Abstract
The objective of this study is to evaluate the degree of symptom improvement and the change of electrophysiological and ultrasonographic findings after sonographically guided local steroid injection using an in-plane ulnar approach in carpal tunnel syndrome (CTS).
Seventy-five cases of 44 patients diagnosed with CTS were included and evaluated at baseline and at 4 and 12 weeks after injection. All patients received injection with 40 mg of triamcinolone mixed with 1 mL of 1% lidocaine into the carpal tunnel using an in-plane Ultrasound (US)-guided ulnar approach, out-plane US-guided approach, and blind injection. For clinical evaluation, we used the Boston Carpal Tunnel Questionnaire (BCTQ) and electrophysiological tests. The ultrasonographic findings were also evaluated with regard to cross-sectional area and the flattening ratio of the median nerve.
Subjective symptoms measured by BCTQ and median nerve conduction parameters showed significant improvement at 4 weeks in the in-plane ulnar approach group compared with the out-plane ulnar approach and blind injection. This improvement was still observed at 12 weeks. The flattening ratio and cross-sectional area of the median nerve showed a more significant decrease with the in-plane ulnar approach than with the out-plane ulnar approach and blind injection (P < 0.05).
US-guided local steroid injection using an in-plane ulnar approach in the CTS may be more effective than out-plane or blind injection.
INTRODUCTION
Carpal tunnel syndrome (CTS) is caused by compression of the median nerve at the wrist level and the most frequent entrapment neuropathy in the upper limb.1 It can be treated with surgical or nonsurgical methods.2 When nonsurgical treatment is indicated, local corticosteroid injection into the carpal tunnel can be used to reduce pain and tingling sensation. On the contrary, direct needle injury of the median nerve is frequent and leakage of the corticosteroid injectate from the carpal tunnel causes complications such as fat tissue atrophy and skin color changes.3,4 Therefore, accurate injection into the carpal tunnel is very important.3 Ultrasound (US)-guided injection can confirm successful injection within the carpal tunnel visually so as to reduce patient discomfort, as well as median nerve injury. Although many approaching methods to carpal tunnel injection have been described, there is no sufficient evidence of one superior technique compared to the others.5–8
Currently, the most widely used CTS-injection method is the longitudinal approach, which paces the needle proximal to distal to the median nerve.7 However, this method cannot offer the benefits of carpal tunnel content images from transverse plane and needle shaft and tip simultaneously even under US guidance. So, even an accurately placed needle within the carpal tunnel following the technique may injure the median nerve because of anatomic variations such as a bifid median nerve or a median nerve in an abnormal location.4
Smith et al7 developed the ulnar approach methods for the performance of US-guided carpal tunnel injection in which the transducer is placed transversely along the wrist crease at the entrance to the carpal tunnel, and the needle is passed into the skin on the ulnar side of the proximal carpal tunnel at the level of the distal wrist crease. Technically, the ulnar approach combines the advantages of longitudinal needle visualization with the flexibility of transverse carpal tunnel imaging. In addition, this approach is easy to learn.
This study was conducted in order to evaluate the degree of symptom improvement, and the change of electrophysiological and sonographic findings after US-guided local steroid injection using an in-plane ulnar approach. We hypothesized that the in-plane ulnar approach injection technique provides better outcomes compared with the out-plane approach or blind injection technique in CTS.
MATERIALS AND METHODS
Patient Selection
Forty-four patients with mild to moderate idiopathic CTS with a neurophysiological confirmation were included in this study. Mild and moderate CTS were defined as slowing of the sensory conduction velocity and/or abnormal distal motor latency according to a validated CTS electrophysiological severity scale.9 We investigated outpatients with idiopathic CTS diagnosed by physical examination and electrodiagnosis. Participation was solicited without preselection. All patients had complaints of paresthesia or numbness in the median nerve distribution area of the hand with nocturnal worsening for a period of at least 3 months.
The exclusion criteria were symptomatic CTS because of diabetes, thyroid disease or rheumatic disease, age <18 years, pregnancy, previous treatment of CTS, previous fracture or deformities at the wrist, cervical radiculopathy, and other polyneuropathy. Approval from the Institutional Review Board of the Gachon University Gil Medical Center was obtained. All subjects participated in this study voluntarily, and informed consent on all aspects of the study was obtained.
Study Design and Therapeutic Intervention Techniques
This is a prospective randomized single-blind clinical trial comparing in-plane ulnar approach carpal tunnel injection versus out-plane carpal tunnel injection and blind injection of 40 mg of triamcinolone in patients with idiopathic CTS in terms of efficacy and safety. The patients were maintained in the supine position, with the forearm supinated and the wrist placed in slight dorsiflexion position to prevent change in the appearance of the median nerve according to wrist position (Figure 1).
FIGURE 1.
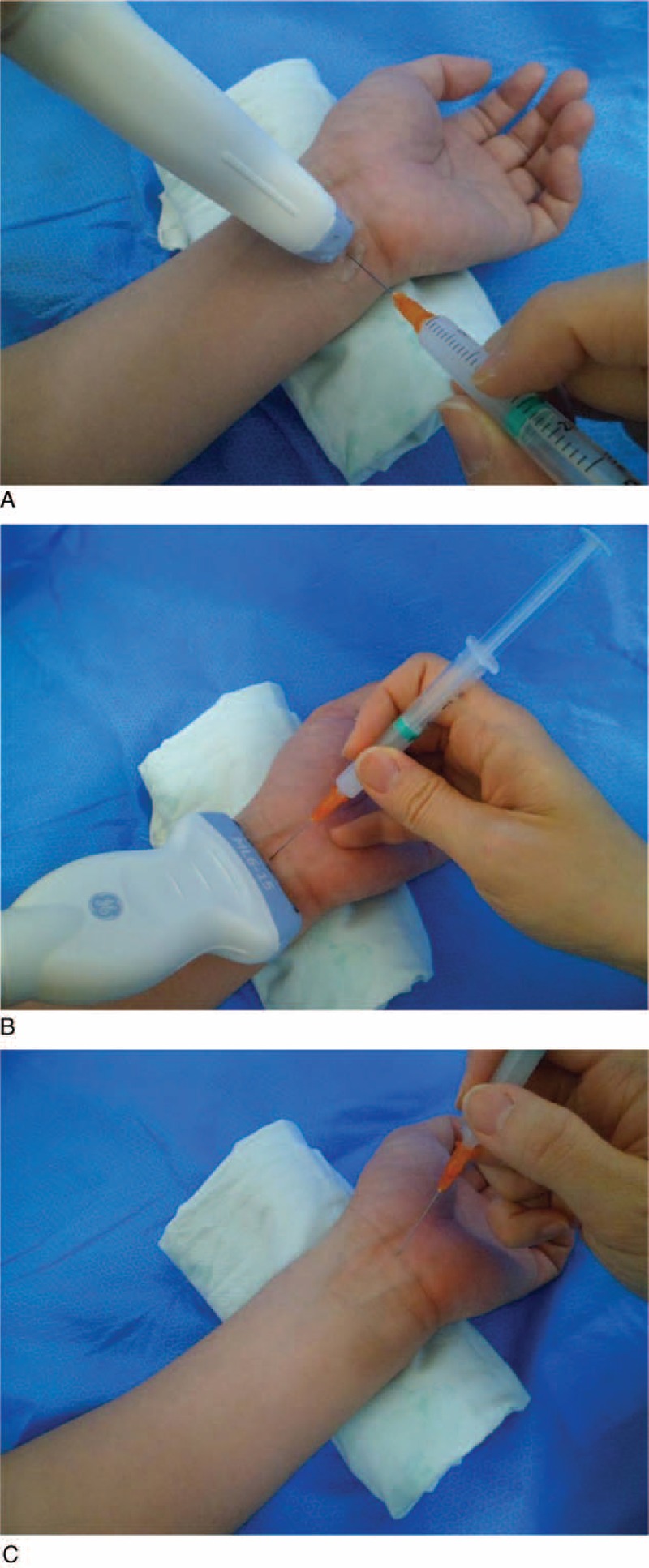
Transducer position and needle approach for each technique. (A) In-plane ulnar approach US-guided carpal tunnel injection, (B) out-plane US-guided carpal tunnel injection, and (C) blind injection. US = ultrasound.
In blind injection, after skin antisepsis, the 26-gauge needle was inserted into the proximal carpal tunnel at the distal wrist crease just ulnar to the palmaris longus tendon. The out-plane approach was performed using a perpendicularly placed transducer, and the needle was inserted into the proximal carpal tunnel at the distal wrist crease just ulnar to the palmaris longus tendon.4 The needle tip was identified as a moving reflector in real time as the tip passed obliquely from the skin surface to the proximal to distal carpal tunnel. In the in-plane ulnar approach, the transducer is moved ulnarly while keeping the median nerve in view (Figure 2A). In this manner, the pisiform, ulnar nerve, and ulnar artery are brought into view (Figure 2B).4 The pisiform appears as a prominent superiorly rounded hyperechoic structure on the ulnar side of the screen. The ulnar nerve lies just radial to the pisiform, and the ulnar artery lies radial to the ulnar nerve. Doppler images can confirm the position of the ulnar artery.7 Although the optimal injectable location has not been determined, target sign which is produced by injectate as a ring form structure is used as a proper injection guideline.
FIGURE 2.
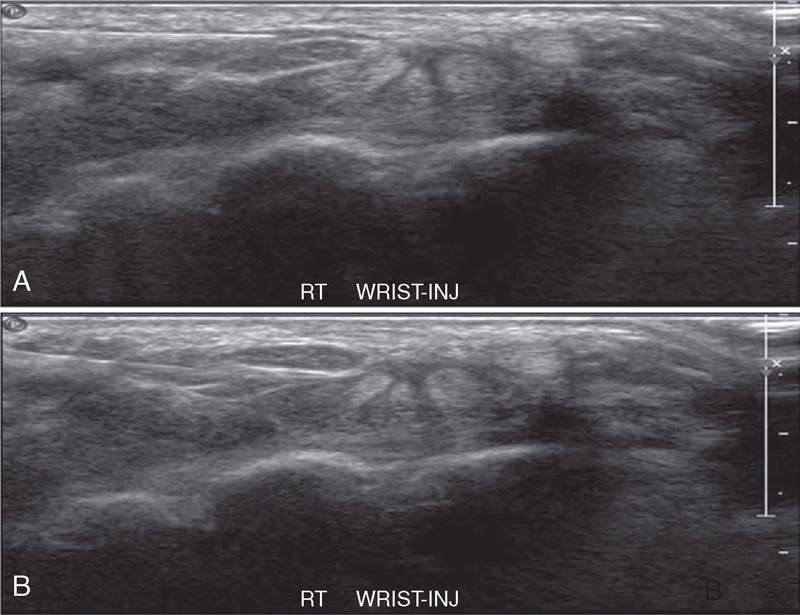
Transverse sonogram of the right carpal tunnel in a patient with idiopathic CTS. A 27-gauge needle is shown passing from the ulnar aspect of the carpal tunnel to a position adjacent to the median nerve. (A) After positioning the needle tip next to the nerve, the local anesthetic-corticosteroid mixture is injected in order to peel the nerve off the overlying flexor retinaculum via hydrodissection. (B) Anechoic injectate is shown surrounding the deep surface of the median nerve and separating it via hydrodissection from the more deeply positioned hyperechoic flexor tendons and associated synovium. CTS = carpal tunnel syndrome.
A typical injectate consists of 1 mL of 40 mg/mL triamcinolone and 1 mL of 1% lidocaine, delivered in equal portions above the nerve, below the nerve, and into the subsynovial connective tissue. After completion of the injection, the distal carpal tunnel is scanned to ensure distribution of injectate throughout the proximal-to-distal extent of the carpal tunnel.7 All injections were performed by the same physician. The US-guided injections were performed using an US device (GE healthcare, Hertfordshire, UK).
Review of Clinical Data
Patients were assessed at baseline, 4 weeks, and 12 weeks after the injection. The follow-up criteria were electrodiagnostic parameters, sonographic findings, and Boston Carpal Tunnel Questionnaire (BCTQ). Nerve conduction recordings were performed using a 2-channel electromyography machine, and bipolar handheld surface stimulating electrodes were used to obtain motor distal latency and compound motor action potentials (CMAPs) at abductor pollicis brevis muscle.3 The median nerve sensory distal latency (SDL) and sensory nerve action potential (SNAP) were evaluated at the second and fourth finger, and the ulnar nerve distal latency was evaluated at fourth digit to calculate median-to-ulnar sensory nerve distal latency ratio.
The median nerve cross-sectional area (CSA) was measured in transverse sections with ultrasonography looking for nerve enlargement at the carpal inlet and outlet. To identify the inlet, the bony landmarks of the scaphoid and pisiform were visualized, which in terms of surface markers approximates to the level of the distal wrist crease. The median nerve was then traced repeatedly from distal to proximal for identification of the maximal cross-sectional area. Once identified, the maximal CSA was evaluated and then the long diameter (LD), the short diameter (SD), and the flattening ratio (FR, SD/LD of the median nerve) were measured.6,10
For clinical evaluation, we used a validated questionnaire, the BCTQ at the inclusion date (baseline) and at 4- and 12-week follow-up. It is the most commonly used outcome measure of assessment for improvements in clinical symptoms and functional recovery of patients with CTS. The BCTQ evaluates the clinical symptoms (symptom severity scale, SSS), including pain, numbness, weakness, paresthesia, and clumsiness using 11 questions with the Likert scale preprinted 5 answers ranging from no complaints to very severe or continuous complaints. The functional handicap (functional status scale [FSS]) is calculated from 8 questions regarding difficulties with daily activities, including writing, holding a telephone, and so on, with a setup similar to the SSS. Each score is calculated as the mean of the responses of the individual items. A higher score indicates the worse symptom or function.7,11
Statistical Analysis
Statistical analyses were performed using the Statistical Package for the Social Sciences Program (SPSS Version 10.0). The main characteristics of patients were evaluated with descriptive studies. The divergence of outcome measure between baseline and posttreatment scores in the third and sixth months for each subject was computed by a general linear model for repeated measures. The level of statistical significance was set as P < 0.05.
RESULTS
Patient Flowchart
Forty-four patients, 75 hands, were enrolled in this study. Demographics, symptom duration, and bilateral involvement of the patients are shown in Table 1. Of the 44 patients diagnosed with CTS, the blind injection group included 15 patients, the out-plane US-guided injection group included 14 patients, and the in-plane ulnar approach US-guided injection group included 15 patients (Figure 3).
Table 1.
Demographics and Symptom Duration of the Patients According to Injection Groups
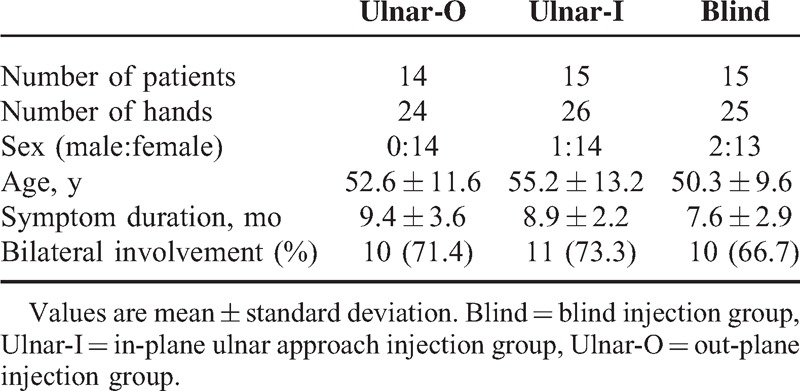
FIGURE 3.
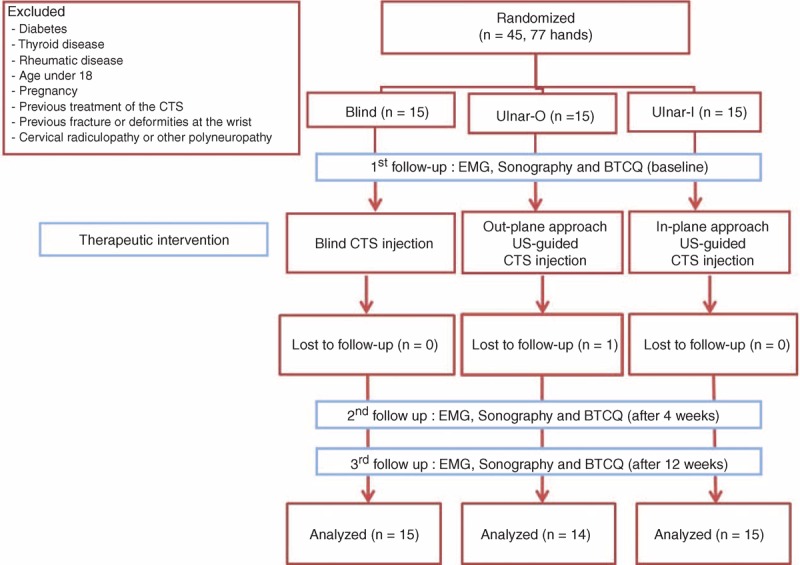
Patients’ flow diagram. BCTQ = Boston Carpal Tunnel Questionnaire, CTS = carpal tunnel syndrome, EMG = electromyography, I = in-plane, O = in-plane.
Electrodiagnostic Findings
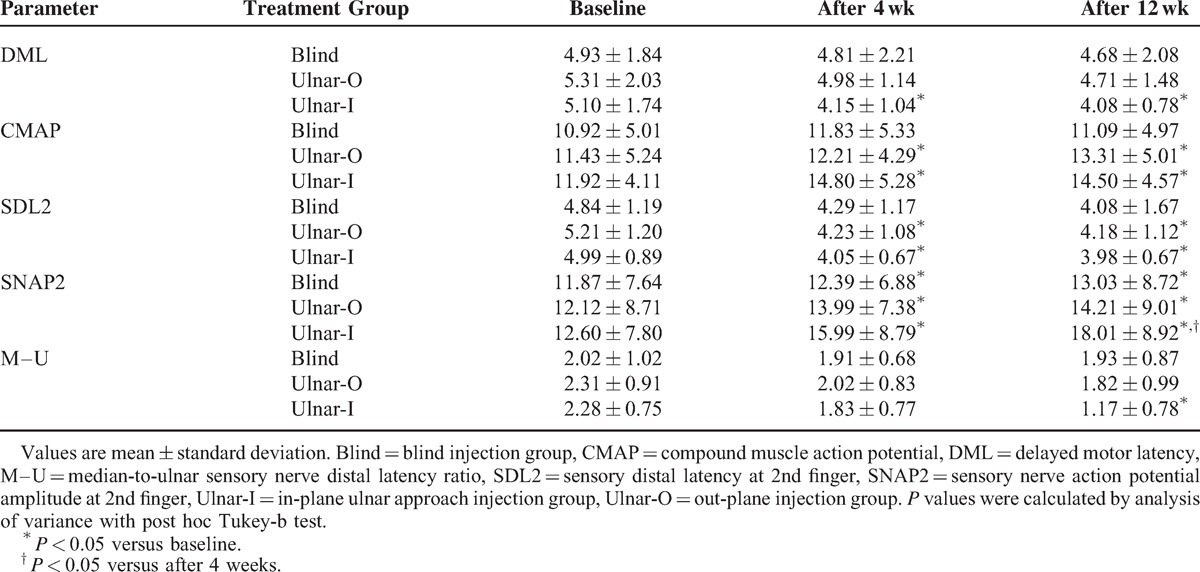
DML, CMAP amplitude, DSL, SNAP amplitude, and median-to-ulnar SDL ratio showed significant improvement at 4 and 12 weeks after the treatment in the in-plane ulnar approach. CMAP amplitude, SNAP amplitude, and SDL were improved at 4 and 12 weeks after out-plane US-guided injection. However, in blind injection, only SNAP amplitude showed statistical improvement after treatment.
At 4- and 12-week follow up, there were significant CMAP amplitudes showed significant improvement in the in-plane ulnar approach and out-plane US-guided injection, and the 2 methods were more efficient than blind injection. For SNAP amplitude at the second finger, significant improvements were observed in all the groups after injection. The in-plane ulnar approach was significantly superior to blind injection at 4 and 12 weeks, statistically. The median-to-ulnar SNAP amplitude ratio showed significant improvement in in-plane ulnar approach at 12 weeks after the treatment, and this method is statistically superior to blind injection or out-plane US-guided injection. There was no significant change in the median-to-ulnar ratio in blind injection or out-plane US-guided injection (Table 2).
Table 2.
Electrophysiological Findings of the Patients According to Injection
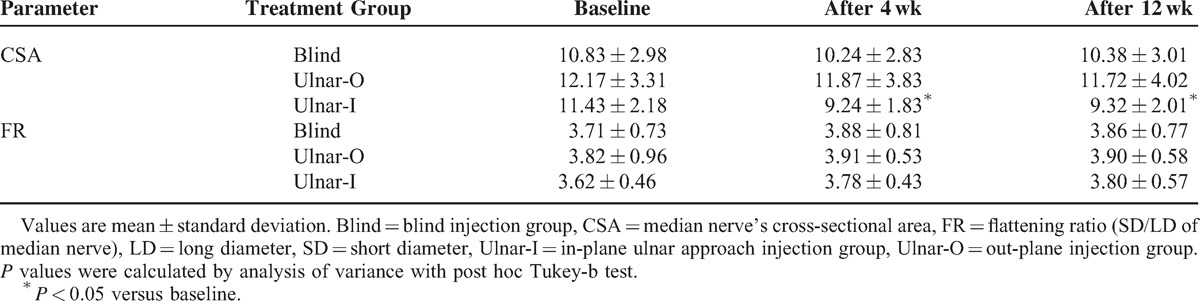
Sonographic Findings
In the blind injection and out-plane US-guided injection group, there were no significant decreases in CSA and FR. In the in-plane ulnar approach group, CSA showed a statistically significant increase at 4 and 12 weeks, and its result was superior to that of the other 2 groups (P < 0.05). However, the FR showed no change in all the groups (Table 3).
Table 3.
Sonographic Results of the Patients According to Injection
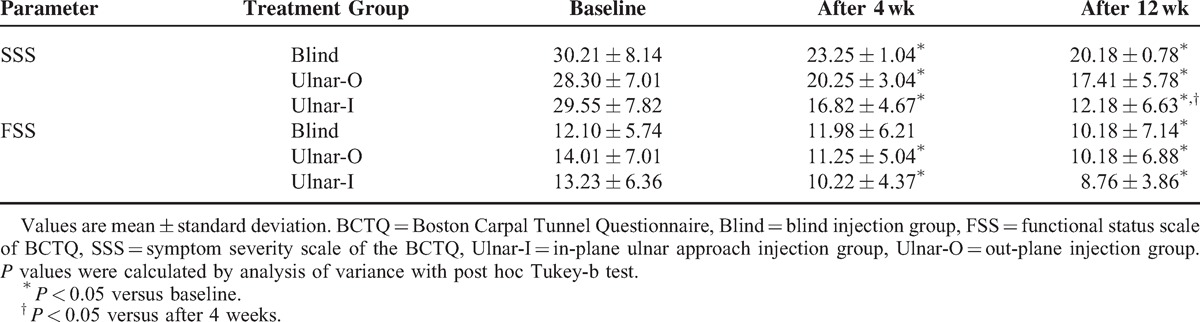
Changes in BCTQ Scores
Both the symptom (SSS) and functional scores (FSS) of the BCTQ showed significant improvement after 12 weeks in all patients (P < 0.05). Obviously, in the in-plane ulnar approach group, more rapid improvement was observed for SSS compared with other methods at 4 weeks. In the in-plane ulnar approach group, the SSS results at 4 and 12 weeks and the FSS result at 12 weeks were significantly superior to baseline (Table 4).
Table 4.
Clinical and Functional Evaluation of Patients With BCTQ
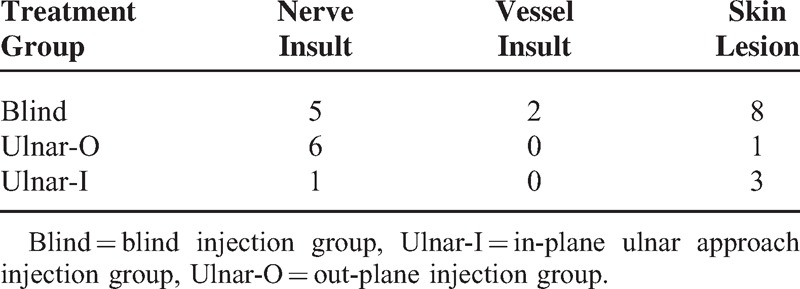
Complications
We checked complication after injection, including nerve insult, vessel insult, and skin lesion (eg, color change). Vessel insult was not detected in US-guided groups (out-plane US-guided injection and in-plane ulnar approach) and nerve insult was not detected in in-plane ulnar approach (Table 5).
Table 5.
Posttreatment Complication of the Patients
DISCUSSION
The primary purpose of this study is to compare the efficacy and safety of the in-plane ulnar approach in US-guided carpal tunnel injection with blind or out-plane US-guided injection. Although steroid injections are routinely administered for CTS, direct needle injury of the median nerve is the major complication of these injections. The safest location of the injection remains controversial. Several cases of median nerve injury during CTS injection have been reported.3
Racasan and Dubert3 reported median nerve irritation following carpal tunnel injection as a frequent problem and identified the fact that the median nerve extends ulnar to the palmaris longus tendon in most hands. They reported that the safest location of injection is through the flexor carpi ulnaris tendon.3 In the US-guided injection, the structure and location can be seen, so that the physician can reach the carpal tunnel without causing damage to neighboring tissue, and it enables visualization of the distribution of the injected substance.
In addition, the clinician can adjust the distance between the median nerve and the needle. Thus, the physician can come as close to the nerve as possible. If we assume the location of the median nerve and the needle is shown passing from the ulnar aspect of the carpal tunnel to a position adjacent to the median nerve, the injection procedure is easier to learn and provides a greater degree of needle control.
The in-plane ulnar approach has many advantages. First, imaging the wrist in the transverse plane enables visualization of all of the carpal tunnel contents and tendon structure around the nerve, facilitating an accurate perineural injection. Racasan and Dubert3 identified the fact that the median nerve extends ulnar to the palmaris longus tendon in most hands, the median nerve can extend up to 13 mm beyond the ulnar side of the palmaris longus tendon. From previous studies, it appears that the safest location for insertion of a needle for injection is through the flexor carpi radialis tendon, proximal to the carpal tunnel.3 However, the in-plane approach allows the needle to reach the median nerve directly with visualization of the whole structure of the carpal tunnel, and there is no penetrating tendon.
Second, both the needle tip and shaft can be visualized in plane relative to the transducer throughout the procedure. Transverse sonogram of the carpal tunnel in a patient with idiopathic CTS showed swelling of the median nerve. A 27-gauge needle is shown passing from the ulnar aspect of the carpal tunnel to a position adjacent to the median nerve, and after positioning the needle tip next to the nerve, the local anesthetic-corticosteroid mixture is injected in order to peel the nerve off the overlying flexor retinaculum via hydrodissection. Anechoic injectate is shown surrounding the deep surface of the median nerve and separating it via hydrodissection from the more deeply positioned hyperechoic flexor tendons and associated synovium. This hydrodissection may disrupt adhesions and encircling of the superior portion of median nerve. Under real-time visualization, additional injectate is delivered with redirected needle to the inferior portion of the nerve. Then, the median nerve was separated from the underlying subsynovial connective tissue.7
The most important advantage of the in-plane ulnar approach injection appears to be its view containing nerve and vessel with a visible needle. Accordingly, novice practitioners can approach the median nerve more easily from basic anatomy of the target tissue.
The current study does have some limitations, primarily the small patient group with female predominance and the lack of long-term follow-up. However, correlation of median nerve conduction parameters, subjective symptoms, and sonographic findings of the patients with injection methods was precisely proven. Likewise, we checked several complications after injection, including nerve insult, vessel insult, and skin lesion. Although there were no statistically significant findings, vessel insult was not detected in US-guided groups (out-plane US-guided injection and in-plane ulnar approach) and nerve insult was not detected in the in-plane ulnar approach. Subsequent to this study, we recommend that additional studies would require very large sample sizes in order to achieve more reliable results.
CONCLUSION
Although in-plane and out-plane US-guided carpal tunnel injection were more effective in improving electrodiagnostic, sonographic findings, and symptoms than blind injection, the in-plane ulnar approach was superior to the out-plane and blind injection in median-to-ulnar sensory nerve distal latency ratio SDL ratio, CSA, and BCTQ result. US-guided local steroid injection using an in-plane ulnar approach in the CTS can be more effective than out-plane or blind injection.
Footnotes
Abbreviations: BCTQ = Boston Carpal Tunnel Questionnaire, CMAP = compound motor action potential, CSA = cross-sectional area, CTS = carpal tunnel syndrome, FR = flattening ratio, FSS = functional status scale, LD = long diameter, SD = short diameter, SDL = sensory distal latency, SNAP = sensory nerve action potential, SSS = symptom severity scale, US = ultrasound.
JYL and YP contributed equally to this work as first authors.
The authors have no funding to disclose.
No conflicts of interest have been reported by the authors or by any individuals in control of the content of this article. We certify that no party having a direct interest in the results of the research supporting this article has or will confer a benefit on us or on any organization with which we are associated.
REFERENCES
- 1.Katz JN, Simmons BP. Clinical practice. Carpal tunnel syndrome. N Engl J Med 2002; 346:1807–1812. [DOI] [PubMed] [Google Scholar]
- 2.Andreu JL, Ly-Pen D, Millan I, et al. Local injection versus surgery in carpal tunnel syndrome: neurophysiologic outcomes of a randomized clinical trial. Clin Neurophysiol 2013; 125:1479–1484. [DOI] [PubMed] [Google Scholar]
- 3.Racasan O, Dubert T. The safest location for steroid injection in the treatment of carpal tunnel syndrome. J Hand Surg Br 2005; 30:412–414. [DOI] [PubMed] [Google Scholar]
- 4.Swan MC, Oestreich K. Re: median nerve damage following local corticosteroid injection for the symptomatic relief of carpal tunnel syndrome. J Hand Surg Eur 2009; 34:135–136. [DOI] [PubMed] [Google Scholar]
- 5.Grassi W, Farina A, Filippucci E, et al. Intralesional therapy in carpal tunnel syndrome: a sonographic-guided approach. Clin Exp Rheumatol 2002; 20:73–76. [PubMed] [Google Scholar]
- 6.Kim DH, Jang JE, Park BK. Anatomical basis of ulnar approach in carpal tunnel injection. Pain Physician 2013; 16:E191–E198. [PubMed] [Google Scholar]
- 7.Smith J, Wisniewski SJ, Finnoff JT, et al. Sonographically guided carpal tunnel injections: the ulnar approach. J Ultrasound Med 2008; 27:1485–1490. [DOI] [PubMed] [Google Scholar]
- 8.Wilson JK, Sevier TL. A review of treatment for carpal tunnel syndrome. Disability and rehabilitation 2003; 24:113–119. [DOI] [PubMed] [Google Scholar]
- 9.Padua L, LoMonaco M, Gregori B, et al. Bilateral clinical-neurophysiological assessment of median nerve in carpal tunnel syndrome patients. Muscle Nerve 1998; 21:264–265. [DOI] [PubMed] [Google Scholar]
- 10.Paliwal PR, Therimadasamy AK, Chan YC, et al. Does measuring the median nerve at the carpal tunnel outlet improve ultrasound CTS diagnosis? J Neurol Sci 2014; 339:47–51. [DOI] [PubMed] [Google Scholar]
- 11.Halil Ucan, Ilker Yagci, Lale Yilmaz, et al. Comparison of splinting, splinting plus local steroid injection and open carpal tunnel release outcomes in idiopathic carpal tunnel syndrome. Rheumatol Int 2006; 27:45–51. [DOI] [PubMed] [Google Scholar]


