Abstract
The purpose of this study was to explore whether differences in patterns of weight control strategies predict 4 year weight change among women. Participants (N = 176), were assessed at baseline and biennially on 3 occasions. Weight control strategies were assessed by the Weight Loss Behavior Scale. Height and weight were measured to calculate BMI. Latent class analysis (LCA) identified groups of women differing in their reported weight control strategies. Repeated measures were employed to examine the relationship between using different types of weight control strategies and weight change before and after adjusting for education, income, and initial BMI. LCA yielded a three group solution: use of none (N); healthy (H); and healthy plus unhealthy (H+U) weight control strategies. The N group had the lowest initial BMIs. Women’s pattern of weight gain differed by latent group membership after adjusting for covariates: H+U group gained significantly more weight (4.56 kg) than the N group (1.51 kg) and H group (1.02 kg). Similar patterns emerged predicting weight change between years 2 and 4: H+U group gained significantly more weight (2.86 kg) than the H group (0.03 kg) and N group (0.44 kg). H+U weight control group had higher scores on weight concerns, dietary restraint, and eating attitudes than women in the H or N groups. Findings provide evidence that self-reported weight control attempts do not necessarily lead to large weight gains; rather the amount of weight gain may depend on the type of weight control strategies that women are practicing.
Keywords: weight maintenance, dieting, weight control, weight gain, women
INTRODUCTION
Dieting to lose weight is common among women of all ages and body weights; in 2000, 46% of American women reported currently dieting to lose weight (1). Despite current preoccupation with weight loss and dieting, obesity continues to be a major public health issue; approximately 60% of adults in the United States are now overweight or obese (2). Longitudinal studies estimate that on average adults gain 0.5-1.0 kg per year (3, 4), which, over time, increases risk of obesity and many leading causes of morbidity and mortality (5). While a major public health objective is to identify factors associated with successful weight maintenance, few longitudinal studies have examined the influence of the use of specific strategies for weight control on patterns of weight change during adulthood.
For successful weight loss, both the U.S. Department of Health and Human Services Dietary Guidelines (6) and The National Heart, Lung, and Blood Institute (7) recommend balancing calories from food with energy expenditure or making small decreases in food and beverage calories and increasing physical activity. Results from the few longitudinal studies that have examined the effect of self-reported dieting on weight change reveal that dieting may not be an effective weight maintenance strategy (8-10). For example, Lowe and colleagues (8) reported that a history of dieting predicted greater weight gain and that women who self-reported that they were currently dieting to lose weight gained three times as much weight as non-dieters. However, in that research, women did not provide information regarding the specific strategies they were using when dieting.
In one study (10) that examined the independent effects of specific weight control strategies on weight change in adults recruited from a weight gain prevention study, French and colleagues reported that although self reports of dieting to lose weight were not significantly related to weight change, specific weight control strategies including calorie reduction, increasing fruit and vegetable intake, fat reduction, eliminating sweets and reducing the amount of food eaten were associated with gaining less weight over 4 years. However, little is known about the long term combined effects of using different patterns of self-initiated weight control strategies on weight change among free-living women, and such information could inform the development of recommendations promoting weight maintenance.
The primary aim of this research was to use latent class analysis to examine whether distinct combinations of specific weight control strategies, reported using the Weight Control Scale (11), are associated with different patterns of weight change over 4 years in women. A secondary aim was to examine latent class membership differences in body weight, dietary restraint and disinhibition, disordered eating and body image. Based on previous research (8, 11-14), we hypothesized that 1) use of healthy weight control strategies would be common, but a small percentage of women would report engaging in unhealthy weight control; 2) women using weight control strategies would report greater body dissatisfaction and weight concerns than non-users; and 3) unhealthy weight control efforts would be ineffective, with individuals using unhealthy weight control strategies gaining more weight over time compared to non-users.
METHODS AND PROCEDURES
Participants
Participants included 183 non-Hispanic white women living in central Pennsylvania recruited as part of a longitudinal study designed to examine parental influences on girls’ growth and development; the sample was not recruited based on weight status. Only data for mothers are considered in this study. At time 1, participants included 183 women, of whom 177 and 168 women were reassessed at time 2 and time 3, respectively, representing a 92% retention rate. Attrition was primarily due to family relocation outside of the study area. Women who were missing weight control strategy data at 2 or more time points, were excluded from all analyses, leaving a final sample of (n = 176).
Design and Procedures
Data were collected on three occasions of measurement across a 4-year period, with 2-year intervals between assessments. At each time of assessment, women completed a series of self-report questionnaires during a scheduled visit to the laboratory. The Pennsylvania State University Institutional Review Board approved all study procedures, and women provided consent for their family’s participation in the study before the initiation of data collection. Background characteristics and correlates of weight control strategies were collected at study entry; height and weight were collected at all three occasions. At time 2, data on the use of specific weight control strategies during the previous two years were collected; these data were used in the LCA analyses to examine associations with different patterns of weight change over the study period.
Measures
Background characteristics
Women completed a Background Questionnaire that assessed family background characteristics including combined family income and mothers’ and fathers’ years of education at study entry. In addition, women retrospectively reported on their weight as a child using a 3-point scale: 1 = underweight; 2 = average weight; and 3 = overweight.
Weight and body mass index (BMI)
Height and weight measurements were assessed in triplicate at each occasion by a trained staff member following the procedure outlined by Lohman and colleagues (15). Average height and weight were used to calculate body mass index [BMI;weight (kg)/height (m)2]. Recommendations made by the World Health Organization (16) were used to classify women as overweight (BMI = 25-29.9) and obese (BMI ≥ 30). Finally percent weight change over 4 years was calculated by taking the difference between Time 1 and Time 3 body weight (kg) and dividing by Time 1 body weight. Weight maintenance was defined as a weight change of ≤ 3% of initial body weight (17).
Weight control strategies
Weight control strategies were assessed using an amended version of the Weight Loss Behavior Scale (11). This measure consists of 24 items assessing the use of a set of specific weight control strategies used to lose or maintain weight during the past 2 years (Refer to Table 1 for example items). Items are measured on a 5-point response scale ranging from 1 (never) to 5 (always). Principal component analysis was conducted to gain insight into the dimensionality of the revised measure in the current sample. Examining loading values, the scree plot, eigenvalues, and the interpretability of the factor solution (18) revealed a healthy weight control factor (11 items) and relatively harmful or unhealthy weight control factor (9 items), similar to the healthy and unhealthy weight control factors reported by French and colleagues (11). Item loadings ranged from 0.36 to 0.86. Items that did not load on either factor (decreasing alcohol intake, attending weight loss groups, vomiting, and “other” weight control strategies) were dropped from further consideration. Internal consistency for the healthy and unhealthy factor were α=0.94 and α=0.73, respectively. Lastly, dichotomous indicators of the remaining 20 weight control strategies were created for the current study, coded two if they have engaged in the behavior in the past two years and one if they have not. These items were used as indicators of weight loss strategies latent classes.
Table 1.
Percent and Probabilities of Women (N=176) of Endorsing each Specific Weight Control Strategy given Latent Class Membership
| Latent Class | ||||
|---|---|---|---|---|
|
| ||||
| Percent reporting Yes | Non-Users (N) (21%) | Healthy Users (H) (43%) | Healthy + Unhealthy Users (H+U) (35%) | |
| Healthy weight control strategies
| ||||
| Reduce calories and amount of food | 76% | 0.03 | 0.94 | 1.00 |
| Eliminate sweets/junk food/snacks | 76% | 0.14 | 0.89 | 1.00 |
| Increasing exercise | 74% | 0.22 | 0.88 | 0.86 |
| Eat more fruit & vegetables | 72% | 0.13 | 0.83 | 0.95 |
| Eat less fat | 71% | 0.08 | 0.81 | 1.00 |
| Change type of foods eaten | 59% | 0.06 | 0.65 | 0.86 |
| Eat less high-CHO foods | 43% | 0.03 | 0.45 | 0.66 |
| Eat less meat | 28% | 0.02 | 0.24 | 0.52 |
|
| ||||
| Extreme or Unhealthy weight control strategies
| ||||
| Skipping meals | 51% | 0.11 | 0.36 | 1.00 |
| Use of diet pills, liquid diets, appetite suppressants | 21% | 0.03 | 0.18 | 0.38 |
| Fasting | 19% | 0.00 | 0.05 | 0.55 |
| Use of laxatives, enemas, diuretics | 3.4% | 0.00 | 0.01 | 0.09 |
Notes: Principal components factor analysis was performed to identify subscales of weight control strategy; Practicing a healthy weight control strategy was identified when responding 3 (sometimes); Practicing an unhealthy or extreme weight control strategy was identified when responding 2 (rarely) or greater.
Weight concerns
An amended version of the Weight Concern Scale (19) was used to measure fear of weight gain, worry over weight and body shape, importance of weight, diet history, and perceived fatness at study entry. An average weight concerns score was created by calculating the mean of all 5 items. In the current study, internal consistency score of weight concerns was 0.83.
Restraint and disinhibition
The Eating Inventory (EI) developed by Stunkard and Messick (20) was used to assess dietary restraint (21 items) and dietary disinhibition (16 items) at study entry. The restraint scale measures cognitive control of eating (e.g. “I consciously hold back at meals in order not to gain weight”). The dietary disinhibition scale measures loss of cognitive control of eating (e.g. “Sometimes when I start eating, I just can’t seem to stop”). Scores for each subscale are calculated by summing respective items. Internal consistency coefficients for restraint and disinhibition subscales were both 0.83.
Eating Attitudes Test (EAT)
The EAT is a 26-item self-report instrument that assesses maladaptive or problematic eating attitudes and behaviors at study entry. A higher score is representative of more problematic or maladaptive eating attitudes and a cutoff of 20 is indicative of eating disorder pathology. In the current study, the internal consistency score of the EAT was good (α =.78).
Body satisfaction
The Body Figures Rating Scale developed by Stunkard, Sorenson and Schulsinger measures perceptions about body size and is made up of nine body figures varying in shape (21). The figures are numbered and placed in order and participants are asked to indicate the figure that represents their ideal self and the figure that represents their actual self. The difference between these ratings is a discrepancy score that is considered to represent the individual’s level of body satisfaction.
Statistical Analyses
Data were analyzed using the SAS software (version 9.1, 2001, SAS institute, Cary NC) (22). Descriptive information was generated for all variables of interest. Both predictor and outcome variables were assessed for normality.
Model specification
Latent class analysis was used to identify a set of discrete, mutually exclusive latent groups of individuals based on their reported weight control strategies. A detailed description of this procedure is described elsewhere (23, 24). Briefly, the goal of latent class analysis (LCA) is to identify the minimum number of “latent” groups that describe the association among “manifest” variables (specific weight control strategies). LCA estimates two sets of parameters: the prevalence of each group (latent group membership probability) and the probability of endorsing each specific weight control strategy given membership in a certain group (item-response probabilities).
In order to reduce sparseness in the observed data contingency table, which is particularly important with a sample of this small size, exploratory factor analysis (18) was conducted on the 20 binary indicators of healthy and unhealthy weight control strategies. These results suggest individual weight loss strategies that can be combined with others in the latent class model without much loss of information. Specifically, 10 weight control strategies were aggregated into 4 super ordinate strategies including: 1) eliminating sweets, junk food, and snacks; 2) reducing the amount of food consumed, calories, and eating low-calorie foods; 3) use of diet pills, liquid diets, and appetite suppressants; and 4) use of laxatives or enemas and diuretics. Ten items that did not load on any primary factors, such as eating more fruits and vegetables, were retained as unique latent class indicators. The final set of 14 super ordinate weight control strategy indicators (eight healthy and six unhealthy weight control strategies) were used to create latent classes.
The best fitting model was determined using three criteria. The first is using the G2 fit statistic. The second is examining the Bayesian Information Criteria (BIC) and Akaike Information Criterion (AIC). The third criterion was the interpretability of the estimated parameter results: measurement parameter estimates that were close to zero and one, signaling non-random responses to indicators, and latent status membership estimates that were not too small were desired. Indicators were removed from the final model if they did not discriminate between latent groups. Once a final model was selected, each individual was assigned to the latent group corresponding to their maximum posterior probability of membership. Latent group membership was then used to assess differences among weight control groups on measures of continuous and categorical data using ANOVA with Tukey HSD pos hoc tests and Chi-Square tests. Finally, latent group membership was used to examine whether differences among weight control groups are associated with different patterns of weight change using repeated measures mixed effect models.
Longitudinal Analyses: Predicting Patterns of Weight Change over Time
For the primary analyses of interest, a mixed modeling approach (Proc MIXED) was used to examine the association between using different types of weight control strategies and change in body weight (kg) over 4 years. Mixed modeling is a useful tool for analyzing repeated measures over time, and a major advantage is its ability to retain cases with one or more missing data points (25). Determination of model fit was based on several criteria: (1) model convergence, (2) a positive definite G matrix and (3) statistical fit comparison based on the Akaike Information Criteria (AIC) (26). An unstructured covariance matrix was selected, as determined by the aforementioned model fit criteria. The main effect of time, main effect of weight control group, and weight control group by time interaction were tested to examine associations with patterns of weight change. In addition, a three-way interaction among BMI category (normal versus overweight), weight control group, and time (after including all relevant main effects and 2-way interactions) was tested to examine whether the association between weight control group and time would vary across normal and overweight women. All models adjusted for initial BMI, education and income level based on associations between socioeconomic status and weight as well as evidence that women who use weight control strategies are often heavier than non-users (11, 12, 27). In all models, the inclusion of the interaction of weight control group by time provided a test of the major hypothesis, as a significant interaction effect provides evidence for a differential pattern of change over time for women using weight control strategies. Lastly, general linear models (Proc GLM) were used to compare mean differences among weight control groups on weight change from Time 2 to Time 3 after adjusting for income, education, initial BMI, and recent weight change (weight change from Time 1 to Time 2).
RESULTS
Descriptive Characteristics
Mean age of women at study entry was 39.5 (± 4.8) ranging from 28.0 to 50.7 years. Women were in general well-educated, with a mean of 14.8 (± 2.3) years of education and approximately an equal proportion of families at entry into the study reported incomes below $35,000, between $35,000 and $50,000, and above $50,000. On average, women were slightly overweight (BMI: M = 27.38, SD = 6.3). Of the 176 participants, 54 (31%) were classified as overweight (BMI = 25-29.9) and 47 (27%) were obese (BMI ≥ 30) at baseline.
Prevalence of Reported Weight Control Strategies
Table 1 shows the percentage of women using specific weight control strategies. Reported use of healthy weight control practices was common; more than 50% of women reported using each healthy strategy, with the exception of eating less meat and less carbohydrates. Elimination of sweets and junk food, increased exercise, increased fruit and vegetable intake, and decreased fat intake were most common, reported by more than 70% of women. Weight control strategies that were considered unhealthy or harmful were not frequently reported, with the exception of skipping meals.
Identifying groups differing in probability of using weight control strategies - Selection of LCA model
One- to five-group solutions were investigated. The first set of models included all 14 indicators; however, parameter estimates for cigarette smoking and attending diet centers were not close to 0 or 1, so these items were removed from the final model. The three group model was the best fitting model. As shown in Table 1, the parameter estimates indicated that the groups are distinguishable and nontrivial, and meaningful labels could be assigned to each. For example, 21% of women were predicted to belong to the Non-user (N) group, defined by not using any weight control strategies; these individuals were not expected to endorse any weight control strategies. The largest of the three groups was the Healthy (H) Weight Control group (43%). Among the Healthy group, 81% to 93% were predicted to endorse 1) reducing caloric intake and amount of food eaten; 2) eliminating snacks, sweets, and junk food; 3) increased exercise; 4) increased fruit and vegetable intake; and 5) decreasing fat intake; this group was not expected to endorse unhealthy weight control strategies. The third group was the Healthy plus Unhealthy (H+U) weight control group (35%); this group had very high probabilities of endorsing all 12 weight control strategies. For example, 100% of these women were expected to 1) endorse decreasing fat intake; 2) reduce caloric intake and amount of food consumed; 3) eliminate sweets, snacks, and junk food; and 4) skipping meals. In addition, the probability of the H+U group to endorse fasting was 55% and the probability of endorsing the use of diet pills, liquid diets, and appetite suppressants for weight control was 38%.
Cross Sectional Analyses: differences among weight control strategy groups
Table 2 displays descriptive statistics for all background, correlates of weight control use, and outcome variables at study entry for the total sample and by latent weight control strategy group. At baseline, weight control groups did not differ on measures of socioeconomic status or age; however, the N group had significantly lower initial body weight and BMI compared to women using H or H+U weight control strategies. Women in the N group also reported being more underweight as a child than the H or H+U groups. In addition, women practicing H+U strategies had significantly higher scores on weight concerns, dietary restraint, and problematic eating attitudes than either the H or N groups. H and H+U groups also had higher dietary disinhibition and body dissatisfaction scores than the N group. Finally, N women reported significantly lower weight concerns, dietary restraint, dietary disinhibition, and body dissatisfaction than either the H or H+U groups. Similar patterns emerged after adjusting for initial BMI, with the exception that weight control groups no longer differed on dietary disinhibition or body dissatisfaction.
Table 2.
Descriptive Characteristics and Covariates for the Total Sample and Weight Control Strategy Groups at study entry 1
| Latent Class | ||||
|---|---|---|---|---|
|
| ||||
| Non-Users (n = 37) | Healthy Users (n = 76) | Healthy + Unhealthy Users (n = 63) | Total sample (N= 176) | |
|
| ||||
| M (SD) | M (SD) | M (SD) | M (SD) | |
| Age (years) | 39.0 (4.4) | 40.4 (4.5) | 38.6 (4.7) | 39.5 (4.8) |
| Family income 2 | 2.4 (0.7) | 2.4 (0.8) | 2.5 (0.7) | 2.4 (0.8) |
| Education 3 | 15.3 (2.7) | 14.9 (2.2) | 14.3 (2.1) | 14.8 (2.3) |
| Weight (kg) | 66.4 a (12.9) | 75.1 b (17.5) | 77.0 b (17.4) | 74.0 (17.1) |
| BMI | 24.2 a (4.4) | 27.7 b (6.7) | 28.8 b (6.2) | 27.4 (6.3) |
| Weight as a child 4 | 0.6 a (0.7) | 1.0 b (0.7) | 1.1 b (0.7) | 0.9 (0.7) |
| Weight concerns | 1.1 a (0.7) | 1.7 b (0.7) | 2.1 c (0.7) | 1.7 (0.8) |
| Restraint | 3.5 a (2.5) | 8.5 b (4.3) | 10.6 c (4.3) | 8.2 (4.7) |
|
| ||||
| Latent Class | ||||
|
| ||||
| Non-Users | Healthy Users | Healthy + Unhealthy Users | Total Sample | |
|
| ||||
| Disinhibition | 5.0 a (3.8) | 7.1 b (4.0) | 7.9 b (3.4) | 6.9 (3.9) |
| Eating attitudes | 2.7 a (2.8) | 4.3 a (3.7) | 6.7 b (7.1) | 4.8 (5.2) |
| Body dissatisfaction | 0.7 a (0.7) | 1.3 b (0.8) | 1.4 b (0.9) | 1.2 (0.9) |
Notes.
Weight control strategy groups were identified using latent class analysis (LCA) posterior probabilities from the Weight Loss Behavior Scale.
Family income where 0 is < $20,000, 1 = $20,000 - $35,000, 2 = $35,000 – $50,000 and 3 is > $50,000.
Education where 1 = high school, 2 = Associates, 3 = Technical, 4 = Bachelor Degree, 5 = Masters Degree, 6 = PhD/MD.
Weight as a child where 0 = underweight, 1 = average, 2 = overweight
Superscripts indicate significant group differences (p < 0.05, Tukey HSD comparison); Analysis of variance was used to test group differences
Abbreviations: M = Mean; SD = Standard Deviation
Longitudinal Analyses: associations between weight control strategy group and patterns of weight change
Repeated measures mixed effect models
Polynomial models were first specified with a random intercept only. A fixed linear effect of time was significant (p < 0.001), such that average weight increased across time. The mean weight at baseline was 72.76 kg. The mean linear rate of change was 1.13 kg (2.5 pounds) every two years, with a 95% random effects CI of -3.9 to 6.13, indicating that not all women were expected to gain weight over time, although on average, women gained 2.4 kg (5.3 pounds) across the 4 year period. Predictive models were estimated next to examine associations between weight control strategy group (N, H, and H+U) and patterns of weight change after adjusting for BMI, income, and education at study entry. As shown in Figure 1, results revealed a significant weight control group by time interaction (p<.01.) A woman’s pattern of weight gain was dependent on which weight control strategy group she belonged to (i.e., N, H, or H+U weight control). Specifically, the increase in body weight over the 4 year period was significantly greater among women using H+U weight control strategies (MΔT1–T3 = 4.56, SD = ± 7.2 kg), than for women who used None (MΔT1–T3 = 1.02 ± 3.7 kg) ; t(163)= 1.28, p<.01) or women who only used H weight control strategies (MΔT1–T3 = 1.51 ± 4.9 kg); t(163)= 1.48, p<.05). The pattern of weight change was not significantly different between the N and H weight control strategy groups. Comparable results were obtained when the same models were used to predict BMI change (data not shown). A three-way interaction was also tested (after including all relevant main effects and two-way interactions) to examine whether the association between weight control group and time would vary across normal and overweight women (three-way interaction) after adjusting for covariates. However, the 3-way interaction was not significant; indicating that patterns of weight change among the weight control groups did not differ for normal weight and overweight women (data not shown).
Figure 1. Weight Gain over 4 years by Weight Control Strategy Group 1 after adjusting for covariates 2 (N = 176).
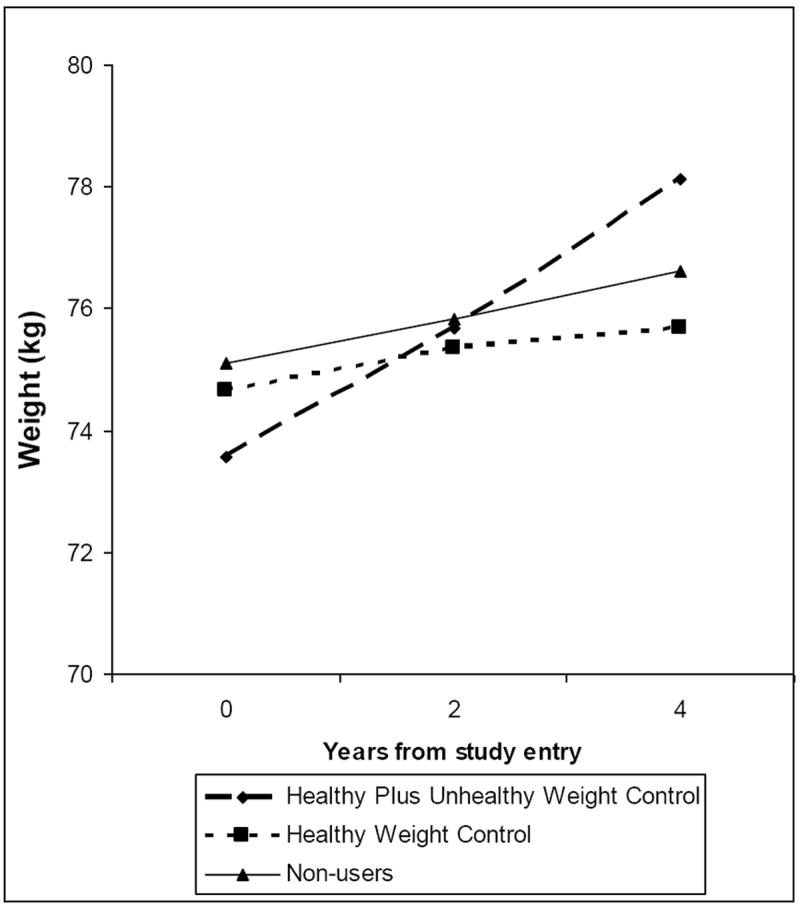
1Weight control groups were identified using latent class analysis: women reporting that they use None (n =3 7), Healthy (n = 76), or Healthy + Unhealthy (n = 63) weight control strategies.
2 Models adjusted for initial BMI, education and income level
Data were analyzed using Repeated Measures Mixed Models
General linear model. A final model was tested examining the relationship between weight control strategy group and weight change from Time 2 to Time 3 after adjusting for income, education, initial BMI, and recent weight change from Time 1 to Time 2. Results revealed that this model explained 21% of variance for subsequent weight change. The covariates (income, education, and initial BMI) explained 3% of the variance, with income emerging as the only significant predictor (p < 0.01). When recent weight change was entered to the model, an additional 12% of the variance was explained (p < 0.001). Lastly, the addition of weight control strategy group accounted for an additional 6% of the variance (p < 0.01) such that the H+U group gained significantly more weight (2.8 kg) than the H (0.03 kg) and N (0.4 kg) groups. Post hoc analyses revealed that recent weight change from Time 1 to Time 2 was inversely associated (p <.01) with weight change from Time 2 to Time 3 for women who used None (r = -0.47), H (r = -0.43), and H + U (r = -0.32) weight control strategies. A two-way interaction between recent weight change and weight control strategy group was also tested (after including all relevant main effects) but was not significant indicating that weight change among H, H+U, and N groups from Time 2 to Time 3 was not affected by recent weight change from Time 1 to Time 2. Lastly, follow-up analyses examined the influence of using specific weight control practices on weight maintenance (percent weight change >3%). On average, women gained 3.2% of their initial body weight from Time 1 to Time 3. However, percent weight change was significantly greater among the H+U weight control group (M = 5.7%, SD = 9.0) compared to the H weight control group (M = 1.7%, SD = 6.2).
DISCUSSION
The reported use of weight control practices has become normative (1), but it is unclear how use of specific weight control strategies is related to weight change over time. In the present study, women on average gained 2.4 kg (range = - 17 to 27 kg) over 4 years or 0.6 kg per year, which is consistent with other estimates indicating that adults tend to gain 0.5-1.0 kg per year (3, 4). Women who practiced Healthy plus Unhealthy weight control strategies gained the most weight, 4.6 kg over 4 years, whereas women who used None or only Healthy weight control strategies only gained 1.5 and 1.0 kg, respectively, after adjusting for covariates. This association did not differ for normal weight compared to overweight women (three-way interaction among weight control strategy group, time and BMI classification). Similar patterns emerged predicting weight change from Time 2 to Time 3, adjusting for recent weight change. Finally, in accordance with previous literature (11, 14, 28-32), after adjusting for initial BMI, women practicing unhealthy weight control strategies reported higher weight concerns, dietary restraint, and disordered eating attitudes than women who only used healthy weight control strategies. Together, these findings provide evidence that on average, women are gaining weight; however, self reported weight control attempts do not necessarily lead to large weight gains; rather the amount of weight gain may depend on the type of weight control strategies that women are practicing.
The present study is the first to examine how the use of different patterns of weight control strategies relates to weight change over a 2 year and 4 year period in free-living women. Three distinct patterns of weight control strategies were identified using latent class analysis, which were associated with differences in weight gain among women. Specifically, using healthy weight control strategies moderated weight gain, whereas practicing both healthy and unhealthy or extreme weight control strategies may promote weight gain. In addition, percent weight change among the H+U weight control group was significantly greater than women using N or only H weight control strategies who successfully maintained weight. Previous literature indicates that the percent weight gain experienced by women using H and U weight control strategies may be substantial enough to cause negative shifts in metabolic indicators of cardiovascular disease and metabolic syndrome components (17, 33, 34). One potential explanation for the differences in patterns of weight gain between the H and H+U groups is that women who choose healthy weight control strategies are able to sustain these behaviors long-term, promoting weight maintenance or loss. Women practicing unhealthy strategies may lose weight in the short term but are not able to sustain the stringent restriction demanded by the unhealthy strategies, including skipping meals and fasting, which may lead to loss of control, overeating and weight gain over time (35, 36).
Another potential explanation for the H+U group gaining significantly more weight than the H group is that women may use more desperate or extreme measures because they are overweight or initiate use of unhealthy weight control strategies in response to recent weight gain. To test this hypothesis, we examined a three-way interaction among recent weight gain, weight control strategy group, and time. This interaction was not significant indicating that recent weight gain did not influence the association between weight control strategy use and subsequent weight change. While this finding does not provide support for the view that recent weight gain “causes” the use of unhealthy weight control strategies, a failure to note a significant interaction only provides weak evidence. A lack of association could be the result of our small sample size and lack of power. Thus, additional research is warranted to examine the directionality of association between body weight and use of specific weight control strategies.
To date, one located study has examined the independent effect of practicing specific weight control strategies on weight change in a sample of adults participating in a weight prevention program. French and colleagues (10) found that duration of practicing calorie reduction, increased fruit and vegetable intake, fat reduction, elimination of sweets, and reducing the amount of food consumed were independently associated with less weight gain over time; however, there was no association between the independent use of unhealthy weight control strategies and weight change. In combination, findings from the present study and others suggest that normal and overweight women should be advised to increase fruit and vegetable intake, exercise more, reduce fat and caloric intake, reduce the amount food consumed, and eliminate snacks, sweets and junk food. Perhaps the most important implication of our findings is that there are strategies that women should be advised to avoid because they may be ineffective, unhealthy, and may lead to weight gain; women who added unhealthy weight control strategies such as skipping meals, fasting, using diet pills, liquid diets, or appetite suppressants, to healthy strategies gained significantly more weight after adjusting for initial weight and recent weight change. However, to test the effectiveness of avoiding unhealthy weight control strategies, a randomized clinical trial is required.
A secondary aim of the present study was to examine factors associated with weight control group membership. As previously reported (11, 12, 27), women who reported not using weight control strategies were significantly lighter than the H and H+U weight control groups. In addition, women in the N group retrospectively reported being “slightly underweight” whereas women in the H and H+U groups reported being “average” weight as a child. Thus, while causality cannot be determined in the present study, women who did not report using weight control efforts have a history of being thinner, suggesting that they may be constitutionally thin, and may have little need to initiate the use of weight control behavior for weight maintenance (37). Moreover, after adjusting for initial BMI, women in the H+U reported significantly greater weight concerns and disordered eating attitudes than H and N weight control users. These findings are in agreement with previous studies suggesting that individuals who are more highly concerned with their weight tend to engage in unhealthy weight control strategies such as fasting, purging, and diet pill use (14, 32) and disordered eating attitudes (31). Also similar to previous reports (11, 28-30), women practicing H+U weight control strategies reported greater body dissatisfaction and disinhibited eating than N weight control users, which may have contributed to their weight gain. However, after adjusting for initial BMI, body dissatisfaction and dietary disinhibition were not longer significant suggesting that the difference may actually be a reflection of women in the H+U and H only groups being heavier than N users at study entry. Thus, the potential of interventions aimed at reducing weight concerns and enhancing body image while preventing the use of unhealthy weight control strategies to reduce the incidence of disordered eating attitudes should be evaluated.
This study is not without limitations. First, this sample was racially and demographically homogenous, and included only women, which prevents us from generalizing to men or to other racial and socioeconomic groups. Similarly, different patterns of weight control may be observed in other age groups because our sample is limited to young, middle adulthood mothers. In addition, models predicting weight change over 4 years were not truly prospective because weight control strategy groups were identified at Time 2, asking participants to report use over the past 2 years. However, additional analyses revealed that women in the H + U group still gained significantly more weight between Time 2 and Time 3 than the H group after adjusting for recent weight change from Time 1 to Time 2; further demonstrating the negative effects of using unhealthy weight control strategies on weight maintenance. Another potential limitation is that this study did not assess frequency or duration (i.e., days, weeks, or months) of specific weight control strategy use which may also influence weight change (10). Thus, additional research is warranted to explore the duration and frequency of using specific weight control strategies that is required to promote maintain weight. Finally, these data were self reported; thus, there is the potential for reporting bias.
In conclusion, findings provide evidence that some women who were trying to lose or maintain weight were using ineffective strategies that were associated with greater weight gain. Specifically, using unhealthy weight control strategies in combination with healthy strategies was associated with weight gain over time after adjusting for recent weight gain; whereas only using healthy weight control strategies was more effective in moderating weight gain and associated with weight maintenance. Additional research is needed to examine how the frequency and duration of using specific weight control strategies is related to patterns of weight change. In our current obesogenic environment women often fail to maintain weight. Therefore, public health messages for weight control need to continue to encourage women to increase their fruit and vegetable intake, reduce fat intake, reduce calories, and eliminate snacks, sweets and junk food. Perhaps more importantly, to prevent future weight gain, women also need to be advised to avoid unhealthy, ineffective, restrictive weight control strategies such as skipping meals, fasting, use of diet pills and appetite suppressants.
Acknowledgments
This research was supported by the National Institutes of Health Grant NIH HD 32973 and The National Dairy Council. The services provided by the General Clinical Research Center of the Pennsylvania State University (supported by the NIH Grant M01 RR10732) are appreciated. The authors wish to thank Stephanie T. Lanza of the Methodology Center at the Pennsylvania State University for her consultation on latent class analyses.
References
- 1.Bish CL, Blanck HM, Serdula MK, Marcus M, Kohl HW, 3rd, Khan LK. Diet and physical activity behaviors among Americans trying to lose weight: 2000 Behavioral Risk Factor Surveillance System. Obes Res. 2005;13:596–607. doi: 10.1038/oby.2005.64. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Fryar CD, Carroll MD, Flegal KM. Mean body weight, height, and body mass index, United States 1960-2002. Adv Data. 2004:1–17. [PubMed] [Google Scholar]
- 3.Burke GL, Bild DE, Hilner JE, Folsom AR, Wagenknecht LE, Sidney S. Differences in weight gain in relation to race, gender, age and education in young adults: the CARDIA study. Ethne Health. 1996;1:237–335. doi: 10.1080/13557858.1996.9961802. [DOI] [PubMed] [Google Scholar]
- 4.Brown WJ, Williams L, Ford JH, Ball K, Dobson A. Identifying the energy gap: Magnitude and determinants of 5-year weight gain in midage women. Obesity Research. 2005;13:1431–1441. doi: 10.1038/oby.2005.173. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. Diet, nutrition, and the prevention of chronic diseases: report of the joint WHO/FAO expert consultation. Geneva: World Health Organization; 2003. WHO technical report series, No. 916. [Google Scholar]
- 6.U.S. Department of Health and Human Services and U.S. Department of Agriculture. Dietary Guidelines for Americans, 2005. 6. Washington, D.C: U.S. Govt Printing Office; Jan, 2005. [Google Scholar]
- 7.National Institutes of Health: National Heart Lung and Blood Institute. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. Bethesda, MD: National Institutes of Health; 1998. [PubMed] [Google Scholar]
- 8.Lowe MR, Annunziato RA, Markowitz JT, et al. Multiple types of dieting prospectively predict weight gain during the freshman year of college. Appetite. 2006;47:83–90. doi: 10.1016/j.appet.2006.03.160. [DOI] [PubMed] [Google Scholar]
- 9.French SA, Jeffery RW, Forster JL, McGovern PG, Kelder SH, Baxter JE. Predictors of weight change over two years among a population of working adults: the Healthy Worker Project. International Journal of Obesity Related Metabolic Disorders. 1994;18:145–154. [PubMed] [Google Scholar]
- 10.French SA, Jeffery RW, Murray D. Is dieting good for you?: Prevalence, duration and associated weight and behaviour changes for specific weight loss strategies over four years in US adults. Int J Obes Relat Metab Disord. 1999;23:320–7. doi: 10.1038/sj.ijo.0800822. [DOI] [PubMed] [Google Scholar]
- 11.French SA, Perry CL, Leon GR, Fulkerson JA. Dieting behaviors and weight change history in female adolescents. Health Psychol. 1995;14:548–55. doi: 10.1037//0278-6133.14.6.548. [DOI] [PubMed] [Google Scholar]
- 12.Kruger J, Galuska DA, Serdula MK, Jones DA. Attempting to lose weight: Specific practices among U.S. adults American. Journal of Preventive Medicine. 2004;26:402–406. doi: 10.1016/j.amepre.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 13.French SA, Jeffery JW, Murray DM. Is dieting good for you?: Prevalence, duration and associated weight and behaviour changes for specific weight loss strategies over four years in US adults. International Journal of Obesity. 1999;23:320–327. doi: 10.1038/sj.ijo.0800822. [DOI] [PubMed] [Google Scholar]
- 14.Goodrick GK, Poston WS, 2nd, Foreyt JP. Methods for voluntary weight loss and control: update 1996. Nutrition. 1996;12:672–6. doi: 10.1016/s0899-9007(96)00243-2. [DOI] [PubMed] [Google Scholar]
- 15.Lohman T, Roche A, Martorell R. Anthropometric Standardization Reference Manual. Illinois: Human Kinetics Book; 1991. [Google Scholar]
- 16.World Health Organization. Report of a WHO Consultation on Obesity World Health Organization. Geneva, Switzerland: 1998. Preventing and Managing the Global Epidemic. [Google Scholar]
- 17.Stevens J, Truesdale KP, McClain JE, Cai J. The definition of weight maintenance. Int J Obes (Lond) 2006;30:391–9. doi: 10.1038/sj.ijo.0803175. [DOI] [PubMed] [Google Scholar]
- 18.Hatcher L. A Step-by-Step Approach to Using the SAS(R) System for Factor Analysis and Structural Equation Modeling. Cary, N.C.: SAS Publishing; 1994. [Google Scholar]
- 19.Killen JD, Taylor CB, Hayward C, et al. Pursuit of thinness and onset of eating disorder symptoms in a community sample of adolescent girls: a three-year prospective analysis. Int J Eat Disord. 1994;16:227–38. doi: 10.1002/1098-108x(199411)16:3<227::aid-eat2260160303>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 20.Stunkard AJ, Messick S. The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J Psychosom Res. 1985;29:71–83. doi: 10.1016/0022-3999(85)90010-8. [DOI] [PubMed] [Google Scholar]
- 21.Stunkard AJ, Sorensen T, Schulsinger F. Use of the Danish Adoption Register for the study of obesity and thinness. Res Publ Assoc Res Nerv Ment Dis. 1983;60:115–20. [PubMed] [Google Scholar]
- 22.SAS Institute I. Statistical Analysis Software. SAS Institute, Inc; Cary, NC: 2001. [Google Scholar]
- 23.Lanza ST, Collins LM, Lemmon DR, Schafer JL. PROC LCA: A SAS procedure for latent class analysis. Structural Equation Modeling. 2007;14:671–694. doi: 10.1080/10705510701575602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lanza ST, Flaherty BP, Collins LM. Latent class and latent transition analysis. In: Schinka JA, Velicer WF, editors. Handbook of Psychology Research Methods in Psychology. Hoboken, NJ: Wiley; 2003. pp. 663–685. [Google Scholar]
- 25.Singer JD. Using SAS PROC MIXED to fit multilevel models, hierarchical models, and individual growth models. Journal of Educational and Behavioral Statistics. 1998;23:323–355. [Google Scholar]
- 26.Figueroa-Colon R, Arani RB, Goran MI, Weinsier RL. Paternal body fat is a longitudinal predictor of changes in body fat in premenarcheal girls. Am J Clin Nutr. 2000;71:829–34. doi: 10.1093/ajcn/71.3.829. [DOI] [PubMed] [Google Scholar]
- 27.French SA, Jeffery RW, Forster JL. Dieting status and its relationship to weight, dietary intake, and physical activity changes over two years in a working population. Obes Res. 1994;2:135–44. doi: 10.1002/j.1550-8528.1994.tb00639.x. [DOI] [PubMed] [Google Scholar]
- 28.Putterman E, Linden W. Appearance versus health: does the reason for dieting affect dieting behavior? J Behav Med. 2004;27:185–204. doi: 10.1023/b:jobm.0000019851.37389.a7. [DOI] [PubMed] [Google Scholar]
- 29.Anderson LA, Eyler AA, Galuska DA, Brown DR, Brownson RC. Relationship of satisfaction with body size and trying to lose weight in a national survey of overweight and obese women aged 40 and older, United States. Prev Med. 2002;35:390–6. doi: 10.1006/pmed.2002.1079. [DOI] [PubMed] [Google Scholar]
- 30.Provencher V, Drapeau V, Tremblay A, Despres JP, Bouchard C, Lemieux S. Eating behaviours, dietary profile and body composition according to dieting history in men and women of the Quebec Family Study. Br J Nutr. 2004;91:997–1004. doi: 10.1079/BJN20041115. [DOI] [PubMed] [Google Scholar]
- 31.Cachelin FM, Regan PC. Prevalence and correlates of chronic dieting in a multi-ethnic U.S. community sample. Eat Weight Disord. 2006;11:91–9. doi: 10.1007/BF03327757. [DOI] [PubMed] [Google Scholar]
- 32.Celio CI, Luce KH, Bryson SW, et al. Use of diet pills and other dieting aids in a college population with high weight and shape concerns. Int J Eat Disord. 2006;39:492–7. doi: 10.1002/eat.20254. [DOI] [PubMed] [Google Scholar]
- 33.Carnethon MR, Loria CM, Hill JO, Sidney S, Savage PJ, Liu K. Risk factors for the metabolic syndrome: the Coronary Artery Risk Development in Young Adults (CARDIA) study, 1985-2001. Diabetes Care. 2004;27:2707–15. doi: 10.2337/diacare.27.11.2707. [DOI] [PubMed] [Google Scholar]
- 34.Lloyd-Jones DM, Liu K, Colangelo LA, et al. Consistently stable or decreased body mass index in young adulthood and longitudinal changes in metabolic syndrome components: the Coronary Artery Risk Development in Young Adults Study. Circulation. 2007;115:1004–11. doi: 10.1161/CIRCULATIONAHA.106.648642. [DOI] [PubMed] [Google Scholar]
- 35.Kroke A, Liese AD, Schulz M, et al. Recent weight changes and weight cycling as predictors of subsequent two year weight change in a middle-aged cohort. Int J Obes Relat Metab Disord. 2002;26:403–9. doi: 10.1038/sj.ijo.0801920. [DOI] [PubMed] [Google Scholar]
- 36.Field AE, Byers T, Hunter DJ, et al. Weight cycling, weight gain, and risk of hypertension in women. Am J Epidemiol. 1999;150:573–9. doi: 10.1093/oxfordjournals.aje.a010055. [DOI] [PubMed] [Google Scholar]
- 37.Germain N, Galusca B, Le Roux CW, et al. Constitutional thinness and lean anorexia nervosa display opposite concentrations of peptide YY, glucagon-like peptide 1, ghrelin, and leptin. Am J Clin Nutr. 2007;85:967–71. doi: 10.1093/ajcn/85.4.967. [DOI] [PubMed] [Google Scholar]


