Abstract
This article aims to compare the risks of depression and anxiety in patients with ankylosing spondylitis (AS) and nonradiographic axial spondyloarthritis (nr-axSpA) and investigate the relationship among self-reported outcome measures, clinical parameters, and physical variables of patients with axSpA.
Patients with axSpA were recruited from Erciyes Spondyloarthritis Cohort. The patients met Assessment of Spondyloarthritis International Society classification criteria for axial SpA and were assessed in a cross-sectional study design for visual analog scale (VAS) pain, Bath Ankylosing Spondylitis Disease Activity Index (BASDAI), Bath Ankylosing Spondylitis Functional Index (BASFI), Ankylosing Spondylitis Quality of Life questionnaire (ASQoL), and Ankylosing Spondylitis Disease Activity Score–C-reactive protein (ASDAS-CRP). Psychological status was evaluated using the hospital anxiety and depression scale (HADS). Multivariate logistic regression analysis was applied to determine the associations between psychological variables and clinical parameters after adjusting for confounding variables.
Of the 316 patients (142 nr-axSpA, 174 AS), 139 (44%) had high risk for depression (HADS-D score ≥7) and 71 (22.5%) for anxiety (HADS-A score ≥10). HADS-D and HADS-A scores were similar between patients with AS and nr-axSpA. Patients with high risk for depression and anxiety had higher scores in BASDAI, BASFI, and ASDAS-CRP, and also poorer scores in VAS pain and ASQoL. Multivariate logistic regression analysis showed that the ASDAS-CRP, ASQoL, BASDAI, as well as educational level were factors associated with the risk of depression whereas the ASQoL and educational level were factors associated with the risk of anxiety.
Patients with nr-axSpA and AS have similar burden of psychological distress. The quality of life (ASQoL) and educational level were factors associated with the risk of both depression and anxiety whereas disease activity (BASDAI and ASDAS-CRP) was the independent risk factor associated with depression but not anxiety in axSpA. These findings suggest that psychological status should be examined while assessing patients with axSpA including AS and nr-axSpA.
INTRODUCTION
Axial spondyloarthritis (axSpA) is a chronic progressive inflammatory disease characterized by predominant involvement of the axial skeleton. The concept of axSpA embraces the nonradiographic axial SpA (nr-axSpA) (without definitive radiographic sacroiliitis on x-ray examination) and ankylosing spondylitis (AS) (with radiographic sacroiliitis according to the modified New York criteria).1
In axSpA, inflammatory low back pain is the leading symptom and a significant number of patients might have structural damage or radiographic progression resulting in loss of lumbar lordosis, thoracic kyphosis, reduced spinal mobility, compensatory hip flexion deformities, or restriction in chest wall motion. Moreover, several symptoms and clinical features (ie, reduced spinal mobility, stiffness, pain, and fatigue) may significantly contribute to the functional impairment, reduced quality of life, sleep disturbances, workforce decline, and psychological distress especially depression and anxiety.2–5 Because of the fact that axSpA usually starts in early adulthood (<45 years), the impact of the disease on different aspects of life (career, family, and social life) can be considerably lifelong.
Psychological distress including depressive and anxiety symptoms is frequently reported in patients with various rheumatic disorders and is considered to be important with regard to outcome measurements. For instance, the reported prevalence of depression in AS changes between 20% to 55.5%.6,7
Until now, a few studies have reported a significant association between the psychological status and functional limitation, health-related quality of life, and disease activity in AS.3,4,8,9 Additionally, a number of studies have highlighted significant differences in several clinical aspects including baseline characteristics (gender distribution, human leukocyte antigen B27), functional impairment, spinal mobility, level of inflammatory markers (C-reactive protein [CRP] or erythrocyte sedimentation rate [ESR]), spinal inflammation, and radiographic damage between patients with nr-axSpA and AS.10–12 According to those studies, functional impairment (assessed by Bath Ankylosing Spondylitis Functional Index [BASFI]), spinal mobility (assessed by Bath Ankylosing Spondylitis Metrology Index [BASMI]), as well as spinal inflammation tended to be less severe in patients with nr-axSpA than AS, despite having similar disease activity status. However, to the best of our knowledge, no prior study compared the psychological status of patients with AS and nr-axSpA. Therefore, the aim of this study was to compare the depression and anxiety risks in patients with AS and nr-axSpA and investigate the associations among self-reported outcome measures, clinical parameters, and physical variables of patients with axSpA.
MATERIALS AND METHODS
Patients with axSpA were recruited from Erciyes Spondyloarthritis Cohort between 2009 and 2014. This cohort consisted of patients who were consecutively included from our outpatient clinic and who met Assessment of Spondyloarthritis International Society classification criteria for axSpA.1 All of the recruited patients were evaluated for evidence of radiographic sacroiliitis. In order to reduce bias, digital sacroiliac (SI) joint radiographs were anonymized by using picture archiving and communication system software and blindly evaluated by 3 rheumatologists. A radiograph of the SI joints was marked positive for sacroiliitis if 2 of 3 readers agreed according to the modified New York criteria. Patients without definite radiographic sacroiliitis on x-ray examination were defined as nr-axSpA and patients with definite radiographic sacroiliitis according to the modified New York criteria were defined as AS. The study protocol was approved by the local Ethics Committee of our institution. Demographic characteristics and anthropometric measurements were evaluated in all patients.
All of the assessments including the anthropometric measurements were made by the same physician (G.K.) and standardized case report forms were filled out. Clinical assessments, blood sampling, and questionnaires were done within 2 days of enrollment and the baseline values were used in the analyses.
Assessment of Disease Status
Disease activity was assessed by using ASDAS-CRP and the Turkish version of Bath Ankylosing Spondylitis Disease Activity Index (BASDAI).13,14 The Turkish versions of BASFI and Ankylosing Spondylitis Quality of Life questionnaire (ASQoL) were used to assess functional status and quality of life.15,16 Spinal limitation was assessed by using the BASMI.17 ESR (mm/h) and CRP (mg/L) levels were also obtained.
Assessment of Psychological Status
Psychological status was evaluated by using Hospital Anxiety and Depression Scale (HADS) including the depression (HADS-D) and anxiety (HADS-A) subscales.18 This is a Likert-type self-reported scale that comprises 14 items: 7 items for depression symptoms and the 7 items for anxiety symptoms. Each item is scored between 0 (no distress) and 3 (maximum distress) and higher scores reflect greater level of depression or anxiety risk. HADS can be used efficiently to identify cognitive processes independent of somatic symptoms associated with anxiety or depressive in the general population. Also, the scale is easy to apply in clinical practice and takes only a few minutes.19 The HADS was developed by Zigmond and Snaith.18 Until now, the HADS has been translated into various languages including Arabic, Chinese, Danish, Turkish, Dutch, Finnish, French, German, Hebrew, Hungarian, Italian, Japanese, Korean, Norwegian, Portuguese, Spanish, Swedish, Thai, and Urdu. The HADS has been widely used in various patient population (patients with cancer, traumatic brain injury, cardiac disorders, stroke, intellectual disabilities, hepatitis, diabetes mellitus, epilepsy, chronic obstructive pulmonary disease, Parkinson disease, chronic pain, amputations, spinal cord injury, and several rheumatic diseases).19 A number of previous studies assessed psychometric properties of HADS.20 According to most of those studies HADS has good reliability and validity as indicated by high internal consistency (Cronbach α) ranging from 0.68 to 0.93 for the anxiety and 0.67 to 0.90 for the depression subscales and good discriminative ability for assessing anxiety and depression.20,21 Score for each subscale (anxiety and depression) can range from 0 to 21. Scores for the entire scale (emotional distress) range from 0 to 42.
The validity and reliability of the Turkish version was determined by Aydemir et al.22 We used a cut-off point of ≥10 to define the anxiety subgroup, and ≥7 to define the depressed subgroup as reported by Aydemir et al.22
STATISTICAL ANALYSIS
Statistical analysis was performed using Statistical Package for Social Sciences (SPSS 20.0; IBM, Armonk, NY) software. Results are expressed as mean ± standard deviations or percentages unless indicated otherwise. The normal distribution of variables was tested by the Kolmogorov–Smirnov test. Subgroup comparisons of patients with nr-axSpA and AS were performed using t test. Differences in categorical variables were assessed by the χ2 or Fisher exact test. Relationship between parameters (all were normally distributed) was analyzed by using Pearson correlation coefficients. The variables that were biologically meaningful (such as demographics or having nr-axSpA or AS) or that had a P value <0.25 on univariate analysis were subjected to a stepwise multivariate logistic regression analysis to determine which factors were independent predictors of depression or anxiety risk in patients with axial SpA.23 Adjusted odds ratios were recorded with a 95% confidence interval for each. Unless stated otherwise, statistical significance was set at a P value of <0.05.
RESULTS
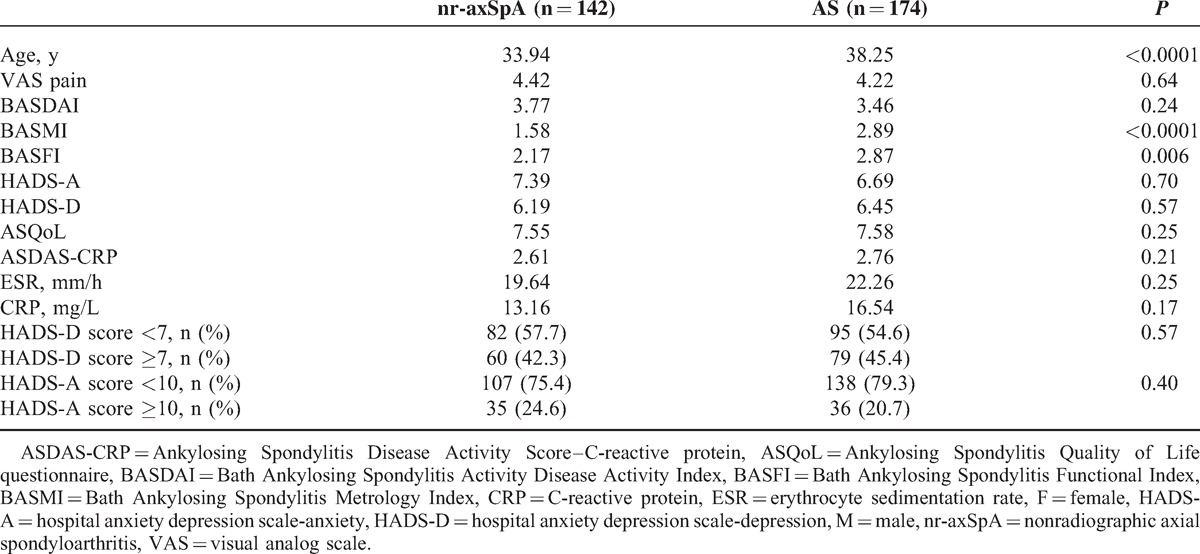
Demographic and clinical characteristics of the patients (199 M, 117 F) with axSpA are given in Table 1. Of the 316 patients (142 nr-axSpA, 174 AS) with axial SpA, 139 (44%) had high risk for depression and 71 (22.5%) for anxiety. There was no significant difference in HADS-D and HADS-A scores, and the percentages of patients with higher risks of depression/anxiety between AS and nr-axSpA (Table 2). Patients having a high risk of depression were predominantly female (58.3%) in the nr-axSpA group whereas predominantly male (72.2%) in the AS group. Patients having a high risk of anxiety were predominantly female (57.1%) in the nr-axSpA group whereas predominantly male (69.4%) in the AS group. Comparison between the subgroups of nr-axSpA and AS for the measured parameters is shown in Table 2.
TABLE 1.
Demographic Characterizations, Clinical Parameters, and Laboratory Result of the Patients With Axial Spondyloarthritis (Mean ± SD)
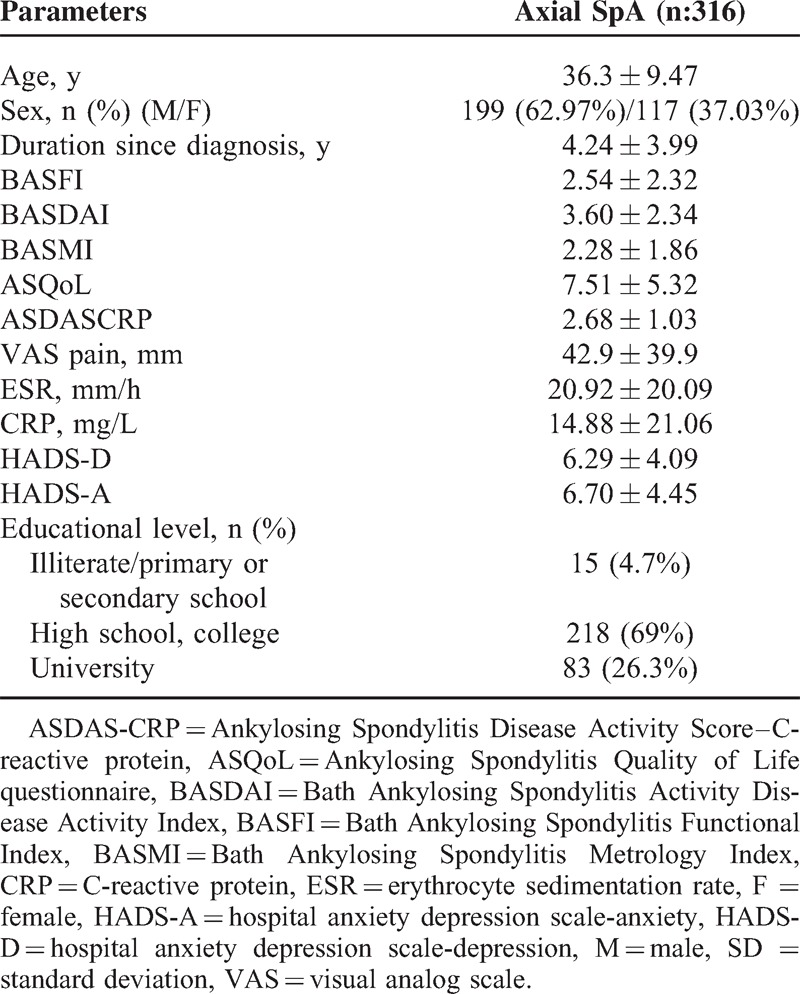
TABLE 2.
Comparison Between Nonradiographic Axial Spondyloarthritis and Ankylosing Spondylitis Groups for the Measured Parameters
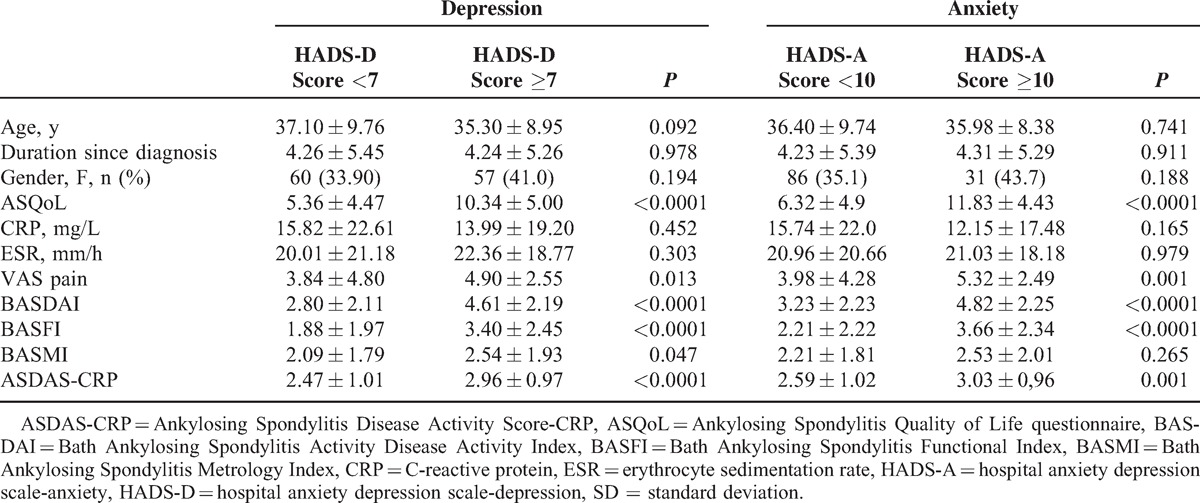
Patients having high risks of depression (HADS-D score ≥7) and anxiety (HADS-A score ≥10) had higher scores in BASDAI, BASFI, and ASDAS-CRP, and also poorer scores in visual analog scale (VAS) pain and ASQoL. Clinical and laboratory results of axSpA patients with and without depression/anxiety are given in Table 3.
TABLE 3.
Clinical and Laboratory Results in Patients With Axial Spondyloarthritis With and Without Depression or Anxiety (Mean ± SD)
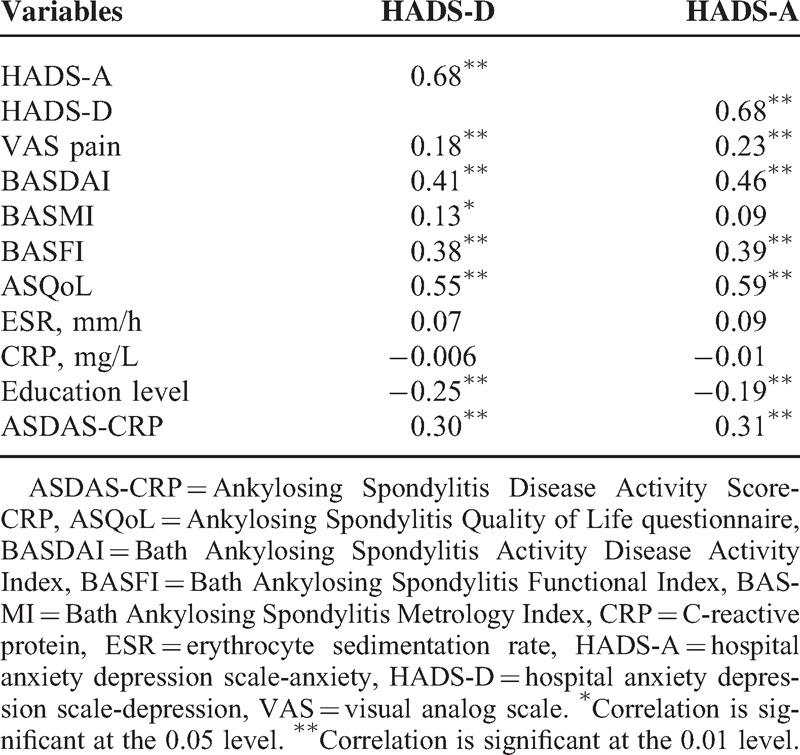
Both HADS-D and HADS-A scores positively correlated with ASQoL, BASDAI, BASFI, VAS pain, and ASDAS-CRP but not with acute phase reactants (CRP and ESR). Furthermore, educational level of the patients had negative correlations with HADS-D and HADS-A scores. The correlation coefficients are shown in Table 4.
TABLE 4.
Correlation Between the Psychological Scores and the Clinical and Laboratory Results in Patients With Axial Spondyloarthritis
Multivariate logistic regression analysis revealed that ASDAS-CRP, ASQoL, BASDAI, and education level were independent risk factors associated with the risk of depression (Table 5) whereas the ASQoL and educational level were the independent risk factors associated with the risk of anxiety (Table 5). Having nr-axSpA or AS did not seem to be an independent risk factor for either depression or anxiety. This was analyzed by entering this subgrouping variable into the multivariate regression analysis as a potential factor for the risk of depression or anxiety.
TABLE 5.
ORs and 95% CIs for the Factors Influencing Depression and Anxiety Risk in Patients With Axial Spondyloarthritis

DISCUSSION
To our knowledge, this is the first study assessing the psychological status in axial SpA and comparing the patients with AS and nr-axSpA. The results of this study revealed that patients with nr-axSpA and AS have similar burden of psychological distress. Also multivariate logistic regression analysis showed that disease activity, quality of life, and educational level were factors associated with the risk of depression or anxiety in axSpA. The psychological variables, specifically depression and anxiety, had close relationship with disease activity, functional limitations, and quality of life in patients with axSpA.
Major depression is prevalent in patients with chronic medical illnesses and it is associated with increased health-risk behavior such as overeating, sedentary lifestyle, and smoking, which may also increase the risk of incidence of medical illnesses.24 Chronic medical diseases may contribute to the development of physiologic distress, functional impairment, indirect pathophysiologic effects (increased cytokine levels or other inflammatory factors), or changes in biologic variables (eg, activation of hypothalamic–pituitary–adrenal axis and autonomic nervous system).25–27 Several studies have also reported the negative impact of depression and/or anxiety on chronic medical diseases, including poor adherence to self-care regimens (diet, exercise, and quitting smoking) and medical treatment recommendations. Depression and anxiety were also found to be risk factors for increased burden of physical symptom, decreased quality of life, poorer treatment outcomes, repeated medication changes, or polypharmacy as well as increased health care costs in patients with chronic medical diseases.24–28
The impact of chronic rheumatic disease on the physiologic status is an important concern for both research and clinical care. Psychological distress including depression and anxiety symptoms is more common (about 2-fold) in patients with rheumatic diseases when compared with the general population.26 The course of axSpA is usually progressive and leads to poorer health-related quality of life (ie, fatigue, sleep disturbances, stiffness, and chronic pain), functional impairment, workforce decline, and psychological distress especially depression and anxiety over time.
Psychological distress is important in determining the outcome in patients with AS. Until now, a few studies showed that there was a close association between physiologic status and measures of self-reported disease activity, functional status, and health-related quality of life in AS.3,4,8,9 In a longitudinal study of 89 patients with AS, Martindale et al3 reported that disease status scores including BASDAI, BASFI, and BASMI were significantly correlated with anxiety, depression, internality, and health status. However, in those studies, demographic and medical variables that had significant effects on psychological factors were not assessed by multivariate analysis and relatively small sample sizes were used. Brionez et al4,8 assessed the role of psychological factors in self-reported disease activity and functional limitation in a sample of 294 patients with AS by controlling for demographic and medical variables within 2 separate studies. They found that there was a significant correlation between BASDAI/BASFI and psychological variables including arthritis helplessness, passive coping, and depression. However, in those studies, the impact of anxiety on self-reported measures was not assessed. Baysal et al9 examined the impact of anxiety and depression (measured by HADS) on both disease activity and quality of life in 243 patients with AS. They indicated that HADS-D, HAQ-S, VAS pain score, and ESR were independent risk factors for higher anxiety scores but that HADS-A and ASQoL were independent risk factors for higher depression scores. However, they did not assess ASDAS-CRP that is currently being used as an outcome measure, already taking the place of BASDAI.
Findings from our cohort indicated that both HADS-D and HADS-A scores correlated with BASDAI, BASFI, ASQoL, VAS pain, and ASDAS-CRP in axSpA. BASMI scores correlated only with HADS-D scores but with lowest coefficients. In contrast, there was no significant correlation between psychological status of the patients and the inflammatory markers. These findings are noteworthy and indicate that BASDAI, BASFI, and ASQoL (widely used patient-reported outcome measures) may be influenced by the psychological variables. Therefore, clinicians should also be advised to take into account the psychological status of their patients with axSpA while assessing the self-reported outcome measures.
In our study, ASDAS-CRP was shown to be an independent risk factor for depression. This finding is also important since ASDAS is a composite disease activity index that contains patient-reported outcome data (BASDAI: back pain, peripheral pain/swelling morning stiffness, and patient's global assessment) and also objective signs of inflammation (ESR or CRP). The ASQoL, a disease-specific quality-of-life questionnaire, has also been shown to be closely associated with the psychological status.
According to the study by Bjelland et al,29 there is a significant association between low educational level and the anxiety/depression measures. Similarly, we observed that the educational level of the patients had a negative correlation with both HADS-D and HADS-A scores. Furthermore, lower education level was an independent risk factor for anxiety and depression in patients with axSpA. Higher educational level may be associated with better socioeconomic status and coping ability with disease-related problems. Previous study by Roussou et al30 showed that patients from higher occupational group had less disease activity, lower pain, and depression than patients from the lowest occupational group. Unfortunately, we did not assess the occupational or socioeconomic status of the patients in our study and this may be considered as a limitation.
In this study, we confirmed a similar burden of disease activity as measured by the BASDAI and ASDAS-CRP between patients with AS and nr-axSpA. However, functional limitation (BASFI) and spinal mobility (BASMI) were less impaired in patients with nr-axSpA compared with patients having AS. In accordance with the previous studies,10,11,31 the nr-axSpA population enrolled in this study was younger and had a greater proportion of women compared with the AS population. Health-related quality of life (ASQoL), educational levels, and levels of acute-phase reactants (CRP and ESR) in patients with nr-axSpA and AS were similar. Interestingly, we showed, for the first time, that there was no major differences concerning the risk of anxiety and depression between patients with AS and nr-axSpA. Based on these results, we suggest that patients with nr-axSpA and AS may have similar burden of psychological distress.
Our study also has some limitations. Because of the cross-sectional design of this study, it is difficult to discern whether the burden of psychological distress is a consequence of the adverse impact of the disease-related problems, underlying inflammatory processes, or other factors associated with having a chronic disease in axSpA. Moreover, we could not assess the psychometric variables and personality characteristics of the patients in a more detailed way.
In conclusion, patients with nr-axSpA and AS have similar burden of psychological distress. ASDAS-CRP, ASQoL, BASDAI, and educational level are associated with psychological distress in patients with axSpA. Therefore, psychological status should not be overlooked in the assessment of patients with axSpA.
Footnotes
Abbreviations: AS = Ankylosing spondylitis, ASDAS-CRP = Ankylosing Spondylitis Disease Activity Score-CRP, ASQoL = Ankylosing Spondylitis Quality of Life questionnaire, axSpA = Axial spondyloarthritis, BASDAI = Bath Ankylosing Spondylitis Disease Activity Index, BASFI = Bath Ankylosing Spondylitis Functional Index, BASMI = Bath Ankylosing Spondylitis Metrology Index, CRP = C-reactive protein, ESR = erythrocyte sedimentation rate, HADS-A = hospital anxiety depression scale-anxiety, HADS-D = hospital anxiety depression scale-depression, nr-axSpA = nonradiographic axial spondyloarthritis, SI = sacroiliac, VAS = visual analog scale.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Rudwaleit M, van der Heijde D, Landewe R, et al. The development of Assessment of Spondyloarthritis International Society classification criteria for axial spondyloarthritis (part II): validation and final selection. Ann Rheum Dis 2009; 68:777–783. [DOI] [PubMed] [Google Scholar]
- 2.Li Y, Zhang S, Zhu J, et al. Sleep disturbances are associated with increased pain, disease activity, depression, and anxiety in ankylosing spondylitis: a case-control study. Arthritis Res Ther 2012; 14:R215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Martindale J, Smith J, Sutton CJ, et al. Disease and psychological status in ankylosing spondylitis. Rheumatology (Oxford) 2006; 45:1288–1293. [DOI] [PubMed] [Google Scholar]
- 4.Brionez TF, Assassi S, Reveille JD, et al. Psychological correlates of self-reported functional limitation in patients with ankylosing spondylitis. Arthritis Res Ther 2009; 11:R182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ozgul A, Peker F, Taskaynatan MA, et al. Effect of ankylosing spondylitis on health-related quality of life and different aspects of social life in young patients. Clin Rheumatol 2006; 25:168–174. [DOI] [PubMed] [Google Scholar]
- 6.Barlow JH, Macey SJ, Struthers GR. Gender, depression, and ankylosing spondylitis. Arthritis Care Res 1993; 6:45–51. [DOI] [PubMed] [Google Scholar]
- 7.Hakkou J, Rostom S, Aissaoui N, et al. Psychological status in Moroccan patients with ankylosing spondylitis and its relationships with disease parameters and quality of life. J Clin Rheumatol 2011; 17:424–428. [DOI] [PubMed] [Google Scholar]
- 8.Brionez TF, Assassi S, Reveille JD, et al. Psychological correlates of self-reported disease activity in ankylosing spondylitis. J Rheumatol 2010; 37:829–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baysal O, Durmus B, Ersoy Y, et al. Relationship between psychological status and disease activity and quality of life in ankylosing spondylitis. Rheumatol Int 2011; 31:795–800. [DOI] [PubMed] [Google Scholar]
- 10.Rudwaleit M, Haibel H, Baraliakos X, et al. The early disease stage in axial spondylarthritis: results from the German Spondyloarthritis Inception Cohort. Arthritis Rheum 2009; 60:717–727. [DOI] [PubMed] [Google Scholar]
- 11.Kiltz U, Baraliakos X, Karakostas P, et al. Do patients with non-radiographic axial spondylarthritis differ from patients with ankylosing spondylitis? Arthritis Care Res 2012; 64:1415–1422. [DOI] [PubMed] [Google Scholar]
- 12.Wallis D, Haroon N, Ayearst R, et al. Ankylosing spondylitis and nonradiographic axial spondyloarthritis: part of a common spectrum or distinct diseases? J Rheumatol 2013; 40:2038–2041. [DOI] [PubMed] [Google Scholar]
- 13.van der Heijde D, Lie E, Kvien TK, et al. ASDAS, a highly discriminatory ASAS-endorsed disease activity score in patients with ankylosing spondylitis. Ann Rheum Dis 2009; 68:1811–1818. [DOI] [PubMed] [Google Scholar]
- 14.Akkoc Y, Karatepe AG, Akar S, et al. A Turkish version of the Bath Ankylosing Spondylitis Disease Activity Index: reliability and validity. Rheumatol Int 2005; 25:280–284. [DOI] [PubMed] [Google Scholar]
- 15.Duruoz MT, Doward L, Turan Y, et al. Translation and validation of the Turkish version of the Ankylosing Spondylitis Quality of Life (ASQOL) questionnaire. Rheumatol Int 2013; 33:2717–2722. [DOI] [PubMed] [Google Scholar]
- 16.Yanik B, Gursel YK, Kutlay S, et al. Adaptation of the Bath Ankylosing Spondylitis Functional Index to the Turkish population, its reliability and validity: functional assessment in AS. Clin Rheumatol 2005; 24:41–47. [DOI] [PubMed] [Google Scholar]
- 17.Jenkinson TR, Mallorie PA, Whitelock HC, et al. Defining spinal mobility in ankylosing spondylitis (AS). The Bath AS Metrology Index. J Rheumatol 1994; 21:1694–1698. [PubMed] [Google Scholar]
- 18.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983; 67:361–370. [DOI] [PubMed] [Google Scholar]
- 19.Smarr KL, Keefer AL. Measures of depression and depressive symptoms: Beck Depression Inventory-II (BDI-II), Center for Epidemiologic Studies Depression Scale (CES-D), Geriatric Depression Scale (GDS), Hospital Anxiety and Depression Scale (HADS), and Patient Health Questionnaire-9 (PHQ-9). Arthritis Care Res (Hoboken) 2011; 63 Suppl 11:S454–S466. [DOI] [PubMed] [Google Scholar]
- 20.Herrmann C. International experiences with the Hospital Anxiety and Depression Scale: a review of validation data and clinical results. J Psychosom Res 1997; 42:17–41. [DOI] [PubMed] [Google Scholar]
- 21.Bjelland I, Dahl AA, Haug TT, et al. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res 2002; 52:69–77. [DOI] [PubMed] [Google Scholar]
- 22.Aydemir Ö, Güvenir T, Küey L, et al. Validity and Realibility of Turkish Version of Hospital Anxiety and Depression Scale. Turk Psikiyatri Derg 1997; 8:280–287. [Google Scholar]
- 23.Hosmer DW, Lemeshow S, Sturdivant RX. Model-building strategies and methods for logistic regression. Applied Logistic Regression 3rd edHoboken, NJ: John Wiley & Sons; 2013; 1–459. [Google Scholar]
- 24.Katon WJ. Clinical and health services relationships between major depression, depressive symptoms, and general medical illness. Biol Psychiatry 2003; 54:216–226. [DOI] [PubMed] [Google Scholar]
- 25.Katon W, Sullivan M, Walker E. Medical symptoms without identified pathology: relationship to psychiatric disorders, childhood and adult trauma, and personality traits. Ann Intern Med 2001; 134:917–925. [DOI] [PubMed] [Google Scholar]
- 26.Geenen R, Newman S, Bossema ER, et al. Psychological interventions for patients with rheumatic diseases and anxiety or depression. Best Pract Res Clin Rheumatol 2012; 26:305–319. [DOI] [PubMed] [Google Scholar]
- 27.Leonard BE. The concept of depression as a dysfunction of the immune system. Curr Immunol Rev 2010; 6:205–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Katon W, Lin EH, Kroenke K. The association of depression and anxiety with medical symptom burden in patients with chronic medical illness. Gen Hosp Psychiatry 2007; 29:147–155. [DOI] [PubMed] [Google Scholar]
- 29.Bjelland I, Krokstad S, Mykletun A, et al. Does a higher educational level protect against anxiety and depression? The HUNT study. Soc Sci Med 2008; 66:1334–1345. [DOI] [PubMed] [Google Scholar]
- 30.Roussou E, Kennedy LG, Garrett S, et al. Socioeconomic status in ankylosing spondylitis: relationship between occupation and disease activity. J Rheumatol 1997; 24:908–911. [PubMed] [Google Scholar]
- 31.Kilic E, Kilic G, Akgul O, et al. Discriminant validity of the Ankylosing Spondylitis Disease Activity Score (ASDAS) in patients with non-radiographic axial spondyloarthritis and ankylosing spondylitis: a cohort study. Rheumatol Int 2014; [Epub ahead of print]. doi: 10.1007/s00296-014-3168-y. [DOI] [PubMed] [Google Scholar]


