Abstract
Objective
Law enforcement is a stressful occupation associated with significant health problems. To date, most studies have focused on one specific factor or one domain of risk factors (e.g., organizational, personal). However, it is more likely that specific combinations of risk factors are differentially health relevant and further, depend on the area of police work.
Methods
A self-selected group of officers from the criminal, community, and emergency division (N = 84) of a Swiss state police department answered questionnaires assessing personal and organizational risk factors as well as mental and physical health indicators.
Results
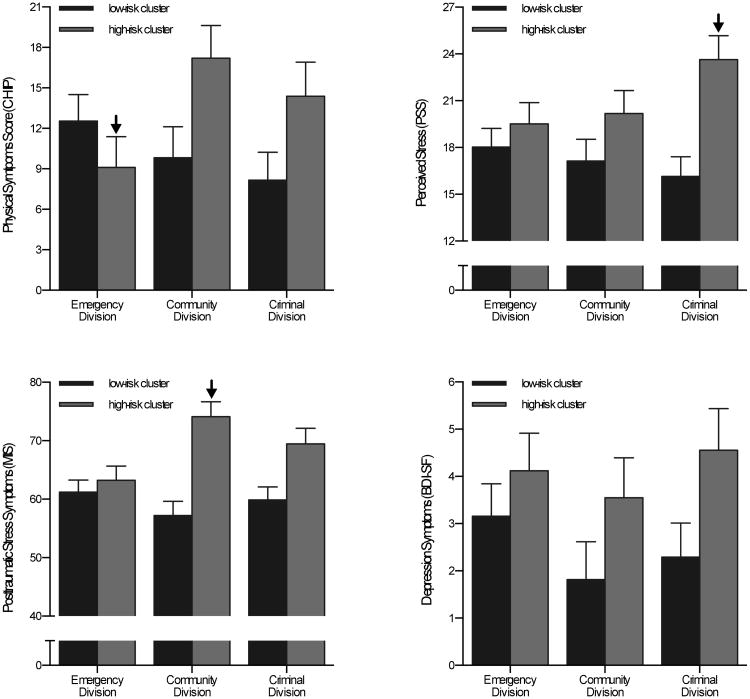
In general, few differences were observed across divisions in terms of risk factors or health indicators. Cluster analysis of all risk factors established a high-risk and a low-risk cluster with significant links to all mental health outcomes. Risk cluster-by-division interactions revealed that, in the high-risk cluster, Emergency officers reported fewer physical symptoms, while community officers reported more posttraumatic stress symptoms. Criminal officers in the high-risk cluster tended to perceived more stress. Finally, perceived stress did not mediate the relationship between risk clusters and posttraumatic stress symptoms.
Conclusion
In summary, our results support the notion that police officers are a heterogeneous population in terms of processes linking risk factors and health indicators. This heterogeneity thereby appeared to be more dependent on personal factors and individuals' perception of their own work conditions than division-specific work environments. Our findings further suggest that stress-reduction interventions that do not target job-relevant sources of stress may only show limited effectiveness in reducing health risks associated with police work.
Keywords: police division, health outcomes, risk factors, cluster analysis
Law enforcement is one of the most stressful occupations and has been associated with significantly elevated stress-related health risks (e.g., Dantzer, 1987). While some research has focused on operational risk factors, such as exposure to violence and volatile situations (e.g., Arial, Gonik, Wild, & Danuser, 2010), organizational factors such as decision latitude, psychological demands, and institutional support (Arial et al., 2010; Hall, Dollard, Tuckey, Winefield, & Thompson, 2010; Martinussen, Richardsen, & Burke, 2007; Morash, Haarr, & Kwak, 2006), as well as personal factors such as coping style (Aaron, 2000; Harvey-Lintz & Tidwell, 1997; Pienaar, Rothmann, & van de Vijver, 2007) contribute significantly to higher levels of perceived stress among police officers and are related to negative health outcomes. To date, most studies have focused on one specific factor or one domain of risk factors (e.g. organizational, operational or personal) when examining links to police health outcomes. Perceived organizational and personal factors vary greatly across police officers (e.g., Galatzer-Levy et al., 2013; Maia et al., 2007; Marmar et al., 2006). For instance, recent work showed that personal factors such as emotionality could lead to different health trajectories among officers (Galatzer-Levy et al., 2013). However, organizational risk factors related to objective work structure are also inherently different among various divisions of law enforcement. This raises the question whether approaches that treat police officers as a homogenous group in terms of working conditions related to area of police work are adequate to capture what puts them at such high risk for health problems.
Instead, it is likely that combinations of organizational and personal risk factors are differentially health relevant and furthermore, that these combinations of risk factors differ depending on the area of police work (i.e., police divisions). To identify the combinations of risk factors that are most health-relevant for police officers, an important first step is to explore which patterns of factors naturally occur. Increasing our understanding of the complex interplay between work environment and personal factors and health outcomes is crucial for the development of targeted prevention and health intervention programs.
Stress and health in police officers
Numerous studies have reported that compared with other professions, police officers are at increased risk for stress-related physical illnesses including heart disease, chronic pain, and insomnia (Alkus & Padesky, 1983; Lobel & Dunkel-Schetter, 1990), as well as for stress-related psychological problems such as depression, domestic violence, over-eating, drug and alcohol abuse (Arter, 2008; Harpold & Feenster, 2002; Lott, 1995; Sheehan & Van Hasselt, 2003; Swatt, Gibson, & Piquero, 2007). Organizational risk factors, such as lack of institutional support (from colleagues and superiors) and high job-related psychological demands were found to have a significant impact on the health of police officers (Arial et al., 2010; Hall et al., 2010; Morash et al., 2006). Lastly, personal factors, including coping strategies employed when confronted with a stressful environment were linked to physical and psychological outcomes (e.g., Aaron, 2000; Gershon, Barocas, Canton, Li, & Vlahov, 2009). The majority of previous studies investigated operational, organizational and/or personal risk factors with the aim of determining which one had the strongest impact on a specific (e.g., posttraumatic stress) or generic (e.g., general health index) health outcomes. However, police officers are exposed to a wide range of risk factors simultaneously. Thus, specific combinations of factors rather than individual factors may create particularly unfavorable conditions, which then contribute to the development of psychological and physical illnesses.
Risk factor differences between police divisions
Studies investigating health-related risk factors in law enforcement usually assess ‘police officers’, implying a group homogenous in terms of exposure to work environments (e.g., Morash et al., 2006; Violanti et al., 2006). However, police departments are composed of various divisions or squads responsible for different aspects of law enforcement. Consequently, officers are exposed to different tasks and work conditions. The range of tasks and responsibilities and work environments among police officers leads to differences in levels of psychological demand, perceptions of social support from colleagues and superiors, and feelings of loneliness. For example, in some divisions police officers work alone and have relative autonomy in carrying out tasks, whereas others work in teams and rely on a superior officer for orders and guidance. Lastly, within the hierarchical structure of the police, some divisions may have higher social status than others due to the nature of their work, level of autonomy, or socioeconomic factors such as level of education or pay rate. Thus, in order to understand how combinations of environmental and personal factors contribute to negative physical and mental health outcomes in the police force, it is important to investigate the possibility that for each police division, different combinations of risk factors may be health relevant.
Study aims
In summary, many studies compared police work to other professions and identified organizational, operational, and individual factors that are linked to health issues. However, the majority of these studies do not address the complex interplay among health risk factors as well as lack specificity in terms of police work environment. Hence, the first aim of the current study was to examine organizational and personal factors that differ between police divisions (i.e., emergency division, criminal division, and community division). Next, instead of investigating each of the risk factors individually, we aimed to identify naturally occurring patterns of factors and to evaluate whether these patterns occur more frequently in various police divisions. The third aim was to explore general and division-specific links between patterns of risk factors and health outcomes (i.e., perceived stress, mental health, and physical health). Lastly, we considered perceived stress as a potential mediator of these links between risk factor patterns and health.
Method
Participants
A total of 101 participants were recruited from the three main divisions of a state police department in Switzerland (emergency, community, and criminal; see below for descriptions). All participants were French-speaking Swiss nationals. Officers who were pregnant or had less than one year of police duty were excluded from participation. Among those eligible, 15 were excluded due to failure to return questionnaires and two due to missing data. The final sample of 84 police officers was predominantly male (n=68 male), with an even distribution across the three divisions (emergency: n=31, community: n=28, criminal: n=25; see Table 1). The study was approved by the Ethics Commission for Studies in Humans in Lausanne, Switzerland, the Institutional Review Board at Brandeis University, police administration, as well as both police labor unions. All data were identified only with participant numbers and did not include names or other identifiable information. The consent forms containing the participants' signature were stored by the study physician who had no access to the data. None of the data collected were shared with the police administration or anyone else besides study personnel. Participants were not compensated.
Table 1.
Socio-demographic differences between police divisions.
| Emergency (n=31) |
Community (n=28) |
Criminal (n=25) |
Test | |
|---|---|---|---|---|
| mean (SD) | mean (SD) | mean (SD) | F | |
|
|
||||
| Age | 31.71 (6.81) | 42.86 (9.02) | 40.16 (8.21) | 3.03 |
| Years in duty | 12.39 (6.93) | 18.00 (9.81) | 15.72 (8.80) | 3.24+ |
| BMI | 27.11 (2.45) | 27.41 (4.13) | 25.50 (3.63) | 2.33 |
|
|
||||
| n (%) | n (%) | n (%) | χ2 | |
|
|
||||
| Gender: | 4.69 | |||
| - Male | 28 (90.3) (90.3) | 19 (67.9) | 21 (84.0) | |
| - Female | 3 (9.7) | 9 (32.1) | 4 (16.0) | |
| Marital Status: | 2.94 | |||
| - Single | 7 (22.6) | 9 (32.1) | 7 (28.0) | |
| - Married | 19 (61.3) | 13 (46.6) | 16 (64.0) | |
| - Divorced | 5 (16.1) | 6 (21.4) | 2 (8.0) | |
| Children (yes) | 20 (64.5) | 20 (71.4) | 16 (64.0) | 0.47 |
Note:
p<.10
Police divisions
Emergency division
Police officers in the Emergency division (or Rescue section) are the first responders to emergency calls (e.g., car accident, burglary, fights). Besides field interventions, tasks include administrative reports and legal procedures. Officers wear a police uniform and work in rotating teams. To be eligible for joining the police academy they need to have completed at least 3 years of post-graduation training.
Community division
This division is dedicated to addressing minor delinquency and public security. Police officers work closely with members of the community and focus on prevention and cooperation with the public. The majority of work time is dedicated to administrative tasks, such as registering complaints and writing reports, and to a lesser extent to investigating minor cases as assigned by the public prosecutor's office. Community division officers wear a police uniform, work in teams and have similar education requirements to those of emergency division officers.
Criminal division
The criminal division is composed of detectives and forensic scientists who carry out serious crime investigation. Officers work in different squads, and in close collaboration with the public prosecutor's office; however, compared to officers in the community division, they have relative autonomy in carrying out investigations. Similar to the other divisions, administrative procedures are a large part of their duty. However, they do not wear uniforms and usually do not work in teams. Officers in the criminal division typically have a university degree and thus a higher education background than officers in the other divisions.
Procedure
Police officers were recruited through the office of psychological services of the State Police via emails and flyers displayed throughout the police department. Interested officers scheduled their study participation on the department's intranet (blind registration). Data collection took place in the police department, during duty time, in the administrative floor where officers usually do not go, in a private, confidential area. During the first one-on-one appointment, the objectives and procedures of the study were explained, any questions or concerns addressed, and written consent collected. Participants then underwent a 20-minute interview collecting socio-demographic information as well as information concerning medication use, health, smoking, substances use, and physical symptoms. Subsequently, participants were asked to complete a set of questionnaires assessing job content, perceived stress, symptoms of posttraumatic stress and depression, past year stress and trauma exposure, subjective social status, and ways of coping with stress.
Measures
Risk factors
The MacArthur Scales of Subjective Social Status (SSS; Adler, Epel, Castellazzo, & Ickovics, 2000) consist of two ladder measures assessing participants' perceived position in the social hierarchy relative to the country as a whole and their community, defined as whatever is most meaningful to the individual. Specifically, participants place an ‘X’ on the ladder rung from 1 to 10 where they feel they stand, with higher rungs representing higher status. The current study added two additional ladders asking participants to rate their perceived social status compared to the police as a whole and compared to their friends. The four scales are analyzed separately. In previous research, SSS has been shown to predict health outcomes independent of socioeconomic status (Adler et al., 2000; Singh-Manoux, Adler, & Marmot, 2003) and to have adequate test-retest reliability at six month follow-up (ρ = .62, p < .01; Operario, Adler, & Williams, 2004).
The Social Readjustment Rating Scale (French version: Harmon, Masuda, & Holmes, 1970; Holmes & Rahe, 1967) is a 43-item questionnaire identifying major stressful life events over the past year. Items include events such as “marital separation” or “foreclosure of a mortgage” and are answered “yes” if such event happened in the past 12 months. Each of the 43 events is awarded a Life Change Unit (ranging from 11 to 100), a previously determined score reflecting how traumatic an event was rated by a large sample population. A total score is computed by adding up the units for each of the events a participant identified. Less than 150 life change units are associated with a 37% risk, scores between 151 and 299 with a 50% risk, and scores over 300 with a 80% risk of developing a stress-related illness within the next 2 years. The stability of the SRRS over a 2-year period in groups of healthy males ranges from r = .89 to r = .96 (Gerst, Grant, Yager, & Sweetwood, 1978). Consistency in the absolute weight assigned to various events over time ranges from r = .59 to r = .83 for all events (Gerst et al., 1978).
The French version of the Job Content Questionnaire (Niedhammer, Chastang, Gendrey, David, & Degioanni, 2006) is a 29-item self-report questionnaire assessing stress in the workplace through three main dimensions: psychological demands (9 items, α = .84), decision latitude (9 items, α = .67) and social support (8 items, α = .69). Each item is rated on a 1 to 4-point Likert scale (1= do not agree at all; 4 = totally agree), with higher mean scores representing higher social support, higher decision latitude, and higher psychological demands. The social support scale can be divided into support from superiors (4 items, α = .73) and support from colleagues (4 items, α = .74).
The French Ways of Coping Checklist (Cousson-Guélie et al., 2010; Folkman & Lazarus, 1980) is a 21-item measure assessing strategies used to cope with stress and trauma. Each item is rated on a scale from 1 (not used) to 4 (used a great deal). Three subscales can be computed: problem-focused coping (8 items; α = .78), emotion-focused coping (7 items; α = .74) and seeking social support (6 items; α = .79). Subscale scores range from 1 to 4 with higher scores indicating higher use of the coping strategy. Problem-focused coping strategies are active problem-solving strategies involving information gathering in an attempt to control or better understand the situation. Emotion-focused coping strategies are passive or avoidant, aim to decrease the intensity of emotions, and involve cognitive efforts to change the meaning of the situation, avoiding unpleasant thoughts or places related to the situation, or re-interpreting the information in a more positive light. Seeking social support strategies involve social contact as a means to take control over the stressful situation.
The UCLA Loneliness Scale (French version: de Grâce, Joshi, & Pelletier, 1993; Russel, Peplau, & Cutrona, 1980) is a 20-item scale designed to measure one's subjective feelings of loneliness and social isolation. Participants rate items such as “I have nobody to talk to” or “I am no longer close to anyone” on a scale from 0 (Never) to 3 (Often). A sum score of loneliness is computed with higher scores indicating more feelings of loneliness. The French validation shows Cronbach's α ranging from .84 to .93, depending on the population assessed (de Grâce et al., 1993).
Health indicators
The French Perceived Stress Scale at work (PSS; Rolland, 1991) is a 14-item questionnaire adapted from the Perceived Stress Scale (Cohen, Kamarck, & Mermelstein, 1983) measuring an individual's perceived stress at work during the past month. Items such as “Do you think about the amount of work that still needs to be done?” are rated on a scale ranging from 0 (never) to 4 (most of the time). A sum score is computed with higher scores indicating higher stress. The adapted version has sufficient reliability (α = .78).
The Cohen-Hoberman Inventory of Physical Symptoms (CHIPS; Cohen & Hoberman, 1983) is a list of 33 common physical symptoms (e.g., back pain, headache). Each item is rated on how much each symptom bothered the individual during the past two weeks on a 0 (“not at all”) to 4 (“extremely”) scale. A total score is computed by summing items, with scores ranging from 0 to 132. The inventory is reliable (α = .88) and positively correlated with use of health facilities in the following seven weeks (Cohen & Hoberman, 1983).
The Mississippi Scale – Police version (MIS; Lilly, Pole, Best, Metzler, & Marmar, 2009) is a validated adaptation (α = .84) of the Mississippi Scale for Combat-Related Posttraumatic Stress Disorder (Keane, Caddell, & Taylor, 1988). Respondents rated 35-items describing PTSD-related symptoms such as “If someone pushes me too far, I am likely to become violent”, on a Likert-type scale from 1 (not at all true) to 5 (extremely true). Items are summed to compute a cumulative PTSD symptom severity score.
The Beck Depression Inventory – Short Form (BDI-SF; Beck, Steer, & Brown, 1996) is a 13-item version of the Beck Depression Inventory questionnaire measuring severity of depression symptoms according to DSM-IV criteria for depression. Participants rate symptoms on a 0 (absent) to 3 (very often) scale of intensity. Sum scores range from 0 to 39, with higher scores indicating more severe depressive symptoms. Scores of ten and higher indicate high depression (Sensitivity=100% and Specificity = 83.1; Furlanetto, Mendlowicz, & Bueno, 2005). The present study used the validated French version (Bourque & Beaudette, 1982), for which test–retest procedure indicated adequate stability over a 4-months period and internal consistency was high (α = .90).
Demographic and ancillary measures
Gender, marital status, children (yes/no), Body mass index (BMI – computed using the standard formula: weight in kg divided by height in meters squared), age and years of police service were investigated. Participants' tendency to give socially desirable responses was assessed via the Marlowe-Crowne Social Desirability - Short Version instrument (Blais, Lachance, & Riddle, 1991; Crowne & Marlowe, 1960). Specifically, participants agreed or disagreed with 13 statements such as “I am always courteous, even to people who are disagreeable” or “I am sometimes jealous of what good happens to other people.” The validated French version was used (test-retest stability over one year: r = .70) which, similar to the original version, consists of two main components, denial and pretention. Since socially desirable tendencies may result in lower self-reports of stress and health conditions (e.g. Brunet, Boucher, & Boyer, 1996), its assessment is highly recommended when studying populations with high male-norm pressure like police officers (Liberman, Best, Metzler, & Fagan, 2002; Pole et al., 2001).
Analytical Plan
A two-step approach was chosen for the current analyses. First, preliminary analyses included assessment of demographic differences between police divisions by ANCOVA and Chi2-test. To replicate earlier findings, partial correlations (controlling for social desirability) tested for associations between risk factors and health indicators. This was followed by the statistical examination of the study's aims. Aim 1: To identify differences in risk factors between the three police divisions, a MANCOVA was computed including subjective social status, job content, coping, loneliness, past year stressful events (covariates: social desirability, gender and years of duty). A second MANCOVA assessed differences between police divisions in health indicators (perceived stress, depression symptoms, posttraumatic stress symptoms, and physical symptoms; same covariates). Aim 2: To identify naturally occurring combinations of risk factors, all risk factors were entered into a hierarchical cluster analysis using Ward method (algorithm guaranteeing interclasses maximal inertia) and Euclidian distances (hierarchical proximity structure). A Chi2 test was computed to assess frequency distributions of risk clusters in each police divisions. To address Aim 3, police division-dependent differences in health indicators between risk factor clusters were assessed by MANCOVA (covariates: social desirability, gender, and years of duty). Lastly, to test for stress mediation (Aim 4), those findings were compared to effects from analyses including stress as a covariate.
Results
Socio-demographic comparisons across the police divisions
Differences in socio-demographic variables between the three police divisions are summarized in Table 1. While participants in the three divisions did not differ in terms of age, gender distribution, BMI, marital status, or children, officers in the community division served more years in the police force compared to officers in the criminal division and the emergency division (p = .055).
Associations between risk factors and health indicators
Partial correlations (controlling for social desirability) were computed to test for associations between risk factors and health indicators. A higher risk for negative mental health outcomes across all three indices assessed, i.e., elevated perceived chronic stress, PTSD symptoms, and depressive symptoms, was observed in those police officers who also reported lower social standing in their community, lower social standing among their friends, less social support from superiors, more loneliness, as well as less problem-focus coping. Risk factors for physical symptoms were low social support from superiors as well as low social standing in the country and a strong preference for emotion-focused coping. See Table 2 for statistical details and more differential links between risk factors and health indicators.
Table 2.
Associations between risk factors and health indicators across the three police divisions.
| Perceived stress | PTSD symptoms | Depressive symptoms | Physical symptoms | |
|---|---|---|---|---|
|
|
||||
| SSS Country | -.207 | -.296** | -.220 | -.243* |
| SSS Community | -.233* | -.248* | -.282* | -.210 |
| SSS Police | .096 | -.101 | -.062 | -.118 |
| SSS Friends | -.269* | -.367** | -.275* | -.176 |
| Past year stress and trauma | .063 | .148 | .085 | .194 |
| Decision latitude | -.290** | -.404** | -.133 | -.212 |
| Psychological demand | .329** | .044 | .031 | .073 |
| Social support from colleagues | -.385** | -.315** | -.206 | -.221 |
| Social support from superiors | -.419** | -.450** | -.331** | -.247* |
| Problem-focused coping | -.243* | -.345** | -.242* | -.100 |
| Emotion-focused coping | .105 | .256* | .260* | .225* |
| Seeking social support | -.128 | -.163 | -.167 | .002 |
| Loneliness | .315** | .565** | .427*** | .139 |
Note: SSS=MacArthur Scale of Subjective Social Status. Partial correlations between health indicators: .22≤r≤.51 (.001<p≤.045).
p<.05.
p<.01.
Differences in risk factors and health indicators between police divisions
Assessing covariates' simple main effects on risk factors beyond any risk factor associations with police division, MANCOVA (covariates: years of duty, gender and social desirability) revealed a positive association between years of duty and subjective social status in the police (F(1,82) = 21.46; p < .001; ηp2 = .22). Furthermore, females were more likely to use emotion-focused coping than men (F(1,82) = 4.66; p = .034; ηp2 = .06). As expected, social desirability significantly influenced participants' responses to several of the questionnaires assessing risk factors. Specifically, participants scoring higher on social desirability reported higher subjective social status in the police (F(1,82) = 4.24; p = .043; ηp2 = .05), more decision latitude (F(1,82) = 8.89; p = .004; ηp2 = .10), more social support from colleagues (F(1, 82) = 8.85; p = .004; ηp2 = .10), more social support from superiors (F(1,82) = 7.49; p = .008; ηp2 = .09), less emotion-focused coping (F(1, 82) = 22.29; p < .001; ηp2 = .23) and less loneliness (F(1,82) = 8.65; p = .004; ηp2 = .10) compared to participants scoring lower on social desirability.
Assessing conditional main effects of divisions on risk factors, officers in the three divisions differed in terms of subjective social status in the police (p < .001), and past year's stressful life events (p = .019; see Table 3). In more detail, officers in the community division reported the lowest perceived social status in the police force, while officers in the Emergency division reported the highest level of past year exposure to stressful life events.
Table 3.
Differences between the three police divisions in risk factors and health indicators.
| Estimated Means (S.E.) | F | p | η2 | |||
|---|---|---|---|---|---|---|
| Emergency | Community | Criminal | ||||
| Risk factors: | ||||||
|
| ||||||
| SSS Police | 4.56 (0.27) | 3.99 (0.31) | 5.72 (0.29) | 8.84 | .00 | .19 |
| SSS Friends | 6.60 (0.27) | 6.60 (0.31) | 7.03 (0.29) | 0.74 | .48 | .02 |
| SSS Community | 6.03 (0.23) | 6.06 (0.26) | 6.22 (0.24) | 0.20 | .82 | .01 |
| SSS Country | 5.95 (0.22) | 5.94 (0.25) | 6.21 (0.24) | 0.47 | .63 | .01 |
| Past Year Stressful Events | 198.25 (21) | 165.41 (23) | 112.69 (22) | 4.19 | .02 | .10 |
| Decision Latitude | 3.33 (0.07) | 3.14 (0.08) | 3.22 (0.07) | 1.65 | .20 | .04 |
| Psychological Demand | 2.84 (0.07) | 2.74 (0.08) | 2.87 (0.08) | 0.76 | .47 | .02 |
| Social Support: Colleagues | 3.28 (0.08) | 3.22 (0.09) | 3.25 (0.08) | 0.11 | .90 | .00 |
| Social Support: Superiors | 3.10 (0.09) | 3.18 (0.10) | 3.16 (0.10) | 0.15 | .86 | .00 |
| Problem-Focused Coping | 3.06 (0.08) | 3.00 (0.09) | 3.01 (0.09) | 0.15 | .86 | .00 |
| Emotion-Focused Coping | 1.83 (0.08) | 1.94 (0.09) | 1.75 (0.09) | 1.12 | .33 | .03 |
| Seeking Social Support | 2.61 (0.11) | 2.73 (0.12) | 2.41 (0.12) | 1.72 | .19 | .04 |
| Loneliness | 32.90 (1.6) | 36.75 (1.7) | 33.42 (1.7) | 0.08 | .92 | .00 |
|
| ||||||
| Health indicators: | ||||||
|
| ||||||
| Perceived Stress | 18.75 (0.99) | 18.46 (1.07) | 19.20 (1.06) | 0.12 | .89 | .00 |
| Depression Symptoms | 3.57 (0.54) | 2.74 (0.58) | 3.18 (0.57) | 0.49 | .61 | .01 |
| PTSD Symptoms | 62.43 (1.87) | 65.27 (2.01) | 63.80 (1.98) | 0.48 | .62 | .01 |
| Physical Symptoms | 11.29 (1.60) | 13.50 (1.72) | 10.67 (1.69) | 0.71 | .49 | .02 |
Note. S.E.=Standard error. SSS=MacArthur Scales of Subjective Social Status.
Repeating the above analysis for health indicators revealed a simple main effect of gender on depression symptoms (F(1,82) = 12.93; p < .001; ηp2 = .14). Furthermore, as expected, participants scoring higher on social desirability reported less perceived stress (F(1,82) = 19.52; p < .001; ηp2 = .20), depression symptoms (F(1,82) = 27.29; p < .001; ηp2 = .26), posttraumatic stress symptoms (F(1,82) = 37.15; p < .001; ηp2 = .32), and physical symptoms (F(1,82) = 6.65; p = .012; ηp2 = .08) than officers scoring high on social desirability.
Assessing conditional MANCOVA main effects, police divisions do not differ significantly in terms of mental health indicators and of physical symptom severity (see Table 3).
Hierarchical cluster analysis of risk factors
All risk factors were standardized and entered into a hierarchical cluster analysis. Dendrogram analysis suggested a 2-cluster solution with individuals in cluster 1 (n = 46; low-risk cluster) having higher subjective social status in general, higher decision latitude, higher social support from both colleagues and superiors, used more problem-focused coping and reported less loneliness than individuals in cluster 2 (n = 36; high-risk cluster; see Table 4).
Table 4.
Risk factor composition of 2-cluster solution (unstandardized means (SD);
| Cluster 1 “Low-risk” (n=46) |
Cluster 2 “High-risk” (n=36) |
|
|---|---|---|
|
|
||
| SSS in the Police* | 5.02 (1.95) | 4.36 (1.55) |
| SSS Friends | 7.28 (1.39) | 6.03 (1.08) |
| SSS Community | 6.57 (1.15) | 5.50 (1.03) |
| SSS Country | 6.61 (1.00) | 5.28 (0.88) |
| Past year's Stressful Events* | 146.54 (112.1) | 181.19 (108.7) |
| Decision Latitude | 3.35 (0.29) | 3.09 (0.44) |
| Psychological Demand* | 2.79 (0.40) | 2.85 (0.35) |
| Support from Colleagues | 3.42 (0.42) | 3.05 (0.37) |
| Support from Superiors | 3.36 (0.37) | 2.87 (0.51) |
| Problem-Focused Coping | 3.20 (0.32) | 2.81 (0.50) |
| Emotion-Focused Coping* | 1.79 (0.56) | 1.91 (0.50) |
| Seeking Social Support | 2.89 (0.51) | 2.20 (0.47) |
| Loneliness | 30.65(5.82) | 38.92 (9.46) |
Note. SD=Standard deviation. SSS= MacArthur Scales of Subjective Social Status.
Non-significant difference.
Mann-Whitney U-tests showed that most variables entered into the cluster analysis differed significantly between clusters (p-values range from < .001 to .004), except subjective social status in the police, past year's stressful life events, psychological demand and emotion-focused coping. Assessing occurrence of risk clusters in the three police divisions revealed no significant differences, i.e., low-risk cluster membership was slightly more prevalent in each of the three divisions (χ2 = 0.60 p = .73).
Associations between risk clusters, police divisions and health indicators
A MANCOVA assessing effects of risk clusters, police divisions and risk clusters-by-police divisions interaction on health indicators (years of duty, gender and social desirability as covariates) showed simple main effects for gender (depressive symptoms: F(1, 82) = 14.42, p < .001, ηp2 = .17) and for social desirability (perceived stress: F(1, 82) = 13.06, p = .001, ηp2 = .15; depression symptoms: F(1, 82) = 20.67, p < .001, ηp2 = .22; posttraumatic stress symptoms: F(1, 82) = 27.98, p < .001, ηp2 = .28; and physical symptoms: F(1, 82) = 3.23, p = .08, ηp2 = .04).
In terms of conditional cluster main effects, significant differences between clusters emerged for all mental health indicators (perceived stress: F(1, 82) = 12.96, p = .001, ηp2 = .15; posttraumatic stress symptoms: F(1, 82) = 23.94, p < .001, ηp2 = .25; depression symptoms: F(1, 82) = 6.64, p = .012, ηp2 = .08), but only reached a trend level for physical symptoms (F(1, 82) = 3.42, p = .069, ηp2 = .05). Specifically, participants in the high-risk cluster (cluster 2) scored higher on perceived stress, posttraumatic stress symptoms and depression symptoms, compared with participants in cluster 1. In line with the earlier analyses, no main effects of police division were observed (all p > .50).
Testing for division-dependent associations between cluster membership and health outcomes revealed that police officers in cluster 2 appeared to be protected by being in the emergency division in terms of physical symptoms (F(2, 82) = 3.57, p = .033, ηp2 = .09). However, officers in the high-risk cluster (cluster 2) showed a trend for an elevated risk for perceived stress (F(2, 82) = 2.67, p = .08, ηp2 = .07) when they were in the Criminal division and were at elevated risk for posttraumatic stress symptoms (F(2, 82) = 4.87, p = .010, ηp2 = .12) when they were in the Community division. No division-dependent associations between cluster membership and depressive symptoms were observed (F(2, 82) = 0.36, p = .70, ηp2 = .01), i.e., the high-risk cluster was linked to elevated depressive symptoms in all three divisions (see Figure 1 for more details).
Figure 1. Division-dependent associations between risk clusters and health indicators.
Note: Arrows point to cluster subgroups within divisions that are further discussed in the text.
Finally, to assess the potential mediating role of stress, the above analyses were repeated with perceived stress included as a covariate. Reduced effects sizes suggested that stress partially mediated conditional cluster main effects on all assessed health indicators. More specifically, conditional cluster main effects on posttraumatic stress symptoms were reduced from ηp2 = .25 to ηp2 = .15 when including perceived stress (F(1, 82) = 12.17, p = .001). Similarly, cluster-dependent differences in depression symptoms were slightly reduced from ηp2 = .08 to ηp2 = .05 (F(1, 82) = 4.12, p = .046). Lastly, the trend for higher physical symptoms in officers assigned to cluster 2 became non-significant when considering perceived stress (F(1, 82) = 1.18, p = .28), with effect sizes changing from ηp2 = .05 to ηp2 = .02.
Contrarily, division-dependent cluster differences in posttraumatic stress symptoms were not mediated by perceived stress (F(2, 82) = 5.15, p = .008, ηp2 = .13; without perceived stress ηp2 = .12) and although the cluster-by-division interaction effect for physical symptoms changed from a significant effect to a trend, no decreases in effect size was observed (F(2, 82) = 2.91, p = .061, ηp2 = .08; without perceived stress ηp2 = .01; depressive symptoms: F(2, 82) = 0.19, p = .83, ηp2 = .01; without perceived stress ηp2 = .01).
Discussion
In summary, the current findings support the idea that individual perceptions of work conditions and personal factors are as relevant as objective work structure when studying health outcomes in police officers. In general, despite the different working environments and types of duty, few differences were reported by police officers across divisions in terms of risk factors or health indicators. When exploring whether natural patterns of risk factors emerged, cluster analysis revealed a low-risk and a high-risk cluster that were strongly related to mental health indicators, but were not distributed differently across the police divisions. However, cluster-by-division interactions revealed that officers in the Emergency division appeared to be protected from the negative physical health effects of being in the high-risk cluster. In contrast, being in the high-risk cluster as a Community officer or Criminal officer was related to an increased risk for posttraumatic stress symptoms or perceived stress, respectively. Finally, perceived stress mediated the relationships between risk clusters and perception of physical symptoms as well as depression symptoms, while it did not play a role for cluster-dependent differences in PTSD symptoms.
Differences in risk factors and health indicators between police divisions
Overall, no differences across divisions were found for mental and physical health indicators, however, police divisions differed on two risk factors. Specifically, Emergency officers scored the highest and Criminal officers the lowest with regard to past year's stressful events. It is interesting to note that as first responders, Emergency officers are the most exposed to direct violence (e.g., car accident, shooting, etc.), yet they did not report more occupational stress or more posttraumatic stress symptoms than other officers. It can be speculated that because of the high male-normative police environment, police officers may not express or acknowledge their stress at work, however, the stress accumulated at work may be expressed in the home environment. In line with this idea, some studies have reported a high rate of domestic violence among police officers (Waters & Ussery, 2007), suggesting that work related-stress may be translated to some aspect of their private life where normative pressure is lower.
Furthermore, subjective social status in the police was highest among Criminal officers and lowest in Community officers. While subjective social status relative to the country and community are widely used status measures in addition to or instead of socioeconomic status indicators, the current study is among the first to use police as a reference group (Akinola & Mendes, 2014). Interestingly, status relative to country and community and even status relative to friends did not distinguish between the divisions, however, subjective social status in the police explained 19% of the between-division variance. With regard to division-specific differences, it is not surprising to find higher status in officers from the Criminal divisions compared to others, as a higher education level is required for being selected for this division and the pay is higher as well. Moreover, depictions of criminal and forensics investigators as being highly intelligent and solving complex cases may contribute to the higher status perception among Criminal division officers.
The fact that more of the assessed risk factors did not differ across divisions is noteworthy. Indeed, we expected that objective duty-related work conditions (e.g., exposure to violence) that have been linked to stress would have influenced perception of organizational risk factors and would therefore be different across divisions. However, it appears that individual perceptions of work environment may be less related to the actual work conditions but perhaps more to personal factors such as individual history or personality traits (e.g., Haisch & Meyers, 2004; Lau, Hem, Berg, Ekeberg, & Torgersen, 2006).
Risk factor patterns
Instead of investigating each of the differentiating risk factors individually, the current study aimed to identify naturally occurring patterns of risk factors and to evaluate whether these patterns occur more frequently in various police divisions. A two-cluster solution emerged with a “high-risk” cluster characterized by lower subjective social status in the community, in the country, and among friends, lower decision latitude, lower support from colleagues and superiors, lower problem-focused coping and higher loneliness compared to the “low-risk” cluster. To our knowledge, this is the first study to use cluster analysis to investigate the complex co-occurrence of personal and organizational risk factors in the police. Most prior research has used linear regression models to identify individual risk factors that are the most relevant for stress-related illnesses (e.g., Arial et al., 2010). However, this kind of analysis does not allow for assessment of the impact of combination of factors. A police officer's work environment is complex and officers are likely to be exposed to a variety of different risk factors simultaneously. The current study was able to show that a variety of important risk factors may work together to put police officers at risk for mental health problems.
In terms of factors contributing to cluster differences, the current study is among the first to confirm the role of low subjective social status relative to the country and community as mental health risk factors for police officers and is the first to identify this association for subjective status among friends. Interestingly, factors that previously differentiated police divisions, namely subjective social status in the police and past year's stressful events were not significantly different between clusters. This may suggest that higher perceived status in the police does not protect against being exposed to the same risk factors as officers perceiving their status as lower. Perhaps aside from decision latitude, those other risk factors are more personal and may affect police officers from all places in the hierarchy in the same way. However, status ratings relative to the police as a whole were also lower compared to status ratings relative to friends, community, and country. This in line with the above interpretation, that status in the police may capture to a large extent a more consistent underlying negative work environment factor. Concerning the lack of cluster-specific differences in past year's stressful events, assessing the mean scores suggests that officers did differ, i.e., officers in the high-risk cluster had a 50% risk of developing a stress-related illness within the next two years compared to a 37% risk for officers in the low-risk cluster. However, we observed a large variability in this measure between officers. This variability may have prevented us from finding cluster differences and thus this finding should be interpreted cautiously until confirmed in future studies.
Two additional risk factors that did not differentiate between risk clusters were psychological demand and emotion-focused coping. The latter may be explained by the fact that in line with earlier findings on particularly male participants, police officers appeared to use problem-focused and social support-seeking coping strategies more frequently than emotion-focused coping strategies (Evans, Coman, Stanley, & Burrows, 1993). In terms of job strain-related variables, psychological demands are thought to be particularly detrimental in combination with low decision latitude and low social support (Garbarino, Cuomo, Chiorri, & Magnavita, 2013; Jones, O'Connor, Conner, McMillan, & Ferguson, 2007; Sargent & Terry, 2000). Hence, although the risk clusters did not differ in level of psychological demand, the observed levels may have contributed differentially to the job strain risk pattern.
Lastly, divisions did not differ in risk cluster frequency, that is, neither the high-risk cluster nor the low-risk cluster was more prevalent in any of the three divisions. This finding is in line with the above interpretations suggesting that naturally occurring combinations of organizational and personal risk factors are not division-dependent, but rather related to individual perceptions of the work environment.
General and division-specific links between patterns of risk factors and health outcomes
Importantly, the risk factor combinations revealed by cluster analysis showed strong associations with mental health, such that officers in the high-risk cluster reported more perceived stress, more depressive symptoms, and more posttraumatic stress symptoms. In contrast, officers in the high-risk cluster were only at a trend level more bothered by their physical symptoms compared to the low-risk cluster. However, physical symptom scores were unexpectedly low in general, which may be related to the fact that the questionnaire does not assess clinician-diagnosed presence of symptoms, but perception of symptoms. Self-reported perceptions of symptoms, in turn, may be especially prone to high male-norm pressure.
Furthermore, with the exception of depression, clusters were also differentially linked to specific health outcomes depending on division. Specifically, being in the Emergency division appeared to protect officers against the negative physical health effects of being in the high-risk cluster, while officers in the Community and Criminal division reported to be more bothered by physical symptoms when they were in the high-risk cluster. One possible explanation for this differential finding might be that at the end of their police training, those officers who prefer physically demanding jobs are more likely to choose the Emergency division. Their physical training may then act as a buffer against the negative health effects of being exposed to work-related risk factors (e.g., Gerber & Pühse, 2009).
In contrast, officers from the Community division in the high-risk cluster reported more posttraumatic stress symptoms and officers from the Criminal division in the high-risk cluster reported more perceived stress symptoms. The finding that Community officers in the high-risk cluster reported more posttraumatic stress symptoms may partially be due to division assignment practices. After completing police academy, officers sometimes first enter the Emergency division and then later request to transfer to the Community division due to the rotating shiftwork and exposure to volatile situations associated with Emergency division duty. Hence, Community division officers in the high-risk cluster may represent some of those officers previously exposed to traumatic events during their time in the Emergency division. These experiences may then influence their perception of their current job and in that way emphasize potential individual differences in initial risk factor susceptibility.
Finally, Criminal officers in the high-risk cluster reported more perceived stress than other officers in the high-risk cluster. This may be related to the fact that they carry out their investigations alone and therefore may feel a higher personal responsibility for the quality of the work done, especially given the potential legal consequences of work mistakes. In such a situation, the lack of protective factors such may be particularly damaging. More specifically, in the Emergency and Community divisions, work is often done in teams of three to four junior officers lead by one senior officer allowing for shared responsibility and access to guidance from the senior officer. This advice and support may help to keep stress perceived due to a high-risk context at bay.
Stress-mediated links between patterns of risk factors and health indicators
Lastly, in line with previous police literature (e.g., Gershon et al., 2009), perceived stress was found to be a central pathway linking patterns of risk factors and negative health outcomes. Specifically, in the current study, perceived stress partially mediated the relationships between risk clusters and physical symptoms as well as depressive symptoms and PTSD symptoms.
In terms of physical symptoms, it is unclear to what extent the mediational role of stress is due to known links between stress and physical health outcomes (e.g., Cohen, Janicki-Deverts, & Miller, 2007) or stress effects on how bothersome officers rated their physical symptoms. However, a strong body of work supports both interpretations. Similarly, the role of stress in depressive symptoms has been identified in previous studies and our current findings further support this literature (e.g., Hammen, 2005). In contrast, the fact that stress only partially mediated relationship between risk clusters and posttraumatic stress symptoms suggests that the assessed risk factors may play a stronger role than perceived stress in developing and maintaining PTSD symptoms. For example, severity of posttraumatic stress symptoms appears to be more strongly related to social support and/or non-adaptive coping strategies (e.g., Harvey-Lintz & Tidwell, 1997; Stephens & Long, 2000).
Limitations
Findings from the current study have to be interpreted in light of several limitations. Most importantly, the study's cross-sectional design did not allow for causal interpretations of the results. However, while it is possible that psychological or physical health problems lead to biased perceptions of environmental and individual factors, several longitudinal studies have highlighted the fact that stressful working conditions are an important risk factor for the development of negative health outcomes (De Lange, Taris, Kompier, Houtman, & Bongers, 2004). Second, the organizational structure of police departments varies widely between states and countries, limiting generalizability of the results to police department outside of Switzerland. Third, studies in settings like the current one are prone to selection biases. For example, the study may have appealed the most to chronically stressed police officers but officers who were highly stressed and had limited time may have also decided against participating. Despite assurance of confidentiality regarding participation and anonymity of the data collected, the study took place in the police department building, which may have discouraged some officers from participating. Finally, only a few individuals reached clinical cut-offs in terms of posttraumatic stress disorder and depression, a fact that may explain, for example, the lack of division-dependent cluster differences in depression. However, as expected, social desirability was generally very high in the current study population and is known to be linked to underreporting of problems (e.g., Brunet et al., 1996), especially in high male-norm environments such as the police (Liberman et al., 2002; Pole et al., 2001).
Conclusion and Relevance
In summary, results of the current study support the notion that police officers are a heterogeneous population in terms of processes linking risk factors and health-related indicators. This heterogeneity appeared to be only to some extent related to division-specific work environments and may be more dependent on individuals' perception of their own work conditions as well as personal factors. Hence, some officers may be more at-risk for poor health than others, independent of the type of work they do.
Furthermore, our findings concerning the mediational role of perceived stress are particularly important to consider when implementing prevention programs or interventions. Specifically, while very popular and easy to implement, stress-reduction interventions that do not target job-relevant sources of stress may not be effective in preventing posttraumatic stress (Richardson and Rothstein (2008). Our findings support an intervention approach that focuses on combinations of risk factors and provide a basis upon which future studies can build to determine how these factors may influence each other (e.g., improving social support from superiors may also decrease loneliness) to develop individualized treatment programs.
Highlights.
Police officers from Emergency, Community, and Criminal divisions were assessed.
Cluster analysis revealed 2 patterns of organizational and individual risk factors.
Risk factor patterns were linked to mental health outcomes (e.g., PTSD, stress).
This was specifically true in Community (PTSD) and Criminal officers (stress).
However, physical health appeared to be less affected in Emergency officers.
Acknowledgments
The authors wish to thank the representatives of the police unions, as well as the police management (psychological office, human resources and top management) who promoted and supported this study. We are grateful to all police officers who took the time to participate in the study and gave us this valuable information. The authors would also like to thank Professor André Kuhn at the Swiss-French Center for Research in Criminology, University of Neuchâtel, Switzerland, Professor Serge Guimond at the Laboratory for Social Psychology, University Blaise Pascal, France, as well as Professor Raymund Schwan, at the University of Lorraine, France for their valuable support during the course of this study.
Funding source: This work was supported by a NIGMS “Brain-Body-Behavior Interface in Learning and Development Across the Lifespan” training grant #T32GM084907 (AMG) and a FNS #P2LAP1_148426 Early Post-Doc Mobility Fellowship (SAH).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Stephanie A. Habersaat, Email: Stephanie.Habersaat@gmail.com.
Ashley M. Geiger, Email: ageiger@brandeis.edu.
Sid Abdellaoui, Email: sidhamed.abdellaoui@univ-lorraine.fr.
References
- Aaron JDK. Stress and coping in police officers. Police Quarterly. 2000;3(4):438–450. doi: 10.1177/109861110000300405. [DOI] [Google Scholar]
- Adler N, Epel E, Castellazzo G, Ickovics J. Relationships of subjective and objective social status with psychological and physiological functioning: preliminary data in healthy, White women. Health Psychology. 2000;19(6):586–592. doi: 10.1037//0278-6133.19.6.586. [DOI] [PubMed] [Google Scholar]
- Alkus S, Padesky C. Special problems of police officers: stress-related issues and interventions. Counseling Psychologist. 1983;11:55–64. doi: 10.1177/0011000083112010. [DOI] [Google Scholar]
- Arial M, Gonik V, Wild P, Danuser B. Association of work related chronic stressors and psychiatric symptoms in a Swiss sample of police officers; a cross sectional questionnaire study. International Archives of Occupational and Environmental Health. 2010;83:323–331. doi: 10.1007/s00420-009-0500-z. [DOI] [PubMed] [Google Scholar]
- Arter ML. Stress and deviance in policing. Deviant Behavior. 2008;29:43–69. doi: 10.1080/01639620701457774. [DOI] [Google Scholar]
- Beck AT, Steer RA, Brown GK. The Beck Depression Inventory. 2nd. San Antonio: 1996. [Google Scholar]
- Blais MR, Lachance L, Riddle A. Unpublished manuscript. University of Quebec; Montreal, Canada: 1991. Validation of the French version of the Marlowe-Crowne measure of social desirability. [Google Scholar]
- Bourque P, Beaudette D. Psychometric study of the Beck Depression Inventory on a sample of French-speaking university students. Canadian Journal of Behavioural Science/Revue canadienne des sciences du comportement. 1982;14(3):211–218. doi: 10.1037/h0081254. [DOI] [Google Scholar]
- Brunet A, Boucher C, Boyer R. Social Desirability in the Assessment of Trauma. Psychological Reports. 1996;79:511–514. doi: 10.2466/pr0.1996.79.2.511. [DOI] [PubMed] [Google Scholar]
- Cohen S, Hoberman H. Positive events and social supports as buffers of life change stress. Journal of Applied Social Psychology. 1983;13:99–125. [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24:385–396. [PubMed] [Google Scholar]
- Cousson-Guélie F, Cosnefroy O, Christophe V, Segrestan-Crouzet C, Merckaert I, Fournier E, et al. Razavi D. The ways of coping cecklist (WCC): validation in French speaking cancer patients. Journal of Health Psychology. 2010;20(5):1–11. doi: 10.1177/1359105310364438. [DOI] [PubMed] [Google Scholar]
- Crowne DP, Marlowe D. A new scale of social desirability independent of psychopathology. Journal of Consulting Psychology. 1960;24(4):349–354. doi: 10.1037/h0047358. [DOI] [PubMed] [Google Scholar]
- Dantzer ML. Police-related stress: a critique for future research. Journal of Police Criminal Psychology. 1987;3:43–48. doi: 10.1007/BF02806523. [DOI] [Google Scholar]
- de Grâce GR, Joshi P, Pelletier R. L'échelle de solitude de l'Université Laval (ÉSUL): validation canadienne-française du “UCLA loneliness scale”. Revue Canadienne des Sciences du Comportement. 1993;25(1):12–27. [Google Scholar]
- De Lange AH, Taris TW, Kompier MAJ, Houtman ILD, Bongers PM. The relationships between work characteristics and mental health: examining normal, reversed and reciprocal relationships in a 4-wave study. Work & Stress. 2004;18(1):149–166. doi: 10.1080/02678370412331270860. [DOI] [Google Scholar]
- Evans Barry J, Coman Greg, Stanley Robb O, Burrows Graham D. Police officers' coping strategies: An Australian police survey. Stress Medicine. 1993;9(4):237–246. [Google Scholar]
- Folkman S, Lazarus RS. An analysis of coping in middle-aged community sample. Journal of Health and Social Behavior. 1980;21(3):219–239. [PubMed] [Google Scholar]
- Furlanetto LM, Mendlowicz MV, Bueno JR. The validity of the Beck Depression Inventory-Short form as a screening and diagnostic instrument for moderate and severe depression in medical patients. Journal of Affective Disorders. 2005;86(1):87–91. doi: 10.1016/j.jad.2004.12.011. [DOI] [PubMed] [Google Scholar]
- Galatzer-Levy IR, Brown AD, Henn-Haase C, Metzler TJ, Neylan TC, Marmar CR, et al. Positive and negative emotion prospectively predict trajectories of resilience and distress among high-exposure police officers. Emotion. 2013;13(3):545–553. doi: 10.1037/a0031314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garbarino S, Cuomo G, Chiorri C, Magnavita N. Association of work-related stress with mental health problems in a special police force unit. BMJ open. 2013;3(7):e002791. doi: 10.1136/bmjopen-2013-002791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gershon R, Barocas B, Canton AN, Li X, Vlahov D. Mental, physical, and behavioral outcomes associated with perceived work stress in police officers. Criminal Justice and Behavior. 2009;36(3):275–289. doi: 10.1177/0093854808330015. [DOI] [Google Scholar]
- Gerst MS, Grant I, Yager J, Sweetwood H. The reliability of the social readjustment rating scales: moderate and long-term stability. Journal of Psychosomatic Research. 1978;22(6):519–523. doi: 10.1016/0022-3999(78)90008-9. [DOI] [PubMed] [Google Scholar]
- Haisch DC, Meyers LS, et al. MMPI-2 assessed post-traumatic stress disorder related to job stress, coping, and personality in police agencies. Stress and Health. 2004;20(4):223–229. [Google Scholar]
- Hall GB, Dollard MF, Tuckey MR, Winefield AH, Thompson BM. Jobs demands, work-family conflict, and emotional exhaustion in police officers: A longitudinal test of competing theories. Journal of Occupational and Organizational Psychology. 2010;83:237–250. doi: 10.1348/096317908X401723. [DOI] [Google Scholar]
- Harmon DK, Masuda M, Holmes TH. The social readjusment rating scale: a cross-cultural study of Western Europeans and Americans. Journal of Psychosomatic Research. 1970;14(4):391–400. doi: 10.1016/0022-3999(70)90007-3. [DOI] [PubMed] [Google Scholar]
- Harpold J, Feenster SL. Negative influences of police stress. FBI Law Enforcement Bulletin. 2002;71(9):1–7. [Google Scholar]
- Harvey-Lintz T, Tidwell R. Effects of the 1992 Los Angeles civil unrest: post traumatic stress disorder symptomatology among law enforcement officers. The Social Science Journal. 1997;34:171–183. doi: 10.1016/S0362-3319(97)90049-5. [DOI] [Google Scholar]
- Holmes TH, Rahe RH. The Social Readjustment Rating Scale. Journal of Psychosomatic Research. 1967;11(2):213–218. doi: 10.1016/0022-3999(67)90010-4. [DOI] [PubMed] [Google Scholar]
- Jones F, O'Connor DB, Conner M, McMillan B, Ferguson E. Impact of daily mood, work hours, and iso-strain variables on self-reported health behaviors. Journal of Applied Psychology. 2007;92(6):1731. doi: 10.1037/0021-9010.92.6.1731. [DOI] [PubMed] [Google Scholar]
- Keane TM, Caddell JM, Taylor KL. Mississippi Scale for Combat-Related Posttraumatic Stress Disorder: Three studies in reliability and validity. Journal of Consulting and Clinical Psychology. 1988;56:85–90. doi: 10.1037/0022-006X.56.1.85. [DOI] [PubMed] [Google Scholar]
- Lau B, Hem E, Berg AM, Ekeberg Ø, Torgersen S. Personality types, coping, and stress in the Norwegian police service. Personality and Individual Differences. 2006;41(5):971–982. [Google Scholar]
- Liberman AM, Best SR, Metzler TJ, Fagan JA. Routine Occupational Stress and Psychological Distress in Police. Policing: An International Journal of Police Strategies & Management. 2002;25(2):421–439. [Google Scholar]
- Lilly MM, Pole N, Best SR, Metzler T, Marmar CR. Gender and PTSD: What Can We Learn From Female Police Officers? Journal of Anxiety Disorders. 2009;23(6):767–774. doi: 10.1016/j.janxdis.2009.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lobel M, Dunkel-Schetter C. Conceptualizing stress to study the effects on health: Environmental, perceptual and emotional components. Anxiety Research. 1990;3:213–230. doi: 10.1080/08917779008248754. [DOI] [Google Scholar]
- Lott LD. Deadly secrets: violence in the police family. FBI Law Enforcement Bulletin. 1995;64(11):12–17. [Google Scholar]
- Maia DB, Marmar CR, Metzler T, Nóbrega A, Berger W, Mendlowicz MV, et al. Figueira I. Post-traumatic stress symptoms in an elite unit of Brazilian police officers: prevalence and impact on psychosocial functioning and on physical and mental health. Journal of Affective Disorders. 2007;97(1):241–245. doi: 10.1016/j.jad.2006.06.004. [DOI] [PubMed] [Google Scholar]
- Marmar CR, McCaslin SE, Metzler TJ, Best S, Weiss DS, Fagan J, et al. Neylan T. Predictors of posttraumatic stress in police and other first responders. Annals of the New York Academy of Sciences. 2006;1071(1):1–18. doi: 10.1196/annals.1364.001. [DOI] [PubMed] [Google Scholar]
- Martinussen M, Richardsen AM, Burke RJ. Job demands, job resources, and burnout among police officers. Journal of Criminal Justice. 2007;35:239–249. doi: 10.1016/j.jcrimjus.2007.03.001. [DOI] [Google Scholar]
- Morash M, Haarr R, Kwak DH. Multilevel Influences on Police Stress. Journal of Contemporary Criminal Justice. 2006;22(1):26–43. [Google Scholar]
- Niedhammer I, Chastang JF, Gendrey L, David S, Degioanni S. Propriétés psychométriques de la version française des échelles de la demande psychologique, de la latitude décisionnelle et du soutien social du “Job Content Questionnaire” de Karasek: résultats de l'enquête nationale SUMER. Santé publique. 2006;18(3):413–427. doi: 10.3917/spub.063.0413. [DOI] [PubMed] [Google Scholar]
- Pienaar J, Rothmann S, van de Vijver FJR. Occupational stress, personality, coping strategies and suicide ideation in the South African police service. Criminal Justice and Behavior. 2007;34(2):246–258. doi: 10.1177/0093854806288708. [DOI] [Google Scholar]
- Pole N, Best SR, Weiss DS, Metzler T, Liberman AM, Fagan J, Marmar CR. Effects of gender and ethnicity on duty-related posttraumatic stress symptoms among urban police officers. Journal of Nervous and Mental Disease. 2001;189(7):442–448. doi: 10.1097/00005053-200107000-00005. [DOI] [PubMed] [Google Scholar]
- Richardson KM, Rothstein HR. Effects of occupational stress management intervention programs: a meta-analysis. Journal of Occupational Health Psychology. 2008;13(1):69. doi: 10.1037/1076-8998.13.1.69. [DOI] [PubMed] [Google Scholar]
- Rolland JP. Traduction française du Perceived Stress Scale. Université Paris Ouest Nanterre La Défense; 1991. [Google Scholar]
- Russel D, Peplau LA, Cutrona CE. The revised U.C.L.A. loneliness scale: concurrent and discriminant validity evidence. Journal of Personality and Social Psychology. 1980;39:472–480. doi: 10.1037/0022-3514.39.3.472. [DOI] [PubMed] [Google Scholar]
- Sargent Leisa D, Terry Deborah J. The moderating role of social support in Karasek's job strain model. Work & Stress. 2000;14(3):245–261. [Google Scholar]
- Sheehan R, Van Hasselt V. Identifying law enforcement stress reactions early. FBI Law Enforcement Bulletin. 2003;72(1):12–17. [Google Scholar]
- Singh-Manoux A, Adler NE, Marmot MG. Subjective social status: Its determinants and its association with measures of ill-health in the Whitehall II study. Social Science and Medicine. 2003;56:1321–1333. doi: 10.1016/S0277-9536(02)00131-4. [DOI] [PubMed] [Google Scholar]
- Stephens C, Long N. Communication with police supervisors and peers as a buffer of work-related trauamtic stress. Journal of Organizational Behavior. 2000;21:407–424. doi: 10.1002/(SICI)1099-1379(200006)21:4<407∷AID-JOB17>3.0.CO;2-N. [DOI] [Google Scholar]
- Swatt ML, Gibson CL, Piquero NL. Exploring the utility of general strain theory in explaining problematic alcohol consumption by police officers. Journal of Criminal Justice. 2007;35:596–611. doi: 10.1016/j.jcrimjus.2007.09.005. [DOI] [Google Scholar]
- Violanti JM, Burchfiel C, Miller DB, Andrew M, Dorn J, Wactawski-Wende J, et al. Trevisan M. The Buffalo Cardio-Metabolic Occupational Police Study (BCOPS). Pilot Study: Methods and Participants Characteristics. Annals of Epidemiology. 2006;16(2):148–156. doi: 10.1016/j.annepidem.2005.07.054. [DOI] [PubMed] [Google Scholar]
- Waters JA, Ussery W. Police stress: History, contributing factors, symptoms, and interventions. Policing: An International Journal of Police Strategies & Management. 2007;30(2):169–188. [Google Scholar]