Highlights
-
•
ACC is a rare and aggressive type of tumor, the prognosis is poor.
-
•
Frequently, vena cava invasion occurs.
-
•
Infrequently, tumor thrombus can extend to the right atrium.
-
•
R0 resection is the only curative option.
-
•
Thrombectomy required the assistance of cardiopulmonary bypass and hypothermia.
Keywords: Adrenocortical carcinoma, Thrombus, Invasion, Inferior vena cava
Abstract
Introduction
Adrenocortical carcinoma (ACC) is a rare, but highly aggressive type of tumor with an annual incidence of 1–2 cases per million. The prognosis is poor with a five-year overall survival rate of ∼35%. The poor prognosis may be related to the advanced stage at which the majority of ACCs are detected. Complete surgical resection remains the most effective treatment.
Presentation of the case
A 51-year-old female patient with recent onset of dyspepsia, ascites and peripheral edema was referred to our institution. Computed tomography (CT) and Magnetic Resonance Imaging (MRI) displayed a 8 cm Ø right adrenal mass. Moreover a tumor thrombus jutted out into the IVC, left renal vein and right atrium. An echocardiographic evaluation confirmed the presence of the tumor thrombus in the right atrium. The patient underwent adrenalectomy with removal of its intravascular extension with the assistance of cardiopulmonary bypass and hypothermia.
Discussion
ACC is a rare malignancy and ACC with tumor thrombus extension is a rare presentation. Patients can present with a variety of sign and symptoms, depending on the extent of the tumor. CT scan of chest and abdomen represents the gold standard in ACC staging while magnetic resonance imaging (MRI) is preferred for tumor thrombus characterization. Complete surgical resection with a negative margin, R0 resection, is the only curative option for localized disease. Kidney sparing surgery should be performed when possible.
Conclusion
We present a rare case of Adrenocortical carcinoma with tumor thrombus extending into the IVC and right atrium. Complete resection with negative margins represents the best therapeutic chance for these patients.
1. Introduction
Adrenocortical carcinoma (ACC) is a rare, but highly aggressive type of tumor with an annual incidence of 1–2 cases per million [1–3]. Furthermore, a higher incidence of ACC has been reported in females. ACC behave a bimodal age distribution with two peaks: the first, concerning children in the first decade of life and the other regarding adults in the fourth to fifth decades of life [4–6]. The prognosis is poor with a five-year overall survival rate of ∼35%. These low survival rates are in part related to the advanced stage of ACCs detection. Complete surgical resection remains the most effective treatment and, along with an early staging, is among the strongest predictors of overall survival. Up to 40% of adrenal tumors are nonfunctional with late clinical manifestation during the course of disease as a large mass causing early satiety, weight loss, or abdominal pain [7]. The general surgical strategy for ACC is “en bloc” resection, which often includes adjacent organs like kidney, liver, pancreas, spleen, or bowel. Vena cava invasion, which qualifies ACC as stage III disease, occurs most commonly with larger, right-sides tumors. Infrequently, tumor thrombus can extend to the renal vein, IVC and right atrium without invading the vascular endothelium. In these cases, extensive thrombectomy has been advocated [8–9]. Herein, we report a rare case of ACC with inferior vena cava and left renal vein involvement plus an additional right atrium tumor thrombus extension in a female patient.
2. Case report
A 51-year-old female patient with a family history of renal cell carcinoma and retroperitoneal carcinoma was admitted to our institution for a recent onset of dyspepsia, ascites and peripheral edema. Laboratory values for plasma free metanephrines, aldosterone, potassium, and testosterone were all within normal range. CT scan and MRI displayed a 8 cm Ø, right adrenal mass. A thrombus extended into the IVC, left renal vein and right atrium. An echocardiographic evaluation confirmed the presence of the tumor thrombus in the right atrium. Since the symptoms of the patient worsened, the patient underwent urgent adrenalectomy with the assistance of cardiopulmonary bypass and hypothermia with full removal of its intravascular extension. The surgery required the collaboration of the general surgery team and the cardiothoracic one
The right atrium was opened and by direct visualization the tumor thrombus was completely removed by the atrium and by the IVC (Figs. 1 and 2). The procedure was completed as usual without complications, the postoperative course was uneventful and the patient was discharged on postoperative day 10 without morbidity. The histopathology confirmed the diagnosis of ACC with tumor thrombosis of IVC, left renal vein and right atrium. The patient receive adjuvant mitotane therapy post operatively [13,14]. At the follow up time of 12 months, the patients remains free of local/systemic recurrence.
Fig. 1.
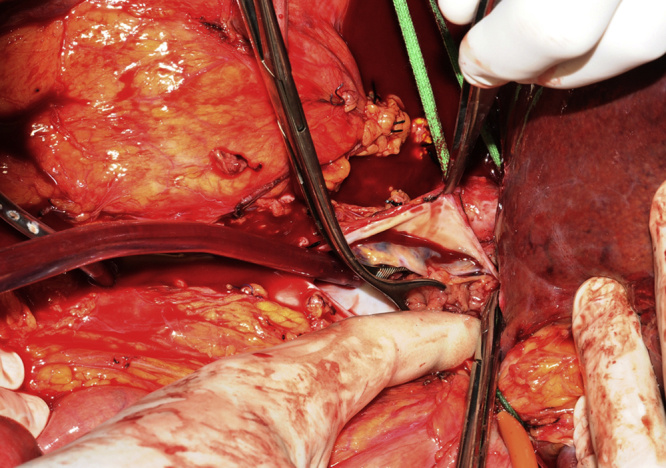
Intraoperative Photographs. The IVC thrombus was removed.
Fig. 2.
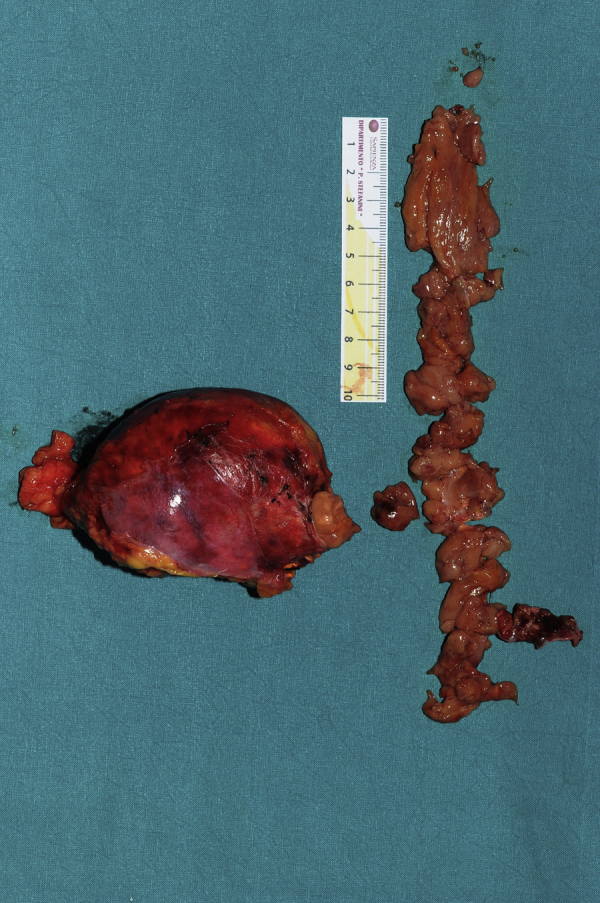
Operative specimen: right adrenalectomy and tumor thrombus into the IVC, right atrium and left renal vein was performed.
3. Discussion
ACC is a rare malignancy and ACC with tumor thrombus extension is a rare presentation of this pathology [1–3]. Patients can present with a variety of sign and symptoms, depending on the extent of the tumor. CT scan of the chest and the abdomen is represents to date, the gold standard for ACC staging. With regards to the tumor thrombus, magnetic resonance imaging (MRI) represents the better imaging modality in order to assess the extension and the features of the thrombus. Complete surgical resection with a negative margin, R0 resection, is the only curative option for localized disease [5]. The presence of a thrombus represent an additional risk factor due to the supplementary complexity of the surgery. Accordingly for tumors extending into the atrium, the institution of a cardiopulmonary bypass as well as a cardiothoracic surgical assistance is mandatory [9–12]. Kidney sparing surgery should be performed when possible, reserving en bloc nephrectomy only in the case of renal invasion. Yet, even with an R0 resection, 50–80% of patients develop relapse and/or progression to metastatic disease. The role of surgery in patients with recurrent and metastatic disease remains controversial. A recent study by Erdogan et al., [15] compared clinical outcomes in ACC relapsing patients who underwent surgery with relapsing patients who did not. They concluded that progression-free survival was improved if the time elapsed from the first relapse was greater than 12 months and if patients were suitable to undergo an R0 resection for their recurrence. Although a debulking surgery, R2 resection, did not significantly improve progression-free survival. In this case, we accomplished a R0 resection with an aggressive approach leading to a 12 month survival in absence of any signs of recurrence and with a good quality of life. This confirms that aggressive surgery should be considered even in the setting of most advanced ACCs probably offering the only chance of survival for this aggressive tumor.
4. Conclusion
Given the current and predicted impact of ACCs, although our results have been obtained on a single patient and thus need to be confirmed on a wider sample, they prompt us to suggest a meditation concerning the indication for an aggressive surgical intervention. Since the long-term survival and remission are closely related to the stage of the disease, complete resection with negative margins thus represents, to date, the best chance of cure for the patient prolonging and improving their quality of life.
Conflict of interest
None.
Funding
None.
Ethical approval
Not requested.
Consent
Not requested.
Authors’ contributions
Pronio A.: study concept and writing the paper.
Piroli S.: data analysis.
Ciamberlano B.: data collection.
De Luca A.: data collection.
Marullo A: paper reviewer.
Barretta A.: paper reviewer.
Mazzesi G.: cardiovascular surgeon.
Rossi M: general surgeon.
Montesani C.: general surgeon chief.
Research registry
Not requested
Guarantor
Pronio Annamaria.
References
- 1.Chiche L., Dousset B., Kieffer E., Chapuis Y. Adrenocortical carcinoma extending into the inferior vena cava: presentation of a 15-patient series and review of the literature. Surgery. 2006;139(1):15–27. doi: 10.1016/j.surg.2005.05.014. [DOI] [PubMed] [Google Scholar]
- 2.Ayala-Ramirez M., Jasim S., Feng L. Adrenocortical carcinoma: clinical outcomes and prognosis of 330 patients at a tertiary care center. Eur. J. Endocrinol. 2013;169:891–899. doi: 10.1530/EJE-13-0519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wandoloski Melissa, Kimberly Bussey Kimberly J., Michael Demeure Michael J. Adrenocortical cancer. Surg. Clin. N. Am. 2009;89:1255–1267. doi: 10.1016/j.suc.2009.06.019. [DOI] [PubMed] [Google Scholar]
- 4.Fassnacht Martin, Allolio Bruno. Clinical management of adrenocortical carcinoma. Best Pract. Res. Clin. Endocrinol. Metab. 2009;23:273–289. doi: 10.1016/j.beem.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 5.Fassnacht M., Libé R., Kroiss M., Allolio B. Adrenocortical carcinoma: a clinician’s update. Nat. Rev. Endocrinol. 2011;7:323–335. doi: 10.1038/nrendo.2010.235. [DOI] [PubMed] [Google Scholar]
- 6.Wei Yong-Bao, Gao Yun-Liang, Wu Hong-Tao, Ou- Yang Shi-Feng, Xu Tao, Mao Dong-Fanf, Yang Jin-Rui. Rare Incidence of primary adrenocortical carcinosarcoma: a case report and literature review. Oncol. Lett. 2015;9:153–158. doi: 10.3892/ol.2014.2635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patalano A., Brancato V., Mantero F. Adrenocortical cancer treatment. Horm. Res. 2009;71(suppl. 1):99–104. doi: 10.1159/000178049. [DOI] [PubMed] [Google Scholar]
- 8.Mezhir James J., Song Jie, Piano Giancarlo, Testa Giuliano, Raman Jaishankar, Al-Ahmadie Hikmat A., Angelos Peter. Adrenocortical carcinoma invading the inferior vena cava: case report and literature review. Endocr. Pract. 2008;Vol 14(6):271. doi: 10.4158/EP.14.6.721. [DOI] [PubMed] [Google Scholar]
- 9.Yavascaoglu Ismet, Yilmaz Mert, Kordan Yakup. Cardiac and caval invasion of left adrenocortical carcinoma. Urol. Int. 2008;81:244–246. doi: 10.1159/000144071. [DOI] [PubMed] [Google Scholar]
- 10.Chiappini B., Savini C., Marinelli G., Suarez S.M., Di Eusanio M., Fiorani V., Pierangeli A. Cavoatrial tumor thrombus: single-stage surgical approach with profound hypothermia and circulatory arrest, including a review of the literature. J. Thorac. Cardiovasc. Surg. 2002;124(October (4)):684–688. doi: 10.1067/mtc.2002.124295. [DOI] [PubMed] [Google Scholar]
- 11.Ohwada S., Izumi M., Tanahashi Y. Combined liver and inferior vena cava resection for adrenocortical carcinoma. Surg. Today. 2007;37:291–297. doi: 10.1007/s00595-006-3404-5. [DOI] [PubMed] [Google Scholar]
- 12.Shahian D.M., Nieh P.T., Libertino J.A. Resection of atriocaval adrenal carcinoma using hypothermic circulatory arrest. Ann. Thorac. Surg. 1989;48:421–422. doi: 10.1016/s0003-4975(10)62870-6. [DOI] [PubMed] [Google Scholar]
- 13.Lacroix A. Approach to the patient with adrenocortical carcinoma. J. Clin. Endocrinol. Metab. 2010;95:4812–4822. doi: 10.1210/jc.2010-0990. [DOI] [PubMed] [Google Scholar]
- 14.Rachel Aufforth D., Nilubol Naris. Emerging therapy for adrenocortical carcinoma. Int. J. Endocr. Oncol. 2014;1(2):173–182. doi: 10.2217/ije.14.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Erdogan I., Deutschbein T., Jurowich C. The role of surgery in the management of recurrent adrenocortical carcinoma. J. Clin. Endocrinol. Metab. 2013;98(1):181–191. doi: 10.1210/jc.2012-2559. [DOI] [PubMed] [Google Scholar]


