Abstract
A 30-year-old male presented to the dermatology department with complaints of multiple ulcers over both legs of 6 years duration. The ulcers had a waxing and waning course with present exacerbation of lesions since 1 month. Dermatological examination revealed multiple ulcers distributed in a reticular pattern over medial and lateral aspects of both lower legs, extensor aspect of both ankles and dorsum of both feet. Multiple interspersed atrophic porcelain white scars were also present. Investigations revealed raised serum homocysteine levels. A skin biopsy from the ulcers showed features of livedoid vasculopathy. Following recurrence of lesions after oral corticosteroid therapy, the patient was given a course of hyperbaric oxygen therapy for the ulcers to which he responded very well. This case is being presented for the novel option of hyperbaric oxygen therapy in livedoid vasculopathy, which by itself is rarely reported in this part of the world.
Keywords: Hyperbaric oxygen, livedoid vasculopathy, procoagulant, thrombosis
What was known?
Livedoid vasculopathy is a disorder of uncertain pathogenesis with prothrombotic causes being predominant
Anticoagulants, immunosuppressants and anti-inflammatory agents are prime candidates for inducing remission of livedoid ulcers.
Introduction
Livedoid vasculopathy (LV) is a rare cutaneous disease which manifests mainly as recurrent leg ulcers. These ulcers heal with atrophic, porcelain white scars called atrophie blanche, which is an alternative named used for the disease. Inflammation, autoimmunity and hypercoagulability are the main pathogenetic factors with the latter being the most predominant among them. The treatment is controversial with antithrombotic measures taking precedence over the others. The recurrent nature and controversial pathogenesis makes this disorder a very challenging one to treat. We herein report a case of LV associated with hyperhomocysteinemia which responded well to hyperbaric oxygen therapy (HBOT), thus providing a novel, efficient and safe option for management.
Case Report
This 30-year-old male presented with complaints of multiple ulcers over both legs of 6 years duration. The patient gave history of initially developing few ulcers on the left foot after prolonged wearing of boots for duration of 7 days (18 hours/day). He progressively developed similar multiple ulcers over both lower legs and dorsum of feet over a duration of 2 weeks. They were associated with moderate intensity pain and would increase on walking or running and reduce with rest. The ulcers had a waxing and waning course and would generally heal with course of antibiotics and rest. Presently he had exacerbation of lesions since 1 month. There were no other associated complaints or history of any other risk factors.
General and systemic examination was essentially normal. Dermatological examination revealed multiple ulcers distributed in a reticular pattern over medial and lateral aspects of both lower legs, extensor aspect of both ankles and dorsum of both feet [Figure 1]. Multiple atrophic porcelain white scars were also present in the interspersed and adjoining regions along with post inflammatory hyperpigmentation. Ulcers had well-defined margins, sloping edges and the floor had granulation tissue with no discharge [Figure 2]. They were mildly tender to touch. Arterial pulsations were normal in both lower limbs. Ankle brachial pressure index was normal.
Figure 1.
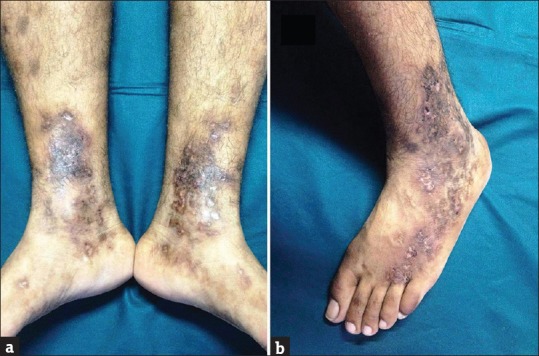
Distribution of ulcers on: (a) the medial aspect of both legs and feet. (b) Lateral aspect of dorsum of left feet and leg
Figure 2.
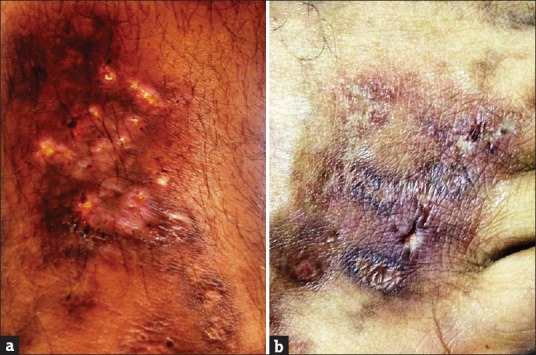
Close up images revealing (a) livedoid ulcers on leg long with atrophie blanche and (b) reticulate pattern of ulcers on dorsum of foot
Investigations revealed normal hemogram, liver and renal function tests. C-reactive protein was raised. Antinuclear antibodies, hepatitis B surface antigen (HbsAg), anti-Hepatitis C, VDRL and HIV testing were all negative. Antineutrophil cytoplasmic antibodies (ANCA), antiphospholipid antibodies (APLA), protein C and S, antithrombin III, factor V Leiden, prothrombin gene mutation and methylene tetrahydrofolate reductase (MTHFR) gene polymorphisms were all negative. Serum homocysteine levels were raised (24.6 μmol/L). Chest X-ray, ECG and USG abdomen were normal. CDFI of both arterial and venous systems were normal. A skin biopsy from the ulcers revealed ulcerated epidermis with intervening orthokeratotic epidermis, mild acanthosis and spongiosis. Extensive congestion of vessels and extravasation of RBCs was present. Most of the vessels showed thickened walls with fibrin deposition and thrombus formation [Figure 3]. With these features a diagnosis of LV with associated homocystenemia was made.
Figure 3.
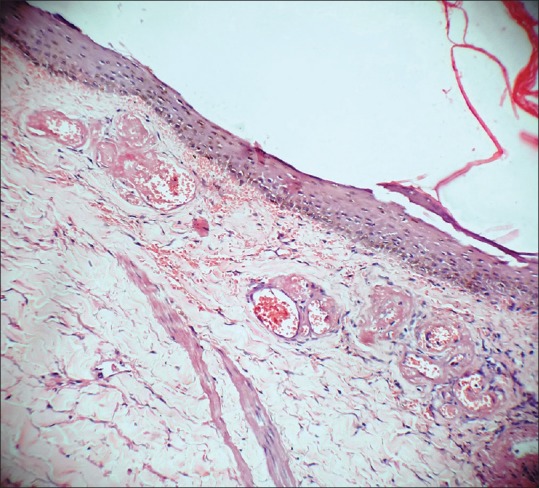
Histopathology revealing extensive fibrin deposition and thrombus formation in the dermal vessels with absent inflammation [hematoxylin and eosin stain – ×10]
He was prescribed oral prednisolone 60 mg along with, pentoxyphylline, low-dose aspirin, folic acid and local cleaning of ulcers with normal saline. The ulcers were non-healing even after 12 weeks of therapy. Oral prednisolone was stopped. In view of contradictory evidence for anticoagulants and immunosuppressants, patient was given a course of HBOT for the ulcers along with continuation of pentoxyphylline, aspirin and folic acid.
The patient was administered HBOT in a multiplace chamber at pressure of 2.5 atmospheres for 90 min daily, 6 days a week. At the end of 10 sittings of HBOT, the patient reported a reduction in the pain. Ulcers in the feet and ankles showed signs of healing in the form of appearance of granulation tissue in the base, shrinking margins, reduced inflammation and reduced tenderness. By the end of 15 sittings, the ulcers had completely healed and the patient could walk comfortably without any analgesic. The patient was followed up for 1 year during which no recurrence of ulcers was noted.
Discussion
LV is presently described as a condition manifesting as recurrent leg ulcers with thrombosis of the microcirculation as the main pathogenesis. The important procoagulant causes include hyperhomocysteinemia, proteins C and S deficiency, factor V Leiden mutation, prothrombin gene mutation, antithrombin III deficiency and antiphospholipid antibody syndrome.
Hyperhomocystenemia can either be genetic or acquired. The genetic causes of homocystenemia are mainly due to enzyme defects such as cystathione-β-synthase, methylenetetrahydrofolate reductase and methionine synthase deficiencies. Acquired causes include nutritional deficiencies, renal failure, use of folic acid and vitamin B6 antagonists, cardiovascular diseases and peripheral arterial occlusive disease. Folic acid, vitamin B6/B12 are the most common nutritional deficiencies associated with homocystenemia. Serum homocysteine levels higher than 5–15 μmol/L have been found to correlate more with LV.[1]
HBOT is a recognized modality of treatment of various problem wounds and non-healing ulcers due to various etiologies. The non-healing ulcers form the single largest group of indications for which HBOT is being administered. This group includes various indications like diabetic foot ulcers, arterial insufficiency ulcers, ulcers due to venous stasis, decubitus ulcers and fungal infections.[2] These disorders have a common pathology in having ischemia and infection as the most common causes of non-healing.[3]
Hyperbaric oxygen acts by delivering 100% oxygen at high pressures (2-3 atmospheres pressure) wherein oxygen dissolves 20 times more in plasma and tissue fluids than at room air pressure.[4] Therefore, a high oxygen gradient is produced across the wound site negating the damaging effects of tissue ischemia. It also increases the release of fibrinolytics from endothelial cells, promotes angiogenesis of ischemic tissue and facilitates neovascularization, thereby accelerating healing in LV.[5,6,7] Other proposed mechanisms include increased collagen formation, inhibition of bacterial overgrowth and reduced tissue reperfusion injury.[8,9]
Contraindications for HBOT include previous chest or ear surgery, pregnancy, seizures, malignancy, pneumothorax, emphysema and upper respiratory tract infections. So chest X-ray, pulmonary function tests, and eardrum examination are a must before starting therapy. Severe adverse effects are very rare and middle ear barotraumas are the most common reported adverse effects.
Our patient had LV associated with homocystenemia and he showed very good response to HBOT. LV itself has been very rarely reported from India and few reports globally have reported use of HBOT for LV.[10,11] HBOT therapy is therefore a novel, relatively cost-effective, OPD treatment option in LV. It is probably not only a means of therapy for healing the ulcers, but also to get longer recurrence free periods.
What is new?
Hyperbaric oxygen therapy is a novel, safe and beneficial therapy for livedoid vasculopathy
Hyperbaric oxygen therapy can not only help in healing ulcers, it can also help in prolonging remission periods in such cases.
Footnotes
Source of support: Nil
Conflict of Interest: Nil.
References
- 1.Meiss F, Marsch WC, Fischer M. Livedoid vasculopathy. The role of hyperhomocysteinemia and its simple therapeutic consequences. Eur J Dermatol. 2006;16:159–62. [PubMed] [Google Scholar]
- 2.Kalani M, Jorneskog G, Naderi N, Lind F, Brismar K. Hyperbaric oxygen (HBO) therapy in treatment of diabetic foot ulcers. Long-term follow-up. J Diabetes Complications. 2002;16:153–8. doi: 10.1016/s1056-8727(01)00182-9. [DOI] [PubMed] [Google Scholar]
- 3.Mathieu D. Role of hyperbaric oxygen therapy in the management of lower extremity wounds. Int J Low Extrem Wounds. 2006;5:e233–5. doi: 10.1177/1534734606294450. [DOI] [PubMed] [Google Scholar]
- 4.Tibbles PM, Edelsberg JS. Hyperbaric-oxygen therapy. N Engl J Med. 1996;334:1642–8. doi: 10.1056/NEJM199606203342506. [DOI] [PubMed] [Google Scholar]
- 5.Tjarnstrom J, Holmdahl L, Falk P, Falkenberg M, Arnell P, Risberg B. Effects of hyperbaric oxygen on expression of fibrinolytic factors of human endothelium in a simulated ischaemia/reperfusion situation. Scand J Clin Lab Invest. 2001;61:539–45. doi: 10.1080/003655101753218300. [DOI] [PubMed] [Google Scholar]
- 6.Pizzo SV, Murray JC, Gonias SL. Atrophie blanche. A disorder associated with defective release of tissue plasminogen activator. Arch Pathol Lab Med. 1986;110:517–9. [PubMed] [Google Scholar]
- 7.Heng MC, Harker J, Csathy G, Marshall C, Brazier J, Sumampong S, et al. Angiogenesis in necrotic ulcers treated with hyperbaric oxygen. Ostomy Wound Manage. 2000;46:30–2. [PubMed] [Google Scholar]
- 8.Tompach PC, Lew D, Stoll JL. Cell response to hyperbaric oxygen treatment. Int J Oral Maxillofac Surg. 1997;26:82–6. doi: 10.1016/s0901-5027(05)80632-0. [DOI] [PubMed] [Google Scholar]
- 9.Zamboni WA, Roth AC, Russell RC, Graham B, Suchy H, Kucan JO, et al. Morphologic analysis of the microcirculation during reperfusion of ischemic skeletal muscle and the effect of hyperbaric oxygen. Plast Reconstr Surg. 1993;91:1110–23. doi: 10.1097/00006534-199305000-00022. [DOI] [PubMed] [Google Scholar]
- 10.Yang CH, Ho HC, Chan YS, Liou LB, Hong HS, Yang LC. Intractable livedoid vasculopathy successfully treated with hyperbaric oxygen. Br J Dermatol. 2003;149:647–52. doi: 10.1046/j.1365-2133.2003.05546.x. [DOI] [PubMed] [Google Scholar]
- 11.Juan WH, Chan YS, Lee JC, Yang LC, Hong HS, Yang CH. Livedoid vasculopathy: Long-term follow-up results following hyperbaric oxygen therapy. Br J Dermatol. 2006;154:251–5. doi: 10.1111/j.1365-2133.2005.06843.x. [DOI] [PubMed] [Google Scholar]


