Abstract
Background
Contralateral C7 (CC7) transfer has been used for treating traumatic brachial plexus injury. However, the effectiveness of CC7 transfer remains a subject of debate. We performed a systematic review to study the overall outcomes of CC7 transfer to different recipient nerves in traumatic brachial plexus injuries.
Methods
A literature search was conducted using PubMed and EMBASE databases to identify original articles related to CC7 transfer for traumatic brachial plexus injury. The data extracted were study/ patient characteristics, and objective outcomes of CC7 transfer to the recipient nerves. We normalized modifications of MRC and other outcome measures into an MRC-based outcome scale for comparisons.
Results
Thirty-nine studies were identified. The outcomes were categorized based on the three major recipient nerves: median, musculocutaneous, and radial/triceps nerves. Regarding overall functional recovery, 11% of patients achieved MRC grade M4 wrist flexion and 38% achieved M3. Grade M4 finger flexion was achieved by 7% of patients whereas 36% achieved M3. Finally, 56% of patients achieved ≥S3 sensory recovery in the median nerve territories. In the musculocutaneous nerve group, 38% of patients regained elbow flexor strength to M4 and 37% regained to M3. In the radial/triceps nerve group, 25% regained elbow or wrist extension strength to an MRC grade M4 and 25% regained to M3.
Conclusions
Outcome measures in the included studies were not consistently reported to uncover true patient-related benefits from the CC7 transfer. Reliable and validated outcome instruments should be applied to critically evaluate patients undergoing CC7 transfer.
Keywords: Traumatic Brachial Plexus Palsy, Contralateral C7 transfer
INTRODUCTION
Traumatic brachial plexus injuries are devastating, causing paralysis and loss of sensation in the affected limb. Nerve reconstruction consists of nerve transfer and nerve repair.1, 2 In cases of total brachial plexus avulsion injuries when proximal nerves are not available for repair, nerve transfer is suggested to restore useful limb functions.3 However, even with advanced microsurgery techniques, treatment of these injuries remains challenging.
Contralateral C7 (CC7) transfer was first introduced by Gu in 1986 to treat total brachial plexus avulsion injuries when donor nerves are in short supply.4 In this surgical technique the whole or partial seventh cervical nerve on the uninjured side is transferred to neurotize the injured nerve on the injured side using nerve graft. Theoretically, C7-innervated muscles are cross-innervated by C6 and C8, with C5 and T1 contributing partially.5 Therefore, the donor-site limb would most likely maintain satisfactory motor functions after C7 is harvested. The major advantage of CC7 transfer is that C7 nerve contains more myelinated nerve fibers than other available donor nerves, which can provide adequate power for neurotization.6 On the other hand, the noticeable disadvantages of CC7 transfer are long distance over which nerve must regenerate and potential donor-site deficits.
CC7 transfer has been widely used for treating brachial plexus injuries, especially for total brachial plexus avulsion injury. However, current literature reports different results, and the effectiveness of CC7 transfer remains controversial. Some studies presented optimistic results and suggested CC7 transfer as an acceptable and desired treatment for total brachial plexus avulsion injury.7, 8 Others reported unsatisfying outcomes and believed this technique was unreliable.9, 10 High levels of evidence data may be difficult to obtain for rare conditions when clinical trials are ethically not possible and prospective outcomes studies may take years to obtain sufficient number of cases. Evidence may be collected via an ambitious multicenter study leveraging participation of high volume centers around the world, but studies such as this are costly and logistically difficult. Systematic review is a research method that can pool the highest level of evidence by scientifically collecting and analyzing relevant data from the conflicting studies.11 Moreover, systematic review is the only possible method to quantitatively obtain the best evidence on the clinical question if a randomized controlled trial is not available.12
In this systematic review, we will focus on the overall outcomes of CC7 transfer to different recipient nerves. We strive to provide the best evidence on this controversial procedure, and then to help guide clinical decision-making and counsel patients on the use of this procedure for treatment of traumatic brachial plexus injury.
MATERIALS AND METHODS
Literature Search
Following the PRISMA guideline13, we performed a systematic search of literature from January 1986 to April 2014 using PubMed and EMBASE databases to identify original articles related to CC7 transfer for traumatic brachial plexus injury. We searched with the following terms: “C7” or “C-7” or “seventh cervical nerve” and “brachial plexus” in abstract and title. After removing duplicates, two reviewers (G.Y. and K. W. C. C) who were trained in systematic review techniques screened the titles and abstracts according to the predetermined inclusion criteria and exclusion criteria. Studies in which content was unclear based on a review of the abstracts underwent the full-text review.
Inclusion and Exclusion Criteria
Inclusion criteria are indicated in Table 1. We excluded studies from review if they met any of the following exclusion criteria: (1) review articles, (2) without CC7 transfer to nerve report, (3) CC7 transfer for neonatal brachial plexus injuries, (4) surgical technique without primary outcome report, (5) electrophysiological study or anatomical study without outcome report, (6) data duplication from the same author, (7) lacking extractable data in the study.
Table 1.
Inclusion criteria
| Literature style |
| Original article |
| Human subjects |
| Published from Jan 1, 1986 to April 1, 2014 |
| Treatment option |
| Contralateral C 7 transfer to the injured nerves for treating traumatic brachial plexus injury |
| Report of objective functional outcomes (at least 1 of following) |
| Recipient nerves innerved motor strength evaluation |
| Recipient nerves sensory recovery evaluation |
Data Extraction and Analysis
Study patient demographic data and descriptive statistics included study published year, location, number of patients, gender, age, injury type, pre-operative period (interval between injury and surgery) and follow-up period. Although most of the available data were from case series and case reports with limited samples, we included the highest level of evidence possible. For articles presenting individual patient information tables, we collected the data and measured the pooled estimates of patients who met our inclusion criteria. If the individual patient demographic information was not available, we used the reported overall mean value. We also extracted the objective outcomes of CC7 transfer to the injured nerve, including motor and sensory functions with measurement scale at the final follow-up visit.
In this systematic review, we would like to study the overall CC7 transfer outcome as well as the outcomes of various recipient nerves (median, musculocutaneous, radial/triceps and other nerves). After reviewing the outcome measures reported in the literature, we found that the Medical Research Council (MRC) scale was used for reporting most of the median nerve, Musculocutaneous (MC) nerve, and radial/triceps nerve outcomes. However, results in other nerves were difficult to normalize because of variability in reporting outcome measures. Therefore, we normalized modifications of MRC and others into an MRC-based outcome scale for median nerve, MC nerve, and radial/triceps nerve (Table 2). For other recipient nerves, we reported study characteristics and patient demographic information.
Table 2.
Muscle and sensory function grading scales
| Grade System and Measurement |
Study | Range and Definition |
|---|---|---|
| Motor function | ||
| MRC £ | M0–M5 | |
| M0, no contraction; M1, flick or trace of contraction; M2, active movement with gravity eliminated; M3, active movement against gravity; M4, active movement against gravity and resistance; M5, normal strength. | ||
| Modified MRC | M0–M5 | |
| Chen 200730, Lin 201137 | M0, no contraction; M1, flick or trace of contraction; M2, active movement with gravity eliminated; M2+, active movement partially against gravity (≥ one half range); M3, active movement against gravity; M4, active movement against gravity and resistance; M5, normal strength. For M2+, we assign grade M2 in MRC; for other grades, we assign in corresponding grade in MRC. |
|
| Sammer 201210 | M0, no contraction; M1, palpable or visible contraction; M2, full range of motion with gravity eliminated; M3, full range of motion against gravity; M4, full range of motion against resistance but with decreased strength; M5, normal. We assign the reported grades to corresponding grades in MRC. |
|
| Terzis 200919, Terzis 201241, Wang 201346 | MRC expanded further with intermediate grade of + and − (e.g. M2, M2+, M3−, M3). Poor, M0 to M2; Fair, M2+ to M3; Good, M3+ or M4 −; Excellent, M4 to M5−. For poor, we assign grade M2 in MRC; fair, M3; good and excellent, M4. |
|
| Sunderland’s Muscle Power Test | M0–M5 | |
| Waikakul 199921, Gu 20027 | M0, no palpable or visible contractions and no movement attributable to the muscle; M1, feeble contractions, no voluntary movement; M2, feeble movement but not against resistance or gravity. In this state the muscle may maintain a part in a position into which it has been passively moved; M3, movement against gravity and some resistance. M4, movement against gravity and strong resistance. M5, normal power and range of movement. For M0 to M2, we assign grade <M3 in MRC; M3–M5, we assign the corresponding grades in MRC. |
|
| Functional Primitive Grip | Hierner 200731 | We assign the functional primitive grip to grade M3 in MRC. |
| Sensory function | ||
| MRC | S0–S4 | |
| S0, no sensation; S1, deep pain; S2, superficial pain and some touch; S2+, grade S2 without over-response; S3, grade S2 with some two-point discrimination; S4, normal. | ||
| Highet’s Scale | S0–S4 | |
| El-Gammal 200223, El-Gammal 200324 | S0, no recovery of sensibility in the autonomous zone of the nerve; S1, recovery of deep cutaneous pain sensibility within the autonomous zone of the nerve; S1+, recovery of superficial pain sensibility; S2, recovery of superficial pain and some touch sensibility; S2+, as in S2, but with over-response; S3, recovery of pain and touch sensibility with disappearance of over-response; S3+, as in S3, but location of the stimulus is good and there is imperfect recovery of two-point discrimination; S4, complete recovery. For S0 to S3, we assign < S3 in MRC; S3+ and S4, ≥ S3 in MRC. |
|
| Protective sensibility | Chen 200414, Hattori 200549 | We assign protective sensibility to grade S2in MRC. |
MRC, Medical Research Council
In the median nerve group, we reported the hand motor functional outcomes (wrist flexion, finger flexion) and sensory recovery. Studies reporting hand and grip functions were categorized as finger flexion. Four studies14–17 reported the finger flexor muscles (FDS or FDP) strength as motor outcomes, and we assigned them as finger flexion strength. Likewise, we categorized wrist flexor muscles (FCR, PL, FCU) strength reported into wrist flexion function. There were different areas of sensory recovery reported in the studies, and three studies did not define the sensory recovery area of CC7 transfer to median nerve.14, 18, 19 These areas were combined as the median nerve area (Table 3). In the MC nerve group, biceps muscle power was assigned as elbow flexion for MC nerve outcome (Table 4). In the radial/ triceps nerve group, triceps and wrist extensor muscle power was assigned as elbow or wrist extension power respectively for radial/triceps nerve recovery (Table 5).
Table 3.
Study and patient demographics, CC7 transfer to median nerve§
| Study | Location | N | M | Age, y | Injury Type |
Pre-op Period, mo |
Follow -up, mo |
Motor Measures |
Motor Recovery | Sensory Area |
Sensory Recovery |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wrist Flexion | Finger Flexion | ||||||||||||||||
| M4 | M3 | < M3 | M4 | M3 | < M3 | ≥ S3 | < S3 | ||||||||||
| Gu 199217£ | Shanghai, China | 4 | 3 | 27 | Total BPAI | 11 | 35 | FCR/FDS | 2 | 0 | 1 | 1 | 0 | 3 | 1–3 palmar digits | 3 | 1 |
| Gu 199818 | Shanghai, China | 8 | NA | 26 | Total BPAI | 12 | 41 | WFF | 3 | 2 | 3 | 3 | 2 | 3 | NA | 6 | 2 |
| Waikakul 199921 | Bangkok, Thailand | 96 | 96 | 27 | Total BPAI | 3 | 36 | WF and FF | 0 | 28 | 68 | 0 | 20 | 76 | NA | NA | NA |
| Songcharoen 200122 | Bangkok, Thailand | 21 | 19 | 25 | Total BPAI | 5 | 42 | WFF | 0 | 6 | 15 | 0 | 6 | 15 | Median nerve area | 10 | 11 |
| Ei-Gammal 200223 | Assiut, Egypt | 7 | 7 | 26 | Total BPAI | 4 | 35 | NA | NA | NA | NA | NA | NA | NA | Palm | 0 | 7 |
| Gu 20027 | Shanghai, China | 14 | NA | 26 | Total BPAI | 10 | 24 | WF or FF | NA | NA | NA | NA | NA | NA | Median nerve area | 12 | 2 |
| Ei-Gammal 200324 | Assiut, Egypt | 2 | 2 | 9 | Total BPAI/ Total BPI | 5 | 60 | Hand function | NA | NA | NA | 0 | 0 | 2 | Palm | 0 | 2 |
| Chen 200414 | Shanghai, China | 1 | 1 | 25 | Total BPAI | 11 | 18 | FCR, PL/FDS | 1 | 0 | 0 | 0 | 1 | 0 | NA | 0 | 1 |
| Hattori 200549 | Ogori, Japan | 1 | 0 | 4 | Total BPI | 4 | 49 | NA | NA | NA | NA | NA | NA | NA | Median nerve area | 0 | 1 |
| Sun 200515 | Shanghai, China | 8 | 6 | 28 | Total BPAI | 6 | 21 | FDP | NA | NA | NA | 1 | 4 | 3 | Median nerve area | 4 | 4 |
| Xu 200629 | Shanghai, China | 2 | 2 | 27 | Total BPAI | 7 | 29 | WFF | 0 | 2 | 0 | 0 | 2 | 0 | Median nerve area | 2 | 0 |
| Chen 200730 | Shanghai, China | 3 | NA | 6 | Total BPAI/ Total BPI | 5 | 46 | WFF | 3 | 0 | 0 | 3 | 0 | 0 | Median nerve area | 3 | 0 |
| Hierner 200731 | Leuven, Belgium | 4 | NA | NA | Total BPI | NA | 60 | Primitive grip | NA | NA | NA | 0 | 1 | 3 | NA | NA | NA |
| Terzis 200919 | Norfolk, USA | 29 | NA | 23 | NA | 30 | 73 | WFF | 10 | 8 | 11 | 10 | 8 | 11 | NA | 12 | 17 |
| Zuo 201035 | Shanghai, China | 8 | 8 | 25 | Total BPAI | 5 | 68 | WFF | 4 | 4 | 0 | 4 | 4 | 0 | NA | NA | NA |
| Lin 201137 | Shanghai, China | 10 | 6 | 26 | Total BPAI | 4 | 39 | WFF | 0 | 5 | 5 | 0 | 5 | 5 | Thumb, index and middle finger tips | 7 | 3 |
| Muhetidier 201138 | Urumqi, China | 16 | 16 | 33 | Total BPAI | 6 | 18 | WF and FF | 3 | 7 | 6 | 1 | 6 | 9 | Median nerve area | 11 | 5 |
| Wang 201139 | Shanghai, China | 5 | 5 | 17 | Total BPAI | 9 | 57 | WFF | 0 | 2 | 3 | 0 | 2 | 3 | Median nerve area | NA | NA |
| Chuang 201240 | Taoyuan, Taiwan | 78 | NA | 26 | NA | 4 | 48 | FF | NA | NA | NA | 0 | 39 | 39 | Fingers | NA | NA |
| Hua 201216 | Shanghai, China | 1 | 1 | 30 | Total BPAI | NA | 48 | FCR, FCU, FPL/Digitorum muscles of all 4 fingers | 1 | 0 | 0 | 1 | 0 | 0 | NA | NA | NA |
| Sammer 201210 | Rochester, USA | 15 | 14 | 27 | NA | 5 | 40 | Composite grip | NA | NA | NA | 0 | 0 | 15 | NA | NA | NA |
| Gao 201343 | Shanghai, China | 22 | 20 | 26 | Total BPAI | 5 | 76 | WFF | 0 | 15 | 7 | 0 | 15 | 7 | Median nerve area | 10 | 12 |
| Gao 201344 | Shanghai, China | 51 | 46 | 29 | Total BPAI | NA | 83 | WFF | 0 | 25 | 26 | 0 | 25 | 26 | 1–3 palmar digits | 32 | 19 |
| Hua 201345 | Shanghai, China | 5 | 5 | 25 | Total BPAI | 2 | 71 | WFF | 3 | 2 | 0 | 3 | 2 | 0 | NA | NA | NA |
| Tu 201447 | Tainan, Taiwan | 40 | 36 | 27 | Total BPAI | 4 | 72 | Hook-grip | NA | NA | NA | 5 | 14 | 21 | Hand | 21 | 19 |
N, patient number; M, male; y, year; Pre-op, pre-operative; mo, month; BPAI, brachial plexus avulsion injury; FDS, flexor digitorum superficialis; NA, not available; WFF, wrist and finger flexion; WF, wrist flexor; FF, finger flexor; BPI, brachial plexus injury; FCR, flexor carpi radialis; PL, palmaris longus; FDP, Flexor digitorum profundus; FCU, flexor carpi ulnaris; FPL, flexor pollici slongus.
One patient did not report wrist function.
Table 4.
Study and patient demographics, CC7 transfer to MC nerve§
| Study | Location | N | M | Age, y | Injury Type |
Pre-op Period, mo |
Follow-up, mo |
Motor Measures |
Motor Recovery | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| M4 | M3 | < M3 | |||||||||
| Gu 199217 | Shanghai, China | 3 | 3 | 23 | Total BPAI | 11 | 33 | Biceps | 2 | 0 | 1 |
| Gu 199818 | Shanghai, China | 6 | NA | 26 | Total BPAI | 12 | 41 | Biceps | 2 | 2 | 2 |
| Gu 20027 | Shanghai, China | 10 | NA | 26 | Total BPAI | 10 | 24 | Biceps | 1 | 7 | 2 |
| Beaulieu 200628 | Paris, France | 5 | 5 | 32 | Total BPAI | 4 | 20 | Biceps | 2 | 0 | 3 |
| Chen 200730 | Shanghai, China | 1 | NA | 3 | Total BPAI | 4 | 63 | Biceps | 1 | 0 | 0 |
| Hierner 200731 | Leuven, Belgium | 6 | 5 | NA | Total BPI | 6 | 60 | Elbow flexion | 5 | 1 | 0 |
| Terzis 200919 | Norfolk, USA | 23 | NA | 23 | NA | 30 | 73 | Biceps | 12 | 5 | 6 |
| Beisteiner 201150 | Vienna, Austria | 1 | 1 | 6 | Total BPI | 5 | 78 | Elbow flexion | 1 | 0 | 0 |
| Bertelli 201136 | Santa Catarina, Brazil | 1 | 1 | 20 | Total BPAI | 4 | 20 | Elbow flexion | 0 | 1 | 0 |
| Lin 201137 | Shanghai, China | 10 | 6 | 26 | Total BPAI | 4 | 39 | Biceps | 2 | 4 | 4 |
| Muhetidier 201138 | Urumqi, China | 3 | 3 | 33 | Total BPAI | 6 | 18 | Elbow flexion | 1 | 1 | 1 |
| Chuang 201240 | Taoyuan, Taiwan | 23 | NA | 28 | NA | 4 | 48 | Elbow flexion | 0 | 19 | 4 |
| Gao 201343 | Shanghai, China | 12 | NA | 26 | Total BPAI | 5 | 76 | Elbow flexion | 0 | 8 | 4 |
| Wang 201346 | Beijing, China | 47 | NA | NA | Total BPAI | 4 | 57 | Elbow flexion | 28 | 8 | 11 |
N, patient number; M, male; y, year; Pre-op, pre-operative; mo, month; BPAI, brachial plexus avulsion injury; NA, not available;
Table 5.
Study and patient demographics, CC7 transfer to radial nerve and triceps nerve§
| Recipient Nerve |
Study | Location | N | M | Age, y |
Injury Type |
Pre-op Period, mo |
Follow -up, mo |
Motor Measures |
Motor Recovery (Elbow or wrist extension) |
||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M4 | M3 | < M3 | ||||||||||
| Radial Nerve | ||||||||||||
| Gu 199217 | Shanghai, China | 2 | 1 | 37 | Total BPAI | 11 | 31 | Triceps/ECRL | 1 | 0 | 1 | |
| Gu 199818 | Shanghai, China | 4 | NA | 26 | Total BPAI | 12 | 41 | Triceps | 2 | 0 | 2 | |
| Gu 20027 | Shanghai, China | 6 | NA | 26 | Total BPAI | 10 | 24 | Wrist or finger extension | 2 | 2 | 2 | |
| Hattori 200549 | Ogori, Japan | 1 | 1 | 5 | Total BPI | 5 | 54 | Elbow extension | 0 | 0 | 1 | |
| Terzis 200919£ | Norfolk, USA | 10 | NA | 23 | NA | 30 | 73 | Wrist and finger extension | 2 | 2 | 6 | |
| Muhetidier 201138 | Urumqi, China | 2 | 2 | 33 | Total BPAI | 6 | 18 | Wrist extension | 0 | 1 | 1 | |
| Triceps Nerve | ||||||||||||
| Terzis 200919£ | Norfolk, USA | 21 | NA | 23 | NA | 30 | 73 | Triceps | 7 | 5 | 9 | |
| Terzis 201241 | New York, USA | 20 | NA | 26 | NA | 17 | 56 | Triceps | 5 | 7 | 8 | |
| Gao 201343 | Shanghai, China | 10 | NA | 26 | Total BPAI | 5 | 76 | Elbow extension | 0 | 2 | 8 | |
N, patient number; M, male; y, year; Pre-op, pre-operative; mo, month; BPAI, brachial plexus avulsion injury; ECRL, extensor carpi radialis longus; NA, not available; PD, posterior division.
The study (Terzis 200919) reported two procedures.
We assigned the MRC grade of M3 and S3 as the cut-off point for functional recovery. Motor functions were categorized into MRC grade of M4, M3, and lower than M3. If the primary reported outcomes only stated ≥M3 in the studies, we assigned them as M3. Sensory recoveries were categorized into greater and lower than S3 in the study tables.
Statistical Analysis
The data were categorized based on the recipient nerves: median nerve (Table 3), MC nerve (Table 4), radial/triceps (Table 5), and other nerves (Table 6). Study patient demographic information and descriptive statistics were summarized in Table 7. One-way ANOVA was applied for interval data (percentage of males, mean age, mean pre-op period, and follow-up period). Probability values less than 0.05 were considered statistically significant, and all statistical analyses were performed using SAS statistical software (version 9.2). We also reported the percentages of functional recovery (M4, M3 and/or ≥ S3) for median, MC, and radial/triceps nerves.
Table 6.
Study and patient demographics, CC7 transfer to other nerves§
| Study | Location | N | M | Age, y |
Injury Type |
Pre-op Period, mo |
Follow -up, mo |
Target Nerve | Procedure | Stage | Outcomes |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Gu 199217 | Shanghai, China | 1 | 1 | 27 | Total BPAI | 11 | 35 | Thoracodorsal nerve | CC7 root transfer to thoracodorsal nerve and MC nerve via ulnar nerve graft with ulnar artery and vein | 2 | Latissimus dorsi: M2-1 |
| Gu 199818 | Shanghai, China | 2 | NA | 26 | Total BPAI | 12 | 41 | Thoracodorsal nerve | CC7 transfer to thoracodorsal nerve via ulnar nerve graft | 2 | Latissimus dorsi: M4 in one case |
| Bertelli 199920 | Santa Catarina, Brazil | 1 | 1 | 26 | Partial BPAI | 4 | 24 | Axillary and suprascapular nerves | Motor rootlets of CC7 transfer to axillary and suprascapular nerves via sural nerve graft | 1 | The patient was capable of 120° of active should abduction and hold an 800-g weight at 90°. |
| Gu 20027 | Shanghai, China | 2 | NA | 26 | Total BPAI | 10 | 24 | Thoracodorsal nerve | CC7 transfer to thoracodorsal nerve by using sural nerve graft | 1 | Latissimus dorsi: M4 in one case; M0 in another case |
| Doi 200348 | Ogori, Japan | 1 | 1 | 6 | Total BPI | NA | 24 | Suprascapular nerve | CC7 transfer to suprascapular nerve by using ulnar graft | 1 | Shoulder abduction: 40°; external rotation: 60° |
| Yu 200325 | Shanghai, China | 3 | 3 | 25 | Total BPAI | 6 | 32 | Ulnar nerve | CC7 was coaptated to ulnar nerve after upper arm shortening | 1 | Hand sensation ≥ S3 and FCU ≥ M3 in all cases |
| Bertelli 200426 | Santa Catarina, Brazil | 24 | 23 | 22 | Total BPAI/Partial BPI | 4 | 36 | Suprascapular nerve | Total or partial CC7 motor rootlet transfer to suprascapular nerve by a sural nerve graft | 1 | The mean recovery in shoulder abduction was 90° and 92° in external rotation. |
| Amr 200527 | Cairo, Egypt | 8 | 7 | 27 | Total/Partial BPI/BPAI | 3 | 26 | Roots, trunks, cords or braches | CC7 transfer to roots, trunks, cords or braches by end-to-side, side-to-side grafting | 1 | Different level functional recovery was found in the deltoid and triceps, biceps, pronator teres, FCU, FDP, wrist extensors and extensor digitorum longus. |
| Hattori 200549 | Ogori, Japan | 1 | 1 | 5 | Total BPI | 5 | 54 | Suprascapular nerve | CC7 transfer to suprascapular nerve via free vascularized ulnar nerve graft | 1 | Shoulder abduction: 30°; external rotation: 60° |
| Beaulieu 200628 | Paris, France | 2 | 2 | 25 | Total BPAI | 4 | 20 | Lateral cord | CC7 transfer to lateral cord by using sural nerve graft | 1 | Reinnervated musecle: M2 |
| Chen 200730£ | Shanghai, China | 2 | NA | 2 | Total BPAI/Total BPI | 3 | 23 | Upper trunk | PD or whole CC7 transfer to upper trunk via conventional nerve graft | 1 | One case: Biceps, M4; Median nerve, S3+. Deltoid, M2+; another: Biceps, M4; WFF, M4; Median nerve, S3+. |
| Xu 200832 | Shanghai, China | 8 | 8 | 30 | Total BPAI/Total BPI | 4 | 12 | Upper trunk or lateral and posterior cords | CC7 transfer to the upper trunk or lateral and posterior cords via a prespinal and tetropharyngeal route by using sural nerve graft | 1 | Shoulder abduction and elbow flexion were found in all cases. |
| Terzis 200919£ | Norfolk, USA | 10 | NA | 23 | NA | 30 | 73 | Axillary | Selective CC7 transfer to axillary nerve | 1 | Deltoid: M3+ or M4− in 2 cases; M2+ to M3 in 3 cases; M0 to M2 in 5 cases |
| Feng 201033 | Shanghai, China | 4 | 3 | 26 | Total BPAI | 2 | 32 | Lower trunk or C8-T1 spinal nerves | CC7 repair the lower trunk or the C8-T1 spinal nerves via the subcutaneous tunnel across the anterior surface of the chest and neck | 1 | Digital flexion: M1–M3; carpal flexion: M2–M4; hand sensation S1–S3 in all cases |
| Wang 201034 | Beijing, China | 20 | 16 | 13 | Total BPAI/Total/Partial BPI | 5 | 27 | Lower trunk | CC7 transfer to lower trunk directly through the prespinal route | 1 | Muscle strength of finger flexion: M4, in 18 cases, M2 in 2 cases; thumb flexion: M4 in 10 cases; M3 in 8 cases, M2 in 2 cases; intrinsic muscles M3 in 2 cases |
| Sammer 201210 | Rochester, USA | 13 | 11 | 25 | NA | 5 | 27 | Axillary and/ or suprascapular nerve | Hemi-CC7 transfer to axillary or suprascapular nerve via sural nerve grafts | 1 | Only 3 patients achieved M3 or greater shoulder abduction. |
| Wang 201242 | Beijing, China | 41 | 37 | 29 | Total/Partial BPAI | 3 | 47 | Upper trunk | CC7 transfer to upper trunk or C5/C6 nerve roots via the modified prespinal route | 1 | Muscle strength was graded M4 or M3 for the biceps muscle in 85.4% of patients, for the deltoid muscle in 82.9% of patients, and for the upper parts of pectoral major in 92.7% of patients. |
| Wang 201346 | Beijing, China | 75 | 70 | 28 | Total BPAI | 4 | 57 | Lower trunk | CC7 transfer via the modified prespinal route and direct coaptation with the lower trunk | 1 | Motor function with a grade of M3 or greater was attained in 60% of the patients for elbow flexion, 64% of the patients for finger flexion, 53% of the patients for thumb flexion, and 72% of the patients for wrist flexion. |
N, patient number; M, male; y, year; Pre-op, pre-operative; mo, month; BPAI, brachial plexus avulsion injury; NA, not available; FCU, flexor carpi ulnaris; FDP, Flexor digitorum profundus; BPI, brachial plexus injury; PD, posterior division; WFF, wrist and finger flexion
These outcomes were reported in modified MRC.
Table 7.
Patient demographics summaries§
| Overall | Median Nerve | MC Nerve | Radial/ Triceps Nerve |
Other Nerves € | P-value | |
|---|---|---|---|---|---|---|
| Study N | 39£ | 25 | 14 | 9¥ | 18 | - |
| Patient N | 754‡ | 451 | 151 | 76 | 218 | - |
| Male% (N) | 91% (531/585) | 93% (293/315) | 83% (24/29) | 80% (4/5) | 91% (184/202) | 0.35 |
| Mean age± SD, y | 23±8 | 24±7 | 23±9 | 25±9 | 22±9 | 0.65 |
| Mean pre-op period± SD, mo | 6±5 | 7±6 | 8±7 | 14±10 | 7±7 | 0.05 |
| Mean follow-up period± SD, mo | 43±20 | 48±19 | 46±22 | 50±22 | 34±15 | 0.12 |
N, number; y, year; Pre-op, pre-operative; mo, month.
Other nerves include upper trunk, lower trunk, lateral cord and posterior cord, thoracodorsal nerve, axillary nerve, suprascapular nerve and ulnar nerve.
One study (Terzis 200919) reported 5 procedures; three studies (Gu 199217, Gu 199818, Gu 20027) reported 4 procedures; four studies (Hattori 200549, Chen 200730, Muhetidier 201138, Gao 201343) reported 3 procedures; six studies (Beaulieu 200628, Hierner 200731, Lin 201137, Sammer 201210, Chuang 201240, Wang 201346) reported 2 procedures; thus, there are 39 reference studies.
One study (Terzis 200919) reported 2 procedures; thus, there are 8 reference studies.
There are 56 patients underwent CC7 transfer to 93 target nerves. In addition, 46 patients underwent CC7 transfer to both MC and median nerves, 47 patients underwent CC7 transfer to both MC nerve and lower trunk, 10 patients underwent CC7 transfer to both median and triceps nerves, 1 patient underwent CC7 transfer to both radial and suprascapular nerves, and 1 patient underwent CC7 transfer to both MC and thoracodorsal nerves; thus actually there are 754 patients included in this systematic review.
RESULT
Study and patient demographic characteristics
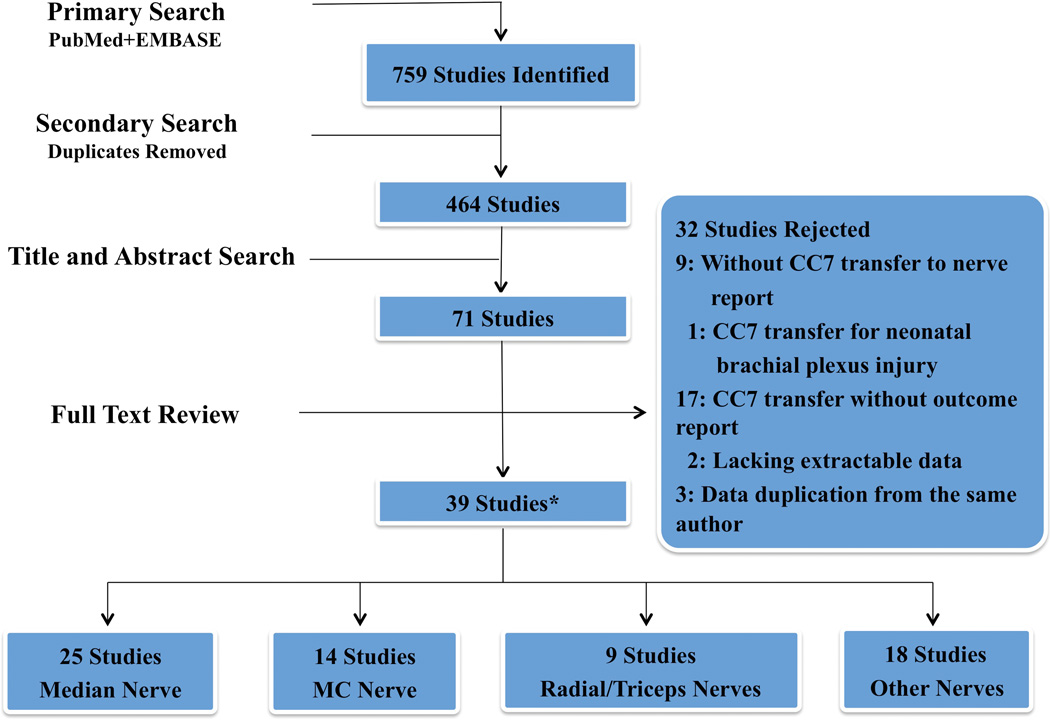
Database search and number of studies retrieved and excluded are presented in Figure 1 and all the included articles are presented in Supplemental Digital Content 1, Appendix I, INSERT LINK. Ultimately, 39 studies met the inclusion and exclusion criteria.7, 10, 14–50 One prospective randomized control trial was identified,47 and all others were retrospective studies. These studies were divided into 4 groups: median nerve group (n=25), MC nerve group (n=14), radial/triceps nerve group (n= 9) and other nerves group (n=18). Fourteen studies reported outcomes of multiple procedures.7, 10, 17–19, 28, 30, 31, 37, 38, 40, 43, 46, 49
Figure 1.
Flow diagram of database search and number of studies retrieved and excluded from review. * See Supplemental Digital content 1, Appendix I, INSERT LINK, for all included articles; 14 studies had multiple procedures and were added more than once for the analysis.
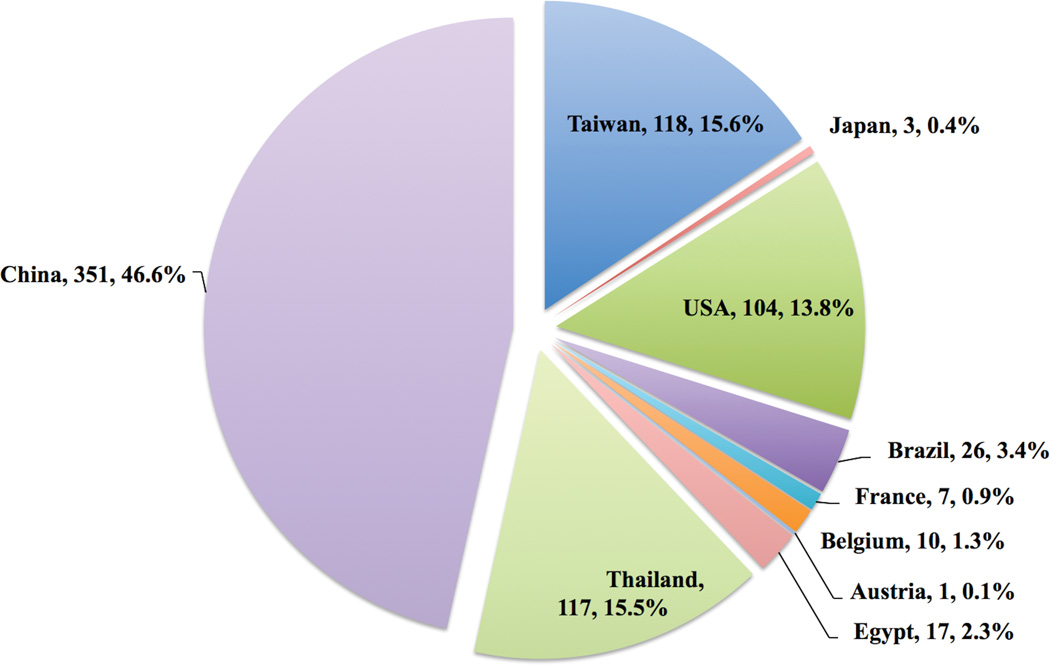
The majority of the studies (n =21) were published in China and account for 54% of studies (Figure 2). A total of 754 patients underwent CC7 transfer for treatment of traumatic brachial plexus injury in this systematic review. Geographic distribution of the patients is presented in Figure 3. The largest series of 96 patients in one study was conducted by Waikakul.21 Gu and his colleagues presented 181 out of 754 patients (24%) in 15 studies,7, 14–18, 29, 30, 32, 33, 35, 39, 43–45 and other surgeons from China reported 170 out of 754 patients (23%) in 6 studies25, 34, 37, 38, 42, 46.
Figure 2.
Geographic distribution of 39 studies in the systematic review (n, patient number)
Figure 3.
Geographic distribution of 754 patients in the systematic review (Location, patient number, %); percentages added up to 99.9% because of rounding.
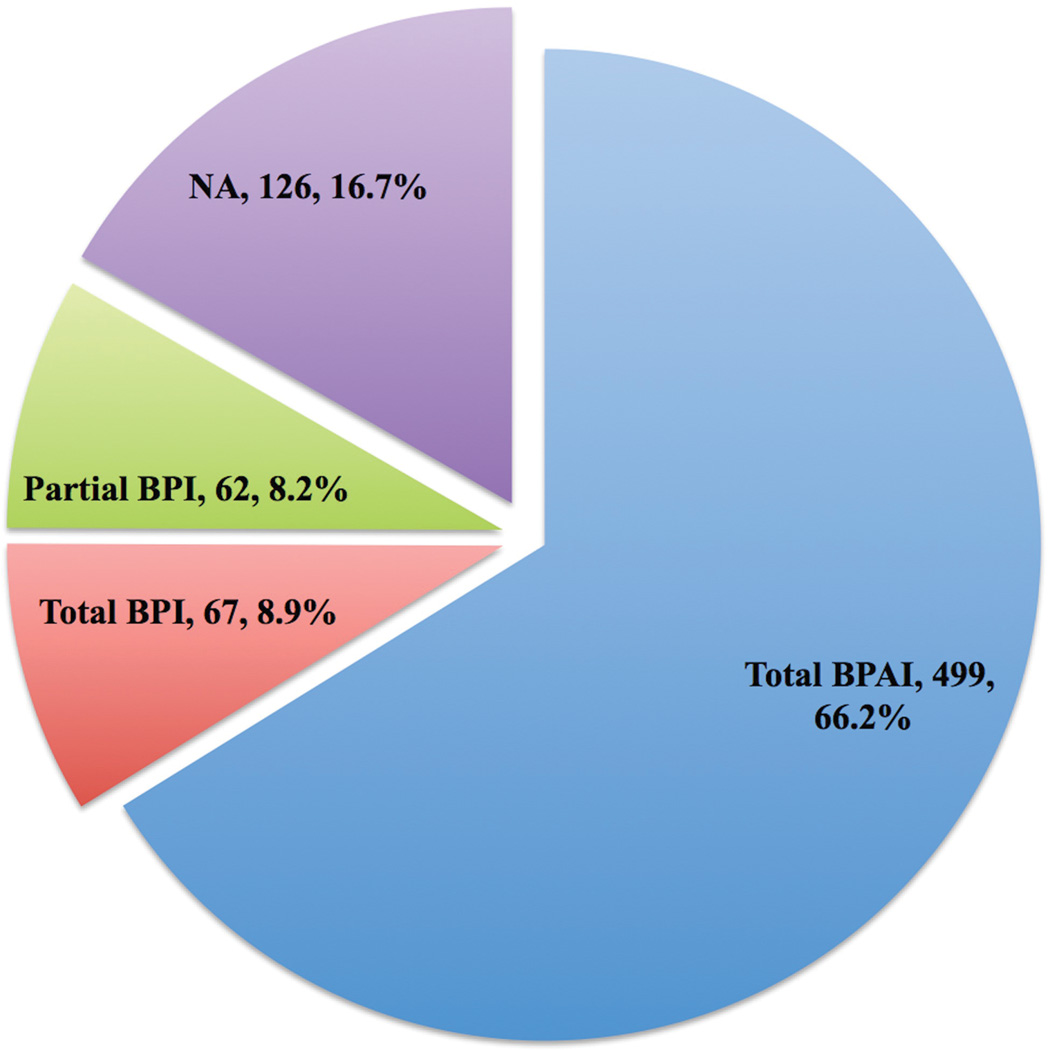
The patients who underwent CC7 transfer had different brachial plexus injury types in the studies (Figure 4). Sixty-six percent of patients (499/754) had total brachial plexus avulsion injuries, and 9% of patients (67/754) had total brachial plexus injuries with mixed root avulsion or rupture injury. Partial brachial plexus injury occurred in 8% of patients (62/754). Three studies mixed total brachial plexus injury with other types of injuries or only described the traumatic brachial plexus injury;10, 40, 41 therefore the specified injury pattern in 17% of patients (126/754) could not be identified. Overall, 91% of patients were male, and mean age was 23 years, mean pre-operative period (interval between injury and surgery) was 6 months, and mean follow-up period was 43 months (Table 7). There were no significant differences in age, pre-operative period, or follow-up period among the four recipient nerve groups.
Figure 4.
Distribution of injury types of 754 patients in the systematic review (Injury type, patient number, %) * BPI, brachial plexus injury; BPAI, brachial plexus avulsion injury.
Median nerve outcomes
In total, 451 patients were treated with CC7 transfer to median nerve to improve wrist and hand functions. Considering the overall functional recovery of those with reported data and without subgroup analysis of various surgical techniques, 30 of 281 patients (11%) achieved an MRC grade of M4 and 106 (38%) achieved M3 in wrist flexion. Thirty-two of 429 (7%) patients achieved M4, and 156 patients (36%) achieved M3 in finger flexion, whereas 133 of 239 patients (56%) achieved ≥S3 sensory recovery in median nerve territories (Table 8).
Table 8.
Outcome summaries of CC7 transfer to median, MC and radial/triceps nerves§
| Study N |
Elbow or Wrist Extension N (%) |
Elbow Flexion N (%) |
Wrist Flexion N (%†) |
Finger Flexion N (%) |
Sensory Recovery N (%) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M4 | M3 | <M3 | M4 | M3 | <M3 | M4 | M3 | <M3 | M4 | M3 | <M3 | ≥S3 | <S3 | ||
| Median Nerve | 25 | - | - | - | - | 30 (11%) | 106 (38%) | 145 (52%) | 32 (7%) | 156 (36%) | 241 (56%) | 133 (56%) | 106 (44%) | ||
| MC Nerve | 14 | - | - | 57 (38%) | 56 (37%) | 38 (25%) | - | - | - | - | - | - | |||
| Radial/Triceps Nerve | 9 | 19 (25%) | 19 (25%) | 38 (50%) | |||||||||||
N, number
Because of rounding, percentages do not equal 100%
MC nerve outcomes
Of the 151 patients who underwent CC7 transfer to the MC nerve for elbow flexion for treatment of brachial plexus injury, 57 patients (38%) regained elbow flexor strength of an MRC grade of M4 and 56 patients (37%) achieved M3, whereas 38 patients (25%) achieved less than a grade of M3 (Table 8).
Radial/triceps nerves outcomes
Seven studies reported the outcomes of CC7 transfer to radial or triceps nerve, and one study reported both radial and triceps nerves outcomes (Table 5). Twenty-five percent of 76 patients regained elbow or wrist extension strength of an MRC of M4 and M3 respectively, and the remaining 50% of patients had less than M3 (Table 8).
Other nerve outcomes
The CC7 nerves were also transferred to other nerves in total 218 cases, including upper trunk,30, 32, 42 lower trunk,33, 34, 46 lateral cord and posterior cord,28, 32 thoracodorsal nerve,7, 17, 18 axillary nerve,10, 19, 20 suprascapular nerve10, 20, 26, 48, 49 and ulnar nerve25. Outcomes of the included patients were quite variable and demonstrated in Table 6.
DISCUSSION
Traumatic injuries to the brachial plexus occurred in slightly more than 1% of adult multitrauma patients in a regional trauma facility in North America.51 Motor vehicle accidents are the most frequent cause of these injuries, especially in developing countries, where motor vehicle is the primary transportation mode.1, 52, 53 Approximately 60% of brachial plexus injuries in the literature are total five roots injuries that can cause flail arm.2 Young men are most likely to sustain these disabling injuries.1, 21, 40 Surgical reconstruction might be challenging when direct nerve repair is not applicable for avulsion injuries and prolonged denervation time causes irreversible atrophy of the muscle fibers, especially in hand muscles.54 In the last decade, nerve transfer has been widely adopted and is considered as the only means of providing motor axons in treatment of total brachial plexus avulsion injuries.2 Theoretically, this procedure can connect the donor nerve closer to the target nerve, which results in the reduction of distance and duration of axonal regrowth.3, 55 Owing to this benefit, spinal accessory nerve,56 intercostal nerve,56, 57 and phrenic nerve58, 59 have been successfully transferred to restore shoulder and elbow functions in brachial plexus injuries. However, the effectiveness of CC7 transfer is unproven.
CC7 was commonly transferred to the median nerve to restore the hand function in patients with brachial plexus injuries. In this review, two thirds of the studies reported the outcomes of CC7 transfer to median nerve, and 60% of the patients underwent this reconstruction procedure. Theoretically, C7 root provides 17,000 to 40,000 myelinated nerve fibers and contains both sensory and motor fibers, which are suitable for median nerve re-innervation.6, 7, 47 Therefore, median nerve is considered as the first choice of the recipient nerve for CC7 transfer.
The motor recoveries of CC7 transfer to median nerve varied dramatically in the studies. In 1998, Gu and his colleagues reported 5 of 8 patients regained grade M3 or greater wrist and finger flexor strength at average of 3 years follow-up period.18 In their latest case series in 2013, they reported wrist and finger flexors recovered to M3 or greater in 25 of 51 patients at a mean of 7 years follow-up period.44 Reinnervation of thenar muscle had been reported in 5 out of 32 patients with total brachial plexus avulsion injury at mean 5 years after CC7 transfer to median nerve.39 However, in a large series with 96 patients underwent anterior part of CC7 transfer to median nerve, only 20% to 30% of all patients regained significant hand function at 3 years follow-up perios.21 In Sammer’s report, none of the 15 patients achieved a functional composite grip at a mean of 40 months postoperatively.10 Our findings indicated less than half of patients achieved an MRC grade of M3 or greater in wrist (11% of M4 and 38% of M3) and finger flexion (7% of M4 and 36% of M3). For sensory recovery, our results indicated more than half of patients (56%) had S3 or greater. Potential confounders that could affect treatment outcome, including patient age, denervation time, and different surgical techniques of CC7 transfer, were not studied in this systematic review.
Anatomy could explain the various motor recovery outcomes. It has been found that adult denervated muscles atrophy and motor end plates lost their restorative ability after 12 to 18 months.60 In CC7 to median nerve transfer, axons must regenerate for over 30 centimeters distance before they reach the target muscles.37 It will take approximately 10 months for axons at a regenerate rate of 1mm/day to reach 30 centimeters, except the time for crossing nerve suture lines. Another difficulty is that although the CC7 have almost twice the number of nerve fibers as median nerve, the numbers of myelinated nerve fibers that grow across the nerve graft are still limited by the nerve graft size and some fibers might not contribute to recovery.
More importantly, even if patients regain wrist and finger flexion strength to grade M3 or M4, whether this provides patients with functional hand usage is questionable. First, finger flexion against gravity, especially in the absence of intrinsic muscles, is not sufficient for basic hand functions.23 Secondly, most patients could not achieve independent active movement of the injured hand without simultaneous activation of the contralateral muscles innervated by the CC7 nerve. Cortical reorganization from contralateral shoulder or elbow motion to ipsilateral hand function is a difficult and time-consuming process. Therefore, simply measuring a patient’s motor function recovery does not represent meaningful recovery of the involved hand.
As for the CC7 transfer to MC nerve outcomes, our data demonstrated that 75% of patients regained elbow flexor strength of M3 and M4. This recovery rate is similar to the phrenic nerve transfer to the MC nerve (mean recovery rate of 78%).58 Regaining elbow flexion is useful for patients to maintain some control over the involved limb, and be able to use their normal contralateral arm for daily activities instead of stabilizing the flail limb.37 On the other hand, elbow and wrist extension functions are not as critical for the patients with total brachial plexus injury; therefore, only a few reports of CC7 transfer to radial or triceps nerve, which contained a small number of patients.7, 17–19, 38, 43, 49 In our study, 66% of the included patients had total brachial plexus avulsion injuries; spontaneous recovery innervated with the other root is very unlikely. The short distance between CC7 and biceps and triceps muscles could possibly contribute to these enhanced recoveries. Another factor may be that their innervated muscles are larger and the atrophy rate is slower.
Additionally, CC7 has been rarely transferred to other nerves using modified techniques. Wang et al. reported CC7 transfer to lower or upper trunks via the prespinal route with motor recovery rates of M3 or greater in the different innervated muscles over 50% out of 116 cases.42, 46 In a case series, 3 cases were treated by shortening the upper arm to perform CC7 coaptation to the ulnar nerve without nerve graft.25 Amr et al. applied CC7 to repair brachial plexus injures by end-to-side or side-to-side grafting neurorrhaphy.27 Although satisfactory results were indicated in these reports, these techniques were immature or unconventional and patients might be unwilling to undergo these procedures.
This review is not without limitations. First, we limited the search in only PubMed and EMBASE databases. Some non-English studies might not be included in these databases and elimination of those studies may reduce the power of this review. Furthermore, most included studies were retrospective uncontrolled studies. The results in this review could also be affected by the inconsistency and variability in outcome reports. We normalized the outcomes by each joint using MRC scale to provide a clearer overview of the outcomes. There might be potential confounders such as patient age, targeted muscles and different CC7 procedures, which are out of the scope of this review. Lastly, there might be publication bias in that studies with positive outcomes were more likely to be published and these studies might not represent the general outcomes. About one-fourth of the published cases in this study were reported by Dr. Gu and his colleagues with favorable outcomes, which might be attributed to their experience with CC7 transfer procedure. These limitations make reliable analysis difficult. Without consistent use of outcomes measures, statistical power was lacking to support the comparison between studies. Therefore, we used descriptive statistics in this systematic review to investigate the overall outcome of CC7 transfer.
Despite some limitations, we screened and summarized the data in the most rigorous way to provide the best available evidence on CC7 transfer. However, outcomes measures in the included studies were not consistent and specific enough to uncover true patient-related benefits from the CC7 transfer. Reliable and validated outcomes instruments should be created to evaluate patients undergoing CC7 transfer. Other than overall outcomes, aspects such as motor and sensory donor-site morbidity should also be investigated, which we will discuss in the second part of this paper.
Supplementary Material
Acknowledgments
Research reported in this publication was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under Award Number 2 K24-AR053120-06. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Supplemental Digital Content 1, Appendix I shows all included articles, INSERT LINK.
REFERENCES
- 1.Terzis JK, Vekris MD, Soucacos PN. Outcomes of brachial plexus reconstruction in 204 patients with devastating paralysis. Plast Reconstr Surg. 1999;104:1221–1240. doi: 10.1097/00006534-199910000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Wehrli L, Bonnard C, Anastakis DJ. Current status of brachial plexus reconstruction: restoration of hand function. Clin Plast Surg. 2011;38:661–681. doi: 10.1016/j.cps.2011.07.003. [DOI] [PubMed] [Google Scholar]
- 3.Colbert SH, Mackinnon SE. Nerve transfers for brachial plexus reconstruction. Hand Clin. 2008;24:341–361. doi: 10.1016/j.hcl.2008.07.001. v. [DOI] [PubMed] [Google Scholar]
- 4.Gu YD, Zhang GM, Chen DS, et al. Cervical nerve root transfer from the healthy side for treatment of brachial plexus root avulsion. Chin Med J. 1989;69:563–565. [PubMed] [Google Scholar]
- 5.Chuang DC, Wei FC, Noordhoff MS. Cross-chest C7 nerve grafting followed by free muscle transplantations for the treatment of total avulsed brachial plexus injuries: a preliminary report. Plast Reconstr Surg. 1993;92:717–725. discussion 726-717. [PubMed] [Google Scholar]
- 6.Chuang DC. Neurotization procedures for brachial plexus injuries. Hand Clin. 1995;11:633–645. [PubMed] [Google Scholar]
- 7.Gu Y, Xu J, Chen L, Wang H, Hu S. Long term outcome of contralateral C7 transfer: a report of 32 cases. Chin Med J (Engl) 2002;115:866–868. [PubMed] [Google Scholar]
- 8.Gu YD. Contralateral C7 root transfer over the last 20 years in China. Chin Med J (Engl) 2007;120:1123–1126. [PubMed] [Google Scholar]
- 9.Oberlin C, Durand S, Belheyar Z, et al. Nerve transfers in brachial plexus palsies. Chir Main. 2009;28:1–9. doi: 10.1016/j.main.2008.11.010. [DOI] [PubMed] [Google Scholar]
- 10.Sammer DM, Kircher MF, Bishop AT, Spinner RJ, Shin AY. Hemi-contralateral C7 transfer in traumatic brachial plexus injuries: outcomes and complications. J Bone Joint Surg Am. 2012;94:131–137. doi: 10.2106/JBJS.J.01075. [DOI] [PubMed] [Google Scholar]
- 11.Haines T, McKnight L, Duku E, Perry L, Thoma A. The role of systematic reviews in clinical research and practice. Clin Plast Surg. 2008;35:207–214. doi: 10.1016/j.cps.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 12.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 13.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1–e34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 14.Chen L, Gu YD, Xu L. Clinical application of axonal repair technique for treatment of peripheral nerve injury. Chin J Traumatol. 2004;7:153–155. [PubMed] [Google Scholar]
- 15.Sun G, Gu Y, Yu C, et al. Clinical application and efficiency of two stage multiple nerves transfer for treatment of root avulsion of brachial plexus. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2005;19:450–452. [PubMed] [Google Scholar]
- 16.Hua XY, Zuo CT, Xu WD, et al. Reversion of transcallosal interhemispheric neuronal inhibition on motor cortex after contralateral C7 neurotization. Clin Neurol Neurosurg. 2012;114:1035–1038. doi: 10.1016/j.clineuro.2012.01.047. [DOI] [PubMed] [Google Scholar]
- 17.Gu YD, Zhang GM, Chen DS, et al. Seventh cervical nerve root transfer from the contralateral healthy side for treatment of brachial plexus root avulsion. J Hand Surg Br. 1992;17:518–521. doi: 10.1016/s0266-7681(05)80235-9. [DOI] [PubMed] [Google Scholar]
- 18.Gu YD, Chen DS, Zhang GM, et al. Long-term functional results of contralateral C7 transfer. J Reconstr Microsurg. 1998;14:57–59. doi: 10.1055/s-2007-1006902. [DOI] [PubMed] [Google Scholar]
- 19.Terzis JK, Kokkalis ZT. Selective contralateral c7 transfer in posttraumatic brachial plexus injuries: a report of 56 cases. Plast Reconstr Surg. 2009;123:927–938. doi: 10.1097/PRS.0b013e31819ba48a. [DOI] [PubMed] [Google Scholar]
- 20.Bertelli JA, Ghizoni MF. Selective motor hyperreinnervation by using contralateral C-7 motor rootlets in the reconstruction of an avulsion injury of the brachial plexus. Case report. J Neurosurg. 1999;90:1133–1136. doi: 10.3171/jns.1999.90.6.1133. [DOI] [PubMed] [Google Scholar]
- 21.Waikakul S, Orapin S, Vanadurongwan V. Clinical results of contralateral C7 root neurotization to the median nerve in brachial plexus injuries with total root avulsions. J Hand Surg Br. 1999;24:556–560. doi: 10.1054/jhsb.1999.0264. [DOI] [PubMed] [Google Scholar]
- 22.Songcharoen P, Wongtrakul S, Mahaisavariya B, Spinner RJ. Hemi-contralateral C7 transfer to median nerve in the treatment of root avulsion brachial plexus injury. J Hand Surg Am. 2001;26:1058–1064. doi: 10.1053/jhsu.2001.27764. [DOI] [PubMed] [Google Scholar]
- 23.El-Gammal TA, Fathi NA. Outcomes of surgical treatment of brachial plexus injuries using nerve grafting and nerve transfers. J Reconstr Microsurg. 2002;18:7–15. doi: 10.1055/s-2002-19703. [DOI] [PubMed] [Google Scholar]
- 24.El-Gammal TA, El-Sayed A, Kotb MM. Surgical treatment of brachial plexus traction injuries in children, excluding obstetric palsy. Microsurgery. 2003;23:14–17. doi: 10.1002/micr.10084. [DOI] [PubMed] [Google Scholar]
- 25.Yu ZJ, Sui S, Yu S, Huang Y, Sheng J. Contralateral normal C7 nerve transfer after upper arm shortening for the treatment of total root avulsion of the brachial plexus: a preliminary report. Plast Reconstr Surg. 2003;111:1465–1469. doi: 10.1097/01.PRS.0000049634.97185.2D. [DOI] [PubMed] [Google Scholar]
- 26.Bertelli JA, Ghizoni MF. Contralateral motor rootlets and ipsilateral nerve transfers in brachial plexus reconstruction. J Neurosurg. 2004;101:770–778. doi: 10.3171/jns.2004.101.5.0770. [DOI] [PubMed] [Google Scholar]
- 27.Amr SM, Moharram AN. Repair of brachial plexus lesions by end-to-side side-to-side grafting neurorrhaphy: experience based on 11 cases. Microsurgery. 2005;25:126–146. doi: 10.1002/micr.20036. [DOI] [PubMed] [Google Scholar]
- 28.Beaulieu JY, Blustajn J, Teboul F, et al. Cerebral plasticity in crossed C7 grafts of the brachial plexus: an fMRI study. Microsurgery. 2006;26:303–310. doi: 10.1002/micr.20243. [DOI] [PubMed] [Google Scholar]
- 29.Xu W, Lu J, Xu J, Gu Y. Full-length ulnar nerve harvest by means of endoscopy for contralateral C7 nerve root transfer in the treatment of brachial plexus injuries. Plast Reconstr Surg. 2006;118:689–693. doi: 10.1097/01.prs.0000232980.37831.76. discussion 694-685. [DOI] [PubMed] [Google Scholar]
- 30.Chen L, Gu YD, Hu SN, et al. Contralateral C7 transfer for the treatment of brachial plexus root avulsions in children - a report of 12 cases. J Hand Surg Am. 2007;32:96–103. doi: 10.1016/j.jhsa.2006.05.013. [DOI] [PubMed] [Google Scholar]
- 31.Hierner R, Berger AK. Did the partial contralateral C7-transfer fulfil our expectations? Results after 5 year experience. Acta Neurochir Suppl. 2007;100:33–35. doi: 10.1007/978-3-211-72958-8_7. [DOI] [PubMed] [Google Scholar]
- 32.Xu L, Gu Y, Xu J, et al. Contralateral C7 transfer via the prespinal and retropharyngeal route to repair brachial plexus root avulsion: a preliminary report. Neurosurgery. 2008;63:553–558. doi: 10.1227/01.NEU.0000324729.03588.BA. discussion 558–559. [DOI] [PubMed] [Google Scholar]
- 33.Feng J, Wang T, Gu Y, et al. Contralateral C7 transfer to lower trunk via a subcutaneous tunnel across the anterior surface of chest and neck for total root avulsion of the brachial plexus: a preliminary report. Neurosurgery. 2010;66:252–263. doi: 10.1227/01.NEU.0000369658.43380.95. discussion 263. [DOI] [PubMed] [Google Scholar]
- 34.Wang SF, Li PC, Xue YH, et al. The clinical study of reconstruction of traumatic brachial plexus root avulsion injury in children. Zhonghua Wai Ke Za Zhi. 2010;48:35–38. [PubMed] [Google Scholar]
- 35.Zuo CT, Hua XY, Guan YH, et al. Long-range plasticity between intact hemispheres after contralateral cervical nerve transfer in humans. J Neurosurg. 2010;113:133–140. doi: 10.3171/2010.1.JNS09448. [DOI] [PubMed] [Google Scholar]
- 36.Bertelli JA, Ghizoni MF. Transfer of the platysma motor branch to the accessory nerve in a patient with trapezius muscle palsy and total avulsion of the brachial plexus: case report. Neurosurgery. 2011;68:E567–E570. doi: 10.1227/NEU.0b013e318202086c. discussion E570. [DOI] [PubMed] [Google Scholar]
- 37.Lin H, Lv D, Hou C, Chen D. Modified C-7 neurotization in the treatment of brachial plexus avulsion injury. J Neurosurg. 2011;115:865–869. doi: 10.3171/2011.6.JNS101604. [DOI] [PubMed] [Google Scholar]
- 38.Muhetidier A, Yilixiati S, Gulinaer Y, Aihemaitijiang Y. Clinical outcome of contralateral C7 nerve root transposition for treatment of brachial plexus root avulsion injury. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2011;25:1364–1366. [PubMed] [Google Scholar]
- 39.Wang L, Zhao X, Gao K, Lao J, Gu YD. Reinnervation of thenar muscle after repair of total brachial plexus avulsion injury with contralateral C7 root transfer: report of five cases. Microsurgery. 2011;31:323–326. doi: 10.1002/micr.20836. [DOI] [PubMed] [Google Scholar]
- 40.Chuang DC, Hernon C. Minimum 4-year follow-up on contralateral C7 nerve transfers for brachial plexus injuries. J Hand Surg Am. 2012;37:270–276. doi: 10.1016/j.jhsa.2011.10.014. [DOI] [PubMed] [Google Scholar]
- 41.Terzis JK, Barmpitsioti A. Our experience with triceps nerve reconstruction in patients with brachial plexus injury. J Plast Reconstr Aesthet Surg. 2012;65:590–600. doi: 10.1016/j.bjps.2011.11.027. [DOI] [PubMed] [Google Scholar]
- 42.Wang S, Yiu HW, Li P, et al. Contralateral C7 nerve root transfer to neurotize the upper trunk via a modified prespinal route in repair of brachial plexus avulsion injury. Microsurgery. 2012;32:183–188. doi: 10.1002/micr.20963. [DOI] [PubMed] [Google Scholar]
- 43.Gao K, Lao J, Zhao X, Gu Y. Outcome of contralateral C7 transfer to two recipient nerves in 22 patients with the total brachial plexus avulsion injury. Microsurgery. 2013;33:605–611. doi: 10.1002/micr.22137. [DOI] [PubMed] [Google Scholar]
- 44.Gao KM, Lao J, Zhao X, Gu YD. Outcome of contralateral C7 nerve transferring to median nerve. Chin Med J (Engl) 2013;126:3865–3868. [PubMed] [Google Scholar]
- 45.Hua XY, Liu B, Qiu YQ, et al. Long-term ongoing cortical remodeling after contralateral C-7 nerve transfer. J Neurosurg. 2013;118:725–729. doi: 10.3171/2012.12.JNS12207. [DOI] [PubMed] [Google Scholar]
- 46.Wang SF, Li PC, Xue YH, et al. Contralateral C7 nerve transfer with direct coaptation to restore lower trunk function after traumatic brachial plexus avulsion. J Bone Joint Surg Am. 2013;95:821–827. S821–S822. doi: 10.2106/JBJS.L.00039. [DOI] [PubMed] [Google Scholar]
- 47.Tu YK, Tsai YJ, Chang CH, et al. Surgical treatment for total root avulsion type brachial plexus injuries by neurotization: a prospective comparison study between total and hemicontralateral C7 nerve root transfer. Microsurgery. 2014;34:91–101. doi: 10.1002/micr.22148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Doi K, Hattori Y, Ikeda K, Dhawan V. Significance of shoulder function in the reconstruction of prehension with double free-muscle transfer after complete paralysis of the brachial plexus. Plast Reconstr Surg. 2003;112:1596–1603. doi: 10.1097/01.PRS.0000085820.24572.EE. [DOI] [PubMed] [Google Scholar]
- 49.Hattori Y, Doi K, Ikeda K, Pagsaligan JM, Watanabe M. Restoration of prehension using double free muscle technique after complete avulsion of brachial plexus in children: a report of three cases. J Hand Surg Am. 2005;30:812–819. doi: 10.1016/j.jhsa.2004.12.011. [DOI] [PubMed] [Google Scholar]
- 50.Beisteiner R, Hollinger I, Rath J, et al. New type of cortical neuroplasticity after nerve repair in brachial plexus lesions. Arch Neurol. 2011;68:1467–1470. doi: 10.1001/archneurol.2011.596. [DOI] [PubMed] [Google Scholar]
- 51.Midha R. Epidemiology of brachial plexus injuries in a multitrauma population. Neurosurgery. 1997;40:1182–1188. doi: 10.1097/00006123-199706000-00014. discussion 1188–1189. [DOI] [PubMed] [Google Scholar]
- 52.Dorsi MJ, Hsu W, Belzberg AJ. Epidemiology of brachial plexus injury in the pediatric multitrauma population in the United States. J Neurosurg Pediatr. 2010;5:573–577. doi: 10.3171/2010.3.PEDS09538. [DOI] [PubMed] [Google Scholar]
- 53.Jain DK, Bhardwaj P, Venkataramani H, Sabapathy SR. An epidemiological study of traumatic brachial plexus injury patients treated at an Indian centre. Indian J Plast Surg. 2012;45:498–503. doi: 10.4103/0970-0358.105960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fu SY, Gordon T. Contributing factors to poor functional recovery after delayed nerve repair: prolonged denervation. J Neurosci. 1995;15:3886–3895. doi: 10.1523/JNEUROSCI.15-05-03886.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mackinnon SE, Novak CB. Nerve transfers. New options for reconstruction following nerve injury. Hand Clin. 1999;15:643–666. ix. [PubMed] [Google Scholar]
- 56.Terzis JK, Kostas I. Suprascapular nerve reconstruction in 118 cases of adult posttraumatic brachial plexus. Plast Reconstr Surg. 2006;117:613–629. doi: 10.1097/01.prs.0000203410.35395.fa. [DOI] [PubMed] [Google Scholar]
- 57.Nagano A, Tsuyama N, Ochiai N, Hara T, Takahashi M. Direct nerve crossing with the intercostal nerve to treat avulsion injuries of the brachial plexus. J Hand Surg Am. 1989;14:980–985. doi: 10.1016/s0363-5023(89)80047-4. [DOI] [PubMed] [Google Scholar]
- 58.Siqueira MG, Martins RS. Phrenic nerve transfer in the restoration of elbow flexion in brachial plexus avulsion injuries: how effective and safe is it? Neurosurgery. 2009;65:A125–A131. doi: 10.1227/01.NEU.0000338865.19411.7F. [DOI] [PubMed] [Google Scholar]
- 59.Sulaiman OA, Kim DD, Burkett C, Kline DG. Nerve transfer surgery for adult brachial plexus injury: a 10-year experience at Louisiana State University. Neurosurgery. 2009;65:A55–A62. doi: 10.1227/01.NEU.0000341165.83218.AC. [DOI] [PubMed] [Google Scholar]
- 60.Gorio A, Carmignoto G. Reformation, maturation and stabilization of neuromuscular junctions in peripheral nerve regeneration. In: Gorio A, Millesi H, Mingrino S, editors. Posttraumatic peripheral nerve regeneration. 1st ed. New York: Raven Press; 1981. pp. 481–492. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.