Abstract
For proximal varus osteotomy of the femur in children, a stable fixation, is a concern regarding the safety and the protection of the surgery. The methods of fixation are mostly represented by plating systems; however, the tension band wiring is a simple and eligible option for fixation of proximal femur osteotomy. The purpose of this retrospective case series study is to evaluate outcomes and bone remodelation after using the tension band wiring technique to fixate proximal femoral varus osteotomies in children.
The study enrolled 20 patients who underwent femoral varus osteotomy to treat Legg–Calvé–Perthes disease and other causes of necrosis of the femoral head. The mean patient age at the time of surgery was 7.4 ± 2.3 years (range, 4.3–13.8 y), and the follow-up period averaged 10 ± 4.3 years (range, 4.7–20.8 y). To assess the effects of the osteotomy at the neck-shaft angle and its evolution over time, radiographs obtained preoperatively and during the follow-up were analyzed. The neck-shaft angle was measured independently by 2 observers, and intraclass correlation coefficients (ICCs) were assessed for reliability.
The ICC analysis showed good reliability. There was a significant reduction in the neck-shaft angle (P < 0.001) between the preoperative and the immediate postoperative periods, with an estimated difference of 14.3°. Between the immediate and the early postoperative periods, the estimated difference was 2.1°, which indicated a significant increase in the neck-shaft angle (P = 0.003). Between the early postoperative period and the final evaluation, there was a significant increase (P < 0.001), with an estimated difference of 7.0°. No implant failures or other complications were observed, but 1 case of peri-implant femoral fracture occurred >17 years postsurgery.
The tension band wiring technique proved to be a simple and effective method for fixating proximal femoral varus osteotomy in children.
The level IV is appropriated for our study (case series, retrospective).
INTRODUCTION
Recently, more suitable pediatric implants, such as locking plate/screw system, have been designed to overcome some of the limitations of earlier stabilization systems.1,2 However, over the past few decades, there have been few options in plate designs to fix proximal femoral osteotomies in children, considering the range in patient ages and the variety of bone morphology and quality; thus, only 2 different hardware models have been available. The angled blade plate has been widely used for fixating osteotomies, but it can be technically demanding, and the device is sometimes undersized or oversized. Another alternative is the Coventry plate, which offers more options in terms of implant size3; when used for varus osteotomies, it may create a subcutaneous prominence in the trochanteric region that irritates the patient or causes pain. Another consideration regarding the plates and screws system is that it might not be suitable for osteoporotic bones, which may be present in patients with cerebral palsy.
In 1982, Brunner and Weber4 suggested that there could be more indications for cerclage wires in osteosynthesis than those classically recommended by the Association for the Study of Internal Fixation, using the cerclage principle, as developed by Pauwels.5 Based on these principles, Brunner and Weber4 presented a simple, low-cost, and efficient technique that consisted of 2 Kirschner wires and a cerclage acting as a tension band, for fixating femoral varus intertrochanteric osteotomies in children. This system transforms the bending stresses on the proximal femur into compression forces across the osteotomy. The Kirschner wires act as drivers, and they neutralize shear and torsional forces.
Proximal femoral varus osteotomy is also frequently indicated for treating Legg–Calvé–Perthes disease (LCPD) and other causes of necrosis of the femoral head in children.6–9 The aim of this surgery is to improve the containment of the femoral head into the acetabulum by decreasing the neck-shaft angle, thereby providing a better environment to heal the necrosis. After the healing has completed, a gradual remodeling of the neck-shaft angle is expected for growing children.
The purpose of this study was to assess the performance of the tension band wiring technique in the fixation of intertrochanteric varus osteotomies in children.
METHODS
This retrospective case series research was approved by the Institutional Review Board of the Hospital das Clínicas of Ribeirão Preto Medical School, University of São Paulo, São Paulo, Brazil (180.178; January 19, 2013). As a long-term retrospective study using patient’s records and radiographs, the Institutional Review Board waived the need for informed consent.
Twenty patients (16 males and 4 females) who underwent proximal femoral varus osteotomy and fixation with the tension band wiring technique between June 1991 and January 2003 were retrospectively evaluated. Eighteen patients had LCPD, 1 patient had femoral head necrosis secondary to sickle-cell disease, and 1 patient had femoral head necrosis secondary to septic arthritis. Thirteen patients underwent surgery on the left side, and 7 underwent surgery on the right side. In the 18 patients with LCPD, 3 had bilateral involvement, but the varus osteotomy was performed on only one side. The mean age at the time of surgery was 7.4 ± 2.3 years (range, 4.3–13.8 y). For the Legg–Calvé–Perthes cases, the disease indication for surgery was based on clinical and radiographic signs of a femoral head at risk.
Surgical Technique
Initially, a hip arthrogram was obtained to examine the joint motion and congruence, and to exclude the hinge abduction phenomenon. For the 20 cases in this study, congruence was improved with hip abduction. All surgeries were performed using a conventional longitudinal lateral approach. The proximal femur was exposed, and an osteotomy was performed in the intertrochanteric region by removing an average of 15° of the medial-based bone wedge, which was measured using a triangular guide. Mild medialization of the femoral shaft was achieved before closing the wedge to maintain the mechanical axis alignment. After reducing the osteotomy, 2 Kirschner wires (2.0–2.5 mm) were driven through the greater trochanter, crossing the osteotomy line and penetrating the medial cortex of the distal fragment. The level of the osteotomy, the reduction, and the wire insertion were performed under C-arm control. A transverse hole was created in the lateral cortex of the distal fragment, and a 1.0-mm flexible steel wire was introduced. Making a figure-8, the ends of the wire were anchored in the Kirschner wires over the greater trochanter and then tensioned and tied. To prevent migration, the proximal ends of the Kirschner wires were bent and affixed into the cartilage of the greater trochanter (Figure 1). No rotation of the fragments was performed during the procedure. No external immobilization was used and the hospital discharge was at the second postoperative day. Younger children were allowed to use wheelchairs but avoid weight bearing on the operated side. Children with more age, in general, with more than 8 or 9 years, were permitted to use orthopedic walker or 2 crutches, with toe-touch weight bearing. They were advised to return to school after 2 or 3 weeks after the surgery, and to take lessons at home when schooling was not possible.
FIGURE 1.
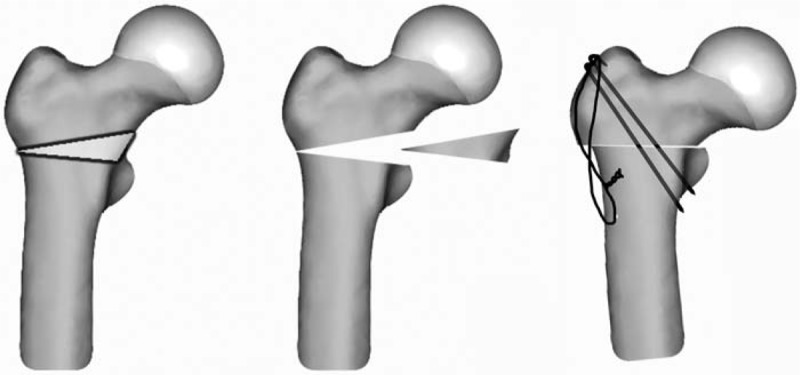
Schematics of the tension band fixation of the proximal femoral varus osteotomy. A 15° medial bone wedge was removed from the intertrochanteric region; the osteotomy was closed, and stabilization was achieved with two Kirschner wires and a figure-8 cerclage.
Radiological Assessment
The authors reviewed the radiographs obtained from 4 follow-ups: the preoperative, immediate postoperative, early postoperative (between 6 and 18 mo), and final follow-up (late postoperative) periods. All images were scanned and converted into digital imaging and communications in medicine files. Measurement of the neck-shaft angle was performed to assess the degree of varus achieved by the osteotomy and the evolution of this change in the angulation of the proximal femur over time. Two blinded observers (i.e., RGP, second author, and DAM, first author, with 17 and 7 years of experience in pediatric orthopedic surgery, respectively) measured the neck-shaft angle on 2 occasions with 3–4-week intervals between the measurements. The angle measurements were calculated using OsiriX open-source software, version 3.9.4 (OsiriX Foundation, Geneva, Switzerland).
Statistical Analysis
The intraobserver and interobserver reliability was estimated using intraclass correlation coefficients (ICCs). Poor reliability is suggested for values between 0 and 0.20, fair reliability from 0.21 to 0.40, moderate reliability from 0.41 to 0.60, substantial or good reliability from 0.61 to 0.80, and nearly perfect or very good reliability from 0.81 to 1.0.10,11
The value of neck-shaft angle used for the statistical analysis was the average between all measurements of both the observers. The data were submitted to the Kolmogorov–Smirnov normality test, and there was no rejection for normality of the average value of the neck-shaft angle.
Repeated-measures analysis of variance was used to evaluate the continuous data related to measurements over all observation periods, and the Bonferroni post-hoc test was applied. For all statistical analyses, P values <0.05 were considered to be significant.
RESULTS
The 20 patients were followed for an average of 10 ± 4.3 years (range, 4.7–20.8 y). The mean patient age at surgery was 7.4 ± 2.3 years, and the mean age at final evaluation was 17.4 ± 4.6 years (range, 12.0–28.0 y). Fourteen patients had reached skeletal maturity by the final follow-up, whereas 6 were immature. All patients showed complete healing of the osteotomy at the end of 6 weeks, with no intercurrence during the immediate postoperative period. There were no cases of deep or superficial infection, implant failure, or other procedure-related complications.
Prior to the varus osteotomy, 1 patient underwent Salter osteotomy and 2 patients underwent arthrodiastasis; varus osteotomy was indicated because of the failure of such interventions. One patient underwent lateral Tönnis acetabuloplasty at the same time as the varus osteotomy because of residual acetabular dysplasia. After the varus osteotomy, 5 patients underwent complementary surgical procedures to treat late hip deformities: 1 patient underwent triple pelvic osteotomy; 2 underwent Chiari osteotomy; 2 underwent arthrodiastasis; and 1 patient underwent greater trochanteric osteotomy. One patient had a high-energy automobile accident with a peri-implant femoral fracture 17 years after the femur osteotomy. In 3 of these patients, the tension band implants were removed at the time of the complementary surgery, whereas 4 patients underwent implant removal as isolated procedures (3 for mild scar tenderness; 1 asked for removal despite no local symptoms). There were no surgical procedures that could have significantly interfered with the femoral remodeling process (Table 1).
TABLE 1.
Clinical Data and Average Measurements of the Neck-Shaft Angle
There was good or very good intraobserver and interobserver reliability among the radiographic measurements of the neck-shaft angle. The intraobserver variability was related to single ICC measurements varying from 0.69 to 0.79 for one observer and from 0.96 to 0.99 for the other observer. The interobserver variability was related to single ICC measurements that varied from 0.69 to 0.85 among the ratings.
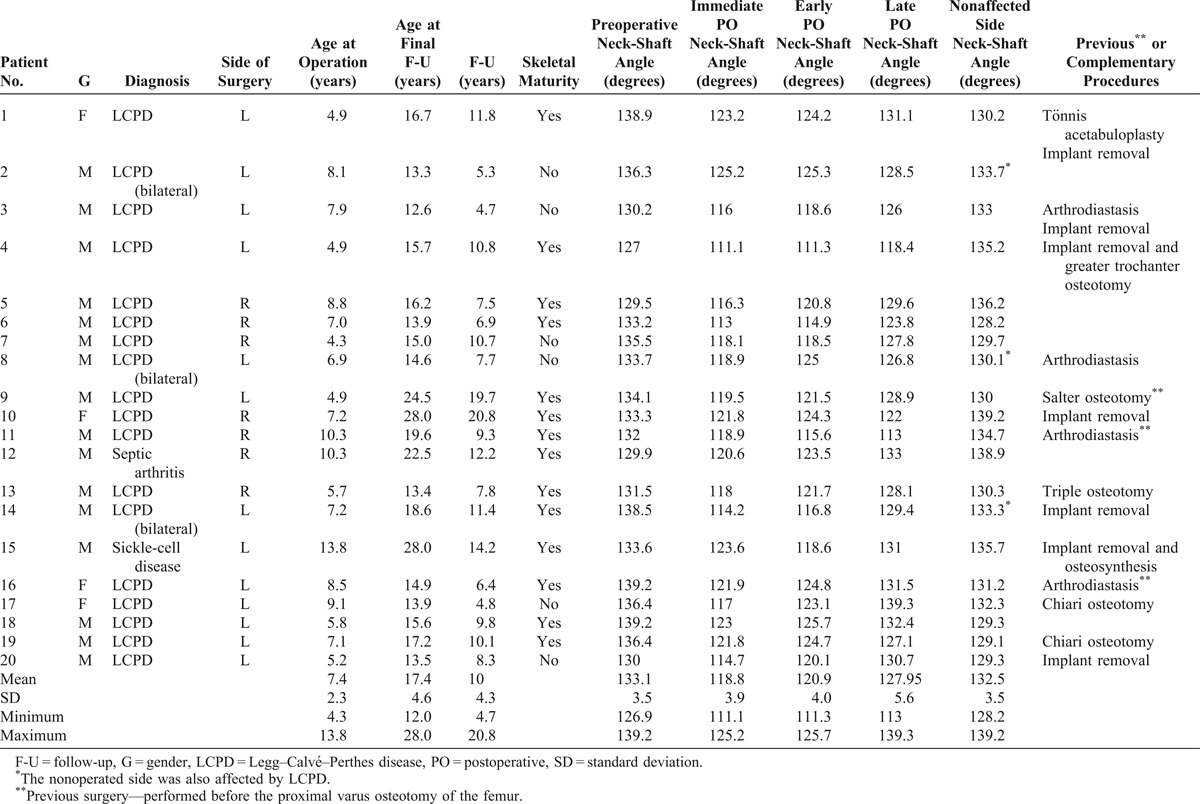
The preoperative mean neck-shaft angle was 133.1° ± 3.5° on the affected side (range, 126.9°–139.2°), and the immediate postoperative mean angle was 118.8° ± 3.9° (range, 111.1°–125.2°). After 6–18 months postsurgery (average 12 ± 3.8 mo), the mean angle was 120.9° ± 4.0° (range, 111.3°–125.7°). At the final follow-up, the mean neck-shaft angle was 127.9° ± 5.6° (range, 113°–139.3°) (Figure 2). Two patients maintained a varus inclination of the femoral neck at the final follow-up (patients 4 and 11, Table 1), with a neck-shaft angle of <125°. The patient 4 had an incomplete remodeling process associated with a severe coxa breva and an insufficient increase of 7.3° between the immediate and the late postoperative periods, whereas the patient 11 had a decrease of 5.9° in the neck-shaft angle between the immediate and the late postoperative periods (Table 1).
FIGURE 2.
Remodeling of the neck-shaft angle over time after varus osteotomy. Frequency distribution of neck-shaft angle of the operated hip in the preoperative (PRE), immediate postoperative (Immed PO), early postoperative (Early PO), and late postoperative periods (Late PO). The Late Normal column refers to normal, nonaffected hips (17 patients). There were significant differences between all comparisons (P < 0.01), except for between the PRE and the Late Normal periods (P = 0.59).
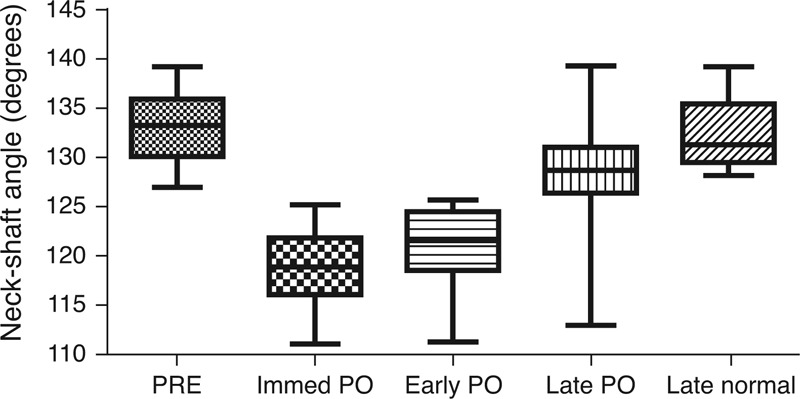
Comparing the values of the neck-shaft angle between the preoperative and the immediate postoperative periods (Figure 3), the estimated difference was 14.3° ± 2.4° of varus (95% confidence interval [CI], 13.2°–15.4°), indicating a significant decrease in the neck-shaft angle (P < 0.001). The estimated difference between the immediate and the early postoperative periods was 2.1° ± 2.8° of valgus (95% CI, 0.8°–3.4°), indicating a significant increase in neck-shaft angle (P = 0.003). The estimated difference between the early and the late postoperative periods was 7° ± 4.7° (95% CI, 4.8°–9.2°), which demonstrated a significant increase in the neck-shaft angle (P < 0.001). Therefore, there was a final difference between the immediate postoperative period and the final evaluation (late postoperative) of 9.1° ± 5.9° (95% CI, 6.3°–11.8°; P < 0.001). At the final evaluation, the estimated difference between the preoperative angle and the late postoperative neck-shaft angle was 5.2° ± 6.5° (95% CI, 2.2°–8.2°; P = 0.002) of varus.
FIGURE 3.
Estimated differences in neck-shaft angle among several comparisons. A negative value indicates varus and a positive value indicates valgus. PRE: preoperative; Immed PO: immediate postoperative; Early PO: early postoperative period; Late PO: late postoperative period; Normal PRE: nonoperated side previous to the contralateral surgery; and Late Normal: nonoperated side at the final follow-up. The asterisks (*) indicate significant differences.
For the nonaffected hip, the initial preoperative mean neck-shaft angle was 133.7° ± 4.6° (range, 127° 142°), and at the final follow-up, it was 132.5° ± 3.5°(range, 128.2°–139.2°). There was no significant difference in the neck-shaft angle of the nonoperated hip during the follow-up (P = 0.39). At the final evaluation, there was a significant difference between the neck-shaft angle of the operated and the nonoperated hips of 4.6° ± 6.9° (95% CI, 0.7°–8.6°; P = 0.02), and for this analysis, the 3 bilateral cases of Perthes disease were not considered (Figure 3).
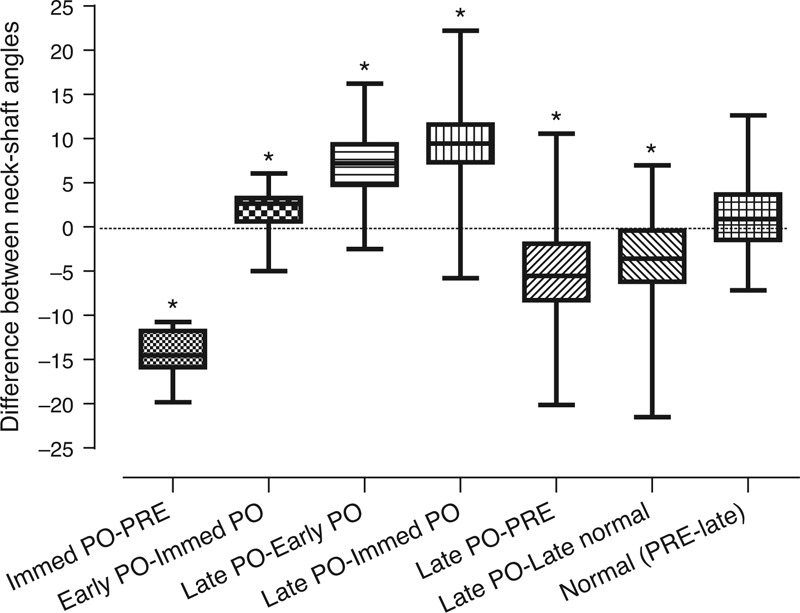
Figure 4 shows 1 representative case.
FIGURE 4.
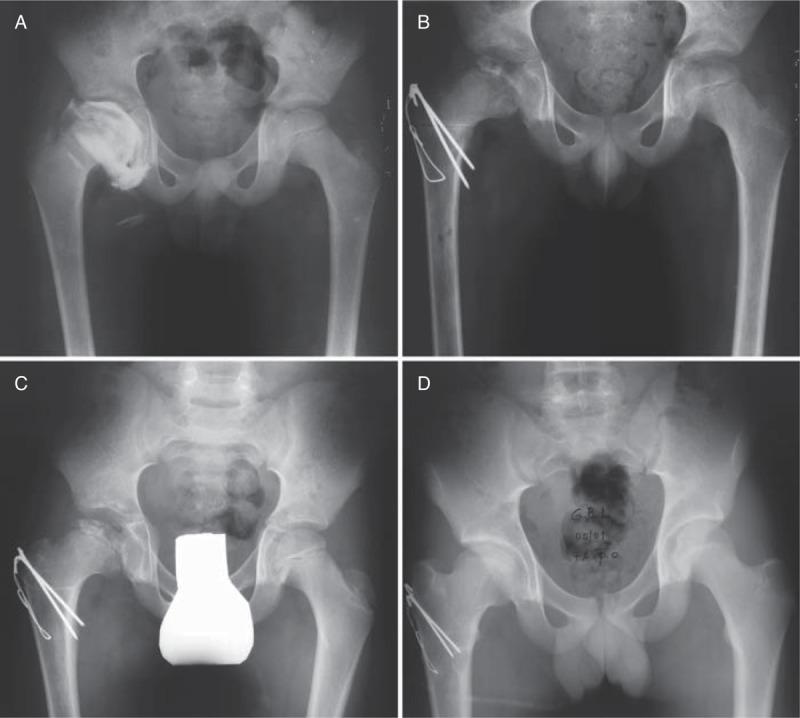
Case of Legg-Calvé-Perthes disease on the right hip treated with proximal varus osteotomy of the femur at the age of 8 years (case 5 in Table 1). (A) Anteroposterior radiograph of the pelvis showing the preoperative arthrogram. (B) Immediate postoperative radiograph in showing the tension band fixation after the varus osteotomy, with a decrease of 13.2° in the neck-shaft angle. (C) Early postoperative radiograph in showing the osteotomy completely healed after 10 months postsurgery. (D) Seven years postsurgery, the final follow-up radiograph showing a complete remodeling of the proximal femur, with a neck-shaft angle of 129°, similar to the preoperative radiograph.
DISCUSSION
Angled blade plates have been the standard fixation devices used for proximal femoral varus osteotomy in children.12 Nevertheless, problems remain with this technique, such as the plate being an unsuitable size for some children and the technical skill required for its insertion. Despite the recent development of locking plates that are specially designed for the pediatric femur,1,2 the possibility of an alternative fixation technique that could help to overcome some of these disadvantages led us to conduct this study.
Experimental studies have indicated that the principle of tension band wiring fixation of the proximal femur, as proposed by Pauwels and adapted by Weber, could overcome such limitations and provide simple and stable fixation.13,14 Most of the studies on the clinical application of this principle have focused on valgus osteotomy and the treatment of coxa vara.15,16 Several medical conditions are associated with bone fragility, in which the use of plates is not recommended. This study focused on assessing the effectiveness of this fixation type over time to maintain the initially obtained varus and the remodeling process of the proximal femur after surgery and did not focus on the treatment results of the basic condition.
As expected, there was a significant varus change in the proximal femur after osteotomy, with a mean reduction of 14.3° in the neck-shaft angle and an average postoperative angle of 118.8° (minimum: 111.1°). It is debatable how much varus is desirable for this type of osteotomy. Some authors have reported that the femoral neck angle could be reduced to 100°–110° without producing harmful shortening or a positive Trendelenburg sign.17,18 However, another study emphasized that the neck-shaft angle must not be <105° after surgery,19 while 2 prospective studies suggested that a neck-shaft angle between 110° and 115° was desirable.20,21
There is evidence that neck-shaft angles of less than 110° will not remodel, and a persistent varus deformity could result. Although our first case of tension band wiring fixation was performed approximately 20 years ago, we chose 15° as a standard wedge to be resected. This choice aligns with a recent study that indicated that 10°–15° of varus should be achieved when the surgery is performed in the early stages of LCPD and that greater varus angulation does not necessarily produce better results in preserving the femoral head.22 A residual coxa vara can be associated with labral and chondral abnormalities and with the femoroacetabular impingement phenomenon.23
Between the immediate and the early postoperative periods, which represented an average interval of 12 months, there was a statistically significant increase in the neck-shaft angle of 2.1°. This finding indicated an initial remodeling process that is consistent with a previous report.24 Nevertheless, 2 patients presented decreases in the angle during this period of 3.3° (patient 11) and 5.0° (patient 15). A possible loss of the osteotomy reduction could explain these more severe cases of postoperative varus, although there were no signs of implant loosening. Patient 15 had a complete remodeling process of the neck-shaft angle and ended up with 130°, but patient 11 persisted with a varus tendency and ended with 113°. In some cases of avascular necrosis of the femoral head, the development of coxa vara and breva can persist despite treatment, perhaps because of growth disturbance, which can affect the entire region.
Between the early and the late postoperative periods, with an average 10-year follow-up period, a subsequent remodeling process occurred, with a significant increase of 7.0° in the neck-shaft angle. Expressive thickening of the medial cortical was observed in all cases. All but 2 patients had angles that were >125° at the final follow-up; these values are within the normal range25 but were still different from the normal or nonoperated side. Some patients had not reached skeletal maturity at the final assessment; however, in our opinion, this fact did not invalidate the analysis of the remodeling process because the minimum postoperative follow-up period in this series was 4.7 years, which matches the suggested maximum remodeling potential.24
In the present study, the decision-making for additional surgeries was related to the severity of the disease. Some of these procedures preceded varus osteotomy, and others were indicated at a follow-up assessment, based on signs of a worsening condition or to prevent further consequences. Implant removal was indicated in 3 patients as part of other procedures, and in 4 as isolated procedure. One patient had a polytraumatic injury with a peri-implant femoral fracture. Because the implant is considered to be a minor device with load-shearing properties and relatively few harmful effects, it seems to offer advantages over the standard devices.
We are aware that this study had limitations, namely that it included a small number of cases, and there was no control group with similar patient characteristics. As this study was retrospective, radiographic images were obtained without having an accurate standardization method. In addition, clinical and radiographic comparisons with more recent locking compression pediatric hip plates could be helpful, and further studies of new implants are also necessary. However, to our knowledge, this study was the first to describe a consecutive series of pediatric patients submitted to proximal femoral varus osteotomy using the tension band wiring technique.
In conclusion, with this group of patients, the application of this fixation technique proved to be simple and effective, with few complications. The safety of the procedure allows us to recommend it as a good option for the fixation of proximal femoral varus osteotomy in children.
Footnotes
Abbreviations: CI = confidence interval, ICC = intraclass correlation coefficient, LCPD = Legg–Calvé–Perthes disease.
The authors and the Institution did not receive any funding or financial support. There were no payments, benefits, agreements, or commitments related to this research from any organization and there was no commercial aim.
The authors have no conflicts of interest to declare.
References
- 1.Rutz E, Brunner R. The pediatric LCP hip plate for fixation of proximal femoral osteotomy in cerebral palsy and severe osteoporosis. J Pediatr Orthop. 2010;30:726–731. [DOI] [PubMed] [Google Scholar]
- 2.Joeris A, Audige L, Ziebarth K, et al. The locking compression paediatric hip plate: technical guide and critical analysis. Int Orthop. 2012;36:2299–2306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Canale ST, Holand RW. Coventry screw fixation of osteotomies about the pediatric hip. J Pediatr Orthop. 1983;3:592–600. [DOI] [PubMed] [Google Scholar]
- 4.Brunner CF, Weber BG. Special Techniques in Internal Fixation. Berlin, Germany: Springer; 1982. [Google Scholar]
- 5.Pauwels F. Biomechanics of the normal and diseased hip: theoretical foundation, technique and results of treatment, an atlas. Berlin, Germany: Springer; 1976. [Google Scholar]
- 6.Lloyd-Roberts GC, Catterall A, Salamon PB. A controlled study of the indications for and the results of femoral osteotomy in Perthes’ disease. J Bone Joint Surg Br. 1976;58:31–36. [DOI] [PubMed] [Google Scholar]
- 7.Joseph B, Rao N, Mulpuri K, et al. How does a femoral varus osteotomy alter the natural evolution of Perthes’ disease? J Pediatr Orthop B. 2005;14:10–15. [DOI] [PubMed] [Google Scholar]
- 8.Sponseller PD, Desai SS, Millis MB. Comparison of femoral and innominate osteotomies for the treatment of Legg-Calve-Perthes disease. J Bone Joint Surg Am. 1988;70:1131–1139. [PubMed] [Google Scholar]
- 9.Noonan KJ, Price CT, Kupiszewski SJ, et al. Results of femoral varus osteotomy in children older than 9 years of age with Perthes disease. J Pediatr Orthop. 2001;21:198–204. [PubMed] [Google Scholar]
- 10.Fleiss J, Cohen J. The equivalence of weighted kappa and the intraclass correlation coefficient as measures of reliability. Educ Psychol Meas. 1973;33:613–619. [Google Scholar]
- 11.Shrout P, Fleiss J. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–428. [DOI] [PubMed] [Google Scholar]
- 12.Beauchesne R, Miller F, Moseley C. Proximal femoral osteotomy using the AO fixed-angle blade plate. J Pediatr Orthop. 1992;12:735–740. [PubMed] [Google Scholar]
- 13.Engel EE, Volpon JB, Shimano AC. Mechanical testing of the tension band wire fixation in the proximal femur. Arch Orthop Trauma Surg. 1997;116:266–270. [DOI] [PubMed] [Google Scholar]
- 14.Volpon JB, Batista LC, Shimano MM, et al. Tension band wire fixation for valgus osteotomies of the proximal femur: a biomechanical study of three configurations of fixation. Clin Biomech. 2008;23:395–401. [DOI] [PubMed] [Google Scholar]
- 15.Cordes S, Dickens DR, Cole WG. Correction of coxa vara in childhood. The use of Pauwels’ Y-shaped osteotomy. J Bone Joint Surg Br. 1991;73:3–6. [DOI] [PubMed] [Google Scholar]
- 16.Widmann RF, Hresko MT, Kasser JR, et al. Wagner multiple K-wire osteosynthesis to correct coxa vara in the young child: experience with a versatile “tailor-made” high angle blade plate equivalent. J Pediatr Orthop B. 2001;10:43–50. [PubMed] [Google Scholar]
- 17.Heikkinen E, Puranen J. Evaluation of femoral osteotomy in the treatment of Legg-Calve-Perthes disease. Clin Orthop Relat Res. 1980;150:60–68. [PubMed] [Google Scholar]
- 18.Kamegaya M, Saisu T, Ochiai N, et al. A paired study of Perthes’ disease comparing conservative and surgical treatment. J Bone Joint Surg Br. 2004;86:1176–1181. [DOI] [PubMed] [Google Scholar]
- 19.Weiner SD, Weiner DS, Riley PM. Pitfalls in treatment of Legg-Calve-Perthes disease using proximal femoral varus osteotomy. J Pediatr Orthop. 1991;11:20–24. [DOI] [PubMed] [Google Scholar]
- 20.Herring JA, Kim HT, Browne R. Legg-Calve-Perthes disease. Part II: prospective multicenter study of the effect of treatment on outcome. J Bone Joint Surg Am. 2004;86-A:2121–2134. [PubMed] [Google Scholar]
- 21.Wiig O, Terjesen T, Svenningsen S. Prognostic factors and outcome of treatment in Perthes’ disease: a prospective study of 368 patients with five-year follow-up. J Bone Joint Surg Br. 2008;90:1364–1371. [DOI] [PubMed] [Google Scholar]
- 22.Kim HK, da Cunha AM, Browne R, et al. How much varus is optimal with proximal femoral osteotomy to preserve the femoral head in Legg-Calve-Perthes disease?. J Bone Joint Surg Am. 2011;93:341–347. [DOI] [PubMed] [Google Scholar]
- 23.Maranho DA, Nogueira-Barbosa MH, Zamarioli A, et al. MRI abnormalities of the acetabular labrum and articular cartilage are common in healed Legg-Calve-Perthes disease with residual deformities of the hip. J Bone Joint Surg Am. 2013;95:256–265. [DOI] [PubMed] [Google Scholar]
- 24.Herceg MB, Cutright MT, Weiner DS. Remodeling of the proximal femur after upper femoral varus osteotomy for the treatment of Legg-Calve-Perthes disease. J Pediatr Orthop. 2004;24:654–657. [DOI] [PubMed] [Google Scholar]
- 25.Tonnis D. Normal values of the hip joint for the evaluation of X-rays in children and adults. Clin Orthop Relat Res. 1976;119:39–47. [PubMed] [Google Scholar]


