Abstract
BACKGROUND
“Rush to surgery” among patients with worse symptoms, delays related to morbidity, and inclusion of patients with advanced disease in study populations have produced a mixed picture of importance of time to treatment to survival of non-small cell lung cancer. Our objective was to assess the contribution of diagnosis to first surgery interval to survival among patients diagnosed in the community with early-stage non-small cell lung cancer.
METHODS
Patients with early-stage lung cancer (N = 174) at the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins who were diagnosed and treated from 2003 to 2009 and followed through 2011 made up a prospective study of overall survival. Diagnosis to first surgery interval was examined overall, as 2 segments (referral interval and treatment interval), as short and longer intervals, and as a continuous variable.
RESULTS
The majority of patients were female (55%) and aged more than 65 years (61%). The average mean referral and treatment delays were 61.2 and 5.9 days, respectively. Cox method hazard analysis revealed that older age (years) at diagnosis (hazard ratio [HR], 1.02; 95% confidence interval [CI], 1.00–1.05), stage UB (HR, 2.17; 95% CI, 1.12–4.21), large (>4 cm) (HR, 3.68; 95% CI, 1.05–12.93) or unknown tumor size (HR, 4.45; 95% CI, 1.21–16.38), and weeks from diagnosis to first surgery interval (HR, 1.04; 95% CI, 1.00–1.09) predicted worse overall survival. The threshold period of less than 42 days from diagnosis to surgery did not reach statistical significance.
CONCLUSIONS
Patients seem to benefit from rapid reduction of tumor burden with surgery. Reasons for delay were not available. Nevertheless, referral delay experienced in the community is unduly long. In addition to patient choices, an unconscious patient or physician bias that lung cancer is untreatable or an inevitable consequence of smoking may be operating and needs further investigation.
Keywords: Lung, Lung cancer biology, Lung cancer surgery, Quality care management, Statistics, Survival analysis
Surgery after diagnosis for stage I to II non-small cell lung cancer is the best chance for cure.1,2 Because doubling time for growth of detectable early-stage lung tumors is approximately 4 months,3 timely surgery is all the more important, although studies thus far have yielded mixed survival results, perhaps because studies to date evaluated patients with both early- and late-stage non-small cell lung cancer.4,5 Thus, findings may be due in part to a “rush to treatment” for those with the worst symptoms6 or “treatment delay” for the sickest,7,8 who undergo additional pre-surgery examination.9 In addition, specialist care is an intervening step that extends time to treatment.5,10
Demographic factors of African American race, female gender, never married, and older age may have a role in surgery uptake or postponement.11–13 Individuals who receive no surgery, which may be thought of as an indeterminate time to surgery and longer treatment delay, have worse survival compared with survival among those opting for surgery.14 Completion of treatment referrals may be more timely, depending on one’s resources, distance from care, social support,15,16 and having never smoked.16
Another factor contributing to delay is care at a cancer center, which is often not the first place a person with cancer is treated.7 At times, the person with cancer receives a diagnosis of lung cancer from a community physician and is referred to a cancer center for surgery and other therapies. In other cases, the person is referred directly to the cancer center for both diagnosis and treatment. In each case, it may be beneficial to the patient to minimize time before surgery because the time from symptom to general consult and to specialty care has been found to be longer than the time from first contact at a cancer center to surgery.4,5,16
Nevertheless, cancer centers strive to provide timely care and have taken steps to assess a patient’s cancer, to assign a working diagnosis, to agree on the strategy for care with a multidisciplinary team, and to facilitate scheduling of all necessary diagnostic and pretreatment procedures with efficiency17 in response to National Cancer Centers Network guidelines for treatment of non-small cell lung cancer.18 Multidisciplinary clinics and biweekly case conferences are now the norm at cancer centers and are effective in facilitating receipt of timely care.19 Despite best efforts to date, there may still be opportunity for shortening the interval from diagnosis to first surgery, especially if delay directly affects survival.7,15
This examination of patients diagnosed elsewhere and treated at the Sidney Kimmel Comprehensive Cancer Center (SKCCC) at Johns Hopkins will evaluate the time from diagnosis to first surgery among patients with early-stage non-small cell lung cancer. We first evaluated the hypothesis that delay to first surgery and other time-related factors reduce survival after treatment (surgery). We then assessed the hypothesis that age, race, gender, place of residence, tumor characteristics, and morbidity confound the relationship between these factors and survival.
CLINICAL SIGNIFICANCE.
In addition to the stage of disease, tumor size, and age at diagnosis, each week the referral interval is lengthened conveys a 5% increase in the risk of death.
There was no minimal time from diagnosis to surgery when risk was not elevated.
After community diagnosis, referral times may be longer for non-small cell lung cancer than other cancer sites.
MATERIALS AND METHODS
Participants
Study patients were diagnosed with lung cancer in the community and referred to Johns Hopkins medical institutions for treatment. Patients receiving surgery for early-stage (American College of Surgeons [Sixth Edition] stages I–II), incident (newly diagnosed) non-small cell lung cancer at SKCCC between 2003 and 2009 were included (N = 174). This study is a retrospective cohort or nonconcurrent design.20 Clinical diagnoses of cancer were made elsewhere and histologically confirmed at first surgery. Patients who refused surgery or were not candidates for surgery were excluded. Patient follow-up and data assemblage were conducted by the Committee on Cancer certified Johns Hopkins Hospital Tumor Registry. This study was approved by the Johns Hopkins Bloomberg School of Public Health institutional review board.
Diagnosis to First Surgery Interval
Time from first contact at SKCCC to first surgery was calculated in days for each patient; this is defined as the treatment interval. Time from diagnosis to first contact at SKCCC was determined for all patients; this is defined as the referral interval. The sum of treatment interval and referral interval is the diagnosis to first surgery interval (Figure 1). During analysis, we examined diagnosis to first surgery intervals of short interval (≤6 weeks) and long interval and delay (>6 weeks). Six weeks has been cited in the literature as an indicator of timely care.5,14 We have used the term “delay” to indicate the longer interval. Finally, we evaluated the hazard effect when considering time from diagnosis to first surgery as a continuous variable and then split this interval into referral interval and treatment interval to assess where the major contribution to the risk of death resided. Date of diagnosis was that assigned by the hospital cancer registry from the medical record.
Figure 1.
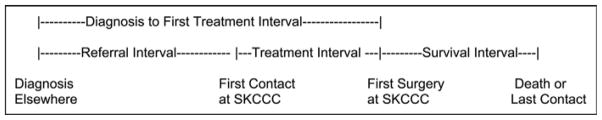
Timeline for patients diagnosed in the community and treated with surgery at a cancer center. SKCCC = Sidney Kimmel Comprehensive Cancer Center.
Overall Survival
Overall survival is defined as time from first surgery to death or last contact (Figure 1). In any year, at least 95% of cases known to be alive at last contact are reached to confirm vital status, matched with a death certificate, or updated from state’s cancer registries information. Person time was accrued through 2011 in this nonconcurrent study. During the study period, 56 patients (32%) had died, 107 patients (62%) were known within the last 2 years to be alive, and 11 patients (6%) were confirmed to be alive more than 2 years previously. Three of 38 patients (7.9%) with a short interval and 8 of 80 patients (10.0%) with a longer diagnosis to surgery interval were not contacted in the past 2 years; there were no differences in follow-up time (Fisher exact test, P = .50). Because of the small number not contacted in the past 2 years, we did not assess the characteristics that distinguish those who were lost to follow-up from those remaining under observation.
Covariates
Known and potential correlates of survival after surgery include demographics: age (continuous and categoric, <75/≥75 years), gender, race/ethnicity (Hispanic, white race, black race, other race); cancer tumor characteristics: stage (IA, IB-IIA, IIB) and tumor size (<2 cm, 2–4 cm, >4 cm, unknown); barriers to care: place of residence (Baltimore City; the SKCCC patient catchment area not Baltimore City (57 adjacent counties)21; and outside the SKCCC catchment area); health insurance (yes, no, unknown); lifestyle factors: marital (never married, married, unknown); and smoking status (never, former, current, unknown). The American Society of Anesthesiology (ASA) 5-grade classification system22 was used as an index of comorbidity. All covariates are time-independent measurements. Because of small numbers of individuals diagnosed in stage IIA and the consistency of the hazard ratio (HR) for IIA with IB, we combined these 2 stages in all analyses. In the final model, we further combined stages IA, IB, and IIA, which were neither qualitatively nor statistically different from one another. We used the Sixth Edition of the Tumor, Node, and Metastasis staging manual because it is still the basis of treatment algorithms.23
Data Analysis
The effect of delayed surgery defined as categoric intervals on survival was first measured univariately by Kaplan-Meier estimator. Cox proportional hazard models were fitted adjusting potential confounders and covariates. All variables met the Cox model assumption of proportional hazard.24 Fitting of the final model was done by beginning with the full model and carrying out backward stepwise removal of the least significant predictors (threshold level: P ≥ .10). The Fisher exact test was conducted to determine independence of covariates and categoric intervals. P value less than .05 was the cut point for statistical significance. Statistical software R (Free Software Foundation, Inc., Boston, Mass) was used to perform the analysis.
RESULTS
Patient Population
Details of the patient population under study are shown in Table 1. The majority were aged 65 years or more (61%), female (55%), white (90%), former smokers (60%), insured (97%), residents of 57 counties adjacent to Baltimore City (70%), and married (87%); had an ASA of 3 (86%); were diagnosed at stage IB, IIA, or IIB (60%); and had a tumor >2 cm (60%).
Table 1.
Diagnosis to Surgery Interval by Demographics, Personal Risk Factors, and Tumor Characteristics
| Diagnosis to Surgery Interval
|
P Value | |||
|---|---|---|---|---|
| All Patients (N = 174) | ≤42 d (N = 52) | >42 d (N = 122) | ||
| Age | .36 | |||
| <65 y | 68 (39%) | 17 (33%) | 51 (42%) | |
| 65–74 y | 60 (35%) | 22 (42%) | 38 (31%) | |
| 75+y | 46 (26%) | 13 (25%) | 33 (27%) | |
| Female | 96 (55%) | 28 (54%) | 68 (56%) | .87 |
| White race | 156 (90%) | 46 (88%) | 110 (90%) | .79 |
| Smoking history | .94 | |||
| Current | 44 (25%) | 12 (23%) | 32 (26%) | |
| Former | 105 (60%) | 32 (62%) | 73 (60%) | |
| Never | 17 (10%) | 5 (10%) | 12 (10%) | |
| Unknown | 8 (5%) | 3 (6%) | 5 (4%) | |
| Insurance | .18 | |||
| Yes | 168 (97%) | 52 (100%) | 116 (95%) | |
| No/unknown | 6 (3%) | 0 (0%) | 6 (5%) | |
| Residence | .62 | |||
| Baltimore City | 12 (7%) | 5 (10%) | 7 (6%) | |
| Adjacent counties | 121 (70%) | 35 (67%) | 86 (70%) | |
| Noncatchment | 41 (24%) | 12 (23%) | 29 (24%) | |
| Married | .47 | |||
| Ever | 152 (87%) | 44 (85%) | 108 (89%) | |
| Single/unknown | 22 (13%) | 8 (15%) | 14 (11%) | |
| ASA | .44 | |||
| 1–2 | 24 (14%) | 4 (8%) | 16 (11%) | |
| 3 | 200 (86%) | 47 (90%) | 106 (88%) | |
| Stage | .47 | |||
| 1A | 70 (40%) | 22 (42%) | 48 (39%) | |
| 1B/2A | 74 (43%) | 24 (46%) | 50 (41%) | |
| 2B | 30 (17%) | 6 (12%) | 24 (20%) | |
| Tumor size | .35 | |||
| <2 cm | 35 (20%) | 9 (17%) | 26 (21%) | |
| 2–4 cm | 70 (40%) | 25 (48%) | 45 (37%) | |
| >4 cm | 50 (29%) | 11 (21%) | 39 (32%) | |
| Unknown | 19 (11%) | 7 (13%) | 12 (10%) | |
ASA = American Society of Anesthesiology.
P values were based on 2-sided Fisher exact test (Statistical software R).
Six weeks from diagnosis to first surgery is considered timely care. There were no differences in age, race, gender, smoking history, place of residence, marital status, morbidity, or tumor stage and size between the short (≤42 days) and the long (>42 days) interval lengths (Table 1). In addition, all of our study patients had a preoperative ASA of ≤3.
Interval Length
Although mean treatment interval (first SKCCC contact to first surgery) was 5.9 days (95% confidence interval [CI], 3.3–8.6), the mean referral interval was approximately 2 months (61.2 days; 95% CI, 54.7–67.8). The mean diagnosis to first surgery interval was 67.2 days (95% CI, 60.5–73.9).
Considering the diagnosis to first surgery interval categories of ≤6 weeks and >6 weeks, interval length did not predict survival probability (Table 2). Diagnosis to surgery interval as a continuous variable was significant after adjusting for age, gender, smoking history, insurance, place of residence, year of diagnosis, marital status, stage, and tumor size and was relatively unchanged by any of the univariate adjustments (Table 2).
Table 2.
Cox Proportional Hazard Model of Overall Survival Adjusting for Delay From Diagnosis to First Surgery Interval
| Interval From Diagnosis to First Surgery Treated as Category (≥42 vs <42 d)
|
Interval From Diagnosis to First Surgery Treated as Continuous Outcome (wk)
|
|||
|---|---|---|---|---|
| HR | 95% CI | HR | 95% CI | |
| Delay from diagnosis | 1.34 | 0.73–2.46 | 1.04 | 1.00–1.08 |
| Delay from diagnosis | 1.31 | 0.72–2.41 | 1.04 | 1.00–1.08 |
| Age at diagnosis (>75 vs ≤75 y) | 1.51 | 0.87–2.61 | 1.62 | 0.93–2.82 |
| Delay from diagnosis | 1.38 | 0.75–2.53 | 1.05 | 1.01–1.09 |
| Age at diagnosis (y) | 1.02 | 0.99–1.05 | 1.03 | 1.00–1.05 |
| Delay from diagnosis | 1.34 | 0.73–2.46 | 1.04 | 1.00–1.09 |
| Gender (male vs female) | 1.15 | 0.68–1.94 | 1.22 | 0.72–2.08 |
| Delay from diagnosis | 1.33 | 0.72–2.44 | 1.04 | 1.00–1.08 |
| Race (white vs nonwhite) | 0.81 | 0.32–2.04 | 0.80 | 0.32–2.02 |
| Delay from diagnosis | 1.35 | 0.74–2.48 | 1.04 | 1.00–1.08 |
| Smoking history (former vs current/unknown) | 1.10 | 0.58–2.06 | 1.11 | 0.59–2.09 |
| Smoking history (never vs current/unknown) | 0.74 | 0.26–2.09 | 0.72 | 0.26–2.03 |
| Delay from diagnosis | 1.37 | 0.74–2.42 | 1.04 | 1.00–1.08 |
| Insurance (yes vs no) | 0.91 | 0.22–3.79 | 0.83 | 0.20–3.40 |
| Delay from diagnosis | 1.35 | 0.74–2.48 | 1.04 | 1.00–1.08 |
| Residence (catchment vs Baltimore City) | 0.95 | 0.34–2.68 | 0.91 | 0.32–2.55 |
| Residence (noncatchment vs Baltimore City) | 0.80 | 0.43–1.48 | 0.76 | 0.41–1.42 |
| Delay from diagnosis | 1.38 | 0.75–2.56 | 1.04 | 1.00–1.09 |
| Diagnosis year (05–06 vs 03–04) | 1.13 | 0.59–2.18 | 1.19 | 0.62–2.30 |
| Diagnosis year (07–09 vs 03–04) | 0.75 | 0.37–1.55 | 0.72 | 0.35–1.49 |
| Delay from diagnosis | 1.24 | 0.67–2.28 | 1.03 | 0.99–1.07 |
| Stage (2B vs 1A–2A) | 2.50 | 1.36–4.60 | 2.39 | 1.29–4.40 |
| Delay from diagnosis | 1.41 | 0.75–2.63 | 1.04 | 1.00–1.08 |
| Marital status (married/ever vs single) | 0.77 | 0.38–1.58 | 0.85 | 0.41–1.76 |
| Delay from diagnosis | 1.32 | 0.71–2.43 | 1.04 | 1.00–1.08 |
| Tumor size (2–4 cm vs 0–2 cm) | 4.11 | 1.24–13.66 | 3.94 | 1.19–13.11 |
| Tumor size (>4 cm vs 0–2 cm) | 4.82 | 1.42–16.42 | 4.79 | 1.41–16.31 |
| Tumor size (unknown vs 0–2 cm) | 5.19 | 1.43–18.82 | 5.40 | 1.48–19.63 |
CI = confidence interval; HR = hazard ratio.
Cox Proportional Survival Analysis
Proportional hazard assumption was verified before applying the Cox proportional hazard model. The final Cox proportional hazards model retained variables significant at the P < .05 level were diagnosis to first surgery interval, age at diagnosis, stage 2B, and tumor size 4 cm or unknown; thus, after controlling for these 3 variables that also predict survival, interval remained a statistically significant predictor of survival (Table 3). Race, place of residence, and smoking history were not significant and were dropped from the full model because model coefficients did not change appreciably. Overall 1-, 2-, and 5-year survivals were 92% (95% CI, 88–96), 83% (95% CI, 77–89), and 60% (95% CI, 51–71), respectively.
Table 3.
Final Cox Proportional Hazard Models, Patients Diagnosed in the Community and Treated at a Cancer Center
| Model 1: Predictor Variables Including Diagnosis to Surgery Interval | Hazard Ratio (95% CI) | Model 2: Predictor Variables Including Constituents of the Diagnosis to Surgery Interval | Hazard Ratio (95% CI) |
|---|---|---|---|
| Diagnosis to surgery interval (wk) | 1.04 (1.00–1.09) | Referral interval (wk) | 1.05 (1.01–1.09) |
| Treatment interval (wk) | 0.82 (0.62–1.08) | ||
| Age at diagnosis (y) | 1.02 (1.00–1.05) | Age at diagnosis (y) | 1.02 (0.99–1.05) |
| Stage | Stage | ||
| 1A–2A | Reference | 1A–2A | Reference |
| 2B | 2.17 (1.12–4.21) | 2B | 2.14 (1.11–4.13) |
| Tumor size | Tumor size | ||
| <2 cm | Reference | <2 cm | Reference |
| 2–4 cm | 3.32 (0.99–11.13) | 2–4 cm | 3.03 (0.90–10.20) |
| >4 cm | 3.68 (1.05–12.93) | >4 cm | 3.67 (1.04–12.95) |
| Unknown | 4.45 (1.21–16.38) | Unknown | 4.78 (1.30–17.58) |
CI = confidence interval.
For each week of delay from diagnosis to first surgery, the relative hazard of death increases 4% adjusting for age at diagnosis, stage IIb (yes/no), and tumor size (Table 3). We segmented the diagnosis to first surgery interval in the final model, which shows reduced odds of survival or higher HR concentrated in the referral interval portion only (HR, 1.05; 95% CI, 1.01–1.09).
Each year of age at diagnosis carried a relative 2% increase in risk of death (HR, 1.02; 95% CI, 0.99–1.05) (Table 3). Additional testing of age >75 years did not show an additive risk of dying for the oldest patients with non-small cell lung cancer.
Stage IIB was the only stage boding significantly poorer survival. The HR for this stage is 2.14 (95% CI, 1.11–4.13). Initially, all stages relative to IA were tested, and stage IIB (yes/no) presented the most parsimonious model. Greater or unknown tumor size is significant to the risk of death, conveying HRs between 3.0 and 4.7 (Table 3).
DISCUSSION
In this group of relatively healthy patients diagnosed in the community with early-stage non-small cell lung cancer and treated initially with surgery at SKCCC, time variables indicating greater delay to diagnosis or surgery predicted survival probabilities. Although this study does not examine events before diagnosis, higher cancer stage and larger size may indicate a longer time before diagnosis with preclinical cancer or unrecognized or unaddressed symptoms. Delay to first surgery after diagnosis carried a significant increment in risk of death. Risk of death associated with diagnosis to surgery interval appears to be continuous, having no threshold at 6 weeks. The risk of poorer survival was focused on the referral interval, although the mean referral delay was more than 7 times the delay to treatment, and this is not atypical.4 Timing of surgery in early-stage non-small cell lung cancer is all the more important as lung cancer screening and subsequent treatment are becoming more common.25,26
In addition to referral and treatment delays, a tumor >2 cm, a diagnosis of stage 2B at surgery, and older age conveyed worse prognosis. Personal characteristics of race, gender, place of residence, insurance status, marital, and smoking history were not key to survival in this cohort of patients or associated with interval. The ASA score and frailty indicated by age >75 years did not convey an additional hazard of death. We could not replicate the contributions of gender, race, and socioeconomic status measured by place of residence to survival others have found in stage IA-IB cancers,27,28 in settings where health care is generally more accessible. Still, age and tumor size in addition to delay were confirmed as predictive.29 This is the first study of early-stage lung cancers diagnosed in the community to show a poorer prognosis with delay.
Patients diagnosed elsewhere and treated at this cancer center experienced a shorter mean therapeutic interval compared with the referral interval found in earlier studies. Nevertheless, it is not possible to rule out that morbidity accounts for longer intervals, because age is an independent influence on the risk of dying and may account for greater morbidity occurring with advancing age despite no age threshold. Greater morbidity as measured by the ASA before surgery was not a factor in this study because patients with early-stage cancer in this cohort had ASAs of ≤3; thus, after excluding those for whom surgery was not recommended and those who refused surgery, these patients are relatively healthy adults. Patients with early-stage cancer who refused or were not recommended for surgery, excluded from this study, may have a different morbidity profile.
Estimates of tumor doubling size at early-stage non-small cell lung cancer are thought to be among the shortest by cancer site, within the span of the time from diagnosis to surgery identified in this population and thus a concern.3 With the prospect of lung cancer screening detecting cancers <2 cm,30,31 potential survival gains may be eliminated if there are barriers to emergent care. Referral delay was more than 1 month (first quartile = 33.3 days) for approximately three quarters of patients, and 7.5% of patients had treatment delays of more than 1 month. For the latter group of patients, future studies may elucidate the delays encountered.
Sample Patients
This study underscores the importance of timely surgery for survival of patients with early-stage non-small cell lung cancer. With the use of the parameters in our final model, a patient diagnosed at age 60 years with stage IIB non-small cell lung cancer >4 cm and treated within 2 weeks has a 50% chance of surviving 5 years (Table 4). If this patient is treated at 4 weeks after diagnosis, 5-year survival likelihood decreases to 47%. This is equivalent to living an additional 0.4 years (assuming survival time follows an exponential distribution). It is important to point out that 5-year early-stage survival is good in this patient group compared with all patients diagnosed with lung cancer.32 Table 4 shows the results for a comparable patient who is aged 30 years. For this 30-year-old patient, 5-year survival is 71% with treatment at 2 weeks.
Table 4.
Example Diagnosis to Surgery Delay Effects in Patients with Stage IIB, Tumor Size ≥4 Centimeters
| Treatment Delay (wk) | Patient Age 30 y
|
Patient Age 60 y
|
||
|---|---|---|---|---|
| 5-y Survival rate | Median Survival (y)* | 5-y survival rate | Median Survival (y) | |
| 2 | 71% | 10.1 | 50% | 5.0 |
| 4 | 69% | 9.3 | 47% | 4.6 |
| 6 | 67% | 8.7 | 44% | 4.2 |
| 8 | 65% | 8.0 | 41% | 3.9 |
Median survival is calculated from 5-year survival rate, assuming survival time follows exponential distribution.
This study demonstrates that any delay to treatment once the diagnosis of cancer is made results in suboptimal survival. Furthermore, this study did not find a threshold for timeliness. With the prospect of lung cancer screening finding cancers <2 cm,30,31 potential survival gains may be eliminated if there are barriers to emergent care.
Study Limitations
This survival study included a homogeneous group of 174 patients with early-stage non-small cell lung cancer who were diagnosed in the community over a period of 7 years, treated at a cancer center, and followed for at least 3 years (median survival time >6 years), whose observed survival is somewhat higher (60%; 95% CI, 51–70) than that of non-small cell lung cancer SEER cases (52%, 2000).32 Thus, the statistically significant diagnosis to treatment interval finding is in the context of what may have been an underpowered study. Although follow-up was near complete (94%) and contact did not differ significantly among the survivors by interval, the number of survivors with less follow-up and short interval did not lend itself to meaningful analysis of their characteristics. Even so, this analysis of a well-characterized patient population points to a few important predictors of survival in early-stage non-small cell lung cancer, at least one of which is modifiable.
It has yet to be determined what delays care. Among the patients in this study with delays of more than 6 weeks, half were diagnosed during October, November, and December, indicating that including seasonality or holidays and myriad personal reasons account for delay. At a specialty hospital, interactions between the referring physicians and the oncologist may dictate the pace of surgery, although we found that treatment interval already was less than 1 week. Referral, even if seamless, is an additional medical care step that takes time, and efficiencies might be introduced if this reason is identified with further study at SKCCC.33
Finally, by investigating registry patients, we were not able to document extenuating medical circumstances (eg, treatment of a current lung infection) or further workup to rule out mediastinal node assessment that may have resulted in delay. Nevertheless, in our final model of survival, clinical stage 2B and interval from diagnosis to surgery are each independent risk factors of survival, supporting the idea that interval increases risk of death separate from stage. Moreover, shortening the time to surgery when feasible has prospects for improving lung cancer outcomes among those undergoing surgery.
One impediment to timely treatment may be attitudes toward treatment of lung cancer because of the stigma of smoking—physician or patient nihilism.34 In our institution’s breast cancer program (2003–2005), we observed an average diagnosis to first surgery interval of 32 days among women diagnosed elsewhere, with 38% receiving first surgery within 3 weeks. This is short when contrasted with our patients with lung cancer, whose average diagnosis to first surgery interval is approximately double and among whom only 9% receive first surgery within 3 weeks. In addition to patient and physician awareness of treatment effectiveness, it is possible that patients with breast cancer and their practitioners have overcome a treatment nihilism that has not been accomplished in lung cancer.35 Chambers et al36 systematically reviewed 15 studies that focused on the stigma of smoking history and underestimation by physicians of the success of treatment, even at early stages.37
CONCLUSIONS
Patients would profit from universal consideration of lung cancer as an urgent condition that merits full attention and rapid response to reduce tumor burden among patients with small, early-stage tumors.5,31,38–40 In a position to treat afflicted patients, primary care providers and specialists are obligated to look at their own unconscious bias37 as a matter of life and death to these patients and to ensure that patients with early-stage lung cancer are treated most efficaciously and effectively, with timely surgery.34
Acknowledgments
Funding: Funding for this project was provided by the Maryland Cigarette Restitution Fund (FY12).
Footnotes
Conflict of Interest: None.
Authorship: All authors had access to the data and played a role in writing this manuscript.
Posters presented at: the American Association for Cancer Research Conference on the Science of Cancer Health Disparities in Racial/Ethnic Minorities and the Medically Underserved, October 27–30, 2012, San Diego, California; and Society of Black Academic Surgeons, April 12–14, 2012, Baltimore, Maryland.
References
- 1.Ettinger DS, Kris MG. NCCN: Non-small cell lung cancer. Cancer Control. 2001;8:22–31. [PubMed] [Google Scholar]
- 2.Harless W, Qiu Y. Cancer: a medical emergency. Med Hypotheses. 2006;67:1054–1059. doi: 10.1016/j.mehy.2006.04.032. [DOI] [PubMed] [Google Scholar]
- 3.Lin RS, Plevritis SK. Comparing the benefits of screening for breast cancer and lung cancer using a novel natural history model. Cancer Causes Control. 2012;23:175–185. doi: 10.1007/s10552-011-9866-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gould MK, Ghaus SJ, Olsson JK, Schultz EM. Timeliness of care in veterans with non-small cell lung cancer. Chest. 2008;133:1167–1173. doi: 10.1378/chest.07-2654. [DOI] [PubMed] [Google Scholar]
- 5.Aragoneses FG, Moreno N, Leon P, Fontan EG, Folque E. Influence of delays on survival in the surgical treatment of bronchogenic carcinoma. Lung Cancer. 2002;36:59–63. doi: 10.1016/s0169-5002(01)00458-5. [DOI] [PubMed] [Google Scholar]
- 6.Myrdal G, Lambe M, Hillerdal G, Lamberg K, Agustsson T, Stable E. Effect of delays on prognosis in patients with non-small cell lung cancer. Thorax. 2004;59:45–49. [PMC free article] [PubMed] [Google Scholar]
- 7.Jensen AR, Mainz J, Overgaard J. Impact of delay on diagnosis and treatment of primary lung cancer. Acta Oncol. 2002;41:147–152. doi: 10.1080/028418602753669517. [DOI] [PubMed] [Google Scholar]
- 8.Powell AA, Schultz EM, Ordin DL, et al. Timeliness across the continuum of care in veterans with lung cancer. J Thorac Oncol. 2008;3:951–957. doi: 10.1097/JTO.0b013e3181839b60. [DOI] [PubMed] [Google Scholar]
- 9.Christensen ED, Harvald T, Jendresen M, Aggestrup S, Petterson G. The impact of delayed diagnosis of lung cancer on the stage at the time of operation. Eur J Cardiothorac Surg. 1997;12:880–884. doi: 10.1016/s1010-7940(97)00275-3. [DOI] [PubMed] [Google Scholar]
- 10.Perez G, Porta M, Borrell C, et al. Interval from diagnosis to treatment onset for six major cancers in Catalonia, Spain. Cancer Detect Prev. 2008;32:267–275. doi: 10.1016/j.cdp.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 11.Ou SH, Zell JA, Ziogas A, Anton-Culver H. Low socioeconomic status is a poor prognostic factor for survival in stage I nonsmall cell lung cancer and is independent of surgical treatment, race, and marital status. Cancer. 2008;112:2011–2020. doi: 10.1002/cncr.23397. [DOI] [PubMed] [Google Scholar]
- 12.Bryant AS, Cerfolio RJ. Impact of race on outcomes of patients with non-small cell lung cancer. J Thorac Oncol. 2008;3:711–715. doi: 10.1097/JTO.0b013e31817c60c7. [DOI] [PubMed] [Google Scholar]
- 13.Lathan CS, Neville BA, Earle CC. The effect of race on invasive staging and surgery in non-small-cell lung cancer. J Clin Oncol. 2006;24:413–418. doi: 10.1200/JCO.2005.02.1758. [DOI] [PubMed] [Google Scholar]
- 14.Bozcuk H, Martin C. Does treatment delay affect survival in non-small cell lung cancer? A retrospective analysis from a single UK centre. Lung Cancer. 2001;34:243–252. doi: 10.1016/s0169-5002(01)00247-1. [DOI] [PubMed] [Google Scholar]
- 15.Shugarman LR, Mack K, Sorbero ME, et al. Race and sex differences in the receipt of timely and appropriate lung cancer treatment. Med Care. 2009;47:774–781. doi: 10.1097/MLR.0b013e3181a393fe. [DOI] [PubMed] [Google Scholar]
- 16.Saint-Jacques N, Rayson D, Al-Fayea T, Virik K, Morzycki W, Younis T. Waiting times in early-stage non-small cell lung cancer (NSCLC) J Thorac Oncol. 2008;3:865–870. doi: 10.1097/JTO.0b013e318180210c. [DOI] [PubMed] [Google Scholar]
- 17.Bilimoria KY, Ko CY, Tomlinson JS, et al. Wait times for cancer surgery in the United States: trends and predictors of delays. Ann Surg. 2011;253:779–785. doi: 10.1097/SLA.0b013e318211cc0f. [DOI] [PubMed] [Google Scholar]
- 18.Ettinger DS, Akerley W, Bepler G, et al. Non-small cell lung cancer. J Natl Compr Canc Netw. 2010;8:740–801. doi: 10.6004/jnccn.2010.0056. [DOI] [PubMed] [Google Scholar]
- 19.Murray PV, O’Brien ME, Sayer R, et al. The pathway study: results of a pilot feasibility study in patients suspected of having lung carcinoma investigated in a conventional chest clinic setting compared to a centralised two-stop pathway. Lung Cancer. 2003;42:283–290. doi: 10.1016/s0169-5002(03)00358-1. [DOI] [PubMed] [Google Scholar]
- 20.Greene BR, Filerman GL. Reinventing CME: the role of the care pilot in the medical group practice. J Ambul Care Manage. 2007;30:283–290. doi: 10.1097/01.JAC.0000290396.58790.f0. [DOI] [PubMed] [Google Scholar]
- 21.Su SC, Kanarek N, Fox MG, Guseynova A, Crow S, Piantadosi S. Spatial analyses identify the geographic source of patients at a National Cancer Institute Comprehensive Cancer Center. Clin Cancer Res. 2010;16:1065–1072. doi: 10.1158/1078-0432.CCR-09-1875. [DOI] [PubMed] [Google Scholar]
- 22.Keats AS. The ASA classification of physical statuse a recapitulation. Anesthesiology. 1978;49:233–236. doi: 10.1097/00000542-197810000-00001. [DOI] [PubMed] [Google Scholar]
- 23.Nair A, Klusmann MJ, Jogeesvaran KH, Grubnic S, Green SJ, Vlahos I. Revisions to the TNM staging of non-small cell lung cancer: rationale, clinicoradiologic implications, and persistent limitations. Radiographics. 2011;31:215–238. doi: 10.1148/rg.311105039. [DOI] [PubMed] [Google Scholar]
- 24.Cox DR. Regression models of life tables. Journal of the Royal Statistical Society. Series B. 1972;34:187–220. [Google Scholar]
- 25.Libby DM, Wu N, Lee IJ, et al. CT screening for lung cancer: the value of short-term CT follow-up. Chest. 2006;129:1039–1042. doi: 10.1378/chest.129.4.1039. [DOI] [PubMed] [Google Scholar]
- 26.Allgar VL, Neal RD. Delays in the diagnosis of six cancers: analysis of data from the National Survey of NHS Patients: Cancer. Br J Cancer. 2005;92:1959–1970. doi: 10.1038/sj.bjc.6602587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ou SH, Zell JA, Ziogas A, Anton-Culver H. Prognostic factors for survival of stage I nonsmall cell lung cancer patients: a population-based analysis of 19,702 stage I patients in the California Cancer Registry from 1989 to 2003. Cancer. 2007;110:1532–1541. doi: 10.1002/cncr.22938. [DOI] [PubMed] [Google Scholar]
- 28.Padilla J, Calvo V, Penalver JC, et al. Survival and risk model for stage IB non-small cell lung cancer. Lung Cancer. 2002;36:43–48. doi: 10.1016/s0169-5002(01)00450-0. [DOI] [PubMed] [Google Scholar]
- 29.Diaconescu R, Lafond C, Whittom R. Treatment delays in non-small cell lung cancer and their prognostic implications. J Thorac Oncol. 2011;6:1254–1259. doi: 10.1097/JTO.0b013e318217b623. [DOI] [PubMed] [Google Scholar]
- 30.Toyoda Y, Nakayama T, Kusunoki Y, Iso H, Suzuki T. Sensitivity and specificity of lung cancer screening using chest low-dose computed tomography. Br J Cancer. 2008;98:1602–1607. doi: 10.1038/sj.bjc.6604351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Quarterman RL, McMillan A, Ratcliffe MB, Block MI. Effect of preoperative delay on prognosis for patients with early stage non-small cell lung cancer. J Thorac Cardiovasc Surg. 2003;125:108–114. doi: 10.1067/mtc.2003.93. [DOI] [PubMed] [Google Scholar]
- 32.Howlader N, Noone AM, Krapcho M, et al., editors. SEER Cancer Statistics Review, 1975–2009. Bethesda, MD: National Cancer Institute; 2012. [Google Scholar]
- 33.Aasebø U, Strøm HH, Postmyr M. The Lean method as a clinical pathway facilitator in patients with lung cancer. Clin Respir J. 2012;6:169–174. doi: 10.1111/j.1752-699X.2011.00271.x. [DOI] [PubMed] [Google Scholar]
- 34.Dovidio JF, Fiske ST. Under the radar: how unexamined biases in decision-making processes in clinical interactions can contribute to health care disparities. Am J Public Health. 2012;102:945–952. doi: 10.2105/AJPH.2011.300601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wassenaar TR, Eickhoff JC, Jarzemsky DR, Smith SS, Larson ML, Schiller JH. Differences in primary care clinicians’ approach to non-small cell lung cancer patients compared with breast cancer. J Thorac Oncol. 2007;2:722–727. doi: 10.1097/JTO.0b013e3180cc2599. [DOI] [PubMed] [Google Scholar]
- 36.Chambers SK, Dunn J, Occhipinti S, et al. A systematic review of the impact of stigma and nihilism on lung cancer outcomes. BMC Cancer. 2012;12:184. doi: 10.1186/1471-2407-12-184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schroen AT, Detterbeck FC, Crawford R, Rivera MP, Socinski MA. Beliefs among pulmonologists and thoracic surgeons in the therapeutic approach to non-small cell lung cancer. Chest. 2000;118:129–137. doi: 10.1378/chest.118.1.129. [DOI] [PubMed] [Google Scholar]
- 38.O’Rourke N, Edwards R. Lung cancer treatment waiting times and tumour growth. Clin Oncol (R Coll Radiol) 2000;12:141–144. doi: 10.1053/clon.2000.9139. [DOI] [PubMed] [Google Scholar]
- 39.Friberg S, Mattson S. On the growth rates of human malignant tumors: implications for medical decision making. J Surg Oncol. 1997;65:284–297. doi: 10.1002/(sici)1096-9098(199708)65:4<284::aid-jso11>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 40.Raz DJ, Zell JA, Ou SH, Gandara DR, Anton-Culver H, Jablons DM. Natural history of stage I non-small cell lung cancer: implications for early detection. Chest. 2007;132:193–199. doi: 10.1378/chest.06-3096. [DOI] [PubMed] [Google Scholar]


