Abstract
Purpose
Malignancies may cause urinary tract obstruction, which is often relieved with placement of a percutaneous nephrostomy tube, an internal double J nephro-ureteric stent (double J), or an internal external nephroureteral stent (NUS). We evaluated the affect of these palliative interventions on quality of life (QoL) using previously validated surveys.
Methods
Forty-six patients with malignancy related ureteral obstruction received nephrostomy tubes (n = 16), double J stents (n = 15), or NUS (n = 15) as determined by a multidisciplinary team. QoL surveys were administered at 7, 30, and 90 days after the palliative procedure to evaluate symptoms and physical, social, functional, and emotional well-being. Number of related procedures, fluoroscopy time, and complications were documented. Kruskal–Wallis and Friedman’s test were used to compare patients at 7, 30, and 90 days. Spearman’s rank correlation coefficient was used to assess correlations between clinical outcomes/symptoms and QoL.
Results
Responses to QoL surveys were not significantly different for patients receiving nephrostomies, double J stents, or NUS at 7, 30, or 90 days. At 30 and 90 days there were significantly higher reported urinary symptoms and pain in those receiving double J stents compared with nephrostomies (P = 0.0035 and P = 0.0189, respectively). Significantly greater fluoroscopy time was needed for double J stent–related procedures (P = 0.0054). Nephrostomy tubes were associated with more frequent minor complications requiring additional changes.
Conclusion
QoL was not significantly different. However, a greater incidence of pain in those receiving double J stents and more frequent tube changes in those with nephrostomy tubes should be considered when choosing palliative approaches.
Keywords: Quality of life, Nephrostomy, Nephroureteral stent, Ureteral obstruction
Introduction
In patients with malignancy-related urinary tract obstruction, relief of obstruction is usually achieved by placement of a percutaneous nephrostomy tube, an internalized double J nephroureteral stent (double J), or an internal/external nephroureteral stent (NUS). These approaches provide immediate treatment for obstruction with palliation of flank pain, deteriorating renal function, aversion of risk of infection, and rupture of calyces [1]. When choosing which of these approaches to use, factors including underlying infection, ability to cross the obstruction with a wire for stent placement, urinary continence, and preference of the referring clinician and patient are considered [2]. Each approach can relieve the obstruction, and it is not clear if either is more or less effective [3]. However, each intervention may cause untoward symptoms and may positively or negatively affect patient quality of life (QoL). Specifically, the placement of nephrostomy tubes mandates the use of a leg bag for gravity drainage. Double J stents and NUS may be associated with bladder irritation. Double J stents may entail potentially lengthy procedures for exchanging the stent every several months to maintain patency. Often, in our institution, these procedures are performed with the patient under general anesthesia. Because these approaches are for palliation in patients who often have terminal illness, it is important to assess and compare the effect of these methods of intervention from the patient’s perspective of symptom palliation and QoL.
Assessment of QoL has become an important measure of efficacy and outcome in clinical studies representing a valid outcome measure, particularly for procedures aimed at symptom palliation. QoL surveys can be used to compare outcomes between alternative treatment modalities and used in utility analysis as part of effectiveness comparison studies [4]. Joshi et al. [2] evaluated QoL in patients with nephroureteral lithiases who underwent nephrostomy or stent placement. A number of investigators have studied QoL in the setting of prostate cancer; however, they did not evaluate the effect of palliative procedures [5]. To date, there have been no studies comparing how QoL is affected in patients undergoing these palliative procedures for malignancy-related urinary tract obstruction.
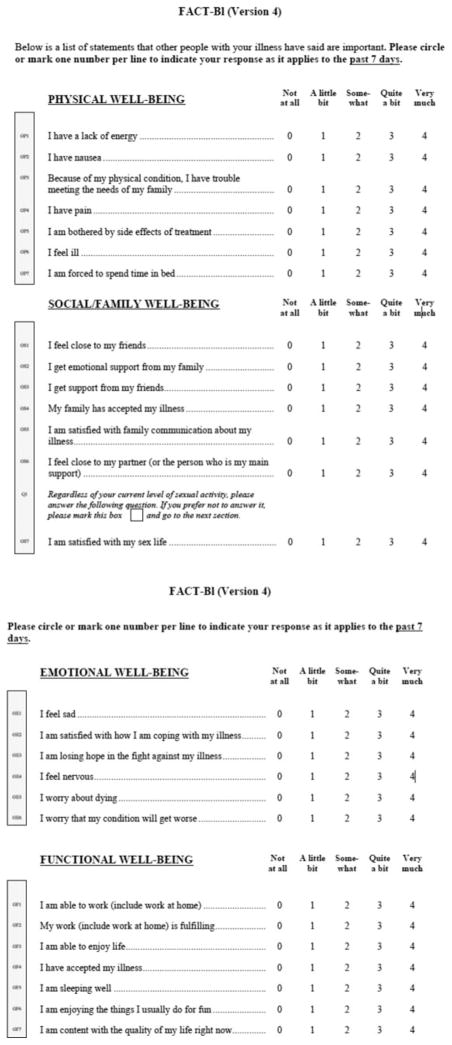
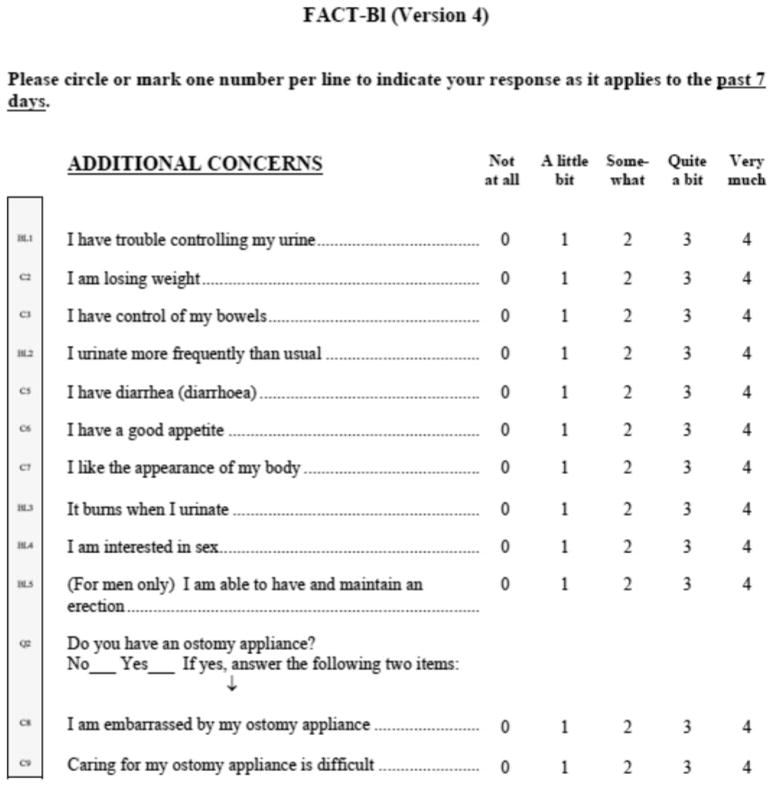
The purpose of the current study was to prospectively and longitudinally compare the impact of each of these approaches on patient disease-specific QoL using previously validated survey tools, including the Functional Assessment of Cancer Therapy–General and Bladder (FACT-BL) (Fig. 1) tool, which includes survey questions initially developed to evaluate urinary assessing urinary symptoms including; dysuria, urgency and frequency, pain and additional problems encountered in day-to-day life such as tube leakage and dislodgment [2, 6, 7] (Fig. 2). Details of procedures and related complications are also compared.
Fig. 1.
Functional assessment of cancer therapy–general and bladder (FACT-BL). Survey for assessment of physical, social/family, emotional and functional well-being. Taken, with permission, from www.facit.org/FACITOrg/Questionnaires. Copyright 1987, 1997 by David Cella, PhD
Fig. 2.
Survey for assessment of additional concerns related to symptoms and complications. Taken, with permission, from www.facit.org/FACITOrg/Questionnaires. Copyright 1987, 1997 by David Cella, PhD
Methods
The study was first approved by the Institutional Investigational Review Board. All patients signed written informed consent. Data collection was performed in accordance with Health Insurance Portability and Accountability Act regulations. The study is a prospective longitudinal survey-based assessment of QoL after palliative decompression procedures for malignancy-related ureteral obstruction. During a 16-month period, 45 consecutive patients with malignancy-related ureteral obstruction received either of the following: nephrostomy tubes (8.5F) (24 tubes in 15 patients [9 bilateral and 6 unilateral]), double J stents (8.5F, 22 to 26 cm) (24 stents in 15 patients [9 bilateral and 6 unilateral]), or NUS (8.5F, 22–26 cm) (22 stents in 15 patients [7 bilateral and 8 unilateral]). Thus, a total of 70 nephrostomy tubes (Boston Scientific, Natick, MA), double J stents (Boston Scientific), and NUS (Boston Scientific) were placed during the study (W. M., D. F.). The choice of tube was prospectively determined in a multidisciplinary manner. Factors including patient preference, urinary continence, and referring clinician preference were taken into account. Patients were initially referred to interventional radiology with symptomatic urinary obstruction with hydronephrosis, and/or palliation of pain, and/or deterioration of renal function, and/or infection. Enhanced computed tomography–confirmed malignancy-related obstruction in all patients. Conscious sedation was used in 15 nephrostomy tube and 12 nephroureteral stent placements, whereas general anesthesia was used in 1 nephrostomy and 3 nephroureteral stent placements. However, 65 % of the double J stent placements and exchanges were performed with the patient under general anesthesia. Nephrostomy tubes and NUS were fixed to the skin with a single stitch to prevent displacement. All procedures were performed with the patient receiving antibiotic coverage with ciprofloxacin. Patients were discharged home, once they were clinically stable, after temporary relief of the obstruction. At the time of discharge, patients with percutaneous nephrostomy tubes were instructed about nephrostomy tube care.
Previously validated and published questionnaires were designed to assess the impact of these palliative interventions on patient QoL. The initial development of these questionnaires was based on a literature review and the opinions of urologists as well as nursing staff [2, 8–11]. For each group, the questionnaire included a common validated health index (FACT-BL) as a generic measure of physical, social, functional, and emotional well-being (Fig. 1) (www.facit.org). An additional intervention-specific questionnaire was included for assessing urinary symptoms; dysuria, urgency and frequency, pain and additional problems encountered in day-zto-day life such as tube leakage and dislodgement (Fig. 2) [2] One interventional radiology attending and one fellow as well as one resident performed surveys, including 51 questions, by phone at 7, 30, and 90 days after initial placement of the tube or stent (D. F., W. M., T. N.). The data were tabulated, and median scores for each group of patients at each time point were analyzed statistically (C. M., B. J., C. S. L.). Correlations between the average of the scores related to symptoms and the average of the scores directly reflecting QoL were evaluated for each procedure at each time point.
Procedural details and complications requiring tube changes, in addition to routine changes every 3 months, were documented (S. L., T. N.). Procedure time for the initial placement and each tube change, as well as frequency of required tube changes, were compared. The use of additional pain medication and antibiotics for urinary tract infection was also documented.
Statistical Analysis
For each survey question, Kruskal–Wallis test was used to compare the expected median of the response variable of interest among the three procedure groups; if the overall comparison was statistically significant, Dunn’s test [12] was used for post hoc pairwise comparisons where the SAS macro written by Elliott and Hynan [13] was used to perform a multiple comparison post hoc test for Kruskal–Wallis analysis.
Friedman’s test [14–16], a nonparametric randomized block analysis, was used to determine whether there was a difference in QoL scores at 7, 30, and 90 days. If this test was statistically significant, post hoc (pairwise comparison) analysis was performed to decide which (time) groups were significantly different from each other. Post hoc analysis for Friedman’s test was performed using the “agricolae” package (R-2.13.2), which was downloaded online. Spearman’s rank correlation coefficient was used to assess the correlation between clinical outcomes and symptoms and QoL metrics within each procedure at each of 7, 30, and 90 days.
Results
Demographics for patients in the study are listed in Table 1. It is noteworthy that five of the patients with double J stents and one with nephrostomy tube underwent urinary-diverting ostomies for urinary diversion after cystectomy. However, none of the patients receiving NUS had ostomies.
Table 1.
Patient demographics
| Procedure | Malignancy | Sex | Stent/tube size | |
|---|---|---|---|---|
| Nephrostomy tube | 5 bladder | 1 colon | 10 Male | 8.5 F |
| 3 cervical | 1 lymphoma | 5 Female | ||
| 2 uterine | 1 sarcoma | |||
| 2 prostate | ||||
| Internal–external nephroureteral stents | 5 bladder | 1 anal | 10 Female | 8F, 22–26 cm |
| 4 cervical | 2 endometrial | 5 Male | ||
| 3 prostate | ||||
| Double J nephroureteral stents | 4 bladder | 2 ovarian | 11 Female | 8F, 22–26 cm |
| 6 cervical | 1 endometrial | 4 Male | ||
| 1 prostate | 1 fallopian |
QOL Evaluation
FACT-BL survey statements pertaining to physical, social and family, emotional, and functional well-being are listed in Figure 1. There were no statistically significant differences in responses to QoL survey questions evaluating physical well-being at 7, 30, or 90 days (P = 0.80, 0.93, and 0.23, respectively) (Table 2). There were no statistically significant differences in responses to QoL survey questions evaluating social and family well-being at 7, 30, or 90 days (P = 0.21, 0.15, and 0.35, respectively) (Table 3). There were also no statistically significant differences in responses to QoL survey questions evaluating emotional well-being at 7, 30, or 90 days (P = 0.56, 0.29, and 0.66, respectively) (Table 4). Furthermore, there were no statistically significant differences in responses to QoL survey questions evaluating functional well-being at 7, 30, or 90 days (P = 0.81, 0.78, and 0.98, respectively) (Table 5). Survey results related to clinical outcomes or symptoms, including pain, bladder irritation, dysuria, urinary frequency infection, and feeling ill, did not significantly correlate with an average score reflecting overall QoLe at 7, 30, and 90 days regardless of which procedure was performed (P > 0.05).
Table 2.
Summary of responses to physical well-being–related QoL surveya
| Procedure type | Median | Minimum | Maximum |
|---|---|---|---|
| 7 days after the procedureb | |||
| NUS | −0.85714 | −2.57143 | −0.14286 |
| Stent | −1 | −2.28571 | −0.28571 |
| Tube | −1.14286 | −0.14286 | −0.14286 |
| 30 days after the procedurec | |||
| NUS | −0.71429 | −2.71429 | 0 |
| Stent | −0.71429 | −2.28571 | −0.14286 |
| Tube | −1 | −2.42857 | 0 |
| 90 days after the procedured | |||
| NUS | −0.57143 | −2.42857 | −0.14286 |
| Stent | −0.85714 | −1.85714 | −0.42857 |
| Tube | −0.42857 | −1.28571 | −0.14286 |
Raw scores 0–4 are summated for each response. A negative value is applied as responses represent a negative effector on overall QoL
P value of Kruskal–Wallis test for comparison of physical well-being at 7 days after the procedure among the three procedure groups = 0.8. P value of Friedman’s test for comparison of physical well-being among the three time points within the NUS procedure group = 0.28
P value of Kruskal–Wallis test for comparison of physical well-being at 30 days after the procedure among the three procedure groups = 0.93. P value of Friedman’s test for comparison of physical well-being among the three time points within the Stent procedure group = 0.63
P value of Kruskal–Wallis test for comparison of physical well-being at 90 days after the procedure among the three procedure groups = 0.23. P value of Friedman’s test for comparison of physical well-being among the three time points within the TUBE procedure group = 0.13
Table 3.
Summary of responses to social and family well-being–related QoL surveya
| Procedure type | Median | Minimum | Maximum |
|---|---|---|---|
| 7 days after the procedureb | |||
| NUS | 3 | 1.85714 | 4 |
| Stent | 3.42857 | 0.42857 | 4 |
| Tube | 2.85714 | 0.71429 | 4 |
| 30 days after the procedurec | |||
| NUS | 3 | 1.42857 | 4 |
| Stent | 3.42857 | 0.42857 | 4 |
| Tube | 3 | 1.42857 | 3.71429 |
| 90 days after the procedured | |||
| NUS | 3.28571 | 2 | 4 |
| Stent | 3.42857 | 0.42857 | 4 |
| Tube | 3.14286 | 1.66667 | 3.85714 |
Raw scores 0–4 are summated for each response. A positive value is applied as responses represent a positive effector on overall QoL
P value of Friedman’s test for comparison of social/family well-being among the three time points within the NUS procedure group = 0.34. P value of Kruskal–Wallis test for comparison of social/family well-being at 7 days after the procedure among the three procedure groups = 0.21
P value of Friedman’s test for comparison of social/family well-being among the three time points within the STENT procedure group = 0.76. P value of Kruskal–Wallis test for comparison of social/family well being at 30 days after the procedure among the three procedure groups = 0.15
P value of Friedman’s test for comparison of social/family well-being among the three time points within the TUBE procedure group = 0.11. P value of Kruskal–Wallis test for comparison of social/family well-being at 90 days after the procedure among the three procedure groups = 0.35
Table 4.
Summary of responses to emotional well-being–related QoL surveya
| Procedure | Median | Minimum | Maximum |
|---|---|---|---|
| 7 days after the procedureb | |||
| NUS | −0.33333 | −1.83333 | 0.66667 |
| Stent | 0 | −1.16667 | 0.66667 |
| Tube | 0 | −0.83333 | 0.66667 |
| 30 days after the procedurec | |||
| NUS | −0.33333 | −1.5 | 0.5 |
| Stent | 0.08333 | −1.16667 | 0.66667 |
| Tube | 0 | −1.66667 | 0.66667 |
| 90 days after the procedured | |||
| NUS | −0.16667 | −0.83333 | 0.33333 |
| Stent | 0.08333 | −1.66667 | 0.66667 |
| Tube | 0.16667 | −0.83333 | 0.33333 |
Raw scores 0–4 are summated for each response. A negative value is applied as responses represent a negative effector on overall QoL
P value of Friedman’s test for comparison of emotional well-being among the three time points within the NUS procedure group = 0.66. P value of Kruskal–Wallis test for comparison of emotional well-being at 7 days after procedure among the three procedure groups = 0.56
P value of Friedman’s test for comparison of emotional well-being among the three time points within the STENT procedure group = 0.91. P value of Kruskal–Wallis test for comparison of emotional well-being at 30 days after the procedure among the three procedure groups = 0.29
P value of Friedman’s test for comparison of emotional well-being among the three time points within the TUBE procedure group = 0.65. P value of Kruskal–Wallis test for comparison of emotional well-being at 90 days after the procedure among the three procedure groups = 0.66
Table 5.
Summary of responses to functional well-being–related QoL surveya
| Procedure | Median | Minimum | Maximum |
|---|---|---|---|
| 7 days after the procedureb | |||
| NUS | 2.16667 | 1.14286 | 3.71429 |
| Stent | 2.28571 | 0.66667 | 3.14286 |
| Tube | 2.46429 | 1 | 3.71429 |
| 30 days after the procedurec | |||
| NUS | 2 | 1.14286 | 3.85714 |
| Stent | 2.64286 | 0.83333 | 3.57143 |
| Tube | 2.42857 | 0.85714 | 3.28571 |
| 90 days after the procedured | |||
| NUS | 2.57143 | 0.85714 | 3.28571 |
| Stent | 2.71429 | 0.83333 | 3.57143 |
| Tube | 2.42857 | 1.14286 | 4 |
Raw scores 0–4 are summated for each response. A positive value is applied as responses represent a positive effector on overall QoL
P value of Friedman’s test for comparison of functional well-being among the three time points within the NUS procedure group = 0.8. P value of Kruskal–Wallis test for comparison of functional well-being at 7 days after the procedure among the three procedure groups = 0.81
P value of Friedman’s test for comparison of functional well-being among the three time points within the STENT procedure group = 0.37. P value of Kruskal–Wallis test for comparison of functional well-being at 30 days after the procedure among the three procedure groups = 0.78
P value of Friedman’s test for comparison of functional well-being among the three time points within the TUBE procedure group = 0.80. P value of Kruskal–Wallis test for comparison of functional well-being at 90 days after the procedure among the three procedure groups = 0.98
Attrition from the study was low. Of the patients receiving double J stents, two could not be contacted at 7 days; one could not be contacted at 30 days; and one died before 90-day follow-up. Of the patients receiving nephrostomy tubes, one patient could not be contacted at 30 days, one withdrew from the study, one could not be contacted, and one died before 90-day follow-up. Of the patients receiving nephroureteral stents, one patient withdrew at 7 days, one withdrew before 30 days, one could not be contacted, one withdrew from the study, and one died before 90-day follow-up.
Procedural Details and Complications
Patients who had double J stents reported significantly more urinary symptoms, including dysuria and urinary frequency, compared with those with nephrostomy tubes and NUS at 30 and 90 days (P = 0.0035 and 0.0216, respectively) but not at 7 days after placement (P = 0.062). Furthermore, patients with double J stents had significantly greater use of pain medications at 30 and 90 days after placement (Friedman’s test; P = 0.0189) but not at 7 days after placement. Patients who received nephrostomy and NUS did not require significantly more pain medications at any time point. Although symptoms differed, there was no significant difference in occurrence of urinary tract infections in any group at 7, 30, and 90 days (P > 0.05), and there was no difference in antibiotic use. None of the procedures or symptoms significantly affected patient ability to have and maintain an erection or interest in sexual activity at each time point.
Median fluoroscopy times for initial tube placement and subsequent changes were 1.4 min (range 1–74] mean ± SD = 5.70 ± 11.55])/procedure in the nephrostomy tube group, 2.1 min (range 0.25–36.7 [mean ± SD = 3.82 ± 6.66])/procedure in the NUS group, and 4.12 min (range 0.21–43.6 [mean ± SD = 7.71 ± 9.35])/procedure in the double J stent group. There was a statistically significant difference in fluoroscopy time between the three groups (Kruskal–Wallis test; P = 0.005). Post hoc pairwise comparison using Dunn’s test showed significantly greater median fluoroscopy time for double J stent–related procedures compared with nephrostomy tube procedures, but there was no statistical difference when compared with NUS or when NUS is compared with nephrostomy tube procedure times.
During the course of this study, routine clinical care included changing nephrostomy tubes, NUS, and double J stents at 3-month intervals. More frequent changes were at times clinically required as a result of minor and major complications (Table 6). These included tube dislodgement, refractory pain, and refractory or severe urinary tract infection with “colonized,” clogged, or leaking tubes. In one case, a double J stent was exchanged for a nephrostomy tube when a malignancy-related vesicular vaginal fistula formed and urinary diversion was indicated. Patients with nephrostomy tubes had greater rates of complications, requiring additional tube changes, compared with those having NUS or double J stents (P = 0.051). During the course of the study, a total of 83 % of the nephrostomy tubes required additional tube changes, whereas 36 % of the nephroureteral stents and 16 % of the double J stents were changed because of these major and minor complications.
Table 6.
Complications requiring additional tube/stent changes
| Complication | Neph tube | NUS | Stent |
|---|---|---|---|
| Dislodged | 7 | 1 | 1 |
| Pain | 4 | 2 | 1 |
| Infection | 3 | 1 | 1 |
| Clogged | 4 | 2 | 0 |
| Leak | 1 | 2 | 0 |
| Fistula | 0 | 0 | 1 |
| Total | 20 | 8 | 4 |
Discussion
Validated QOL surveys can be used to evaluate palliative outcomes. A number of studies have evaluated the impact of various palliative procedures on QoL in patients with malignancy, including radioembolization, chemoembolization, radiofrequency ablation, ports for management of malignant effusions/ascites, and decompression for biliary obstruction [17–21]. The impact of stents versus nephrostomy tubes on QoL has been studied in the setting of obstructive nephrolithiasis [2] Evaluation of comparative effectiveness, including economic impact and QoL, is an emerging important area of study being applied to making decisions regarding reimbursement by organizations such as The Center for Medicare and Medicaid Services [22]. An increasing number of validated surveys have been developed to evaluate health-related QoL. The purpose of this study is to evaluate the effect of these palliative procedures on patient QoL using validated standardized surveys.
In this study, results may be confounded by the fact that most health-related QoL questions, in these validated surveys, are general and do not directly relate to the nephrostomy or stent. Hence, multiple other factors, particularly as they pertain to the patient’s underlying malignancy, may affect QoL. For this reason, questions from a previously published survey specific to nephrostomy and NUS placement were also included [2].
Responses to the questions about lower urinary tract symptoms indicated a high incidence of irritative urinary symptoms in patients with double J stents compared with those having nephrostomy tubes and NUS. This finding is in agreement with similar observations made by other investigators [2, 8, 9]. On further questioning, patients with stents experienced pain in the pelvis and bladder region, likely due to mechanical bladder irritation. It was surprising that patients with NUS did not have similar greater incidence of pain related to bladder irritation because similar length stents were used.
Although patients with double J stents report more urinary symptoms and an increased incidence of pain, there was no significant difference in health-related QoL, including physical and psychosocial well-being. Surprisingly, there was no statistically significant correlation of symptoms with QoL. Because nephrostomy tubes entail the presence of an external tube and drainage bag [10], it was hypothesized that having external tubes may adversely affect QoL, including emotional, functional, and physical well-being. However, in this pilot study, no significant differences in QoL were shown in patients with nephrostomy tubes, double J stents, or NUS. This was also showed by Joshi et al. [2] who evaluated QoL after nephrostomy tube versus double J stent placement for urinary obstruction caused by nephroureterolithiasis.
It is relevant that patients with nephrostomy tubes had greater rates of complications, including dislodgement, pain, infection, and clogging, requiring more frequent tube changes in addition to the routine 3-month tube changes. Nephrostomy tube dislodgement may likely be a function of patient compliance and reliability.
It may be concerning that patients with nephrostomy tubes required more frequent tube changes and that more fluoroscopy time was required for double J stent changes. In truly terminal patients, one might not expect multiple tube changes to be required. Patients in this study presented for palliation of symptoms attributable to malignancy-related ureteral obstruction. The disease was not necessarily imminently terminal. In fact, only three patients died during the 90-day course of the study.
An implication of the study is that QoL assessment can be applied to palliative procedures performed by interventional radiologists to further evaluate if these procedures are in fact palliating symptoms, particularly in terminal patients. The number of patients in this series is relatively small. With a larger sample size, it may be possible to detect a significant difference in QoL. However, this future research would likely require a multicenter study and is beyond the scope of the current single-center study. The development and use of formally validated intervention-specific questionnaires such as these, in a large randomized trial, should substantiate such assessments and their application in clinical practice.
A limitation of the study is that patients were not randomized to a treatment group. This was not usually practical, and it was most commonly decided in multidisciplinary discussion between the urologist and interventional radiologist. Initial nephroureteral stent placement may often be difficult in the setting of hydronephrosis. At times, initial placement of a nephrostomy tube to decompress the collecting system allows easier subsequent placement of a double J stent. When technically possible, initial antegrade double J stent placement was attempted. This might explain the high fluoroscopy times that were incurred in the JJ internal stent group in this study.
The largest limitation of this study is that patient QoL was not assessed at the start of the study. Hence, although QoL did not differ in the end, we do not know if all three groups started at a similar baseline or whether the change in QoL was different in any of the procedure groups. QoL was not evaluated at baseline because patients were not generally seen until just before the procedure in the interventional radiology preprocedure holding area. Workflow time limitations were prohibitive for completing preprocedure surveys. Furthermore, patients may have been initially seen by a resident, fellow, or nurse practitioner who may not have been familiar with the study. Because QoL was not significantly different for any of the procedures groups during the course of the study and patients all presented for palliation, it may be presumed that QoL was similar at the start of the study.
In conclusion, the results of this pilot study suggested that there is no significant difference in health-related QoL between these treatment groups. However, patients with double J stents have significantly more irritative urinary symptoms and pain versus patients with nephrostomy tubes or NUS. Furthermore, procedures for placement and exchange of double J stents require more fluoroscopy time and often require general anesthesia. This might suggest preferential consideration of nephrostomy tubes for patients with malignancy-related ureteral obstruction. However, nephrostomy tubes may be associated with minor complications requiring more frequent tube changes. These findings should be considered when performing these palliative therapies.
Acknowledgments
Statistical support for this publication was made possible by Grant No. UL1 RR024146 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research.
Footnotes
Conflict of interest No conflict of interest exists for any of the authors; W. Monsky, C. Molloy, B. Jin, T. Nolan, D. Fernando, S. Loh, C-Y, Lin.
Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH.
Contributor Information
Wayne Laurence Monsky, Email: wemonsky@msn.com, Department of Radiology, University of Washington Medical Center, 1959 Pacific Ave NE, Box 357115, Seattle, WA 98195, USA. Department of Radiology, University of California Davis Medical Center, Sacramento, CA, USA.
Chris Molloy, School of Medicine, University of California, Davis, Sacramento, CA, USA.
Bedro Jin, School of Medicine, University of California, Davis, Sacramento, CA, USA.
Timothy Nolan, Department of Radiology, University of California Davis Medical Center, Sacramento, CA, USA.
Dayantha Fernando, Department of Radiology, University of California Davis Medical Center, Sacramento, CA, USA. Department of Radiology, University of California, Irvine, Irvine, CA, USA.
Shaun Loh, Department of Radiology, University of California Davis Medical Center, Sacramento, CA, USA.
Chin-Shang Li, Division of Biostatistics, Department of Public Health Sciences, University of California, Davis, Davis, CA.
References
- 1.Dagli M, Ramchandani P. Percutaneous nephrostomy: technical aspects and indications. Semin Intervent Radiol. 2011;28(4):424–437. doi: 10.1055/s-0031-1296085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Joshi HB, Adams S, Obadeyi OO, Rao PN. Nephrostomy tube or ‘JJ’ ureteric stent in ureteric obstruction: assessment of patient perspectives using quality-of-life survey and utility analysis. Eur Urol. 2001;39(6):695–701. doi: 10.1159/000052529. [DOI] [PubMed] [Google Scholar]
- 3.Watson G. Double J (JJ) versus nephrostomy tube drainage. In: Yachia D, editor. Stenting the urinary system. Isis Medical Media; Oxford: 1998. pp. 109–119. [Google Scholar]
- 4.Feeney D, Labelle R, Torrance G. Integrating economic evaluations and quality of life assessments. In: Spiker B, editor. Quality of life assessments in clinical trials. Raven; New York, NY: 1990. pp. 71–82. [Google Scholar]
- 5.Sonn GA, Sadetsky N, Presti JC, Litwin MS. Differing perceptions of quality of life in patients with prostate cancer and their doctors. J Urol. 2013;189(Suppl 1):S59–S65. doi: 10.1016/j.juro.2012.11.032. [DOI] [PubMed] [Google Scholar]
- 6.Winstead-Fry P, Schultz A. Psychometric assessment of the Functional Assessment of Cancer Therapy-General (FACT-G) scale in a rural sample. Cancer. 1997;79(12):2446–2452. [PubMed] [Google Scholar]
- 7.Allareddy V, Kennedy J, West MM, Konety BR. Quality of life in long-term survivors of bladder cancer. Cancer. 2006;106(11):2355–2362. doi: 10.1002/cncr.21896. [DOI] [PubMed] [Google Scholar]
- 8.Pollard SG, MacFarlane R. Symptoms arising from double J ureteral stents. J Urol. 1988;139:37–38. doi: 10.1016/s0022-5347(17)42282-8. [DOI] [PubMed] [Google Scholar]
- 9.Bregg K, Riehle RA., Jr Morbidity associated with indwelling internal ureteral stents after shock wave lithotripsy. J Urol. 1989;141:510–512. doi: 10.1016/s0022-5347(17)40875-5. [DOI] [PubMed] [Google Scholar]
- 10.Stables DP. Percutaneous nephrostomy—technique, indications and results. Urol Clin North Am. 1982;9:15–29. [PubMed] [Google Scholar]
- 11.Guyatt G, Bombardier C, Tugwell P. Measuring diseases-specific quality of life in clinical trials. Can Med Assoc J. 1986;134:889–895. [PMC free article] [PubMed] [Google Scholar]
- 12.Dunn OJ. Multiple contrasts using rank sums. Technometrics. 1964;6:241–252. [Google Scholar]
- 13.Elliott AC, Hynan LS. A SAS® macro implementation of a multiple comparison post hoc test for a Kruskal–Wallis analysis. Comput Methods Programs Biomed. 2011;102:75–80. doi: 10.1016/j.cmpb.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 14.Friedman M. The use of ranks to avoid the assumption of normality implicit in the analysis of variance. J Am Stat Assoc. 1937;2:675–701. [Google Scholar]
- 15.Friedman MA. The use of ranks to avoid the assumption of normality implicit in the analysis of variance. J Am Stat Assoc. 1939;34:109. [Google Scholar]
- 16.Friedman M. A comparison of alternative tests of significance for the problem of m rankings. Ann Math Stat. 1940;11:86–92. [Google Scholar]
- 17.Steel J, Baum A, Carr B. Quality of life in patients diagnosed with primary hepatocellular carcinoma: hepatic arterial infusion of cisplatin versus 90-yttrium microspheres (therasphere) Psychooncology. 2004;13(2):73–79. doi: 10.1002/pon.725. [DOI] [PubMed] [Google Scholar]
- 18.Wible BC, Rilling WS, Drescher P, Hieb RA, Saeian K, Frangakis C, Chen Y, et al. Longitudinal quality of life assessment of patients with hepatocellular carcinoma after primary transarterial chemoembolization. J Vasc Intervent Radiol. 2010;21(7):1024–1030. doi: 10.1016/j.jvir.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 19.Wang YB, Chen MH, Yan K, Yang W, Dai Y, Yin SS. Quality of life after radiofrequency ablation combined with transcatheter arterial chemoembolization for hepatocellular carcinoma: comparison with transcatheter arterial chemoembolization alone. Qual Life Res. 2007;16(3):389–397. doi: 10.1007/s11136-006-9133-9. [DOI] [PubMed] [Google Scholar]
- 20.Monsky WL, Yoneda KY, MacMillan J, Deutsch LS, Dong P, Hourigan H, Schwartz Y, Magee S, Duffield C, Boak T, Cernilia J. Peritoneal and pleural ports for management of refractory ascites and pleural effusions: assessment of impact on patient quality of life and hospice/home nursing care. J Palliat Med. 2009;12(9):811–817. doi: 10.1089/jpm.2009.0061. [DOI] [PubMed] [Google Scholar]
- 21.Dy SM, Harman SM, Braun UK, Howie LJ, Harris PF, Jayes RL. To stent or not to stent: an evidence-based approach to palliative procedures at the end of life. J Pain Symptom Manage. 2012;43(4):795–801. doi: 10.1016/j.jpainsymman.2011.12.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Meyer AM, Carpenter WR, Abernethy AP, Stürmer T, Kosorok MR. Data for cancer comparative effectiveness research: past, present, and future potential. Cancer. 2012 doi: 10.1002/cncr.27552. [DOI] [PMC free article] [PubMed] [Google Scholar]