Abstract
Cervical spondylosis and hypertension are all common diseases, but the relationship between them has never been studied. Patients with cervical spondylosis are often accompanied with vertigo. Anterior cervical discectomy and fusion is an effective method of treatment for cervical spondylosis with cervical vertigo that is unresponsive to conservative therapy. We report 2 patients of cervical spondylosis with concomitant cervical vertigo and hypertension who were treated successfully with anterior cervical discectomy and fusion. Stimulation of sympathetic nerve fibers in pathologically degenerative disc could produce sympathetic excitation, and induce a sympathetic reflex to cause cervical vertigo and hypertension. In addition, chronic neck pain could contribute to hypertension development through sympathetic arousal and failure of normal homeostatic pain regulatory mechanisms.
Cervical spondylosis may be one of the causes of secondary hypertension. Early treatment for resolution of symptoms of cervical spondylosis may have a beneficial impact on cardiovascular disease risk in patients with cervical spondylosis.
PRESENTING CONCERNS
Cervical spondylosis is a common cause of chronic neck pain, radiculopathy and/or myelopathy resulting in significant disability. When patients do not respond to conservative therapy, anterior cervical discectomy and fusion (ACDF) usually is used to achieve neural decompression, maintain cervical lordosis, and provide segmental stabilization.1 In our practice, it was often found that patients with cervical spondylosis tended to have concomitant cervical vertigo symptoms such as tinnitus, headache, blur vision, and palpitation. Recent studies have indicated that cervical spondylosis patients with cervical vertigo symptoms could be managed successfully with ACDF.2,3 In this study, we report 2 cases of cervical spondylosis with concomitant cervical vertigo and hypertension that were treated successfully with ACDF. This study obtained the approval of the medical ethics committee of our hospital (General Hospital of Armed Police Force, Beijing, China). The written informed consent was obtained from the 2 patients before anterior cervical surgery.
CLINICAL FINDINGS
Case 1, a 49-year-old female, was admitted with 2 years of history of chronic neck pain, headache, and episodic vertigo and tinnitus. Episode occurred 1 to 2 times every day, and lasted 1 to 2 h each time. Her vertigo was not related to head and neck rotation. Tests of labyrinthine function revealed no abnormality that could have accounted for her vertigo. She felt numbness of both upper extremities and weakness of all 4 extremities for 1 year. Physical examination showed that limited neck motion, slightly diminished sensation in both arms, and brisk deep tendon reflexes. No specific trauma could be recalled. Radiographic examination of the cervical spine showed mild diminution in the height of the C5/6 disc space (Figure 1). Magnetic resonance imaging (MRI) scan showed cord compression by a large central herniation of C5/6 disc with signs of myelomalacia (Figure 2).
FIGURE 1.

Lateral radiograph of cervical spine before operation showed slight narrowing of the C5/6 disc space.
FIGURE 2.

T2-weighted sagittal magnetic resonance imaging (MRI) revealed a large herniation of C5/6 disc before operation, with marked compression of cervical cord, resulting in myelomalacia.
The patient had a 2-year history of hypertension, blood pressure was 160/100 mmHg at onset, and then controlled in the normal range (110–130/70–80 mmHg) by oral medications (betaloc, 100 mg, once daily; enalapril, 10 mg, once daily).
Case 2, a 60-year-old male, was admitted with 10 years of history of chronic neck pain and stiffness. He also experienced vertigo, palpitation, nausea and vomiting with noted numbness of upper limbs, and heaviness of 4 limbs for over 6 months before admission. His vertigo was not related to head and neck rotation. Tests of labyrinthine function revealed no abnormality. Physical examination showed limited neck motion and brisk tendon reflexes on both sides. Radiographic examination of the cervical spine revealed large anterior and posterior spur formation at the C5/6 and C6/7 disc levels, severe diminution in the height of the C5/6 disc space, and moderate diminution in the height of the C6/7 disc space. MRI scan showed cervical canal stenosis with marked cord compression secondary to spondylotic changes in C5/6 and C6/7 discs.
The patient had a 1-year history of hypertension (maximum at 180/120 mmHg), which was controlled within the normal range by oral medications (irbesartan, 150 mg, once daily; nifedipine sustained release tablets, 20 mg, once daily; amlodiping besylate, 5 mg, once daily). He did not have history of diabetes and coronary heart disease.
DIAGNOSTIC FOCUS AND ASSESSMENT
Cervical spondylotic myelopathy was diagnosed and subsequently cervical anterior surgery was recommended for the 2 patients preoperatively based on clinical findings consistent with imaging study.
THERAPEUTIC FOCUS AND ASSESSMENT
Case 1 underwent ACDF at the C5/6 disc level (Figures 3 and 4). After surgery, strength in all 4 limbs was significantly recovered, and symptoms of neck pain, headache, vertigo, and tinnitus disappeared. Interestingly, her blood pressure also dropped to within the normal range after surgery even without oral medications.
FIGURE 3.
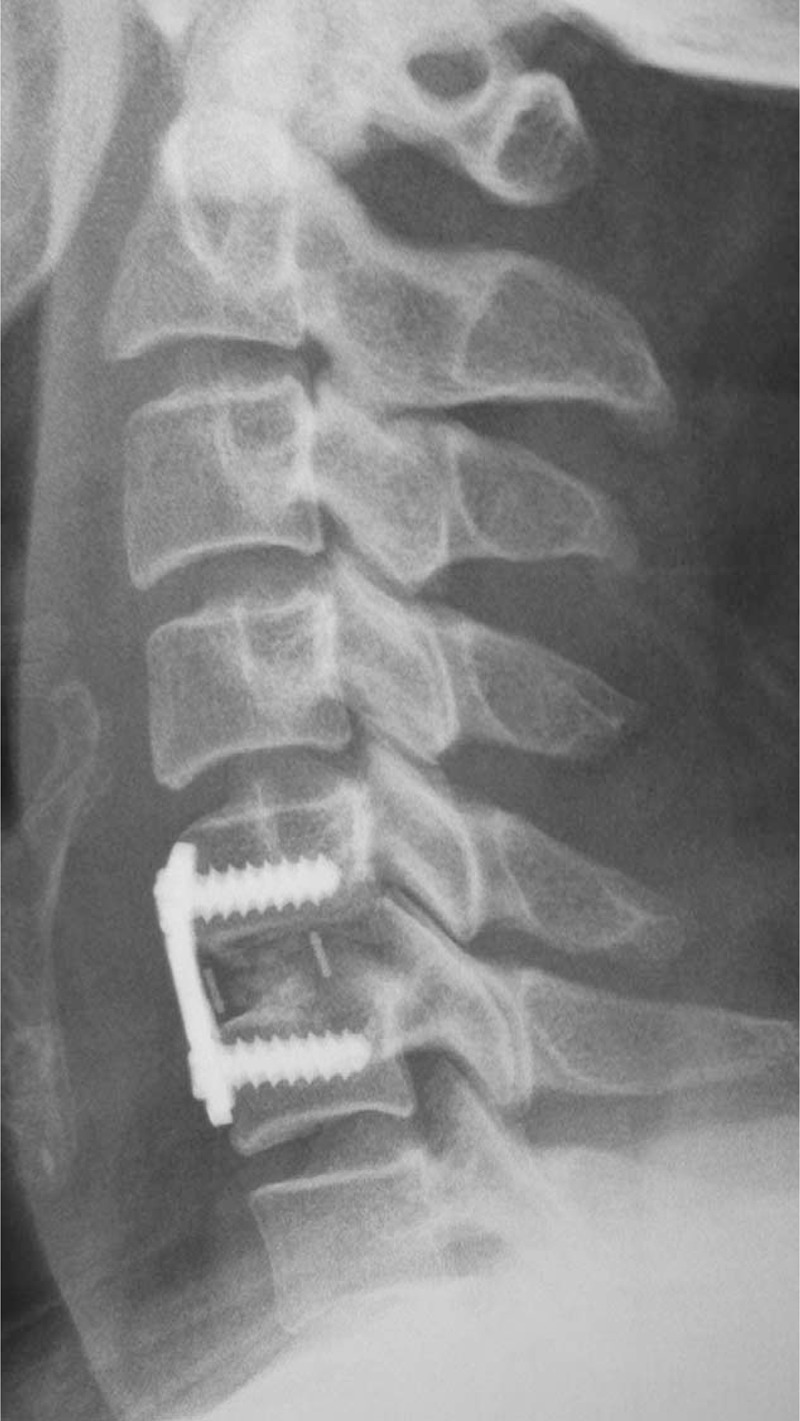
Lateral radiograph of cervical spine 3 months after operation showed anterior cervical plate fixation with cage fusion at C5/6 disc level.
FIGURE 4.

T2-weighted sagittal magnetic resonance imaging (MRI) 7 days after operation showed disappearance of cord compression at C5/6 disc level.
Case 2 underwent ACDF surgery at C5/6 and C6/7 levels. His symptoms of cervical vertigo completely disappeared, numbness of both upper limbs significantly released, and muscle strength of 4 limbs obviously increased. Similarly to case 1, his blood pressure also restored after the surgery without taking any antihypertensive drugs.
FOLLOW-UP AND OUTCOMES
Case 1 has undergone a follow-up of 12 months. Her cervical vertigo never recurred, and her blood pressure remained normal without the use of antihypertensive medications. Case 2 has undergone a follow-up of 14 months, the patient never had cervical vertigo anymore, and his blood pressure remained normal throughout (120–130/75–85 mmHg).
DISCUSSION
Clinical results indicated that ACDF can eliminate the concomitant vertigo symptoms in the 2 patients. However, the exact mechanisms of resolution of symptoms cannot be elucidated precisely. Because cervical spondylosis is a common disease, vertigo occurred in patients with cervical spondylosis is of particular importance.4 Cervical vertigo is attributed to many etiologies and several mechanisms.4,5 One previous study showed that vertigo was present in 50% of patients with cervical spondylosis,6 whereas another study identified cervical spondylosis as the cause of dizziness in 65% of elderly patients.7 It has been shown that the patients with cervical spondylosis complaining of vertigo have significant lower blood flow parameters than non-vertigo patients with cervical spondylosis.4 Insufficient blood supply to posterior circulation is called vertebrobasilar insufficiency. The most common complaint in patients with vertebrobasilar insufficiency is vertigo. Insufficient blood supply does not necessarily cause symptoms if there is sufficient collateral circulation, whereas a full range of symptoms commonly occur as a result of an insufficient terminal vessel.8,9 The vascular supply to the vestibulocochlear organ, being an end artery, makes this organ more susceptible to vertebrobasilar insufficiency. Neurons, axons, and hair cells in the vestibulocochlear system are known to respond to ischemia by depolarizing, causing transient hyperexcitability with ectopic discharges, manifesting as tinnitus, vertigo, and dizziness.4,5
It was hypothesized that vertebral artery insufficiency secondary to cervical spondylosis could result in vertigo.10 However, the mechanisms of vertigo caused by cervical spondylosis are not clear so far. The mechanical compression on vertebral artery from spurs of the Luschka joint was considered as a main mechanism. The reduction of vertebral artery flow can be more obvious with the rotation and hyperextension of the head.4 In our current study, we have not found any spur compression on vertebral artery. In addition, mechanical compression cannot explain some other symptoms such as palpitation, nausea, vomiting, etc. Recent clinical studies by Hong et al2 and Li et al3 demonstrated that the stimulation of the sympathetic nerve fibers other than the compression of the vertebral artery induces these symptoms such as vertigo, tinnitus, nausea, and vomiting.
Current study clearly indicates that hypertension can be associated with cervical spondylosis, as a secondary condition. The mechanisms are not well known. We speculate that the mechanisms of hypertension induced by cervical spondylosis could be the same as that of cervical vertigo. It is well known that cervical disc,11 dura mater, and posterior longitudinal ligament12–14 are rich in sympathetic fibers. Sympathetic nerve fibers distributed around the vertebral artery have been implicated in the autoregulation of vertebrobasilar artery blood flow and cerebral blood flow.13 It has been evidenced that sympathetic nerve activity withdraws the blood flow, whereas sympathectomy can increase it.13,15,16 A previous study investigated sympathetic and parasympathetic changes incited by the stimulation of nerves around the proximal vertebral artery in cat model and found subsequent papillary changes, pulse and blood pressure changes.13
Degenerative painful discs are always inflammatory discs.17 Elevation in levels of inflammatory cytokines has been detected in painful discs of humans, and thought to be related to degeneration and pain.18 The pathogenic change in the painful disc is featured with the formation of zones of vascularized granulation tissue and extensive innervation extending from the outer layer of the annulus fibrosus into the nucleus pulposus.19,20 Degenerative changes in the disc, such as loss of the normal structure and a mechanical load, can lead to abnormal motion, which can provoke mechanical stimulation.21 Mechanical stimuli, which are normally innocuous to disc nociceptors can, in certain circumstances such as inflammation, generate an amplified response termed peripheral sensitization.22
The vertebral arteries are mainly innervated by nerve fibers from the cervical sympathetic ganglia (13). Innervation in cervical disc is analogous to that in the lumbar spine, receiving innervation posteriorly from the sinuvetebral nerves, laterally from the vertebral nerve, and anteriorly from the sympathetic trunks.23 Recently, an animal study 24 revealed a reciprocal neural connection between cervical spinal and sympathetic ganglia. It seems likely that stimulation of sympathetic nerve fibers in the pathologically degenerative disc and surrounding tissues produce sympathetic excitation, and induce a sympathetic reflex to cause vertebrobasilar insufficiency and hypertension. Improvement of neurological function, resolution of vertigo, and recovery of blood pressure following surgery could be attributed to the excision of degenerative and herniated cervical disc, the decompression of the dura mater and posterior longitudinal ligament, and the stabilization of degenerated segment.
Another possible source of cervical spondylosis-induced hypertension is pain. Chronic neck pain is one of the major symptoms in patients with cervical spondylosis, whereas some studies have indicated that resting blood pressure levels may be elevated in patients with persistent pain. In healthy individuals, elevated blood pressure is associated with diminished acute pain sensitivity.25 These interactions are believed to reflect a homeostatic feedback loop that helps restore arousal levels in the presence of acutely painful stimuli. A role for baroreceptors in this feedback loop appears likely, with pain triggering sympathetically driven blood pressure increases, resulting in increased stimulation of baroreceptors, which in turn activates descending pain inhibitory pathways.26 Previous studies suggested that blood pressure/pain regulatory relationship may be substantially altered in chronic pain conditions.27 A retrospective study by Bruehl et al28 suggested that chronic pain could be associated with increased risk of hypertension. Their study found that over 39% of patients with chronic pain were diagnosed with clinical hypertension, compared with only 21% of pain-free internal medicine patients. Hypertension prevalence in the pain-free patients was comparable with national population values. They thought that chronic pain-related impairments in overlapping systems modulating both pain and blood pressure would result in a higher prevalence of clinically diagnosed hypertension in patients with chronic pain than in comparable pain-free patients. Our study indicates a possible relation between chronic neck pain and hypertension. If chronic neck pain could lead to hypertension through sympathetic arousal and failure of normal homeostatic pain regulatory mechanisms, early treatment for resolution of chronic neck pain may have a beneficial impact on cardiovascular disease risk in patients with cervical spondylosis.
CONCLUSION
We report here 2 patients of cervical spondylosis with concomitant cervical vertigo and hypertension that were treated successfully with anterior cervical discectomy and fusion. Stimulation of sympathetic nerve fibers in pathologically degenerative disc could produce sympathetic excitation, and induce a sympathetic reflex to cause cervical vertigo and hypertension. In addition, chronic neck pain could contribute to hypertension development through sympathetic arousal and failure of normal homeostatic pain regulatory mechanisms. Early treatment for resolution of symptoms of cervical spondylosis may have a beneficial impact on cardiovascular disease risk in patients with cervical spondylosis.
PATIENT CONSENT
Both patients gave consent to publish this case reports.
Footnotes
Abbreviations: ACDF = anterior cervical discectomy and fusion, MRI = magnetic resonance imaging.
No conflict of interest or financial interest was declared.
All patients gave consent to publish this case report.
REFERENCES
- 1.Fallah A, Akl EA, Ebrahim S, et al. Anterior cervical discectomy with arthroplasty versus arthrodesis for single-level cervical spondylosis: a systematic review and meta-analysis. PLOS One 2012; 7:e43407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hong L, Kawaguchi Y. Anterior cervical discectomy and fusion to treat cervical spondylosis with sympathetic symptoms. J Spinal Disord Tech 2011; 24:11–14. [DOI] [PubMed] [Google Scholar]
- 3.Li J, Jiang DJ, Wang XW, et al. Mid-term outcomes of anterior cervical fusion for cervical spondylosis with sympathetic symptoms. J Spinal Disord Tech 2013; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 4.Machaly SA, Senna MK, Sadek AG. Vertigo is associated with advanced degenerative changes in patients with cervical spondylosis. Clin Rheumatol 2011; 30:1527–1534. [DOI] [PubMed] [Google Scholar]
- 5.Brandt T, Baloh RW. Rotational vertebral artery occlusion. A clinical entity or various syndromes? Neurology 2005; 65:1156–1157. [DOI] [PubMed] [Google Scholar]
- 6.Olszewski J, Majak J, Pietkiewicz P, et al. The association between positional vertebral and basilar artery flow lesion and prevalence of vertigo in patients with cervical spondylosis. Otolaryngol Head Neck Surg 2006; 134:680–684. [DOI] [PubMed] [Google Scholar]
- 7.Colledeg NR, Barr-Hamilton RM, Lewis SJ, et al. Evaluation of investigations to diagnose the cause of dizziness in elderly people: a community based controlled study. BMJ 1996; 313:788–792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bayrak IK, Durmus D, Bayrak AO, et al. Effect of cervical spondylosis on vertebral arterial flow and its association with vertigo. Clin Rheumatol 2009; 28:59–64. [DOI] [PubMed] [Google Scholar]
- 9.Peng B, Pang X, Yang H. Chronic neck pain and episodic vertigo and tinnitus. Pain Med 2015; 16:200–202. [DOI] [PubMed] [Google Scholar]
- 10.Ptrek P, Reron E, Maga P, et al. A possible correlation between vertebral artery insufficiency and degenerative changes in the cervical spine. Eur Arch Otorhinolaryngol 1998; 255:437–440. [DOI] [PubMed] [Google Scholar]
- 11.Fujimoto K, Miyagi M, Ishikawa T, et al. Sensory and automonic innervation of the cervical intervertebral disc in rats: The pathomechanics of chronic discogenic neck pain. Spine 2012; 37:1357–1362. [DOI] [PubMed] [Google Scholar]
- 12.Johnson GM. The sensory and sympathetic nerve supply within the cervical spine: review of recent observations. Man The r 2004; 9:71–76. [DOI] [PubMed] [Google Scholar]
- 13.Wang Z, Wang X, Yuan W, et al. Degenerative pathological irritations to cervical PLL may play a role n presenting sympathetic symptoms. Med Hypotheses 2011; 77:921–923. [DOI] [PubMed] [Google Scholar]
- 14.Li J, Gu T, Yang H, et al. Sympathetic nerve innervation in cervical posterior longitudinal ligament as a potential causative factor in cervical spondylosis with sympathetic symptoms and preliminary evidence. Med Hypotheses 2014; 84:631–635. [DOI] [PubMed] [Google Scholar]
- 15.Cassaglia PA, Griffiths RI, Walker AM. Sympathetic withdraw augments cerebral blood flow during acute hypercapnia in sleeping lambs. Sleep 2008; 31:1729–1734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Heistad DD, Marcus ML, Gross PM. Effects of sympathetic nerves on cerebral vessels in dog, cat, and monkey. Am J Physiol 1978; 235:H544–552. [DOI] [PubMed] [Google Scholar]
- 17.García-Cosamalón J, del Valle ME, Calavia MG, et al. Intervertebral disc, sensory nerves and neurotrophins: who is who in discogenic pain? J Anat 2010; 217:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burke JG, Watson RW, McCormack D, et al. Intervertebral discs which cause low back pain secrete high levels of proinflammatory mediators. J Bone Joint Surg Br 2002; 84:196–201. [DOI] [PubMed] [Google Scholar]
- 19.Peng B, Wu W, Hou S, et al. The pathogenesis of discogenic low back pain. J Bone Joint Surg Br 2005; 87:62–67. [PubMed] [Google Scholar]
- 20.Peng B, Hao J, Hou S, et al. Possible pathogenesis of painful interverterbral disc degeneration. Spine 2006; 31:560–566. [DOI] [PubMed] [Google Scholar]
- 21.Choi YS. Pathophysiology of degenerative disc disease. Asian Spine J 2009; 3:39–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hadjipavlou AG, Tzermiadianos MN, Bogduk N, et al. The pathophysiology of disc degeneration. A critical review. J Bone Joint Surg Br 2008; 90:1261–1270. [DOI] [PubMed] [Google Scholar]
- 23.Onyewu O, Manchikanti L, Falco FJ, et al. An update of the appraisal of the accuracy and utility of cervical discography in chronic neck pain. Pain Physician 2012; 15:E777–E806. [PubMed] [Google Scholar]
- 24.Zuo J, Han J, Qiu S, et al. Neural reflex pathway between cervical spinal and sympathetic ganglia in rabbit: implication for pathogenesis of cervical vertigo. Spine J 2014; 14:1005–1009. [DOI] [PubMed] [Google Scholar]
- 25.Bruehl S, Chung OY. Interactions between the cardiovascular and pain regulatory systems: an updated review of mechanisms and possible alterations in chronic pain. Neurosci Biobehav Rew 2004; 28:395–414. [DOI] [PubMed] [Google Scholar]
- 26.Bruehl S, McCubbin JA, Harden RN. Theoretical review: Altered pain regulatory systems in chronic pain. Neurosci Biobehav Rew 1999; 23:877–890. [DOI] [PubMed] [Google Scholar]
- 27.Chung OY, Bruehl S. The impact of blood pressure and baroreflex sensitiveity on wind-up. Anesth Analg 2008; 107:1018–1025. [DOI] [PubMed] [Google Scholar]
- 28.Bruehl S, Chung OY, Jirjis JN, et al. Prevalence of clinical hypertension in patients with chronic pain compared to nonpain general medical patients. Clin J Pain 2005; 21:147–153. [DOI] [PubMed] [Google Scholar]


