Abstract
Background
It is unclear how radiographic measurements of cup position are sensitive to deviations from a perfect AP pelvis image.
Purpose
To quantify changes in radiographic measurements of cup abduction angle due to pelvic tilt or obliquity.
Methods
Part A, a retrospective comparison of radiographic cup abduction angle measurements from intraoperative and post-operative radiographs of 23 patients undergoing THA. Part B, a pelvic sawbones model was used to quantify changes in radiographic measurement of cup abduction angle due to known changes in pelvic tilt or obliquity.
Results
Part A, a perfect AP pelvis was obtained in just 30% of intraoperative radiographs. The mean intraoperative cup angle measurement was underestimated by 3.4° compared to post-operative standard radiographs. In Part B, pelvic tilt caused cup abduction angle measurement to decrease on inlet view and increase on outlet view. Pelvic obliquity caused cup abduction angle measurement to decrease on obturator oblique view and increase on iliac oblique view.
Conclusions
A trend exists toward slight underestimation of cup abduction angle measurement using intraoperative radiographs. Pelvic tilt or obliquity alters the measured cup abduction angle in known directions.
Keywords: Total hip arthroplasty, Component malposition, Intraoperative radiograph, Acetabular component inclination angle
1. Introduction
Proper acetabular component positioning is essential to a successful total hip arthroplasty.1 A poorly positioned acetabular component may lead to unfavorable hip kinematics, hip instability, and bearing surface accelerated wear rates.2–5 To accurately measure acetabular component version a CT scan is currently the gold standard, however standard radiographs have been validated as an accurate tool to measure acetabular component abduction angle when compared to CT.6 Intraoperative standard portable radiography is one technique to assess component positioning.7 Recently, intraoperative computed radiography (CR) has been utilized as a time-efficient alternative to assess component positioning.8 For both standardized portable X-ray and CR it is assumed that accurate measurement of component positioning requires perfect AP pelvis imaging without pelvic obliquity or tilt.
We are unaware of any reports in the English language literature that report the accuracy of intraoperative imaging to obtain a perfect AP pelvic image. Furthermore, to our knowledge no study has determined how radiographic measurements of acetabular component positioning are sensitive to deviations from an ideal AP pelvic image on either computed radiography or standard radiographs.
This two-part study aims to determine the following: First, what is the accuracy of intraoperative CR imaging in the lateral decubitus position to obtain a perfect AP image compared to post-operative standard supine images? Second, are acetabular component abduction angle measurements as measured on intraoperative CR images consistent with measurements on post-operative standard radiographs? Finally, to what degree does a less than perfect AP pelvic image due to alterations in patient positioning change the radiographic measurements of the acetabular component abduction angle?
2. Materials and methods
This two-part study utilizes radiographs of both in-vivo acetabular components and radiographs of an acetabular component in a pelvic model to determine how measurements of acetabular component abduction angles are affected by changes in pelvic positioning or incident beam trajectory.
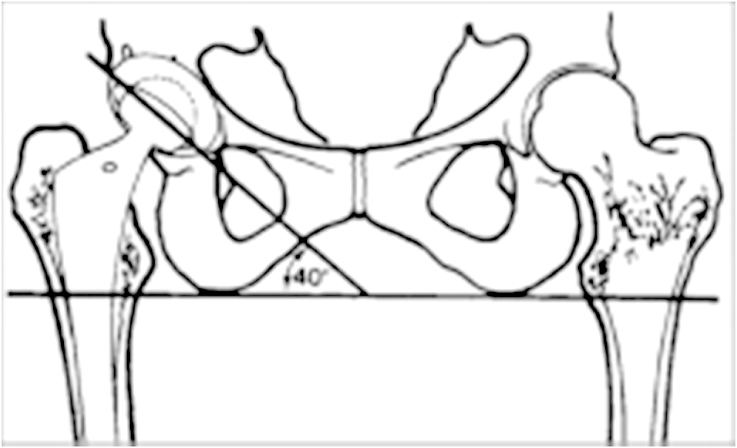
For both parts of this study a “perfect” AP pelvic image was defined by a significant lack of pelvic obliquity or tilt (Fig. 1). Pelvic obliquity was considered “perfect” if the obturator foramina were symmetric and imperfect if the obturator foramina were asymmetric. Likewise, tilt was considered “perfect” if the distance from the tip of the coccyx to the superior aspect of the symphysis pubis was less than 3 cm and imperfect if the coccyx overlapped the symphysis pubis or the distance was larger than 3 cm.9
Fig. 1.

An example of an AP pelvis image without rotation or tilt. The obturator foramina are symmetric and the distance from the tip of the coccyx to the superior aspect of the symphysis pubis is less than 3 cm without overlap.
2.1. Part A
After IRB approval was obtained, a retrospective analysis was performed utilizing radiographic measurements of acetabular component abduction angles from twenty-three consecutive primary THAs in 23 patients for a diagnosis of primary osteoarthritis. Pelvic radiographs of intraoperative, immediate post-operative, and 3-month office visit were reviewed for each patient. Low anteroposterior pelvis digital images were obtained during surgery using portable computed radiography (CR) technology (RadLink Redondo Beach, CA) with the patient in the lateral decubitus position. Immediately post-operative standard radiographs were obtained with the patient supine in the post-anesthesia care unit (PACU), and again in the supine position in the office at a 3-month postoperative visit. First, all films were reviewed to determine the percentage of films that were truly “perfect AP pelvis” images as defined above. If the images were not perfect AP pelvis images then the image was categorized based on the direction of tilt or obliquity (inlet view, obturator view, iliac oblique, obturator oblique). The rates of perfect AP pelvis images obtained were compared for both intraoperative images and post-operative images. Secondly, acetabular component abduction angles were measured on all films by determining the angle between the face of the acetabular component and the intra-ischial line (Fig. 2). For each patient the trends in cup abduction angle were statistically compared over time using a one-way repeated measures analysis of variance (RMANOVA) with Time (3 levels) as the within-subjects factor. Contrasts were used to compare the mean angle at various times. Statistical software: SAS version 9.2 (Cary, North Carolina).
Fig. 2.
Acetabular component abduction angle was measured by determining the angle between the face of the acetabular component and the intra-ischial line.
2.2. Part B
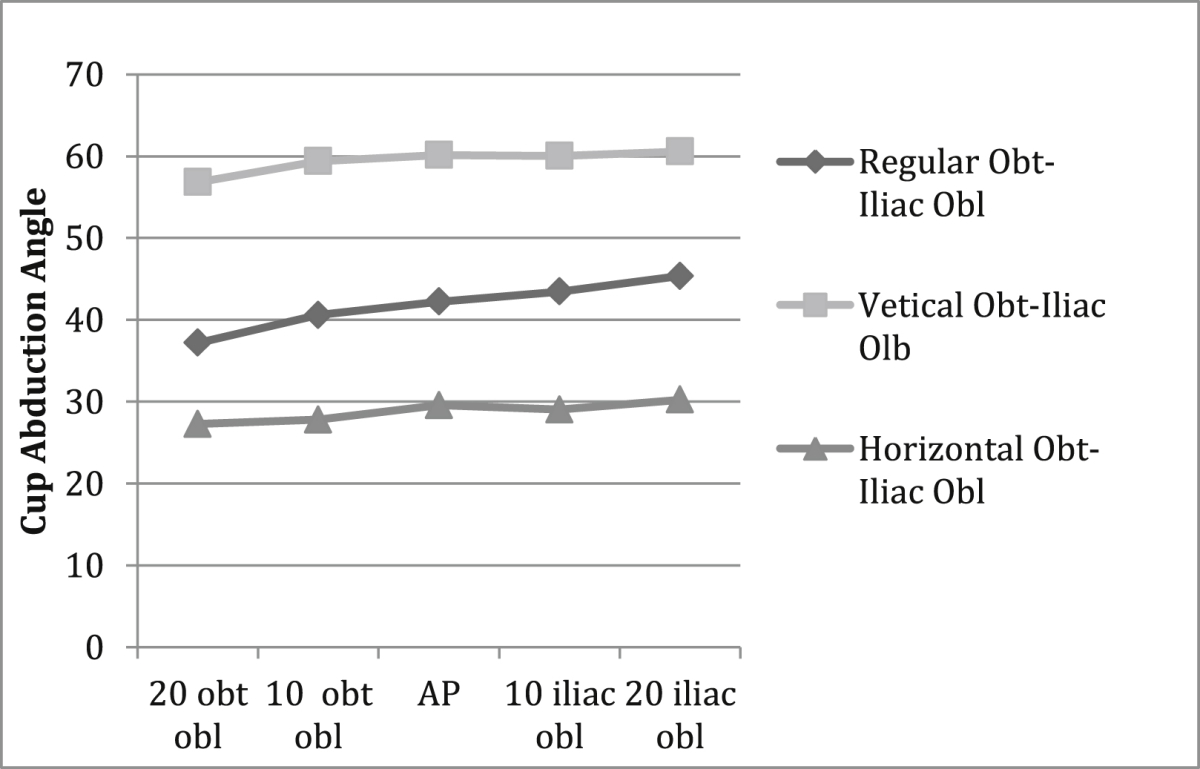
A saw-bones pelvic model was reamed and fitted for a press-fit acetabular component (Zimmer, Warsaw IN). The component was placed in 15 of anteversion and abducted. A perfect AP image of the pelvic model was obtained and the acetabular component abduction angle was measured on the image using the same technique as in phase 1. Subsequent images were taken after the pelvic model was repositioned in multiple known degrees of deviation away from the perfect AP position, including- 10° and 20° inlet, 10° and 20° outlet, 10° and 20° obturator oblique, and 10° and 20° iliac oblique. Acetabular component abduction angles were measured, as in phase 1, for each change in position (Fig. 3). Correlations between cup angle measurements and pelvic orientation were then made. This exercise was performed for three different starting cup abduction angles as measured on the initial perfect AP image in order to replicate a neutral cup position (42°), a more horizontal cup position (29°), and a more vertical cup position (60°). The anteversion of 15° was unchanged for each of these starting cup angles.
Fig. 3.
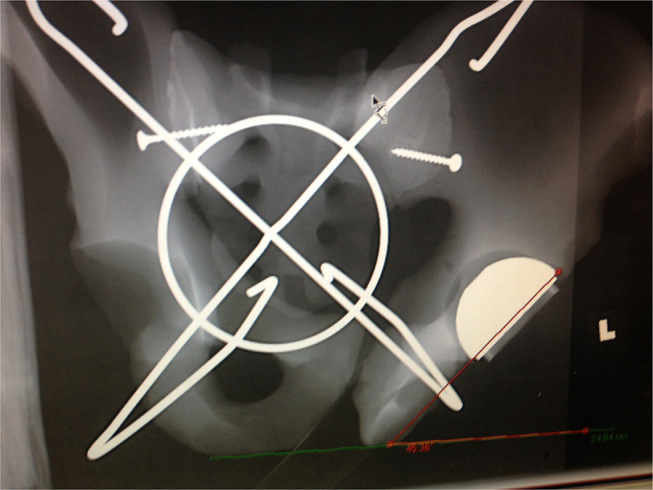
Sawbones pelvic cup model with cup abduction angle initially measured to be 42° on a perfect AP image. While maintaining the incident beam trajectory stationary, the pelvic model was rotated 20° to create a 20° iliac oblique image (Fig. 3). The cup angle was re-measured to be 46.36°.
3. Results
3.1. Part A
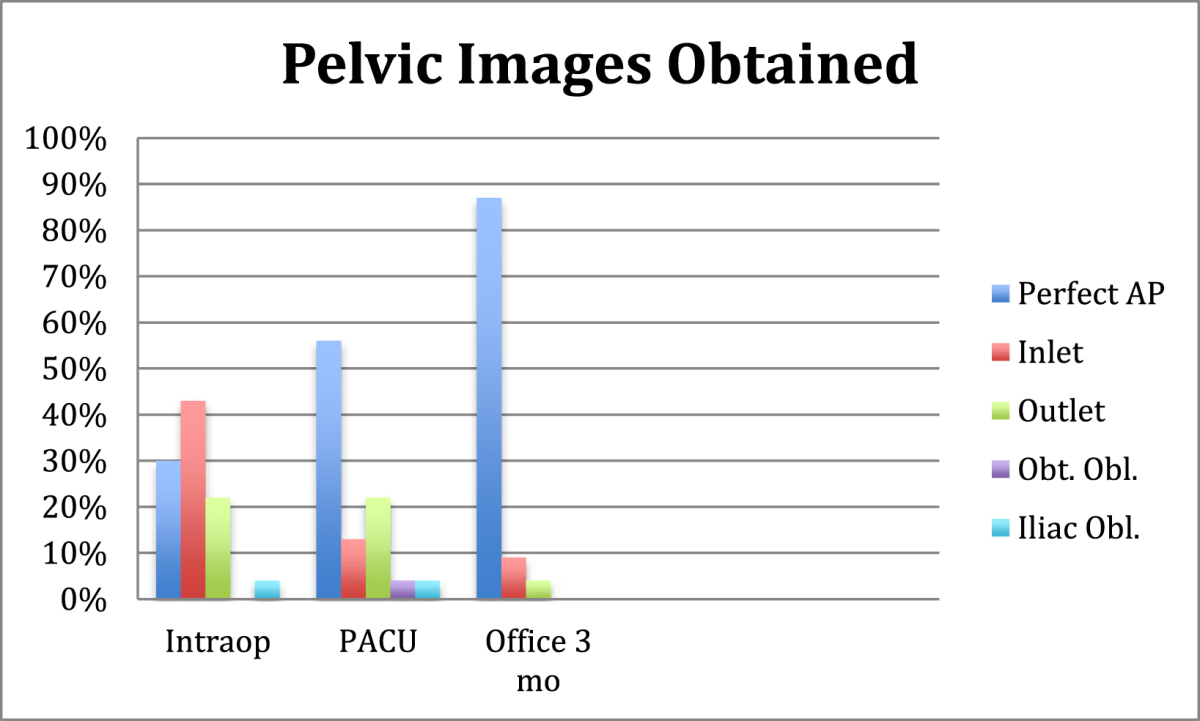
All intraoperative, immediate post-op PACU, and 3 months office visit images were reviewed to quantify the percentage of images deemed as perfect AP pelvis images. Imperfect pelvic X-rays were more commonly seen on intraoperative CR images than in portable X-rays obtained in the PACU or at 3-month office visit images. For the intraoperative CR images the most common images was an inlet view 43% (10/23), followed by a perfect AP image obtained in 30% (7/23), and an outlet view was seen in 22% (5/23), while just 1 image was deemed to have pelvic obliquity 4% (1/23). In comparison, perfect AP pelvic X-rays were more commonly attained in the PACU and 3-month office visit X-rays. A perfect AP pelvis was obtained in 56% (13/23) of PACU images and 87% (20/23) of 3-month office visit images (Table 1).
Table 1.
Perfect AP pelvis image was obtained only 30% of the time intraoperatively in the lateral decubitus position compared to 57% and 87% in the supine position immediate post-op and at 3 month visit.
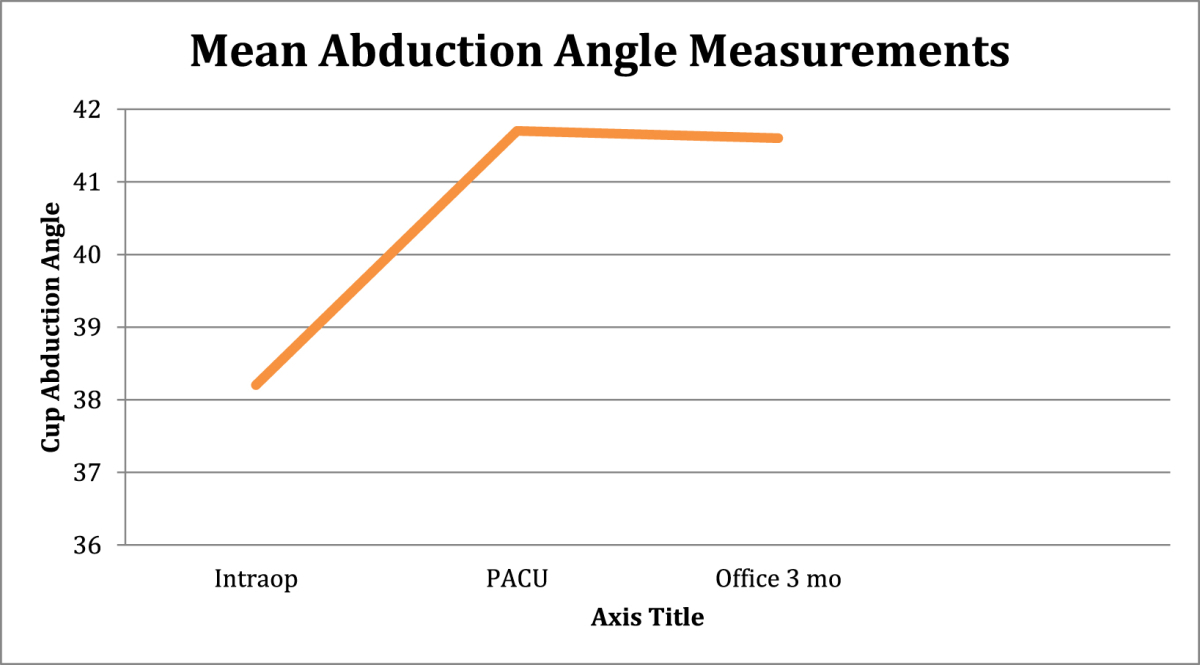
Acetabular component abduction angles were then measured on all films and compared. The mean intraoperative cup angle of 38.2° (R 29°–55°) significantly increased (p < .0001) to 41.7° (R31°–55°) in the PACU and to 41.6° (R 30°–55°) in the office. The mean variance between intraoperative CR cup abduction angle measurements to PACU portable X-rays was 3.4° (Range −3° to +10°). Three angles decreased, 3 remained unchanged, and 17 increased between intra-op and PACU images. The mean variance of cup abduction angle between intraoperative CR images to 3 month office visit portable X-rays was 3.4° degrees (R −3° to +9°). Only 1 angle decreased, 4 remained unchanged, and 18 increased between intra-op and 3 months post-op images. There was no difference in measured cup abduction angle measured on portable X-rays obtained in the PACU and during the 3-month office visit (Table 2). No study patient reported any post surgical events such as hip or pelvic trauma or dislocation event that could have been responsible for changes seen in acetabular component position measurements.
Table 2.
Mean abduction angle measurements of 23 patients including intraoperative lateral decubitus, immediate post-operative supine and 3 month office supine images showed a trend towards intraoperative underestimation of cup abduction angle measurement compared to post-operative angle measurements.
3.2. Part B
Pelvic model cups with initial abduction angles of 42.22° (regular) and 29.57° (horizontal) on standard AP images were measured to be slightly lower when the pelvic model was positioned in 10° and 20° inlet views (−1.05°to −0.72°and −0.24° to −0.06°, respectively). The initial more vertical orientated cup (60.14°) on standard AP was measured to be slightly overestimated on 10°, 20° inlet views (+1.28° to +1.42°, respectively). Outlet views of 10°, 20° overestimated the abduction angle of the neutral cup by +0.58° to +3.96°, and the horizontal cup by +0.12° to +2°, and the vertical cup by +2.73° to +5.58° (Table 3). Obturator Oblique views of 10°, 20° degrees underestimated the abduction angle of the neutral cup by −1.63° to −5.01°, the horizontal cup by −1.75° to −2.29°, and the vertical cup by −0.74° to −3.31°. Iliac oblique views of 10°, 20° changed the neutral cup measurement by +1.24° to +3.14°, the horizontal cup by −0.52° to +0.68°, and the vertical cup by + 0.1° to +0.45° (Table 4).
Table 3.
Compared to a perfect AP image, the inlet views tend to slightly underestimate cup abduction angle whereas outlet views tend to overestimated cup abduction angles. These trends were consistent for both regular cup position (42°) and the more horizontal cup position (29°). The more vertical cup (60°) actually appeared underestimated with both inlet and outlet views.
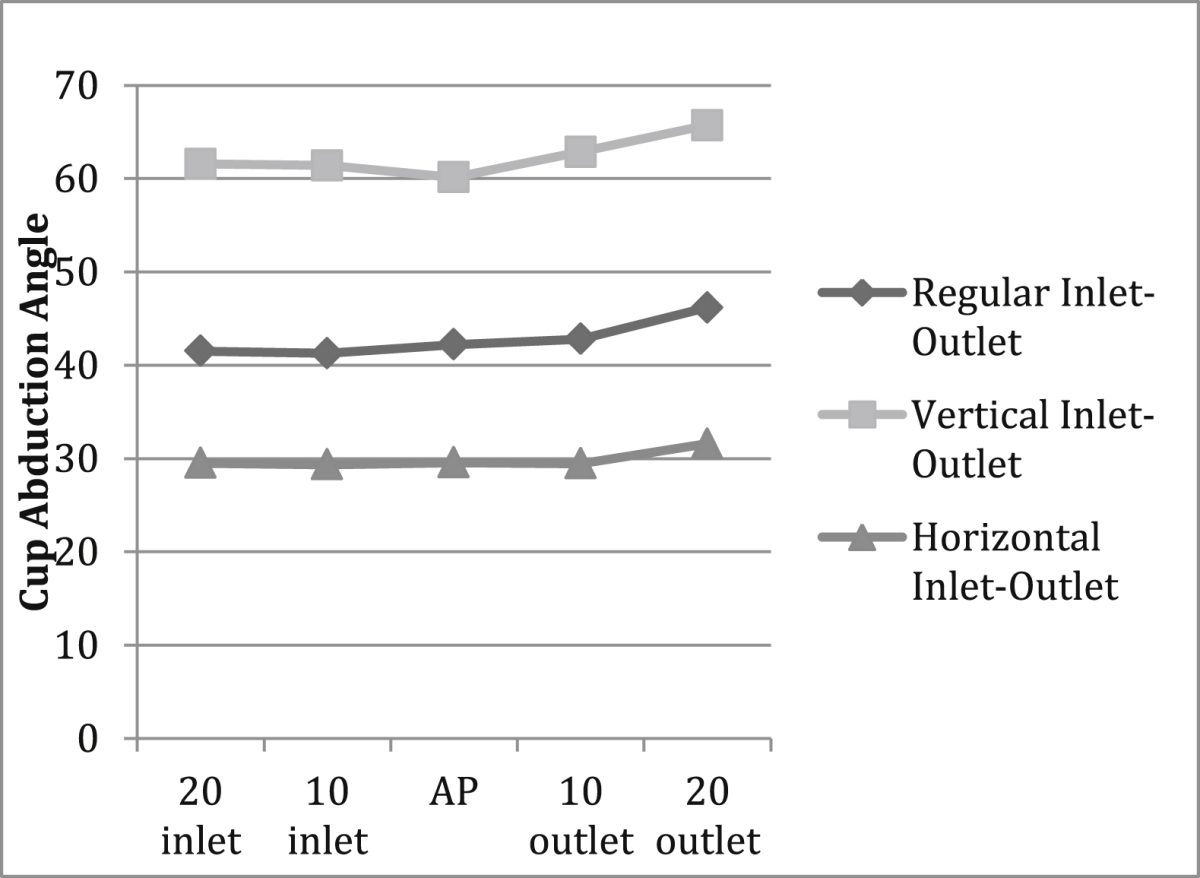
Table 4.
Compared to a perfect AP image, the obturator oblique views underestimated cup abduction angle measurements whereas iliac oblique images overestimated cup abduction angle measurements. These trends were consisted with acetabular components in regular (42°), horizontal (29°), or vertical (60°) position.
4. Discussion
Consistently accurate acetabular component positioning is crucial to successful THA.1–5 A surgeon's ability to recognize intraoperative acetabular component malposition may not be as accurate as once believed. In a study of fifty consecutive THAs evaluating a surgeon's ability to accurately predict the acetabular component abduction angle using intraoperative alignment guides and anatomic landmarks the surgeon was outside of the desired zone 21/50 times with an average error of 5° (range 0–20°) when compared to standard postoperative X-ray measurements.10 Intraoperative radiographs during total hip arthroplasty can provide the surgeon with important information regarding component positioning. With this information surgeons can confirm proper component position, or when necessary make adjustments to correct component mal-positioning and reduce outliers. The two most popular methods of obtaining intraoperative radiographs are standard portable radiographs or computed radiography. Standard portable radiographs may require a potentially lengthy processing time that can delay surgical progression and prolong anesthesia. Intraoperative computed radiography provides rapid image processing in the operating room that avoids surgical delay. Regardless of radiographic imaging method used, the goal is to obtain a perfect AP image of the pelvis to accurately measure acetabular component position. If the pelvis imaged has obliquity or pelvic tilt due to either patient mal-positioning or improper incident beam trajectory then radiographic measurements of the acetabular component abduction angle may be inaccurate or misleading. Hayakawa et al compared acetabular cup abduction angle measurements from intraoperative radiographs in lateral decubitus position to postoperative supine position and noted a mean 5.3° difference in measurement in one hundred consecutive total hip arthroplasties.11 The authors postulated that the difference in cup abduction measurement was due to difference in patient positioning while obtaining the radiographs.11 To our knowledge this series is the first to report the accuracy of intraoperative pelvic images to obtain a perfect AP image and to quantify how radiographic measurements of acetabular component abduction angle are sensitive to deviations from an ideal AP pelvis image.
The clinical results from Part A demonstrate that a perfect AP pelvis image was more difficult to obtain intraoperatively with the patient in the lateral decubitus position than compared to post-operative supine images in the PACU or office visit. A perfect AP image was obtained in just 30% of intraoperative radiographs compared with 56% of PACU films and 87% of office visit films. The most common mal-positioned intraoperative image obtained in the clinical series was an inlet view (43%) followed by an outlet view (22%). Pelvic obliquity was found in just one patient (4%). Overall there was a trend of underestimation of the acetabular component abduction angle on the intraoperative images by 3.4° compared to the post-operative images however the range varied (−3 to +9°).
Part B attempted to quantify how pelvic obliquity or tilt would alter radiographic measurements of acetabular component abduction angle. Pelvic tilt, including inlet and outlet views affected abduction angle measurements. An inlet view was shown to slightly underestimate the true cup abduction angle measurement as compared with a true AP however this trend was not uniform for all starting cup angles. When beginning with a neutral cup position (42°) or a more horizontal cup position (29°) then the inlet view slightly underestimated (less than or equal to 1°) the true abduction angle, however when beginning with a more vertical cup position (60) an inlet view actually slightly overestimated the abduction angle (+1.42°). A pelvic outlet view uniformly overestimated the cup abduction angle. This overestimation was more severe (+5.58°) with a more vertically placed cup (60°) than with a horizontally (29°) placed cup (+2°). Similarly pelvic obliquity, including obturator oblique and iliac oblique images uniformly affected abduction angle measurements regardless of starting cup position, however the changes were most dramatic in the neutral (42°) starting cup position compared with the vertical (60) or horizontal (29) starting cups. Obturator oblique images underestimated the abduction angle of the neutral cup by up to 5°, and the horizontal and vertical cup were underestimated by 2.3° and 3.3° respectively. Iliac oblique images uniformly overestimated the abduction angle, more severely in the neutral cup (+3.3°) compared to the horizontal (+0.68) and vertical cup positions (+0.45).
Limitations of this study must be acknowledged. First, radiographic measurements of abduction angles are subject to intra-observer and inter-observer variability. This variability may be solely responsible for the differences in abduction angles seen for each change in pelvic orientation. During this study the same investigator made all radiographic measurements of abduction angles. Second, the saw-bones model analysis did not include evaluation of combined pelvic obliquity and tilt. For example, no evaluation was performed for a combined 10° inlet +10° iliac oblique view. Finally, the analysis of acetabular component positioning was isolated to changes in abduction angle measurements and did not include changes to acetabular component anteversion. Furthermore, changes in acetabular component anteversion were not evaluated as a variable that may affect radiographic measurement of abduction angle. Throughout each saw-bones pelvic image the anteversion was unchanged at 15°. For the senior author, intraoperative assessment of acetabular component anteversion is made clinically and adjusted based on hip stability and not routinely assessed radiographically.
In this study, intraoperative images in the lateral decubitus position commonly resulted in a less than perfect AP pelvic image, most commonly due to pelvic tilt. On average, abduction angles were underestimated on intraoperative images obtained in lateral decubitus position as compared to immediate post-op and 3-month post-op supine images. Pelvic model analysis verified that the radiographic measurement of an acetabular component abduction angle is sensitive to deviations from a perfect AP pelvis image. The knowledge of the trends presented in this study, along with an acknowledgement of the study limitations, may allow the hip arthroplasty surgeon to make a more educated assessment of acetabular component position when evaluating a less than perfect AP pelvic image.
Conflicts of interest
Chris Mellano has no conflicts of interest.
Andrew Spitzer has the following conflicts of interest to disclose:
-
1
Royalties from Depuy
-
2
Speakers Bureau/ Paid Presentations for Genzyme Sanofi Biosurgical
-
3
Paid consulant for Genzyme Sanofi Biosurgical
-
4Research Support from:
-
1Genzyme Sanofi
-
2Baxter
-
3Depuy
-
1
References
- 1.Daines B.K., Dennis D.A. The importance of acetabular component position in total hiparthroplasty. Orthop Clin North Am. 2012 Nov;43:e23–34. doi: 10.1016/j.ocl.2012.08.002. [DOI] [PubMed] [Google Scholar]
- 2.Biedermann R., Tonin A., Krismer M., Rachbauer F., Eibl G., Stöckl B. Reducing the risk of dislocation after total hip arthroplasty: the effect of orientation of the acetabular component. J Bone Jt Surg Br. 2005 Jun;87:762–769. doi: 10.1302/0301-620X.87B6.14745. [DOI] [PubMed] [Google Scholar]
- 3.Wan Z., Boutary M., Dorr L.D. The influence of acetabular component position on wear in total hip arthroplasty. J Arthroplast. 2008 Jan;23:51–56. doi: 10.1016/j.arth.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 4.Del Schutte H., Jr., Lipman A.J., Bannar S.M., Livermore J.T., Ilstrup D., Morrey B.F. Effects of acetabular abduction on cup wear rates in total hip arthroplasty. J Arthroplast. 1998 Sep;13:621–626. doi: 10.1016/s0883-5403(98)80003-x. [DOI] [PubMed] [Google Scholar]
- 5.Kennedy J.G., Rogers W.B., Soffe K.E., Sullivan R.J., Griffen D.G., Sheehan L.J. Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear, and component migration. J Arthroplast. 1998;13:530–534. doi: 10.1016/s0883-5403(98)90052-3. [DOI] [PubMed] [Google Scholar]
- 6.Kalteis T., Handel M., Herold T., Perlick L., Paetzel C., Grifka J. Position of the acetablar cup- accuracy of radiographic calculation compared to CT-based measurement. Euro J Rad. 2006 May;58:294–300. doi: 10.1016/j.ejrad.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 7.Gross T.P., Liu F., Webb L. Intraoperative radiographs for placing acetabular components in hip resurfacing arthroplasty. Clin Orthop Relat Res. 2011 Jun;469:1554–1559. doi: 10.1007/s11999-010-1701-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Penenberg B.L., Riley M.E., Woehnl A. Intra-operative Digital Radiography in Total Hip Arthroplasty. Bone Joint J. 2013;95-B(Supp 28):58. [Google Scholar]
- 9.Botrager K., Lampignano J. 6th ed. Elsevier Mosby; St. Louis, MO: 2005. Radiographic Positioning and Related Anatomy; p. 275. [Google Scholar]
- 10.Hassan Douglas M., Johnston Geoffrey H.F., Dust William N.C., Watson Glen, Dolovich Allan T. Accuracy of intraoperative assessment of acetabular prosthesis placement. J Arthroplast. 1998 Jan;13:80–84. doi: 10.1016/s0883-5403(98)90079-1. [DOI] [PubMed] [Google Scholar]
- 11.Hayakawa K., Minoda Y., Aihara M., Sakawa A., Ohzono K., Tada K. Acetabular component orientation in intra-and postoperative positions in total hip arthroplasty. Orthop Trauma Surg. 2009 Sep;129:1151–1156. doi: 10.1007/s00402-008-0638-2. [DOI] [PubMed] [Google Scholar]