Highlights
-
•
The real cause of symptoms in patients with neuropathy may not be related with diabetes.
-
•
It is essential to investigate the etiology of the disease with more localized pathologies in such complicated cases.
-
•
Tarsal tunnel syndrome gives a more segmental clinical profile with nerve entrapment.
Keywords: Tarsal tunnel syndrome, Diabetic polyneuropathy, Pain, Magnetic resonance, Superficial ultrasound
Abstract
Introduction
Various causes influence the etiology of tarsal tunnel syndrome including systemic diseases with progressive neuropathy, such as diabetes.
Presentation of case
We describe a 52-year-old male patient with complaints of numbness, burning sensation and pain in both feet. The laboratory results showed that the patient had uncontrolled diabetes, and the EMG showed distal symmetrical sensory-motor neuropathy and nerve entrapment at the right. Ultrasonography and MRI showed the cyst in relation to medial plantar nerve, and edema- moderate atrophy were observed at the distal muscles of the foot.
Discussion
Foot neuropathy in diabetic patients is a complex process. So, in planning the initial treatment, medical or surgical therapy is selected based on the location and type of the pathology. Foot deformities can be corrected with resting, anti-inflammatory treatment, appropriate shoes, orthesis and socks, and if required, ankle stabilization can be attempted. If the patient is still unresponsive, surgical treatment may be applied.
Conclusion
It is essential to investigate more localized reasons like tarsal tunnel syndrome that may mimic diabetic neuropathy, should be treated primarily.
1. Introduction
The tarsal tunnel is a fibroosseous structure of the foot positioned posteromedially, extending from the medial malleolus toward the navicular bone. It encloses the posterior tibial tendon, flexor hallucis longus tendon and flexor digitorum longus tendon, along with the posterior tibial artery, veins, nerves and branches [1].
Tarsal tunnel syndrome is an entrapment neuropathic syndrome that develops upon compression of the posterior tibial nerve or its branches (medial and lateral plantar nerves) by the flexor retinaculum. Systemic disease progression with neuropathy such as diabetes should be considered during differential diagnosis. Elucidating the etiology is the first step in treatment. We report a case with tarsal tunnel syndrome masked by painful diabetic polyneuropathy in an effort to raise awareness of this syndrome and describe to diagnostic approach to the patient.
2. Presentation of case
A 52-year-old male patient was admitted with complaints of numbness, burning sensation and pain in both feet (but predominantly in the right foot). These complaints were present for the preceding 5 months but increased within the last 1 month. He had been using oral antidiabetics due to type 2 diabetes. He suffered from the pain in his right foot increased upon walking, which intensified through the first toe and medial foot.
On neurological examination, bilateral hypoactive Achilles reflexes, hypoesthesia and hypoalgesia were present on both feet, more prominent on right foot. Tinel test was positive in right ankle. No weakness was detected.
The laboratory results were as follows: fasting plasma glucose 243 mg/dl, hemoglobin A1c 9.2%, spot urine creatinine 299 mg/dl and microalbumin 232 mg/dl. The laboratory results showed that the patient had uncontrolled diabetes, and his complaints were considered to be related to this finding. His paraesthetic complaints improved after insulin treatment for diabetes; however, his pain remained.
Nerve conduction studies revealed low compound muscle action potential (CMAP) amplitude in right tibialis nerve, non-detectable sensory nerve action potential (SNAP) of medial plantar nerve and chronic neurogenic changes on needle EMG (long term, polyphasic, high-amplitude motor unit potentials with decreased recruitment) of right abductor hallucis (AH) and abductor digiti quinti (ADQ) muscles. These findings suggested an entrapment of the posterior tibial nerve at tarsal tunnel level (Fig. 1). A mild sensory-motor polyneuropathy was also suspected, because of slowing in motor nerve velocity of examined nerves and a slight decrease in both sural nerves' SNAP amplitudes. This was thought to be diabetes related. In addition, results compatible with bilateral carpal tunnel syndrome were found.
Fig. 1.
Nerve conduction studies of bilateral posterior tibial nerves. Med. Malleo: medial malleol, Pop. Fossa: popliteal fossa, ADQ: abductor digiti quinti, AH: abductor hallucis.
Superficial US imaging showed a homogenous cystic lesion sized 15 × 10 mm located medially to the medial plantar artery and vein (Fig. 2).
Fig. 2.
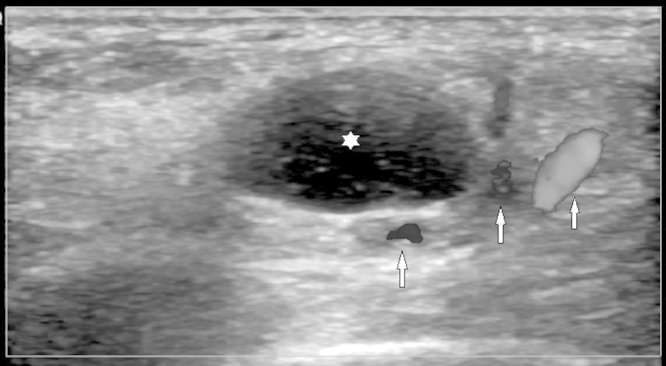
Well circumscribed, anechoic cystic lesion (asterisk) adjacent to the posterior tibial artery and vein (arrows) in the medial foot.
MRI of the foot and ankle revealed a homogenous, T1 hypo-, T2 hyperintense ganglion cyst located at the medial calcaneus, showing peripheral contrast uptake. The localization of the cyst in relation to the flexor hallucis longus tendon, posterior tibial artery and medial plantar nerve was assessed (Fig. 3). Edema and moderate atrophy were observed at the abductor hallucis and flexor hallucis brevis muscles (Fig. 4).
Fig. 3.

(a) Axial T1 turbo spin echo (TSE), (b) axial short tau inversion recovery (STIR) TSE, (c) axial post contrast T1 spectral presaturation with inversion recovery (SPIR) demonstrate T1 hypointense, T2 hyperintense and peripherally contrasted cystic lesion (ganglion cyst) (star) with closed relations in the flexor retinaculum (small arrow), medial plantar nerve (black arrow), flexor hallucis longus tendon (arrow head) and posterior tibial artery–vein (large arrow) positioned medially on the calcaneus (C) in the tarsal tunnel localization.
Fig. 4.
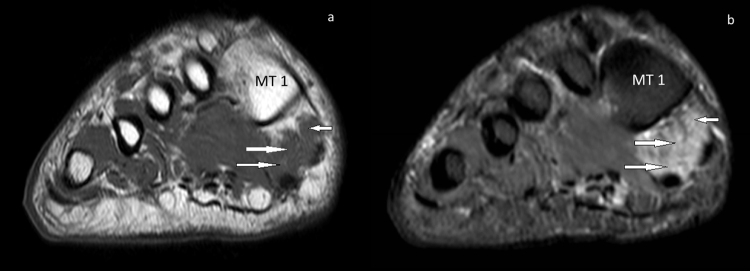
(a) coronal T1 TSE, (b) coronal short tau inversion recovery (STIR) TSE. Moderate volume loss in a and hyperintensity in b are seen in the abductor hallucis (small arrow) and flexor hallucis brevis (large arrows) muscles at the plantar side of the distal foot. The findings are compatible with muscle atrophy. (MT 1): first metatarsal.
Tarsal tunnel syndrome in relation with mild sensory-motor polyneuropathy of diabetic origin was diagnosed based on clinical symptoms, electrophysiological findings and imaging of a ganglion cyst at the tarsal tunnel level on US and MRI.
The patient was referred to the department of surgery with the diagnosis of tarsal tunnel syndrome. However, the patient refused surgery and regularly used his anti-diabetes medication during the following four months, electrophysiological findings worsened at control investigation.
3. Discussion
Tarsal tunnel syndrome develops from compression of the posterior tibial nerve and its branches within the tarsal tunnel. Compression may occur due to traumatic causes such as fracture, surgery or scar tissue [2], but it may also be associated with space-occupying lesions including tumors, ganglion, varicose vascular structures and abnormal muscle tissue (accessory flexor digitorum longus muscle or hypertrophic adductor hallucis) [3]. In addition, it may develop in the foot in relation to deformities such as valgus/ varus deformity, pes planus and tarsal coalition [4]. Systemic diseases such as diabetes, rheumatoid arthritis and peripheral arterial disease may also cause tarsal tunnel syndrome [5]. Despite all possible causes, the exact cause of the disease is sometimes unclear.
The symptoms depend on which branch of the posterior tibial nerve is involved and the location of the involvement. Physical examination generally shows loss of sensation at the plantar face of the foot and positive Tinel’s findings. Patients suffer from pain with a burning sensation at the toes and plantar region. The condition may be accompanied by paraesthesia and dysesthesia, and the findings increase with activity. Motor function impairment is a late finding that is generally unnoticeable, and weakness may develop rarely at the toe flexors. In addition to the clinical manifestations, decreased conduction rate in the posterior tibial nerve as seen on EMG confirms the diagnosis.
US examinations can show space-occupying solid or cystic lesions; however, it is difficult to assess muscle innervations in the absence of atrophy.
MRI examinations are extremely useful in assessing the tarsal tunnel, defining the etiology of the syndrome and determining the differential diagnosis. Flexor hallucis longus tenosynovitis may become the cause of nerve compression in severe conditions. In some cases, ankle ganglions cause these symptoms. In the majority of cases, the nerve cannot be visualized completely along its trace. However, the nerve volume, signal alterations and distortions in the nerve trace should be considered [6]. These evaluations can help eliminate the above-mentioned etiologic causes. Some cases may present with a mild signal alteration in the abductor hallucis and flexor hallucis brevis muscles innerved by the medial plantar nerve, and advanced cases may develop atrophy. As in the case presented here, atrophy generally affects distal muscles.
Systemic disease progression with neuropathy should be considered during differential diagnosis. Diabetic neuropathy is diagnosed in diabetic patients with complaints and findings of peripheral nerve dysfunction in the absence of other causative conditions [7]. The most common symptoms of polyneuropathy in diabetic patients are tingling, coldness, pain and paraesthesia in the legs, particularly notable at distal sites. Examination shows stocking-glove sensory loss. Moderate atrophy and paresis may be encountered at the intrinsic muscles of the foot [8].
Carpal tunnel syndrome, another entrapment neuropathy, is encountered in the diabetic population at higher rate than that in the general population. Watanabe et al. reported that tibial nerve in tarsal tunnel and median nerve in carpal tunnel increase in terms of cross sectional area in diabetic patients [9]. Those results were compatible with systemic effects of diabetes and our patient also had carpal tunnel syndrome accompanying tarsal tunnel syndrome.
Whether the entrapment neuropathies that develop in diabetic patients are directly associated with diabetes is controversial [10,11]. Foot neuropathy in diabetic patients is a complex process. So, in planning the initial treatment, medical or surgical therapy is selected based on the location and type of the pathology. Foot deformities can be corrected with resting, anti-inflammatory treatment, appropriate shoes, orthesis and socks, and if required, ankle stabilization can be attempted. Physical therapy modalities might be preferred in suitable cases. Tricyclic antidepressant medications and antiepileptic agents such as gabapentin and pregabalin may be useful. Lidocain and cortisone can be injected locally to the nerve trace. If the patient is still unresponsive, surgical treatment may be applied [1].
4. Conclusion
Successful treatment of the initial condition of neuropathic foot pain in diabetic patients involves elimination of the causes of neuropathic pain, particularly tarsal tunnel syndrome. Pathologies that may mimic diabetic neuropathy should be treated primarily.
Funding
None.
Ethical approval
N/A.
Consent
Obtained.
Conflict of interest
None.
Contributor Information
Tugrul Ormeci, Email: tug_ormeci@yahoo.co.uk.
Mahir Mahirogulları, Email: mmahirogullari@medipol.edu.tr.
Fikret Aysal, Email: fikretaysal@yahoo.com.
References
- 1.Delfaut E.M., Demondion X., Bieganski A., Thiron M.C., Mestdagh H., Cotten A. Imaging of foot and ankle nerve entrapment syndromes: from well-demonstrated to unfamiliar sites. Radiographics. 2003;23:613–623. doi: 10.1148/rg.233025053. [DOI] [PubMed] [Google Scholar]
- 2.Aszmann O.C., Ebmer J.M., Dellon A.L. Cutaneous innervation of the medial ankle: an anatomic study of the saphenous, sural, and tibial nerves and their clinical significance. Foot Ankle Int. 1998;19:753–756. doi: 10.1177/107110079801901108. [DOI] [PubMed] [Google Scholar]
- 3.Sammarco G.J., Conti S.F. Tarsal tunnel syndrome caused by an anomalous muscle. J. Bone Joint Surg. Am. 1994;76:1308–1314. doi: 10.2106/00004623-199409000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Trepman E., Kadel N.J., Chisholm K., Razzano L. Effect of foot and ankle position on tarsal tunnel compartment pressure. Foot Ankle Int. 1999;20:721–726. doi: 10.1177/107110079902001108. [DOI] [PubMed] [Google Scholar]
- 5.Donovan A., Rosenberg Z.S., Cavalcanti C.F. MR imaging of entrapment neuropathies of the lower extremity. Part 2. The knee, leg, ankle, and foot. Radiographics. 2010;30(4):1001–1019. doi: 10.1148/rg.304095188. [DOI] [PubMed] [Google Scholar]
- 6.Lee M.F., Chan P.T., Chau L.F., Yu K.S. Tarsal tunnel syndrome caused by talocalcaneal coalition. Clin. Imaging. 2002;26:140–143. doi: 10.1016/s0899-7071(01)00355-2. [DOI] [PubMed] [Google Scholar]
- 7.Boulton A.J., Gries F.A., Jervell J.A. Guidelines for the diagnosis and outpatient management of diabetic peripheral neuropathy. Diabet. Med. 1998;15:508–514. doi: 10.1002/(SICI)1096-9136(199806)15:6<508::AID-DIA613>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 8.Bird S.J., Brown M.J. Diabetic neuropahhies. In: Katırjı B., Kominski H.J., Preston D.C., Ruff R.L., Shapino B.E., editors. Neuromuscular Disorders in Clinical Practice. Butterworth Heinemann; USA: 2002. pp. 598–621. [Google Scholar]
- 9.Watanabe T., Ito H., Sekine A., Katano Y., Nishimura T., Kato Y. Sonographic evaluation of the peripheral nerve in diabetic patients: the relationship between nerve conduction studies, echo intensity, and cross-sectional area. J. Ultrasound Med. 2010;29:697–708. doi: 10.7863/jum.2010.29.5.697. [DOI] [PubMed] [Google Scholar]
- 10.Fraser D.M., Campbell I.W., Ewing D.J., Clarke B.F. Mononeuropathy in diabetes mellitus. Diabetes. 1979;28:96–101. doi: 10.2337/diab.28.2.96. [DOI] [PubMed] [Google Scholar]
- 11.Boyd B.S., Dilley A. Altered tibial nerve biomechanics in patients with diabetes mellitus. Muscle Nerve. 2014;50:216–223. doi: 10.1002/mus.24155. [DOI] [PubMed] [Google Scholar]



