Abstract
Recent cognitive models of paranoid delusions highlight the role of self-concepts in the development and maintenance of paranoia. Evidence is growing that especially interpersonal self-concepts are relevant in the genesis of paranoia. In addition, negative interpersonal life-experiences are supposed to influence the course of paranoia. As dysfunctional family atmosphere corresponds with multiple distressing dyadic experiences, it could be a risk factor for the development and maintenance of paranoia. A total of 160 patients with a diagnosis of schizophrenia were assessed twice within 12 months. Standardized questionnaires and symptom rating scales were used to measure interpersonal self-concepts, perceived family atmosphere, and paranoia. Data were analyzed using longitudinal cross-lagged structural equation models. Perceived negative family atmosphere was associated with the development of more pronounced negative interpersonal self-concepts 12 months later. Moreover, paranoia was related to negative family atmosphere after 12 months as well. As tests revealed that reversed associations were not able to explain the data, we found evidence for a vicious cycle between paranoia, family atmosphere, and interpersonal self-concepts as suggested by theoretical/cognitive model of paranoid delusions. Results suggest that broader interventions for patients and their caretakers that aim at improving family atmosphere might also be able to improve negative self-concepts and paranoia.
Key words: self-schema, psychosis, structural equation modelling, relatives, social cognition
Introduction
Patients with schizophrenia show a quite heterogeneous set of different symptoms1 that can be categorized into 3 dimensions2: positive symptoms, negative symptoms, and disorganized symptoms. With regard to positive symptoms, delusions are a common feature, as about 70% of people diagnosed with a psychotic order report of delusions, paranoid delusions being the most common.3 Only a few models try to explain the whole heterogeneous phenomena of schizophrenia,4 and they usually focus on single features like, for example, paranoid delusions,5–8 which are particularly related to low well-being.9
Cognitive behavioral therapy (CBT) and family interventions are recommended in current reviews and guidelines for psychotic disorders,10,11 and the broad use of both treatments are supported by strong evidence.10,12,13
Cognitive models for paranoid delusions emphasize the influence of attributional style, negative emotions, cognitive biases, and low self-esteem/dysfunctional self-concepts.6,14–16 Interpersonal processes, such as a high level of expressed emotions (EEs) in families of patients with schizophrenia and experiences of social defeat, are underrepresented in these models, although their predictive value is evident.17,18 One reason for the limited consideration of interpersonal processes may be that the causality of the relationship between family atmosphere and relapse could not be clarified.18,19
Relapse rates20 and duration of untreated first-episode psychosis are associated with family conditions like perceived criticism21 and emotional over-involvement, both aspects of the high EE concept.25,26 Nevertheless, general literature on family atmosphere22,23 suggests that EE is often24 but not always25 related to higher relapse rates and criticism is a better predictor than the EE composite score in the long run.26
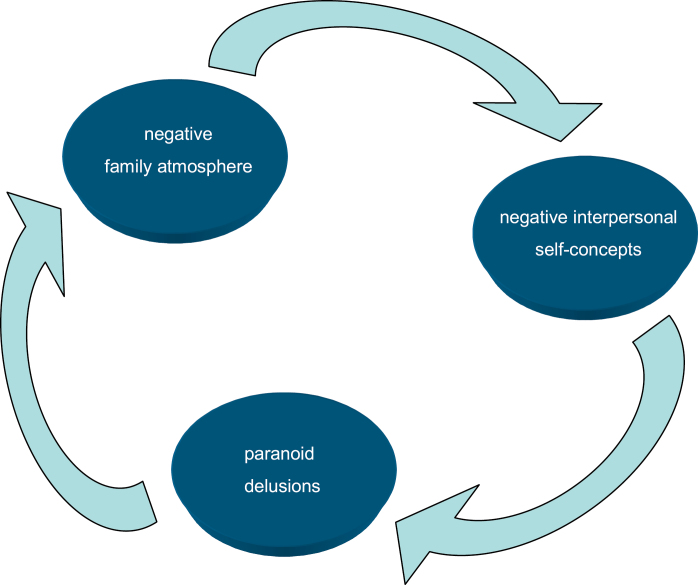
Other aspects of family atmosphere, like warmth in family relations or feelings of resignation, have often been neglected in studies investigating EE.27 In a cross-sectional study, Barrowclough and colleagues28 found an association between family atmosphere, negative self-evaluation, and positive symptoms. A more critical attitude from family members was associated with a more pronounced negative self-evaluation. In light of this evidence, a recent cognitive model of paranoid delusions proposed by Kesting and Lincoln8 integrates the influence of interpersonal stress (eg, negative family atmosphere) on interpersonal self-concepts and finally on the genesis and course of paranoia. In the core of their model, the authors propose a vicious cycle of interpersonal stress, self-concepts, and paranoid delusions.8 An adapted, testable model is displayed in figure 1.
Fig. 1.
Vicious cycle between paranoia, family atmosphere, and interpersonal self-concepts, adapted from Kesting and Lincoln.8
The purpose of the present study was to test the proposed interpersonal expansion to established cognitive models of delusions.15 First, we investigated the longitudinal relationships between family atmosphere and paranoid delusions. Second, we explored the relationships between family atmosphere and interpersonal self-concepts. We expected directional pathways leading from paranoid delusions to family atmosphere and from family atmosphere to interpersonal self-concepts, not vice versa, as proposed by Kesting and Lincoln.8 Third, the whole model was tested as displayed in Figure 1.
Methods
Subjects and Procedures
The sample comprised 160 outpatients from a randomized controlled trial for the treatment of negative symptoms with CBT (TONES-study, ISRCTN25455020). The Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) diagnosis of schizophrenia was confirmed by a structured clinical interview (SCID-I). The design and the characteristics of the patient sample of the TONES-study are described in detail elsewhere.29 Briefly, the patients involved in the trial presented at least a moderate level of negative symptoms but no severe positive symptoms or severe depression at baseline (any item of the Positive and Negative Symptom Scale [PANSS] positive scale or depression item ≥6). All participants gave informed consent. The study protocol was approved by the local ethics committees. The two treatment groups did not differ significantly with regard to any of the variables included in the present analyses.30 Patients received monetary rewards for all assessments; external data monitoring was implied and the loss of data to follow-up was 19%. For 160 participants out of 198, baseline and follow-up data (12 months) were available. Across all variables and measurements, a total of 2.3% of data points were missing. Missing data on single scores were imputed with expectation–maximization imputation models. We used maximum-likelihood estimation, which assumes that missing values were missing at random conditional on the other variables in the model.
Statistical Analyses
Results of the clinical trial, published by Klingberg et al,30 showed no differences between the two treatment groups (cognitive remediation vs CBT). Nevertheless, we conducted an ANCOVA in our subsample in order to test treatment effects on the different groups, using family atmosphere at follow-up as the dependent variable and family atmosphere at baseline as well as treatment group as independent variables. Structural equation modelling (SEM) was used in order to test the longitudinal relations between family atmosphere, symptoms, and interpersonal self-concept. SEM is a technique allowing the study of latent, ie, unobserved, variables. The latent constructs are measured by observed indicators. In our models, all latent constructs were operationalized with 2 indicators each. First, we checked the appropriateness of the measurement models by investigating factor loadings. In a second step, we fitted cross-lagged models to test the longitudinal associations between family atmosphere, symptoms, and interpersonal self-concepts. Models were compared regarding parameter estimates and global fit. A total of 3 longitudinal models were defined using data from baseline (t0) and 12-month follow-up (t1) assessments. We compared nested models by restricting these models stepwise. We analyzed separate models for paranoid delusions, interpersonal self-concepts, and a combination of the 2. Consequently, both constructs of interest (paranoid delusions and interpersonal self-concepts) were tested in different models: (a) an unrestricted model, in which all possible paths were modelled, as seen in figure 2; (b) a model incorporating only a direct pathway from family atmosphere to the variable of interest. These models omit a path from baseline variable of interest to t1 family atmosphere; (c) a model with a direct path between the variable of interest and family atmosphere, omitting the path from baseline family atmosphere to the t1 variable of interest; (d) a restricted model omitting both cross-lagged pathways, allowing only for concurrent associations and paths between t0 and t1 within the same construct (stability). The error indicators were correlated across time to control for bias due to indicator-specific variance.31 For each construct, the loading of the first indicator was set to 1 and the factor loading of the second indicator was constrained to be equal across time by implying factorial invariance in order to improve estimability. Cross-sectional covariations between the constructs were unrestricted. For the comparison of the nested models, the best-fitting models were compared with the more restricted model using a chi-squared difference test; a statistically significant (P < .05) result suggests a more adequate fit of the less restricted model in comparison to the more restricted one. On the contrary, a statistically nonsignificant result suggests that restricting the model does not lead to an inferior fit.
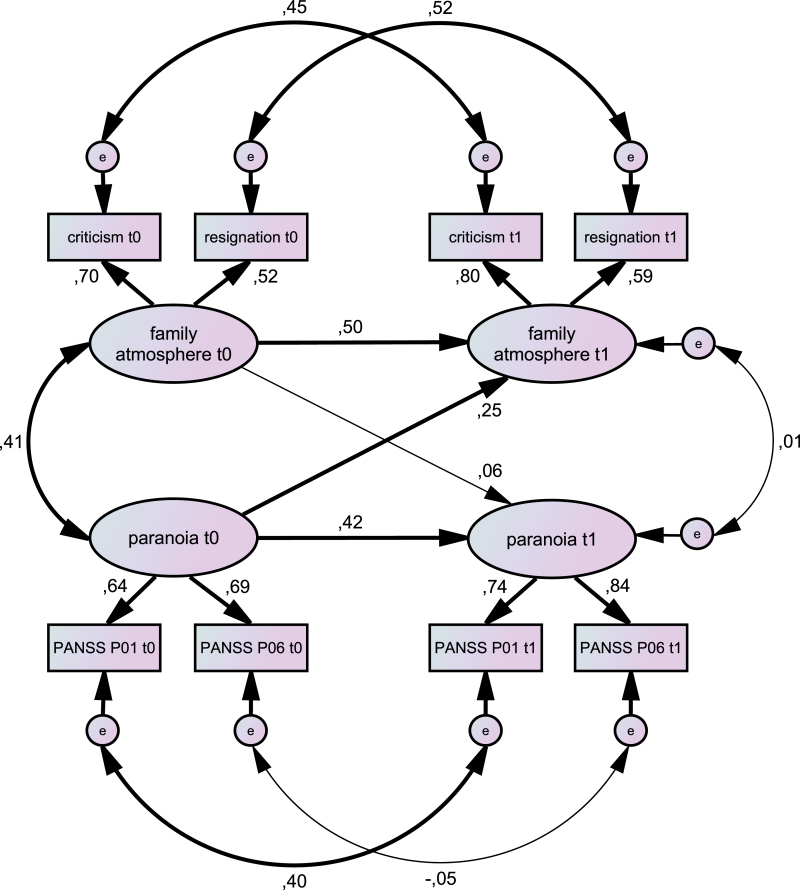
Fig. 2.
Unrestricted longitudinal model of family atmosphere and paranoia. Rectangles indicate observed indicator variables. Ovals indicate unobserved latent variables. Single-headed arrows indicate standardized regression weights; double-headed arrows indicate correlations. Bold paths are statistically significant (P < .05), narrow paths are not. Positive and Negative Symptom Scale (PANSS) P01, delusions; PANSS P06, suspiciousness/persecution. The overall model fit was χ2 = 4.71, df = 12, P = .97; Comparative Fit Index (CFI) = 1.000, Tucker–Lewis Index (TLI) = 1.055, root mean squared error of approximation (RMSEA) = 0.000 (0.000–0.000).
Moreover, we investigated the significance of the paths with theoretical relevance. We checked assumptions of SEM in a preparatory investigation of skewedness and kurtosis of the modelled indicators.32 All analyses were performed with AMOS and SPSS (Version 21.0. Armonk, NY: IBM Corp.).
Measures and Latent Variable Construction
For the purpose of structure equation modeling, we grouped pairs of scales to build latent constructs.
Paranoia was measured by the “delusions” item (P1) of the PANSS33 and the “suspiciousness/persecution” item (P6). The standardized factor loadings for paranoia were between 0.65 and 0.89, respectively.
Interpersonal self-concept was assessed using 2 subscales of the Frankfurt Self-Concept Scales (FSKN): “valued by others” (FSVO) and “emotions and relations to others” (FSEO). The internal consistency of the scales has proven to be highly satisfactory (α = 0.93–0.97; n = 1794).34 The questionnaire has been used frequently in psychosis research.35–37 The subscale FSVO investigates the self-concept of being respected, trusted, loved, and accepted by relevant others and is assessed by 6 items (eg, I feel loved by my family). The subscale FSEO consists of 6 items (eg, In general I feel I can trust others). These items paraphrase the perceived personal ability to build intense/deep relationships, and the belief of being unconditionally accepted by others/for “what you are,” even with individual weaknesses. The factor loadings of these subscales were 0.70 and 0.90.
Family atmosphere was measured using 2 subscales from the German “Fragebogen zur Erfassung der Familienatmosphäre” (FEF),38 which assesses perceived negative family atmosphere, especially blame and neglect by a significant relative. In previous research, the instrument showed good reliability38 and moderate correlations to the EE status assessed with the “five minute speech sample.”39 The scales criticism (eg, “he/she rebukes me a lot”; 10 items) and resignation (eg, “he/she is not interested in how I am doing”; 8 items) were used. The factor loadings of the 2 indicators for family atmosphere ranged from 0.44 to 0.83.
Results
With regard to the ANCOVA assessing differences in family atmosphere, there were no statistically significant differences between the 2 treatment groups. Moreover, results of the clinical trial, published by Klingberg et al,30 showed no differences between the 2 treatment groups (cognitive remediation vs CBT). Thus, it was not necessary to consider treatment group in further analyses. The mean age of the sample (n = 160) was 36.9 years (SD = 9.8), including 94 men and 66 women (41%), and most patients had graduated from high school (n = 84, 52%). The majority were single (n = 95, 59%) and unemployed (n = 116, 72%). The mean length of illness was 9.2 years (SD = 8.3); only a few patients (n = 11, 7%) presented with a first episode of psychosis. The mean item score of the PANSS modified negative syndrome (Items N1, N2, N3, N4, N6, G7, G16) scale was 3.02 (SD = 0.80), indicating moderate negative symptoms in the sample; the positive subscale mean (Items P1, P2, P3, P4, P5, P6, P7) was 1.51 (SD = 0.41), indicating mild positive symptoms at baseline. The mean Global Assessment of Functioning (GAF) score was 59.23 (SD = 8.81), indicating a moderate to severe impairment in social functioning. More than half of the patients (n = 86) had close social relationships outside their family. Many patients (n = 77, 48%) met their relatives on a daily basis, but other patients reported less frequent contact. The average verbal IQ score (Mehrfachwahl-Wortschatz-Intelligenztest, MWT-B) was 107.96 (SD = 17.07).
The models incorporating paranoia, interpersonal self-concepts, and family atmosphere are shown in Table 1. With regard to paranoid delusions, the unrestricted model is presented in figure 2. The standardized coefficient between paranoia and family atmosphere was 0.25 (P = .046). Moreover, the chi-square statistics for the model including this path fitted significantly better than the restricted model (df = 1; Δχ2 = 3.98; P = .046). The model including the other cross-lagged path was not superior to the restricted model (df = 1; Δχ2 = 1.48; P = .700).
Table 1.
Goodness-of-Fit Indices for Models Incorporating Family Atmosphere, Paranoia, and Interpersonal Self-Concepts
| χ2 | χ2/df | CFI | TLI | RMSEA | BIC | AIC | Standardized Coefficient (SE; P) | |
|---|---|---|---|---|---|---|---|---|
| Threshold for good models | n.a. | ≤2 | ≥0.950 | ≥0.950 | ≤0.050 | n.a. | n.a. | P < .05 |
| Paranoia | ||||||||
| a) Unrestricted model (df = 12) | 4.71; P = .97 | 0.39 | 1.000 | 1.055 | 0.000 | 126.52 | 52.74 | |
| b) FA t0 → PA t1 (df = 13) | 8.74; P = .79 | 0.67 | 1.000 | 1.030 | 0.000 | 125.47 | 54.74 | 0.06 (0.54; 0.665) |
| c) PA t0 → FA t1 (df = 13) | 4.91; P = .98 | 0.38 | 1.000 | 1.056 | 0.000 | 121.64 | 50.91 | 0.25 (0.51; 0.046) |
| d) Restricted model (df = 14) | 8.89; P = .83 | 0.64 | 1.000 | 1.033 | 0.000 | 120.54 | 52.89 | |
| Interpersonal self-concept | ||||||||
| a) Unrestricted model (df = 10) | 15.79; P = .11 | 1.58 | 0.990 | 0.971 | 0.060 | 147.74 | 67.79 | |
| b) FA t0 →IPS t1 (df = 11) | 15.85; P = .15 | 1.44 | 0.991 | 0.978 | 0.053 | 142.73 | 65.85 | −0.33 (0.64; 0.044) |
| c) IPS t0 → FA t1 (df = 11) | 21.71; P = .03 | 1.97 | 0.981 | 0.951 | 0.078 | 148.59 | 71.71 | −0.04 (0.05; 0.787) |
| d) Restricted model (df = 12) | 22.39; P = .03 | 1.87 | 0.981 | 0.956 | 0.074 | 144.19 | 70.39 | |
| Combined model | ||||||||
| a) Unrestricted model (df = 36) | 49.39; P = .07 | 1.37 | 9.82 | 9.66 | 0.048 | 262.55 | 133.39 | |
| b) Vicious cycle model (df = 39) | 50.72; P = .10 | 1.30 | 9.84 | 9.73 | 0.043 | 248.65 | 128.72 | |
| c) Restricted model (df = 36) | 68.74; P = .06 | 1.64 | 9.63 | 9.42 | 0.063 | 251.45 | 140.74 | |
Note: FA, family atmosphere; PA, paranoia; IPS, interpersonal self-concept; df, degrees of freedom; χ2/df, normal chi-squared statistic; SE, standard error of the unstandardized coefficient; P, significant level of the coefficient; CFI, Comparative Fit Index; TLI, Tucker–Lewis Index; RMSEA, root mean squared error of approximation; BIC, Bayes Information Criterion; AIC, Akaike’s Information Criterion; n.a., not applicable (no absolute threshold definable).
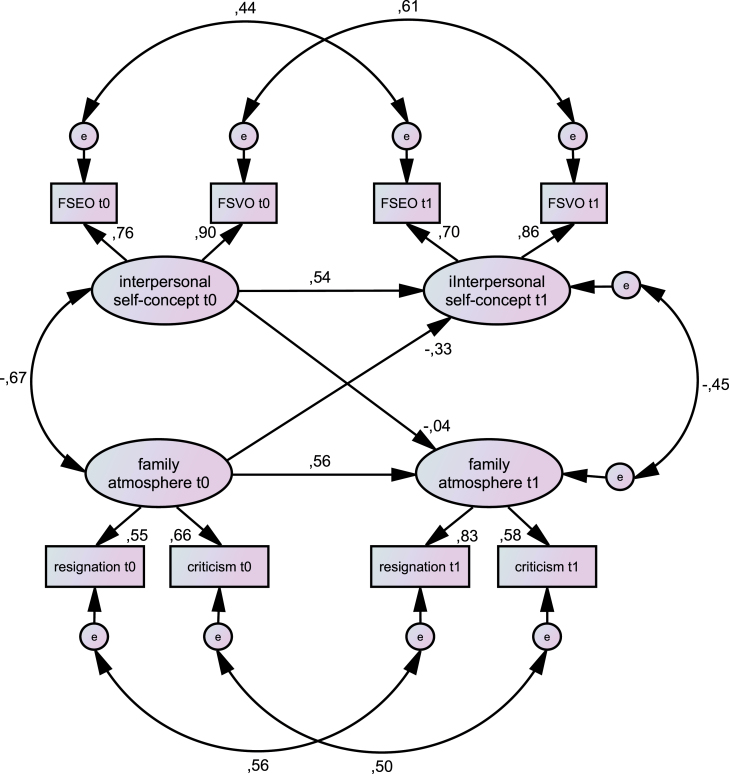
With regard to interpersonal self-concept, models implying factorial invariance, technically by constraining the factor loadings of the second indicator to be invariant across time, resulted in an unacceptable fit. Accordingly, these assumptions were not made for models incorporating interpersonal self-concepts. With regard to interpersonal self-concepts, the model including a path between family atmosphere and interpersonal self-concepts showed better fitting indices in comparison to other models. These models are summarized in Table 1. The unrestricted model is presented in figure 3. The standardized coefficient on the path between family atmosphere at baseline and interpersonal self-concepts at follow-up was −0.33 (P = .044). Moreover the chi-square statistics of the cross-lagged model showed a significantly better fit in comparison to the restricted model (df = 1; Δχ2 = 6.54; P = .011).
Fig. 3.
Longitudinal model of family atmosphere and interpersonal self-concept. Rectangles indicate observed indicator variables. Ovals indicate unobserved latent variables. Figures on single-headed arrows indicate standardized regression weights; figures on double-headed arrows indicate correlations. Bold paths are significant (P < .05), narrow paths are not. FSVO, valued by others; FSEO, emotions and relations to others. The overall model fit was χ2 = 15.79, df = 10, P = .11; Comparative Fit Index (CFI)= 0.990, Tucker–Lewis Index (TLI) = 0.971, root mean squared error of approximation (RMSEA) = 0.060 (0.000–0.114).
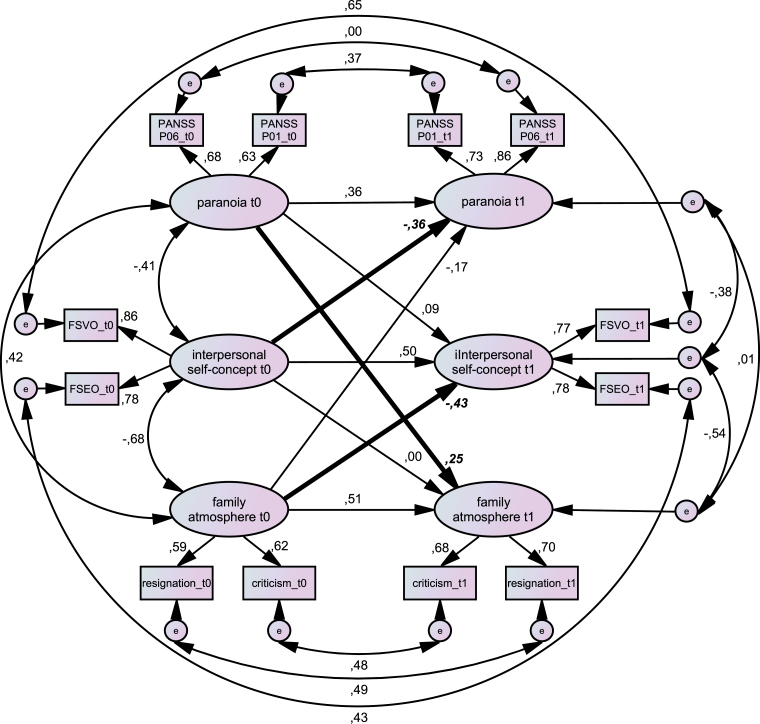
In the next step, we fitted a composite model of the constructs that showed longitudinal cross-lagged associations in the previous models. The combined models of paranoia, interpersonal self-concept, and family atmosphere are in line with our hypotheses. As expected, a model including the three proposed paths representing the vicious cycle model (see figure 1) shows a better fit than a restricted model without any cross-lagged paths between constructs (df = 3; Δχ2 = 15.972; P = .001). These significant (P < .05) paths are (1) between paranoia (t0) and family atmosphere (t1); (2) between family atmosphere (t0) and interpersonal self-concepts (t1); and (3) between interpersonal self-concepts (t0) and paranoia (t1). A model including paths in the opposite direction (family atmosphere (t0) and paranoia (t1); interpersonal self concepts (t0) and family atmosphere (t1); paranoia (t0) and interpersonal self-concepts (t1)) did not result in a better fit in comparison to a restricted model (df = 3; Δχ2 = 1.442; P = .696). The unrestricted model is displayed in figure 4 and Table 1. Details of all models are summarized in supplement 1. A model including treatment as a covariate is displayed in supplement 4. The main findings remain comparable if analyses controlled for treatment, as all paths of the vicious cycle model are still statistically significant.
Fig. 4.
Longitudinal model of paranoid delusions, interpersonal self-concept, and family atmosphere. Rectangles indicate observed indicator variables. Ovals indicate unobserved latent variables. Single-headed arrows indicate standardized regression weights; double-headed arrows indicate correlations. Bold arrows and parameters represent significant cross-lagged paths. Positive and Negative Symptom Scale (PANSS) P01, delusions; PANSS P06, suspiciousness/persecution; Frankfurt Self-Concept Scales: (FSVO, valued by others; FSEO, emotions and relations to others). The overall model fit was χ2 = 49.39, df = 36, P = .068; Comparative Fit Index (CFI) = 0.982, Tucker–Lewis Index (TLI) = 0.966, root mean squared error of approximation (RMSEA) = 0.048 (0.000–0.079).
Discussion
We examined longitudinal relationships between family atmosphere, interpersonal self-concepts, and paranoia in patients with schizophrenia. As expected, the presence of paranoid delusions at first assessment predicted a negative family atmosphere 12 months later. Furthermore, a negative family atmosphere at first assessment is related to dysfunctional interpersonal self-concepts 12 months later. Moreover, negative interpersonal self-concepts at first assessment are connected with paranoia 12 months later. Although we assessed these variables at 2 different points in time, our results suggest that a vicious circle might exist between a negative family atmosphere that leads to negative interpersonal self-concepts that might induce paranoia, as suggested by the theoretical model by Kesting and Lincoln.8 Not only did we test the hypothesized model against a situation in which the variables are unrelated, moreover we have excluded a vicious circle in which the circle moves in the opposite direction. Strictly speaking, vicious circles are always vicious repeating spirals, the model presented in figure 1 is a testable model, but a spiral would actually be a better representation of reality. In general, our findings indicate that theoretical models regarding the formation and maintenance of paranoia should incorporate interpersonal self-concepts and family atmosphere as possible causal factors. The vicious cycle displayed in figure 1 could be one complementary feature of models explaining paranoia.
The finding that a perceived negative family atmosphere might create negative interpersonal concepts is in line with several main assumptions of therapies like CBT, Schema Therapy, or psychodynamic approaches and is supported by several studies and meta-analyses in almost all patients with mental disorders. Moreover, the assumption that negative interpersonal self-concepts are involved in the formation and maintenance of paranoia is in line with cognitive models of paranoia.6,15
Our finding of a longitudinal relationship between paranoid delusions and family atmosphere suggest that paranoia is disturbing the family atmosphere in a severe way. This relationship remained significant even when interpersonal self-concepts were entered into the model. A recent publication highlights the predictive worth of perceived criticism to quality of life and to the patients’ conceptions of their illness.40 Our results are in line with Barrowclough and colleagues,28 who reported that negative self-concepts mediate the association between family atmosphere and paranoia on a cross-sectional level. Our findings of a vicious cycle presented in figure 1 confirm and extend their findings on a longitudinal level. Moreover, our results support the studies with higher relapse rates in families with a negative atmosphere and high EE.20,21 However, negative family atmosphere not only affects patients with schizophrenia, but also represents an increased burden to the caregiver as well.41 Thus, increased stress and the burden of care might lead to a more pronounced level of EEs, thus, forming a second vicious circle between paranoia, family atmosphere, increased burden of care, and more pronounced paranoia, as well.42 These hypothesized cycles act slowly, which could explain why family interventions lasting a longer time seem to be more effective.43
Possible ways in which the family atmosphere might influence paranoia are suggested by an experimental study showing increased levels of anxiety, anger, and distress after exposure to a person’s speech that contained a high level of EEs. Moreover, patients who were exposed to this speech showed an increase in general positive symptom like perceived controllability of voices, a higher level of delusional preoccupation and conviction.44 Thus, it is possible that the association between a negative family atmosphere and paranoia might be mediated by an increase of negative emotions. Negative emotions, especially anxiety and depression, are related to paranoid delusions on a cross-sectional and longitudinal level.45 Moreover, in experimental studies, patients with schizophrenia who react with increased levels of negative emotions to stress induced by an urban environment show a more pronounced level of paranoia as well.46 In addition, patients with schizophrenia use dysfunctional emotion regulation strategies (suppression of emotions) more often in comparison to controls.47–51 Thus, it could be speculated that the impact of a negative family atmosphere on paranoia could be mediated by negative emotions and problems that patients with schizophrenia have regulating their emotions. In addition, a negative family atmosphere might be a maintaining factor that increases pre-existing negative interpersonal concepts that are related to paranoia. A dysfunctional communication style within a family could mediate the association between interpersonal self-concepts and paranoia.52
This study has several strengths. The first strength is the longitudinal design, enabling stronger tests of causality in comparison to cross-sectional designs. The second strength is the clearly theory-driven test of relationships between symptoms and family atmosphere. The third strength is the use of cross-lagged structural equation models to test these hypotheses, as this method allows for estimation of longitudinal effects while controlling for multiple associations within the model.
Nevertheless, some limitations need to be considered. First, models with 3 latent variables and 2 assessments are usually called half-longitudinal because assumptions are made, like stationarity (eg, covariances are constant over time) and cannot be tested.31 A design with 3 datapoints would have allowed a test of the assumption of stationarity and would have been more robust against biases. Second, perceived family atmosphere, like perceived criticism, is usually measured with just 1 item,53 but in our study it was measured with a well-established questionnaire; however, both measures correlate substantially, thus, the results are not completely comparable.39 In our study, family atmosphere as well as self-concepts are measured by self-reports, additional observer-based ratings of these constructs would have allowed for a more differentiated view. Paranoia was measured with only 2 items of the PANSS, more indicators could have enhanced reliability and validity. Third, we examined paranoid delusions in a randomized controlled trial sample with an initially low amount of positive symptoms. Thus, our findings may be limited to a subgroup of people with persistent negative symptoms, however, about 85% of the screened people diagnosed with schizophrenia fulfilled these wide symptom related inclusion criteria.30 Then again, the relative high levels of negative symptoms may have influenced social competences and thereby interpersonal self-concepts and interpersonal relationships. Lastly, one could argue that differential treatment effects could have influenced the change in the variable of interest; we repeated all analyses controlling for treatment effects and no treatment effect between the 2 therapies occurred.
If negative interpersonal concepts and family atmosphere are important causal factors in the formation and maintenance of paranoia, it might be highly important to include these variables in the therapy process, eg, in standardized diagnostic, case formulation, and planning of interventions. When it is not possible to change paranoid delusions directly using cognitive methods and behavioral interventions,54 it could be possible to target delusions in an indirect way by improving negative interpersonal self-concepts and family atmosphere, if possible. This is especially important, as these factors are involved in the maintenance and relapse of paranoid delusions. Especially family atmosphere as a target of CBT has been forgotten, possibly because newer studies did not always support evidence for family interventions55 and family interventions pose more pronounced organizational barriers. The possibility to improve interpersonal self-concepts by changing family atmosphere and thus reduce paranoid persecutions on the long run could give new perspectives for the broader implementation of effective psychosocial interventions for patients and their carers.56,57
Supplementary Material
Supplementary material is available at http://schizophreniabulletin.oxfordjournals.org.
Funding
German Research Foundation (Deutsche Forschungsgemeinschaft, grants Kl 1179/2-1 and Kl 1179/3-1).
Supplementary Material
Acknowledgments
We thank Johannes Harbort, Michael Ruch, Hanna Smoltczyk, and Maia Weickert for their contribution in the assessments and Anne McWerthor for proofreading. The authors have declared that there are no conflicts of interest in relation to the subject of this study.
References
- 1. Keshavan MS, Nasrallah HA, Tandon R. Schizophrenia, “Just the Facts” 6. Moving ahead with the schizophrenia concept: from the elephant to the mouse. Schizophr Res. 2011;127:3–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. van Os J, Kapur S. Schizophrenia. Lancet 2009;374:635–645. [DOI] [PubMed] [Google Scholar]
- 3. Kimhy D, Goetz R, Yale S, Corcoran C, Malaspina D. Delusions in individuals with schizophrenia: factor structure, clinical correlates, and putative neurobiology. Psychopathology. 2005;38:338–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Howes OD, Murray RM. Schizophrenia: an integrated sociodevelopmental-cognitive model. Lancet. 2014;383:1677–1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bentall RP, Kinderman P, Kaney S. The self, attributional processes and abnormal beliefs: towards a model of persecutory delusions. Behav Res Ther. 1994;32:331–341. [DOI] [PubMed] [Google Scholar]
- 6. Freeman D. Suspicious minds: the psychology of persecutory delusions. Clin Psychol Rev. 2007;27:425–457. [DOI] [PubMed] [Google Scholar]
- 7. Salvatore G, Lysaker PH, Popolo R, Procacci M, Carcione A, Dimaggio G. Vulnerable self, poor understanding of others’ minds, threat anticipation and cognitive biases as triggers for delusional experience in schizophrenia: a theoretical model. Clin Psychol Psychother. 2012;19:247–259. [DOI] [PubMed] [Google Scholar]
- 8. Kesting ML, Lincoln TM. The relevance of self-esteem and self-schemas to persecutory delusions: a systematic review. Compr Psychiatry. 2013;54:766–789. [DOI] [PubMed] [Google Scholar]
- 9. Freeman D, Startup H, Dunn G, et al. Persecutory delusions and psychological well-being. Soc Psychiatry Psychiatr Epidemiol. 2014;49:1045–1050. [DOI] [PubMed] [Google Scholar]
- 10. Mueser KT, Deavers F, Penn DL, Cassisi JE. Psychosocial treatments for schizophrenia. Annu Rev Clin Psychol. 2013;9:465–497. [DOI] [PubMed] [Google Scholar]
- 11. Excellence NIfHaC. Psychosis and schizophrenia in adults: treatment and management (CG178). London: National Institute for Health and Clinical Excellence; 2014. [PubMed] [Google Scholar]
- 12. Pharoah F, Mari J, Rathbone J, Wong W. Family intervention for schizophrenia. Cochrane Db Syst Rev 2010(12). doi: 10.1002/14651858.CD000088.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Turner DT, van der Gaag M, Karyotaki E, Cuijpers P. Psychological interventions for psychosis: a meta-analysis of comparative outcome studies. Am J Psychiatry. 2014;171:523–538. [DOI] [PubMed] [Google Scholar]
- 14. Bentall RP, Corcoran R, Howard R, Blackwood N, Kinderman P. Persecutory delusions: a review and theoretical integration. Clin Psychol Rev. 2001;21:1143–1192. [DOI] [PubMed] [Google Scholar]
- 15. Garety PA, Bebbington P, Fowler D, Freeman D, Kuipers E. Implications for neurobiological research of cognitive models of psychosis: a theoretical paper. Psychol Med. 2007;37:1377–1391. [DOI] [PubMed] [Google Scholar]
- 16. Freeman D, Garety P. Advances in understanding and treating persecutory delusions: a review. Soc Psychiatry Psychiatr Epidemiol. 2014;49:1179–1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Freeman D, Evans N, Lister R, Antley A, Dunn G, Slater M. Height, social comparison, and paranoia: an immersive virtual reality experimental study. Psychiatry Res. 2014;218:348–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hooley JM. Expressed emotion and relapse of psychopathology. Annu Rev Clin Psychol. 2007;3:329–352. [DOI] [PubMed] [Google Scholar]
- 19. Wearden AJ, Tarrier N, Barrowclough C, Zastowny TR, Rahill AA. A review of expressed emotion research in health care. Clin Psychol Rev. 2000;20:633–666. [DOI] [PubMed] [Google Scholar]
- 20. van Os J, Marcelis M, Germeys I, Graven S, Delespaul P. High expressed emotion: marker for a caring family? Compr Psychiatry. 2001;42:504–507. [DOI] [PubMed] [Google Scholar]
- 21. Alvarez-Jimenez M, Gleeson JF, Cotton SM, Wade D, Crisp K, Yap MBH, McGorry PD. Differential predictors of critical comments and emotional over-involvement in first-episode psychosis. Psychol Med. 2010;40:63–72. [DOI] [PubMed] [Google Scholar]
- 22. Brown GW, Monck E, Carstairs GM, Wing JK. Influence of family life on the course of schizophrenic illness. Br J Prev Soc Med. 1962;16:55–68. [Google Scholar]
- 23. Brown GW, Birley JL, Wing JK. Influence of family life on the course of schizophrenic disorders: a replication. Br J Psychiatr. 1972;121:241–258. [DOI] [PubMed] [Google Scholar]
- 24. Butzlaff RL, Hooley JM. Expressed emotion and psychiatric relapse: a meta-analysis. Arch Gen Psychiatry. 1998;55:547–552. [DOI] [PubMed] [Google Scholar]
- 25. Carrà G, Cazzullo CL, Clerici M. The association between expressed emotion, illness severity and subjective burden of care in relatives of patients with schizophrenia. Findings from an Italian population. BMC Psychiatry. 2012;12:140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Marom S, Munitz H, Jones PB, Weizman A, Hermesh H. Expressed emotion: relevance to rehospitalization in schizophrenia over 7 years. Schizophr Bull. 2005;31:751–758. [DOI] [PubMed] [Google Scholar]
- 27. Lee G, Barrowclough C, Lobban F. Positive affect in the family environment protects against relapse in first-episode psychosis. Soc Psychiatry Psychiatr Epidemiol. 2014;49:367–376. [DOI] [PubMed] [Google Scholar]
- 28. Barrowclough C, Tarrier N, Humphreys L, Ward J, Gregg L, Andrews B. Self-esteem in schizophrenia: relationships between self-evaluation, family attitudes, and symptomatology. J Abnorm Psychol. 2003;112:92–99. [PubMed] [Google Scholar]
- 29. Klingberg S, Wittorf A, Herrlich J, et al. Cognitive behavioural treatment of negative symptoms in schizophrenia patients: study design of the TONES study, feasibility and safety of treatment. Eur Arch Psychiatry Clin Neurosci 2009;259:149–154. [DOI] [PubMed] [Google Scholar]
- 30. Klingberg S, Wolwer W, Engel C, et al. Negative symptoms of schizophrenia as primary target of cognitive behavioral therapy: results of the randomized clinical tones study. Schizophr Bull 2011;37:98–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Cole DA, Maxwell SE. Testing mediational models with longitudinal data: questions and tips in the use of structural equation modeling. J Abnorm Psychol. 2003;112:558–577. [DOI] [PubMed] [Google Scholar]
- 32.Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 1987;13:261–276. [DOI] [PubMed] [Google Scholar]
- 33. Kline RB. Principles and Practice of Structural Equation Modeling. 3rd ed. New York, NY: Guilford; 2011. [Google Scholar]
- 34. Deusinger IM. Die Frankfurter Selbstkonzeptskalen (FSKN). Göttingen: Hogrefe; 1986. [Google Scholar]
- 35. Wittorf A, Wiedemann G, Buchkremer G, Klingberg S. Quality and correlates of specific self-esteem at the beginning stabilisation phase of schizophrenia. Psychiatry Res. 2010;179:130–138. [DOI] [PubMed] [Google Scholar]
- 36. Lincoln TM, Mehl S, Ziegler M, Kesting ML, Exner C, Rief W. Is fear of others linked to an uncertain sense of self? The relevance of self-worth, interpersonal self-concepts, and dysfunctional beliefs to paranoia. Behav Ther. 2010;41:187–197. [DOI] [PubMed] [Google Scholar]
- 37. Lincoln TM, Mehl S, Kesting ML, Rief W. Negative symptoms and social cognition: identifying targets for psychological interventions. Schizophr Bull. 2011;37 Suppl 2:S23–S32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Feldmann R, Buchkremer G, Minneker-Hügel E, Hornung WP. Fragebogen zur Erfassung der Familienatmosphäre (FEF): Einschätzung des emotionalen Angehörigenverhaltens aus der Sicht schizophrener Patienten [Questionnaire for the assessment of the family atmosphere (FEF). The assessment of the emotional behaviour of relatives from the perspective of schizophrenc patients]. Diagnostica. 1995;41:334–348. [Google Scholar]
- 39. Bachmann S, Bottmer C, Jacob S, Schröder J. Perceived criticism in schizophrenia: a comparison of instruments for the assessment of the patient’s perspective and its relation to relatives’ expressed emotion. Psychiatry Res. 2006;142:167–175. [DOI] [PubMed] [Google Scholar]
- 40. von Polier GG, Meng H, Lambert M, et al. Patterns and correlates of expressed emotion, perceived criticism, and rearing style in first admitted early-onset schizophrenia spectrum disorders. J Nerv Ment Dis. 2014;202:783–787. [DOI] [PubMed] [Google Scholar]
- 41. Hesse K, Klingberg S. Examining the cognitive model of caregiving–a structural equation modelling approach. Psychiatry Res. 2014;217:171–176. [DOI] [PubMed] [Google Scholar]
- 42. Kuipers E, Onwumere J, Bebbington P. Cognitive model of caregiving in psychosis. Br J Psychiatry. 2010;196:259–265. [DOI] [PubMed] [Google Scholar]
- 43. Pitschel-Walz G, Leucht S, Bäuml J, Kissling W, Engel RR. The effect of family interventions on relapse and rehospitalization in schizophrenia–a meta-analysis. Schizophr Bull. 2001;27:73–92. [DOI] [PubMed] [Google Scholar]
- 44. Finnegan D, Onwumere J, Green C, Freeman D, Garety P, Kuipers E. Negative communication in psychosis: understanding pathways to poorer patient outcomes. J Nerv Ment Dis. 2014;202:829–832. [DOI] [PubMed] [Google Scholar]
- 45. Fowler D, Hodgekins J, Garety P, et al. Negative cognition, depressed mood, and paranoia: a longitudinal pathway analysis using structural equation modeling. Schizophr Bull. 2012;38:1063–1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Ellett L, Freeman D, Garety PA. The psychological effect of an urban environment on individuals with persecutory delusions: the Camberwell walk study. Schizophr Res. 2008;99:77–84. [DOI] [PubMed] [Google Scholar]
- 47. Kimhy D, Vakhrusheva J, Jobson-Ahmed L, Tarrier N, Malaspina D, Gross JJ. Emotion awareness and regulation in individuals with schizophrenia: Implications for social functioning. Psychiatry Res. 2012;200:193–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Lincoln TM, Hartmann M, Köther U, Moritz S. Do people with psychosis have specific difficulties regulating emotions? [published online ahead of print September 24, 2014] Clin Psychol Psychot. 2014. doi:10.1002/cpp.1923. [DOI] [PubMed] [Google Scholar]
- 49. Perry Y, Henry JD, Grisham JR. The habitual use of emotion regulation strategies in schizophrenia. Br J Clin Psychol. 2011;50:217–222. [DOI] [PubMed] [Google Scholar]
- 50. Rowland JE, Hamilton MK, Lino BJ, et al. Cognitive regulation of negative affect in schizophrenia and bipolar disorder. Psychiatry Res. 2013;208:21–28. [DOI] [PubMed] [Google Scholar]
- 51. Westermann S, Rief W, Lincoln TM. Emotion regulation in delusion-proneness: deficits in cognitive reappraisal, but not in expressive suppression. Psychol Psychother. 2014;87:1–14. [DOI] [PubMed] [Google Scholar]
- 52. de Sousa P, Varese F, Sellwood W, Bentall RP. Parental communication and psychosis: a meta-analysis. Schizophr Bull. 2014;40:756–768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Renshaw KD. The predictive, convergent, and discriminant validity of perceived criticism: a review. Clin Psychol Rev. 2008;28:521–534. [DOI] [PubMed] [Google Scholar]
- 54. Freeman D, Pugh K, Dunn G, et al. An early Phase II randomised controlled trial testing the effect on persecutory delusions of using CBT to reduce negative cognitions about the self: the potential benefits of enhancing self confidence. Schizophr Res. 2014;160:186–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Garety PA, Fowler DG, Freeman D, Bebbington P, Dunn G, Kuipers E. Cognitive–behavioural therapy and family intervention for relapse prevention and symptom reduction in psychosis: randomised controlled trial. Br J Psychiatry. 2008;192:412–423. [DOI] [PubMed] [Google Scholar]
- 56. Insel TR. Translating scientific opportunity into public health impact: a strategic plan for research on mental illness. Arch Gen Psychiatry. 2009;66:128–133. [DOI] [PubMed] [Google Scholar]
- 57. Kuipers E, Yesufu-Udechuku A, Taylor C, Kendall T. Management of psychosis and schizophrenia in adults: summary of updated NICE guidance. BMJ. 2014;348:g1173. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.