Abstract
Background
Planar bone scintigraphy (PBS) is often advocated for diagnosing occult scaphoid fractures. PBS is a sensitive diagnostic modality, but lacks specificity, which may result in over-diagnosis.
Purpose
To examine, in a pilot study, the potential additional value of single photon emission computed tomography (SPECT) combined with low dose computed tomography (CT) for the diagnosis of an occult scaphoid fracture.
Material and Methods
Ten patients that underwent combined PBS and SPECT/CT for a clinically suspected scaphoid fracture, where radiographs could not detect a fracture, were included in this pilot study. The PBS and SPECT/CT results were independently and separately evaluated by a nuclear physician for scaphoid fractures and other injuries.
Results
PBS was positive for a scaphoid fracture in four patients and diagnosed three other fractures. SPECT/CT showed five scaphoid fractures and one other fracture. SPECT/CT – PBS had discrepant results in three patients. In two patients PBS diagnosed a trapezoid fracture where SPECT/CT showed a scaphoid fracture. The other patient was diagnosed with a scaphoid fracture on PBS, whereas SPECT/CT showed bone bruise of other carpal bones.
Conclusion
SPECT/CT has the potential to be more accurate than PBS as it uses anatomical information of the CT to discriminate between the scaphoid, other carpal bones, and bone bruises. Larger studies with an independent reference standard are needed for confirmation of these preliminary data.
Keywords: Scaphoid bone, single photon emission computed tomography (SPECT), computed tomography (CT), fracture
Introduction
Magnetic resonance imaging (MRI), computed tomography (CT), or planar bone scintigraphy (PBS) are performed to detect an occult scaphoid fracture if scaphoid radiographs show no fracture. The value of these diagnostic tools have been widely investigated and still no consensus exists on the preferred workup of a patient with a clinically suspected scaphoid fracture and with a normal conventional radiograph (1). The American College of Radiology recommends scaphoid radiographs as the first line of investigation in patients with a suspected scaphoid fracture. If these do not show a fracture, a second line of investigation such as MRI or CT is proposed (2). PBS can also be used as second line investigation; however, it is usually not appropriate.
It is important to diagnose an occult scaphoid fracture early because, if left untreated, it may give rise to serious complications such as osteonecrosis, non-union, carpal instability, and functional impairment (3–8). Among the advanced diagnostic modalities for this specific patient group, PBS is favored for its high sensitivity in confirmation of scaphoid fractures. The disadvantage of PBS, however, is its lower specificity compared to MRI and CT (9–12).
PBS uses a radiopharmaceutical, technetium-99 m hydroxymethylene diphosphonate (99mTc HDP), which accumulates on the surface of the by osteoblasts induced growing hydroxyapatite crystal. After trauma, osteoblasts at the fracture site are activated and the HDP will accumulate at the activated osteoblasts. The PBS will show increased uptake. However, not only fractures will show increased activity; there will also be accumulation of the radiopharmaceutical in activated osteoblasts at the site of osteoarthritis and extensive bone bruise. Also infections or other inflammation lead to increased activity (13). A concern related to PBS is the determination of the exact localization of the fracture. Especially when there is a fracture of one of the bones articulating with the scaphoid, a false positive diagnosis of a scaphoid fracture may result (10,14). Single photon emission computed tomography (SPECT) can improve the diagnostic performance of bone functional imaging (15). The hybrid SPECT/CT systems combine SPECT with CT and have proven to result in a more accurate localization and characterization of other than carpal skeletal lesions (16,17).
The aim of the current pilot study was to investigate if SPECT/CT is of additional value, in comparison with PBS, in the diagnostic workup for suspected scaphoid fractures.
Material and Methods
Patients
The study proposal was approved by the institutional Ethics Committee and financial and logistic resources were organized for 10 patients. Between May 2010 and May 2011, in patients who visited the Emergency Department (ED) with a clinically suspected scaphoid fracture and negative scaphoid radiographs, an additional PBS was made. The attending nuclear physician evaluated the PBS. If there was any activity on the PBS an additional SPECT/CT was made. Inclusion was stopped after the first 10 patients had agreed to participate.
Study protocol
A clinically suspected scaphoid fracture with negative scaphoid radiographs was defined as pain in the anatomic snuffbox when applying axial pressure on the first or second digit (18), after a recent trauma (within 48 h) and no evidence of a fracture on conventional scaphoid radiographs (PA, lateral, and 2–4 specific views). If a patient was suitable for inclusion, a SPECT/CT was performed after informed consent. Poly-trauma patients, patients aged less than 18 years, and those with contraindications for bone scintigraphy were excluded.
The PBS was made 3–5 days after injury. A three-phase bone scintigraphy was performed immediately after intravenous injection of 550 MBq 99mTc-HDP. Dynamic images were acquired during 2 min on a single or two-headed gamma camera (Symbia T6, Siemens, Erlangen, Germany or Toshiba GCA-7200 pi/7200di/7100ui, Toshiba, Tokyo, Japan), displayed on a 128 × 128 matrix, zoom factor 1.0, with the hands on the camera head in palmar projection. Five hours after tracer injection planar images of the hands were made for osteoblast activity analysis. The same study protocol and position as the dynamic images were applied, but now displayed on a 256 × 256 matrix, zoom factor 1.5.
The SPECT/CT was performed on the two-headed gamma camera (Symbia T6, Siemens, Erlangen, Germany, with 6-slice CT), using a low-energy high-resolution collimator. Images were acquired for 15 s in each camera position. A total of 64 views were taken to cover 360°. The energy window was set to 140 keV with a 20% window. The images were acquired in a 128 × 128 matrix with a zoom factor of 1.23. Reconstruction was performed using iterative reconstruction OSEM (ordered subset expectation maximization). We used a low dose CT, step and shoot protocol (25 mA, 130 kV, FOV 300 mm) with 2.0 mm slice thickness. Images were reconstructed in the axial, coronal and sagittal planes. SPECT and low dose CT were fused on a dedicated nuclear medicine workstation using the MedView (MedImage Inc., Ann Arbor, MI, USA) software package.
Image analysis
The images were analyzed by one nuclear physician with 4 years of experience as a specialist. The PBS results and additional SPECT/CT images were evaluated independently and separately. Clinical information and data were anonymized. The age of the patient was not blinded as the information is needed to evaluate a PBS for osteoarthritic changes. The images were evaluated in random order by a nuclear physician for scaphoid fractures, other fractures, bone bruise, and other diagnoses. The PBS and SPECT/CT images were evaluated separately but because of the small number of scans the observer could recognize a PBS and SPECT/CT of the same patient.
Results
Ten patients were included (5 men, 5 women; mean age, 40.4 years; age range, 19–72 years). Table 1 summarizes the results for the PBS and SPECT/CT.
Table 1.
Final diagnosis of PBS and SPECT/CT – in the last column the congruence or incongruence between PBS and SPECT/CT are indicated.
| Patient | Diagnosis on PBS | Diagnosis on SPECT/CT | Congruent +/Incongruent (–) |
|---|---|---|---|
| 1 | Distal radius fracture | Distal radius fracture | + |
| 2 | Scaphoid fracture | Scaphoid fracture | + |
| 3 | Trapezium fracture | Scaphoid fracture | – |
| 4 | Scaphoid fracture | Scaphoid fracture | + |
| 5 | Scaphoid fracture | Bone bruise carpus* | – |
| 6 | Trapezoid fracture | Scaphoid fracture | – |
| 7 | No fracture | No fracture | + |
| 8 | Scaphoid fracture | Scaphoid fracture | + |
| 9 | No fracture | No fracture | + |
| 10 | Bone bruise scaphoid | Bone bruise trapezium | + |
In this patient MCP-1, CMC-1, scaphoid, trapezium, triquetrum, and hamatum showed increased activity.
In seven patients PBS and SPECT/CT had corresponding outcomes: In three patients the images showed a scaphoid fracture, in one patient a distal radius fracture and in one patient a bone bruise. Two patients had some atypical activity on PBS with however a final diagnosis of “no fracture nor bone bruise” on PBS and SPECT/CT.
The three discrepant SPECT/CT – PBS results concerned two patients that were diagnosed with a trapezoid fracture with PBS and a scaphoid fracture with SPECT/CT. The third patient was diagnosed with a scaphoid fracture on PBS, whereas SPECT/CT showed bone bruises of other carpal bones.
Figs. 1 and 2 illustrate the discrepancies between PBS and SPECT/CT. Fig. 3 clearly demonstrates the increased exactness of SPECT/CT for anatomical localization, as compared with PBS.
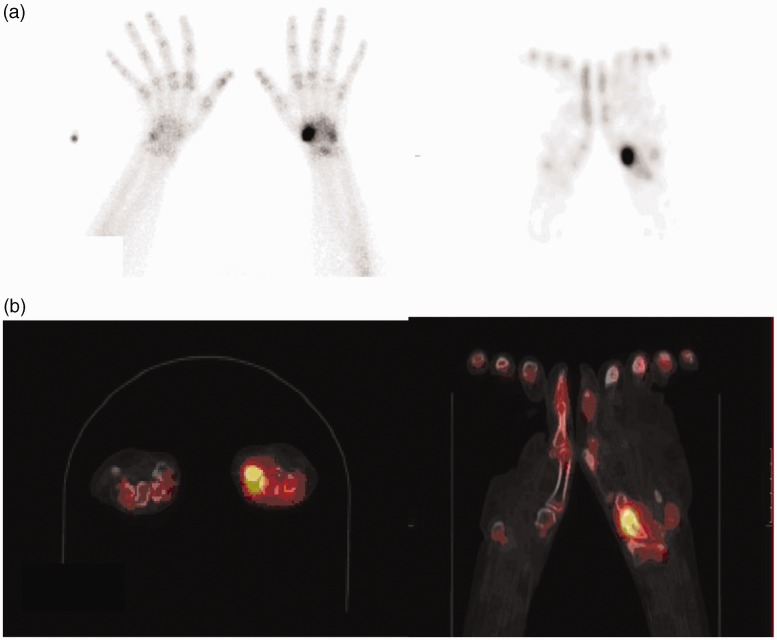
Fig. 1.
Patient 3 in Table 1. PBS (a) revealed increase bone activity in a radial carpal bone, probably trapezium. The fusion image of the SPECT/CT (b) shows the more circumscript area of the tracer uptake to be centred slightly more proximal, very suspect for (distal) scaphoid fracture.
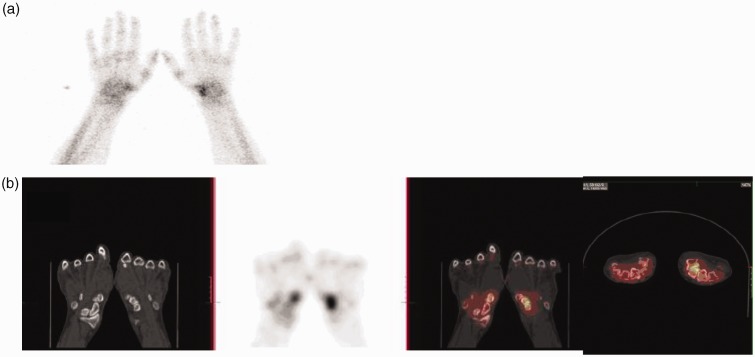
Fig. 2.
Patient 5 in Table 1. PBS (a) was suspect for a scaphoid fracture. SPECT/CT (b) axial and coronal view of the same patient showed no activity around the scaphoid but in the intercarpal region. This scan was evaluated as bone bruise of other carpal bones.
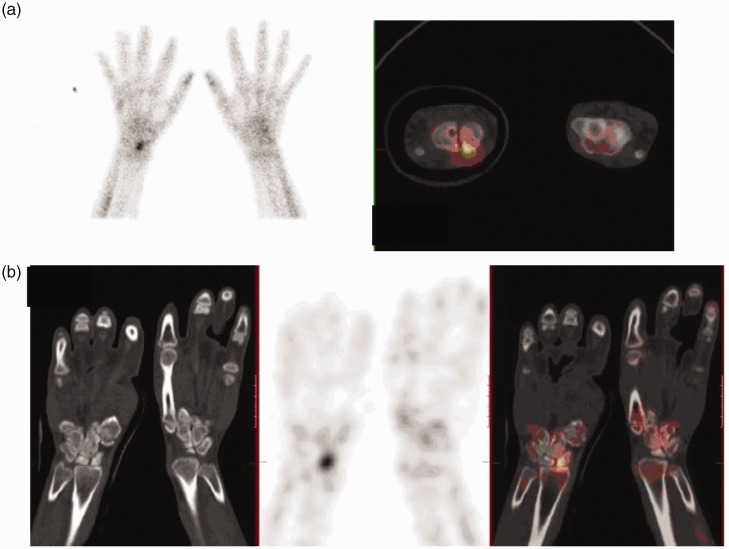
Fig. 3.
Patient 4 in Table 1. PBS (a) was positive for scaphoid fracture. SPECT/CT (b) illustrates that the exact localization of the fracture concerns the proximal pole of the scaphoid and that it concerns a small fracture fragment. You can clearly see that the arm is in plaster.
Discussion
This pilot study investigated the potential additional value of SPECT/CT in the diagnostic workup for suspected scaphoid fractures as compared with PBS.
Within the limitations of a small pilot study we found that SPECT/CT seems to adequately localize fractures in the carpus and therefore may be more specific and even more sensitive than PBS in diagnosing scaphoid fractures, according to anatomical location; the SPECT/CT clearly showed two scaphoid fractures in patients for which the PBS was negative regarding scaphoid fractures. The more exact anatomical information helps to discriminate between scaphoid fracture and fractures of other carpal bones. It also serves to specifically depict the fracture site in the scaphoid bone and whether it is localized proximally or distally in the scaphoid bone. This specification has distinct treatment consequences and is thus a clinically relevant addition in the diagnostic process (19). Moreover, a fracture line visible on CT can distinguish a bone bruise from a fracture.
The definite diagnosis of a scaphoid fracture is still being recognized as a challenge. There is no consensus about the best diagnostic strategy for a patient with a clinically suspected scaphoid fracture with a negative scaphoid specific radiograph (1,20,21). CT, MRI, and PBS all have been widely investigated for their diagnostic performance. A recent meta-analysis of Yin et al. (22) favors MRI, because follow-up radiographs and CT are less sensitive, and PBS is less specific.
The American College of Radiology (ACR) recommends performing MRI in case of a suspected scaphoid fracture with a negative scaphoid radiograph. However, cast immobilization with repeated radiographs after 2 weeks and CT are also appropriate. The ACR does not specifically recommend PBS but states that PBS may be useful when combined with SPECT/CT (2).
With MRI as upcoming diagnostic modality PBS is being used less for diagnosing scaphoid fractures. However PBS is still the most sensitive modality (9,22). Moreover, by combining it with SPECT/CT it may be as specific as MRI. A disadvantage of SPECT/CT is the higher radiation exposure compared with MRI and CT (SPECT/CT 4 mSv, CT 0.03 mSv, MRI no radiation exposure, background radiation 2.5 mSv a year) (10,23).
To our knowledge two similar studies recently investigated the clinical value of SPECT/CT in the diagnosis of radiological occult scaphoid fractures. Alainmat et al. illustrated that SPECT/CT showed bone disruptions as well as carpal-associated lesions and differentiated chronic arthritis or ligament lesions in five patients (24). Querellou et al. evaluated 57 patients with a clinically suspected scaphoid fracture and a negative conventional radiograph, using SPECT/CT and MRI (17). They concluded that SPECT/CT is more sensitive for a fracture in the carpal area, as it detected 10 more carpal fractures than MRI. However, in this study relatively high numbers of bone bruises were diagnosed on MRI. Moreover the discriminative value of the MRI for fractures and bone bruises remains topic of debate. Also the clinical implications of a bone bruise remains disputed (25,26).
Studies on different anatomical areas underline the additional value of SPECT and the potential benefits of combined SPECT/CT in orthopedics and trauma (16,27–30). The major advantage of SPECT/CT is the combination of the high sensitivity of SPECT with the specificity of CT. This may result in a higher diagnostic accuracy.
This increased diagnostic accuracy will be of major benefit, especially for a small and complex anatomic area as the carpal region including the scaphoid bone.
As in many pilot studies, this study presents itself with the inherent limitations of a small pilot study. No statistical significance could be tested. In addition, the lack of a generally accepted reference standard to compare SPECT/CT to, presented a challenge to this study. However, this problem is inherent to the fact that there are no alternative diagnostics that are more reliable by means of both high sensitivity and specificity for occults scaphoid fractures.
Another limitation is that we only made a SPECT/CT of patients with activity on PBS. However as both diagnostic modalities use the same substrate, i.e. the uptake of 99mTc HDP, we believe that if PBS showed no activity, SPECT/CT also would not.
In conclusion, SPECT/CT facilitates the detection of occult fractures and presents additional information about the injury site and localization of the fracture. SPECT/CT could potentially serve as a future reference standard for studies concerning the scaphoid fracture, but additional research with an independent reference standard is needed to confirm these preliminary suggestions.
Footnotes
*Equal contributors.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Yin ZG, Zhang JB, Kan SL, et al. Diagnosing suspected scaphoid fractures: a systematic review and meta-analysis. Clin Orthop Relat Res 2010; 468: 723–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Newberg A, Dalinka MK, Alazraki N, et al. Acute hand and wrist trauma. American College of Radiology. ACR Appropriateness Criteria. Radiology 2000; 215: 375–378. [PubMed] [Google Scholar]
- 3.Brydie A, Raby N. Early MRI in the management of clinical scaphoid fracture. Br J Radiol 2003; 76: 296–300. [DOI] [PubMed] [Google Scholar]
- 4.Cooney WP. Scaphoid fractures: current treatments and techniques. Instr Course Lect 2003; 52: 197–208. [PubMed] [Google Scholar]
- 5.Gaebler C, Kukla C, Breitenseher M, et al. Magnetic resonance imaging of occult scaphoid fractures. J Trauma 1996; 41: 73–76. [DOI] [PubMed] [Google Scholar]
- 6.Krasin E, Goldwirth M, Gold A, et al. Review of the current methods in the diagnosis and treatment of scaphoid fractures. Postgrad Med J 2001; 77: 235–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Prosser GH, Isbister ES. The presentation of scaphoid non-union. Injury 2003; 34: 65–67. [DOI] [PubMed] [Google Scholar]
- 8.Roolker W, Maas M, Broekhuizen AH. Diagnosis and treatment of scaphoid fractures, can non-union be prevented? Arch OrthopTrauma Surg 1999; 119: 428–431. [DOI] [PubMed] [Google Scholar]
- 9.Beeres FJ, Rhemrev SJ, den HP, et al. Early magnetic resonance imaging compared with bone scintigraphy in suspected scaphoid fractures. J Bone Joint Surg Br 2008; 90: 1205–1209. [DOI] [PubMed] [Google Scholar]
- 10.Rhemrev SJ, de Zwart AD, Kingma LM, et al. Early computed tomography compared with bone scintigraphy in suspected scaphoid fractures. Clin Nucl Med 2010; 35: 931–934. [DOI] [PubMed] [Google Scholar]
- 11.Beeres F, Hogervorst M, Den Hollander P, et al. Outcome of routine bone scintigraphy in suspected scaphoid fractures. Injury 2005; 36: 1233–1236. [DOI] [PubMed] [Google Scholar]
- 12.Wilson AW, Kurer MH, Peggington JL, et al. Bone scintigraphy in the management of X-ray-negative potential scaphoid fractures. Arch Emerg Med 1986; 3: 235–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Makino N, Ishigaki T, Takamatsu K, et al. The utility of three-phase bone scintigraphy in the assessment of fractured carpal scaphoid. Kaku Igaku 1993; 30: 1063–1073. [PubMed] [Google Scholar]
- 14.Rhemrev SJ, van Leerdam RH, Beeres FJ, et al. Bone scintigraphy in patients with clinical suspicion of a scaphoid fracture. Eur J Emerg Med 2010; 17: 124–125. [DOI] [PubMed] [Google Scholar]
- 15.Savelli G, Maffioli L, Maccauro M, et al. Bone scintigraphy and the added value of SPECT (single photon emission tomography) in detecting skeletal lesions. Q J Nucl Med 2001; 45: 27–37. [PubMed] [Google Scholar]
- 16.Scharf S. SPECT/CT imaging in general orthopedic practice. Semin Nucl Med 2009; 39: 293–307. [DOI] [PubMed] [Google Scholar]
- 17.Querellou S, Arnaud L, Williams T, et al. Role of SPECT/CT compared with MRI in the diagnosis and management of patients with wrist trauma occult fractures. Clin Nucl Med 2014; 39: 8–13. [DOI] [PubMed] [Google Scholar]
- 18.Rhemrev SJ, Beeres FJ, van Leerdam RH, et al. Clinical prediction rule for suspected scaphoid fractures: A prospective cohort study. Injury 2010; 41: 1026–1030. [DOI] [PubMed] [Google Scholar]
- 19.Bond CD, Shin AY, McBride MT, et al. Percutaneous screw fixation or cast immobilization for nondisplaced scaphoid fractures. J Bone Joint Surg Am 2001; 83: 483–488. [DOI] [PubMed] [Google Scholar]
- 20.Ring D, Lozano-Calderon S. Imaging for suspected scaphoid fracture. J Hand Surg Am 2008; 33: 954–957. [DOI] [PubMed] [Google Scholar]
- 21.Buijze GA, Mallee W, Beeres FJP, et al. Diagnostic performance tests for suspected scaphoid fractures differ with conventional and latent class analysis. Clin Orthop Relat Res 2011; 469: 3400–3407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yin ZG, Zhang Jb, Kan SL, et al. Diagnostic accuracy of imaging modalities for suspected scaphoid fractures: meta-analysis combined with latent class analysis. J Bone Joint Surg Br 2012; 94: 1077–1085. [DOI] [PubMed] [Google Scholar]
- 23.Biswas D, Bible JE, Bohan M, et al. Radiation exposure from musculoskeletal computerized tomographic scans. J Bone Joint Surg 2009; 91: 1882–1889. [DOI] [PubMed] [Google Scholar]
- 24.Allainmat L, Aubault M, Noël V, et al. Use of hybrid SPECT/CT for diagnosis of radiographic occult fractures of the wrist. Clin Nucl Med 2013; 38: 246–251. [DOI] [PubMed] [Google Scholar]
- 25.de Zwart A, Beeres F, Ring D, et al. MRI as a reference standard for suspected scaphoid fractures. Br J Radiol 2012; 85: 1098–1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thavarajah D, Syed T, Shah Y, et al. Does scaphoid bone bruising lead to occult fracture? A prospective study of 50 patients. Injury 2011; 42: 1303–1306. [DOI] [PubMed] [Google Scholar]
- 27.Roolker W, Tiel-van Buul MM, Broekhuizen AH, et al. Improved wrist fracture localization with digital overlay of bone scintigrams and radiographs. J Nucl Med 1997; 38: 1600–1603. [PubMed] [Google Scholar]
- 28.Bryant LR, Song WS, Banks KP, et al. Comparison of planar scintigraphy alone and with SPECT for the initial evaluation of femoral neck stress fracture. Am J Roentgenol 2008; 191: 1010–1015. [DOI] [PubMed] [Google Scholar]
- 29.Henriksen OM, Lonsdale MN, Jensen TD, et al. Two-dimensional fusion imaging of planar bone scintigraphy and radiographs in patients with clinical scaphoid fracture: an imaging study. Acta Radiol 2009; 50: 71–77. [DOI] [PubMed] [Google Scholar]
- 30.Linke R, Kuwert T, Uder M, et al. Skeletal SPECT/CT of the peripheral extremities. Am J Roentgenol 2010; 194: 329–335. [DOI] [PubMed] [Google Scholar]