Abstract
Glaucoma involves a characteristic optic neuropathy, often with elevated intraocular pressure. Before 1850, poor vision with a normal eye appearance, as occurs in primary open-angle glaucoma, was termed amaurosis, gutta serena, or black cataract. Few observers noted palpable hardness of the eye in amaurosis. On the other hand, angle-closure glaucoma can produce a green or gray pupil, and therefore was called, variously, glaucoma (derived from the Greek for glaucous, a nonspecific term connoting blue, green, or light gray) and viriditate oculi. Angle closure, with palpable hardness of the eye, mydriasis, and anterior prominence of the lens, was described in greater detail in the 18th and 19th centuries. The introduction of the ophthalmoscope in 1850 permitted the visualization of the excavated optic neuropathy in eyes with a normal or with a dilated greenish-gray pupil. Physicians developed a better appreciation of the role of intraocular pressure in both conditions, which became subsumed under the rubric “glaucoma”.
Keywords: glaucoma, history of ophthalmology, open-angle glaucoma, angle-closure glaucoma
Introduction
The early history of glaucoma has been described as mysterious and controversial.1–3 The term “glaucoma” is derived from the ancient Greek glaukos (γλαυκóς), a nonspecific term connoting blue, green, or light gray.4 Although glaukos and related terms described the color of the pupil, there is some controversy regarding which of these colors was intended. In the modern era, glaucoma implies nothing about the pupillary color. Rather, glaucoma encompasses a group of disorders with an excavated optic neuropathy, often associated with elevated intraocular pressure. How the meaning of the term evolved is poorly understood.
Our earlier work analyzed ancient color terms relative to the eye.4 In the present work, we discuss the evolution of glaucoma descriptions from antiquity through the 19th century (Table 1). We searched historical texts for findings consistent with glaucoma. As an optic neuropathy, glaucoma eventually produces 1) loss of vision, 2) visual field defects, and 3) difficulty in cure. As intraocular pressure is often elevated in glaucoma, astute observers might have noted 4) ocular discomfort and 5) a tense or palpably hard eye.
Table 1.
Chronological summary of major developments in glaucoma nomenclature before the 20th century.
| YEAR | GLAUCOMA WITH A NORMAL APPEARING EYE (SUCH AS PRIMARY OPEN-ANGLE GLAUCOMA) | GLAUCOMA WITH AN ABNORMAL EYE APPEARANCE (AS IN ACUTE ANGLE-CLOSURE GLAUCOMA) |
|---|---|---|
| 8th century BC | Though glaukos described light-colored eyes (blue, green, or gray), which were healthy, glaukos carried negative connotations as these eye colors were a minority in ancient Greece | |
| 4th century BC | Glaukos sometimes described diseased eyes with a lighter pupil (from cataract or other causes). The condition was incurable because couching was not known | |
| Early Common Era | Amaurosis (severe) and amblyopia (mild) described vision impairment with a normal-appearing eye | A dilated pupil (mydriasis), inflamed eye (ophthalmia), and discolored pupil (glaukos) were all noted as separate conditions. Couching of cataracts was described. The negative connotations of glaukos were entrenched enough that glaukos was retained to describe eye disorders that did not respond to couching. The glaukos hue was hypothesized to result from a large, hard, or anteriorly prominent crystalline lens |
| Medieval Arabic Period (800–1050 AD) | Glaukos was translated into Arabic as zarqaa, which also described both healthy light-colored eyes and (for diseased eyes) a lighter pupil due to a large, hard, or anteriorly prominent crystalline lens | |
| Latin works of the Middle Ages (12th–16th centuries) | Loss of vision with a normal-appearing eye was termed gutta serena | The unfavorable pupillary hue was more specifically described as green (viriditas), and was still believed due to a hard or anteriorly prominent lens |
| Renaissance developments (16th–17th centuries AD) | Banister described a palpably hard eye in gutta serena or black cataract | The lens was understood to be normally located anteriorly and capable of causing visual disorders by pressing against the iris. Lens disorders that did not improve with couching could produce a green pupil and a hard eye |
| More complete descriptions of angle-closure glaucoma (1707–1849) | Amaurosis was only rarely stated to involve a palpably hard eye | Mydriasis, ophthalmia, and a green pupil were integrated into one syndrome, often called glaucoma and noted to involve a palpably hard eye. Authors agreed on the clinical findings, but could not agree on whether glaucoma was due to a disorder of the lens, or more posterior structures (eg, vitreous or choroid) |
| The era of the ophthalmoscope (after 1850) | An excavated optic neuropathy was observed, often associated with elevated intraocular pressure in quiet eyes with a normal pupil and in inflamed eyes with a dilated (and sometimes green or gray) pupil. Both conditions became known as “glaucoma” | |
Glaucoma with a normal-appearing eye before 1850
Today, at-risk populations undergo screening for glaucoma because the condition can develop without changes in eye appearance or any specific symptoms. The most common variety is primary open-angle glaucoma, with a prevalence of 1.9% in adults over the age of 40.5 Some other types of glaucoma, such as chronic angle-closure glaucoma, might also develop insidiously.
In antiquity, glaucoma patients with a normal-appearing eye would typically have been asymptomatic until progressing to visual field defects or loss of central vision. Vision loss with a normal-appearing eye was termed amblyopia (άµβλυωπας)6,7 if mild, and amaurosis (άµαυρώσεως)7 if severe. Amaurosis was believed to be due to a blockage of the optic nerve.7
Of course, numerous conditions could present without a change in eye appearance. Thus, amblyopia and amaurosis would have described not only primary open-angle glaucoma but also optic neuritis, nutritional or traumatic optic neuropathies, retinal detachment, macular diseases, and other conditions.
Acute elevations of intraocular pressure often are accompanied by ocular pain. Experienced clinicians have also noted an aching pain in or around the eye in patients with chronic open-angle glaucoma, but such symptoms are common and nonspecific. Some authorities have stated that patients with open-angle glaucoma do not have headache or eye pain.8 On the other hand, the weight of evidence from modern epidemiologic studies does suggest a higher prevalence of headache in patients with open-angle glaucoma.9
The proportion of such patients experiencing periocular discomfort might have been even higher in ancient populations lacking effective therapies. Interestingly, the 6th century Byzantine author Aetius of Amida noted that amaurosis could follow trauma, but when it occurred without any obvious cause, “so must a necessary feeling (sensation) follow of heaviness [βάρος, baros] of the head, especially deep at the root of the eye.”7 Moreover, for some with amaurosis, the “vision is obstructed through much pressure [θλĩψις, thlipsis] or thick exudates applied on the optic nerve”.7
The ancient Greek texts were translated into medieval Arabic.4 The term gutta serena appeared as a synonym for amaurosis when the Arabic texts were translated into Latin during the Middle Ages. For instance, the 12th or 13th century oculist Benevenutus Grassus used the term gutta serena to describe one type of incurable blindness in which ‘the Nerves optic be oppilate [obstructed] and mortified’.9
The French surgeon Jacques Guillemeau (1550–1613) cited Aetius when describing amaurosis:
“Of the stopping of the sinew of sight, in Greek amaurosis, in Latin…gutta saerena: Amaurosis most commonly is a hindrance of the whole sight, without any appearance thereof in the eye: for the apple [pupil] of the eye remaineth sound, and unchanged… The causes of this which commeth by little and little are like to that malady which is called in Greek amblyopia… Before this effect do plainly appear the party perceiveth great heaviness in his head, specially in the root and bottom of the eyes.”10
The English oculist Richard Banister (1570–1626) was one of the few pre-ophthalmoscopic observers to report palpable hardness of the normal-appearing eye. Banister cited a translation of Grassus, and followed his example in using the term gutta serena, rather than glaucoma. Banister used the term “black cataract” as a synonym for gutta serena, and stated that it was not a true cataract because it did not involve an opacity in the visual axis. The gutta serena involves “stopping of the Nerve Optics” and is not likely to be cured if
“First, if it be of long continuance. Secondly, if they see no light at all. Thirdly, if one feel the Eye by rubbing upon the Eyelids, that the Eye be grown more solid and hard, then naturally it should be. Fourthly, if one perceive no dilatation of the Pupilla, then there is no hope of a Cure.”11
Even after Banister, it is difficult to find explicit descriptions of palpably hard but normal-appearing eyes. In 1836, a summary of the writings of the Viennese ophthalmologist Georg Josef Beer (1763–1821) noted:
“This form of amaurosis is described by Beer as having two stages… The first stage commences with a peculiar sensation of fulness in the eyeball…and a remarkable weakness of sight…without the slightest defect perceptible either in the eye itself, or its surrounding parts… Upon the advance of the disorder into its second stage the headache becomes irregular…as if the dimensions of the eye were increased, and, indeed, it really feels harder than in the healthy state.”12
The rarity of such statements suggests that before the invention of the ophthalmoscope, palpable hardness of the eye was not a cardinal sign of amaurosis. In English, the terms “amblyopia” and “amaurosis” continued with their ancient meanings well into the 19th century.13
Glaucoma with an abnormal eye appearance before 1850
Some types of glaucoma do alter the eye appearance in ways that could have been noted in antiquity. Inflammation might produce conjunctival injection. Acute elevations in intraocular pressure might produce corneal edema, which in glaucoma is classically felt to produce rainbow-colored haloes around lights. Ischemia can produce iris atrophy. As the eye becomes phthisical (from glaucoma or other causes), the cornea may have pannus or band keratopathy. Such cases of glaucoma could include angle-closure glaucoma, angle-recession glaucoma, neovascular glaucoma, ghost-cell glaucoma, iridocorneal endothelial syndrome, and many other types. Recent historians have tended to discuss these entities as “acute glaucoma.” A sudden elevation in intraocular pressure does produce these signs and symptoms. However, the term “acute” is somewhat misleading, because in the era before adequate treatment, the eye appearance was chronically altered. Ophthalmologists historically have recognized chronic and persistent changes from these types of glaucoma. Moreover, the nonspecific term “acute glaucoma” does not adequately convey the importance of angle closure in the etiology of the disorders termed “glaucoma” during this time period. Particularly since the early 18th century, the literature contains descriptions consistent with angle closure, including mydriasis and an anteriorly prominent lens. Today, angle closure does not always produce permanent visual loss, especially if treatment can be rapidly instituted. However, in the era before effective treatments, angle closure significant enough to alter the appearance of the eye would likely produce permanent optic nerve damage and vision loss.
If historical epidemiologic patterns resembled those in the modern era, one would expect angle-closure glaucoma to be predominant among the types of glaucoma that altered the eye appearance. Angle-closure glaucoma affects 0.4% of those with European ancestry over the age of 40, with higher prevalence rates in Asia.14 Therefore, we can search historical descriptions for findings often seen in angle-closure glaucoma15: 1) a dilated, fixed, or irregular pupil, 2) a swollen or anteriorly prominent lens with a narrow anterior chamber, 3) a green pupil, and 4) a name suggesting a green pupil (eg, glaucoma or viriditate oculi).
Angle-closure glaucoma can occur as a result of pupillary block (which responds to iridectomy), lens swelling that closes the angle by displacing the iris anteriorly (ie, phacomorphic glaucoma, which responds to lensectomy), and posterior pathology, which displaces the lens and iris anteriorly (ie, malignant glaucoma or aqueous misdirection).16,17 We meant to include historical descriptions consistent with all of these types of angle-closure glaucoma because all of them might involve the clinical characteristics listed above.
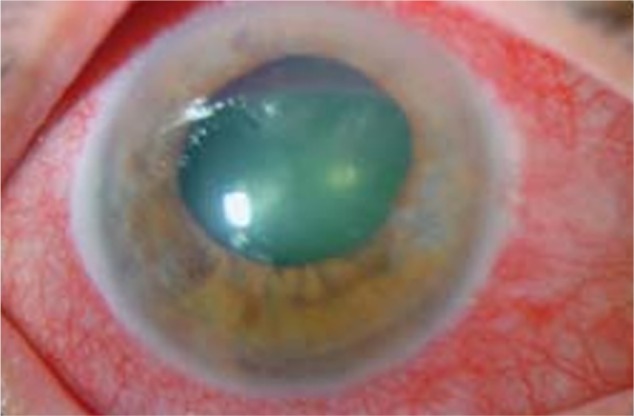
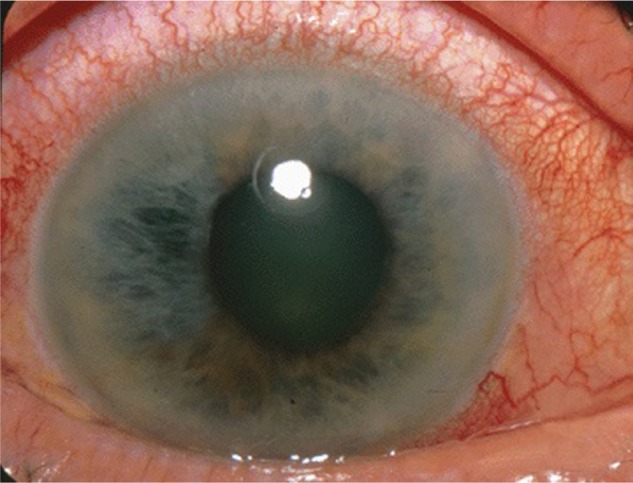
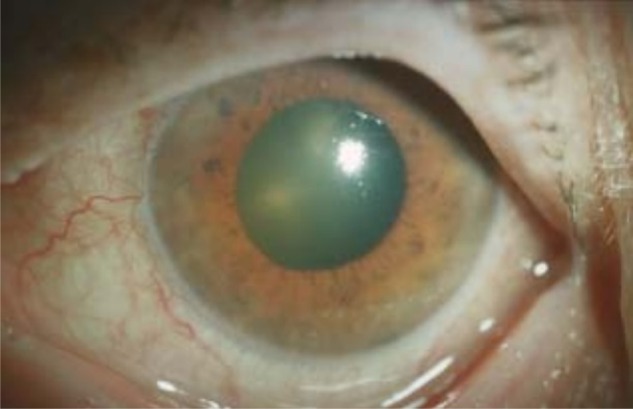
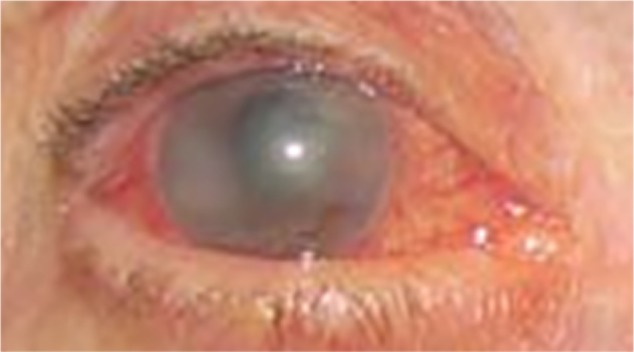
Although a green pupillary hue is not emphasized in modern ophthalmic training, the pupil in angle-closure glaucoma may appear green, as seen in representative photographs (Figs. 1–6).4,18–33 This finding is not universal. For instance, another glaucous color, gray, is sometimes the predominant pupillary hue (Fig. 7). Before the 20th century, the pupil in glaucoma was repeatedly described as green. It has been hypothesized that examination by candlelight or daylight instead of the ophthalmoscope might have produced the green pupillary hue.34 Although the type and direction of lighting and viewing have not been systematically studied, standard photographs can reveal the greenish hue in some cases of angle-closure glaucoma. An alternative explanation for the green pupil involves deposition of “blood pigments” in the lens epithelium following intraocular hemorrhage.35 As shown in the following, for centuries physicians have been astute enough to observe mydriasis and an anteriorly prominent lens. The hyphema hypothesis could be supported by the identification of historical descriptions of a green pupil with hyphema in the absence of mydriasis or an anteriorly prominent lens. Moreover, as described in the following, historical descriptions noted the green color coming from deep within the pupil, while photographs of eyes with neovascularization have dense cataracts in which only the anterior surface can be seen.35
Figure 1.

A green mid-dilated pupil and an intraocular pressure of 50 mmHg, seen in bilateral angle-closure glaucoma and choroiditis due to Hodgkin lymphoma in a 27-year-old male. Courtesy of Wolters Kluwer Health (Baillif et al, 2011).18 Promotional and commercial use of the material in print, digital or mobile device format is prohibited without the permission of the publisher Wolters Klower Health.
Figure 2.
A green, dilated pupil in acute angle-closure glaucoma. No fluorescein was instilled before the photograph. Courtesy of and personal communication (2014) Paulo Pierre-Filho, MD.
Figure 3.

A green, fixed, mid-dilated left pupil in a 70-year-old woman with 3 days of left eye pain and a left afferent pupillary defect. Visual acuity was hand motions in the left eye. The left eye had an intraocular pressure of 46 mmHg, and a narrow anterior chamber angle by gonioscopy. The diagnosis of acute angle-closure glaucoma was made. Medical treatment ended the attack. Cataract surgery of the left eye was performed. No fluorescein was instilled before the photograph.
Figure 4.
A grayish-green, mid-dilated pupil in acute angle-closure glaucoma. Courtesy of Jonathan Trobe, MD, and the University of Michigan Kellogg Eye Center.
Figure 5.
A green, dilated pupil in a 70-year-old woman with acute angle-closure glaucoma and an intraocular pressure of 62 mmHg, secondary to intraocular hemorrhage from macular degeneration while on anticoagulants. Courtesy of Springer Science and Business Media (Schlote et al, 2005).20
Figure 6.
A greenish-gray, dilated pupil due to acute angle-closure attack in the right eye with an intraocular pressure over 70 mmHg. Courtesy of Andrew Doan, MD, PhD.
Figure 7.

A gray pupil is seen in some instances of angle-closure glaucoma. A 54-year-old male with 2 days of right eye pain. The right eye intraocular pressure was 60 mmHg. The visual acuity in the right eye was hand motions, and had been poor for 1 year. The right pupil was fixed and dilated. The attack ended following medical treatment and iridotomy of the right eye. Right eye cataract surgery was performed. The examiner is holding the eyelids open during the photograph. No fluorescein was instilled before the photograph.
Though present-day observers have debated the cause of the green pupil, we will show that 19th century observers offered a simple explanation: the mydriasis permits viewing of the lens, which has at least some degree of nuclear sclerosis in most middle-aged patients. Other factors such as corneal edema or glaukomflecken may also modify the appearance.
Antiquity
Some of the individual signs and symptoms of angle-closure glaucoma were recognized in antiquity. Individual physicians might have used a variety of terms to describe the disorder. Physicians who focused on the pain and injection might have described it as ophthalmia (οφθαλµíα).36 The mid-dilated pupil might have been described as mydriasis (µυδριάσεως).7 Physicians who focused on the green or gray color of the pupil might have described it as glaukos, or a related term. The Roman encyclopedist Cornelius Celsus (c. 25 BC–50 AD) noted pain, an altered pupillary shape, and a glaucous hue as poor prognostic indicators, but these were separate findings rather than a single ophthalmic condition.4
The interpretation of the pupillary hue described as glaukos by the ancient Greeks has been somewhat controversial. Some historians have argued that glaukos must have been blue, though it is not clear what type of pathology would have produced this hue. Other historians have argued that glaukos must have represented either gray or green. Our recent review shows that glaukos probably represented all three colors: blue, gray, or green.4 More generally, in many societies, it is common for one color term to represent all three of these hues.4,37 The now infrequently used English term “glaucous” encompasses the same hues.
Glaukos was most commonly used in ancient Greece to describe healthy light-colored eyes (blue, green, or light gray), beginning with the works of Homer (c. 800 BC). Of 63 authors identified by Maxwell-Stuart38 who used glaukos or a related term in prose, 45 (71%) used the term to describe eyes.4 Usually this hue did not imply ophthalmic disease: 39 authors (87%) described simply healthy, light-colored eyes. As such eyes were a minority among Mediterranean peoples, the glaukos eye carried connotations which might have been considered negative at the time, such as cowardice, greed, violence, thievery, and even homosexuality.38
The way the term glaukos suggested an eye color might be compared to the way the English term “blond” suggests hair color. Just as “blond” suggests a range of hues, and does not correspond with the yellow color of the rainbow, glaukos likely represented a range of light eye colors.
Color terms used for other objects are not always applied to the eye. For instance, the terms for the green of leafy vegetation in ancient Greek (kloros and prasinos) and Latin (viridis) were not used to describe eye color in the classical period.4
Ancient and medieval authors characterized eye disorders based on the color of the pupil. The ancient Greeks sometimes described diseased pupils as glaukos, or related terms such as glaucoma. In the writings of at least 13 of 63 prose authors (21%), beginning with Hippocrates (c. 460–c. 370 BC), the glaucous hue implied disease.4,38 As we discuss in the following, Hippocrates’ belief that disease resulted from an imbalance of bodily fluids (humors) might ultimately have influenced the understanding of the glaukos hue. Because white cataracts have always been a frequent cause of a lighter pupil, and can be seen even with an undilated pupil, many eyes with a pupil described as glaukos during the Hippocratic period probably suffered from cataract. Less commonly, the term might have described a corneal opacity.4
The philosopher Aristotle (383–322 BC) noted that shallow water appears lighter in color than deep water. He theorized that the smaller eyes of newborns had a lighter glaucous hue due to the eye being small, and that elderly eyes with the pathologic glaucous hue suffered from dryness related to age.4
In the early Common Era, detailed descriptions of the crystalline lens and of couching to displace cataracts appeared in the area surrounding the Mediterranean Sea. Authors incorrectly believed that couching displaced a pathologic substance (termed a “hypochyma” or “suffusion”) anterior to the lens, rather than the opacified lens itself. These authors believed that the crystalline lens was the essential photoreceptive organ, as we view the retina today.
From the writings of Celsus and Demosthenes Philalethes (both early 1st Century AD), we see that the glaucous hue became associated with surgical incurability of the hypochyma even before the glaucous hue was associated with an incurable change in the crystalline lens.4 Thus, the glaukos hue might have initially acquired the connotation as incurable before the Common Era simply because the term preceded the cure (couching). By the time couching became more widely available at the start of the Common Era, the term glaukos already had such a negative connotation that it was retained for the incurable cases, while new terms were invented (hypochyma and suffusio) for the curable cases.
Rufus of Ephesus (80–150 AD) made the natural suggestion that the glaukos hue originated with disease of the crystalline lens – specifically excess moisture of the lens.4 After all, disease of the essential organ of vision (the lens) ought not be cured by a procedure to mechanically displace anterior opacities from the visual axis.
The preeminent medical author of this era was Galen of Pergamon (c. 129–199 AD). His description of the pathologic glaukos hue might be deemed a logical synthesis of his predecessors. Like all of them, he believed the glaukos hue implied incurability. Aristotle had stated that the glaucous hue resulted from shallow water (inadequacy of the aqueous layer). Rufus had identified the crystalline lens as the diseased layer. Hippocrates’ view that disease resulted from an imbalance of bodily humors allowed Galen to reconcile these beliefs: the glaucous hue resulted from a relative deficiency of aqueous or an excessively thick or anteriorly prominent crystalline humor (lens). Because an absence of aqueous would be expected to dry the lens, and dried substances often get harder, Galen noted that coagulation (πῆξις, pexis) or hardening (σκληρóτερον, scleroteron) of the lens could produce the glaucous hue.4 Thus, through a sequence of logical deductions proceeding from incorrect theoretical assumptions by his predecessors, Galen ended by describing an incurable glaucous hue resulting from a shallow anterior chamber or a harder and anteriorly prominent lens. Perhaps by chance, this description is remarkably consistent with angle-closure glaucoma. As we discuss in the following, very clear descriptions of the anteriorly prominent lens and narrow anterior chamber in angle-closure glaucoma precede the development of gonioscopy, slit lamp biomicroscopy, and cross-sectional imaging by centuries. Whether Galen and other ancient authors actually observed the shallow anterior chamber, or whether this derivation was entirely theoretical, may never be known with certainty.
The Arabic Middle Ages
Subsequent Arabic authors translated glaukos as zarqaa, which also typically described light-colored eyes. Abu Ali al-Husain Ibn Sina (c. 980–1037 AD), a Persian known later as Avicenna, believed the zarqaa pupillary hue could be associated with anterior prominence of the lens and could occur in an acquired (pathologic) manner. Today, the meaning of the term zarqaa has evolved to represent the basic Arabic term for blue, and so glaucoma is colloquially referred to as “blue water” in Arabic.4
Running in parallel with descriptions of the zarqaa hue in the Arabic literature were descriptions of “migraine of the eye” (shaqiqat al-ayn), a term that dates from the 10th century.4,39 This condition was described by Muhammad ibn Ibrahim Ibn al-Akfani (c. 1286–1348 AD), who died in Cairo, in his treatise “The Discovery of Impurities in Ocular Diseases” (Kashf Al-Rayn Fi Ahwal Al-Ayn).39 (The ophthalmic historian Hirschberg describes al-Akfani as Shams Al-Din.) In this treatise, the condition was also known as “headache of the pupil” (suda’ al-hadaqah). The condition involved deep eye pain, described as a burning or pressure sensation, opacification of the ocular fluids, and sometimes a cataract or dilated pupil.39 This disease definition might have included many cases of angle-closure glaucoma, but we are not aware of direct continuity between this teaching and subsequent European writings.
The green eye in the European Middle Ages
The Arabic works describing the zarqaa pupillary hue were cited in or translated into Latin in medieval Europe. For the most part, these works do not clarify the understanding of this hue, which generally implied incurability and was interpreted as resulting from a thick, anteriorly prominent, or hard crystalline lens. However, instead of nonspecific terms representing “glaucous” hues, the pupil was explicitly described as green (viriditas).
The treatise of Benevenutus Grassus, an oculist in the 12th or 13th century, influenced clinicians for 500 years.9 Grassus described an incurable green (viriditas)40 cataract, occurring suddenly with tearing, and with the eye “bleared”, sometimes following eye pain.41 Given his clinical experience, Grassus’ description of the green (viriditas) pupil in this incurable condition was probably based on his own observations. Grassus noted a separate type of incurable cataract associated with a dilated iris.41
The translation of Avicenna’s Canon in the 12th century42,43 attributed the green eye (viriditate oculi) to a lens that was larger and “nearer to the outer parts”, ie, more anterior.44 The nonspecific zarqaa was translated as viriditate (green). Did this translation result from the blue-green ambiguity present in many languages, or was the translation influenced by observations by oculists such as Grassus? The answer is not known. Jacques Guillemeau (1550–1613) of France9 cited Avicenna and wrote that glaucoma, or viriditas oculi, was incurable, and involved a dry, thick, and green lens.9,45
The French surgeon Jean Riolan the elder (1538–1605) noted that in glaucoma vision was poor, and the lens was gray, with an admixture of white and green, and a surface that was hard [induratur]. Moreover, “Under glaucoma everything is seen by us obscurely, and as if through shade: light is not seen, which occurrence distinguishes it from a cataract [suffusio].”46 Jean Riolan the younger (1580–1657) wrote: “The thickness and hardness of the Chrystallin Humor is properly termed Glaucosis or Glaucoma.”47
Advances in the Renaissance
Two major advances in descriptions consistent with angle-closure glaucoma occurred during the Renaissance. First, the medieval belief that the lens was in the center of the eye was replaced by the correct understanding of the more anterior lens position. The Swiss physician Felix Platter (1536–1614) published anatomic diagrams with the lens anteriorly in 1583.48 Platter wrote that the anterior lens might impair vision by contacting the iris:
“The faults of the grapy Membrane [uvea] hurt the sight, when its hole [the pupil]…is Contracted, or Dilated;… from the proper humors of the Eye the Crystalline [lens] and glassy [vitreous] falling into it…and from the too great largness of the Apple [pupil].”49
Second, the eye as a whole, as opposed to just the lens, was described as palpably hard. As noted above, Richard Banister is well known for his 1622 account of hardness of the eye in gutta serena or “black cataract.”50,51 Less attention has been given to his description of green “cataracts”. After introducing “imperfect cataracts” of the color “Black, Green, Yellow, and White”, Banister explains that the “black Cataract” actually has no anterior opacity, and that
“For the other three imperfect, and uncurable Cataracts [green, yellow, and white], as the humour predominateth, that is the cause of them, so is the colour: yet all have the Nerves stopped, alteration of the colour of the Cristaline humour with a durosity or hardnesse of the whole Eye, and privation of sight.”11
As discussed in the previous section on amaurosis, Banister surmised correctly, as did the ancients, that the nerve damaged in blinding conditions is the optic nerve. Thus, Banister associated a green lens with a hard eye and an optic neuropathy.
The 18th century
Relevant case descriptions and definitions became more complete in the 18th century. The ancient concepts of mydriasis, ophthalmia, and the lighter pupil were merged into one integrated eye disorder. Mydriasis and the anteriorly prominent lens pressing on the iris were repeatedly described. Other clinical features included pain and visual field defects. Couching, while not a cure, was noted to halt disease progression in some patients. Corneal indentation was also noted to break an attack. Clinical features were similar regardless of whether the primary pathology was attributed to the lens or the vitreous.
In 1707, the Parisian surgeon Antoine Maitre Jan (1650–1730)52 described “protuberance of the crystalline”: “This malady is a very particular alteration of the crystalline, in which it is augmented in volume, loses its transparency and natural figure, and becomes more solid than it should be naturally.”53 Patients experienced loss of vision in one or both eyes, and saw shadows. The pupil was slightly dilated and fixed and sometimes irregular due to pressure from the swollen lens. The lens capsule was thicker and harder.53 The condition was thought to be incurable. Maitre Jan wrote (erroneously) that the associated pain in the eye or head was due to other causes.
The same year, John Thomas Woolhouse (1664–1733/4), an English oculist who practiced in Paris, also described the condition, but called it glaucome.54 Woolhouse wrote that the hard lens of glaucoma could be detected because it resists the finger:
“But I have found an infinity of glaucomas of the crystalline humor…In these one feels a hard crystalline, resisting the finger…a true glaucoma comes ordinarily little by little to the two eyes over time, after severe headaches, after blows to the eyes, after long illnesses, or with advanced age.”54
He added:
“In looking obliquely or to the side within the pupil (always almost dilated and immobile) one will clearly see that it is only just the crystalline changed…the hard crystalline being thrown forward and strongly pressed forward against the sluice of the iris while dilating the opening makes us believe that the natural position remains there. Most often the little arteries of the adnexa we see totally swollen.”54
By noting pain and injection as integral findings, Woolhouse incorporated the inflammatory aspects (ophthalmia) that had been missing in Maitre Jan’s description. Modern ophthalmologists speak of an “attack” of angle-closure glaucoma.55 Woolhouse used the expression “attaquez” or “attaquée” to describe the onset of glaucoma.54
Woolhouse’s English lectures56,57 confirmed his belief that palpation of the eye demonstrated its firmness in glaucoma:
“But ye glaucoma adheres not to ye Iris unless it be quite unsheathed and fallen out of its calix [cavity] of ye glassy humor [the vitreous], which all very ripe and hard glaucomas will do in process of time…And then ye feeling is ye only way to have a true knowledge thereof, for such a hard and dry glaucoma reclining upon ye inside of ye iris dilates ye apple of ye eye [the pupil] and makes it immoveable, and without spring if it chance to be pushed upon ye hole in ye iris as a stone in a sling.”56
A recent report on corneal indentation to break an attack of angle closure dated the procedure to the 1970s.58 In fact, Woolhouse might have described this technique in 1707:
“While rubbing and pressing the eye gently with the thumb across the closed eyelid, one senses the hard crystalline ceding, rolling, and moving back…the pupil fraying and becoming oblong, or completely closed, or otherwise irregular. The arterioles of the conunctiva appear obstructed, but withered and relaxed, etc”.54
The published version of the lecture notes explicitly noted that palpation could break the attack:
“Upon this accident the forepart of the eye will feel harder than usual to the finger; and upon reclining the head backwards, and rubbing the eye, the chrystalline humour will fall back…and leave the fore-part again softer.”57
The glaucoma patient might see “little spangles”57 and was amenable to the “palliative cure” of depression (couching).54,57 Woolhouse was aware of Banister’s treatise.9 Of course, Woolhouse was actually using palpation to determine the hardness of the eye, not the lens. We know today that the hardness of the lens is independent of the intraocular pressure. The important point is that Woolhouse added to the tradition of Galen, in which a condition called glaucoma implied both difficulty in cure and an anteriorly prominent lens that was believed to be hard. Woolhouse wrote that glaucoma involved a palpably hard eye, mydriasis, and conjunctival injection, and thereby provided a reasonably accurate description of angle- closure glaucoma.
That Woolhouse made palpation of the eye a regular part of his examinations is also demonstrated by his description of palpable softness of the eye as suggesting an incurable condition, for which couching offered no benefit whatsoever.59,60 Today, we understand ocular hypotony is associated with many severe diseases that would not be helped by couching, including retinal detachment and impending phthisis bulbi. Although ancient authors knew of shrinking of the eye as a sign of atrophy and incurability, Woolhouse is the first author of whom we are aware to note ocular hypotony as a poor prognostic indicator. This teaching is also found in the writings of his students Benedict Duddell (flourished 1718–1759) of England and Johannes Zacharias Platner (1694–1747) of Germany.60
The French physician Michel Brisseau (1676–1743) argued in 1709 that perhaps glaucoma was due to vitreous opacity. Brisseau believed that glaucoma involved a greenish hue that emanated from deep within the eye.61 Vitreous opacities would explain the lack of a complete cure with couching. Brisseau’s anatomic evidence was quite slim. He reported mild vitreous opacification at autopsy in two patients sent to him by the physicians Barbaroux and Mareschal.61 For Mareschal’s patient, the diagnosis during life was simple cataract. During life, neither patient was evaluated by Brisseau, or reported to have had glaucoma or a green pupil.
This shaky foundation notwithstanding, the belief that glaucoma resulted from pathology posterior to the lens ran in parallel with the lens-induced concept thereafter. Regardless of the presumed pathophysiology, the actual clinical observations were remarkably consistent.
Lorenz Heister (1683–1758) of Germany was an early adopter of Brisseau’s theory that a vitreous disorder produced the green pupil of glaucoma.62 Heister described “glaucoma” in a 40-year-old man who in 1721 sustained “a violent hemicrania”. In the right eye “the pupil of which was so much dilated, that scarcely any of the iris could be seen…he became blind with that eye”, while the left eye “was become weaker”. The pupil “was of a grey colour…or rather of a sea-green, the cloudiness lying deep in the eye, and not just behind the pupil”.62
Though the French oculist Charles de Saint Yves (1667–1731) was one of many who continued to favor a lens-induced mechanism, his 1722 clinical description was nearly identical:
“…Glaucoma, in which the Cristalline is of the Colour of Sea-water…afterwards it becomes whitish, or greyish…a Sort of Alteration in the Cristalline, which supervened to a Palsy of the Visual Nerves…known by a Dilatation of the Pupil…They still can see Objects, but…only at the Corner of their Eye, because some Fibres remain not totally obstructed. the Patients feel an acute Pain in the Fund of the Eye, and in the Temples…Remedies are of no Service; and, when one Eye is afflicted with it, the other is in great Danger.”63
Mydriasis, a green pupil, and pain could occur after a trauma, which produced mydriasis, angle-recession glaucoma, and a cataract. However, Heister and Saint Yves’ description of these phenomena in both eyes in sequence, without trauma, would be more typical of angle-closure glaucoma. Generally, observers attributed glaucoma not to trauma, but rather to systemic factors, such as age, gout, or body habitus.
The English oculist John Taylor (1703–1772), who called himself “Chevalier”, was a complex figure who has been considered by many a quack.64 Nonetheless, in 1736 Taylor provided one of the most complete pre-ophthalmoscopic descriptions of angle-closure glaucoma:
“By a Glaucoma I understand a diseas’d Alteration of the Chrystalline…in its last State with an Elevation, Dilatation, and Immobility of the Pupil, and Gutta Serena… the Volume of the Chrystalline is so greatly augmented, as to raise the Circumference of the Pupil towards the Cornea, and violently press on the Uvea…the Plenitude of the Globe is greatly augmented, as to occasion Degrees of a preternatural Pressure on the immediate Organ of Sight…attended with Degrees of a violent Pain…”65
In the final stage, “…we perceive the Volume of the Chrystalline to be so greatly augmented, as to have raised the Circumference of the Pupil towards the Cornea, to near 1/4 of the healthful Thickness of the anterior Chamber of the aqueous… In the last State of this Disease …the alter’d Chrystalline… appears of a pale Green Colour.”65 Taylor treated this entity with couching, which he believed worked only in the earliest stages of the disease.
Platner has traditionally been credited with first calling the palpably hard eye glaucoma66,67 writing in 174568:
“The main pathology lies in the crystalline lens which swells up. This can be recognized with the index fingers. The hard eye will resist finger pressure. In severe cases there will be pain. The color in the eye will change to sea blue [marinae aquae]68. In older cases the pupil will dilate and this is called mydriasis. With that all faculty of vision disappears and amaurosis begins.”67
The English surgeon George Chandler (d. 1823) summarized Platner’s description69:
“a hard eye resisting to the finger…[with] a certain sensation of weight and pain in it;…within the eye hath the colour of the sea: …the pupil is dilated,…because both the vitreous humour and the retina are pressed by the lens, which is much swelled, the faculty of seeing entirely perishes…; they call this disease a glaucoma.”
The early 19th century
In the first half of the 19th century, ophthalmologists continued to offer descriptions consistent with angle-closure glaucoma, and to debate the anatomic structure that produced the disorder. Rainbows around lights were suggested as a sign of the disease. Cataract extraction, as opposed to couching, was offered as a therapy to halt the disease.
The French oculist Antoine-Pierre Demours (1762–1836) noted in 1821 that glaucoma patients had an impaired appetite, pain, a dilated and irregular pupil appearing the color of the sea, vision loss, an augmented crystalline lens, conjunctival injection, and a palpably hard eye, and might see the light of a candle covered by a cloud with the colors of the rainbow at the borders.70 He also noted a palpably hard eye (“le globe deviant dur au toucher.”)70
Georg Josef Beer described a condition he termed cataracta viridis or cataracta glaucomatosa, which influenced many of his students, including the German ophthalmologist Carl Heinrich Weller (flourished 1817–1831),71 George Frick (1793–1870) of the United States, and William Mackenzie (1791–1868) of Glasgow (see Online Supplement). For the most part, Beer’s followers attributed glaucoma to posterior segment pathology.
Weller wrote in 1819:
“A greenish, grey opacity of the vitreous humour…is called Glaucoma.” This condition involves “increasing, piercing, and rending pains…the pupil dilates, and becomes elongated…and the sight progressively decreases…the lens not unfrequently…assumes a greenish, grey aspect, (Cataracta Viridis, Cataracta Glaucomatosa, which consequently can never be operated upon with success), increases in circumference, fills the posterior chamber, pushes the iris forwards, seats itself in the already much enlarged pupil, and now even diminishes considerably the anterior chamber.”72
George Guthrie (1785–1856) of London cited Weller, and wrote in 1823: “The disease termed Glaucoma consists…in an alteration of…the vitreous humour… The lens is generally at last implicated…”73 Guthrie noted “…a turbid state of the cornea, which has lost its brilliancy…” On the sclera appear “several tortuous dark red vessels”. Moreover, “If the eye is examined by the touch, it will be found rather firmer or harder than natural… The dilatation of the pupil is…accompanied by a marked irregularity of its edge…it is…fixed or immoveable… The patient cannot distinguish light from darkness.” In addition, “…the pupil, instead of…a brilliant black, seems dull… This concave appearance [of the pupil] soon becomes of a dull yellowish colour, tending to green…the lens swells, presses the iris forwards into the anterior chamber, and a cataracta glaucomatosa is completely formed.”73 Guthrie also noted the presence of: “…pain…The disease may have come on slowly, it may have developed…under an attack of acute inflammation …”73 According to Guthrie, surgery was indicated if the patient could see light, as without surgery certain blindness will result.73 The wording was not specific enough to reveal whether he preferred couching or extraction for glaucoma.
Mackenzie wrote in 1833: “The eyeball, in glaucomatous amaurosis, always feels firmer than natural.”74 He also noted “…the greenish reflection, which we designate by the name of glaucoma…is seen as if occupying the centre of the vitreous humour…”74 Mackenzie observed:
“…the pressure of the accumulated fluid within the eye, is probably the cause of the total blindness…the sclerotic and conjunctiva become loaded with varicose vessels… the pupil dilates irregularly, the lens…is pushed forward so as almost to touch the cornea…racking pain is complained of…”74
Patients experienced “sensations of fiery and prismatic spectra”. Mackenzie noted “…In some instances the glaucomatous eye is still sensible to objects placed to one or other side of the patient, while in every other direction it distinguishes nothing.”74
Mackenzie noted that: “In its fully formed stage, glaucoma is absolutely incurable.” However, early in the disease: “The removal of the crystalline lens from a glaucomatous eye not only lessens very much the greenish appearance of the humours, but improves the vision of the patient.”74
The English surgeon William Lawrence (1783–1867) noted in 1844: “…glaucoma…is now used to denote…alteration in the colour of the pupil…”75 Patients experience “… pain in the head…” and “…dimness or weakness of sight”. In addition, “…the pupil is sea green, clear green, muddy green, or yellowish green…. The pupil…is rather dilated… Sometimes vision is impaired in one eye and not in the other…” In addition, “…the lens and iris are pushed forwards, so that the latter is convex; it may even be in contact with the cornea. The external vessels of the globe are sometimes enlarged and varicous… It takes place at or after the middle period of life…” Lawrence noted that “The situation of the discolouration has…led to the supposition that it arose from change of…the vitreous humour…” However, Lawrence believed that dissections revealed “disease of the choroid and retina…”. Lawrence noted that observation of the greenish pupillary hue of glaucoma was seen best by the physician while looking directly at the patient, rather than from the side, “whilst in cataract the pupil is grey, or greyish white, and it has the same appearance in whatever direction it is viewed…” Lawrence stated “The prognosis in glaucoma is unfavourable.”75
Specificity of descriptions
Not every green pupil was due to glaucoma. For instance, as early as 1583, the German oculist George Bartisch (1535–c. 1607) wrote that cataracts could be associated with pain, and that an anterior cataract could be accompanied by a dilated pupil.76 However, to Bartisch a green cataract (viridis cataracta) had no such associated signs or prognostic significance.76
Before the invention of the ophthalmoscope, did “glaucoma” always refer to angle-closure glaucoma? This seems unlikely. One 1750 review concluded that glaucoma and cataract were both merely opacities of the lens.77 Woolhouse and his students (eg, Platner) described a second kind of “glaucoma” of the vitreous involving a soft eye in which couching offered no benefit. As noted above, such cases of ocular hypotony probably represented early phthisis bulbi. Before the 18th century in particular, some of the incomplete descriptions might have corresponded with isolated cataract, alternate types of acute or chronic glaucoma, uveitis with cataract, or other diseases.
However, beginning with the 18th century, many clinical descriptions combine mydriasis with anatomic lens abnormalities: a larger or anteriorly prominent lens, pressing against the iris, producing a shallow anterior chamber (Table 2). This combination of mydriasis and anterior prominence of the lens is very suggestive for angle-closure glaucoma. Other findings were consistent with the diagnosis: pain, a hard eye, loss of vision or visual field, a green pupil, and the name glaucoma. Although vision could not be restored, the condition could sometimes be stabilized with couching or lens extraction. These elements in combination strongly suggest that angle-closure glaucoma was a dominant theme in the literature of this period.
Table 2.
Descriptions of vision loss consistent with angle-closure glaucoma.
| DESCRIPTION | AUTHOR (DATE) |
|---|---|
| Mydriasis, lens pressing into the iris | Felix Platter (1664),49,a John Thomas Woolhouse (1707)54,b |
| Mydriasis, large lens, pressing into the iris | Antoine Maitre Jan (1707),53,a Peter Kennedy (1713) |
| Glaucoma involves bilateral, sequential, mydriasis, eye pain, and a sea-colored pupil | Charles Saint-Yves (1722),63 Lorenz Heister (1755)62 |
| Glaucoma involves mydriasis, a large and anteriorly prominent lens, pressing against the iris, a narrow anterior chamber, green pupil, and eye pain | John Taylor (1736),65 Carl Heinrich Weller (1821),72 George Guthrie (1823),73 George Frick (1826) |
| Glaucoma involves mydriasis, a large lens, a palpably hard eye, pain, sea-colored pupil | Johannes Zacharias Platner (1745),68,b Antoine-Pierre Demours (1821)70 |
| Glaucoma involves mydriasis, a palpably hard eye, a sea-colored pupil, pain, and a large and anteriorly prominent lens | George Chandler (1775)69 |
| Glaucoma involves mydriasis, an anteriorly prominent lens, narrow anterior chamber, pain, and conjunctival injection, and a green pupil | William Mackenzie (1833),74 William Lawrence (1844)75 |
Notes:
Did not use the term glaucoma to describe this condition.
Also described another type of “glaucoma” of the vitreous which involved a soft eye and was absolutely incurable.
Variation in pathophysiologic explanations
Observers from the 18th century onward could not agree on the primary anatomic structure producing glaucoma. Those who noted the anteriorly prominent lens could not agree on whether the lens was bigger or whether something was pushing the lens forward (Fig. 8). Many 18th century authors, such as Maitre Jan, Taylor, and Platner, believed that the primary problem was swelling and hardness of the lens. Others, including followers of Brisseau and Beer, believed glaucoma was secondary to pathology of the vitreous, choroid, or retina. Without the ophthalmoscope, these theories were highly speculative. Post-enucleation or postmortem dissections could not reveal whether a particular observation was primary, or even whether it had been present in the living eye. Today it is understood that pupillary block is “the primary mechanism for angle closure”, with forward displacement of the lens from posterior segment pathology involved less frequently.17 But the pathophysiologic speculation must be separated from the actual clinical observations of the period – which consistently support a diagnosis of angle-closure glaucoma.
Figure 8.

Cross-sectional diagram of the glaucomatous eye (top) and normal eye (bottom) as illustrated in the 19th century.83 Glaucoma was ascribed to anterior displacement of the lens, pressing against the iris, causing mydriasis and a narrow anterior chamber,83 well before the development of gonioscopy and cross-sectional imaging.
The era of the ophthalmoscope
The invention of the ophthalmoscope in 1850 allowed ophthalmologists to see the excavated optic neuropathy characteristic of patients with the combination of mydriasis, an anteriorly prominent lens, and a green pupil (glaucoma). Ophthalmologists learned that some eye patients with a normal pupil (amaurosis) also developed this excavated optic neuropathy. It became better appreciated that all of these entities often involved an elevated intraocular pressure. Ultimately, both the classical form of glaucoma and amaurosis with the characteristic optic neuropathy became united under the rubric of glaucoma, and that term became commonly used in English.13 Moreover, the term amaurosis was no longer needed, and faded in frequency in English.13
In the early days of the ophthalmoscope, many descriptions of glaucoma continued to be consistent with angle-closure glaucoma. The German ophthalmologist Albrecht von Graefe (1828–1870)50,78,79 noted: “The name glaucoma formerly indicated a vague, expressionless symptom—a sea-green, bottle-green, or dirty-green background of the eye, seen through a fixed, dilated pupil.”80 Graefe added: “The muddiness of the aqueous humour, and the dulness of the posterior surface of the cornea, with the irregular refraction of light (mydriasis) and the yellow lens (age of the patient), are the chief causes of the glaucomatous hue of the pupil.”80 Graefe introduced iridectomy for this condition.80
For instance, Graefe examined a 40-year-old woman whose eyes had poor vision and “the well-marked appearances of chronic glaucoma: the globes tense…the aqueous humour slightly turbid, the pupils much dilated…on both sides perfectly fixed, of a greenish appearance; the anterior chamber flattened, the iris in spots very discoloured and atrophied. The ophthalmoscope showed…the optic nerve was on both sides very much excavated… The field of vision was extremely contracted.” Her condition improved with iridectomy.80
Graefe further observed “acute inflammatory attacks” and that “…the iris in glaucoma appears more convex anteriorly…”. A patient may see “rainbows around the flame of a candle” and experience “pains in the forehead and temples” with “the pupil irregularly dilated.”80
Graefe observed elevated intraocular pressure and glaucoma from “swelling of the lens”, which might occur due to trauma, with iris contact, or due to a simple cataract. Graefe regarded iridectomy as the primary treatment, but also noted that lens extraction could be curative, sometimes even when iridectomy had failed.80 The efficacy of lens extraction in this circumstance has been highlighted recently.81
In 1857, Graefe was reluctant to embrace the semantics of his contemporaries who used the term “glaucoma” to describe quiet eyes as excavated optic neuropathy. He stated of “amaurosis with excavation of the optic nerve” that such cases “have been often called glaucoma, (but only since the introduction of the ophthalmoscope)”.80
By 1858, Graefe was willing to include under the rubric of “glaucoma” other conditions producing the excavated optic neuropathy if it could be shown that they involved elevated intraocular pressure.80 By 1864, Graefe accepted the term “glaucoma” for completely quiet eyes with an excavated optic neuropathy because it was discovered that many of them had an elevated intraocular pressure.82 Today, many of these cases would be called “primary open-angle glaucoma.” Of course, this expanded definition for glaucoma ultimately prevailed.
A subsequent 19th century observer noted: “The color of the pupil which gave origin to the name of glaucoma (from the Greek for sea-green) as well as to its old title of ‘green cataract,’ is produced by the reflection of the light entering the lens, modified by the state of the cornea and the aqueous humor. It is not peculiar to glaucoma, and is seen in other conditions where dilated pupil and imperfectly transparent media are associated.”83 The accompanying cross-sectional image of the eye proves the anatomical understanding of angle closure, even before gonioscopy and ultrasound imaging were developed (Fig. 8).83
The era of the ophthalmoscope has seen dynamic developments in the diagnosis and treatment of all types of glaucoma. Early types of filtering surgery were introduced as early as 1878.79 Efforts to measure intraocular pressure in the latter half of the 19th century were followed by the introduction of the Schiotz indentation tonometer in 1905, and Goldmann applanation tonometry by 1955.84 Gonioscopy to visualize the anterior chamber angle was reported by 1915.85 Automated perimetry was introduced in the 1970s.86 Pharmacologic agents to lower intraocular pressure have included eserine (physostigmine) and pilocarpine since the 19th century, and epinephrine, adrenergic agonists, carbonic anhydrase inhibitors, beta blockers, and prostaglandin analogs in the 20th century.87
Conclusions
Glaucoma has almost certainly occurred since antiquity. Primary open-angle glaucoma, and other forms with a normal-appearing eye, would have been called amblyopia, amaurosis, gutta serena, and other terms. Prior to the invention of the ophthalmoscope, palpable hardness was only rarely described in amaurosis.
Although not emphasized by present-day ophthalmologists, angle-closure glaucoma may produce a green pupillary hue. Visual loss not readily treated by surgery, and associated with a glaucous or green pupil, has been described from antiquity through the 19th century. Ancient and medieval Arabic authors associated the glaucous hue with a hard or anteriorly prominent lens. The unfavorable pupillary hue was more specifically described as green during the European Middle Ages. During the Renaissance, Felix Platter wrote that the lens is anterior, and can even cause mydriasis and vision loss by contacting the iris. Richard Banister noted a hard eye with a green lens and incurable vision loss. In 1707, surgeons in Paris noted that anterior prominence of the lens could lead to mydriasis, visual loss, and other features of angle-closure glaucoma. John Thomas Woolhouse called the condition glaucoma, and noted palpable hardness of the eye. Specific descriptions of angle-closure glaucoma involving a green pupil, mydriasis, and an anteriorly prominent lens appear in the writings of “Chevalier” John Taylor in the 18th century, William Mackenzie in the 19th century, and many others.
With the development of the ophthalmoscope in 1850, the excavated optic neuropathy was seen to be present not only in classical glaucoma (with a gray or green pupil) but also in certain cases of amaurosis (with a normal pupil). An elevated intraocular pressure became better appreciated in both conditions, and the two became united under the term glaucoma.
Supplementary Materials
This supplementary file contains additional and more complete quotations and translations, and specific pages relevant for cited books.
Acknowledgments
The authors would like to thank David J. Butterfield, PhD, Queens’ College, University of Cambridge, for translating the text by Riolan the Elder and by Avicenna.
Footnotes
ACADEMIC EDITOR: Joshua Cameron, Editor in Chief
PEER REVIEW: Six peer reviewers contributed to the peer review report. Reviewers’ reports totaled 981 words, excluding any confidential comments to the academic editor.
FUNDING: This work was partially supported by the NIH Center Core Grant P30EY014801 and Research to Prevent Blindness Unrestricted Grant to the University of Miami. The authors confirm that the funder had no influence over the study design, content of the article, or selection of this journal.
COMPETING INTERESTS: SS discloses personal fees from Alimera, Baush + Lomb, Stanten and Vindico, outside the submitted work. No authors report any proprietary or commercial interest in any product mentioned or concept discussed in this article. Authors disclose no other potential competing interests.
Paper subject to independent expert blind peer review. All editorial decisions made by independent academic editor. Upon submission manuscript was subject to anti-plagiarism scanning. Prior to publication all authors have given signed confirmation of agreement to article publication and compliance with all applicable ethical and legal requirements, including the accuracy of author and contributor information, disclosure of competing interests and funding sources, compliance with ethical requirements relating to human and animal study participants, and compliance with any copyright requirements of third parties. This journal is a member of the Committee on publication Ethics (COPE).
Author Contributions
Analyzed the data: CTL, SGS, FMG, MTY. Wrote the first draft of the manuscript: CTL. Contributed to the writing of the manuscript: CTL, SGS, FMG, MTY, DB. Agree with manuscript results and conclusions: CTL, SGS, FMG, MTY, DB. Jointly developed the structure and arguments for the paper: CTL, SGS, FMG, MTY. Made critical revisions and approved final version: CTL, SGS, FMG, MTY, DB. All authors reviewed and approved of the final manuscript.
REFERENCES
- 1.Frezzotti R. The glaucoma mystery from ancient times to the 21st century. The glaucoma mystery: ancient concepts. Acta Ophthalmol Scand. 2000;78(S232):14–8. doi: 10.1111/j.1600-0420.2000.tb01081.x. [DOI] [PubMed] [Google Scholar]
- 2.Tsatsos M, Broadway D. Controversies in the history of glaucoma: is it all a load of old Greek? Br J Ophthalmol. 2007;91(11):1561–2. doi: 10.1136/bjo.2007.114298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grzybowski A. Controversies in the history of glaucoma. Acta Ophthalmol. 2013;91(s252) [Google Scholar]
- 4.Leffler CT, Schwartz SG, Hadi TM, Salman A, Vasuki V. The early history of glaucoma: the glaucous eye (800 BC to 1050 AD) Clin Ophthalmol. 2015;9:207–15. doi: 10.2147/OPTH.S77471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eye Diseases Prevalence Research Group Prevalence of open-angle glaucoma among adults in the United States. Arch Ophthalmol. 2004;122:532–8. doi: 10.1001/archopht.122.4.532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Galen JI. In: On Diseases and Symptoms. Galen JI, translator. Vol. 2006. Cambridge, MA: Cambridge University Press; p. 215. [Google Scholar]
- 7.Aetius of Amida Waugh RL. In: The Ophthalmology of Aetius of Amida. Waugh RL, translator. Oostende: J. P. Wayenborgh; 2000. pp. 5–87. [Google Scholar]
- 8.Quigley HA. Open-angle glaucoma. N Engl J Med. 1993;328(15):1097–106. doi: 10.1056/NEJM199304153281507. [DOI] [PubMed] [Google Scholar]
- 9.Leffler CT, Schwartz SG, Davenport B, Randolph J, Busscher J, Hadi T. Enduring influence of elizabethan ophthalmic texts of the 1580s: bailey, grassus, and guillemeau. Open Ophthalmol J. 2014;8:12–8. doi: 10.2174/1874364101408010012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guillemeau J, Bailey W, Hunton A. In: A Worthy Treatise of the Eyes Contayning the Knowledge and Cure of One Hundred and Thirtene Diseases, Incident vnto them: First Gathered & Written in French, by Iacques Guillemeau, Chyrurgion to the French King, and Now Translated into English, Togeather with a Profitable Treatise of the Scorbie; and Another of the Cancer by A.H. Also Next to the Treatise of the eies is Adoiyned a Work Touching the Preseruation of the Sight, Set Forth by VV. Bailey. D. of Phisick. Hunton A, translator. London: Robert Waldegrave; 1587. pp. 188–90. [Google Scholar]
- 11.Banister R, Guillemeau J, Hunton A, Weyer J, Textor B, Bailey W. A Treatise of One Hundred and Thirteene Diseases of the Eyes and Eye-Liddes. The Second Time Published with Some Profitable Additions of Certaine Principles and Experiments. London: Felix Kyngston for Thomas Man Dwelling in Pater-Noster-Row; p. 1622. at the signe of the Talbot. [Google Scholar]
- 12.Cooper S, Reese DM, editors. A Dictionary of Practical Surgery. Vol. 1. New York: Harper; 1836. p. 26. [Google Scholar]
- 13.Leffler CT, Schwartz SG, Stackhouse R, Byrd Davenport B, Spetzler K. Evolution and impact of eye and vision terms in written English. JAMA Ophthalmol. 2013;131(12):1625–31. doi: 10.1001/jamaophthalmol.2013.917. [DOI] [PubMed] [Google Scholar]
- 14.Day AC, Baio G, Gazzard G, et al. The prevalence of primary angle closure glaucoma in European derived populations: a systematic review. Br J Ophthalmol. 2012;96(9):1162–7. doi: 10.1136/bjophthalmol-2011-301189. [DOI] [PubMed] [Google Scholar]
- 15.Patel K, Patel S. Angle-closure glaucoma. Dis Mon. 2014;60(6):254–62. doi: 10.1016/j.disamonth.2014.03.005. [DOI] [PubMed] [Google Scholar]
- 16.Jain IS, Gupta A, Dogra MR, Gangwar DN, Dhir SP. Phacomorphic glaucoma-management and visual prognosis. Indian J Ophthalmol. 1983;31(5):648–53. [PubMed] [Google Scholar]
- 17.Nongpiur ME, Ku JY, Aung T. Angle closure glaucoma: a mechanistic review. Curr Opin Ophthalmol. 2011;22(2):96–101. doi: 10.1097/ICU.0b013e32834372b9. [DOI] [PubMed] [Google Scholar]
- 18.Baillif S, Cornut PL, Girard C, Ghesquieres H, Perard L. Bilateral angle-closure glaucoma and multifocal choroiditis as a first presentation in hodgkin lymphoma. Retin Cases Brief Rep. 2011;5(3):201–5. doi: 10.1097/ICB.0b013e3181f047a1. [DOI] [PubMed] [Google Scholar]
- 19.Pierre Filho Pde T, Carvalho Filho JP, Pierre ET. Bilateral acute angle closure glaucoma in a patient with dengue fever: case report. Arq Bras Oftalmol. 2008;71(2):265–8. doi: 10.1590/s0004-27492008000200025. [DOI] [PubMed] [Google Scholar]
- 20.Schlote T, Freudenthaler N, Gelisken F. Anticoagulative therapy in patients with exudative age-related macular degeneration: acute angle closure glaucoma after massive intraocular hemorrhage. Ophthalmologe. 2005;102(11):1090–6. doi: 10.1007/s00347-004-1096-z. [DOI] [PubMed] [Google Scholar]
- 21.Premsenthil M, Salowi MA, Siew CM, Gudom I, Kah T. Spontaneous malignant glaucoma in a patient with patent peripheral iridotomy. BMC Ophthalmol. 2012;12:64. doi: 10.1186/1471-2415-12-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ahmed IK. Anterior segment optical coherence tomography in glaucoma. J Curr Glaucoma Pract. 2009;3(1):14–23. [Google Scholar]
- 23.Barton K. Secondary glaucoma. In: Spalton DJ, Hitchings RA, Hunter PA, editors. Atlas of Clinical Ophthalmology. 3rd. Vol. 2005. Philadelphia: Elsevier Mosby; p. 225. [Google Scholar]
- 24.Baxter JM, Alexander P, Maharajan VS. Bilateral, acute angle-closure glaucoma associated with Guillain-Barre syndrome variant. [Accessed September 5, 2014];BMJ Case Rep. 2010 2010 doi: 10.1136/bcr.11.2009.2487. Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3027938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rao A. Clear lens extraction in plateau iris with bilateral acute angle closure in young. J Glaucoma. 2013;22(9):e31–2. doi: 10.1097/IJG.0b013e31825c10c4. [DOI] [PubMed] [Google Scholar]
- 26.See J. Phacoemulsification in angle closure glaucoma. J Curr Glaucoma Pract. 2009;3(1):28–35. [Google Scholar]
- 27.Spadoni VS, Pizzol MM, Muniz CH, Melamed J, Fortes Filho JB. Bilateral angle-closure glaucoma induced by trimetoprim and sulfamethoxazole combination: case report. Arq Bras Oftalmol. 2007;70(3):517–20. doi: 10.1590/s0004-27492007000300023. [DOI] [PubMed] [Google Scholar]
- 28.Wilensky JT, Campbell DG. Primary angle-closure glaucoma. In: Albert DM, Jakobiec FA, editors. Principles and Practice of Ophthalmology. 2nd. Vol. 2000. Philadelphia: WB Saunders Company; p. 2691. [Google Scholar]
- 29.Yip LW, Aquino MC, Chew PT. Measurement of anterior lens growth after acute primary angle-closure glaucoma. Can J Ophthalmol. 2007;42(2):321–2. [PubMed] [Google Scholar]
- 30.Wilson FM, editor. Practical Ophthalmology: A Manual for Beginning Residents. 5th. Vol. 2005. San Francisco: American Academy of Ophthalmology; p. 353. [Google Scholar]
- 31.Shima C, Otori Y, Miki A, Tano Y. A case of iridoschisis associated with plateau iris configuration. Jpn J Ophthalmol. 2007;51(5):390–1. doi: 10.1007/s10384-007-0454-1. [DOI] [PubMed] [Google Scholar]
- 32.Turati M, Flores-Sánchez BC, Isida-Llerandi CG, Kahook M, Gil-Carrasco F. Iris ring cyst. Case report. [Quiste en anillo de Iris. Reporte de un caso.] Rev Mexicana Oftalmol. 2013;87:1. [Google Scholar]
- 33.Zhou X, Li G, Zhang H, Li X, Guan Y, Bing L. Multiple layers lens capsule true exfoliation in patient with primary angle closure glaucoma. Ophthalmol Ther. 2012;1(1):4. doi: 10.1007/s40123-012-0004-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Snyder C. Mr. Mackenzie Investigates Green Cataracts. Arch Ophthalmol. 1965;74(1):133–6. doi: 10.1001/archopht.1965.00970040135025. [DOI] [PubMed] [Google Scholar]
- 35.Drews RC. Green cataract. Arch Ophthalmol. 2006;124(4):579–86. doi: 10.1001/archopht.124.4.579. [DOI] [PubMed] [Google Scholar]
- 36.Galen of Pergamon. May MT. In: On the Usefulness of the Parts of the Body De usu partium. May MT, translator. Vol. 2. New York: Cornell University Press; 1968. p. 473. [Google Scholar]
- 37.Berlin B, Kay P. Basic Color Terms: Their Universality and Evolution. Berkeley: University of California Press; 1991. pp. 4–145. [Google Scholar]
- 38.Maxwell-Stuart PG. Studies in Greek Colour Terminology. Vol. 1. Leiden: Glaukos/Brill Archive; 1981. pp. 26–165. [Google Scholar]
- 39.Hirschberg J, Blodi FC. The History of Ophthalmology. Vol. 2. The Middle Ages; the Sixteenth and Seventeenth Centuries. Vol. 1985. Bonn: J.P. Wayenborgh Verlag; pp. 90–188. [Google Scholar]
- 40.Grassus B. De oculis eorumque aegritudinibus et curis. Vol. 8. Ferrara; 1474. [Accessed September 5, 2014]. Available at: http://gallica.bnf.fr/ark:/12148/bpt6k58490t/f14.image.r=.langEN. [Google Scholar]
- 41.Grassus B, Wood CA. In: Benevenutus Grassus of Jerusalem De oculis eorumque egritudinibus et curis: translated with notes and illustrations from the first printed edition, Ferrara, 1474 AD. Wood CA, translator. Stanford, Stanford University Press; 1929. pp. 39–40. [Google Scholar]
- 42.McVaugh MR. The nature and limits of medical certitude at early fourteenth-century montpellier. Osiris. 1990;6:62–84. doi: 10.1086/368695. [DOI] [PubMed] [Google Scholar]
- 43.Ostler N. Ad Infinitum: A Biography of Latin. Vol. 2007. New York: Walker & Co; p. 211. [Google Scholar]
- 44.Ibn Sina AA (Avicenna), Gerardus Cremonensis . Avicennae Arabum medicorum principis, Canon medicinæ. Vol. 1608. Venice: Fabium Paulinum; [Accessed September 5, 2014]. pp. 551–65. Available at: http://books.google.com/books?id=qA4VK-w7WDoC&pg=PA551&lpg=PA551&dq=%22viriditate+oculi%22&source=bl&ots=8bmyuHM_9G&sig=_fJTiGj29u-GKIFYTtd6CfrLan0&hl=en&sa=X&ei=tXt7U_CRCsWBqgbAuYHoCw&ved=0CCsQ6AEwAA#v=onepage&q=%22viriditate%22&f=false. [Google Scholar]
- 45.Guillemeau J. Traité des maladies de l’oeil. Vol. 1585. Paris: Charles Massé; p. 85. [Google Scholar]
- 46.Riolan J(lepère) Ioannis Riolani ambiani medici parisiensis, viri clarissimi pera omnia. Parisiis: ex officina Plantiniana; 1610. [Accessed September 5, 2014]. pp. 443–4. Available at: http://www2.biusante.parisdescartes.fr/livanc/?cote=00326&do=chapitre. [Google Scholar]
- 47.Riolan J. A Sure Guide, or, the Best and Nearest Way to Physick and Chirurgery. London: Peter Cole; 1657. p. 142. [Google Scholar]
- 48.Lindberg DC. Theories of Vision: From Al-Kindi to Kepler. Chicago: University of Chicago Press; 1976. pp. 175–7. [Google Scholar]
- 49.Platter F, Cole A, Culpeper N. In: Platerus Golden Practice of Physic. Cole A, Culpeper N, translators. London: Peter Cole; 1664. pp. 63–5. [Google Scholar]
- 50.Duke-Elder W. A System of Ophthalmology. XI. St. Louis: Mosby; 1969. pp. 381–662. [Google Scholar]
- 51.Sorsby A. Hardness of the eye: an historical note. Br J Ophthalmol. 1932;16(5):292–5. doi: 10.1136/bjo.16.5.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hirschberg J, Blodi FC. The History of Ophthalmology. Vol. 3. Bonn: J. P. Wayenborgh Verlag; 1984. pp. 14–229. (The Renaissance of Ophthalmology in the Eighteenth Century (Part One)). [Google Scholar]
- 53.Maître-Jan A. Traité des maladies de l’oeil et des remedes propres pour leur guerison. Vol. 1707. Troyes: J. LeFebvre; pp. 210–6. [Google Scholar]
- 54.Woolhouse JT, LeCerf C. Dissertations scavantes et critiques de monsieur de Woolhouse sur la cataracte et le glaucoma. Offenbach sur le Main: Bonaventure de Launoy; 1717. pp. 21–298. [Google Scholar]
- 55.Ritch R. Argon laser treatment for medically unresponsive attacks of angle-closure glaucoma. Am J Ophthalmol. 1982;94(2):197–204. doi: 10.1016/0002-9394(82)90075-7. [DOI] [PubMed] [Google Scholar]
- 56.Woolhouse JT. A Treatise of ye Cataract and Glaucoma. Vol. 1721. London: Royal Society of Medicine; p. 51. [Google Scholar]
- 57.Woolhouse JT. A Treatise of the Cataract and Glaucoma: in Which the Specific Distinctions of Those Two Diseases, and the Existence of Membranous Cataracts, are Clearly Demonstrated…Compiled from the Dictates of the Late Learned and Ingenious Mr. Woolhouse, as Taken from Him in Writing, by One of His Pupils. London: Charing-Cross; 1745. pp. 18–99. Printed for M. Cooper, at the Globe in Pater-Noster-Row; and G. Woodfall, at the King’s-Arms. [Google Scholar]
- 58.Masselos K, Bank A, Francis IC, Stapleton F. Corneal indentation in the early management of acute angle closure. Ophthalmology. 2009;116:25–9. doi: 10.1016/j.ophtha.2008.08.032. [DOI] [PubMed] [Google Scholar]
- 59.James RR. Woolhouse (1666–1733/4) Br J Ophthalmol. 1934;18(4):193–217. doi: 10.1136/bjo.18.4.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Leffler CT, Schwartz SG. Cogan Ophthalmic History Society Proceedings. Cogan Ophthalmic History Society; San Francisco, CA: 2014. John Thomas Woolhouse (1666–1734): Bold Ophthalmic Innovator and Teacher; pp. 57–79. [Google Scholar]
- 61.Brisseau M. Traite de la cataracte et du glaucoma. Vol. 1709. Paris: France d’Houry; pp. 42–210. [Google Scholar]
- 62.Heister L, Wirgman G. In: Medical, Chirurgical, and Anatomical Cases and Observations. Heister L, translator. London: J. Reeves; 1755. pp. 582–657. [Google Scholar]
- 63.Saint-Yves C, Stockton J. In: A New Treatise of the Diseases of the Eyes. Containing Proper Remedies, and Describing the Chirurgical Operations Requisite for Their Cures. Stockton J, translator. Vol. 1741. London: Printed for the Society of Booksellers; pp. 231–91. [Google Scholar]
- 64.Coats G. The Chevalier Taylor. R Lond Ophthalmic Hosp Rep. 1915;20:1–90. [Google Scholar]
- 65.Taylor J. A New Treatise on the Diseases of the Chrystalline Humour of a Human Eye: Or, of the Cataract and Glaucoma. London: 1736. pp. 26–30. Printed for James Roberts, Near the Oxford-Arms in Warwick-Lane. [Google Scholar]
- 66.Terson MA. Les premiers observateurs de la durété de l’oeil dans le glaucome. Arch Ophtalmol (Paris) 1907;27:625–30. [Google Scholar]
- 67.Hirschberg J, Blodi FC. The History of Ophthalmology. Vol 6. The First Half of the Nineteenth Century (Part Two) Bonn: J. P Wayenborgh Verlag; 1986. p. 158. [Google Scholar]
- 68.Platner JZ. Institvtiones Chirvrgiae Rationalis. Leipzig: B Casparis Fritschii; 1745. p. 769. [Google Scholar]
- 69.Chandler G. A Treatise of a Cataract, Its Nature, Species, Causes and Symptoms, with a Distinct Representation of the Operations by Couching and Extraction. London: Samuel Chandler; 1775. pp. 12–3. [Google Scholar]
- 70.Demours AP. Précis théorique et pratique sur les maladies des yeux. Paris: Firmin Didot; 1821. pp. 553–5. [Google Scholar]
- 71.Leffler CT, Randolph J, Stackhouse R, Davenport B, Spetzler K. Monteath’s translation of Weller: an underappreciated trove of ophthalmology lexicon. Arch Ophthalmol. 2012;130(10):1356–7. doi: 10.1001/archophthalmol.2012.2084. [DOI] [PubMed] [Google Scholar]
- 72.Weller CH, Monteath GC. A Manual of the Diseases of the Human Eye. Vol. 2. Glasgow: Reid & Henderson; 1821. pp. 27–291. [Google Scholar]
- 73.Guthrie GJ. Lectures on the Operative Surgery of the Eye. London: Burgess and Hill; 1823. pp. 214–9. [Google Scholar]
- 74.Mackenzie W. A Practical Treatise on the Diseases of the Eye. Vol. 1833. Boston: Carter, Hendee and Co; pp. 475–590. [Google Scholar]
- 75.Lawrence W. Treatise on the Diseases of the Eye. 3rd. London: Henry G. Bohn; 1844. pp. 494–9. [Google Scholar]
- 76.Bartisch G, Blanchard DL. In: Ophthalmodouleia. Blanchard DL, translator. Vol. 1996. Oostende: J. P. Wayenborgh; pp. 52–8. [Google Scholar]
- 77.O’Halloran S. A New Treatise on the Glaucoma, or Cataract. Vol. 1750. Dublin: S Powell; p. 27. [Google Scholar]
- 78.Lowe RF, Curran Barkan. Chandler: a history of pupillary obstruction and narrow angle glaucoma. J Glaucoma. 1995;4(6):419–26. [PubMed] [Google Scholar]
- 79.Lowe RF. A history of primary angle closure glaucoma. Surv Ophthalmol. 1995;40(2):163–70. doi: 10.1016/s0039-6257(95)80006-9. [DOI] [PubMed] [Google Scholar]
- 80.Von Graefe A, Windsor T. Three Memoirs on Iridectomy in Certain Forms of Iritis, Choroiditis, and Glaucoma. In: Windsor T, translator. Selected Monographs: Kussmaul and Tenner on Epileptiform Convulsions from Haemorrhage Wagner on the Resection of Bones and Joints Graefe’s Three Memoirs on Iridectomy in Iritis, Choroiditis, and Glaucoma. London: New Sydenham Society; 1859. pp. 288–380. [Google Scholar]
- 81.Brown RH, Zhong L, Lynch MG. Lens-based glaucoma surgery: using cataract surgery to reduce intraocular pressure. J Cataract Refract Surg. 2014;40(8):1255–62. doi: 10.1016/j.jcrs.2014.06.001. [DOI] [PubMed] [Google Scholar]
- 82.Keyser PD. Glaucoma: Its Symptoms, Diagnosis, and Treatment. Philadelphia: Lindsay and Blakiston; 1864. pp. 45–6. [Google Scholar]
- 83.Stirling AW. Glaucoma: Its Symptoms, Varieties, Pathology and Treatment. Vol. 1898. St. Louis: J.H. Parker; p. 8. [Google Scholar]
- 84.Kniestedt C, Punjabi O, Lin S, Stamper RL. Tonometry through the ages. Survey Ophthalmol. 2008;53(6):568–91. doi: 10.1016/j.survophthal.2008.08.024. [DOI] [PubMed] [Google Scholar]
- 85.Alward WL. A history of gonioscopy. Optom Vis Sci. 2011;88(1):29–35. doi: 10.1097/OPX.0b013e3181fc3718. [DOI] [PubMed] [Google Scholar]
- 86.Johnson CA, Wall M, Thompson HS. A history of perimetry and visual field testing. Optom Vis Sci. 2011;88(1):e8–15. doi: 10.1097/OPX.0b013e3182004c3b. [DOI] [PubMed] [Google Scholar]
- 87.Realini T. A history of glaucoma pharmacology. Optom Vis Sci. 2011;88(1):36–8. doi: 10.1097/OPX.0b013e3182058ead. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This supplementary file contains additional and more complete quotations and translations, and specific pages relevant for cited books.


