. 2006;14(11):599–609. doi: 10.5435/00124635-200610000-00002. [DOI] [PubMed] [Google Scholar]
- 50.Moro-oka TA, Hamai S, Miura H, et al. Dynamic activity dependence of in vivo normal knee kinematics. J Orthop Res. 2008;26(4):428–434. doi: 10.1002/jor.20488. [DOI] [PubMed] [Google Scholar]
- 51.Neer CS., 2nd Anterior acromioplasty for the chronic impingement syndrome in the shoulder: a preliminary report. J Bone Joint Surg Am. 1972;54(1):41–50. [PubMed] [Google Scholar]
- 52.Neer CS., 2nd Impingement lesions. Clin Orthop Relat Res. 1983;173:70–77. [PubMed] [Google Scholar]
- 53.Nho SJ, Brown BS, Lyman S, Adler RS, Altchek DW, MacGillivray JD. Prospective analysis of arthroscopic rotator cuff repair: prognostic factors affecting clinical and ultrasound outcome. J Shoulder Elbow Surg. 2009;18(1):13–20. doi: 10.1016/j.jse.2008.05.045. [DOI] [PubMed] [Google Scholar]
- 54.Nich C, Mutschler C, Vandenbussche E, Augereau B. Long-term clinical and MRI results of open repair of the supraspinatus tendon. Clin Orthop Relat Res. 2009;467(10):2613–2622. doi: 10.1007/s11999-009-0917-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Paletta GA, Jr, Warner JJ, Warren RF, Deutsch A, Altchek DW. Shoulder kinematics with two-plane x-ray evaluation in patients with anterior instability or rotator cuff tearing. J Shoulder Elbow Surg. 1997;6(6):516–527. doi: 10.1016/s1058-2746(97)90084-7. [DOI] [PubMed] [Google Scholar]
- 56.Reinold MM, Escamilla RF, Wilk KE. Current concepts in the scientific and clinical rationale behind exercises for glenohumeral and scapulothoracic musculature. J Orthop Sports Phys Ther. 2009;39(2):105–117. doi: 10.2519/jospt.2009.2835. [DOI] [PubMed] [Google Scholar]
- 57.Rokito AS, Zuckerman JD, Gallagher MA, Cuomo F. Strength after surgical repair of the rotator cuff. J Shoulder Elbow Surg. 1996;5(1):12–17. doi: 10.1016/s1058-2746(96)80025-5. [DOI] [PubMed] [Google Scholar]
- 58.Shah AA, Milos S, Deutsch A. The strength and effects of humeral rotation on single- versus double-row repair techniques in small rotator cuff tears. Orthopedics. 2010;33(1):22. doi: 10.3928/01477447-20091124-12. [DOI] [PubMed] [Google Scholar]
- 59.Soslowsky LJ, Flatow EL, Bigliani LU, Pawluk RJ, Ateshian GA, Mow VC. Quantitation of in situ contact areas at the glenohumeral joint: a biomechanical study. J Orthop Res. 1992;10(4):524–534. doi: 10.1002/jor.1100100407. [DOI] [PubMed] [Google Scholar]
- 60.Su WR, Budoff JE, Luo ZP. The effect of posterosuperior rotator cuff tears and biceps loading on glenohumeral translation. Arthroscopy. 2010;26(5):578–586. doi: 10.1016/j.arthro.2009.09.007. [DOI] [PubMed] [Google Scholar]
- 61.van Holsbeeck M, Introcaso JH. Musculoskeletal Ultrasound. 2nd ed. Mosby; Philadelphia: 2001. [Google Scholar]
- 62.van Holsbeeck MT, Kolowich PA, Eyler WR, et al. US depiction of partial-thickness tear of the rotator cuff. Radiology. 1995;197(2):443–446. doi: 10.1148/radiology.197.2.7480690. [DOI] [PubMed] [Google Scholar]
- 63.Warner JJ, Bowen MK, Deng XH, Hannafin JA, Arnoczky SP, Warren RF. Articular contact patterns of the normal glenohumeral joint. J Shoulder Elbow Surg. 1998;7(4):381–388. doi: 10.1016/s1058-2746(98)90027-1. [DOI] [PubMed] [Google Scholar]
- 64.Werner CM, Blumenthal S, Curt A, Gerber C. Subacromial pressures in vivo and effects of selective experimental suprascapular nerve block. J Shoulder Elbow Surg. 2006;15(3):319–323. doi: 10.1016/j.jse.2005.08.017. [DOI] [PubMed] [Google Scholar]
- 65.Werner CM, Weishaupt D, Blumenthal S, Curt A, Favre P, Gerber C. Effect of experimental suprascapular nerve block on active glenohumeral translations in vivo. J Orthop Res. 2006;24(3):491–500. doi: 10.1002/jor.20011. [DOI] [PubMed] [Google Scholar]
- 66.Wu G, van der Helm FC, Veeger HE, et al. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion. Part II: shoulder, elbow, wrist and hand. J Biomech. 2005;38(5):981–992. doi: 10.1016/j.jbiomech.2004.05.042. [DOI] [PubMed] [Google Scholar]
- 67.Wuelker N, Korell M, Thren K. Dynamic glenohumeral joint stability. J Shoulder Elbow Surg. 1998;7(1):43–52. doi: 10.1016/s1058-2746(98)90182-3. [DOI] [PubMed] [Google Scholar]
- 68.Xue Q, Huang G. Dynamic stability of glenohumeral joint during scapular plane elevation. Chin Med J. 1998;111(5):447–449. [PubMed] [Google Scholar]
- 69.Yamaguchi K, Sher JS, Andersen WK, et al. Glenohumeral motion in patients with rotator cuff tears: a comparison of asymptomatic and symptomatic shoulders. J Shoulder Elbow Surg. 2000;9(1):6–11. doi: 10.1016/s1058-2746(00)90002-8. [DOI] [PubMed] [Google Scholar]
- 70.Yamaguchi K, Tetro AM, Blam O, Evanoff BA, Teefey SA, Middleton WD. Natural history of asymptomatic rotator cuff tears: a longitudinal analysis of asymptomatic tears detected sonographically. J Shoulder Elbow Surg. 2001;10(3):199–203. doi: 10.1067/mse.2001.113086. [DOI] [PubMed] [Google Scholar]
- 71.Yu J, McGarry MH, Lee YS, Duong LV, Lee TQ. Biomechanical effects of supraspinatus repair on the glenohumeral joint. J Shoulder Elbow Surg. 2005;14(1 Suppl S):65S–71S. doi: 10.1016/j.jse.2004.09.019. [DOI] [PubMed] [Google Scholar]
- 72.Zumstein MA, Jost B, Hempel J, Hodler J, Gerber C. The clinical and structural long-term results of open repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2008;90(11):2423–2431. doi: 10.2106/JBJS.G.00677. [DOI] [PubMed] [Google Scholar]