Abstract
The prevalence of cervical disc disease is high, and the traditional surgical method of anterior cervical discectomy and fusion (ACDF) carries with it the disadvantages of motion loss at the operated level, and accelerated adjacent level disc degeneration. Preliminary results of the efficacy and reoperative rate comparing TDA versus ACDF have been reported; however, the long-term outcomes of TDA versus ACDF still remain a topic of debate.
This review was prepared following the standard procedures set forth by the Cochrane Collaboration organization, and preferred reporting items for systematic reviews and meta-analyses (PRISMA). The only studies included were randomized controlled trials with a minimum of 4 years of follow-up data. The meta-analysis included the neck disability index (NDI), visual analog scale (VAS) of neck and arm pain, SF-36 physical component scores (SF-36 PCS), over success, neurological success, work status, implant-related complications, and secondary surgery events.
Four randomized controlled trials meet the inclusion criteria. The long-term improvement of NDI, VAS of neck and arm pain, SF-36 PCS, over success, and neurological success favored the TDA group. The TDA group also had a lower incidence of secondary surgery for both the index level (RR: 0.45 [0.28, 0.72]) and adjacent level (RR: 0.53 [0.33, 0.88]).
In this meta-analysis of 4 included RCTs with a minimum 4 years of follow-ups, total disc arthroplasty showed improvements over ACDF as measured by the NDI, VAS of neck and arm pain, and SF-36 PCS.
INTRODUCTION
Anterior cervical discectomy and fusion (ACDF) is widely used to treat cervical disc disease.1,2 However, this technique is in question because of the disadvantages of motion loss at the operated level and accelerated adjacent level disc degeneration.3,4 For this reason, the long-term efficacy and reoperative rate comparing TDA and ACDF are still in debate. Novel dynamic techniques to preserve the segmental motion of operative levels have been investigated by surgeons, including devices such as the Bryan disc, Prestige disc, Kineflex|C, and ProDisc-C.5–8
The potential advantages of these dynamic devices may be that they can postpone the degeneration of adjacent level disc, and avoid secondary operations on adjacent level discs. There have been many studies9–12 on the efficacy and reoperative rates of total disc arthroplasty (TDA) by dynamic device versus traditional ACDF; however, the results have been confounded by the secondary effects spinal decompression has on both methods.13,14
Therefore, the purpose of this study was to use meta-analysis to systematically review the long-term outcomes of TDA versus ACDF for cervical disc disease.
METHODS
This is a meta-analysis of previous reports, so ethical approval is not necessary.
Inclusion criteria: prospective randomized controlled trials (RCTs) comparing TDA with dynamic devices and standard ACDF for cervical disc disease, which included symptomatic cervical disc disease with refractory/intractable radiculopathy or myelopathy; adult population; minimum of 4 years of follow-up data.
Exclusion criteria: non-RCTs or respective studies; follow-up less than 4 years; duplicated publications from the same medical center or investigate site.
Prospective RCTs with follow-up less than 4 years, nonrandomized studies, retrospective studies, and case series are excluded.
Search Strategy and Study Selection
Two authors (A.M.W. and N.F.T.) independently searched the electronic literature database of Medline and Embase for RCTs comparing TDA with dynamic devices and standard ACDF for cervical disc disease. All studies published between January 1966 and December 2013 were included in the search strategy, without limitation of language. Keywords were used as: TDA, cervical disc arthroplasty, total disc replacement, dynamic device, artificial disc, ACDF, cervical spine arthrodesis, RCT, controlled clinical trial, randomized, randomly, and trial and are used in combination with Boolean operators of AND, OR, and NOT. The function of “related article” is also used for search. The reference studies of previous systematic reviews, meta-analysis, and RCTs were manually searched to avoid initial miss. After 2 authors assessed the potentially eligible studies independently, any disagreement was discussed and resolved with the third independent author (Y.L.C.). A track search was performed on October 1, 2014, to include the new studies published between January and October 2014
Data Collection
After confirming the study is eligible for inclusion, 2 authors (H.X. and A.M.W.) independently extracted data for analysis. A standard data extracted form was used at this stage, including publish date, study design, sample size, follow-up duration, characteristics of patients, interventions, NDI scores, VAS of neck pain, VAS of arm pain, SF-36, over success, neurological success, work status, implant-related complication (implant loosing, implant migration, implant subsidence) and secondary surgery of index and adjacent levels.
Secondary surgery includes revision, removals, supplemental fixation, and reoperation. According to the included studies, revision was the procedure to modify the original implant, removal was the procedure that 1 or more components of the original implant configuration were removed without replacement, supplemental fixation was the procedure of implanting additional instrumentation, and reoperation of index level was any surgical procedure at the index level that did not remove, modify, or add any components.
Risk of Bias Assessment
We assessed the risk of bias of included RCTs according to the Cochrane Handbook for Systematic Reviews of Interventions: random sequence generation; allocation concealment; blinding of participants and personnel; blinding of outcome assessment; incomplete outcome data addressed; selective reporting; 7. other bias. And the judgments of reviewers are classified as “low risk,” “high risk,” or “unclear risk” of bias.
Statistical Analysis
The data suitable for meta-analysis were performed with the STATA software (version 12.0; StataCorp, College Station, TX). Relative risk (RR) was calculated for dichotomous outcomes and weighted mean difference (WMD) was calculated for continuous outcomes in this study. Sensitivity analysis involved removing 1 study and evaluating whether the other results would be markedly affected. Heterogeneity was evaluated using the χ2 and I2. We defined the acceptable heterogeneity by P value of χ2 test >0.10 and I2 <50%. Results of homogeneity data were pooled using the fixed-effects model and 95% confidence intervals, and heterogeneity data by random-effects models.
RESULTS
Included Studies and Risk of Bias Assessment
A total of 205 records were identified through Medline (n = 128) and Embase (n = 77) databases. Twenty-nine duplicated papers were deleted, leaving 176 records. Total 63 full-text articles were assessed for eligibility, 18 literatures of them were not RCTs and 15 were minimize follow-up less than 48 months, 2 were study protocols, 4 were from the same site to the including studies, 1 was Cochrane review, and 19 for other reasons were excluded (the list of the these articles is shown in Supplemental List 1). At last 4 randomly controlled trials with a minimum of 4 years of follow-ups were included in this study according to our inclusion criteria, a 7-year study reported by Burkus et al15 was found at track search to replace their 5 years’ results16 (Figure 1).
FIGURE 1.
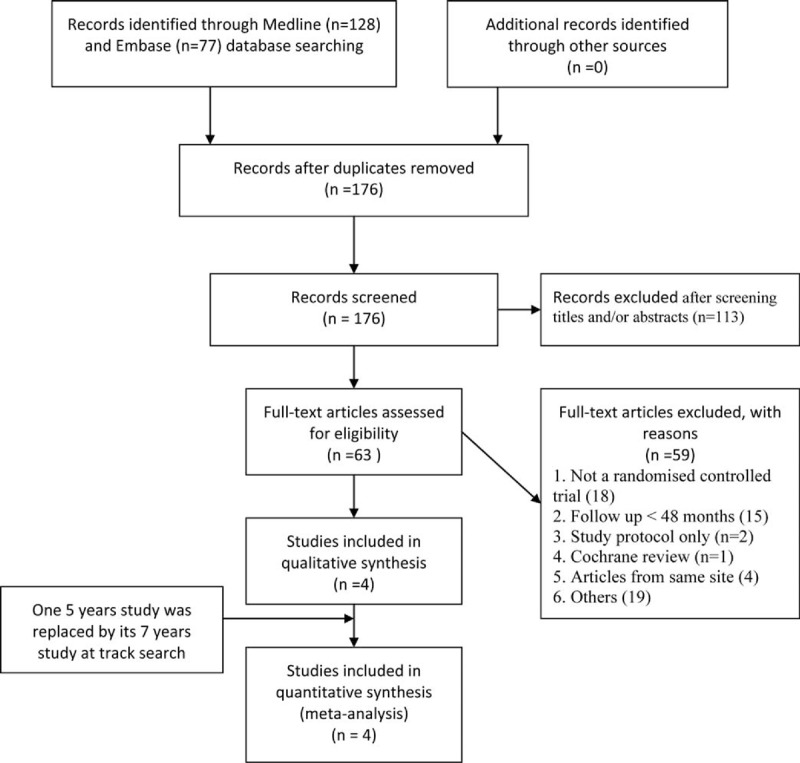
The selection of literatures for included studies.
The characteristics of the 4 included studies are shown in Table 1. A total of 921 patients with cervical disc disease were randomized to the TDA group (n = 506) and ACDF groups (n = 415), respectively.
TABLE 1.
Characteristics of the Included Trials
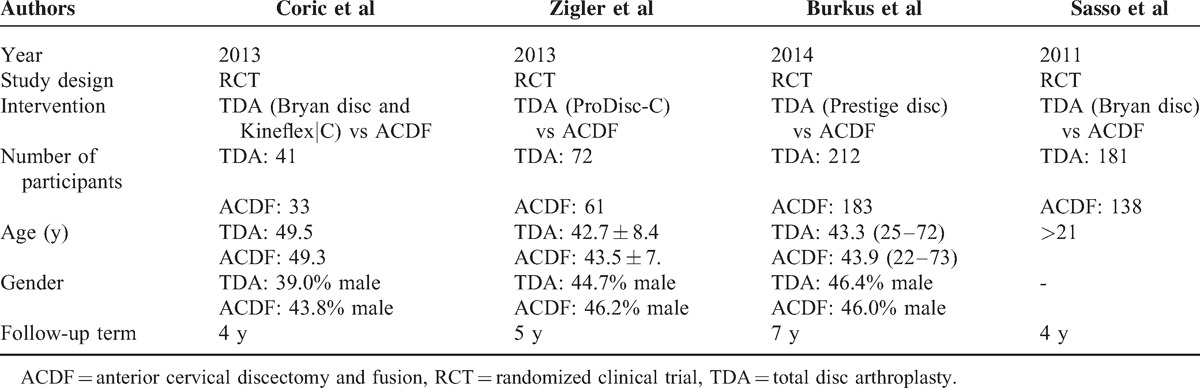
Three included studies15,17,18 were multicenter randomized controlled clinical trials and 1 was from a single investigational site,19 the indications in study of Coric et al19 were 1-level symptomatic cervical disc disease with medically refractory radiculopathy, in study of Zigler et al17 was intractable, debilitating radiculopathy, in studies of Sasso et al18 and Burkus et al15 was 1-level cervical disc disease with radiculopathy or myelopathy, but only C3–4 or C6–7 levels included in study of Burkus et al.15 Information of allocation concealment is not available for all 4 studies. Two of the studies17,18 were blind to the participant, and 1 of the studies15 was not blind, 1 was unclear.19 Due to the difference in appearance of the postoperative radiological data between TDA and ACDF groups, a blind outcome assessment was impossible; the term “blinding of outcome assessment” was assessed as “high risk” for all 4 studies. The risk of bias of included studies is shown in Table 2.
TABLE 2.
Risk of Bias Assessment of All Included Studies
Clinical Outcomes
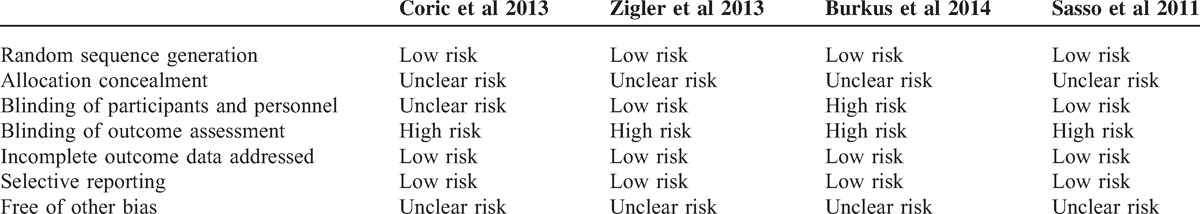
Two studies of Sasso et al and Burkus et al15,18 provide both mean value and standard deviation of the neck disability index (NDI), VAS of arm pain and neck pain, SF-36 physical component scores, over success, neurological success, and work status.
The meta-analysis of NDI, VAS of arm pain and neck pain, SF-36 physical component scores (SF-36 PCS) results showed in favor of TDA group, with RRs (95% CI) of −6.59 (−6.93, −6.26), −4.92 (−7.90, −1.94), −8.91 (−12.06, −5.77), and 3.16 (1.87, 4.44), respectively; all of them had statistical significant difference (Figure 2). Only the I2 of VAS of neck pain subgroup was 53.8%; the others were less than 50%.
FIGURE 2.
TDA versus ACDF for cervical disc disease: forest plot for NDI, VAS of arm pain and neck pain, SF-36 PCS. ACDF = anterior cervical discectomy and fusion, CI = confidence interval, NDI = neck disability index, SF-36 PCS = SF-36 physical component scores, TDA = total disc arthroplasty, VAS = visual analog scale, WMD = weighted mean difference.
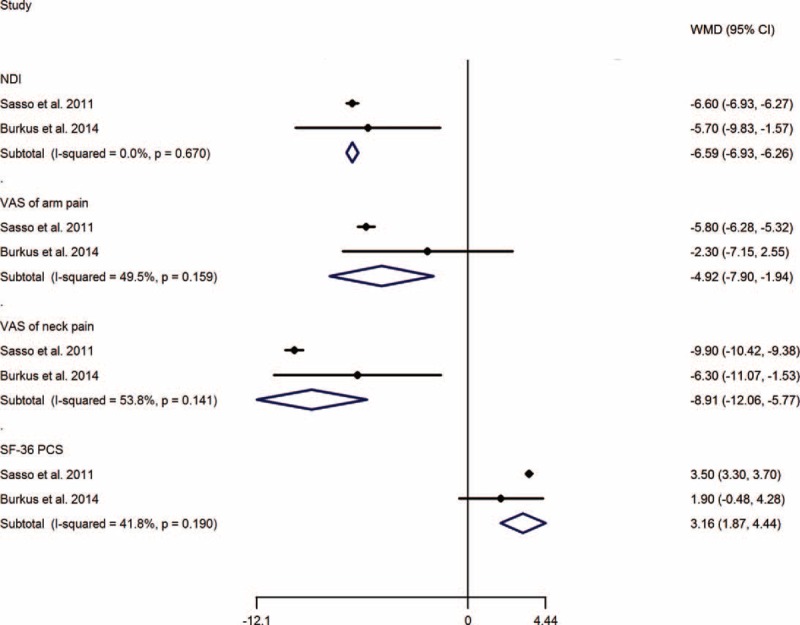
The results of over success and neurological success showed a higher success rate in TDA group than that in ACDF group, with RRs (95%CI) of 1.19 (1.08, 1.30), and 1.06 (1.00, 1.12), respectively. However, no significant difference was calculated of work status, with RR of 1.05 (0.96, 1.15) (Figure 3).
FIGURE 3.
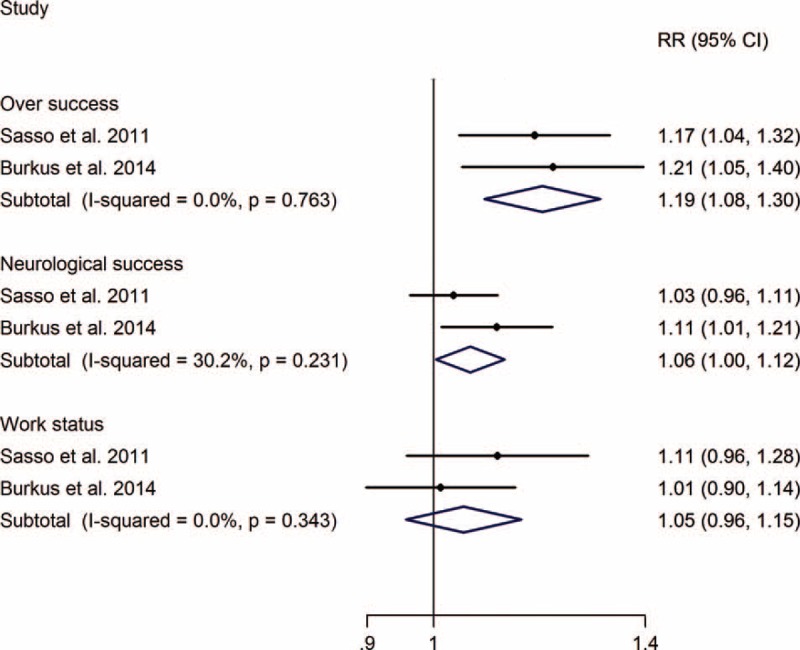
TDA versus ACDF for cervical disc disease: forest plot for over success, neurological success, and work status. ACDF = anterior cervical discectomy and fusion, CI = confidence interval, RR = relative risk, TDA = total disc arthroplasty.
Implant Complication and Secondary Surgery
The RR of implant-related complications of TDA versus ACDF was 5.37 (0.97, 29.63), without significant difference, and the meta-analysis showed that TDA can significantly decrease the risk of secondary surgery at the index and adjacent levels, with RRs of 0.45 (0.28, 0.72) and 0.53 (0.33, 0.88), respectively (Figure 4).
FIGURE 4.
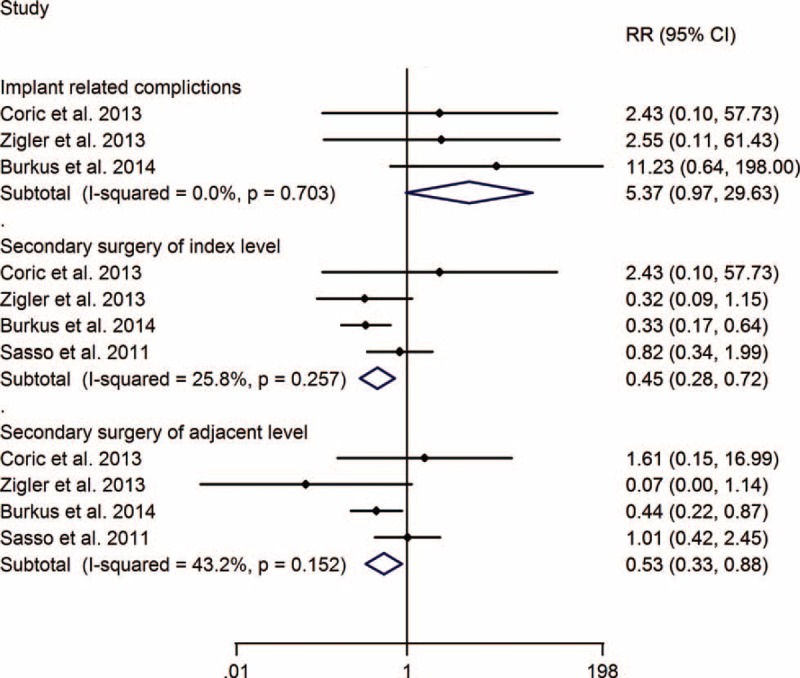
TDA versus ACDF for cervical disc disease: forest plot for implant-related complications, secondary surgery of index level, and adjacent level. ACDF = anterior cervical discectomy and fusion, CI = confidence interval, RR = relative risk, TDA = total disc arthroplasty.
DISCUSSION
ACDF was one of standard treatments for cervical disc disease; many studies proved the safety and efficacy of this method.20–22 However, studies reporting motion loss at the operated level, and accelerated adjacent level disc degeneration, are becoming more prevalent.11,23 Additionally, cadaveric biomechanical studies24,25 suggest that significant increase in intradiscal pressure and segmental motion at the levels adjacent to fusion during normal range of motion. The drawbacks of ACDF necessitate the search for a novel device which could preserve the motion of operated levels.26 Although the radiological outcomes of present studies8,11 showed these novel dynamic devices could preserve the motion of the operative level, the ability of the device to decrease adjacent level disc degeneration was still unclear, primarily because degeneration of adjacent level discs is a slow process. In spite of these problems, there were many preliminary reports of the efficacy of dynamic devices; however, the long-term clinical outcomes and safety of motion preservation devices in the cervical spine is still in debate.
This meta-analysis including 4 prospective RCTs with a minimum of 4 years of follow-ups, 1 of them18 was previously included by Yang et al,27 Boselie et al,28 and Gao et al,29 and other 3 studies15,17,19 were published in 2013 and 2014, and were not included in previous systematic reviews or meta-analysis.
Our present meta-analysis showed that all the long-term improvements of NDI, VAS of neck and arm pain, SF-36 PCS, overall success, and neurological success are in favor of the TDA groups, except for work status; however, since the unclear risk of allocation concealment and high risk of the blinding of outcome assessment, these results should still be interpreted with caution.
The concept of “adjacent segment degeneration” and “adjacent segment disease” were defined differently,30,31 the former was defined as radiographic changes at the adjacent discs without clinical symptoms, and “adjacent segment disease” was defined as the development of new clinical symptoms based on “adjacent segment degeneration.’. For adjacent segment degeneration the patient may be symptom free, and difficult to diagnose accurately. Adjacent segment disease requiring intervention was more related to quality of life. In this study, we focused on the differences in secondary surgeries of the index and adjacent levels between TDA and ACDF groups. The long-term follow-up meta-analysis showed a lower rate of secondary surgery for the index and adjacent levels of the TDA group over ACDF groups. Although these findings were similar to the findings of Gao et al,29 the same reason of the unclear risk of allocation concealment and high risk of the blinding of outcome assessment, these results should still be interpreted with caution.
Strengths of Study
Our meta-analysis compared the long-term efficacy and safety of 2 different treatment modalities, TDA and ACDF, for cervical disc disease. All of included studies were RCTs with follow-ups of more than 4 years, the longest being 7 years.15 Moreover, the total number of patients involved in different cervical artificial disc procedures, including, Bryan disc, Prestige disc, Kineflex|C, and ProDisc-C, was 921. Therefore, the results were credible.
Limitations of Study
This study has several limitations. The blind to participants of 2 included studies was removed immediately after surgery; this was done to avoid the risk of bias induced by participants withdrawing before surgery; however, the risk of bias induced by further subjective evaluation is inevitable. Although the bias of random sequence generation, incomplete outcome data and selective reporting of all included studies is low risk, the blinding of outcomes assessment is high risk of all included studies, and the blinding of participants and personnel is high risk of Burkus et al,15 unclear risk of Coric et al,19 allocation concealment of all included studies is unclear risk too; therefore, the results that TDA in better clinical outcomes of NDI, VAS of neck and arm pain, SF-36 PCS, over success, and neurological success than ACDF and had a lower rate of secondary surgery in both index and adjacent levels should be interpreted with caution. Meanwhile, our present study included most patients with at least 4 years of follow-up data, but 4 studies were still a small number, and we suggest that larger sample sizes and longer-term follow-up studies could be carried out in the future.
CONCLUSION
Our meta-analysis of 4 included RCTs with a minimum 4 years of follow-ups suggested: TDA with dynamic device was a safe and effective method for cervical disc disease, resulting in better clinical outcomes of NDI, VAS of neck and arm pain, SF-36 PCS, over success, and neurological success than ACDF, and had a lower rate of secondary surgery in both index and adjacent levels.
Footnotes
Abbreviations: ACDF = anterior cervical discectomy and fusion, NDI = neck disability index, RCT = randomized controlled trial, RR = relative risk, SF-36 PCS = short form-36 physical component score, TDA = total disc arthroplasty, VAS = visual analog scale, WMD = weighted mean difference.
The authors declare that they have no competing interests.
AMW, HX, and SW contribute to the conception and design of the study. HZX, YLC, KPM, HMJ, ZYH, and QBL contribute to analysis and interpretation of data. AMW, HX, KPM, and SW contribute to drafting the article. All authors revised it critically for important intellectual content, and for final approval of the version to be published.
AMW and HX are the co-first authors.
This work was supported by National Natural Science Foundation of China (81372014). The funders had no role in the design, execution, and writing up of the study.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Bohlman HH, Emery SE, Goodfellow DB, et al. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am 1993; 75:1298–1307. [DOI] [PubMed] [Google Scholar]
- 2.Bolesta MJ, Rechtine GR, 2nd, Chrin AM. Three- and four-level anterior cervical discectomy and fusion with plate fixation: a prospective study. Spine (Phila Pa 1976) 2000; 25:2040–2044.discussion 2045–2046. [DOI] [PubMed] [Google Scholar]
- 3.Hilibrand AS, Carlson GD, Palumbo MA, et al. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am 1999; 81:519–528. [DOI] [PubMed] [Google Scholar]
- 4.Ishihara H, Kanamori M, Kawaguchi Y, et al. Adjacent segment disease after anterior cervical interbody fusion. Spine J 2004; 4:624–628. [DOI] [PubMed] [Google Scholar]
- 5.Duggal N, Pickett GE, Mitsis DK, et al. Early clinical and biomechanical results following cervical arthroplasty. Neurosurg Focus 2004; 17:E9. [DOI] [PubMed] [Google Scholar]
- 6.Bryan VE., Jr Cervical motion segment replacement. Eur Spine J 2002; 11 suppl 2:S92–S97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Coric D, Nunley PD, Guyer RD, et al. Prospective, randomized, multicenter study of cervical arthroplasty: 269 patients from the Kineflex|C artificial disc investigational device exemption study with a minimum 2-year follow-up: clinical article. J Neurosurg Spine 2011; 15:348–358. [DOI] [PubMed] [Google Scholar]
- 8.Auerbach JD, Anakwenze OA, Milby AH, et al. Segmental contribution toward total cervical range of motion: a comparison of cervical disc arthroplasty and fusion. Spine (Phila Pa 1976) 2011; 36:E1593–1599. [DOI] [PubMed] [Google Scholar]
- 9.Nabhan A, Ishak B, Steudel WI, et al. Assessment of adjacent-segment mobility after cervical disc replacement versus fusion: RCT with 1 year's results. Eur Spine J 2011; 20:934–941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Anderson PA, Sasso RC, Hipp J, et al. Kinematics of the cervical adjacent segments after disc arthroplasty compared with anterior discectomy and fusion: a systematic review and meta-analysis. Spine (Phila Pa 1976) 2012; 37 (22 suppl):S85–S95. [DOI] [PubMed] [Google Scholar]
- 11.Kelly MP, Mok JM, Frisch RF, et al. Adjacent segment motion after anterior cervical discectomy and fusion versus Prodisc-c cervical total disk arthroplasty: analysis from a randomized, controlled trial. Spine (Phila Pa 1976) 2011; 36:1171–1179. [DOI] [PubMed] [Google Scholar]
- 12.Riew KD, Schenk-Kisser JM, Skelly AC. Adjacent segment disease and C-ADR: promises fulfilled? Evid Based Spine Care J 2012; 3 (S1):39–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cason GW, Herkowitz HN. Cervical intervertebral disc replacement. J Bone Joint Surg Am 2013; 95:279–285. [DOI] [PubMed] [Google Scholar]
- 14.Helgeson MD, Bevevino AJ, Hilibrand AS. Update on the evidence for adjacent segment degeneration and disease. Spine J 2013; 13:342–351. [DOI] [PubMed] [Google Scholar]
- 15.Burkus JK, Traynelis VC, Haid RW, Jr, et al. Clinical and radiographic analysis of an artificial cervical disc: 7-year follow-up from the Prestige prospective randomized controlled clinical trial. J Neurosurg Spine 2014; 21:516–528. [DOI] [PubMed] [Google Scholar]
- 16.Burkus JK, Haid RW, Traynelis VC, et al. Long-term clinical and radiographic outcomes of cervical disc replacement with the Prestige disc: results from a prospective randomized controlled clinical trial. J Neurosurg Spine 2010; 13:308–318. [DOI] [PubMed] [Google Scholar]
- 17.Zigler JE, Delamarter R, Murrey D, et al. ProDisc-C and anterior cervical discectomy and fusion as surgical treatment for single-level cervical symptomatic degenerative disc disease: five-year results of a Food and Drug Administration study. Spine (Phila Pa 1976) 2013; 38:203–209. [DOI] [PubMed] [Google Scholar]
- 18.Sasso RC, Anderson PA, Riew KD, et al. Results of cervical arthroplasty compared with anterior discectomy and fusion: four-year clinical outcomes in a prospective, randomized controlled trial. J Bone Joint Surg Am 2011; 93:1684–1692. [DOI] [PubMed] [Google Scholar]
- 19.Coric D, Kim PK, Clemente JD, et al. Prospective randomized study of cervical arthroplasty and anterior cervical discectomy and fusion with long-term follow-up: results in 74 patients from a single site. J Neurosurg Spine 2013; 18:36–42. [DOI] [PubMed] [Google Scholar]
- 20.Gao R, Yang L, Chen H, et al. Long term results of anterior corpectomy and fusion for cervical spondylotic myelopathy. PLoS One 2012; 7:e34811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cabraja M, Oezdemir S, Koeppen D, et al. Anterior cervical discectomy and fusion: comparison of titanium and polyetheretherketone cages. BMC Musculoskelet Disord 2012; 13:172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Park HW, Lee JK, Moon SJ, et al. The efficacy of the synthetic interbody cage and Grafton for anterior cervical fusion. Spine (Phila Pa 1976) 2009; 34:E591–595. [DOI] [PubMed] [Google Scholar]
- 23.Rosenthal P, Kim KD. Cervical adjacent segment pathology following fusion: is it due to fusion? World J Orthop 2013; 4:112–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Eck JC, Humphreys SC, Lim TH, et al. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine (Phila Pa 1976) 2002; 27:2431–2434. [DOI] [PubMed] [Google Scholar]
- 25.Park DH, Ramakrishnan P, Cho TH, et al. Effect of lower two-level anterior cervical fusion on the superior adjacent level. J Neurosurg Spine 2007; 7:336–340. [DOI] [PubMed] [Google Scholar]
- 26.Puttlitz CM, Rousseau MA, Xu Z, et al. Intervertebral disc replacement maintains cervical spine kinetics. Spine (Phila Pa 1976) 2004; 29:2809–2814. [DOI] [PubMed] [Google Scholar]
- 27.Yang B, Li H, Zhang T, et al. The incidence of adjacent segment degeneration after cervical disc arthroplasty (CDA): a meta analysis of randomized controlled trials. PLoS One 2012; 7:e35032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boselie TF, Willems PC, van Mameren H, et al. Arthroplasty versus fusion in single-level cervical degenerative disc disease. Cochrane Database Syst Rev 2012; 9:CD009173. [DOI] [PubMed] [Google Scholar]
- 29.Gao Y, Liu M, Li T, et al. A meta-analysis comparing the results of cervical disc arthroplasty with anterior cervical discectomy and fusion (ACDF) for the treatment of symptomatic cervical disc disease. J Bone Joint Surg Am 2013; 95:555–561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Carrier CS, Bono CM, Lebl DR. Evidence-based analysis of adjacent segment degeneration and disease after ACDF: a systematic review. Spine J 2013. [DOI] [PubMed] [Google Scholar]
- 31.Hilibrand AS, Robbins M. Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J 2004; 4 (6 suppl):190S–194S. [DOI] [PubMed] [Google Scholar]


