Abstract
Histoid leprosy is an uncommon entity with specific clinical, histopathological and bacteriological features. Histoid lepromas are sudden eruption of dome shaped lesions usually associated with dapsone resistance, as a variant of lepromatous leprosy or rarely arising de novo. We report a case who presented for the first time with histoid features with no history of taking dapsone/antileprosy treatment earlier in an elderly male with small to large lesions over normal skin in the post-leprosy elimination era.
Keywords: Histoid leprosy, de novo, Multi drug therapy
What was known?
Histoid leprosy is known to occur in patients on anti – leprosy treatment or as a variant of lepromatous leprosy.
Introduction
Histoid leprosy is a well-recognized entity. It usually occurs in lepromatous patients, after dapsone monotherapy or rarely as de novo. It is characterized by cutaneous or subcutaneous nodules and plaques present over apparently normal skin, with unique histopathological and characteristic bacterial morphology. The term “Histoid leprosy” was originally coined by Wade as a histological concept of bacillary-rich leproma composed of spindle-shaped cells, along with the absence of globus formation (so conspicuous in ordinary leproma). It exhibits a fibromatoid tendency in the chronic form.[1] It occurs in lepromatous patients who relapse after the dapsone monotherapy in presence of dapsone resistance or rarely de novo and occasionally seen in unstable borderline and intermediate type of leprosy too. Responsible factors may include: Resistance to dapsone, irregular and inadequate therapies or mutant organism Histoid bacillus. Since then, there have been many reports, with variable findings.[2] We report here a case of de novo histoid leprosy in a 50 year old male, presented with itching and sudden eruption of multiple shiny nodules as main symptoms.
Case Report
A 50 year old male labourer, presented with complaints of multiple nodules and papules associated with itching distributed over generalized body area and bony prominences of elbow and knee joint since 3 months duration [Figure 1a and b]. There was history of fever associated with similar nodular eruption 1 year back which subsided on its own leaving behind hyperpigmentation at few areas. He also had complaints of tingling numbness with joint pain over lower limb and generalized weakness on and off since 1 year. No history of epistaxis and pedal edema.
Figure 1.

Multiple grouped shiny nodules over bony prominences. (a) Elbow joint. (b) Knee joint
No family history and contact history with known case of leprosy. General physical and systemic examinations were within normal limits. On dermatological examination, there were multiple grouped skin-colored, well-demarcated, shiny, non-tender nodules, firm to soft in consistency measuring from 0.5 to 1cm over lower back, upper back, elbow and knee joint [Figure 2]. Bilateral ulnar nerves and right common peroneal nerve were thickened, non-tender.
Figure 2.

Multiple well-demarcated, skin colored, grouped shiny nodules on a normal appearing skin over the back
No lymphadenopathy, muscle weakness/wasting and trophic ulcer was present. Investigation revealed high blood sugar levels of 453 mg% and slight leukocytosis in blood picture. ELISA for HIV and VDRL was negative. Slit skin smear done by Ziehl-Neelsen stain revealed plenty of acid-fast bacilli occuring singly or in clusters, they appeared as uniform solid stained, long rods with tapering ends, with a bacterial index of 6 + and morphological index of >70% [Figure 3]. Histopathology of lower back nodule shows thinned out epidermis, presence of grenz zone and plenty of vacuolated macrophages, lymphocytes and histiocytes which are spindle shape arranged in storiform pattern in the dermis [Figure 4a and b]. The patient has been put on multibacillary multidrug therapy (MBMDT) and is on regular follow-up.
Figure 3.
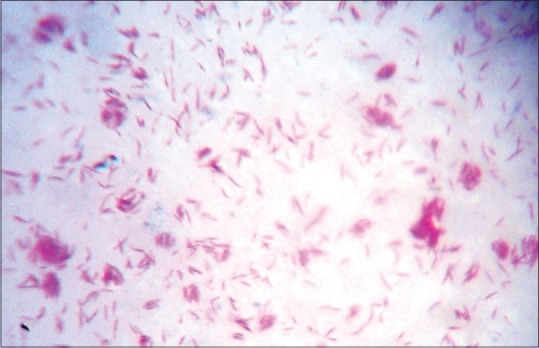
ZN stain showing uniform solid stained AFB with tapering ends, bacterial index of 6+ and morphological index >70%
Figure 4.
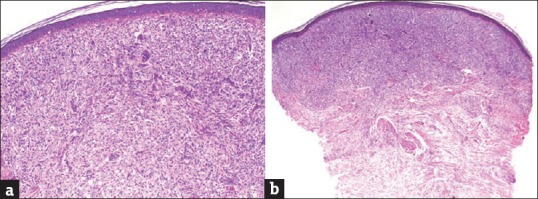
thinned out epidermis, presence of grenz zone and plenty of histiocytes which are spindle shape arranged in storiform pattern in the dermis (H and E Stain) (a) 10 ×. (b) 4 ×
Discussion
Histoid leprosy is considered a variant of lepromatous leprosy[2] and by others as a distinct entity.[3] The incidence in India has been reported to vary from 2.79 to 3.60% among total leprosy patients.[2] There is male preponderance and the average age at diagnosis is between 21 and 40 years.[4] Clinically, it is characterized by cutaneous or subcutaneous nodules and papules, which are painless, firm, discrete, smooth, globular, skin colored to yellowish brown, with apparently normal skin surrounding it. The lesions are usually located on the posterior and lateral aspects of the arms, buttocks, thighs, dorsum of the hands, lower part of the back, and over the bony prominences, especially over elbows and knees.[2] Classical histopathologic findings include epidermal atrophy as a result of dermal expansion by the underlying leproma and an acellular band located immediately below the epidermis. The leproma consists of fusiform histiocytes arranged in a tangled or storiform pattern containing acid fast bacilli.[5] AFB are uniform solid stained and longer than normal bacilli with the absence of globi. There are three histologic variants of histoid hansen: Pure fusocellular, fusocellular with epitheloid component and fusocellular with vacuolated cells. The third pattern is most commonly observed.[6] Clinically, histoid leprosy may mimic lepromatous leprosy or ENL reaction. However, specific histopathology of histoid leprosy differentiates it from LL type which shows macrophage granuloma with variable amount of foamy changes with innumerable bacilli and globi and ENL reaction which shows features of acute inflammation predominantly having neutrophils accompanied by edema along with granular AFB. Histoid leprosy might represent an enhanced response of the multibacillary disease in localizing the disease process. An increase in both cell-mediated and humoral immunity against Mycobacterium leprae, as in lepromatous leprosy, has been hypothesized.[7] Histoid leprosy is managed initially by administering ROM therapy once, followed by MDT for 2 years.[5,8,9] Today, only 1 year of therapy is recommended for multibacillary forms and attempts are being made to further reduce the duration. However, whether histoid should be treated as other multibacillary forms or other immunotherapies should be added to the treatment regimen deserves consideration.
Conclusion
Being a rare entity patient presenting with sudden eruption of multiple shiny nodules and papules over normal looking skin with no history of taking anti-leprosy treatment diagnosis of “de novo histoid leprosy” should be kept in mind and can be confirmed by its unique histopathological and bacteriological features.
What is new?
Histoid leprosy with no previous history of taking anti-leprosy treatment should be diagnosed as De novo case and MBMDT should be initiated with regular follow up.
Acknowledgement
The authors would like to acknowledge and thank Dr. Uday Khopkar for histopathological report and granting permission for publication.
Footnotes
Source of support: Nil
Conflict of Interest: Nil.
References
- 1.Sehgal VN, Srivastava G, Singh N, Prasad PV. Histoid leprosy: The impact of the entity on the postglobal leprosy elimination era. Int J Dermatol. 2009;48:603–10. doi: 10.1111/j.1365-4632.2009.03992.x. [DOI] [PubMed] [Google Scholar]
- 2.Annigeri SR, Metgud SC, Patil JR. Lepromatous leprosy of histoid type. Indian J Med Microbiol. 2007;25:70–1. doi: 10.4103/0255-0857.31069. [DOI] [PubMed] [Google Scholar]
- 3.Shaw IN, Ebeneger G, Rao GS, Natarajan MM, Balasundaram B. Relapse as histoid leprosy after multidrug receiving therapy (MDT): A report of three cases. Int J Lepr Other Mycobact Dis. 2000;68:272–6. [PubMed] [Google Scholar]
- 4.Wade HW. The histoid variety of lepromatous leprosy. Int J Lepr. 1963;31:129–42. [PubMed] [Google Scholar]
- 5.Sehgal VN, Srivastava G. Histoid leprosy A Review. Int J Dermatol. 1985;24:286–92. doi: 10.1111/j.1365-4362.1985.tb05783.x. [DOI] [PubMed] [Google Scholar]
- 6.Mendiratta V, Jain A, Chander R, Khan A, Barara M. A nine-year clinico-epidemiological study of histoid Hansen in India. J Infect Dev Ctries. 2011;5:128–31. doi: 10.3855/jidc.1190. [DOI] [PubMed] [Google Scholar]
- 7.Kalla G, Purohit S, Vyas MC. Histoid, a clinical variant of multibacillary leprosy: Report from so called endemic areas. Int J Lepr Other Mycobact Disease. 2000;68:267–71. [PubMed] [Google Scholar]
- 8.Sehgal VN, Aggarwal A, Srivastava G, Sharma N, Sharma S. Evolution of histoid leprosy (de novo) in lepromatous (multibacillary) leprosy. Int J Dermatol. 2005;44:576–8. doi: 10.1111/j.1365-4632.2004.02540.x. [DOI] [PubMed] [Google Scholar]
- 9.Kaur L, Dogra S, De D Saikia UN. Histoid leprosy: A retrospective study of 40 cases from India. Br J Dermatol. 2009;160:305–10. doi: 10.1111/j.1365-2133.2008.08899.x. [DOI] [PubMed] [Google Scholar]


