Abstract
Information on post-transplant malignancy and mortality risk in kidney transplant tourists remains controversial and is an important concern. The present study aimed to evaluate the incidence of post-transplant malignancy and mortality risk between tourists and domestic transplant recipients using the claims data from Taiwan's universal health insurance.
A retrospective study was performed on 2394 tourists and 1956 domestic recipients. Post-transplant malignancy and mortality were defined from the catastrophic illness patient registry by using the International Classification of Diseases, 9th Revision. Cox proportional hazard regression and Kaplan–Meier curves were used for the analyses.
The incidence for post-transplant de novo malignancy in the tourist group was 1.8-fold higher than that of the domestic group (21.8 vs 12.1 per 1000 person-years). The overall cancer recurrence rate was approximately 11%. The top 3 post-transplant malignancies, in decreasing order, were urinary tract, kidney, and liver cancers, regardless of the recipient type. Compared with domestic recipients, there was significant higher mortality risk in transplant tourists (adjusted hazard ratio = 1.2, 95% confidence interval: 1.0–1.5). In addition, those with either pre-transplant or post-transplant malignancies were associated with increased mortality risk.
We suggest that a sufficient waiting period for patients with pre-transplant malignancies should be better emphasized to eliminate recurrence, and transplant tourists should be discouraged because of the possibility of higher post-transplant de novo malignancy occurrence and mortality.
INTRODUCTION
In 2008, the Declaration of Istanbul stated that all transplant-related organizations should “prevent organ traffic.”1 Given the high prevalence of end-stage renal disease (ESRD) in Taiwan and the relative shortage of organ donors, numerous patients receive overseas commercial kidney transplants annually (these patients are known as transplant tourists).2 The Taiwanese government disapproves this behavior, but transplant tourists are still granted a catastrophic illness card and, without discrimination, are provided the same medical care as the patients who have domestically received kidney transplants (domestic kidney recipients). Patients with catastrophic illness certifications, who obtain care for their illness or related conditions within the certificate's validity period, do not need to pay the copayment for outpatient or inpatient care (http://www.nhi.gov.tw).
In terms of patient and graft survival, previous studies in Taiwan and other countries reported that transplant tourists have similar3–7 or inferior8–10 outcomes compared with domestic recipients. However, no studies on pre-transplant and post-transplant malignancy occurrence, comparing transplant tourists with domestic recipients, have been conducted, except for 1 study conducted by a medical center in Taiwan.11
The present study was the largest study so far and based on a retrospective cohort study from a nationwide database. The purpose of this study was to determine the following: the incidence rates of pre-transplant and post-transplant malignancy in tourist and domestic kidney recipients; patient and graft survival in tourist and domestic kidney recipients; and the effects of malignancy occurrence prior to and after kidney transplant on prognosis.
METHODS
Data Source
We used the catastrophic illness patient registry and the inpatient database from the National Health Insurance Research Database (NHIRD). The NHIRD, which was established by the Taiwan Bureau of National Health Insurance (TBNHI) from the National Health Insurance Program, covers more than 99% of Taiwan residents.12,13 This database contains insurance information and medical claims of all 23 million insured individuals in Taiwan registered from 1996 to 2010. Disease diagnosis included details of medical orders, procedures, and medical diagnoses with codes based on the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) in NHIRD. Because patients applying for the catastrophic illness card are exempt from cost sharing, most patients with catastrophic illness apply for this card, including patients with cancer and those undergoing dialysis and renal transplantation. This arrangement could indirectly increase the validity of disease diagnoses in our analysis. Insurant identification was encrypted before the information was sent to the researcher. This study was approved by the Institutional Review Board, China Medical University Hospital, Taiwan (CMU-REC-101–012). Details of NHIRD are shown on the TBNHI web page (http://w3.nhri.org.tw/nhird/date_01.html).
Study Subjects
Patients with new kidney transplants (ICD-9-CM V42.0 or 996.81) between 1999 and 2009 were included in this study (N = 4507). In addition, diagnoses in kidney recipients were validated according to the Registry for Catastrophic Illness Patient card. We excluded patients aged <18 years (n = 121) and those who had multiple kidney transplants (n = 36). A total of 4350 patients were selected and divided into tourist and domestic groups according to the ICD-9-CM procedure code 55.69, which indicated that the subjects underwent the kidney transplant surgery in Taiwan. Patients with ICD-9-CM 55.69 and had applied for the catastrophic illness card were defined as the domestic group. In contrast, those who applied for the catastrophic illness card but without ICD-9-CM 55.69 were defined as the tourist group. The entry date of the kidney transplant in our analysis was defined as the date of the application for inclusion in the Registry for Catastrophic Illness Patients.
Outcome Variables
The outcomes included the development of post-transplant malignancy (ICD-9-CM 140–208), graft failure (recurrent ESRD, ICD-9-CM 585), and all-cause mortality. Outcome variables of post-transplant malignancy and graft failure were based on primary discharge diagnosis, application for the catastrophic illness card, and confirmation of these events with at least 3 medical visits to increase the validity of the diagnoses. All study subjects were followed up from the entry date until the occurrence of each event, loss to follow-up date, or the end of 2010.
Covariate Assessment
The tested variables included age, gender, occupation, geographic location, and comorbidity. Occupation was divided into 3 groups (white collar, blue collar, and other) according to the workplace. Geographic locations were classified into 4 regions (northern, central, southern, and eastern) based on the subject's residence. Comorbidity included diabetes (ICD-9-CM 250), hypertension (ICD-9-CM 401–405), coronary artery disease (CAD; ICD-9-CM 410–414), cerebrovascular disease (CVD; ICD-9-CM 430–438), pre-transplant malignancy history, hepatitis B viral infection (HBV; ICD-9-CM V02.61, 070.20, 070.22, 070.30, and 070.32), and hepatitis C viral infection (HCV; ICD-9-CM V02.62, 070.41, 070.44, 040.51, and 070.54). All comorbidities were defined before the entry date and were confirmed with at least 3 medical visits.
Statistical Analysis
The SAS 9.3 software for Windows (SAS Institute, Cary, NC) was used for all analyses, and the significance level was set to 0.05 in the 2-tailed test. χ2 and t tests were used to examine the differences in the distribution and the mean age, respectively, between the 2 groups. Mortality after kidney transplant, incidence of post-transplant malignancy, and recurrent ESRD per 1000 person-years were assessed in the 2 groups. The hazard ratios (HRs) and 95% confidence intervals (CIs) for the risk of malignancy and mortality were estimated using Cox proportional hazard regressions. Kaplan–Meier analysis was used to plot the disease-free rate and the cumulative incidence rate curve. The log-rank test was used to determine the difference between the 2 groups.
RESULTS
Comparison of Demographic Profiles of the Tourist and Domestic Groups
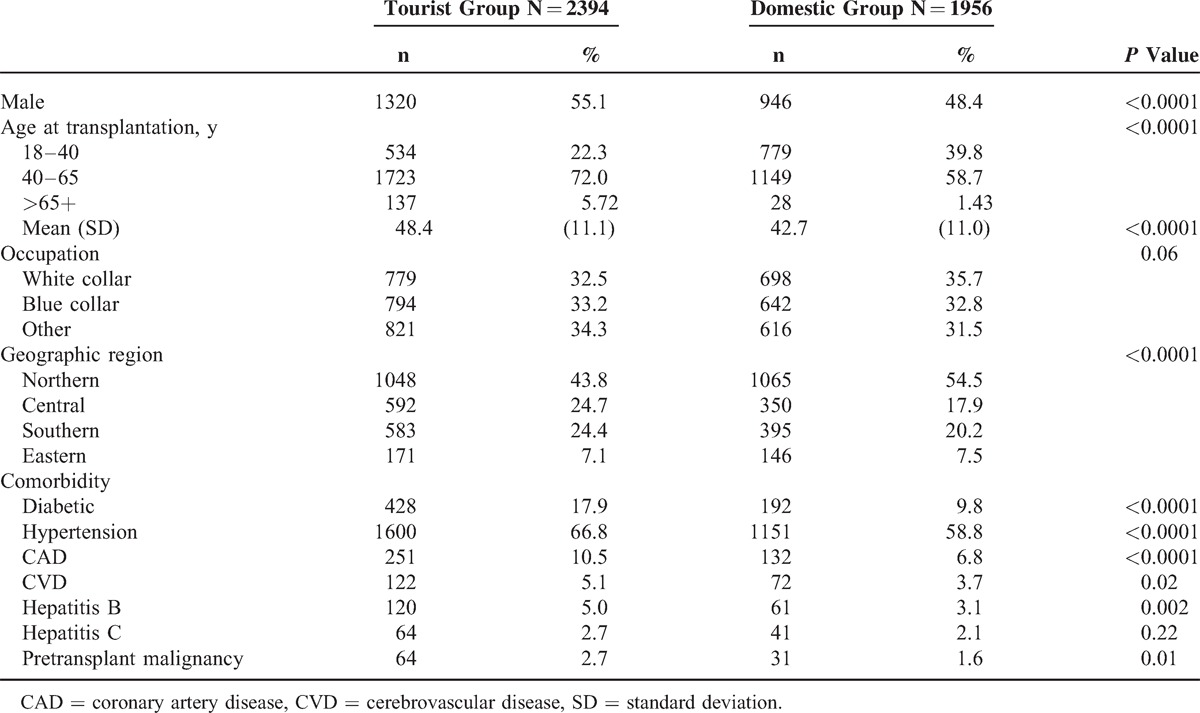
In total, 2394 and 1956 subjects were included in the analyses as tourist and domestic groups, respectively. Compared with the domestic group, the tourist group included more men (55.1% vs 48.4%) and was older (48.4 vs 42.7 years of age) (Table 1). More transplant tourist than domestic kidney recipients lived in the central and southern areas. The tourist group had more comorbidities than the domestic group, and the top 3 comorbidities were hypertension, diabetes, and CAD.
TABLE 1.
Demographic Profiles of the Tourist and Domestic Groups
Incidence and Risk of Post-Transplant Malignancy
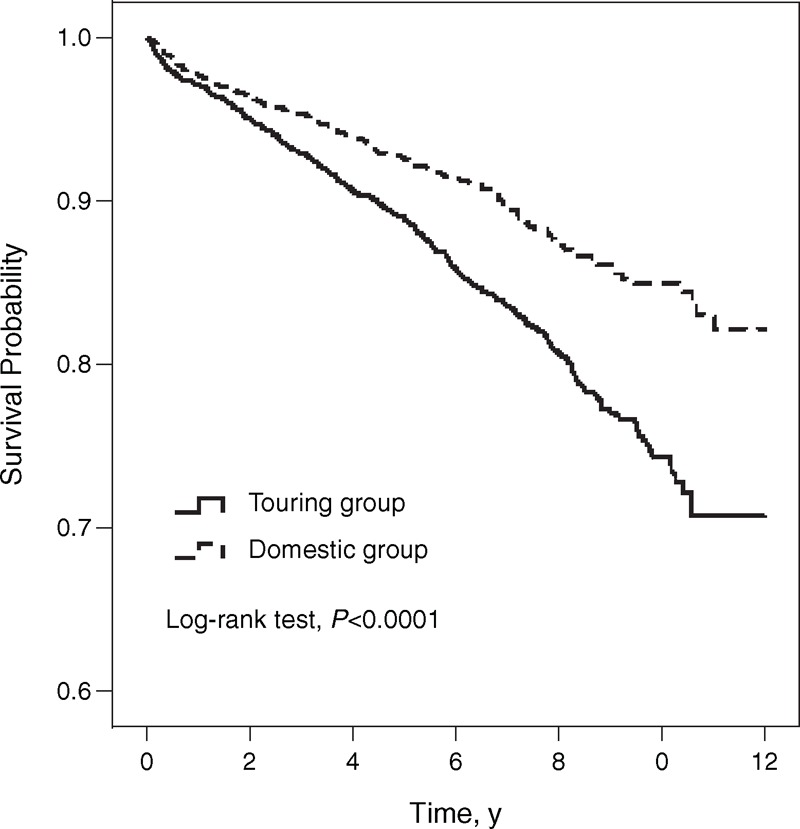
The mean follow-up durations were 5.6 and 5.2 years in the tourist and domestic groups, respectively. The incidence of post-transplant malignancy in the tourist group was 1.8-fold higher than that in the domestic group (21.8 vs 12.1 per 1000 person-years, Table 2). The Kaplan–Meier survival analysis during a 12-year follow-up period revealed that transplant tourists had significantly higher rates of post-transplant malignancy than domestic kidney recipients (log-rank P < 0.0001, Figure 1).
TABLE 2.
Incidence Rate and Hazard Ratios of Post-Transplant Malignancy Stratified by Follow-Up Years
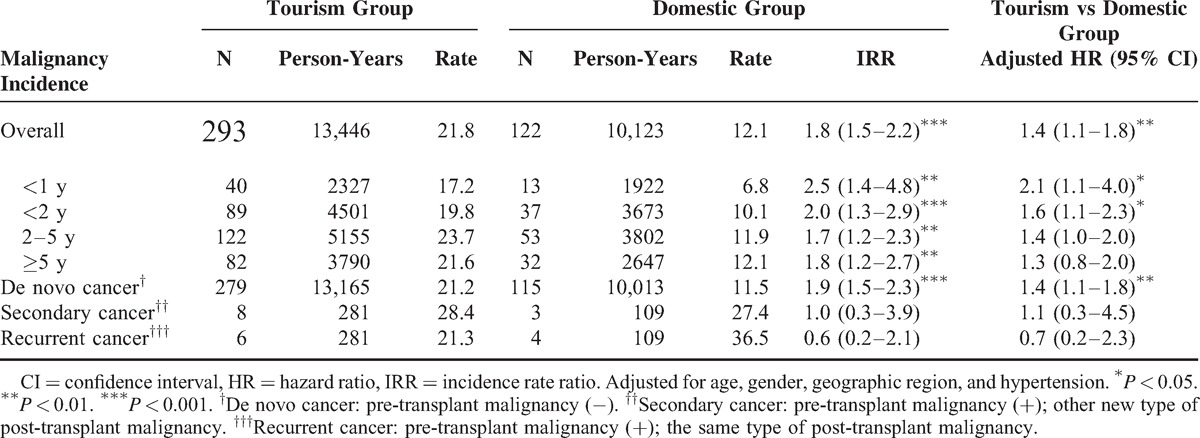
FIGURE 1.
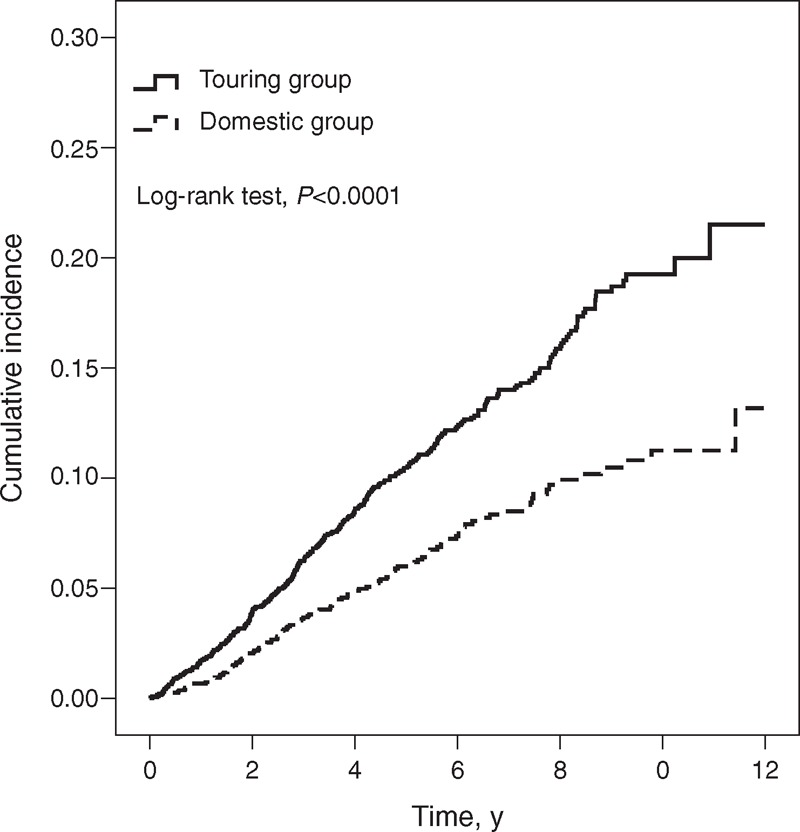
Cumulative incidence rates of overall post-transplant malignancy for the tourist (solid line) and domestic (dashed line) groups.
Pathology and Follow-Up Duration of Post-Transplant and Pre-Transplant Malignancies
A categorization of post-transplant and pre-transplant malignancies in the renal transplant group is presented in Table 3. The top 5 pre-transplant malignancies in the tourist group were urinary tract (25.0%), kidney (17.2%), liver (12.5%), breast (10.9%), and hematologic (9.4%) cancers, whereas malignancies in the domestic group included the kidney (25.8%), breast (22.6%), urinary tract (19.4%), thyroid (12.9%), head and neck (6.5%), and multiple (6.5%) cancers. The top 5 post-transplant malignancies in the tourist group were urinary tract (33.5%), kidney (22.9%), liver (14.3%), colorectal (4.4%), and lung (4.4%) cancers, whereas malignancies in the domestic group included urinary tract (43.4%), kidney (13.9%), liver (9.8%), hematologic (5.7%), and breast (4.1%) cancers. The time from pre-transplant malignancy diagnosis to transplantation was shorter in the transplant tourist group than in the domestic recipient group (2.5 vs 3.8 years, P = 0.042). Most tourist and domestic kidney recipients developed post-transplant malignancies within 2 to 5 years (Table 4), and the 2 groups had similar mean follow-up times (3.68 vs 3.56 years).
TABLE 3.
Pathology of Overall Pre-Transplant and Post-Transplant Malignancy of Renal Transplant Recipients From 1999 to 2009
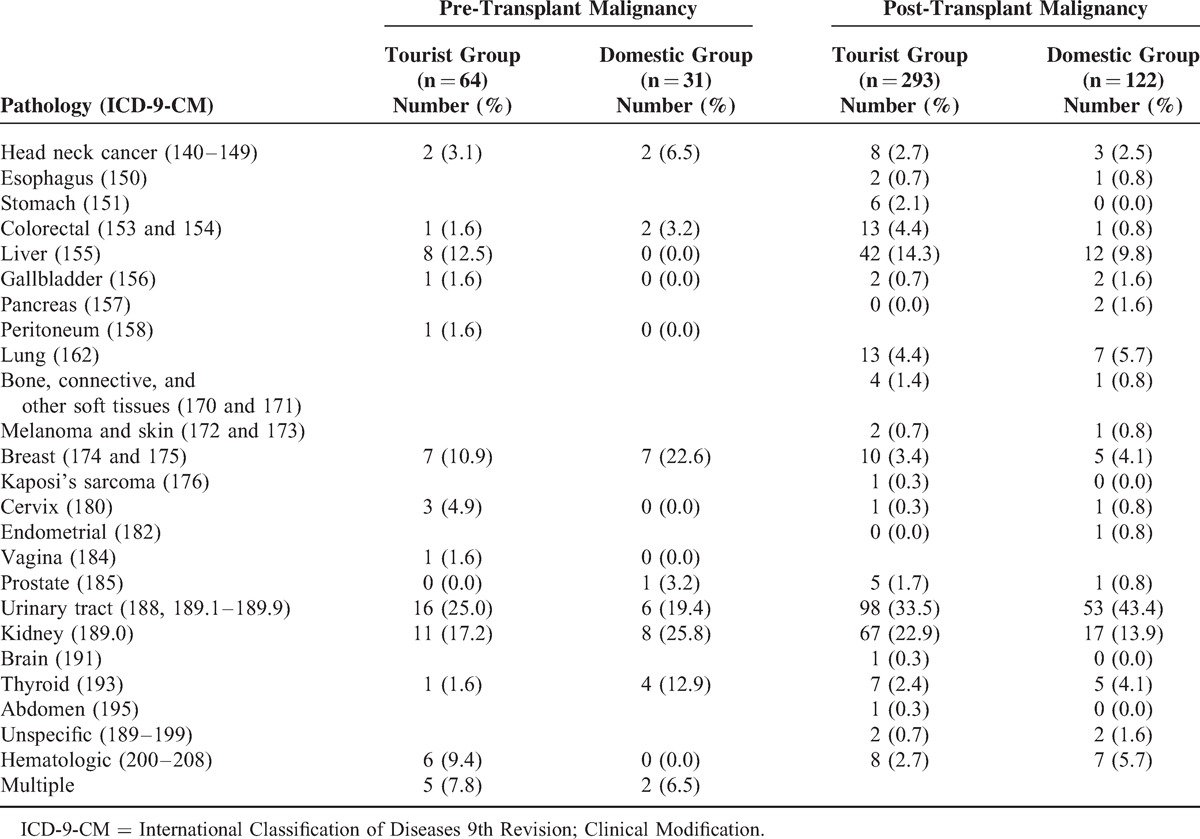
TABLE 4.
Time Relationship of Pre-Transplant and Post-Transplant Malignancy With Kidney Transplant From 1999 to 2009
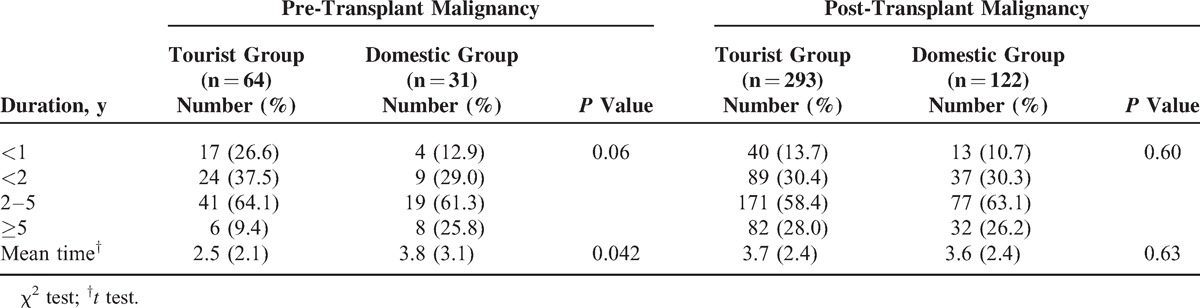
Types and Time Relationship of Kidney Transplants for Recurrent Malignancies
Urinary tract cancer was the most common among the 10 recurrent cancers. Six cancers occurred in the transplant tourists and the other 4 occurred in the domestic kidney recipients. The 10 cancers included 5 urinary tract cancers, 3 kidney cancers, 1 breast cancer, and 1 thyroid cancer. Four of the recurrent cancers occurred within a waiting period of 1 year, and 6 occurred within 2 years (data not shown).
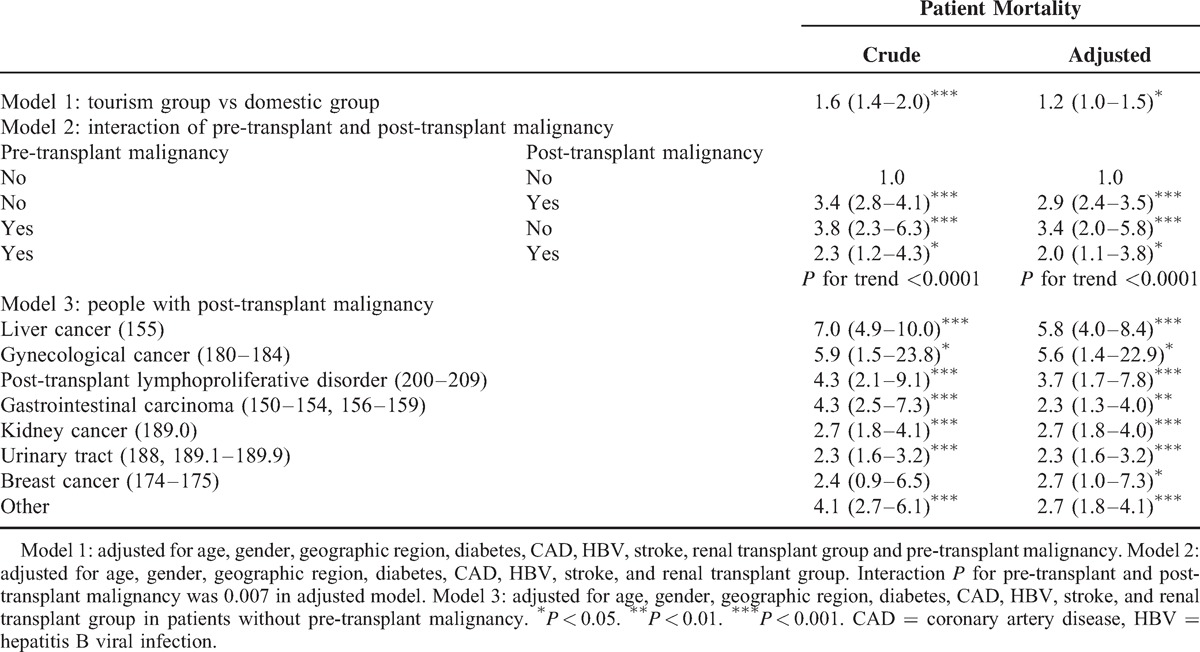
Mortality and Risk of Death
The median follow-up durations were 6.0 and 5.0 years in the tourist and domestic groups, respectively. Kaplan–Meier survival analysis revealed that the transplant tourists had significantly worse survival than the domestic kidney recipients (log-rank P < 0.0001, Figure 2A). Furthermore, the mortality risk between the 2 groups was statistically significant after age, gender, geographic location, diabetes, CAD, HBV, stroke, renal transplant group, and pre-transplant malignancy were controlled (log-rank P < 0.05, Model 1; Table 5). Compared with the subjects without pre-transplant and post-transplant malignancies, the mortality risks were increased in those with pre-transplant and post-transplant malignancies and in those with both malignancies after age, gender, geographic region, diabetes, CAD, HBV, stroke, and tourist/domestic group were controlled (Model 2). We further stratified the subjects with post-transplant malignancies by cancer type to investigate the association between malignancy and mortality risk. Patients with post-transplant liver cancer had significantly higher mortality risk than those without liver cancer (HR = 7.0, 95% CI = 4.9–10.0, Model 3). Similar results were also observed in other cancer types. In addition, no significantly increased risk of graft failure was observed in either the transplant tourist or domestic kidney-recipient groups (P = 0.45, data not shown).
FIGURE 2.
Free probabilities of patient mortality survival for the tourist (solid line) and domestic (dashed line) groups.
TABLE 5.
Adjusted Hazard Ratio by Cox Proportional Hazard Model of Effect of Tourist Group, Pre-Transplant and Post-Transplant Malignancy (Overall/Different Types) on Patient Mortality
DISCUSSION
This study involves the largest cohort in the investigation of transplant tourists. Compared with domestic kidney recipients, transplant tourists showed a significantly higher post-transplant de novo malignancy incidence and mortality risk. The occurrence of malignancy both prior to and after transplant was associated with worse patient survival.
In the present analyses, transplant tourists were significantly older and had higher prevalence rates of diabetes mellitus, hypertension, CAD, CVD, HBV, and even pre-transplant malignancies. This result might be attributed to 2 factors. First, according to the scoring system of receiving deceased donor renal transplants in Taiwan (http://www.torsc.org.tw/assize/assizeWaitKidney.jsp), older patients with more comorbidities might think that they had lower priority to receive deceased renal transplants and seek kidney transplant abroad. Second, we found that transplant tourists with pre-transplant malignancy had a significantly shorter waiting period compared with domestic kidney recipients (2.5 vs 3.8 years, P < 0.05), which indicates that transplant tourists opted to receive kidney transplants abroad to avoid the long waiting period.
A higher percentage of transplant tourists lived in central and southern areas of Taiwan, and a higher percentage of domestic recipients lived in the northern area. A total of 27 hospitals support kidney transplant in Taiwan, 12 and 8 of which are located in the northern and central areas, respectively. Six hospitals are in the southern area, and only 1 is in the eastern area. This geographic difference between the tourist and domestic recipients may be because of the unequal medical resources in Taiwan.
Kidney transplantation itself is a significant risk for post-transplant malignancy.14,15 The types of post-transplant malignancy in Taiwan differ from those in Western countries.14–16 In our findings, tourist and domestic recipients exhibited similar types of post-transplant malignancies. Urinary tract cancer was the most common in both recipients, followed by kidney and liver cancers. However, this ranking was different from the results described by Li et al14 who reported that kidney cancer, not urinary tract cancer, is the most common type of malignancy. This difference may be attributed to the exclusive criteria of patients for pre-transplant malignancy recruitment and duration during kidney transplant to post-transplant malignancy in their study. Additionally, other studies in Taiwan have shown that urinary tract cancer develops more frequently than kidney cancer,11,17–19 which is consistent with our study.
Previous studies have reported prevalence rates of 1.7% to 3.6% for pre-transplant malignancy in kidney recipients.20–22 In our study, the prevalence rates of pre-transplant malignancy were 2.7% and 1.6% in tourist and domestic kidney recipients, respectively. For the total of 95 pre-transplant malignancies, the overall cancer recurrence rate was 11% (10 recurrent cancers). High recurrence rates of 19% (4/21) and 15.4% (6/39) were noted for waiting periods of 1 and 2 years, respectively, which suggests that a waiting period that is >2 years could eliminate 60% of recurrent cancer incidence (6/10). Therefore, patients should be clearly educated on this issue to prevent hasty kidney transplants.
Previous studies have reported post-transplant malignancy-related risk factors such as old age, male gender, and history of cancer.23 After adjusting for these factors, the transplant tourists still exhibited a higher incidence of post-transplant de novo malignancy, especially within 2 years. This result might be also attributed to 2 factors. First, we supposed that transplant tourists had more limited and inadequate preoperation malignancy investigations because 2 years was too short to develop cancers and implied that occult malignancy might exist before kidney transplant. Second, donor-derived malignancy may be a problem, but it could not be confirmed in the present study. A previous study24 reported a high transmission rate of donor-transmitted malignancy to recipients. We inferred that the poor socioeconomic status and poor medical care of tourist donors might result in more unknown malignancies and lead to donor-derived malignancy.
The present study showed that transplant tourists had inferior patient survival compared with domestic kidney recipients despite the same quality of post-transplant medical care available for both groups in Taiwan. High rates of infectious and surgical complications were observed in transplant tourists25 in previous meta-analysis, and transplant tourists had more post-transplant malignancy in the present study, all of which might result in higher patient mortality. Notably, we could not estimate how much transplant tourists died shortly or had primary nonfunction kidney graft after transplants abroad, both of which might lead to underestimation on their mortality or graft failure.
Reulen et al26 reported a significantly higher long-term mortality rate for cancer survivors compared with the general population. Death caused by post-transplant malignancy in kidney transplant recipients has gradually increased in recent years.27,28 Pedotti et al29 reported significantly poorer 10-year survival with post-transplant malignancy, and patients with post-transplant lymphoproliferative disorder had the worst survival. Based on our analysis, patients with pre-transplant or/and post-transplant malignancies had significantly increased mortality risks. In particular, patients with liver cancer as their post-transplant malignancy had the worst prognosis.
The limitations of this study are as follows. First, we could not distinguish living related from deceased kidney transplants from our database, which may affect the mortality risk to a certain extent. Second, no detailed information regarding cancer pathologic types, staging, or treatment was available, which may also affect mortality risk. Third, we could not consider all possible confounders, such as smoking, analgesic usage, Chinese herb usage, and decreased hydration, which have been related to urinary tract cancer.19 Fourth, no detailed information on the immunosuppressant use was available, which may be associated with malignancy occurrence, especially mammalian target of rapamycin (mTOR) inhibitor. However, a previous study30 conducted in Taiwan has shown that only minority of kidney transplant recipients use inhibitors of the mammalian target of mTOR. In addition, the difference in the entry date of recruitment for the tourist and domestic groups was approximately 2 to 3 weeks based on the registry for catastrophic illness and the clinical recovery condition for tourist groups. However, regardless of whether the patient is classified under the tourist or domestic group, they must undergo follow-up examinations and apply for the catastrophic illness card to reduce their medical costs. This action is reflected in the similar follow-up times from transplantation and post-malignancy incidence in these 2 groups. Therefore, the validity of the classification and recruitment of these 2 groups was ensured.
In summary, increased post-transplant de novo malignancy occurrence and mortality risk was observed in transplant tourists. Either pre-transplant or post-transplant malignancies were associated with increased mortality risk. Thus, increased malignancy surveillance prior to and after kidney transplant is required, and hospitals should place more emphasis on a sufficient waiting period. The most important thing is transplant tourists should be discouraged because of the possibility of higher post-transplant de novo malignancy occurrence and mortality.
Footnotes
Abbreviations: CAD = coronary artery disease, CVD = cerebrovascular disease, ESRD = end-stage renal disease, HBV = hepatitis B viral infection, HCC = hepatocellular carcinoma, ICD-9-CM = International Classification of Diseases 9th Revision, Clinical Modification, NHIRD = National Health Insurance Research Database.
M-CC and M-JW contributed equally to this work.
This study was funded by the National Sciences Council, Executive Yuan (Grant Nos. DOH 97-HP-1101, 2008-2010 and NSC 101–2314-B-039–025-MY3), China Medical University Hospital (Grant Nos. 1MS1 and DMR-100–027), the Taiwan Department of Health Clinical Trial and Research Center for Excellence (Grant No. DOH100-TD-B-111–004), and the Taiwan Department of Health Cancer Research Center of Excellence (Grant No. DOH100-TD-C-111–005). The funders had no role in study design, data collection and analysis, decision to publish, or manuscript preparation.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.International Summit on Transplant Tourism and Organ Trafficking. The Declaration of Istanbul on Organ Trafficking and Transplant, Tourism. Clin J Am Soc Nephrol 2008; 3:1227–1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tsai DF. Transplant tourism from Taiwan to China: some reflection on professional ethics and regulation. Am J Bioeth 2010; 10:22–24. [DOI] [PubMed] [Google Scholar]
- 3.Shu KH, Wu MJ, Chen CH, et al. Outcome of kidney transplantation using organs from executed prisoners: is it justified beyond the ethical issue? J Chin Med Assoc 2007; 70:193–199. [DOI] [PubMed] [Google Scholar]
- 4.Sun CY, Lee CC, Chang CT, et al. Commercial cadaveric renal transplant: an ethical rather than medical issue. Clin Transplant 2006; 20:340–345. [DOI] [PubMed] [Google Scholar]
- 5.Ghods AJ, Savaj S. Iranian model of paid and regulated living-unrelated kidney donation. Clin J Am Soc Nephrol 2006; 1:1136–1145. [DOI] [PubMed] [Google Scholar]
- 6.Morad Z, Lim TO. Outcome of overseas kidney transplantation in Malaysia. Transplant Proc 2000; 32:1485–1486. [DOI] [PubMed] [Google Scholar]
- 7.Qunibi W, DE, Al-Gain S. Commercially motivated renal transplantation: results in 540 patients transplanted in India. The Living Non-Related Renal Transplant Study Group. Clin Transplant 1997; 11:536–544. [PubMed] [Google Scholar]
- 8.Rizvi SA, Naqvi SA, Zafar MN, et al. Commercial transplants in local Pakistanis from vended kidneys: a socio-economic and outcome study. Transpl Int 2009; 22:615–621. [DOI] [PubMed] [Google Scholar]
- 9.Salahudeen AK, Woods HF, Pingle A, et al. High mortality among recipients of bought living-unrelated donor kidneys. Lancet 1990; 336:725–728. [DOI] [PubMed] [Google Scholar]
- 10.Sever MS, Kazancioglu R, Yildiz A, et al. Outcome of living unrelated (commercial) renal transplantation. Kidney Int 2001; 60:1477–1483. [DOI] [PubMed] [Google Scholar]
- 11.Tsai MK, Yang CY, Lee CY, et al. De novo malignancy is associated with renal transplant tourism. Kidney Int 2011; 79:908–913. [DOI] [PubMed] [Google Scholar]
- 12.Lu JF, Hsiao WC. Does universal health insurance make health care unaffordable? Lessons from Taiwan. Health Aff (Millwood) 2003; 22:77–88. [DOI] [PubMed] [Google Scholar]
- 13.Wang IK, Chang SN, Liao CC, et al. Hypertensive disorders in pregnancy and preterm delivery and subsequent stroke in Asian women: a retrospective cohort study. Stroke 2011; 42:716–721. [DOI] [PubMed] [Google Scholar]
- 14.Li WH, Chen YJ, Tseng WC, et al. Malignancies after renal transplantation in Taiwan: a nationwide population-based study. Nephrol Dial Transplant 2012; 27:833–839. [DOI] [PubMed] [Google Scholar]
- 15.Vajdic CM, McDonald SP, McCredie MR, et al. Cancer incidence before and after kidney transplantation. J Am Med Assoc 2006; 296:2823–2831. [DOI] [PubMed] [Google Scholar]
- 16.Kasiske BL, Snyder JJ, Gilbertson DT, et al. Cancer after kidney transplantation in the United States. Am J Transplant 2004; 4:905–913. [DOI] [PubMed] [Google Scholar]
- 17.Chiang YJ, Wang HH, Liu KL, et al. Hepatocellular carcinoma following renal transplantation: experience in northern Taiwan. Transplant Proc 2008; 40:2397–2399. [DOI] [PubMed] [Google Scholar]
- 18.Feng WW, Wang TN, Chen HC, et al. Malignancies after renal transplantation in southern Taiwan: experience in one centre. BJU Int 2007; 99:825–829. [DOI] [PubMed] [Google Scholar]
- 19.Wu MJ, Lian JD, Yang CR, et al. High cumulative incidence of urinary tract transitional cell carcinoma after kidney transplantation in Taiwan. Am J Kidney Dis 2004; 43:1091–1097. [DOI] [PubMed] [Google Scholar]
- 20.Chapman JR, Sheil AG, Disney AP. Recurrence of cancer after renal transplantation. Transplant Proc 2001; 33:1830–1831. [DOI] [PubMed] [Google Scholar]
- 21.Kauffman HM, Cherikh WS, McBride MA, et al. Transplant recipients with a history of a malignancy: risk of recurrent and de novo cancers. Transplant Rev 2005; 19:55–64. [Google Scholar]
- 22.Pfeffer PF, Leivestad T, Albrechtsen D, et al. Anamnestic cancer: how long should the cancer-free interval be before renal transplantation? Transplant Proc 1997; 29:3163. [DOI] [PubMed] [Google Scholar]
- 23.Kauffman HM, Cherikh WS, McBride MA, et al. Post-transplant de novo malignancies in renal transplant recipients: the past and present. Transplant Int 2006; 19:607–620. [DOI] [PubMed] [Google Scholar]
- 24.Buell JF, Beebe TM, Trofe J, et al. Donor transmitted malignancies. Ann Transplant 2004; 9:53–56. [PubMed] [Google Scholar]
- 25.Sajjad I, Baines LS, Patel P, et al. Commercialization of kidney transplants: a systematic review of outcomes in recipients and donors. Am J Nephrol 2008; 28:744–754. [DOI] [PubMed] [Google Scholar]
- 26.Reulen RC, Winter DL, Frobisher C, et al. Long-term cause-specific mortality among survivors of childhood cancer. J Am Med Assoc 2010; 304:172–179. [DOI] [PubMed] [Google Scholar]
- 27.Briggs JD. Causes of death after renal transplantation. Nephrol Dial Transplant 2001; 16:1545–1549. [DOI] [PubMed] [Google Scholar]
- 28.Howard RJ, Patton PR, Reed AI, et al. The changing causes of graft loss and death after kidney transplantation. Transplantation 2002; 73:1923–1928. [DOI] [PubMed] [Google Scholar]
- 29.Pedotti P, Cardillo M, Rossini G, et al. Incidence of cancer after kidney transplant: results from the North Italy transplant program. Transplantation 2003; 76:1448–1451. [DOI] [PubMed] [Google Scholar]
- 30.Tsai SF, Cheng CY, Shu KH, et al. Trends in maintenance immunosuppressive drugs used in taiwanese kidney transplant recipients: an analysis of the national health insurance research database. Transplant Proc 2012; 44:190–192. [DOI] [PubMed] [Google Scholar]


