Abstract
Background:
Atopic dermatitis is a distinct age-related clinical entity. Its etiopathogenesis is largely insubstantial. Nevertheless, it seems to be an outcome of interplay of maternal and inheritance, pregnancy/intrauterine and environmental factors. Besides, immune dysregulation, and nutritional supplements also play essential roles. Its diagnosis has been perpetuated by three or more major/minor criteria.
Objectives:
An endeavor to study its demographic and clinical pattern in contemporary prospective.
Materials and Methods:
100 fresh patients of atopic dermatitis, diagnosed on the basis of an established three or more major and minor criteria, salient presentations of which were recorded in a preset proforma, which also recorded age, duration, age of onset, and sex. Serum immunoglobulin E (IgE) levels were determined by conventional technique. The data thus obtained was analysed to study its clinical pattern and to correlate its severity to IgE levels.
Results:
Its overall (new and old) prevalence was 0.98%, while that of new patients was 0.24%. 83 (83%) were in the age group of 2-12 years, of which 54 (83.1%) were males and 29 (82.9%) were female, of which 70 (70%) had urban, while 30 (30%) had rural background. Its duration varied from 8 to 192 weeks, with a mean of 76 weeks, and a standard deviation of 21.42 weeks [76 ± 21.42].
Conclusion:
Atopic dermatitis is a discrete, overt, age and IgE-related entity frequently displaying varying demographic and clinical connotation.
Keywords: Atopic Dermatitis, prospective cross-sectional, immunoglobulin IgE
What was known?
Atopic dermatitis, a well-recognized chronic inflammatory disorder, identified by severe pruritus, erythematous, scaly and oozing plaques, the diagnosis of which is supplemented by universally accepted criteria.
Introduction
Atopic dermatitis (AD)[1] is a non-contagious, intensely pruritic, inflammatory, chronic skin disorder having a course of exacerbations and remissions, occurring in infancy and childhood running in families with a history of atopy. It is frequently associated with an elevated immunoglobulin E (IgE) levels in serum. Disease has an intricate immunological basis influenced by genetic/familial predisposition, and certain environmental, life style and dietary factors. Recent trends suggest a continuous rise in the prevalence of AD in developed nations and in countries undergoing rapid urbanization and industrialization. The clinical phenotype that characterizes AD is the product of complex interactions among susceptibility genes, the host's environment, defects in skin barrier function, and systemic and local immunologic responses.[2,3,4] IgE discovered in 1966 by the Japanese scientist couple Teruka and Kimishige Ishizaka,[5] plays an important role in allergy, and is especially associated with type 1 hypersensitivity. Its pattern may show fluctuation; hence, it is befitting to evaluate the same periodically.
Materials and Methods
Cross-sectional (descriptive) study of 100 AD patients was conducted in Skin Institute and the School of Dermatology, Greater Kailash, New Delhi over a period from May 2010 till December 2011. The diagnosis of AD was made on the basis of Hanifin and Rajka[6] diagnostic criteria, wherein presence of at least three major and three minor criteria's were taken cognizance of. Accordingly, new patients who fulfilled at least three major and three minor criteria were included, while previously diagnosed AD patients and those on treatments were excluded.
Detailed history, comprising age, sex, occupation, residence, total duration of disease, associated itching seasonal variation, associated asthma, allergic rhinitis, atopy, family history of AD, and asthma) was recorded in a preset proforma physical and dermatological examination, including examination of mucous membranes and skin appendages was carried out.
Assessment of severity was carried out by six area, six sign atopic dermatitis (SASSAD) score, which included assessment of six signs: erythema, exudation, excoriation, dryness, cracking and lichenification; at six sites, arms, hands, legs, feet, head and neck, and trunk; each on a scale of 0, 1, 2 and 3, the total range being 0-108.[7]
Serum IgE levels were measured by microwell total-IgE EIA, an enzyme immunoassay for quantitative determination of IgE in human serum or plasma (Syntron Bioresearch, Inc.).
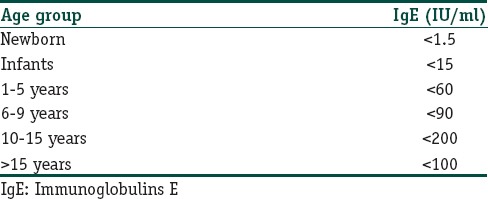
Serum IgE concentrations in general increase with age and peak at some time during adolescence, Wide individual variation exists at all age levels with the following reference representative of the concentration increase with age (vide infra):[8]
Statistical analysis
The findings thus obtained were analyzed to study the clinical pattern of AD and to correlate its severity to IgE levels. The continuous variables are presented as mean ± standard deviation (± SD) or median (range) if the data is skewed. Categorical variables are presented as absolute numbers and percentages. Normally distributed continuous variables were compared using the unpaired t test, whereas the Mann-Whitney U test was used for those variables that were not normally distributed. Spearman's correlation between s-IgE levels and SASSAD score was computed. For all statistical tests, a P value less than 0.05 was taken to indicate a significant difference.
Results
Prevalence
Overall prevalence comprising new and old patients of AD was 0.98%, while that of only new cases alone was 0.24%.
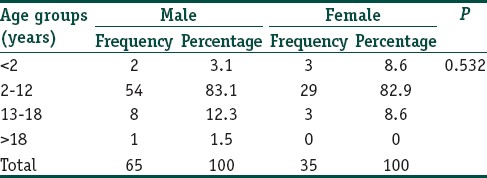
Age and sex distribution
As displayed in the adjoining Table 1, 83 patients (83%) were in the age group of 2-12 years, of which 54 (83.1%) were males and 29 (82.9%) were female, while only 5 (5%) were less than 2 years of age, and 11 (11%) were between 13 and 18 years of age. The latter had 8 males and 3 females.
Table 1.
Atopic dermatitis: Age and sex distribution
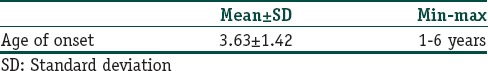
Atopic dermatitis: Age of onset
The mean age of onset of AD was 3.63 ± 1.42 [Table 2].
Table 2.
Atopic dermatitis: Age of onset
Residence
A total of 70 patients (70%) had hailed from urban areas, while 30 (30%) had rural background.
Duration
The duration of AD varied from 8 to 192 weeks. Its mean duration was 76 weeks with a standard deviation (SD) of 21.42 weeks [76 ± 21.42].
Associated features
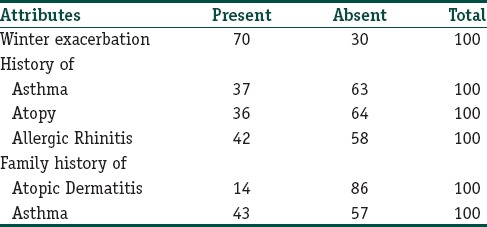
The frequency of associated features is shown in the adjoining Table 3. Winter exacerbation was a cardinal feature in 70 (70%) followed by history of allergic rhinitis in 42 (58%), asthma in 37 (63%), and atopy per se in 36 (64%), whereas a family of AD and asthma was present in 14 (86%) and 43 (57%) of the patients, respectively.
Table 3.
Atopic dermatitis: Frequency of associated factors
Frequency of presenting features is depicted in Table 4. Periorbital darkening [Figure 1] and Dennie Morgan fold [Figure 2] were also seen.
Table 4.
Atopic dermatitis: Frequency of Presenting clinical features
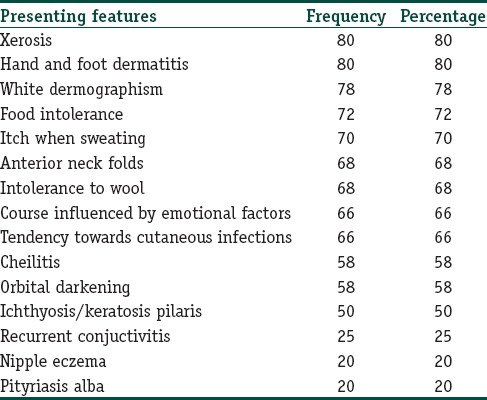
Figure 1.

Atopic dermatitis: Depicting periorbital darkening
Figure 2.

Depicting Dennie Morgan fold
Site of involvement
Area of involvement of AD was asked, recorded and evaluated. We found that the flexures were involved in 45 (45%) patients, extensors were involved in 30 (30%) patients and facial involvement was seen in 25 (25%) patients of the study group.
Serum IgE levels
The minimum serum IgE levels were 72 IU/ml and maximum 3000 IU/ml with a mean value of 1084.73 ± 776.27 and median value of 994.5 IU/ml.
According to the Microwell test, the normal levels of serum IgE are different in different age groups[8] [Table 5].
Table 5.
Atopic dermatitis: Age groups and normal IgE levels
Accordingly, the patients were divided into normal and those with higher values [Table 6]. Seventeen (100%) in the age group of 1-5 years and 28 (90%) in the age group of 6-9 years had higher serum IgE values. Spearman's rank correlation coefficient between serum IgE levels and the SASSAD score was 96.4% between the two variables, indicating highly significant and positive correlation (P value = 0.000).
Table 6.
Atopic dermatitis: Serum IgE levels in different age groups
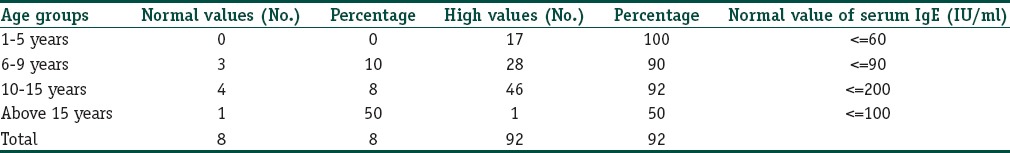
Serum IgE values in different age groups
According to the microwell test used, the normal levels of IgE are different in different age groups and accordingly the patients are divided into two groups, that is, with normal value and with higher values. It was seen that in the study group out of 100 patients, 17 patients were in the age group of 1-5 years, 31 patients in the age group of 6-9 years, 50 patients in the age group of 10-15 years and only 2 patients were in the age group of above 15 years. This is depicted in table number 17.
SASSAD score
Severity grading of all the patients of study group was done according to the SASSAD score and it was seen that the minimum value of SASSAD score was 9 and the maximum value was 56. It showed a mean value of 38.46 ± 12.69 and a median value of 41.5.
Correlation between serum IgE levels and SASSAD score
Spearman's correlation between serum IgE levels and the SASSAD score was computed. The figure stood at 96.4% showing that the two variables had highly significant positive correlation between them (P = 0.000).
Discussion
AD is a chronic relapsing inflammatory dermatosis, characterized by severe pruritus, erythematous, scaly and oozing plaques. It is frequently associated with elevated levels of serum IgE. The diagnosis was made using the Hanifan and Rajka's criteria, continue to be the mainstay for the diagnosis of AD; the other groups[9,10] have suggested a few conceivable modifications in order to achieve perfection. The prevalence of AD was found at 0.24% in the current study, while in another Indian study[11] it was found to be 0.55%, whereas it has a diverse prevalence across the globe[12,13] ranging from 0.7% to 0.26%.
The mean age-of-onset of AD was 3.63 ± 1.42, with a minimum of 1 year to maximum of 6 years, a finding corresponding to other studies[11,14] from the Indian subcontinent, inferring that AD is disease of young children.
Predominance of male over the female patients was explicit, it was 1.8:1, a finding almost similar to that of Sarkar and Kanwar[15] from India, whereas it was 1.3:1 in another study.[11]
Interestingly, 70% of the patients had hailed from urban setting, while remaining of them from rural area (68%), a finding inconsonance with another Indian report.[15]
The duration of AD varied from 8 to 192 weeks with a mean of 76 ± 21.42 weeks, a finding consistent with that of Dhar and Kanwar[14] in which the mean duration of disease at presentation was 84 weeks (in a sample of north Indian children). However, the duration of the disease was found to be 288 weeks in another long-term study.[15]
Itching was a major presenting symptom in the current study, which is in agreement with the other studies from India[15] and elsewhere.[16]
History of exacerbation of AD in winter was another constant feature conforming to that observed by Sarkar and Kanwar[15] and Rddzki et al.[16] In a study conducted at Mayo clinic, 54% of the AD patients had winter aggravation.[17] In another study conducted by Dhar and Kanwar,[14] 58% patients had aggravation in winters. In the included patients, 37% of the patients had history of associated asthma, 36% of the patients had history of associated atopy, and 42% had history of allergic rhinitis. According to Hanifin and Rajka,[6] personal history of atopy was found in 50% of patients with AD, while it was positive in 55% patients in the study by Roth and Kierland.[16] In another study, by Rystedt et al., 32% patients of AD also had bronchial asthma and 60% also had allergic rhinitis.[15] In a study by Ellis et al.,[18] among the most frequently occurring co-morbidities were allergic rhinitis seen in 7% patients with AD and asthma in 5% patients with AD. In another study Halbert et al.[19] reported that children with AD may have a strong personal history of atopy, to the tune of 50% to 80%. Dhar and Kanwar[14] in 672 children showed that in the childhood AD group, 15.35% had a personal history of atopy. Thus, it may be inferred from the above-mentioned findings that children with AD have a strong history of allergic rhinitis, asthma and atopy. Furthermore, 57% of the patients had family history of asthma and 14% of the patients had family history of AD. Family history of atopy varied in different series. It was 70% in a study by Hanifin and Rajka,[6] 60% in Roth and Kierlands,[17] 51% and 45% in two different groups of patients in the study by Rystedt et al.[18] Dhar et al.[20] found a family history of atopy in 40% of the patients. In another study by Dhar et al.,[11] 65% had positive family history of atopy of which 40% had family history of AD and 7% had asthma.
The minor features of Hanifin and Rajka[6] criteria commonly found in the included group were by xerosis and hand/foot dermatitis, white dermatographism and Dennie–Morgan infraorbital fold; 72% of patients had history of food intolerance; 70% had complaints of itch associated with sweating; 68% showed intolerance to wool and; 66% had a tendency to cutaneous infection and its course was influenced by emotional factors. 58% of the patients had cheilitis and orbital darkening; 50% showed ichthyosis or keratosis pilaris; 25% had history of recurrent conjunctivitis. 20% patients had nipple eczema and pityriasis Alba. The overt morphology correspond to that reported earlier.[15,16] Xerosis too was a frequently occurring minor feature. Interestingly, 45% had flexural and 30% extensors, while only 25% of the patients had facial involvement. These findings too are in conformity to those reported by Dhar et al.[11,15]
Mean serum IgE levels were 1084.73(± SD 776.27) with a minimum value of 72 IU/ml and maximum of 3000 IU/ml. Serum IgE levels were found to be raised above normal values in 92% patients in different age groups. Johnson et al.[21] have reported that total serum IgE level was elevated in 43% to 82% in AD patients. Akdis et al.[22] have also reported that serum IgE levels were elevated in about 80% of AD patients, who also showed sensitization against airborne and food allergens and/or concomitant respiratory allergy.
Severity of AD was assessed by SASSAD score. Its value ranged from a minimum of 9 to maximum of 56 with the mean value of 38.46 ± 12.69, and median value as 41.5. Correlation coefficient between SASSAD score and serum IgE value was 0.964, which is suggestive of a highly significant positive correlation between serum IgE levels and the severity of AD, P value = 0.000. Ohman and Johansson[23] and Wuthrich et al.[24] reported that serum IgE levels parallel well with the severity of the dermatitis. Stone et al.[25] also demonstrated that the levels of serum IgE correlate with the extent of the disease in terms of the anatomic extent of the dermatitis. Hence, it may be concluded that the levels of serum IgE are strongly correlated with the severity of AD.
What is new?
An endeavor to form the current demographic and clinical pattern of atopic dermatitis through cross sectional/descriptive study, has been made to highlight its under tones in tropics vis-a-vis to that in temprates, providing refreshing glimses into its ultimate management strategies.
Footnotes
Source of support: Nil
Conflict of Interest: Nil.
References
- 1.Sehgal VN, Srivastava G, Dogra S. Atopic dermatitis: Current options and treatment plans. Skinmed. 2010;8:335–44. [PubMed] [Google Scholar]
- 2.Staab D, Diepgen TL, Fartasch M, Kupfer J, Lob-Corzilius T, Ring J, et al. Age-related structured educational programmes for the management of atopic dermatitis in children and adolescents: Multicentre, randomised controlled trial. BMJ. 2006;332:933–8. doi: 10.1136/bmj.332.7547.933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anonymous Atopic eczema-new insights in the definition, diagnostics and disease management. Proceedings of a LEO eczema workshop. November 2003. Copenhagen, Denmark. Acta Derm Venereol Suppl (Stockh) 2005;215:7–48. [PubMed] [Google Scholar]
- 4.Anonymous Consensus Conference Management of atopic dermatitis in children. Recommendations (short version) Eur J Dermatol. 2005;15:215–23. [PubMed] [Google Scholar]
- 5.Ishizaka K, Ishizaka T, Hornbrook MM. Physicochemical properties of human reaginic antibody IV. J Immunol. 1997;1:75–85. [PubMed] [Google Scholar]
- 6.Hanifin JM, Rajka G. Diagnostic features of atopic dermatitis. Acta Derm Venereol. 1980;92:44–7. [Google Scholar]
- 7.Berth-Jones J. Six area, six sign atopic dermatitis (SASSAD) severity score: A simple system for monitoring disease activity in atopic dermatitis. Br J Dermatol. 1996;135:25–30. doi: 10.1111/j.1365-2133.1996.tb00706.x. [DOI] [PubMed] [Google Scholar]
- 8.Wittig HJ, Belloit J, De Fillippi I, Royal G. Age related serum IgE levels in healthy subjects and in patients with allergic disease. J Allergy Clin Immunol. 1980;66:305–13. doi: 10.1016/0091-6749(80)90026-3. [DOI] [PubMed] [Google Scholar]
- 9.De D, Kanwar AJ, Handa S. Comparative efficacy of Hanifin and Rajka's criteria and the UK working party's diagnostic criteria in diagnosis of atopic dermatitis in a hospital setting in North India. J Eur Acad Dermatol Venereol. 2006;20:853–9. doi: 10.1111/j.1468-3083.2006.01664.x. [DOI] [PubMed] [Google Scholar]
- 10.Eichenfield LF, Hanifin JM, Luger TA, Stevens SR, Pride HB. Consensus conference on pediatric atopic dermatitis. J Am Acad Dermatol. 2003;49:1088–95. doi: 10.1016/s0190-9622(03)02539-8. [DOI] [PubMed] [Google Scholar]
- 11.Dhar S, Mandal B, Ghosh A. Epidemiology and clinical pattern of atopic dermatitis in 100 children seen in a city hospital. Indian J Dermatol. 2002;47:202–4. [Google Scholar]
- 12.Dotterud LK, Kvammen B, Lund E, Falk ES. Prevalence and some clinical aspects of atopic dermatitis in the community of Sor-Varanger. Acta Derm Venereol. 1995;75:50–3. doi: 10.2340/00015555755053. [DOI] [PubMed] [Google Scholar]
- 13.Williams H, Robertson C, Stewart A, Ait-Khaled N, Anabwani G, Anderson R, et al. Worldwide variations in the prevalence of symptoms of atopic eczema in the International Study of Asthma and Allergies in Childhood. J Allergy Clin Immunol. 1999;103:125–38. doi: 10.1016/s0091-6749(99)70536-1. [DOI] [PubMed] [Google Scholar]
- 14.Dhar S, Kanwar AJ. Epidemiology and clinical pattern of atopic dermatitis in a North Indian pediatric population. Pediatr Dermatol. 1998;15:347–51. doi: 10.1046/j.1525-1470.1998.1998015347.x. [DOI] [PubMed] [Google Scholar]
- 15.Sarkar R, Kanwar AJ. Clinico-epidemiological profile and factors affecting severity of atopic dermatitis in north Indian children. Indian J Dermatol. 2004;49:117–22. [Google Scholar]
- 16.Roth HL, Kierland RR. The natural history of atopic dermatitis. A 20-year follow-up study. Arch Dermatol. 1964;89:209–14. doi: 10.1001/archderm.1964.01590260047008. [DOI] [PubMed] [Google Scholar]
- 17.Rystedt I. Prognostic factors in atopic dermatitis. Acta Derm Venereol. 1985;65:206–13. [PubMed] [Google Scholar]
- 18.Ellis CN, Drake LA, Prendergast MM, Abramovits W, Boguniewicz M, Daniel CR, et al. Cost of atopic dermatitis and eczema in the United States. J Am Acad Dermatol. 2002;46:361–70. doi: 10.1067/mjd.2002.120528. [DOI] [PubMed] [Google Scholar]
- 19.Halbert AR, Weston WL, Morelli JG. Atopic dermatitis: Is it an allergic disease? J Am Acad Dermatol. 1995;33:1008–18. doi: 10.1016/0190-9622(95)90295-3. [DOI] [PubMed] [Google Scholar]
- 20.Dhar S, Kanwar AJ, Nagaraja Personal and family history of atopy in children with atopic dermatitis in north India. Indian J Dermatol. 1997;42:9–13. [Google Scholar]
- 21.Johnson EE, Irons JS, Patterson R, Roberts M. Serum IgE concentration in atopic dermatitis. Relationship to severity of disease and presence of atopic respiratory disease. J Allergy Clin Immunol. 1974;54:94–9. doi: 10.1016/0091-6749(74)90037-2. [DOI] [PubMed] [Google Scholar]
- 22.Akdis CA, Akdis M, Bieber T, Bindslev-Jensen C, Boguniewicz M, Eigenmann P, et al. European Academy of Allergology and Clinical Immunology/American Academy of Allergy, Asthma and Immunology. Diagnosis and treatment of atopic dermatitis in children and adults: European Academy of Allergology and Clinical Immunology/American Academy of Allergy, Asthma and Immunology/PRACTALL Consensus Report. J Allergy Clin Immunol. 2006;118:152–69. doi: 10.1016/j.jaci.2006.03.045. [DOI] [PubMed] [Google Scholar]
- 23.Ohman S, Johansson SG. Immunoglobulins in atopic dermatitis with special reference to IgE. Acta Derm Venereol. 1974;54:193–202. [PubMed] [Google Scholar]
- 24.Wuthrich B, Benz A, Skvari F. IgE and IgG4 levels in children with atopic dermatitis. Dermatologica. 1983;166:229–35. doi: 10.1159/000249875. [DOI] [PubMed] [Google Scholar]
- 25.Stone SP, Muller SA, Gleich GJ. IgE levels in atopic dermatitis. Arch Dermatol. 1973;108:806–11. [PubMed] [Google Scholar]


