Supplemental Digital Content is available in the text
Abstract
About 1% of the general population receives long-term systemic glucocorticoids. The monitoring provided to these patients is unknown.
We conducted a population-based cohort study using The Health Improvement Network database. A total of 100,944 adult patients prescribed systemic glucocorticoids for >3 months between January 2000 and December 2012 were studied. The monitoring done before prescribing glucocorticoid therapy and during exposure to the drug was examined. This included measurement of body weight, blood pressure, lipids, glucose and potassium levels, referrals for dual-energy X-ray absorptiometry (DEXA-scan) or to an ophthalmologist/optician, and vaccinations. We assessed factors associated with the odds of being monitored before and during exposure.
Before glucocorticoid initiation, weight and blood pressure were monitored in < 20% and < 50% of patients, respectively. Glucose and lipid levels were monitored in less than one-third of the patients, while DEXA-scan and eye monitoring were offered to <15% of them. Vaccination against flu and pneumococcus was given to 57% and 46% of the patients, respectively. During exposure to the drug, <60% of patients who were prescribed the drug for more than a year had their weight, glucose, or lipid levels recorded at least once and <25% of patients were referred at least once for DEXA-scan or screening for eye diseases. Overall, the odds of being monitored were higher in older patients and in those with comorbidities. There were variations in the level of monitoring provided across the UK, but the monitoring has improved over the last 12 years.
Although the extent of monitoring of people on long-term glucocorticoids has improved over time, the overall monitoring provided is not satisfactory, particularly in young patients and those without comorbidities.
INTRODUCTION
About 1% of the general population receives systemic glucocorticoids.1,2 Long-term oral glucocorticoid prescriptions have increased by 34% over the past 20 years.1 Most patients exposed to the drug for many months or years are at high risk of developing adverse events. Apart for osteoporosis, little data are available on the best way to prevent or manage other glucocorticoid-induced adverse events. For example, there is little focus on the prevention and management of neuropsychiatric disorders, lipodystrophic features, or cutaneous disorders even though they occur in nearly 50% of the patients.3 This lack of scientific data could explain the wide variability in the advice and monitoring offered by physicians who prescribe glucocorticoids to patients. Whilst some recommend a low-sodium, high-protein, and low-sugar diet, others do not.4,5 Similarly, some offer advice on regular physical exercise and/or prescribe potassium supplementation while other do not.4,5 In light of the numbers exposed to prescribed glucocorticoids and the variability of clinical practice coupled with the lack of an evidence-based on the management of its adverse events, experts have published consensus recommendations on monitoring and managing people prescribed glucocorticoid therapy.6–8 These recommendations offer advice on the monitoring to be done before and during treatment. This includes measurements of weight, blood pressure, lipids, and glucose levels. In the UK, much of the long-term prescribing of glucocorticoids is done in general practice. We therefore aimed to examine the monitoring provided to patients prescribed long-term glucocorticoid therapy in this setting. We also aimed to assess the factors associated with the odds of being monitored according to the available recommendations.
MATERIAL AND METHODS
Data Source: The Health Improvement Network
Approximately 98% of the population in the UK is registered with a general practitioner.9 The Health Improvement Network (THIN) is a database of electronic medical records from UK general practices. Participating general practitioners systematically and prospectively retrieve and enter clinical information on patients, including demographics data, diagnoses, and prescriptions so that the database provides a longitudinal medical record for each patient. THIN is representative of the UK population, and comparisons to external statistics and other independent studies have shown that both the clinical diagnostic and prescribing information is well recorded and accurate.10–13 The data are entered in routine general practice and therefore reflect “real-life” clinical care. For this study, we arbitrarily chose to use data from January 1, 2000 to December 31, 2012 from 554 general practices. We excluded events that occurred within 6 months following registration in order to include only incident cases of outcomes.14
Prescriptions of Glucocorticoids
We included people aged 18 years and older who were prescribed systemic glucocorticoids either orally or by intramuscular or intravenous injection. This included prednisolone, prednisone, dexamethasone, triamcinolone, betamethasone, methylprednisolone, and deflazacort. We selected only people prescribed systemic glucocorticoids for at least 3 months. For people who received multiple courses of systemic glucocorticoids during this time period, we included only the first one. In the case of multiple consecutive prescriptions, we considered that the prescriptions were part of a single course of therapy if the previous prescription was issued <3 months earlier. For each course, the treatment time was defined as the time from the first to the last prescription plus the duration of the last prescription. We calculated the initial average daily dosage by multiplying the number of tablets initially prescribed by the dose/tablets (calculated in prednisone-equivalent) and this was then divided by the number of days for which the drug was prescribed. People taking substitutive glucocorticoids for adrenal insufficiency were excluded.
Monitoring Before Glucocorticoid Exposure
We extracted data on entries of weight, blood pressure (measurement at the practice or at home or referral to a hypertension clinic), lipids (cholesterol and/or triglycerides levels), glucose (blood or urine glucose or glycosylated hemoglobin), and serum potassium levels, and bone mineral density assessment (referral for dual energy X-ray absorptiometry [DEXA-scan] or to an osteoporosis clinic). We also searched for assessments of vision by the general practitioner or for referrals to an ophthalmologist or an optician and we extracted data on flu and/or pneumococcal vaccines. We took into account all entries of blood pressure, weight, blood glucose, and serum potassium during the 3 months before exposure. In the case of blood glucose and serum potassium, we also took into account entries made up to 2 weeks after glucocorticoid initiation, as these tests may have been ordered at the time of initiation of therapy but the results received a few days later. We chose to extend the period of baseline testing to 1 year before to 2 weeks after initiation of therapy for lipids. Regarding bone mineral density testing and eye testing, the period was extended to 1 year before to 2 months after initiation of treatment in order to reflect the delay in the reporting of these parameters when ordered by a clinician. For vaccines, we searched for any flu vaccine within the year before glucocorticoid initiation and for any pneumococcal vaccine anytime before exposure.
Monitoring During Glucocorticoid Exposure
The parameters described earlier (see “Monitoring Before Glucocorticoid Exposure” section) were also extracted during exposure to glucocorticoid therapy, excluding the first 2 weeks of exposure for glucose, lipids, or serum potassium levels and the first 2 months of exposure for DEXA-scan and eye testing.
Covariates of Interest
The indications for glucocorticoid treatment were obtained by reviewing the medical diagnosis recorded on the same date when treatment was started. If no medical diagnosis was recorded on this date, we searched for relevant chronic conditions recorded closest to when the prescription was issued, up to 1 year before or 1 year after. We then focused our analysis on 5 diseases, that is, rheumatoid arthritis, polymyalgia rheumatica/giant cell arteritis, asthma, chronic obstructive pulmonary diseases, and inflammatory bowel diseases (ie, Crohn's disease and ulcerative colitis). We chose to study these diseases because they are diseases frequently requiring long-term glucocorticoid therapies1 and they reflect different types of populations exposed to the drug. We also searched the medical and therapeutic records of the patients before the initiation of glucocorticoids to assess their past medical history for hypertension, diabetes, dyslipidemia, osteoporosis, cataract or glaucoma, and hypokalemia. The Townsend deprivation index, a measure of material deprivation within a population classed into quintile was obtained for each person. Lastly, we examined the location (ie, England, Northern Ireland, Scotland, and Wales) and size (number of patients in the practice in the January 1, 2007) of the participating general practice.
Statistical Analyses
First, we extracted data on each measurement before and during follow-up as described earlier in order to describe the monitoring provided to the patients. For each patient, the index date was defined as the date of initiation of the first glucocorticoid course ≥3 months. Second, we used binary logistic regression models to assess the association between the outcomes (ie, having the measurement of interest before or during glucocorticoid exposure) and the characteristics of the patients, treatment, time, and practices. To ensure that we captured measurements relating to the prescription of glucocorticoids rather than the patient condition (eg, blood pressure routinely measured in a hypertensive rather than on account of glucocorticoid prescription) we chose to define a glucocorticoid prescription-related measurement as one that occurred within 1 month before glucocorticoid initiation for clinical parameters, within 1 month before and 2 weeks after for biological parameters, and within 1 month before to 2 months after for DEXA-scan, eye survey, and vaccines. For continuous variables, we checked linearity by using the log-likelihood ratio test. Continuous variables are presented as median and interquartile range. Categorical variables are presented as proportions. All analyses were done using Stata, version 11.2 (StataCorp, College Station, TX). The study was approved by the UCL THIN steering committee and by the THIN scientific review committee.
RESULTS
Study Population
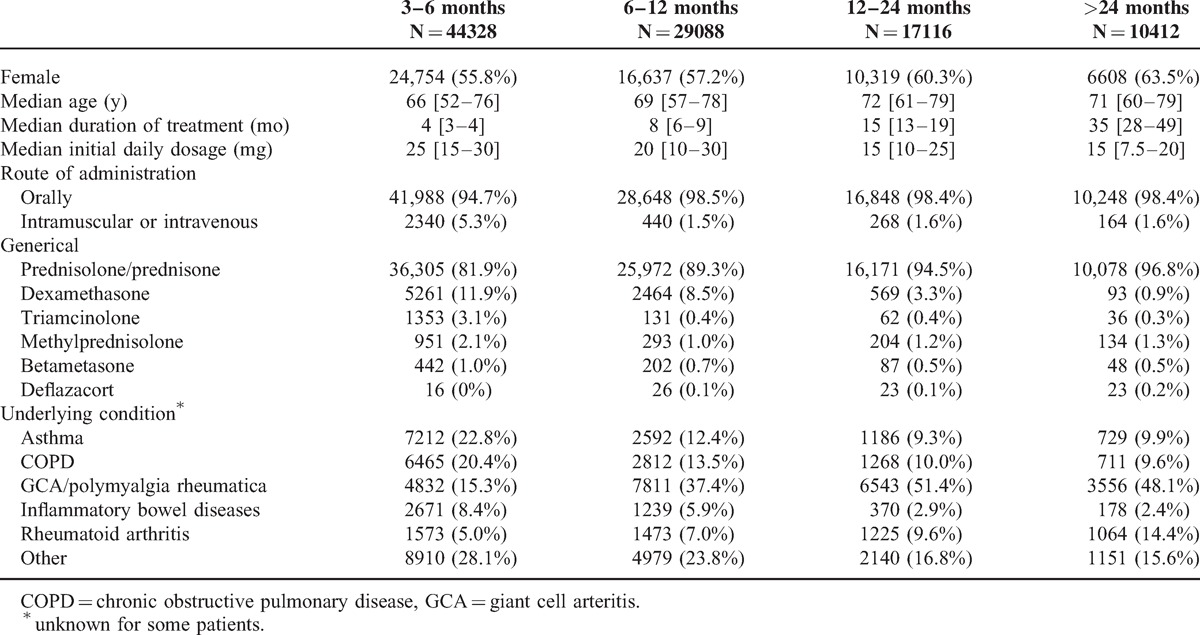
During the study period, 100,944 adult patients (women: 58,318 [58%], median age at the time of glucocorticoid initiation: 69 [56–78] years) were prescribed at least one course of systemic glucocorticoid ≥3 months. Among them, 73,552 (73%) had >1 long-term prescription. Taking into account the first prescription, 27,528 (27%) patients received glucocorticoids for more than a year (Table 1). A history of hypertension was recorded in about half the patients, a history of dyslipidemia in a quarter, a history of diabetes, cataracts and osteoporosis in just over a tenth, and a history of hypokalemia in 925 (1%) patients. Most of the data were from English practices (n = 406, 73.3%), 85 (15.3%) practices being from Scotland, 40 (7.2%) from Wales, and 23 (4.2%) from Northern Ireland.
TABLE 1.
Characteristics of the Study Population
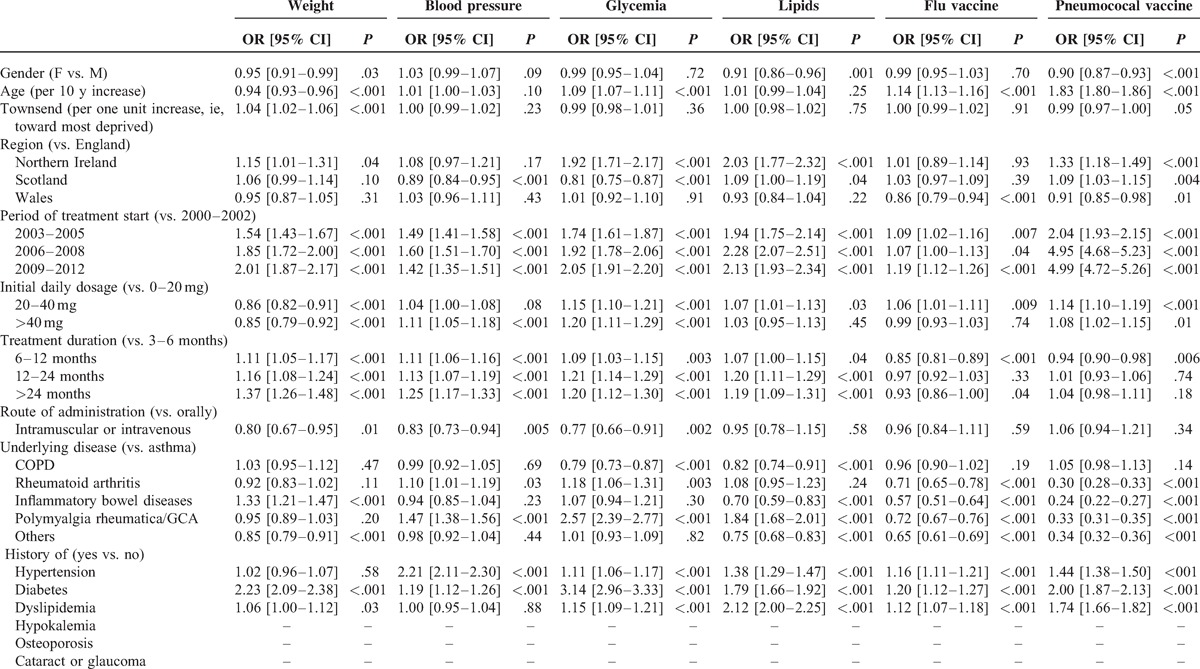
Initial Monitoring
Routine clinical (eg, weight) or biological (eg, glucose or lipid levels) monitoring before the initiation of glucocorticoids occurred in less than one-third of the patients, irrespectively of the duration of the subsequent exposure (Table 2). This was even lower for measures such as osteoporosis or eye screening. About 60% and 45% of the patients have had vaccination against influenza and pneumococcus prior glucocorticoid exposure, respectively (Table 2). These figures varied according to the underlying medical condition (supplementary Table, http://links.lww.com/MD/A244). Factors associated with the odds of being monitored varied according to the parameter being assessed (Table 3 , multivariable analyses). Older patients were more likely to be monitored on most parameters than young patients. The past medical history of the patients influenced the odds of being monitored, patients with diabetes, hypertension, or dyslipidemia being more likely to be monitored for weight, blood pressure, glucose, lipids while those with asthma or chronic obstructive pulmonary disease being more likely to be vaccinated. Patients initiated on higher daily doses or for longer duration were more likely to be monitored. Furthermore, monitoring related to the underlying disease, patients with PMR/GCA being most adequately monitored. There were geographical variations but, overall, the monitoring improved over the 12-year study period. The practices size was not associated with any of the parameters of interest (data not shown).
TABLE 2.
Monitoring of Parameters of Interest Before and During Glucocorticoid Therapy According to the Duration of Exposure
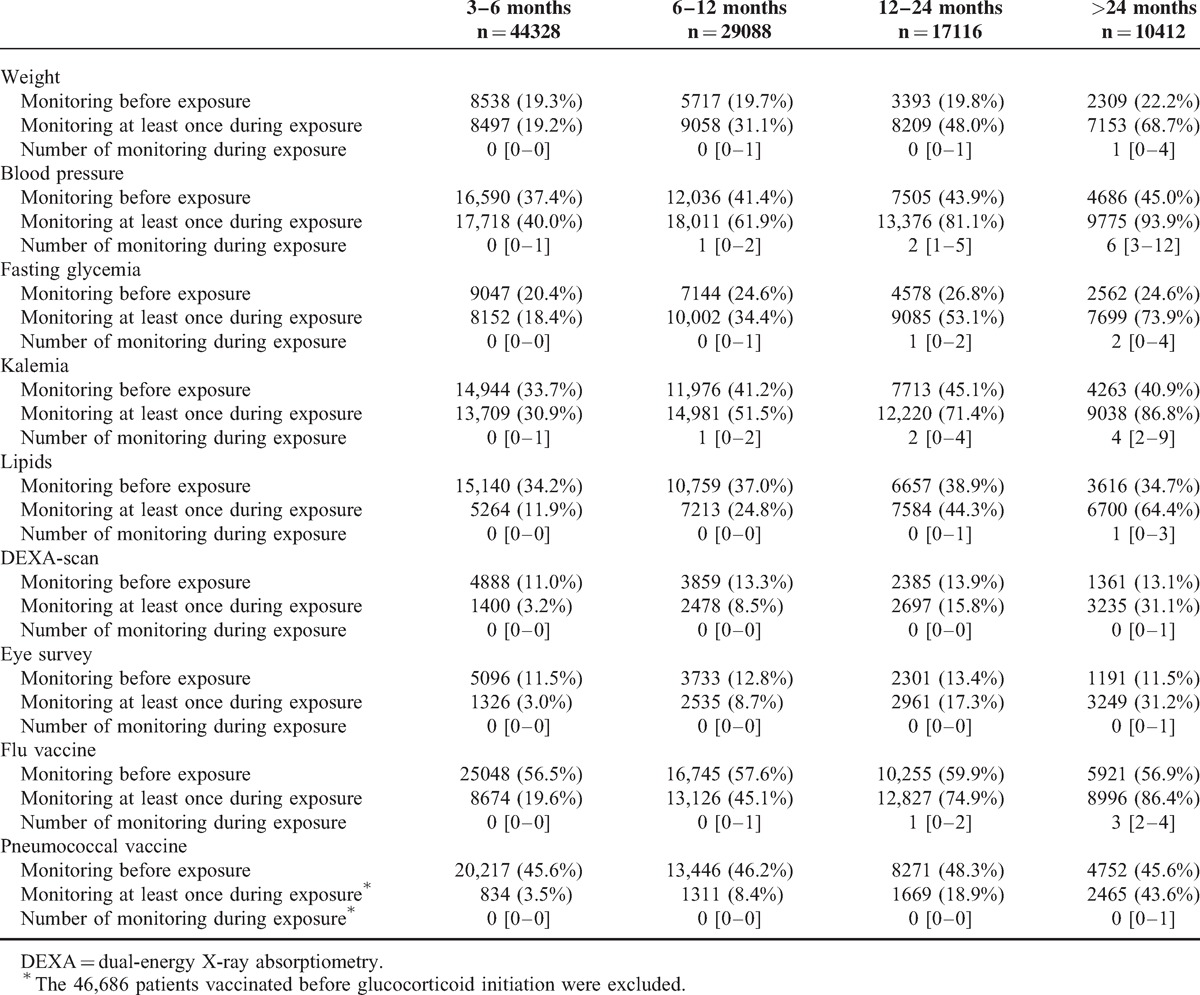
TABLE 3.
Factors Associated With the Odds of Being Monitored Before Glucocorticoid Initiation—Multivariable Analyses
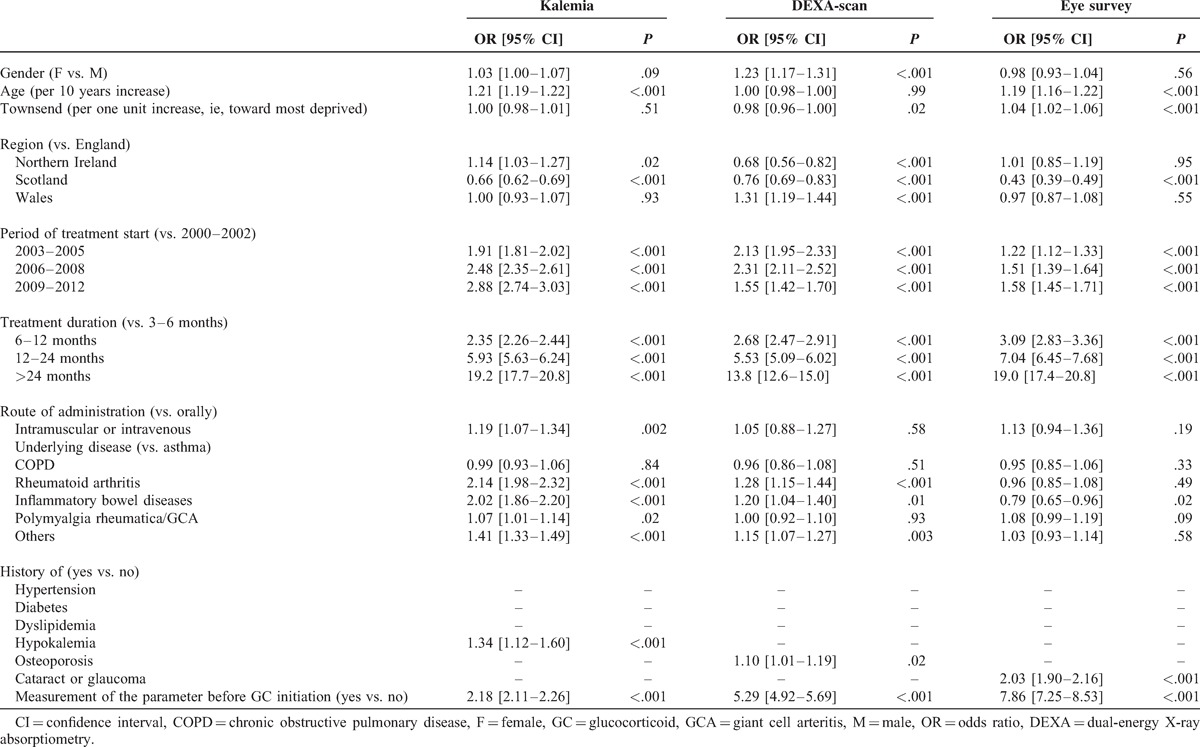
Follow-up Monitoring
The percentage of patients monitored at least once during glucocorticoid exposure and the number of measurements increased proportionally with the duration of exposure (Table 2). However, <60% of patients exposed for >1 year to glucocorticoids were monitored at least once for weight, glucose, or lipid levels and <25% of them had at least one bone density or eyes diseases screening. The factors associated with being monitored during exposure were quite similar than those evidenced for being monitored before exposure (Table 4 , multivariable analyses).
TABLE 3 (Continued).
Factors Associated With the Odds of Being Monitored Before Glucocorticoid Initiation—Multivariable Analyses
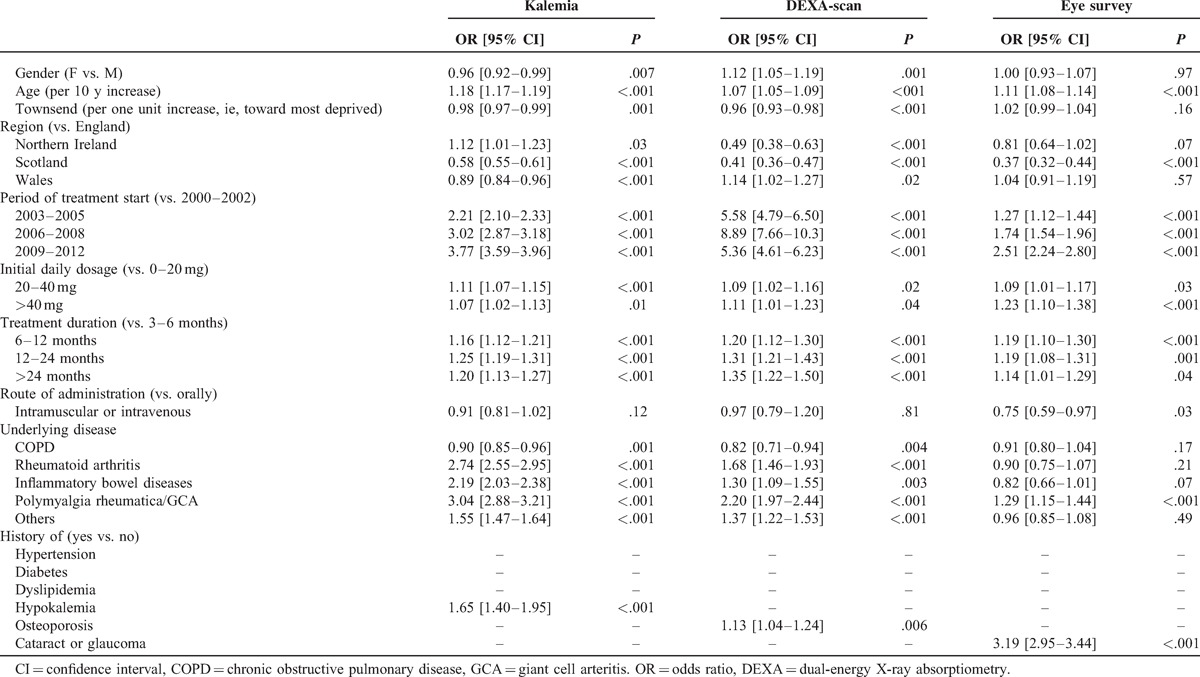
TABLE 4.
Factors Associated With the Odds of Being Monitored During GC Initiation—Multivariable Analyses
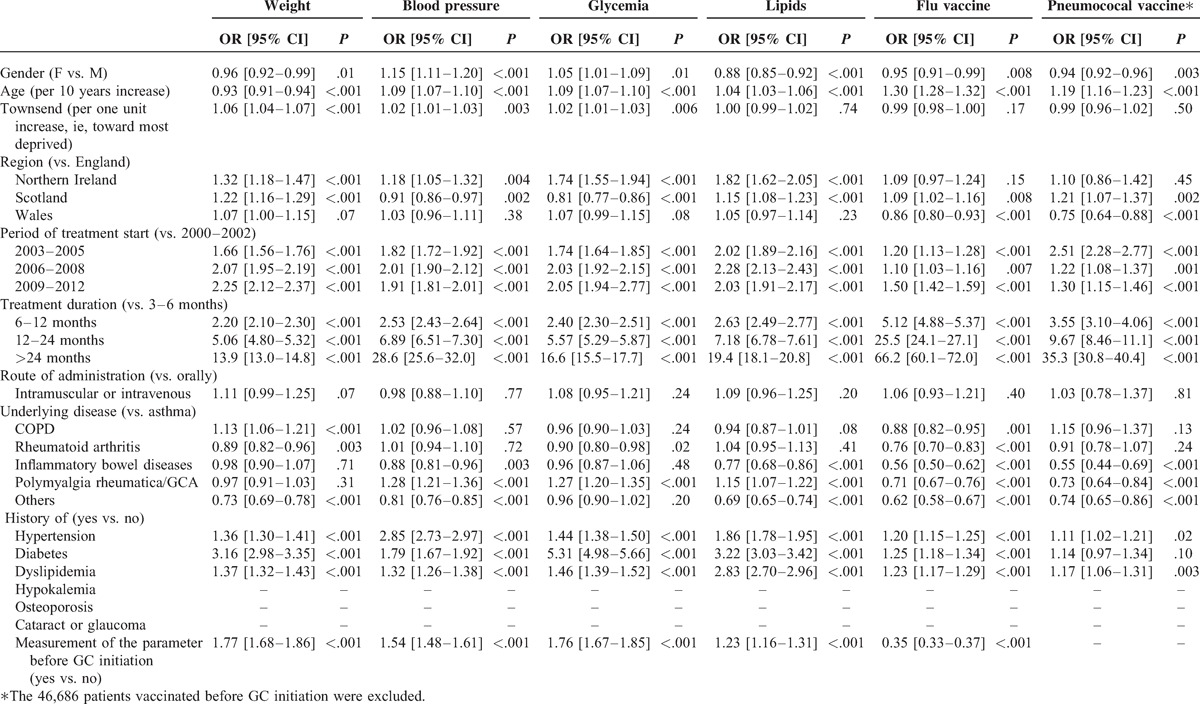
TABLE 4 (Continued).
Factors Associated With the Odds of Being Monitored During GC Initiation—Multivariable Analyses
DISCUSSION
This study of >100,000 patients exposed to long-term systemic glucocorticoid therapy highlights the need for improving the monitoring of these patients in order to ensure safe use of the drug. We found that routine clinical (eg, weight) or biological (eg, fasting glucose or lipid levels) monitoring before initiation of glucocorticoids occurred in less than one-third of patients. This was even lower for measures such as osteoporosis or eye diseases screening. Furthermore, after starting glucocorticoid treatment the percentage of patients monitored whilst on the drug barely improved with <60% of patients exposed for more than a year being monitored at least once for weight, glucose, or lipid levels and <25% of patients being prescribed at least once for osteoporosis or eyes diseases screening. The odds of being adequately monitored were higher in older patients and in those with comorbidities. The level of monitoring had improved over the 12-year study period.
It is remarkable that after almost 70 years of glucocorticoids use15 there still exist uncertainties about their adverse effects and how they should be monitored. In this context, prescribers and patients have offered recommendations on the monitoring and management of these adverse effects largely based on consensus statements by experts.6–8 These recommendations offer good common sense advice such as “the adverse effects of glucocorticoid therapy should be considered and discussed with the patient before glucocorticoid therapy is started” or “when it is decided to start glucocorticoid treatment, comorbidities and risk factors for adverse effects should be evaluated and treated”.7 They also include more specific recommendations on which parameters should be monitored during follow-up, including body weight, blood pressure, serum lipids, blood and/or urine glucose, infections, osteoporotic fractures, or eye adverse effects.6,7 On the other hand, there are national recommendations about the assessment of bone mineral density using DEXA-scan before and during glucocorticoid initiation.16–18 For instance, in the UK, it is recommended that people starting systemic glucocorticoids for > 3 months have a DEXA-scan before exposure and every 1–3 years thereafter if glucocorticoids are continued.18 Furthermore, in many countries including the UK, it is recommended that people on long-term systemic glucocorticoid therapy have a flu vaccine every year and are vaccinated against pneumococcus.19–22 Despite these recommendations, there are, to our knowledge, very limited data on what occurs in daily care.4,5 Yet it seems that this is a necessary prerequisite to adapt the recommendations to daily practice and vice versa.
In this study, we found that basic assessments such as weight, blood pressure, glucose, or lipid levels were rarely done before and during glucocorticoid exposure. Yet, metabolic and cardiovascular adverse events are established complications of chronic glucocorticoid exposure, the risk of diabetes, or cardiovascular events being increased by 2- to 3-fold in these patients.23–26 Moreover, weight gain and lipodystrophic features are observed in >50% of patients after long-term exposure and can lead to poor adherence to the medication, the development of features of the metabolic syndrome, and an increase in cardiovascular risk.27–29
Older patients are more likely to be adequately monitored than young patients. First, three-quarters of patients chronically exposed to the drug are >54 years1,30 and physicians are therefore probably more used to monitor these patients than the younger ones. It is also possible that older patients who are at a higher risk of adverse events such as osteoporosis, cataract or diabetes are anyway more likely to be carefully monitored by their general practitioners. Nevertheless, younger patients are at higher risk of adverse events such as lipodystrophy or weight gain31 and are more likely to receive several long-term glucocorticoid treatments during their lifetime and therefore deserve equal attention. We also found geographical disparities in the way patients were managed. It is unclear whether this could be explained by geographical inequalities regarding local availability of equipment (eg, disparities in DEXA-scan availability32) or access to secondary care physicians (eg, ophthalmologists33) or true geographical variations in general practitioners monitoring behaviors.
Our study has several strengths. It is the first one to assess how patients chronically exposed to systemic glucocorticoids are managed in clinical practice. It is based on a large population-based sample of patients of both sexes, across all age-groups, and suffering for many underlying diseases and comorbidities. It covers a 12-year period time and different regions of the UK which enabled us to study time and geographical variations of practices.
However, there are also some limitations. First, monitoring of some frequent and/or serious adverse events (eg, neuropsychiatric or cutaneous disorders, infections) was not examined as there are no recommendations on how this should be done in practice. For instance, there are no consensus recommendations on how and when infectious diseases such as tuberculosis or viral hepatitis should be screened in glucocorticoid-exposed patients. Second, it could be argued that our findings relate to what was recorded on the computerized notes and this may not reflect actual practice. For instance, weight and blood pressure could have been measured during the consultation without being recorded or some patients may have been assessed for osteoporosis risk only by the FRAX score without DEXA-scan. However, we believe that if this information is missing from the medical records notes it is perhaps as good as not being measured as other clinicians involved with the person's care will not be able to assess the trajectory of symptoms over time. Third, for some conditions (eg, rheumatoid arthritis, inflammatory bowel diseases), the secondary care specialist may have been the initiator for glucocorticoid therapy. Some may therefore argue that the secondary care physician is also responsible for the glucocorticoid monitoring. However, in the UK, the primary care physicians are the cornerstone of patients care and even when drugs are initiated in secondary care the responsibility of long-term prescribing rests solely with primary care physicians. Lastly, some of the assessments/vaccinations may have occurred for reasons other than that of being on glucocorticoid therapy (eg, eye survey in patients with giant cell arteritis). Even though, the exact reason for each of these assessments may not be known, we believe that appropriate monitoring is more important that the reason for which it was done.
It has recently been estimated that more of 600,000 patients in the UK and >2.5 million patients in the USA are chronically exposed to systemic glucocorticoids.1,30 Millions of people are probably exposed across the world making it one of the most prescribed drugs worldwide. Glucocorticoids confer huge clinical benefits and will continue to be used in practice. However, in view of the severity of their adverse effects clinicians should closely monitor all patients prescribed these drugs. Even though the best schedule for monitoring is still unknown and is dependent on the characteristics of the patient and their underlying diseases, small changes geared at structured baseline and follow-up assessments of people on long-term glucocorticoids could make a substantial change to clinical care. This could go some way towards ensuring that glucocorticoids will no longer be the most common cause for producing adverse events requiring hospitalization.34
Footnotes
The authors have no funding and conflicts of interest to disclose.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Website (www.md-journal.com).
REFERENCES
- 1.Fardet L, Petersen I, Nazareth I. Prevalence of long-term oral glucocorticoid prescriptions in the UK over the past 20 years. Rheumatol Oxf Engl 2011; 50:1982–1990. [DOI] [PubMed] [Google Scholar]
- 2.Van Staa TP, Leufkens HG, Abenhaim L, et al. Use of oral corticosteroids in the United Kingdom. QJM 2000; 93:105–111. [DOI] [PubMed] [Google Scholar]
- 3.Fardet L, Flahault A, Kettaneh A, et al. Corticosteroid-induced clinical adverse events: frequency, risk factors and patient's opinion. Br J Dermatol 2007; 157:142–148. [DOI] [PubMed] [Google Scholar]
- 4.Perdoncini-Roux A, Blanchon T, Hanslik T, et al. [Description of French general practitioners’ practices regarding long term systemic corticosteroid therapy-associated measures]. Rev Prat 2009; 59:19–24. [PubMed] [Google Scholar]
- 5.Fardet L, Hanslik T, Blanchon T, et al. [Long-term systemic corticosteroid-therapy associated measures: description of the French internal medicine physicians’ practices]. Rev Méd Interne 2008; 29:975–980. [DOI] [PubMed] [Google Scholar]
- 6.Duru N, van der Goes MC, Jacobs JWG, et al. EULAR evidence-based and consensus-based recommendations on the management of medium to high-dose glucocorticoid therapy in rheumatic diseases. Ann Rheum Dis 2013; 72:1905–1913. [DOI] [PubMed] [Google Scholar]
- 7.Hoes JN, Jacobs JWG, Boers M, et al. EULAR evidence-based recommendations on the management of systemic glucocorticoid therapy in rheumatic diseases. Ann Rheum Dis 2007; 66:1560–1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Van der Goes MC, Jacobs JWG, Boers M, et al. Monitoring adverse events of low-dose glucocorticoid therapy: EULAR recommendations for clinical trials and daily practice. Ann Rheum Dis 2010; 69:1913–1919. [DOI] [PubMed] [Google Scholar]
- 9.Lis Y, Mann RD. The VAMP Research multi-purpose database in the UK. J Clin Epidemiol 1995; 48:431–443. [DOI] [PubMed] [Google Scholar]
- 10.Blak BT, Thompson M, Dattani H, et al. Generalisability of The Health Improvement Network (THIN) database: demographics, chronic disease prevalence and mortality rates. Inform Prim Care 2011; 19:251–255. [DOI] [PubMed] [Google Scholar]
- 11.Bourke A, Dattani H, Robinson M. Feasibility study and methodology to create a quality-evaluated database of primary care data. Inform Prim Care 2004; 12:171–177. [DOI] [PubMed] [Google Scholar]
- 12.Ruigómez A, Martín-Merino E, Rodríguez LAG. Validation of ischemic cerebrovascular diagnoses in the health improvement network (THIN). Pharmacoepidemiol Drug Saf 2010; 19:579–585. [DOI] [PubMed] [Google Scholar]
- 13.Lewis JD, Schinnar R, Bilker WB, et al. Validation studies of the health improvement network (THIN) database for pharmacoepidemiology research. Pharmacoepidemiol Drug Saf 2007; 16:393–401. [DOI] [PubMed] [Google Scholar]
- 14.Lewis JD, Bilker WB, Weinstein RB, et al. The relationship between time since registration and measured incidence rates in the General Practice Research Database. Pharmacoepidemiol Drug Saf 2005; 14:443–451. [DOI] [PubMed] [Google Scholar]
- 15.Chast F. [History of corticotherapy]. Rev Méd Interne 2013; 34:258–263. [DOI] [PubMed] [Google Scholar]
- 16.Grossman JM, Gordon R, Ranganath VK, et al. American College of Rheumatology 2010 recommendations for the prevention and treatment of glucocorticoid-induced osteoporosis. Arthritis Care Res 2010; 62:1515–1526. [DOI] [PubMed] [Google Scholar]
- 17.http://www.has-sante.fr/portail/upload/docs/application/pdf/osteoporose_synthese.pdf Accessed January 2015. [Google Scholar]
- 18.https://www.rcplondon.ac.uk/sites/default/files/documents/glucocorticoid-induced-osteoporosis-concise.pdf Accessed January 2015. [Google Scholar]
- 19.http://www.cdc.gov/mmwr/preview/mmwrhtml/00023141.htm Accessed January 2015. [Google Scholar]
- 20.http://www.nhs.uk/Conditions/vaccinations/Pages/flu-influenza-vaccine.aspx Accessed January 2015. [Google Scholar]
- 21.http://www.nhs.uk/Conditions/vaccinations/Pages/when-is-pneumococcal-vaccine-needed.aspx Accessed January 2015. [Google Scholar]
- 22.http://www.sante.gouv.fr/IMG/pdf/Calendrier_vaccinal_detaille_2013_ministere_Affaires_sociales_et_Sante-_pdf.pdf Accessed January 2015. [Google Scholar]
- 23.Conn HO, Poynard T. Corticosteroids and peptic ulcer: meta-analysis of adverse events during steroid therapy. J Intern Med 1994; 236:619–632. [DOI] [PubMed] [Google Scholar]
- 24.Blackburn D, Hux J, Mamdani M. Quantification of the risk of corticosteroid-induced diabetes mellitus among the elderly. J Gen Intern Med 2002; 17:717–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Souverein PC, Berard A, Van Staa TP, et al. Use of oral glucocorticoids and risk of cardiovascular and cerebrovascular disease in a population based case-control study. Heart Br Card Soc 2004; 90:859–865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wei L, MacDonald TM, Walker BR. Taking glucocorticoids by prescription is associated with subsequent cardiovascular disease. Ann Intern Med 2004; 141:764–770. [DOI] [PubMed] [Google Scholar]
- 27.Fardet L, Cabane J, Kettaneh A, et al. Corticosteroid-induced lipodystrophy is associated with features of the metabolic syndrome. Rheumatol Oxf Engl 2007; 46:1102–1106. [DOI] [PubMed] [Google Scholar]
- 28.Arena C, Morin A-S, Blanchon T, et al. Impact of glucocorticoid-induced adverse events on adherence in patients receiving long-term systemic glucocorticoid therapy. Br J Dermatol 2010; 163:832–837. [DOI] [PubMed] [Google Scholar]
- 29.Fardet L, Petersen I, Nazareth I. Risk of cardiovascular events in people prescribed glucocorticoids with iatrogenic Cushing's syndrome: cohort study. BMJ 2012; 345:e4928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Overman RA, Yeh J-Y, Deal CL. Prevalence of oral glucocorticoid usage in the United States: a general population perspective. Arthritis Care Res 2013; 65:294–298. [DOI] [PubMed] [Google Scholar]
- 31.Fardet L, Cabane J, Lebbé C, et al. Incidence and risk factors for corticosteroid-induced lipodystrophy: a prospective study. J Am Acad Dermatol 2007; 57:604–609. [DOI] [PubMed] [Google Scholar]
- 32.Kanis JA, Johnell O. Requirements for DXA for the management of osteoporosis in Europe. Osteoporos Int 2005; 16:229–238. [DOI] [PubMed] [Google Scholar]
- 33.http://www.rcophth.ac.uk/page.asp?section=293sectionTitle=Ophthalmic+Services+Guidance. 2014 Accessed August 2014. [Google Scholar]
- 34.Elixhauser A, Owens P. Adverse Drug Events in U.S. Hospitals, 2004: Statistical Brief #29. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet]. Rockville (MD): Agency for Health Care Policy and Research (US); 2006. [cited 2014 Aug 4]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK63500/ Accessed August 2014. [Google Scholar]


