Abstract
Displaced midshaft clavicle fractures are frequent injuries. There are 3 treatment methods including conservative treatment, plate fixation, and intramedullary pin fixation. However, which is the best treatment remains a topic of debate.
To establish the optimum treatment for displaced midshaft clavicular fractures, we did a network meta-analysis to compare 3 treatments in terms of postoperative nonunion and infection.
We searched PubMed, the Cochrane Library, and Embase for relevant randomized controlled trials (RCTs) until the end of October 2014. Two investigators independently reviewed the abstract and full text of eligible studies and extracted information. We used WinBUGS 1.4 (Imperial College School of Medicine at St Mary's, London) to perform our Bayesian network meta-analysis. We used the graphical tools in STATA12 (StataCorp, Texas) to present the results of statistical analyses of WinBUGS14. Nonunion and infection were presented as odd ratios (ORs) with 95% confidence intervals (CIs). We also presented the results using surface under the cumulative ranking curve (SUCRA). A higher SUCRA value suggests better results for respective treatment method.
Thirteen RCTs were included in our network meta-analysis, with a total of 894 patients randomized to receive 1 of 3 treatments. Nonunion rates were 0.9%, 2.4%, and 11.4% for intramedullary pin fixation, plate fixation, and conservative method, respectively. Nonunion occurred more commonly in patients treated with conservative method than in patients treated with either plate fixation (OR, 0.18; 95% CI, 0.05–0.46) or intramedullary pin fixation (OR, 0.12; 95% CI, 0.01–0.50). There was no significant difference between plate and intramedullary pin fixation in nonunion (OR, 3.64; 95% CI, 0.31–17.27). Furthermore, SUCRA probabilities were 87.8%, 62.0%, and 0.2% for intramedullary pin fixation, plate fixation, and conservative method, respectively. Infection rates were 3.6% and 3.9% for intramedullary pin fixation and plate fixation, respectively. There was no significant difference between plate and intramedullary pin fixation in infection (OR, 3.64; 95% CI, 0.31–17.27). SUCRA probabilities were 46.5% and 8.5% for intramedullary pin and plate fixation, respectively.
Our network meta-analysis suggested that intramedullary pin fixation is the optimum treatment method for displaced midshaft clavicle fracture because of the low probabilities of nonunion and infection.
INTRODUCTION
Clavicle fractures are frequent injuries, accounting for 2.6% to 4% of all fracture in adults.1 The most common type of clavicle fracture is the midshaft fracture. It frequently results in short-term disability and pain, eventually causing longer-term deformity and disability.2,3 Conservative interventions are widely used and are recommended for treating midshaft clavicle fractures. Traditionally, displaced clavicle fractures are treated conservatively with a figure-of-eight bandage or a sling.4,5 Recently, surgery treatment methods have been increasingly used for displaced midshaft fracture of the clavicle, mainly involving plate or intramedullary pin fixation.
Some randomized controlled trials (RCTs)6–8 have been published regarding surgical treatment versus conservative treatment and comparison of different operation methods. Individual RCTs may be underpowered to show subtle clinical differences because of the smaller patient number. Several meta-analyses or systematic reviews comparing surgical versus conservative interventions for the treatment of midshaft clavicular fracture have also been published.9–11 In addition, 2 systematic reviews also compared the difference between plate and intramedullary pin fixation.12,13 However, traditional meta-analysis methods only directly compare 2 different methods. When comparing ≥3 treatments, it is impossible. Bayesian network meta-analysis is known as mixed treatment comparison and it could combine direct and indirect comparisons to resolve this problem.
To establish the optimum treatment for displaced midshaft clavicular fractures, we did a network meta-analysis to compare 3 treatments including conservative treatment, plate fixation, and intramedullary pin fixation in terms of postoperative nonunion and infection.
METHOD
We did our systematic review in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.14 Ethical approval and informed patient consent was not required as this study was a literature review and had no direct patient contact or influence on patient care.
Search Strategy
We searched PubMed, the Cochrane Library, and Embase for relevant RCTs until the end of October 2014. The following keywords were used: “clavicle” or “clavicular,” “fracture,” and “random”∗. No language or publication restrictions were applied. Articles in languages other than English were translated with the help of medically knowledgeable speakers.
Selection Criteria
We systematically reviewed the literature according to the following criteria: a target population of displaced midshaft clavicular fractures in adults; RCTs evaluating 2 or 3 of the 3 treatments including plate fixation, intramedullary pin fixation, and conservative treatment; and a minimum of 12-month follow-up. We excluded studies if they contained only 1 or none of the 3 treatments. Two authors independently scanned records to exclude irrelevant studies and identify trials that met the eligibility criteria. Differences in opinion between authors were resolved by discussion and consultation with a third author.
Data Extraction
Two investigators independently reviewed the abstract and full text of eligible studies and extracted information into an electronic database, including publication year, patients characteristics, random methods, inclusion and exclusion criteria, treatment methods, and outcomes (nonunion and infection). The primary outcome was the incidence of nonunion. Nonunion was defined as an unsuccessful healing of the bone after 6 months. We also compared the incidence of infection between plate fixation and intramedullary pin fixation.
Assessment of Methodological Quality
The risk of bias was assessed independently by 2 investigators with the Detsky scale.15 Disagreement was resolved through discussing. The Detsky score was used because it has been used previously to determine the methodological quality of published orthopedic RCTs and has shown good consistency and reliability. A quality score of >75% (≥16 scores) was considered to indicate high quality, scores >50% and <75% (11–15 scores) indicated moderate quality, and scores <50% (≤10 scores) indicated low quality, which is consistent with the previous research.16–19
Data Analysis
We used WinBUGS1.4 (Imperial College School of Medicine at St Mary's, London) to perform our Bayesian network meta-analysis using the statistic method described by Chaimani et al.20 Furthermore, we used the graphical tools in STATA12 (StataCorp, Texas) to present the results of statistical analyses of WinBUGS1.4. Funnel plot was used to assess the presence of small-study effects in our meta-analysis. A funnel plot is a scatterplot of study effect size versus some measure of its precision. Inconsistency refers to differences between direct and various indirect effect estimates for the same comparison. To assess inconsistency, we estimated the inconsistency factors in closed loop based on the method described by Chaimani et al.20 Nonunion and infection were presented as odd ratios (ORs) with 95% confidence intervals (CIs). This network meta-analysis could provide information about ranking of all evaluated interventions for the outcome.21 We also presented the results using surface under the cumulative ranking curve (SUCRA). A higher SUCRA value suggests better results for respective treatment method.21
RESULTS
Search Results
We identified 171 potentially relevant references from database searches after screening out repeated literature (Figure 1). Of these references, we excluded 140 at the initial screening through reviewing title and abstract. We retrieved the full text of potential articles. Fifteen eligible publications7,8,22–34 reporting 13 RCTs were included in our network meta-analysis, with a total of 894 patients randomized to receive 1 of 3 treatments. We summarized all included studies in Table 1 . Figure 2 shows all comparisons within the network.
FIGURE 1.
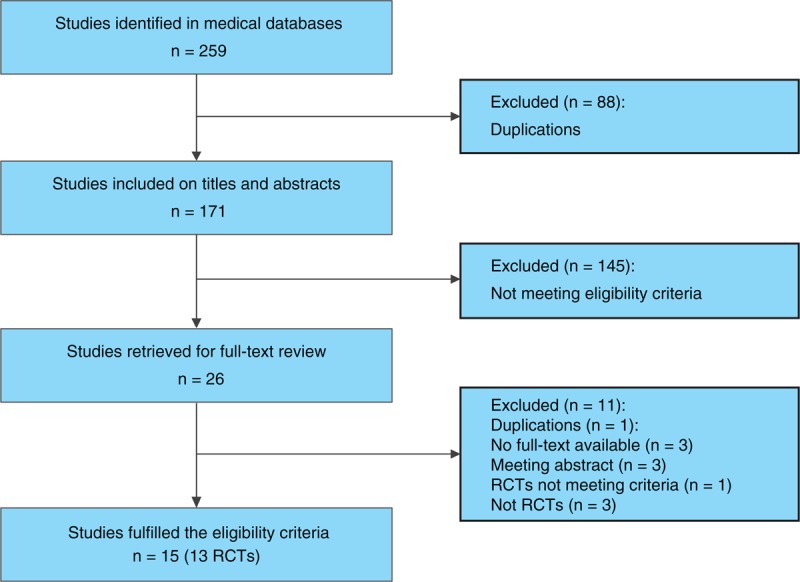
Flow diagram depicting study selection for inclusion in meta-analysis. RCT = randomized controlled trial.
TABLE 1.
Characteristics of the 13 Included Studies
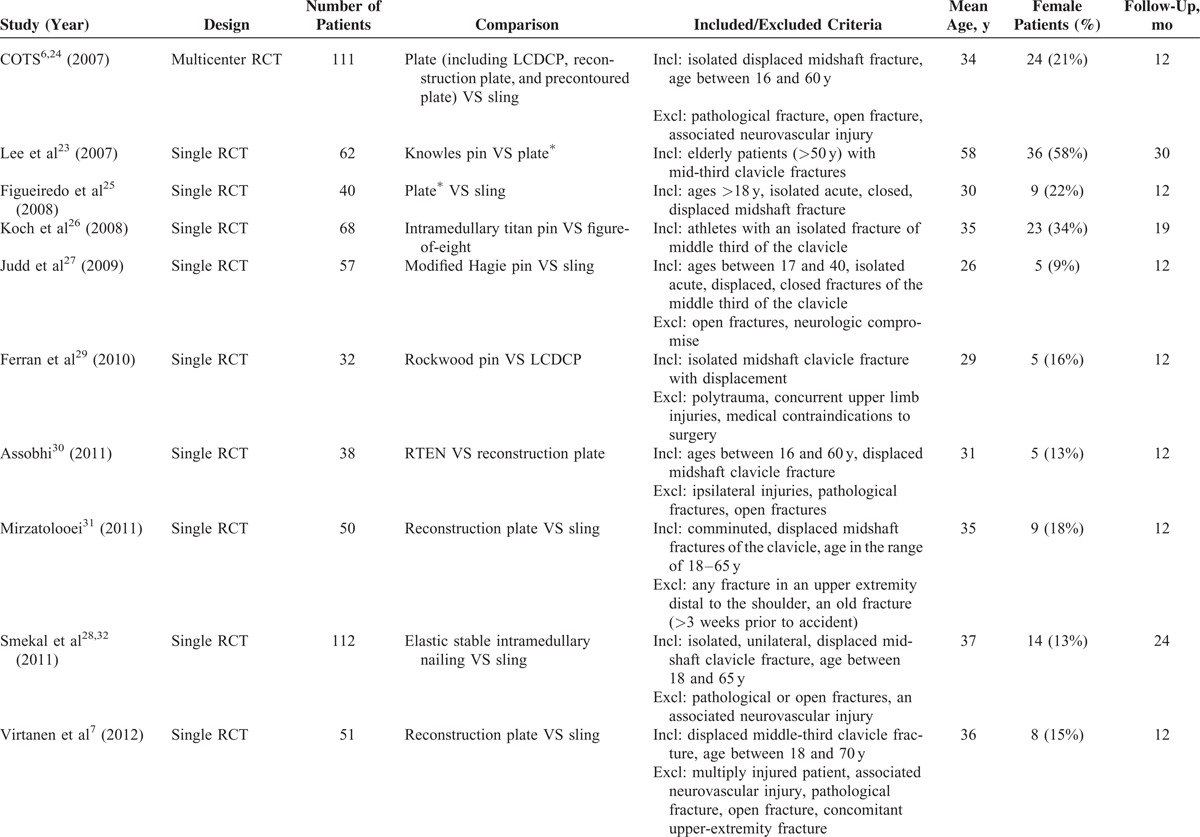
FIGURE 2.
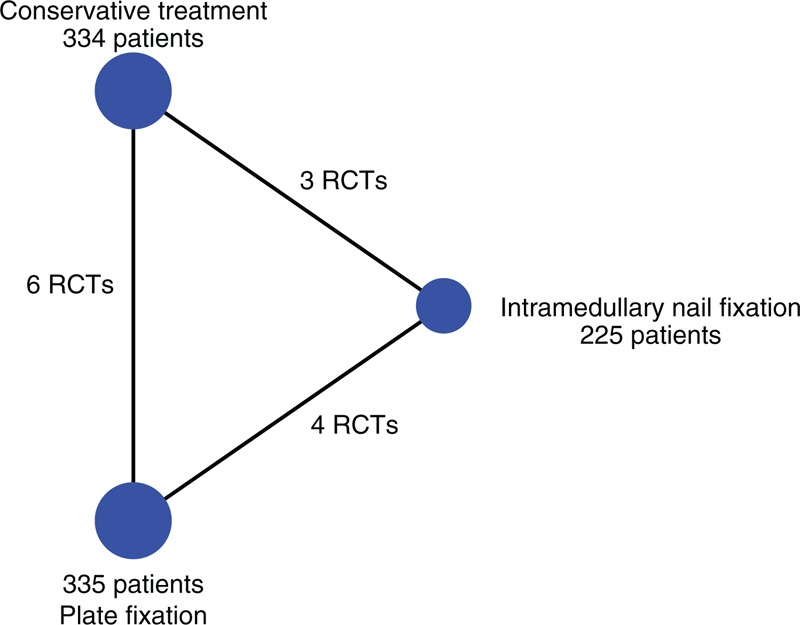
Network of the comparisons for the Bayesian network meta-analysis. RCT = randomized controlled trial.
Methodological Quality
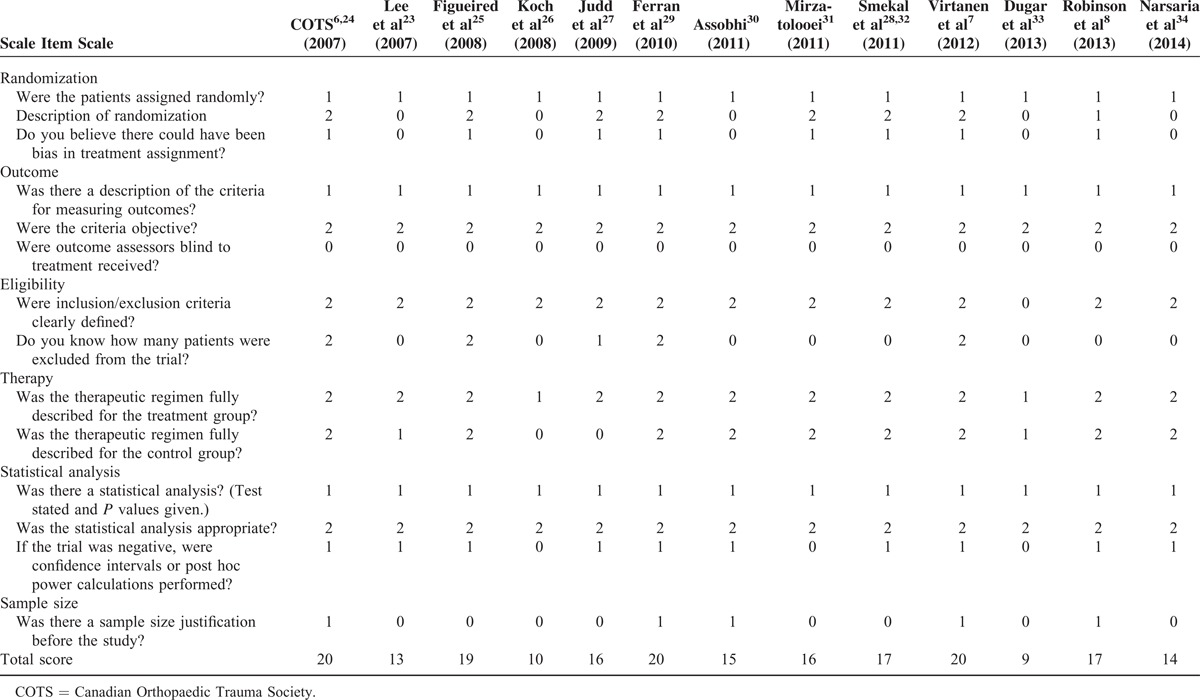
The median Detsky scores for the included trials were 15.8. The overall methodological quality was moderate. The detailed Detsky quality scores of the included studies are listed in Table 2.
TABLE 1 (Continued).
Characteristics of the 13 Included Studies
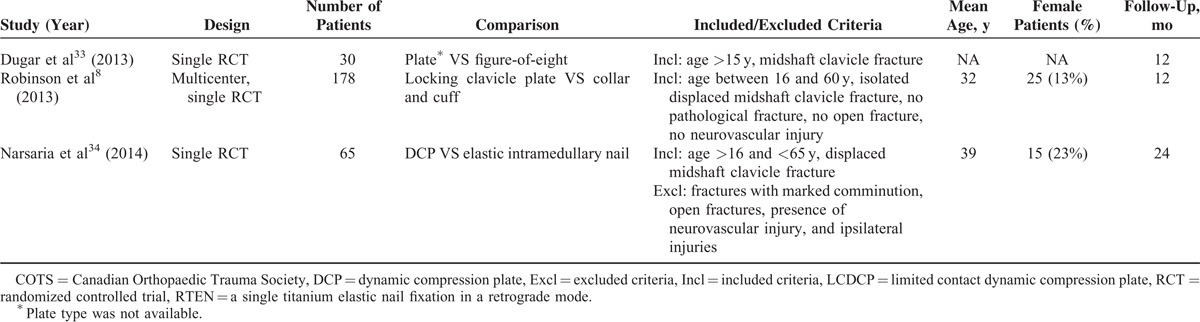
TABLE 2.
Detsky Quality Scores of the Included Randomized Controlled Trials
Inconsistency Test
In Figure 3, the funnel plot is symmetrical to the line and it implies that there are not small-study effects in our network meta-analysis. Figure 4 shows that there is no significant inconsistency as its CIs are compatible with zero.
FIGURE 3.
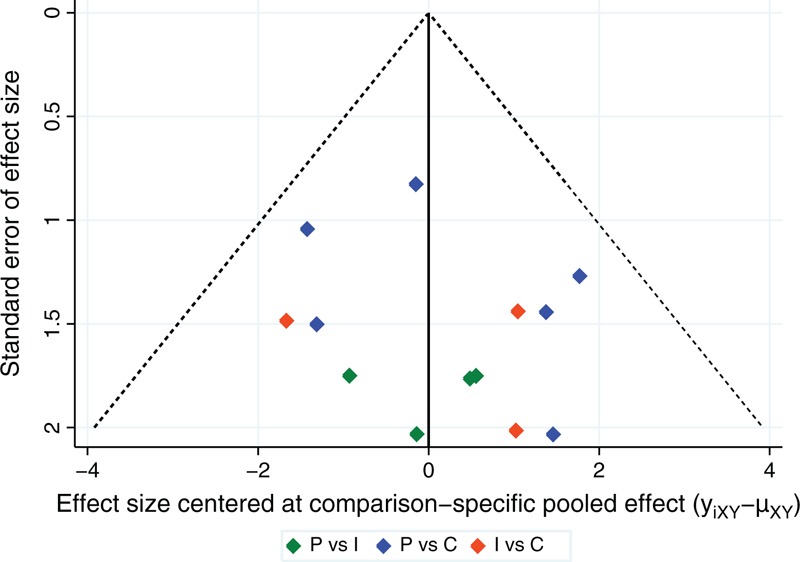
Funnel plot of this network meta-analysis. C = conservative treatment, I = intramedullary pin fixation, P = plate fixation.
FIGURE 4.
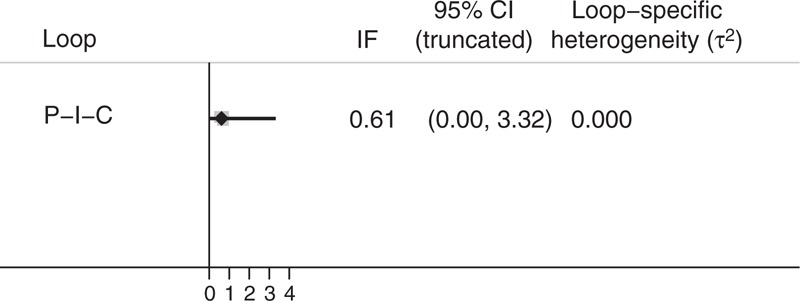
Inconsistency plot of this network meta-analysis. C = conservative treatment, I = intramedullary pin fixation, IFs = inconsistency factors, P = plate fixation.
Nonunion
The nonunion was reported in all 13 included trials. Nonunion rates were 0.9%, 2.4%, and 11.4% for intramedullary pin fixation, plate fixation, and conservative method, respectively. Nonunion occurred more commonly in patients treated with conservative method than in patients treated with either plate fixation (OR, 0.18; 95% CI, 0.05–0.46) or intramedullary pin fixation (OR, 0.12; 95% CI, 0.01–0.50) (Figure 5). There was no significant difference between plate and intramedullary pin fixation in nonunion rate (OR, 3.64; 95% CI, 0.31–17.27). Furthermore, SUCRA probabilities were 87.8%, 62.0%, and 0.2% for intramedullary pin fixation, plate fixation, and conservative method, respectively (Figure 6). In Figure 7, we summarized the ranking of the 3 treatment methods in terms of the probability of nonunion.
FIGURE 5.
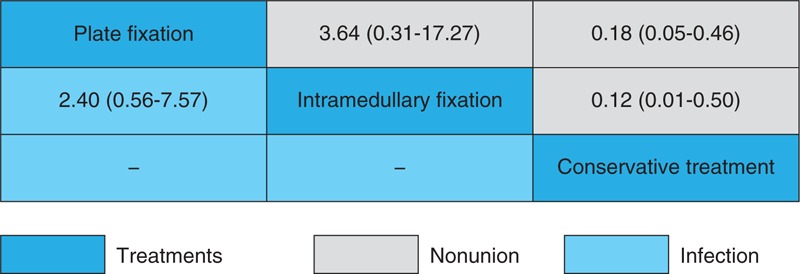
Odd ratios with 95% confidence intervals for nonunion and infection.
FIGURE 6.
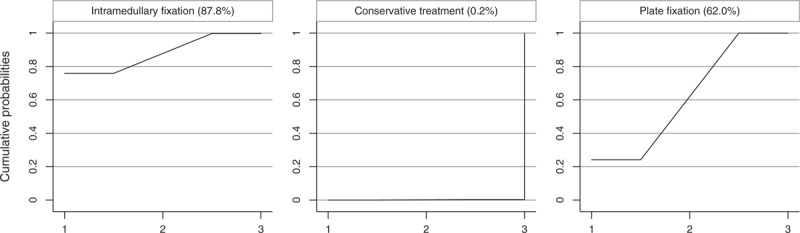
Surface under the cumulative ranking curves for nonunion.
FIGURE 7.
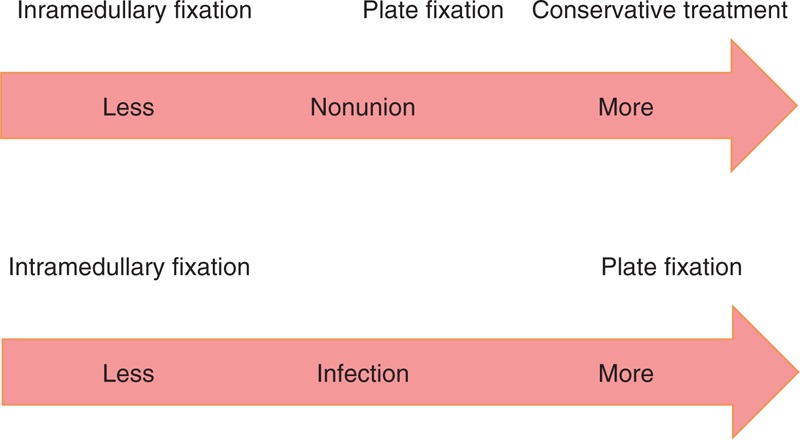
Ranking of treatments in terms of nonunion and infection.
Infection
Infection rates were 3.6% and 3.9% for intramedullary pin fixation and plate fixation, respectively. The direct and indirect result of the meta-analysis showed that there was no significant difference between plate and intramedullary pin fixation in infection rate (OR, 3.64; 95% CI, 0.31–17.27) (Figure 5). Furthermore, SUCRA probabilities were 46.5% and 8.5% for intramedullary pin fixation and plate fixation, respectively (Figure 8). In Figure 7, we summarized the ranking of the 2 treatment methods in terms of the probability of infection.
FIGURE 8.
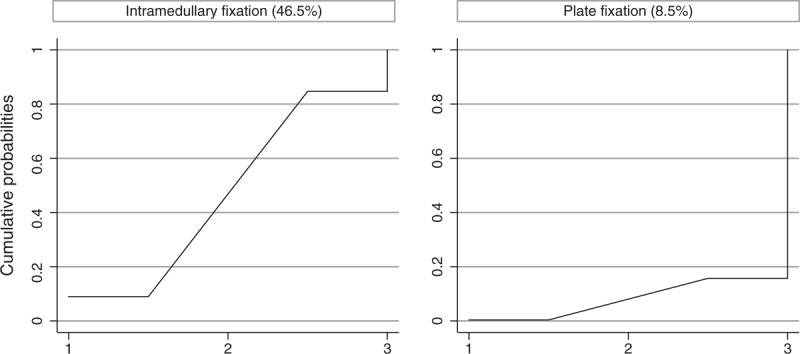
Surface under the cumulative ranking curves for infection.
DISCUSSION
The best treatment for displaced midshaft clavicle fractures remains a topic of debate. Many studies showed a high risk for nonunion after conservative treatment.2,3,35 Operative treatment is playing a more and more important role. Plate fixation and intramedullary pin fixation are main operation methods. Recently, several meta-analyses regarding the management of displaced midshaft clavicle fracture have been published.10–12 Most of them focused on the comparison between operative and nonoperative treatments. However, synthesis of present evidence using traditional meta-analysis methods is a challenging task because there are 3 major treatment methods. No network meta-analysis concerning this topic was published.
This is the first network meta-analysis that assesses the treatments of displaced midshaft clavicle fracture. Network meta-analysis is a well-established research by comparing different treatments. Thirteen RCTs were included in our network meta-analysis, and 4 of them directly compared plate fixation with intramedullary pin. When comparing with conservative treatment, either plate or intramedullary pin significantly decreased the postoperative nonunion rate. Although there was no significant difference between pin and plate based on OR value, the results of SUCRA ranking suggested that intramedullary pin fixation had the lower probability of nonunion than plate fixation (Figures 6 and 7). SUCRA results also suggested that intramedullary pin fixation had a lower probability of infection than plate fixation (Figures 7 and 8). Hence, we concluded that intramedullary pin fixation is the preferred choice for treating displaced midshaft clavicular fractures.
Intramedullary pin fixation had a lower rate of nonunion and infection than plate fixation, which can be explained by less damaged blood supply during the operation. Favorable soft tissue and adequate blood supply are the critical factors for the fracture consolidation. Although plate fixation is better to resist bending and torsional forces than intramedullary pin fixation regarding biomechanics,36 it needs greater exposure and more extensive soft tissue stripping that may affect fracture healing and increase the risk of infection. Intramedullary pin fixation is a minimally invasive alternative that avoids those problems encountered with plating. Furthermore, the removal of plates necessitated new admissions, general anesthesia, and another large-sized incision, whereas nail removal was performed under local anesthesia with minimal sedation and a tiny incision over the tip of the nail. On the other hand, plate fixation has absolute stability, whereas intramedullary pin fixation provides elastic fixation that is an advantage to fracture healing.
We did not compare the incidence of malunion and shoulder scores due to the lack of unified evaluation criteria. Some studies reported symptomatic malunion,22,24,33 but radiologic malunion was assessed in other studies.28,31 Similarly, although all RCTs reported the shoulder scores in their studies, there were multiple shoulder scores among them including the American Shoulder and Elbow Surgeons score,34 Constant score,8,31,34 Disabilities of the Arm, Shoulder, and Hand score,22,24,33 and Oxford Shoulder score.29 Furthermore, some studies did not report the detailed data of mean and standard deviation. Therefore, we did not pool these data to ensure the rationality and validity of this meta-analysis.
The present analysis included more RCTs through an extensive search. The enlarged sample size provided more accurate estimates of effects. The main limitation of the study was that we could not compare the specific fixators. For example, there were several types of intramedullary pins in the included studies such as the elastic intramedullary pin, Rockwood pin, and Knowles pin. It is noteworthy that there were neither small-study effects nor was there significant inconsistency in our network meta-analysis.
CONCLUSION
In conclusion, our network meta-analysis suggested that intramedullary pin fixation is the optimum treatment method for displaced midshaft clavicle fracture because of the low probabilities of nonunion and infection.
Footnotes
Abbreviations: CI = confidence interval, OR = odd ratio, SUCRA = surface under the cumulative ranking curve.
JW, X-HM, Z-MG, and J-GZ contributed equally to this study as first authors.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Robinson CM. Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Joint Surg Br 1998; 80:476–484. [DOI] [PubMed] [Google Scholar]
- 2.McKee MD, Pedersen EM, Jones C, et al. Deficits following nonoperative treatment of displaced midshaft clavicular fractures. J Bone Joint Surg Am 2006; 88:35–40. [DOI] [PubMed] [Google Scholar]
- 3.Hill JM, McGuire MH, Crosby LA. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg Br 1997; 79:537–539. [DOI] [PubMed] [Google Scholar]
- 4.Postacchini R, Gumina S, Farsetti P, et al. Long-term results of conservative management of midshaft clavicle fracture. Int Orthop 2010; 34:731–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nordqvist A, Petersson CJ, Redlund-Johnell I. Mid-clavicle fractures in adults: end result study after conservative treatment. J Orthop Trauma 1998; 12:572–576. [DOI] [PubMed] [Google Scholar]
- 6.Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial. J Bone Joint Surg Am 2007; 89:1–10. [DOI] [PubMed] [Google Scholar]
- 7.Virtanen KJ, Remes V, Pajarinen J, et al. Sling compared with plate osteosynthesis for treatment of displaced midshaft clavicular fractures: a randomized clinical trial. J Bone Joint Surg Am 2012; 94:1546–1553. [DOI] [PubMed] [Google Scholar]
- 8.Robinson CM, Goudie EB, Murray IR, et al. Open reduction and plate fixation versus nonoperative treatment for displaced midshaft clavicular fractures: a multicenter, randomized, controlled trial. J Bone Joint Surg Am 2013; 95:1576–1584. [DOI] [PubMed] [Google Scholar]
- 9.Evaniew N, Simunovic N, McKee MD, et al. Cochrane in CORR(R): surgical versus conservative interventions for treating fractures of the middle third of the clavicle. Clin Orthop Relat Res 2014; 472:2579–2585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lenza M, Buchbinder R, Johnston RV, et al. Surgical versus conservative interventions for treating fractures of the middle third of the clavicle. Cochrane Database Syst Rev 2013; 6:CD009363. [DOI] [PubMed] [Google Scholar]
- 11.McKee RC, Whelan DB, Schemitsch EH, et al. Operative versus nonoperative care of displaced midshaft clavicular fractures: a meta-analysis of randomized clinical trials. J Bone Joint Surg Am 2012; 94:675–684. [DOI] [PubMed] [Google Scholar]
- 12.Barlow T, Beazley J, Barlow D. A systematic review of plate versus intramedullary fixation in the treatment of midshaft clavicle fractures. Scott Med J 2013; 58:163–167. [DOI] [PubMed] [Google Scholar]
- 13.Houwert RM, Wijdicks FJ, Steins Bisschop C, et al. Plate fixation versus intramedullary fixation for displaced mid-shaft clavicle fractures: a systematic review. Int Orthop 2012; 36:579–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 2010; 8:336–341. [DOI] [PubMed] [Google Scholar]
- 15.Detsky AS, Naylor CD, O’Rourke K, et al. Incorporating variations in the quality of individual randomized trials into meta-analysis. J Clin Epidemiol 1992; 45:255–265. [DOI] [PubMed] [Google Scholar]
- 16.Zhao JG, Zhao L, Jiang YX, et al. Platelet-rich plasma in arthroscopic rotator cuff repair: a meta-analysis of randomized controlled trials. Arthroscopy 2015; 31:125–135. [DOI] [PubMed] [Google Scholar]
- 17.Zhao JG, Kan SL, Zhao L, et al. Percutaneous first annular pulley release for trigger digits: a systematic review and meta-analysis of current evidence. J Hand Surg Am 2014; 39:2192–2202. [DOI] [PubMed] [Google Scholar]
- 18.Zhao JG, Wang J, Zhang P. Is lateral pin fixation for displaced supracondylar fractures of the humerus better than crossed pins in children? Clin Orthop Relat Res 2013; 471:2942–2953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang J, Zhao JG, Liang CC. Percutaneous release, open surgery, or corticosteroid injection, which is the best treatment method for trigger digits? Clin Orthop Relat Res 2013; 471:1879–1886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chaimani A, Higgins JP, Mavridis D, et al. Graphical tools for network meta-analysis in STATA. PLoS One 2013; 8:e76654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Salanti G, Ades AE, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol 2011; 64:163–171. [DOI] [PubMed] [Google Scholar]
- 22.McKee MD, Kreder HJ, Mandel S, et al. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures: A multicenter, randomized clinical trial. J Bone Joint Surg Series A 2007; 89:1–10. [DOI] [PubMed] [Google Scholar]
- 23.Lee YS, Lin CC, Huang CR, et al. Operative treatment of midclavicular fractures in 62 elderly patients: Knowles pin versus plate. Orthopedics 2007; 30:959–964. [DOI] [PubMed] [Google Scholar]
- 24.Altamimi SA, McKee MD. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. Surgical technique. J Bone Joint Surg Am 2008; 90 suppl 2, pt 1:1–8. [DOI] [PubMed] [Google Scholar]
- 25.Figueiredo EA, Neves EJ, Yoshizawa H, et al. Prospective randomized study comparing surgical treatments using anterior plate and non-surgical management of fractures of the middle third of the clavicle. Rev Bras Ortop 2008; 43:419–425. [Google Scholar]
- 26.Koch HJ, Raschka C, Tonus C, et al. The intramedullary osteosynthesis of the diaphyseal fracture of the clavicle compared to conservative treatment. Deutsche Zeitschrift Sportmed 2008; 59:91–94. [Google Scholar]
- 27.Judd DB, Pallis MP, Smith E, et al. Acute operative stabilization versus nonoperative management of clavicle fractures. Am J Orthop (Belle Mead, NJ) 2009; 38:341–345. [PubMed] [Google Scholar]
- 28.Smekal V, Irenberger A, Struve P, et al. Elastic stable intramedullary nailing versus nonoperative treatment of displaced midshaft clavicular fractures-a randomized, controlled, clinical trial. J Orthop Trauma 2009; 23:106–112. [DOI] [PubMed] [Google Scholar]
- 29.Ferran NA, Hodgson P, Vannet N, et al. Locked intramedullary fixation vs plating for displaced and shortened mid-shaft clavicle fractures: a randomized clinical trial. J Shoulder Elbow Surg 2010; 19:783–789. [DOI] [PubMed] [Google Scholar]
- 30.Assobhi JE. Reconstruction plate versus minimal invasive retrograde titanium elastic nail fixation for displaced midclavicular fractures. J Orthop Traumatol 2011; 12:185–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mirzatolooei F. Comparison between operative and nonoperative treatment methods in the management of comminuted fractures of the clavicle. Acta Orthop Traumatol Turcica 2011; 45:34–40. [DOI] [PubMed] [Google Scholar]
- 32.Smekal V, Irenberger A, Attal RE, et al. Elastic stable intramedullary nailing is best for mid-shaft clavicular fractures without comminution: results in 60 patients. Injury 2011; 42:324–329. [DOI] [PubMed] [Google Scholar]
- 33.Dugar N, Hossain E, Bandyopadhyay U, et al. A comparative study of non-operative and operative management in fracture clavicle. J Indian Med Assoc 2013; 111:806–809. [PubMed] [Google Scholar]
- 34.Narsaria N, Singh AK, Arun GR, et al. Surgical fixation of displaced midshaft clavicle fractures: elastic intramedullary nailing versus precontoured plating. J Orthop Traumatol 2014; 15:165–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gossard JM. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg Br 1998; 80:558. [PubMed] [Google Scholar]
- 36.Renfree T, Conrad B, Wright T. Biomechanical comparison of contemporary clavicle fixation devices. J Hand Surg Am 2010; 35:639–644. [DOI] [PubMed] [Google Scholar]


