Abstract
Objective
The aim of this study was to analyze the prevalence of HPV and EBV in oral and oropharyngeal squamous cell carcinoma in south-eastern Poland. The correlation between viral infection, OSCC, alcohol use, tobacco smoking, demographic data (gender, age, place of residence), anatomic location, pre-treatment staging, evidence of metastases to lymph nodes, and grading was also investigated.
Methods
The examination samples were collected from paraffin tissue blocks, from 154 patients. Viral DNA was amplified by the nested-PCR method.
Results
HPV DNA was detected in 29.2 % of the tested samples (in 27.4 % of oropharyngeal and in 30.4 % of oral cavity). The HPV type 16 was detected in 15.6 % of all samples, and in 53.3 % of HPV-positive group. In HPV-positive samples from oropharyngeal HPV 16 constitute 76.5 %, and in HPV-positive samples from oral cavity HPV 16 constitute 39.3 %. Mixed infection (more than one type of HPV) was observed in 23.5 and 60.7 %, respectively, and in 46.7 % of all HPV-positive samples, and in 12.3 % of the whole study group. EBV DNA was detected in 27.3 % of the cases and HPV-EBV co-infection in 7.8 % of samples.
Conclusions
In major patients from Southeastern region of Poland with oropharyngeal cancer HPV type 16 was detected but in oral cavity cancer other mixed infections were observed (i.e. 51, 52, 59, 66, 68, 71, 74). HPV 16 was detected more often among patients younger than 50 years of age, whereas the mixed HPV in the group aged 50–59. The pathogenesis of oral squamous cell carcinoma may be connected with EBV infection. Future studies on the mechanisms of HPV/EBV co-infection and/or superinfection and their role in oral squamous cell carcinoma are necessary.
Keywords: Epstein-Barr virus, Human papillomavirus, Oral and oropharyngeal squamous cell carcinoma (OSCC), Co-infection
Introduction
Oral squamous cell carcinoma (OSCC) is a serious public health problem in many parts of the world and in Poland too. In Poland oral and oropharyngeal cancer constitutes 3.8 % cancers among men and 1.3 % cancers among women [1]. Oral and oropharyngeal squamous cell carcinoma (OSCC) in tumor histology accounts for more than 90 % of the cases [2]. The etiology of OSCC is considered to be multifactorial and the factors influencing it include environmental factors, life style, infection agents and genetic alterations. The main predisposing factors are tobacco and alcohol abuse [3]. An important role in the etiology of many of them is played by the oncogenic viruses [2]. The cancerogenecity of HPV in humans was conducted by the International Agency for Research on Cancer (IARC) in 2007 and 2012 [4, 5].
The first original observation that implicated HPV as a risk factor in the development of oral cancer was presented by Syrjänen et al. in 1983 [6]. Since then, several studies have focused on HPV detection in oral cancer [7]. A more recent study by Syrjänen and Syrjänen showed a strong association between the presence of HPV DNA, specifically HPV16, and OSCC [8]. This meta-analysis showed that HPV significantly increases the risk for OSCC, as compared with controls. HPV positive oropharyngeal cancer varied according to the geographical region, i.e. in North America – 56 %, in Japan 52 %, in Australia 45 %, in Northern and West Europe 38 % [9].
Epstein-Barr virus, which is also known as human herpesvirus 4 (HHV-4) and which belongs to the Herpesviridae family, has a double-stranded DNA genome [10]. EBV is an enveloped virus with icosahedral capsids symmetry and the genome takes on a linear form in mature virions and a circular episomal form during the period of latency in the infected cells. This is one of the most common viruses in humans [11]. EBV was the first human virus to which the oncogenic potential was attributed, and it is classified as group 1 carcinogen by the World Health Organization’s International Agency for Research on Cancer [12]. EBV is correlated with nasopharyngeal and gastric carcinoma, squamous cell carcinoma, Hodgkin’s lymphoma, and Burkitt’s lymphoma [10, 13–15]. Current investigations suggest that EBV is correlated with many diseases localized in the oral cavity such as gingivitis, periodontitis, pulpitis, periapical inflammations and periodontal abscesses [14, 16]. A lot of studies indicate co-infection with HPV and EBV viruses in oral squamous cell carcinoma [17, 18].
The aim of this study was to analyze the prevalence of HPV and EBV and their co-infection in oral and oropharyngeal squamous cell carcinoma in south-eastern Poland.
Material and methods
Sample collection
Tissue samples were obtained from 154 patients with primary oral and oropharyngeal SCC treated in the Chair and Department of Otolaryngology and Laryngological Oncology of the Medical University of Lublin. Samples were collected in 2006–2009. The group consisted of 131 males and 23 females, aged between 40 and 87 (average 56.8 years). In the examination group there were 92 patients with oral, and 62 with oropharyngeal SCC. It was a retrospective investigation and the examined materials were obtained from formalin-fixed, paraffin-embedded tissues. The samples were collected during surgery, but TNM was calculated during primary diagnosis (T-tumor, N-nodus, M-metastasis). One hundred percent of the patients were classified as N0, M0. The patients were treated surgically with or without postoperative radiotherapy, depending on the clinical stage of the disease. The patients did not receive radiotherapy or chemotherapy before. TNM classification was done according to the criteria of the Union Against Cancer (UICC) [19]. Histological grading was performed according to the World Health Organization criteria, which divide tumors into three types: well differentiated (G1), moderately differentiated (G2), and poorly differentiated (G3) [20].
This research was approved by the Ethics Committee and it was is in accordance with the GCP regulations (no. KE-0254/181/2012).
DNA extraction from paraffin sections
We used 5 × 10-μm sections of formalin-fixed, paraffin-embedded tissues from OSCC samples. DNA was extracted using a protocol as described in the DNeasy Tissue Kit Handbook (Qiagen GmBH, Hilden, Germany, cat. No 69506). Purified DNA was quantified by spectrophotometry (Epoch Microplate Spectrophotometr, BioTek Instruments Inc., Vinooski, Vermont USA).
EBV DNA detection
The nested PCR was carried out for detection of EBV DNA. The product size was 54 bp. The primer sequences are:
Outer
5′ – GTC ATC TAC GGG GAC ACG GA – 3′
5′ – AAG AAG AGA TAT GTG GGG GT – 3′
Inner
5′ – ACC CGG AGC CTG TTT GTG GC– 3′
5′ – GGA GAA GGT CTT CTC GGC CTC – 3′
All PCR reactions were carried out in the final volume of 25 μl using Taq PCR Core Kit (Qiagen, Hilden, Germany). Concentrations of PCR reaction components were prepared as follows: 2 mM MgCl2, 0.2 mM dNTPs, 0.2 μM of each forward and reverse primers and 0.5 U of Taq DNA polymerase. During each run the samples were tested together with one negative and one positive control. The negative control consisted of nuclease-free water, positive - EBV-positive cell line, Namalwa, ATCC-CRL-1432. The reaction mixture containing 5 μl of extracted DNA was amplified under the following conditions: 94 °C for 3 min of initial denaturation, then 35 cycles of 94 °C for 30 s, 55 °C for 40 s, 72 °C for 1 min with the final extension at 72 °C for 5 min. The second round amplification was performed with 1 μl of the outer product in the same conditions. The final PCR products were analysed on 3 % agarose gel.
HPV DNA detection; HPV detection and genotyping was performed using the INNO-LiPA HPV Genotyping Extraassay (Innogenetics N. V, Gent, Belgium; no cat. 81063) according to the manufacturer’s protocol. The kit is based on the amplification of a 65 bp fragment from the L1 region of the HPV genome. PCR products are subsequently typed with the reverse hybridization assay. The assay covers all currently known high-risk HPV genotypes and probable high-risk HPV genotypes (16, 18, 26, 31, 33, 35, 39, 45, 51, 52, 53, 56, 58, 59, 66, 68, 73, 82) as well as a number of low-risk HPV genotypes (6, 11, 40, 43, 44, 54, 70) and some additional types (69, 71, 74).
Statistical analysis
Statistical analysis was performed to investigate the relationship between EBV and HPV presence and clinical and demographical characteristics of patients were determined by means of Pearson’s chi-square test and with Fisher’s exact test for small groups. Statistical significance was defined as p < 0.05.
Results
Males (85.1 %) with, smoking (85.0 %) and alcohol abuse (64.3 %) problems prevailed in the studied group. The majority of the tumors in the examination group were classified as G2 (81.8 %). T4 (58.4 %) and N2 (50.0 %) traits occurred in the majority of patients. No cases of metastasis were observed (M0 100 %). Characteristics of the study group are shown in Table 1. In the Fig. 1 the prevalence of HPV, EBV and HPV/EBV co-infection were presented.
Table 1.
Epidemiological and clinical characteristics of patients
| Oropharynx | Oral cavity | Total | |||||
|---|---|---|---|---|---|---|---|
| N = 62 | % | N = 92 | % | N = 154 | % | ||
| Sex | female | 6 | 9.7 | 17 | 18.5 | 23 | 14.9 |
| male | 56 | 90.3 | 75 | 81.5 | 131 | 85.1 | |
| Age | 40–49 | 12 | 19.3 | 23 | 25.0 | 35 | 22.8 |
| 50–59 | 46 | 74.2 | 60 | 65.2 | 106 | 68.8 | |
| 70 + | 4 | 6.5 | 9 | 9.8 | 13 | 8.4 | |
| Place of residence | urban | 37 | 59.7 | 55 | 59.8 | 92 | 59.7 |
| rural | 25 | 40.3 | 37 | 40.2 | 62 | 40.3 | |
| Smoking | yes | 52 | 83.9 | 79 | 85.9 | 131 | 85.1 |
| no | 3 | 4.8 | 5 | 5.4 | 8 | 5.2 | |
| No answer | 7 | 11.3 | 8 | 8.7 | 15 | 9.7 | |
| Alkohol abuse | yes | 42 | 67,7 | 57 | 62.0 | 99 | 64.3 |
| No | 7 | 11.3 | 6 | 6.5 | 13 | 8.4 | |
| No answer | 13 | 21.0 | 29 | 31.5 | 42 | 27.3 | |
| Histology stage G | 1 | 2 | 3.2 | 12 | 13.0 | 14 | 9.1 |
| 2 | 50 | 80.6 | 76 | 82.6 | 126 | 81.8 | |
| 3 | 10 | 16.2 | 4 | 4.4 | 14 | 9.1 | |
| T stage | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| 2 | 2 | 3.3 | 31 | 33.7 | 33 | 21.4 | |
| 3 | 12 | 19.4 | 19 | 20.7 | 31 | 20.2 | |
| 4 | 48 | 77.4 | 42 | 45.6 | 90 | 58.4 | |
| N stage | No | 11 | 17.7 | 19 | 20.6 | 30 | 19.5 |
| N1 | 14 | 22.6 | 18 | 19.6 | 32 | 20.8 | |
| N2 | 35 | 56.5 | 42 | 45.7 | 77 | 50.0 | |
| N3 | 2 | 3.2 | 13 | 14.1 | 15 | 9.7 | |
| M stage | 0 | 62 | 100.0 | 92 | 100.0 | 154 | 100.0 |
| 1 | 0 | 0 | 0 | 0 | 0 | 0 | |
Fig. 1.
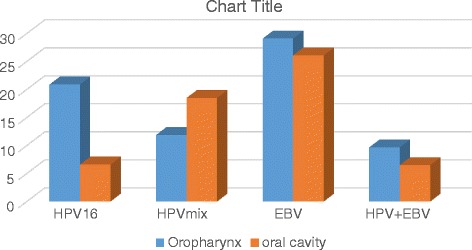
Prevalence of HPV, EBV and HPV/EBV coinfection in oropharyngeal and oral cavity cancer (%)
Of all 154 samples, 29.2 % (45/154) were HPV positive, 27.4 % (17/62) in oropharyngeal and 30.4 % (28/92) in oral cavity cancer. HPV type 16 was detected in 20.9 % (13/62) of oropharyngeal and in 12 % (11/92) of oral cancer. The HPV type 16 was detected in 53.3 % of HPV-positive group; in oropharyngeal more often (76.5 %) than in samples from the oral cavity (39.3 %). This difference is statistically significant (p < 0.01). Other mixed infections (more than one type of HPV i.e. 51, 52, 59, 66, 68, 71, 74) were detected in 23.5 and 60.7 % of the cases, respectively, and in 46.7 % of all HPV-positive samples.
Of all investigated samples, 27.3 % were positive for EBV, in oropharyngeal 29.1 % and in oral cavity 26.1 %. Co-infection HPV/ EBV was detected in 7.8 % (12/154), in oropharyngeal 9.7 % (6/62) and in the oral cavity 6.5 % (6/92). EBV and HPV 16 co-infection was detected in 6 cases i.e. 50.0 % of co-infected samples. There are no correlation between HPV or EBV infection and age and tobacco smoking (Table 2). Table 3 shows the prevalence of HPV and EBV in different histopathological grades and TN classification. Among HPV-positive patients G1 was diagnosed more often (15.6 %) than among HPV-negative ones (6.4 %), and G3 more often in HPV-negative. There is a statistically significant (p < 0.05).
Table 2.
HPV 16, HPV other and EBV by age and smoking
| Age | HPV 16 | HPV mix | EBV |
|---|---|---|---|
| N = 24 | N = 21 | N = 42 | |
| 40–49 | 8 (22.9 %) | 6 (17.1 %) | 5 (14.3 %) |
| N = 35 | |||
| 50–59 | 13 (12.3 %) | 15 (14.2 %) | 33 (31.4 %) |
| N = 106 | |||
| 70+ | 3 (23.1 %) | 0 | 4 (30.8 %) |
| N = 13 | |||
| p | >0.05 | >0.05 | >0.05 |
| Smoking | 20 (83.3 %) | 15 (71.4 %) | 32 (76.2 %) |
| Yes | |||
| N = 131 | |||
| No | 4 (16.7 %) | 6 (28.6 %) | 10 (23.8 %) |
| N = 23 | |||
| p | >0.05 | >0.05 | >0.05 |
Table 3.
Prevalence of HPV and EBV in different histopathological grades and TN classification
| HPV+ n = 45 | HPV- n = 109 | EBV+ n = 42 | EBV- n = 112 | p value | |
|---|---|---|---|---|---|
| G1 | 7 (15.6) | 7 (6.4) | 4 (9.5) | 10 (8.9) | >0.05 |
| n = 14 | |||||
| G2 | 37 (82.2) | 89 (81.7) | 34 (81.0) | 92 (82.2) | |
| n = 126 | |||||
| G3 | 1 (2.2) | 13 (11.9) | 4 (9.5) | 10 (8.9) | |
| n = 14 | |||||
| P | <0.05* | >0.05 | |||
| T1 | 0 | 0 | 0 | 0 | >0.05 |
| n = 0 | |||||
| T2 | 7 (15.6) | 26 (23.8) | 6 (14.3) | 27 (24.1) | |
| n = 33 | |||||
| T3 | 9 (20.0) | 22 (20.2) | 8 (19.0) | 24 (21.4) | |
| n = 31 | |||||
| T4 | 29 (64.4) | 60 (55.0) | 28 (66.7) | 61 (54.5) | |
| n = 89 | |||||
| p | >0.05 | >0.05 | |||
| No | 6 (13.3) | 24 (22.0) | 26 (61.9) | 4 (3.6) | >0.05 |
| n = 30 | |||||
| N1 | 6 (13.3) | 26 (23.9) | 7 (16.7) | 25 (22.3) | |
| n = 32 | |||||
| N2 | 25 (55.6) | 52 (47.7) | 7 (16.7) | 70 (62.5) | |
| n = 77 | |||||
| N3 | 8 (17.8) | 7 (6.4) | 2 (4.7) | 13 (11.6) | |
| n = 15 | |||||
| p | >0.05 | >0.05 | |||
*statistical significant
Discussion
The prevalence of HPV in squamous cell carcinoma of the oral and oropharynx is diverse and ranges from 8 to 74 % [21–24]. This is the first original observation about frequency of HPV and EBV in oral and oropharyngeal cancer among Polish patients. In our study HPV DNA was detected in 29.2 % of the tested samples (27.4 % - oropharynx; 30.4 % - oral cavity) and is lower than in Northern and Western Europe. Poland is located in East Europe, so prevalence of HPV be able to different than in other European countries. HPV infection is a sexually transmitted infection, so sexual behaviors can play a role.
Studies by Robinson et al. [25] did not reveal any association between the histological grade and HPV status in these tumours. Instead, Zhao et al [26] by multivariate analysis have found a correlation between HPV infection and poor histological grade (OR = 104.0, 95 % CI: 11.2–962.1). His study provides evidence that the presence of HPV predicted a better survival.
In the present study a significant relationship was found between the status of HPV and the poor histopathological grades (chi square, p < 0.05; Table 3). In most studies no association was found between HPV presence and TNM clinical stage [26]. Our results are similar.
Confirmation or exclusion of HPV DNA in OSCC influences prognosis and therapy choices. Some researchers state that OSCC patients who are HPV-positive have a more favorable treatment prognosis [20–22], higher survival rates and a lower risk of the disease recurrence in comparison to the HPV-negative patients [27]. Additionally, such patients do not require radio or chemotherapy afterwards [28], and according Khode [29] HPV-positive tumors are more sensitive to chemotherapy.
Although squamous cell carcinoma has been commonly believed to affect people above fifty, the newest data indicate that the age of people afflicted with this disease is constantly decreasing [30]. The study by Golusiński et al. [30] on the occurrence of this disease in people under 45 years of age indicates that these cases constitute up to 0.24–9.0 % of all cases, and that this problem is relatively new. These data show that oral and oropharynx cancers are common among people over 50; however, they also occur at a younger age (80.8 and 19.2 %, respectively) [31]. Among patients younger than 50 HPV 16 was detected more often (22.9 %) than in the group aged 50–59 (12.3 %). In patients 70 years and over was only 3 HPV positive cases (Table 2).
Smokers prevailed among patients infected both with HPV and EBV. It was found out that the largest number of smoking patients were in the group infected with HPV 16 virus (83.3 %; Table 2). Probably, there is a correlation between smoking and HPV 16 infection on the one hand and oropharyngeal squamous cell carcinoma, on the other [32]. Merne et al. [33] suggest a possible synergy between tobacco components and viral oncogenes, especially HPV16 E6/E7 in transformation of oral epithelial cells. Studies by Haukioja et al. [34] found out that smoking is a risk factor for a persistent oral HPV infection. On the other hand, persistent HPV infection in the oral mucosa might increase the risk of developing oral cancer [35].
A number of authors emphasize the role of EBV in the development of OSCC [14, 15, 20].
Zur Hausen drew attention as early as 1976 to the possibility of the involvement of EBV in human cancer [36]. Jaloluli et al. [18] observed the presence of EBV in 55 % of samples from 8 different countries. The frequency of occurrence of EBV virus varies in different populations. Opinions on the role of EBV in OSCC are different. Literature provides a wide range of preponderance for oral, pharynx and larynx viral infections. Nevertheless, the obtained research results suggest that the pathogenesis of oral squamous cell carcinoma is not directly connected with Herpesviridae infection in the oral cavity [37]. EBV DNA was detected in our research in 27.3 % of the cases (42/154), most often in the 50–59 years old group (31.4 %; Table 2). The frequency of EBV DNA in oropharyngeal cancer was slightly higher 29 % (18/62) compared with the oral cavity – 26.1 % (24/92) (Fig. 1). This low infection rate may result from the fact that formalin-fixed, paraffin-embedded tissues was examined.. The presence of the EBV is most likely connected with more aggressive types of oral tumors, particularly in groups of immunosuppressed patients [38]. Infection with EBV can be of importance since EBV is widespread in the human population (antibodies to EBV have approximately 95 % of adults). The infection may be asymptomatic and life-long [39]. According to Kis et al. [40], the prevalence of Epstein-Barr virus in OSCC patients is significantly higher than in the healthy group and higher than that in other mucosa pathologies such as oral leukoplakia and oral lichen planus (73.8, 19.1, 29.5 and 46.6 %, respectively).
Some authors find a connection between EBV infection (especially co-infection with papillomaviruses) and squamous cell carcinoma of the tongue and oropharyngeal sites [14, 17, 41]. In our study HPV-EBV co-infection was detected only in 7.8 % of samples (Fig. 1). This low percentage can not support that co-infection plays a role in OSCC. However, it cannot be completely exluded. Jalouli et al. [42] studied tissue samples obtained from patients with oral cancers and they showed that prevalence of HPV and EBV infections is common and may influence the oral cancer development. Co-infection by multiple oncogenic viruses may be an important risk factor in the development of OSCC [17, 43]. Jiang et al. [17] suggest that coinfected cells can have a higher tumorigenic potential than normal cells, and that co-infection of both HPV and EBV may have a more profound effect on invasion than proliferation.
The question remains whether in these cases we have to do with co-infection or superinfection. It is known that chronic virus infection affects the immunological answer of the host. Primary infection with non-oncogenic virus can favour superinfection with oncogenic virus capable of cancer transformation. The oncogenic potential of HPV is related to the expression of E6 and E7, the oncogenic potential of EBV – to the expression of LMP-1 and LMP-2. Toll-like receptors (TLRs) play a critical role in the early innate immune response to the invading pathogens by sensing a microorganism and they are involved in sensing endogenous danger signals [44, 45]. Fathallah et al [45] established that the EBV oncoprotein latent membrane protein 1 (LMP1) is a strong inhibitor of TLR9 transcription, which can favour the aforementioned superinfection. A limitation in our studies is a too small number of cases of EBV/HPV, coinfection, which makes the epidemiological analysis of this group of patients impossible.
In conclusion, the present study shows that in major patients from Southeastern region of Poland with oropharyngeal cancer HPV type 16 was detected but in oral cavity cancer other mixed infections were observed (i.e. 51, 52, 59, 66, 68, 71, 74). HPV 16 was detected more often among patients younger than 50 age of years, whereas the mixed HPV in the group aged 50–59. EBV may play a role in the development of OSCC. Future both epidemiological and studies on the mechanisms of co-infection and/or superinfection and their role in oral squamous cell carcinoma are necessary. The knowledge about these mechanisms may provide targets for therapy and for development of diagnostic methods.
Acknowledgements
This study was supported by a Research Grant from the Medical University, Lublin, Poland (DS 233).
We are thankful to prof. Wiesław Gołąbek (Chair and Department of Otolaryngology and Laryngological Oncology in Lublin 1998–2010) for his help in clinical material collection.
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contribution
DP-G: Conceived of the study, its design, data analysis, manuscript preparation; KM: Data and clinical samples collection; AS: Carried out the molecular identification; MP-D: Data analysis, coordination and helped to draft the manuscript, review; All authors read and approved the final manuscript.
Contributor Information
Dorota Polz-Gruszka, Email: dorota.polz@umlub.pl.
Kamal Morshed, Email: kamal1@op.pl.
Agnieszka Stec, Email: agnieszka.stec@umlub.pl.
Małgorzata Polz-Dacewicz, Email: m.polz@umlub.pl.
References
- 1.Didkowska J, Wojciechowska U, Zatoński Z. Cancer in Poland in 2011. Warsaw: Oncology Centre- Oncology Institute Maria Skłodowska- Curie; 2013. [Google Scholar]
- 2.Alibek K, Kakpenova A, Yeldar Baiken Y. Role of infectious agents in the carcinogenesis of brain and head and neck cancers. Infect Agent Cancer. 2013;8:7–16. doi: 10.1186/1750-9378-8-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Garbuglia AR. Human papillomavirus in head and neck cancer. Cancers. 2014;6:1705–26. doi: 10.3390/cancers6031705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.IARC . Cancer IARC, ed. Lyon, France: World Health Organization; 2007. Monographs on the evaluation of carcinogenic risks to humans; p. 670. [Google Scholar]
- 5.IARC . Monographs on the evaluation of carcinogenic risks to humans A review of human carcinogens. Biological agents. Lyon: World Health Organization; 2012. p. 255. [Google Scholar]
- 6.Syrjänen KJ, Syrjänen SM, Lamberg MA, Pyrhönen S. Human papillomavirus (HPV) involvement in squamous cell lesions of the oral cavity. Proc Finn Dent Soc. 1983;79:1–8. [PubMed] [Google Scholar]
- 7.Jalouli J, Ibrahim SO, Mehrotra R, Jalouli MM, Sapkota D, Larson PA, et al. Prevalence of viral (HPV, EBV, HSV) infections in oral submucous fibrosis and oral cancer from India. Acta Otolaryngol. 2010;130:1306–311. [DOI] [PubMed]
- 8.Syrjänen K, Syrjänen S. Detection of human papillomavirus in sinonasal carcinoma: systematic review and meta-analysis. Hum Pathol. 2013;44:983–91. doi: 10.1016/j.humpath.2012.08.017. [DOI] [PubMed] [Google Scholar]
- 9.Gillison M, Castellsague X, Chaturvedi A, Goodman M, Smijders P, Tommasino MA, et al. Comparative epidemiology of HPV infection and associated cancers of the head and neck and cervix. Int J Cancer. 2014;134:497–507. [DOI] [PubMed]
- 10.Peh SC, Kim LH, Mun KS, Tam EL, Sam CK, Poppema S. Epstein-Barr virus (EBV) subtypes and variants in malignant tissue from Malaysian patients. J Clin Exp Hematopathol. 2003;43:61–69. doi: 10.3960/jslrt.43.61. [DOI] [Google Scholar]
- 11.Alipov G, Nakayama T, Nakashima M, Wen ChY, Niino D, Kondo H, et al. Epstein-Barr virus-associated gastric carcinoma in Kazakhstan. World J Gastroenterol. 2005;11:27–30. [DOI] [PMC free article] [PubMed]
- 12.Proceedings of the IARC working group on the evaluation of carcinogenic risks to tumors. Epstein-Barr virus and Kaposi’s sarcoma Herpesvirus/Human herpesvirus 8. Lyon, France, 17–24 June 1997. IARC Monogr Eval Cacinog Risks Hum. 1997;70:1-492. [PMC free article] [PubMed]
- 13.Perera RA, Samaranayake LP, Tsang CSP. Shedding dynamics of Epstein-Barr virus: A type 1 carcinogen. Arch Oral Biol. 2010;55:639–47. doi: 10.1016/j.archoralbio.2010.06.009. [DOI] [PubMed] [Google Scholar]
- 14.Slots J, Saygun I, Sabeti M, Kubar A. Epstein-Barr virus in oral diseases. J Periodontal Res. 2006;41:235–44. doi: 10.1111/j.1600-0765.2006.00865.x. [DOI] [PubMed] [Google Scholar]
- 15.Chen MR. Epstein-Barr virus, the immune system, and associated diseases. Front Microbiol. 2011;2:5. doi: 10.3389/fmicb.2011.00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grinde B, Olsen I. The role of viruses in oral disease. J Oral Microbiol. 2010;12:2. doi: 10.3402/jom.v2i0.2127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jiang R, Ekshyyan O, Moore-Medlin T, Rong X, Nathan S, Gu X, et al. Association between human papilloma virus/Epstein-Barr virus co-infection and oral carcinogenesis. J Oral Pathol Med. 2015;44:28–36. [DOI] [PMC free article] [PubMed]
- 18.Jalouli J, Jalouli MM, Sapkota D, Ibrahim SO, Larron PA, Sand L. Human papillomavirus, herpes simplex virus and Epstein-Barr virus in oral squamous cell carcinomas from eight different countries. Anticancer Res. 2012;32:571–80. [PubMed] [Google Scholar]
- 19.Sobin LH, Gospodarowicz M, Wittekind C, editors. TNM classification of malignant tumours 7th edition. Washington DC: Wiley-Blackwell; 2009. [Google Scholar]
- 20.Cardesa A, Gale N, Nadal A, Zidor N. Squamous cell carcinoma in World Heath Organization Classifiation of Tumours. Pathology and Genetics: Head and Neck Tumours. Barnes L, Eveson JW, Reichart P, Sidnousky (eds.) Lyon, International Agency for Research on Cancer, 2010; 118-121.
- 21.Castro Peixoto Patury Galvao T, Busolotti I. Prevalance of Human papillomavirus (HPV) in oral and oropharynx. Rev Bras Otorrinolaringol. 2006;2:1–14. [Google Scholar]
- 22.Ritchie JM, Smith EM, Summersgill KF, Hoffman HT, Wang D, Klussmann JP, et al. Human papillomavirus infection as a prognostic factor in carcinomas of the oral cavity and oropharynx. Int J Cancer. 2003;104:336–44. [DOI] [PubMed]
- 23.Wang D, Ritchie JM, Smith EM, Zhang Z, Turek LP, Haugen TH. Alcohol dehydrogenase 3 and risk of squamous cell carcinoma of the head and neck. Cancer Epidemiol Biomarkers Prev. 2005;14:626–33. doi: 10.1158/1055-9965.EPI-04-0343. [DOI] [PubMed] [Google Scholar]
- 24.Sathish N, Wang X, Yuan Y. Human Papillomavirus (HPV)-associated oral cancers and treatment strategies. J Dent Res. 2014;93:29S–36S. doi: 10.1177/0022034514527969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Robinson M, Suh Y, Paleri V, Devlin D, Ayaz B, Pertl L, et al. Oncogenic human papillomavirus-associated nasopharyngeal carcinoma: an observational study of correlation with ethnicity, histological subtype and outcome in a UK population. Infect Agent Cancer. 2013;8:30. [DOI] [PMC free article] [PubMed]
- 26.Zhao D, Xu Q, Chen X, Fan M. Human Papillomavirus as an Independent Predictor in Oral Squamous Cell Cancer. Int J Oral Sci. 2009;1:119–125. doi: 10.4248/IJOS.09015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mirghani H, Amen F, Moreau F, Guigay J, Ferchion M, Melkane AE, et al. Human papillomavirus testing in oropharyngeal squamous cell carcinoma: What the clinician should know. Oral Oncol. 2014;50:1–9. [DOI] [PubMed]
- 28.Benson E, Li R, Eisele D, Fakhry C. The clinical impact of HPV tumor status upon head and neck squamous cell carcinoma. Oral Oncol. 2014;50:565–74. doi: 10.1016/j.oraloncology.2013.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Khode SR, Dwivedi RC, Rhys-Evans P, Kazi R. Exploring the link between human papilloma virus and oral and oropharyngeal cancers. J Cancer Res Ther. 2014;10:492–98. doi: 10.4103/0973-1482.138213. [DOI] [PubMed] [Google Scholar]
- 30.Golusiński W, Waśniewska E, Kaczmarek J, Kędzia D, Wróbel M, Malinowska B. Patients under 45 years of age “young adults” with head and neck squamous cell carcinoma. Retrospective, multivariable analysis--preliminary report. Otolaryngol Pol. 2003;57:185–9. [PubMed] [Google Scholar]
- 31.Wojciechowska U, Didkowska J, Zatoński W. Cancer in Poland in 2003. Warsaw, Poland: Oncology Centre- Oncology Institute Maria Skłodowska- Curie; 2005. [Google Scholar]
- 32.Chakrobarty B, Roy JG, Majumdar S, Uppala D. Relationship among tobacco habits, human papilloma virus (HPV) infection, p53 polymorphism/mutation and the risk of oral squamous cell carcinoma. J Oral Maxillofac Pathol. 2014;18:211–6. doi: 10.4103/0973-029X.140752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Merne M, Rautava J, Ruutu M, Syrjanen S. Smokeless tobacco increases aneuploidy in oral HPV16E6/E7-transformed keratinocytes in vitro. J Oral Pathol Med. 2014;43:685–90. doi: 10.1111/jop.12185. [DOI] [PubMed] [Google Scholar]
- 34.Haukioja A, Asunta M, Söderling E, Syrjänen S. Persistent oral human papillomavirus infection is associated with smoking and elevated salivary immunoglobulin G concentration. J Clin Virol. 2014;61:101–6. doi: 10.1016/j.jcv.2014.06.012. [DOI] [PubMed] [Google Scholar]
- 35.Rautava J, Syrjänen S. Human papillomavirus infections in the oral mucosa. J Am Dent Assoc. 2011;142:905–14. doi: 10.14219/jada.archive.2011.0297. [DOI] [PubMed] [Google Scholar]
- 36.Hausen Z. Biochemical approaches to detection of Epstein-Barr virus in human cancer. Cancer Res. 1976;26:678–80. [PubMed] [Google Scholar]
- 37.Saravani S, Miri-Moghaddam E, Sanadgol N, Kadeh H, Nazeri MR. Human herpesvirus-6 and Epstein-Barr virus infections at different histopathological grades of oral squamous cell carcinomas. Int J Prev Med. 2014;5:1231–8. [PMC free article] [PubMed] [Google Scholar]
- 38.Slots J. Herpesviruses in periodontal diseases. Periodontol 2000. 2005;38:33–62. doi: 10.1111/j.1600-0757.2005.00109.x. [DOI] [PubMed] [Google Scholar]
- 39.Shah KM, Young LS. Epstein-Barr virus and carcinogenesis: beyond Burkitt’s lymphoma. Clin Microbiol Infect. 2009;15:982–88. doi: 10.1111/j.1469-0691.2009.03033.x. [DOI] [PubMed] [Google Scholar]
- 40.Kis A, Feher E, Gall T, Tar I, Boda R, Toth ED, et al. Epstein-Barr virus prevalence in oral squamous cell cancer and potentially malignant oral disorders in an eastern Hungarian population. Eur J Oral Sci. 2009;117:537–40. [DOI] [PubMed]
- 41.Goldenberg D, Benoit NE, Begun S, et al. Epstein-Barr virus in head and neck cancer assessed by quantitative polymerase chain reaction. Laryngoscope. 2004;114:1027–31. doi: 10.1097/00005537-200406000-00013. [DOI] [PubMed] [Google Scholar]
- 42.Jalouli J, Ibrahim SO, Sapkota D, Jalouli MM, Vasstrand EN, Horsch JM, et al. Presence of human papilloma virus, herpes simplex virus and Epstein-Barr virus DNA in oral biopsies from Sudanese patients with regard to toombak use. J Oral Pathol Med. 2011;19:599–604. [DOI] [PubMed]
- 43.Al Moustafa AE, Chen D, Ghabreau L, Akil N. Association between human papillomavirus and Epstein-Barr virus infections in human oral carcinogenesis. Med Hypotheses. 2009;73:184–6. doi: 10.1016/j.mehy.2009.02.025. [DOI] [PubMed] [Google Scholar]
- 44.Hasan UA, Bates E, Takeshita F, Biliato A, Accardi R, Bouvard V, et al. TLR9 expression and function is abolished by the cervical cancer-associated human papillomavirus type 16. J Immunol. 2007;178:3186–97. [DOI] [PubMed]
- 45.Fathallah I, Parroche P, Gruffat H, Zannetti C, Johansson H, Yue J, et al. EBV latent membrane protein 1 is a negative regulator of TLR9. J Immunol. 2010;185:6439–47. [DOI] [PubMed]


