Supplemental Digital Content is available in the text
Abstract
Revascularization aims at improving walking ability in patients with arterial claudication. The highest measured distance between 2 stops (highest-MDCW), the average walking speed (average-WSCW), and the average stop duration (average-DSCW) can be measured by global positioning system, but their evolution after revascularization is unknown.
We included 251 peripheral artery diseased patients with self-reported limiting claudication. The patients performed a 1-hour stroll, recorded by a global positioning system receiver. Patients (n = 172) with confirmed limitation (highest-MDCW <2000m) at inclusion were reevaluated after 6 months. Patients revascularized during the follow-up period were compared with reference patients (ie, with unchanged lifestyle medical or surgical status). Other patients (lost to follow-up or treatment change) were excluded (n = 89).
We studied 44 revascularized and 39 reference patients. Changes in highest-MDCW (+442 vs. +13 m) and average-WSCW (+0.3 vs. −0.2 km h−1) were greater in revascularized than in reference patients (both P < 0.01). In contrast, no significant difference in average-DSCW changes was found between the groups. Among the revascularized patients, 13 (29.5%) had a change in average-WSCW, but not in highest-MDCW, greater than the mean + 1 standard deviation of the change observed for reference patients.
Revascularization may improve highest-MDCW and/or average-WSCW. This first report of changes in community walking ability in revascularized patients suggests that, beyond measuring walking distances, average-WSCW measurement is essential to monitor these changes. Applicability to other surgical populations remains to be evaluated.
Registration: http://www.clinicaltrials.gov/ct2/show/NCT01141361
INTRODUCTION
Patients with intermittent claudication resulting from lower-extremity peripheral artery disease (PAD) report impaired walking ability, as can also do patients with lumbar spinal stenosis, lower-limb neuropathy or certain musculoskeletal conditions.1,2 In claudication, the maximal walking distance (MWD) is defined by the distance covered before limb discomfort or pain forces the patient to stop walking. The MWD can be self-reported based on history (self-reported MWD) and estimated with questionnaires. In PAD, limitation can be subjectively estimated using the Walking Impairment Questionnaire (WIQ)3,4 or objectively assessed on a treadmill (MWD-on-treadmill).5 MWD-on-treadmill is the major outcome measure used to assess the effect of treatments on PAD patients with intermittent claudication.6–8 Previous studies have shown that walking impairment can be assessed in PAD patients using global positioning system (GPS) recorders.5,9–11 Interestingly, this technique allows for the measurement of the “highest measured distance between 2 stops during community walking” (highest-MDCW), a parameter that correlates with measurements of MWD-on-treadmill5 and with self-reported MWD.12 However, the GPS-measured distance is 3 to 4 times greater than the self-reported distance or the distance measured on a treadmill. Furthermore, parameters other than highest-MDCW, which are difficult to measure in the laboratory and are associated with walking impairment in PAD patients, can be analyzed with GPS.11 Among these parameters are the average walking speed (average-WSCW) of all walking bouts and the average duration of stops (average-DSCW) between 2 bouts of symptom-limited community walking.11 The duration of a walking stop has been shown to be a major determinant of immediately forthcoming walking ability.10 However, to date, changes in highest-MDCW, average-WSCW and average-DSCW have not been specifically studied in revascularized or reference patients (ie, an unchanged medical or surgical status).
We analyzed the following hypotheses: On average, highest-MDCW and average-WSCW would increase and average-DSCW would decrease (for those patients who still had to stop) due to revascularization, whereas no change would be observed in the reference group; At the individual level, various walking strategies (ie, in walking speed and or in distance) would be observed among revascularized patients, with certain patients preferentially increasing their highest-MDCW after revascularization, whereas other patients would preferentially increase their average-WSCW. This point was of particular interest because if this hypothesis were true, the estimation of MWD alone with the usual tools could lead to underestimation of the functional benefit for those patients who increase their average-WSCW rather than their highest-MDCW; and WIQ-distance score changes and highest-MDCW changes would be reasonably correlated together whereas a weaker correlation would be found between WIQ-speed score changes with average-WSCW changes.
METHODS
The protocol was approved and monitored by the University Hospital of Angers (France) and performed according to the international ethics standards and the Declaration of Helsinki. The “Post-GPS” study was approved by the CPP-Ouest-II ethics committee and registered under the reference no. NCT01141361 (ClinicalTrials.gov). Twenty different physicians participated in the study (9 angiologists, 8 vascular surgeons, 2 cardiologists, and 1 rehabilitation physician). The present multi-center study is the second part of previously reported results on the applicability of GPS recording in clinical routine.11
Inclusion Criteria
Patients fulfilling the inclusion criteria (Table 1) were invited to participate. Patients provided written consent after being provided with oral and written information about the protocol.
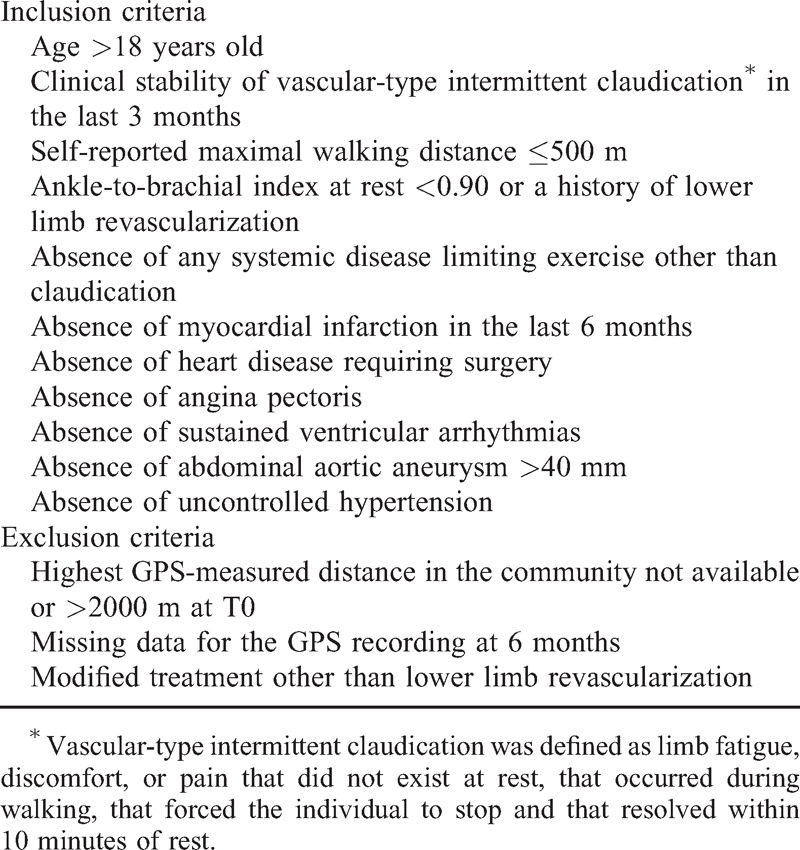
TABLE 1.
Inclusion and Exclusion Criteria
Procedures
We recorded the characteristics of each patient, including gender, age, stature, body weight, the ankle-to-brachial index (ABI; lowest right or left ABI, with ABI calculated as the highest ankle value divided by the highest arm pressure) and self-reported MWD. Thereafter, patients were provided clinical questionnaires that included specific items asking about their medical and surgical histories and ongoing medication, in addition to the Physical Activity Scale for the Elderly (PASE) questionnaire and the WIQ.3,4 Lastly, patients were given oral and written walking (Figure 1) and technical instructions as well as a GPS device to record a 1-hour outdoor stroll in the community. To avoid any confusion between the walking ability measured by the questionnaires and the ability measured by GPS, the outdoor community walk is referred to as a “stroll” throughout this paper, although patients were asked to walk at a regular pace. A pre-stamped envelope was provided to each patient to return the questionnaires and the GPS device to the coordinating center after the stroll. As previously reported,5,10,14 we used DG-100 GPS data loggers and the AT-65 GPS Active Antenna (GlobalSat Technology Corp., New Taipei City, Taiwan) that included the “European Geostationary Navigation Overlay Service” function. The recording rate was preset to 0.5 Hz. Patients only had access to the start and stop buttons of the recorder. Patients were asked to walk at their usual pace for 1 hour on a flat area free of compact trees or buildings. They were instructed to stop only because of lower limb pain and not necessarily to wait for the pain to disappear before beginning walking again.
FIGURE 1.
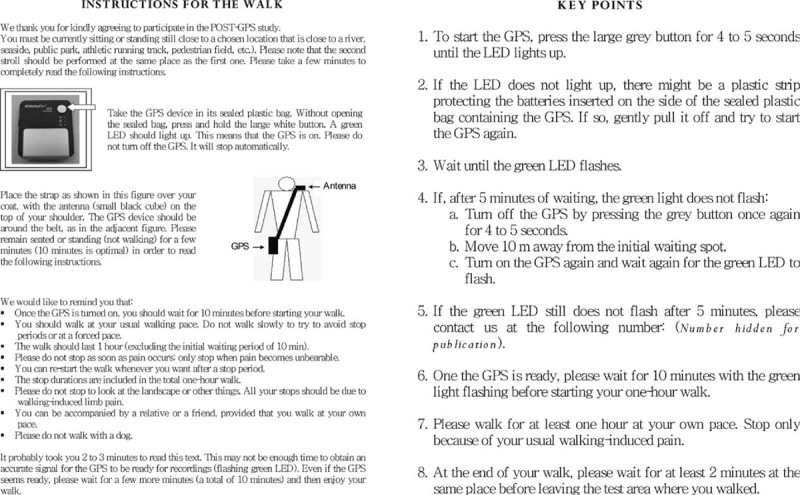
English translation of the recto-verso recommendation sheet provided to each patient for the stroll.
GPS Analysis
Validation of the use of the GPS technique to analyze walking parameters in healthy and PAD patients has been reported elsewhere.10,14 In brief, GPS-derived parameters included the total distance walked, the total duration of the walk (including the stop duration), the number of stops, highest-MDCW, average-WSCW and average-DSCW. A technically satisfactory recording was defined as11: a total walk duration >30 minutes, the presence of recorded data in the GPS device, and the presence of identifiable periods of walking (a succession of periods of displacement compatible with walking, that is, with speeds between 1 and 10 km h−1 and with durations of at least 10 seconds). At time-0 (T0) and time-1 (T1), if the recording was not technically satisfactory, a second attempt was performed within a month of the first attempt.
Follow-up, Exclusion Criteria and Inter-Current Events
Please note that the study is not randomizing patients into different treatment groups but just observing what happened over the follow up period. Following the initial 1-hour stroll (T0), patients for whom a technically satisfactory GPS recording was not available at T0 or who had GPS recording results that were inconsistent with walking limitations (ie, highest-MDCW >2000 m) were excluded. Patients with a successful T0 measurement underwent a second test 6 months later (T1). T1 was eventually delayed to allow a minimum of 3 months to elapse after any surgical or medical event (e.g., revascularization, change in treatment, non-vascular surgery, infraction, and stroke). For the T1 test, the participating patients were recommended to follow the same instructions as for the first test. Following the walk at T1, these patients were asked to complete items on whether they had to stop for any reason other than limb pain (e.g., dyspnea, road crossing, tying shoelaces, urinating, etc.), whether or not they experienced lower limb pain during the walk. Finally, patients for whom no technically satisfactory GPS recording could be obtained after 2 attempts at T1 were also excluded from the study.
Analysis of Data
Patients were classified into the following groups based on treatments or medical status changes that occurred over the study follow-up period: i) revascularized patients were patients who had any type of lower-limb arterial surgery or angioplasty between T0 and T1; ii) reference patients were patients who had no apparent changes in their treatments or medical status and no revascularization procedures between T0 and T1; and iii) patients who had any type of medical or non-vascular surgical intervention between T0 and T1 (e.g., bone or spine surgery, rehabilitation program, modification of cardiovascular drug regimen) were excluded from the study. Excluded patients with available T0 and T1 tests (n = 32) are described in Supplemental Digital Content 1, http://links.lww.com/MD/A265.
Statistical Analysis
The normality of distribution was first assessed for variables of interest using the Kolmogorov-Smirnov test. For continuous variables, the data are expressed as the mean ± standard deviation (SD) for normally distributed variables and as the median [25th;75th percentiles] for non-normally distributed variables. For categorical variables, the data are expressed as numbers and percentages. Accordingly, for continuous variables, between-group differences were examined using paired-t tests (normally distributed variables) or a Wilcoxon test (non-normally distributed variables). For categorical variables, Fisher's exact test was used to assess differences between groups.
We referred to the mean + 1 SD of the changes observed in the reference group to detect meaningful improvements (ie, minimal clinically important improvement: MCII)15 in highest-MDCW, average-WSCW, WIQ-distance and WIQ-speed among the revascularized compared with the reference patients. The concordance between GPS changes and WIQ changes in speed or distance were analyzed with linear regression analysis and Pearson's coefficient of correlation. For all statistical tests, a 2-tailed probability level of P < 0.05 was used to indicate statistical significance. SPSS (V15.0 SPSS Inc., 2004) was used for all statistical analyses. The study was designed to include 250 patients, assuming that nearly half of the patients would have no limitations while walking at T0, would be lost to follow-up, or would have unsatisfactory recordings. We also expected that at least one-third of the patients would undergo revascularization during the follow-up period.
RESULTS
Population Description
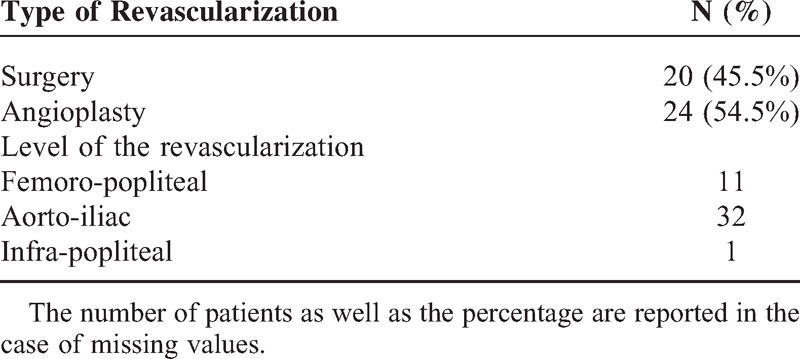
Of the 251 included patients, only 172 had limitations confirmed with GPS at T0 (79 exclusions). Among these 172 patients, 57 patients were excluded, mostly because they refused to perform the second test at T1, and another 32 were excluded because they could not be classified in the reference group because they had no revascularization but changes in medical, lifestyle or non-vascular surgical status between T0 and T1 (Figure 2). The clinical characteristics and results of the included patients at T0 are presented in Table 2. Note that the ABI was missing for 14 patients, either because “non-measurable pressure” or “incompressible arteries” were noted or, in 1 case, because of values that were missing from the data file. Of the 83 studied patients, 44 underwent revascularization (24 had angioplasty, and 20 had surgery) between T0 and T1 (Table 3). The median time interval between revascularization and T1 was 143 [110;176] days. In total, 39 patients reported no revascularization and no significant changes in treatments, rehabilitation or smoking habits between T0 and T1 (reference patients). Additionally, as shown in Table 2, no differences were found between revascularized and reference patients at T0. Thus, no adjustment was required in further analyses of changes in GPS parameters or other functional parameters between T0 and T1. As is also shown in Table 2, few PASE and WIQ questionnaires could not be scored despite the use of pre-defined rules to account for missing answers,3,4 because the patients had not filled out the questionnaires adequately.
FIGURE 2.
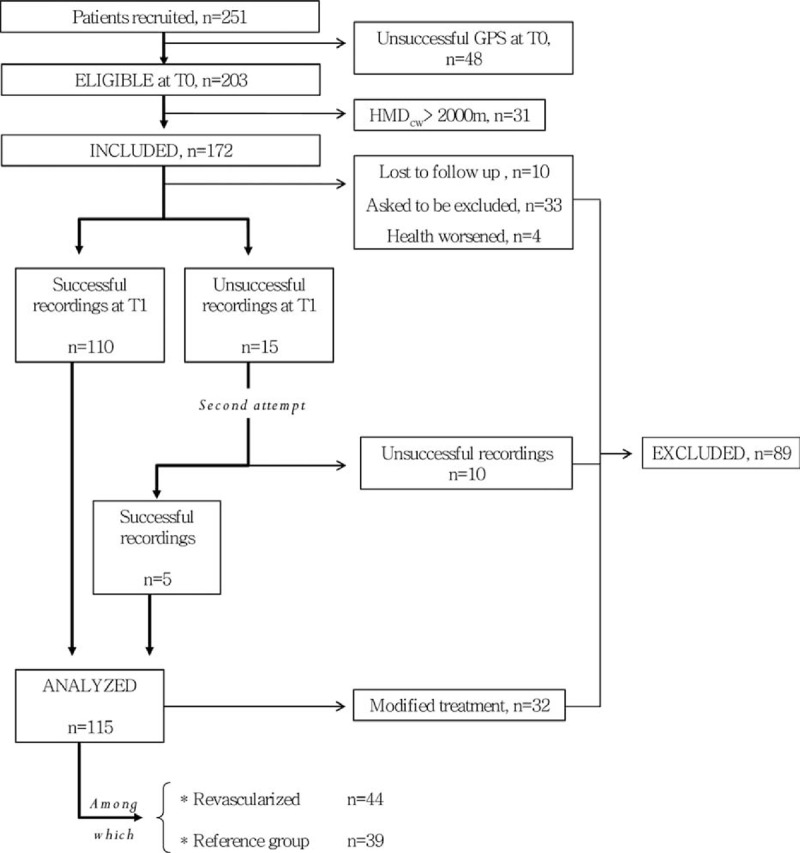
Flow diagram of the patients, with the corresponding numbers of technically satisfactory GPS recordings and the causes of technically unsuccessful GPS recordings.
TABLE 2.
Characteristics of the Patients at Inclusion (T0)
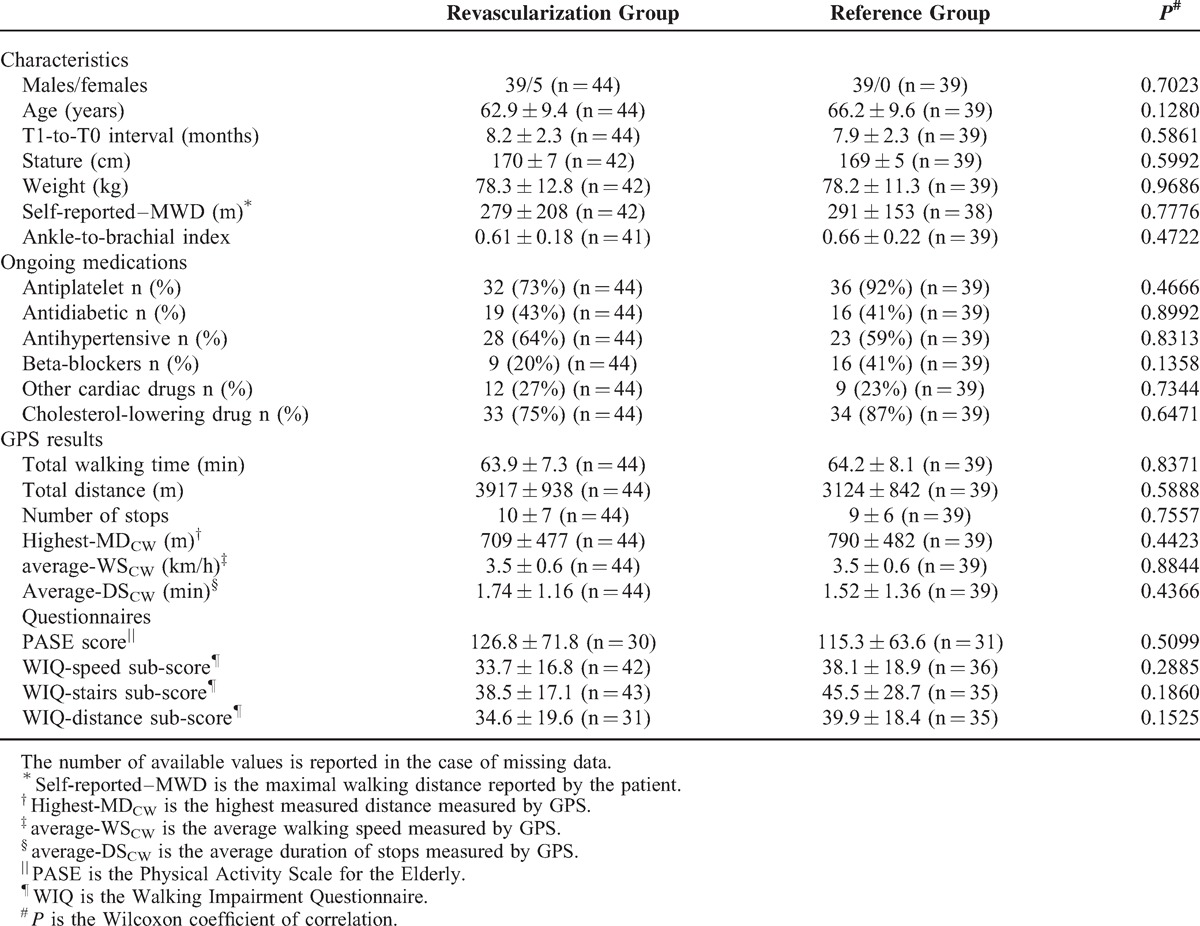
TABLE 3.
Type of Revascularization Occurring Between T0 and T1 Among Patients in the Revascularization Group
GPS Results
Two typical examples of GPS recordings, 1 in a patient who experienced revascularization and in a reference patient, are presented in Figure 3. Figure 3 illustrates the variability in walking bouts and stop durations observed at T0 and T1 and provides the values of highest-MDCW, average-DSCW and average-WSCW. As shown, important variability existed in the peak distances before each stop and in the stop durations during each stroll, whereas walking speed (which can be visually estimated from the slope of each walking bout) remained relatively stable throughout the different walking periods during the stroll. The revascularized patient (upper panel) had circled around 2 football fields. After revascularization, both highest-MDCW and average-WSCW increased, whereas average-DSCW decreased at T1 compared with T0. The reference patient (lower panel) walked along a lake during both strolls. Of interest is the fact that during T1, the patient B stopped multiple times for very short durations but covered a relatively long distance when the previous stop was long enough.
FIGURE 3.
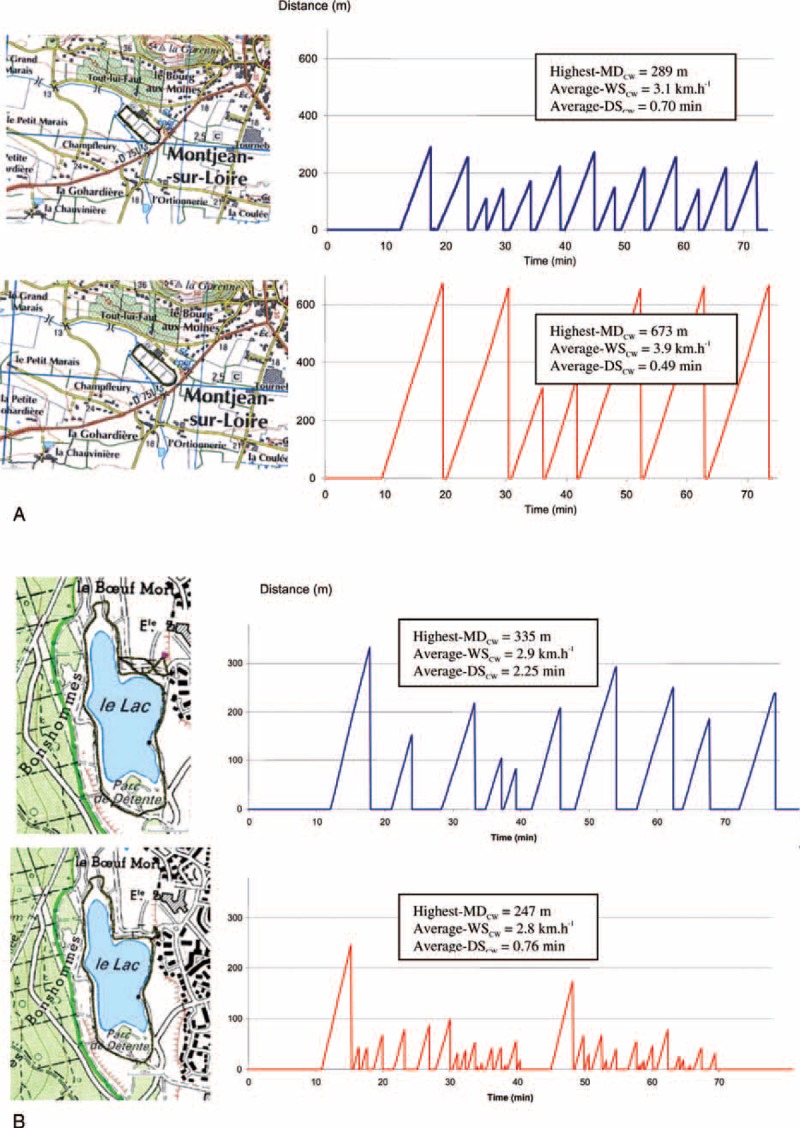
Typical recordings of the distance covered during each walking bout at T0 (upper panels) and T1 (lower panels) for 1 revascularized patient (A) and 1 reference patient (B).
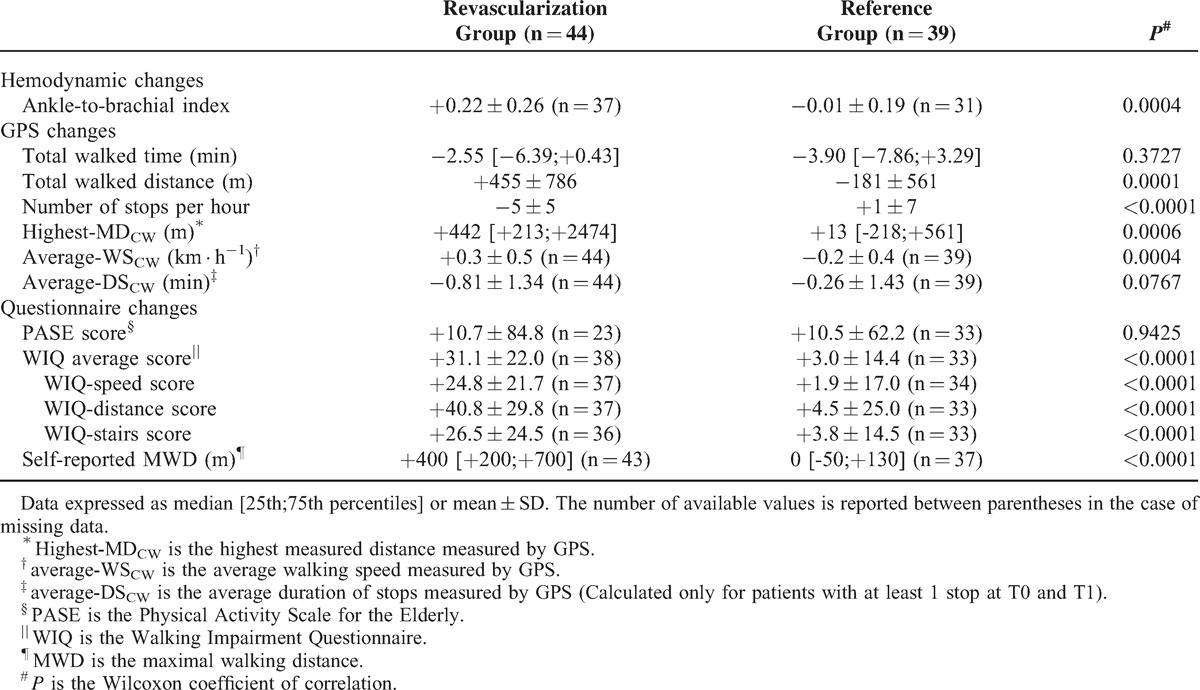
Average Changes Between T0 and T1
Changes in walking limitations that were estimated by the questionnaires and measured by GPS are reported by group in Table 4. As shown, for nearly all questionnaire results, the differences observed in revascularized patients were significantly higher than those found in reference patients. For GPS, the increases in highest-MDCW and average-WSCW were significantly higher in revascularized than in reference patients. However, although the decrease in average-DSCW was nearly 2 times higher in revascularized than in reference patients among those patients who still had to stop at T1, this difference did not reach statistical significance (P = 0.0767).
TABLE 4.
Walking Capacity Changes Between T0 and T1 Among the 83 Studied Patients (Revascularised Group vs. Reference Group)
Individual Changes Between T0 and T1
When using the mean + 1 SD of the changes in the reference group as limits for the detection of MCII among the 44 revascularized patients, 13 patients (29.5%) had MCII in both highest-MDCW and average-WSCW, 3 patients (7%) had MCII in highest-MDCW but non-improved average-WSCW, and 13 (29.5%) patients had MCII in average-WSCW but not highest-MDCW. The other 15 patients (34%) had no MCII in either the average-WSCW or highest-MDCW compared with the reference patients, as shown in Figure 4 (upper panel). However, among the 37 revascularized patients with available data for WIQ distance and speed sub-scores, 2 (5.5%) patients had MCII in both the WIQ distance and speed sub-scores, no patient (0%) had MCII in only the WIQ distance sub-score, and 10 (27%) patients had MCII in the WIQ speed sub-score but not the WIQ distance sub-score. The other 25 patients (67.5%) had no MCII in either the distance or the speed WIQ sub-scores compared with reference patients, as shown in Figure 4 (lower panel).
FIGURE 4.
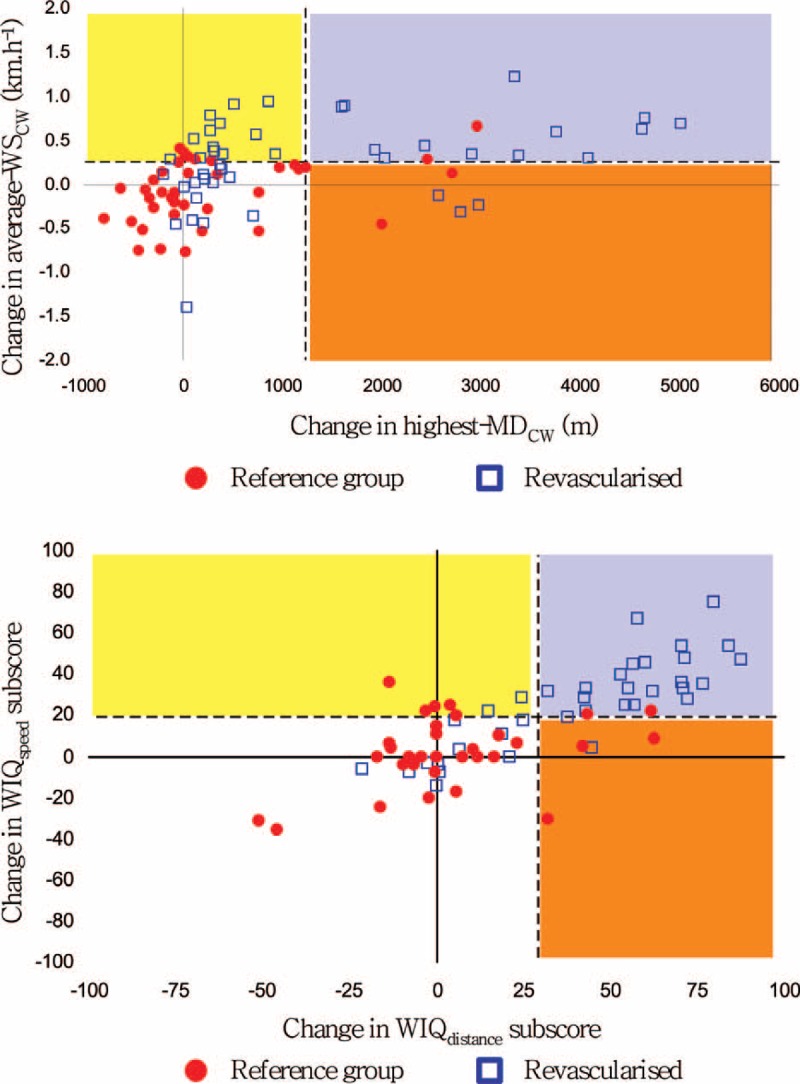
Changes in walking speed (average-WSCW) and the highest measured distance (highest-MDCW) during a community walk among reference (red dots) and revascularized patients (blue squares). The dashed lines represent the mean + 1 SD of changes needed to detect MCII compared with reference patients. Yellow square: average-WSCW or WIQ-speed improved only; Orange square: highest-MDCW or WIQ-distance improved only; Purple square: Both average-WSCW and highest-MDCW or both WIQ-speed and WIQ-distance improved; White square: No MCII.
Concordance of GPS and Questionnaire Changes
Finally, the correlation of highest-MDCW changes with WIQ-distance changes was statistically significant in the patients who had all data available (n = 96, r = 0.599; P < 0.001). The correlation of average-WSCW changes to WIQ-speed changes was also significant (n = 102, r = 0.394; P < 0.001).
DISCUSSION
Isolated case reports using GPS after spine surgery16 or amputation17 have recently been published. To the best of our knowledge, this is the first prospective multicenter study using GPS for the follow-up of revascularized and reference patients.
Many studies have analyzed the changes in MWD-on-treadmill or the changes in the WIQ score after revascularization, with results ranging from 163%18 to 176%19 and from 37%20 to 203%,21 respectively, but the correlation coefficient between the change in the total WIQ score and changes in MWD-on-treadmill has previously been reported to be low (r = 0.331).22 Additionally, we previously reported that self-reported MWD correlates fairly well with community-based measurements (ie, highest-MDCW), as assessed by GPS,12 even though highest-MDCW determined by GPS generally ranges around 3 times higher than self-reported MWD.5,10,12 Consistent with our previous observation,10 a wide variability of distances and stop durations were observed within a single stroll for each patient in the current study, whereas speed remained relatively stable (Figure 3). These findings explain our interest in studying highest-MDCW, average-WSCW and average-DSCW. However, no study to date has simultaneously and separately analyzed changes in highest-MDCW, average-WSCW and average-DSCW after surgery, specifically after revascularization. We report here for the first time that after revascularization, more than one-third of patients appear to improve their speed rather than their distance. This result is of major importance because usual walking speed improvement in the community is rarely studied or measured.
Walking speed has rarely been objectively measured in PAD patients with claudication, despite the well-known decrease in velocity in PAD compared with non-PAD patients,23,24 and despite the inverse relationship that exists between walking distance and walking intensity in claudicants.25,26 It has been shown that women with PAD have a slower walking speed than men do27 and that following revascularization, the WIQ-speed sub-score improves by 18.6%20 to 130%.21 Unlike distance, although significant, the correlation of the WIQ-speed subscore to average-WSCW changes was fair in the present study, suggesting that self-reported responses cannot reliably estimate changes in average-WSCW. Specifically, very few patients reported isolated speed improvement on the WIQ questionnaire, whereas GPS results suggested that more than one-third of patients had MCII in the average-WSCW without improvement in the highest-MDCW. One explanation could be that GPS underestimates the distance improvement in such patients. Another possibility could be that WIQ-distance changes and WIQ-speed changes are not sufficiently independent of one another to assess speed and distance changes separately. Many studies using the WIQ have shown that both the WIQ-speed and the WIQ-distance scores improved after revascularization,18,20–22 but no previous study has analyzed the relationship between measured distance changes and measured speed changes.
Whether certain patients preferentially maintain a constant speed and improve their distance, whereas others increase their walking speed rather than their maximal walking distance, is unknown. Furthermore, no previous study has confirmed these changes using objective measurements. Clearly, in the present study, many more patients had an MCII according to the GPS-derived highest-MDCW result than according to the WIQ-distance. The issue of speed and/or distance changes while walking is of major interest not only in revascularized patients but also in the evolution of PAD in patients. Indeed, in addition to hemodynamic tests, the gold standard for estimating the worsening of PAD is a decrease in MWD. Nevertheless, it is probable that certain patients progressively and unconsciously decrease their community walking speed, while their distance walked remains stable. At worst, the speed decrease could be so extreme that the patients remain asymptomatic while walking. Together with the decrease in lifetime recreational activity in PAD patients,28 this phenomenon could lead to patients remaining asymptomatic while their disease progresses. This situation might explain why the general prognosis of asymptomatic PAD patients is worse than that of symptomatic PAD patients.29 Walking speed for short walking bouts can be estimated using the time required to walk a fixed 4 m1,2,30,31 at the usual pace in a corridor, but there is no evidence that this laboratory measurement correlates to average-WSCW.
We initially expected average-DSCW to be an index of improved perfusion in revascularized patients. Indeed, the recovery time for muscle oxygenation accurately differentiates severe from moderate claudication,32,33 and angioplasty increases the hemoglobin oxygen recovery rate after exercise.34 Although we previously showed that the stop duration between 2 walking bouts limited by usual symptoms is probably an important predictor of forthcoming community-based walking impairment,10 the present study does not appear to confirm one of our initial hypothesis regarding this aspect. One explanation is the absence of concordance between pain relief and hemodynamic recovery in PAD patients.35 This lack of concordance could explain that the duration of a stop is less influenced by revascularization than the hemodynamic parameters are. The GPS device used does not allow physiological parameters to be analyzed, but future developments could allow for the recording of physiological signals and a better estimation of the relationship between average-DSCW and hemodynamic recovery.
Study Limitations
The limitations of the present study include the fact that we did not systematically study bypass patency or the results of angioplasty in terms of hemodynamic improvement (e.g., ABI or Doppler measurements) or MWD-on-treadmill, as many patients received their GPS at home at T1 and did not undergo de novo ABI measurement. It is also possible that certain patients in the revascularized group did not improve because their revascularizations failed. We hoped to avoid any additional visits for the routine follow-up of patients and to allow “at-home” estimation of walking limitation. These “at-home” procedures can also explain the relatively high number of missing scores, specifically for the WIQ and PASE, which are relatively complex questionnaires. Although it is clear that GPS will never replace vascular investigations, we think that it may improve our knowledge of the functional impairments that are associated with PAD.
A second limitation of this study is that we included only PAD patients with classical symptoms of intermittent claudication and for whom self-reported limitation was confirmed during the first GPS test. It would be of interest to evaluate the clinical applicability of and interest in the GPS technique in non-PAD patients (e.g., spinal stenosis, musculoskeletal lesions) or in PAD patients with atypical symptoms. It would also be of interest to analyze whether GPS may help to detect those patients who claim to be asymptomatic or who have stable moderate claudication but in fact progressively decrease walking speed rather than distance. Whether such patients require specific attention is a fascinating issue.
The third limitation is that the ability to perform GPS measurements may depend on the area where the system is used. The present study used a multicenter approach and appears to confirm that when patients are allowed to choose an area consistent with the study requirements, recordings of acceptable quality can be acquired in most cases.
Last, an hour-long stroll may be an unusually long exercise for most PAD patients with claudication. As most elderly patients walk <4000 steps per day,36,37 a 1-hour stroll may not reflect the usual physical activity of most patients. However, we previously showed that walking for 1 hour was considered very difficult in less than one-third of patients;11 nonetheless, reducing the duration of a stroll might dramatically affect the estimation of highest-MDCW (see Supplemental Digital Content 1, http://links.lww.com/MD/A265).
Conclusion and Clinical Perspective
The major results of the present study can be summarized as follows:
In patients who undergo revascularization for arterial claudication, highest-MDCW and average-WSCW are significantly increased. On the contrary average-DSCW changes in revascularized patients do not reach significance compared with reference patients.
Among revascularized patients with MCII compared with reference patients, nearly one-third of the patients increased their average-WSCW, but not their highest-MDCW, emphasizing the importance of evaluating speed changes in PAD patients.
The correlation between average-WSCW and WIQ-speed changes is weaker than between highest-MDCW and WIQ-distance changes.
Previous studies have demonstrated the accuracy of GPS in measuring community-based walking dimensions such as highest-MDCW, average-WSCW and average-DSCW10,12,13 in PAD patients. To the best of our knowledge, this is the first prospective multicenter follow-up study using GPS in patients with claudication. Although the present study focused on PAD patients, we assume that the technique could provide new data and interesting information on changes in walking impairment resulting from various medical or surgical treatments. Of major interest is the fact that, at least in PAD, average-WSCW appears essential to account for the changes observed in revascularized patients, beyond the measurement of walking distance alone.
Acknowledgments
The authors are indebted to Nafi Ouedraogo (MD, PhD), Johann Marchand (MD), Yoanna Onillon, Thomas Sauvaget, Jean-Marie Chrétien (DRCi–Methodology/Biostatistics/Data Management Unit) and Nicolas Hermann for their technical assistance. Moreover, the authors would like to thank the following physicians (in alphabetic order) for their help: Drs Philippe Berlie, Sonia Dulong, Thierry Dutartre, Dominique Eveno, Vincent Jaquinandi, Eric Jouen, Yann Jousset, Georges Leftheriotis, Jean-Pierre Lumineau, Patrick Moreau, Laurent Muller, Jean-Dominique Pegis, Arnaud Perrouillet, and Olivier Regnard.
Footnotes
Abbreviations: ABI = Ankle to brachial index, DSCW = Stop Duration between walking bouts during Community Walking, GPS = Global Positioning System, MCII = Minimal clinically important improvement, MDCW = Measured Distance in Community Walking between two symptom-limited stops. One patient may have multiple MDCW in a 1 hour recording, MWD = Maximal Walking Distance, The absolute maximal distance walked before limb discomfort or pain forces the patient to stop, PAD = Peripheral Arterial disease, PASE = Physical Activity Scale for the Elderly, WIQ = Walking Impairment Questionnaire, WSCW = Walking Speed During Community Walking: Mean walking speed between two stops during community walking.
This study was supported by a grant from the French Ministry of Health (PHRCR 2009–05; Eudract number: 2008-A01244–51) and was funded in part by the GENESIA foundation. No conflicts of interest are declared.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Website (www.md-journal.com).
REFERENCES
- 1.McDermott MM, Liu K, Greenland P, et al. Functional decline in peripheral arterial disease: associations with the ankle brachial index and leg symptoms. JAMA 2004; 292:453–461. [DOI] [PubMed] [Google Scholar]
- 2.McDermott MM, Liu K, Ferrucci L, et al. Decline in functional performance predicts later increased mobility loss and mortality in peripheral arterial disease. J Am Coll Cardiol 2011; 57:962–970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McDermott MM, Liu K, Guralnik JM, et al. Measurement of walking endurance and walking velocity with questionnaire: validation of the walking impairment questionnaire in men and women with peripheral arterial disease. J Vasc Surg 1998; 28:1072–1081. [DOI] [PubMed] [Google Scholar]
- 4.Hiatt WR, Hirsch AT, Regensteiner JG, et al. Clinical trials for claudication. Assessment of exercise performance, functional status, and clinical end points. Vascular Clinical Trialists. Circulation 1995; 92:614–621. [DOI] [PubMed] [Google Scholar]
- 5.Le Faucheur A, Abraham P, Jaquinandi V, et al. Measurement of walking distance and speed in patients with peripheral arterial disease: a novel method using a global positioning system. Circulation 2008; 117:897–904. [DOI] [PubMed] [Google Scholar]
- 6.Dormandy JA, Rutherford RB. Management of peripheral arterial disease (PAD). TASC Working Group. TransAtlantic Inter-Society Consensus (TASC). J Vasc Surg 2000; 31 (1 Pt 2):S1–S296. [PubMed] [Google Scholar]
- 7.Fakhry F, van de Luijtgaarden KM, Bax L, et al. Supervised walking therapy in patients with intermittent claudication. J Vasc Surg 2012; 56:1132–1142. [DOI] [PubMed] [Google Scholar]
- 8.Anonymous. Management of peripheral arterial disease (PAD). TransAtlantic Inter-Society Consensus (TASC). Eur J Vasc Endovasc Surg 2000; 19 Suppl A: Si-xxviii, S1-250. [PubMed] [Google Scholar]
- 9.Nordanstig J, Broeren M, Hensater M, et al. Six-minute walk test closely correlates to “real-life” outdoor walking capacity and quality of life in patients with intermittent claudication. J Vasc Surg 2014; 60:404–409. [DOI] [PubMed] [Google Scholar]
- 10.Le Faucheur A, Noury-Desvaux B, Mahe G, et al. Variability and short-term determinants of walking capacity in patients with intermittent claudication. J Vasc Surg 2010; 51:886–892. [DOI] [PubMed] [Google Scholar]
- 11.Gernigon M, Le Faucheur A, Noury-Desvaux B, et al. Applicability of global positioning system for the assessment of walking ability in patients with arterial claudication. J Vasc Surg 2014; 60:973–981. [DOI] [PubMed] [Google Scholar]
- 12.Tew G, Copeland R, Le Faucheur A, et al. Feasibility and validity of self-reported walking capacity in patients with intermittent claudication. J Vasc Surg 2013; 57:1227–1234. [DOI] [PubMed] [Google Scholar]
- 13.Le Faucheur A, Abraham P, Jaquinandi V, et al. Study of human outdoor walking with a low-cost GPS and simple spreadsheet analysis. Med Sci Sports Exerc 2007; 39:1570–1578. [DOI] [PubMed] [Google Scholar]
- 14.Abraham P, Noury-Desvaux B, Gernigon M, et al. The inter- and intra-unit variability of a low-cost GPS data logger/receiver to study human outdoor walking in view of health and clinical studies. PLoS One 2012; 7:e31338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Copay AG, Subach BR, Glassman SD, et al. Understanding the minimum clinically important difference: a review of concepts and methods. Spine J 2007; 7:541–546. [DOI] [PubMed] [Google Scholar]
- 16.Barzilay Y, Noam S, Meir L, et al. Assessing the outcomes of spine surgery using global positioning systems. Spine (Phila Pa 1976) 2011; 36:E263–E267. [DOI] [PubMed] [Google Scholar]
- 17.Jayaraman A, Deeny S, Eisenberg Y, et al. Global position sensing and step activity as outcome measures of community mobility and social interaction for an individual with a transfemoral amputation due to dysvascular disease. Phys Ther 2014; 94:401–410. [DOI] [PubMed] [Google Scholar]
- 18.Murphy TP, Soares GM, Kim HM, et al. Quality of life and exercise performance after aortoiliac stent placement for claudication. J Vasc Interv Radiol 2005; 16:947–953.quiz 954. [DOI] [PubMed] [Google Scholar]
- 19.Jaquinandi V, Picquet J, Saumet JL, et al. Functional assessment at the buttock level of the effect of aortobifemoral bypass surgery. Ann Surg 2008; 247:869–876. [DOI] [PubMed] [Google Scholar]
- 20.Matsumura JS, Yamanouchi D, Goldstein JA, et al. The United States StuDy for EvalUating EndovasculaR TreAtments of Lesions in the Superficial Femoral Artery and Proximal Popliteal By usIng the Protege EverfLex NitInol STent SYstem II (DURABILITY II). J Vasc Surg 2013; 58:73–83. [DOI] [PubMed] [Google Scholar]
- 21.Regensteiner JG, Hargarten ME, Rutherford RB, et al. Functional benefits of peripheral vascular bypass surgery for patients with intermittent claudication. Angiology 1993; 44:1–10. [DOI] [PubMed] [Google Scholar]
- 22.Nicolai SP, Kruidenier LM, Rouwet EV, et al. The walking impairment questionnaire: an effective tool to assess the effect of treatment in patients with intermittent claudication. J Vasc Surg 2009; 50:89–94. [DOI] [PubMed] [Google Scholar]
- 23.McDermott MM, Ohlmiller SM, Liu K, et al. Gait alterations associated with walking impairment in people with peripheral arterial disease with and without intermittent claudication. J Am Geriatr Soc 2001; 49:747–754. [DOI] [PubMed] [Google Scholar]
- 24.McCully K, Leiper C, Sanders T, et al. The effects of peripheral vascular disease on gait. J Gerontol A Biol Sci Med Sci 1999; 54:B291–294. [DOI] [PubMed] [Google Scholar]
- 25.Gardner AW, Skinner JS, Vaughan NR, et al. Comparison of treadmill walking and stair climbing over a range of exercise intensities in peripheral vascular occlusive disease. Angiology 1993; 44:353–360. [DOI] [PubMed] [Google Scholar]
- 26.Degischer S, Labs KH, Aschwanden M, et al. Reproducibility of constant-load treadmill testing with various treadmill protocols and predictability of treadmill test results in patients with intermittent claudication. J Vasc Surg 2002; 36:83–88. [DOI] [PubMed] [Google Scholar]
- 27.McDermott MM, Greenland P, Liu K, et al. Sex differences in peripheral arterial disease: leg symptoms and physical functioning. J Am Geriatr Soc 2003; 51:222–228. [DOI] [PubMed] [Google Scholar]
- 28.Wilson AM, Sadrzadeh-Rafie AH, Myers J, et al. Low lifetime recreational activity is a risk factor for peripheral arterial disease. J Vasc Surg 2011; 54:427–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McDermott MM, Guralnik JM, Ferrucci L, et al. Asymptomatic peripheral arterial disease is associated with more adverse lower extremity characteristics than intermittent claudication. Circulation 2008; 117:2484–2491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McDermott MM, Liu K, Ferrucci L, et al. Greater sedentary hours and slower walking speed outside the home predict faster declines in functioning and adverse calf muscle changes in peripheral arterial disease. J Am Coll Cardiol 2011; 57:2356–2364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McDermott MM, Tian L, Liu K, et al. Prognostic value of functional performance for mortality in patients with peripheral artery disease. J Am Coll Cardiol 2008; 51:1482–1489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Komiyama T, Shigematsu H, Yasuhara H, et al. Near-infrared spectroscopy grades the severity of intermittent claudication in diabetics more accurately than ankle pressure measurement. Br J Surg 2000; 87:459–466. [DOI] [PubMed] [Google Scholar]
- 33.Comerota AJ, Throm RC, Kelly P, et al. Tissue (muscle) oxygen saturation (StO2): a new measure of symptomatic lower-extremity arterial disease. J Vasc Surg 2003; 38:724–729. [DOI] [PubMed] [Google Scholar]
- 34.Beckitt TA, Day J, Morgan M, et al. Calf muscle oxygen saturation and the effects of supervised exercise training for intermittent claudication. J Vasc Surg 2012; 56:470–475. [DOI] [PubMed] [Google Scholar]
- 35.Gardner AW. Dissipation of claudication pain after walking: implications for endurance training. Med Sci Sports Exerc 1993; 25:904–910. [PubMed] [Google Scholar]
- 36.Storti KL, Arena VC, Barmada MM, et al. Physical activity levels in American-Indian adults: the Strong Heart Family Study. Am J Prev Med 2009; 37:481–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bennett GG, Wolin KY, Puleo E, et al. Pedometer-determined physical activity among multiethnic low-income housing residents. Med Sci Sports Exerc 2006; 38:768–773. [DOI] [PMC free article] [PubMed] [Google Scholar]


